Compass A Provincial Outreach Model to Support Health




- Slides: 25
Compass A Provincial Outreach Model to Support Health Care Providers Caring for Children and Youth with Mental Health and Addiction Concerns Dr Jennifer Russel M. D Child and Adolescent Psychiatrist & Clinical Director Kevin Lorenz, RPN Compass Clinical Nurse Coordinator
Territory Acknowledgment We would like to begin by acknowledging that the land on which we gather is the traditional unceded territory of the Ktunaxa Nation.
Disclosures Nothing to disclose

Overview of Session q Background of Compass q What is Compass? q Case examples q What’s next q How to register q Q&A

BC Children’s Hospital Mental Health VISION All children, youth & their families in BC receive high-quality, evidence-based mental health & substance use services when they need them, regardless of where they live
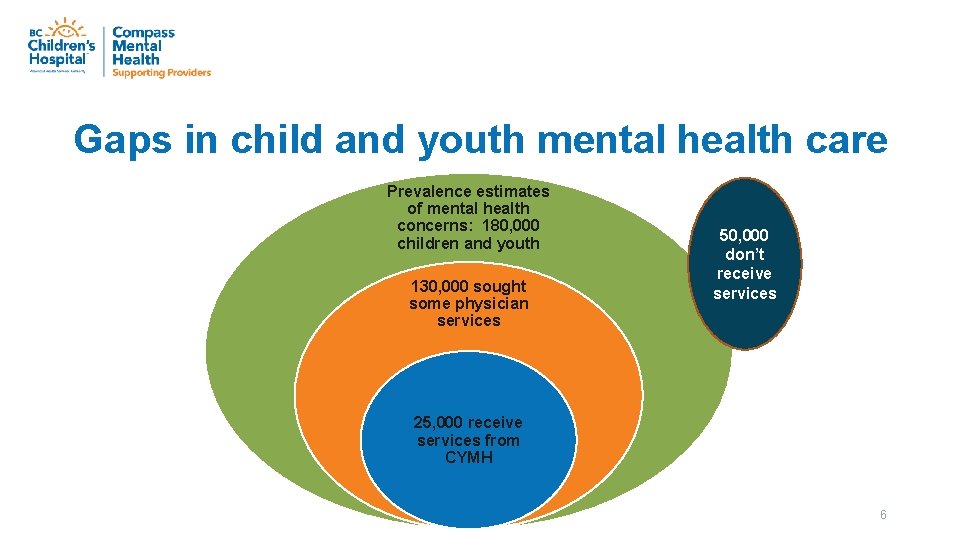
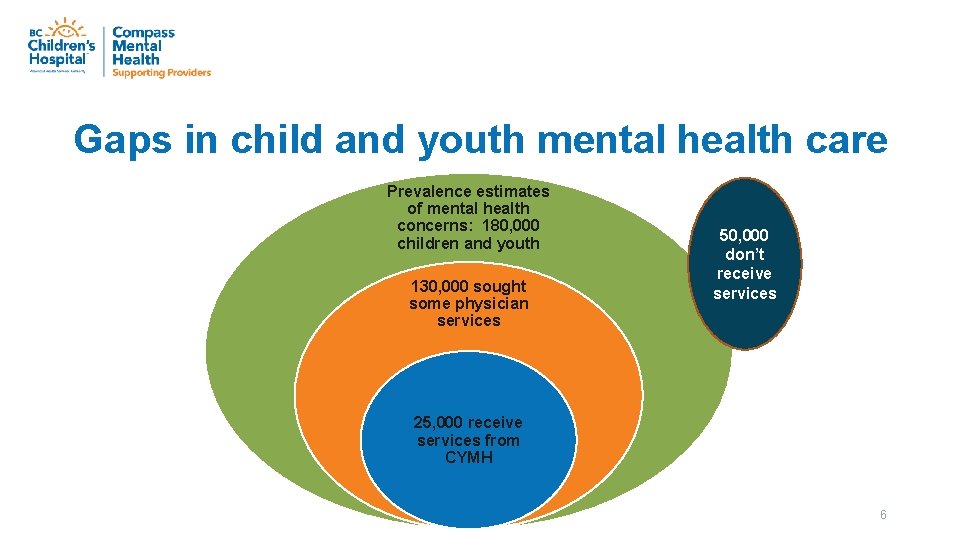
Gaps in child and youth mental health care Prevalence estimates of mental health concerns: 180, 000 children and youth 130, 000 sought some physician services 50, 000 don’t receive services 25, 000 receive services from CYMH 6
About Compass connects community care providers across B. C. to the information, advice and resources they need to provide appropriate and timely mental health and substance use care to children and youth (up to 25 years) close to home.
