Comparison of initial high versus low dose Lthyroxine
![Results 4 – median TSH values TIME OF VISIT TSH median [IQR] in m. Results 4 – median TSH values TIME OF VISIT TSH median [IQR] in m.](https://slidetodoc.com/presentation_image_h/376ee4f99c2c4fe5399f245799726ee4/image-14.jpg)
- Slides: 22
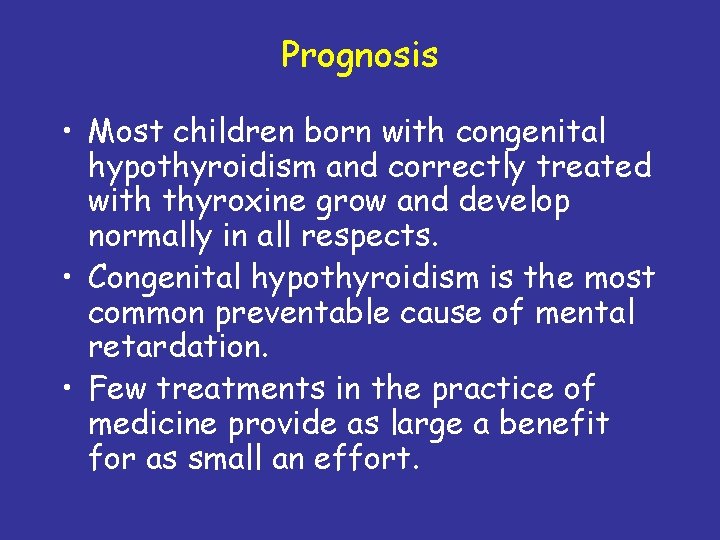
Comparison of initial high versus low dose L-thyroxine (LT 4) for congenital hypothyroidism (CH) BALÁZS GELLÉN MD Ph. D Department of Paediatrics, University of Szeged, Hungary
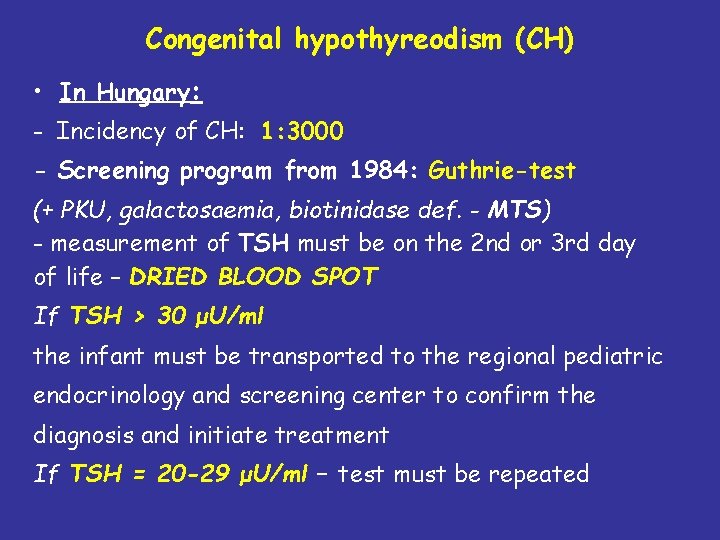
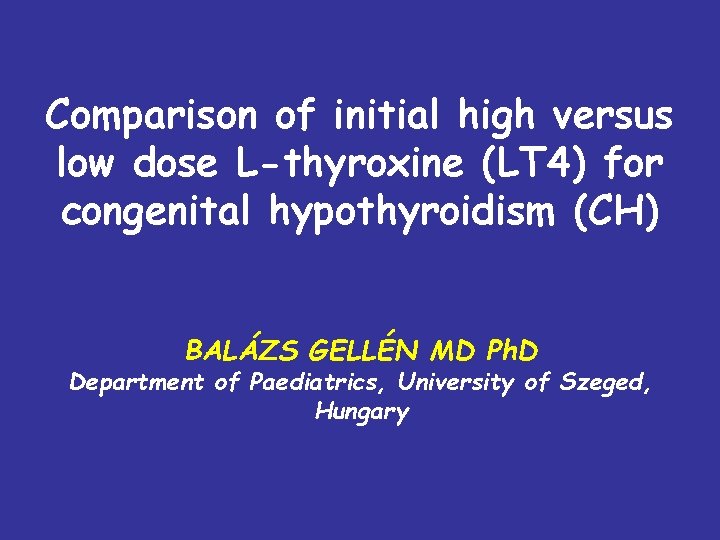
Congenital hypothyreodism (CH) • In Hungary: - Incidency of CH: 1: 3000 - Screening program from 1984: Guthrie-test (+ PKU, galactosaemia, biotinidase def. - MTS) - measurement of TSH must be on the 2 nd or 3 rd day of life – DRIED BLOOD SPOT If TSH > 30 μU/ml the infant must be transported to the regional pediatric endocrinology and screening center to confirm the diagnosis and initiate treatment If TSH = 20 -29 μU/ml – test must be repeated