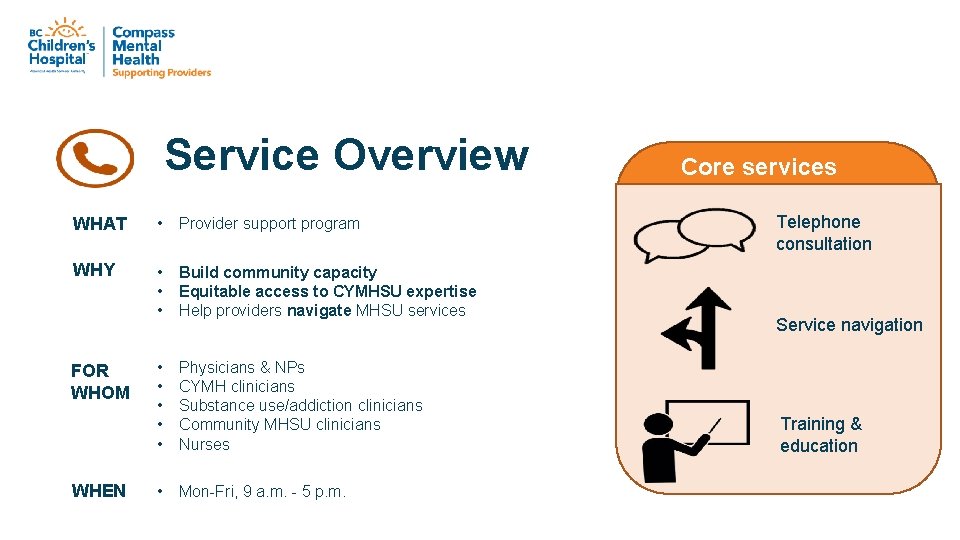
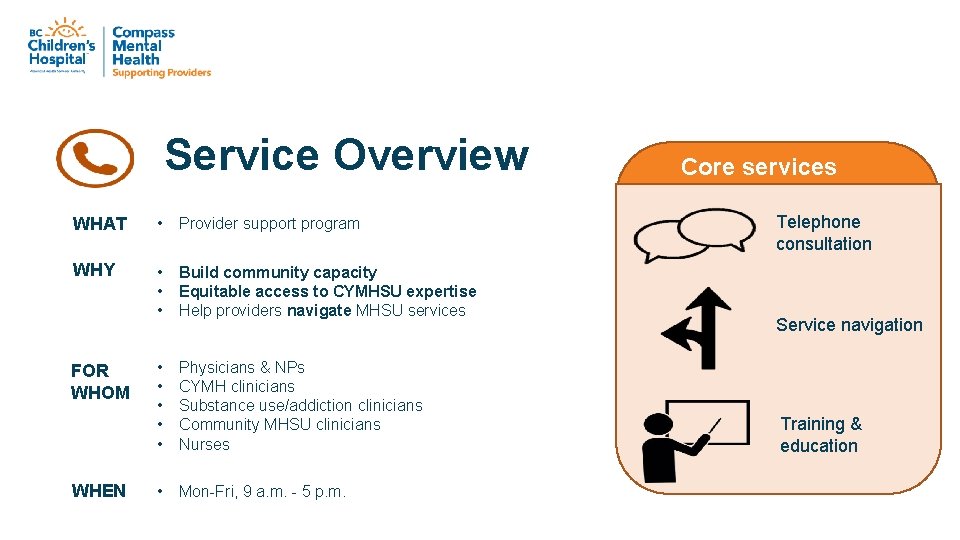
Service Overview WHAT • Provider support program WHY • • • Build community capacity Equitable access to CYMHSU expertise Help providers navigate MHSU services • • • Physicians & NPs CYMH clinicians Substance use/addiction clinicians Community MHSU clinicians Nurses • Mon-Fri, 9 a. m. - 5 p. m. FOR WHOM WHEN Core services Telephone consultation Service navigation Training & education
Service Overview • • • Child & Youth Psychiatrists Mental Heath & Addictions Therapists Addiction Medicine Specialists Care Coordinator Admin Coordinator
Service Overview Guiding Principles • Universal mental health and substance use screening • Validated, evidence-based therapeutic interventions • Consideration of local context & realities (collaboration & co-development) • Family-centred, trauma-informed & culturallysensitive
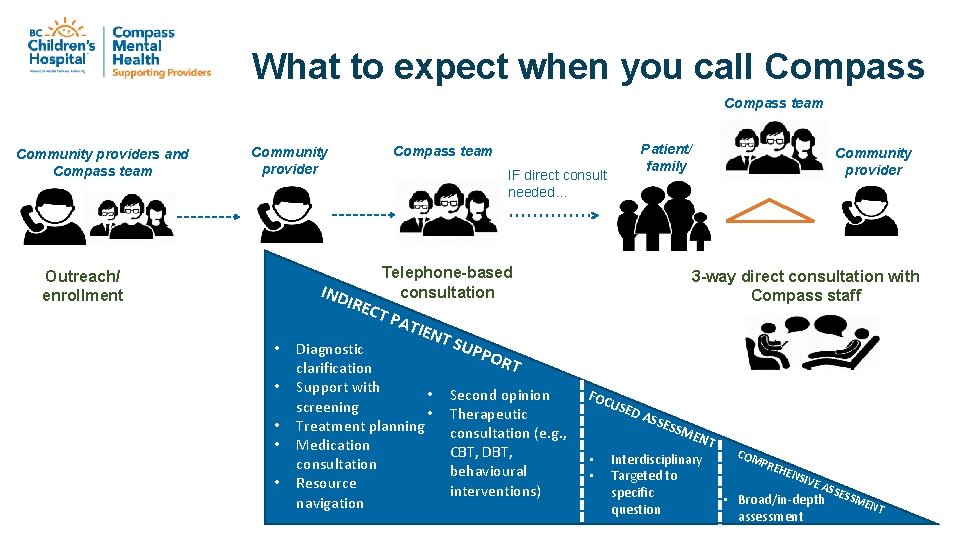
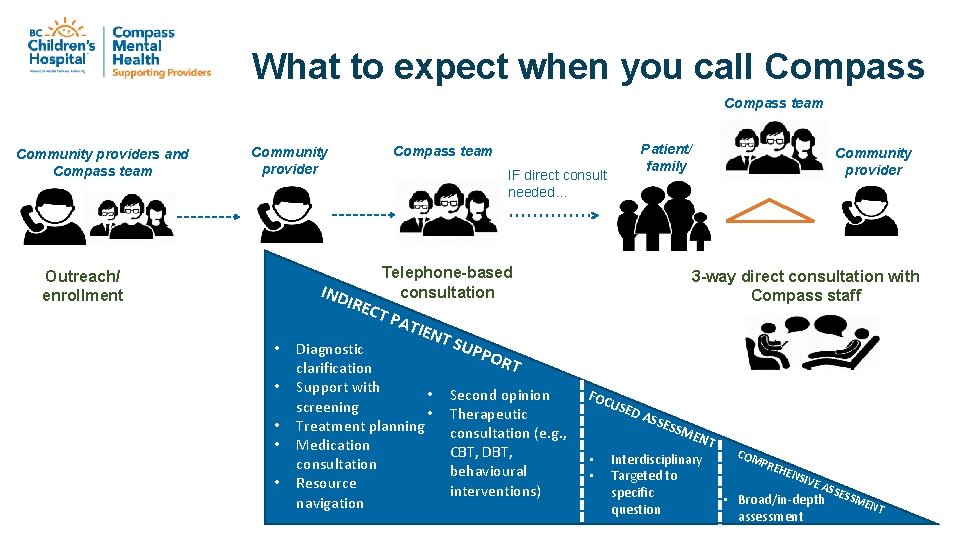
What to expect when you call Compass team Community providers and Compass team Community provider Patient/ family Compass team IF direct consult needed… Telephone-based consultation Outreach/ enrollment 3 -way direct consultation with Compass staff IND IREC T PA • • • TIEN T SU Diagnostic clarification Support with • screening • Treatment planning Medication consultation Resource navigation PPO Community provider RT Second opinion Therapeutic consultation (e. g. , CBT, DBT, behavioural interventions) FOC USE DA SSE • • SSM ENT Interdisciplinary Targeted to specific question COM PRE HEN SIVE ASS • Broad/in-depth assessment ESS MEN T
What we don’t do q Assume direct, ongoing clinical care (Case Management) q Expedite inpatient admissions
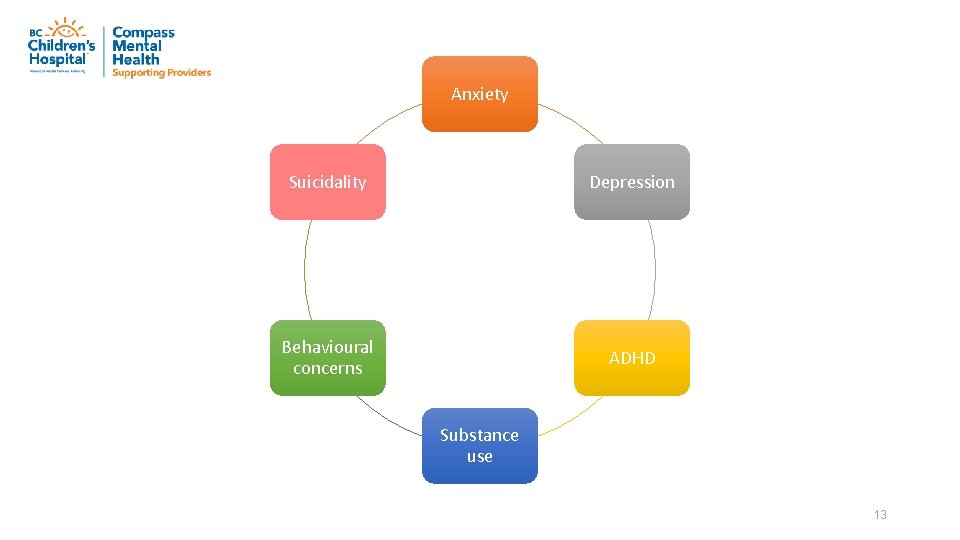
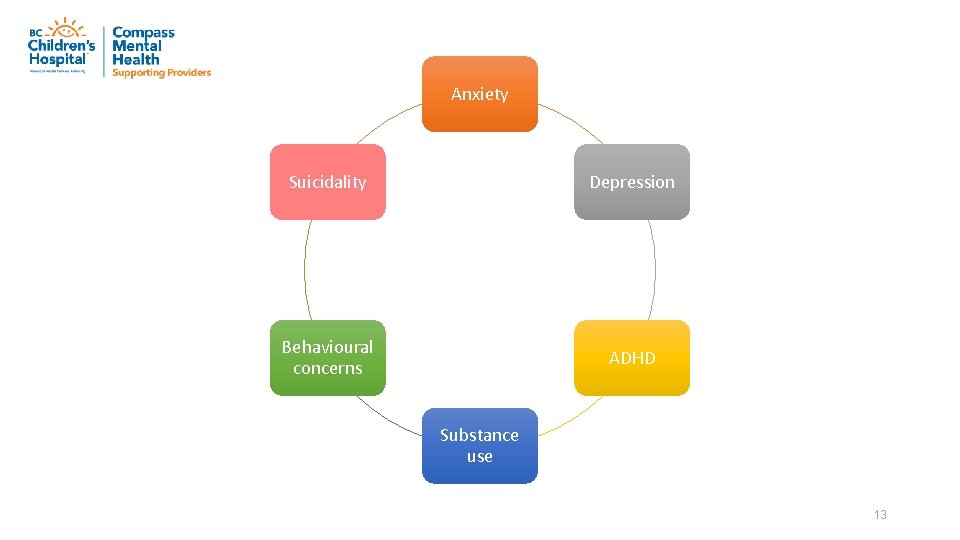
Anxiety Suicidality Depression Behavioural concerns ADHD Substance use 13
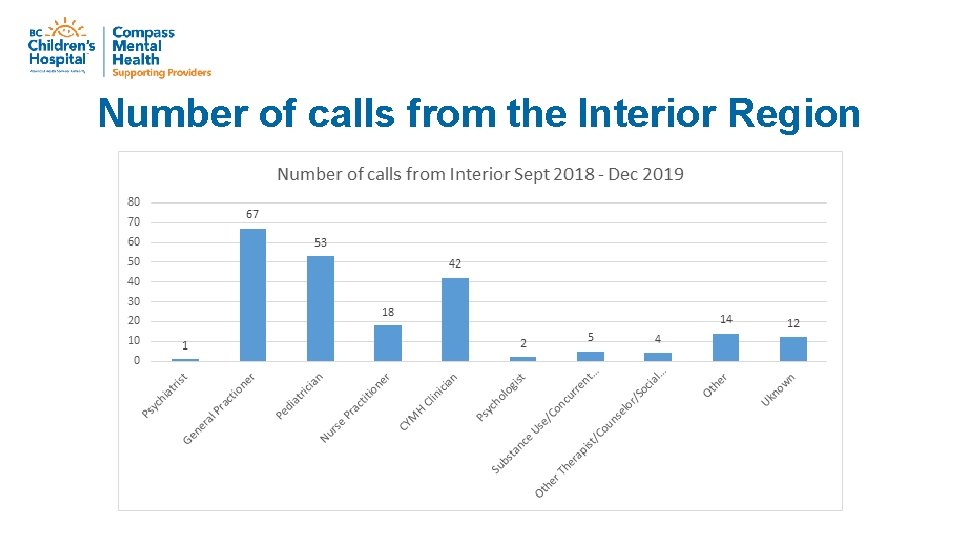
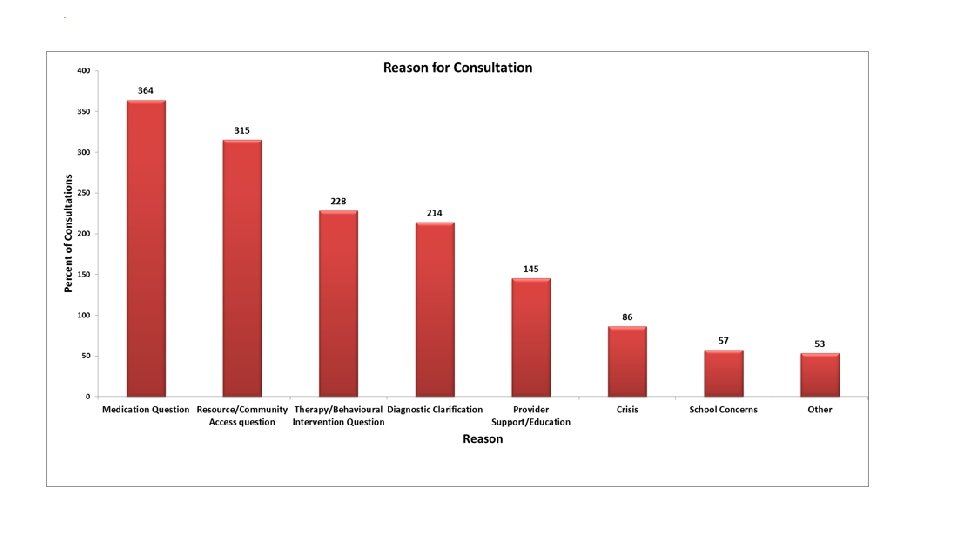
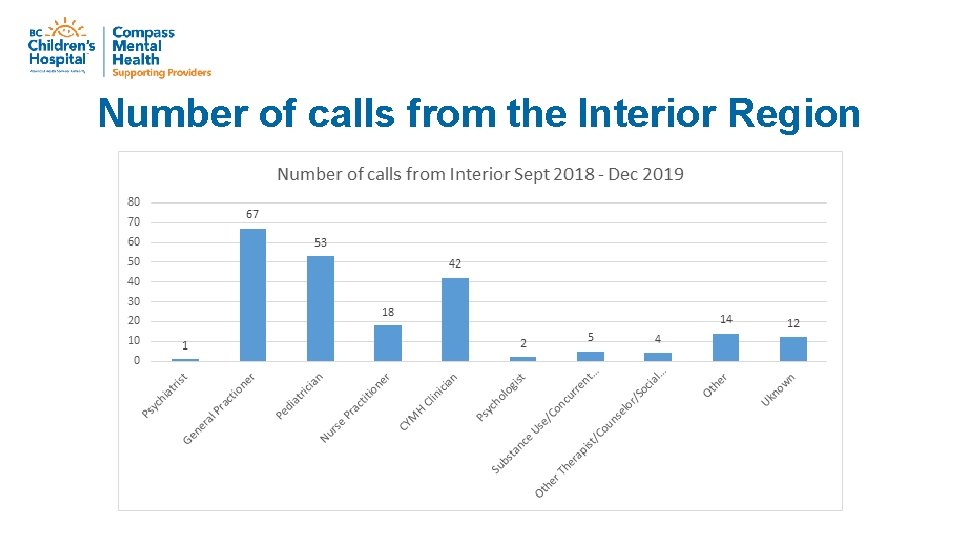
Number of calls from the Interior Region
13 y/o w/ suicidal ideation, MJ, anxiety, trauma in ER. Can Compass expedite my APAU (inpatient) referral? q Build capacity for community to manage the case q Assist w/ safety planning, identifying community support/service plan, and treatment recommendations q Can review whether an inpatient admission is helpful q Review other regional/provincial resource options (e. g. SU services, Maples, BC Children’s…) q Can do assessments and support case conferences in complex cases where community resources are lacking q We cannot expedite the referral, but we can support navigating the case
My patient has severe anxiety. How can I start medication? q First Line treatment is therapy! q Review evidence based therapies and other resources q Confident Parents anxiety program q Taming the Worry Dragons q Anxiety Canada. com q Support Pharmacological Management: i. e. Fluoxetine is the firstchoice for severe anxiety & depressive disorders in children & adolescents q Start 10* mg daily for 2 wks, incr. to 20 mg. Max 40 mg *Consider half doses for children <12 years
I’m seeing a teen but they won’t talk. What can I do? q Repeat visits to build trust q Supporting the role of the primary physician or clinician q Show interest q Ask about things that are important to them q See them alone (w/o caregivers)
Youth has OCD, but we can’t access evidence-based therapy. What to do? q Compass can support by: q Coaching local therapists in use of CBT/ ERP for OCD q Identifying information, apps, treatment options for family q Helping to consider role of / plan for medication q Strategizing around difficult cases/ complex presentations

9 y/o in rural community w/ ADHD, trauma, ++ disruptive behavior at school. Help! q Diagnostic clarifications (FASD, neurodevelopmental disorders) q Screen comorbid disorders (ie ADHD, ODD, Conducat) q Refer to CYMH and CYSN q Confident Parents behavior program q Compass can support team with therapeutic, behavioral & medication interventions (e. g. , school, CYMH clinician) q Compass can support complex case meetings with team
Top CYMHSU Resources q Kelty. Mental. Health. ca q Foundry q Confident Parents (behavior & anxiety) q Drug. Cocktails. ca (drug-med interactions) q Rolling. With. ADHD. ca
What’s next? EDUCATION & TOOLS • Co-development of educational tools and resources: o Accessible online resources (adaptable to providers’ needs) o Case-based interactive webinars o Opportunities for continuing education credits o Face-to-face visits o Others
What are your needs? q How can Compass specifically support the clinicians in the East Kootenays? q Clinically? q Education? q Supervision?
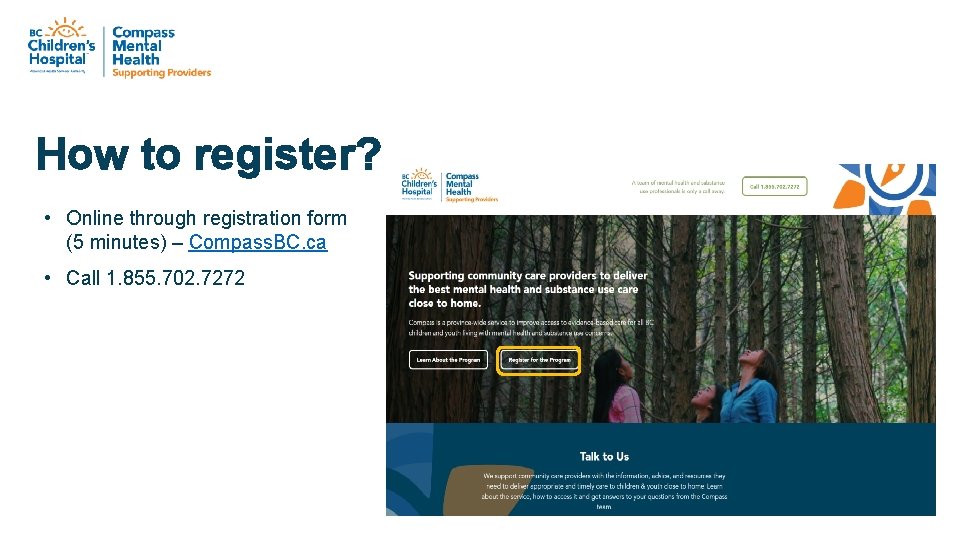
How to register? • Online through registration form (5 minutes) – Compass. BC. ca • Call 1. 855. 702. 7272

We are here, and we are in it together. A team of mental health and substance use professionals is only a call away. Call Compass at 1. 855. 702. 7272 Monday to Friday, 9 a. m. to 5 p. m. Questions? Email compass@cw. bc. ca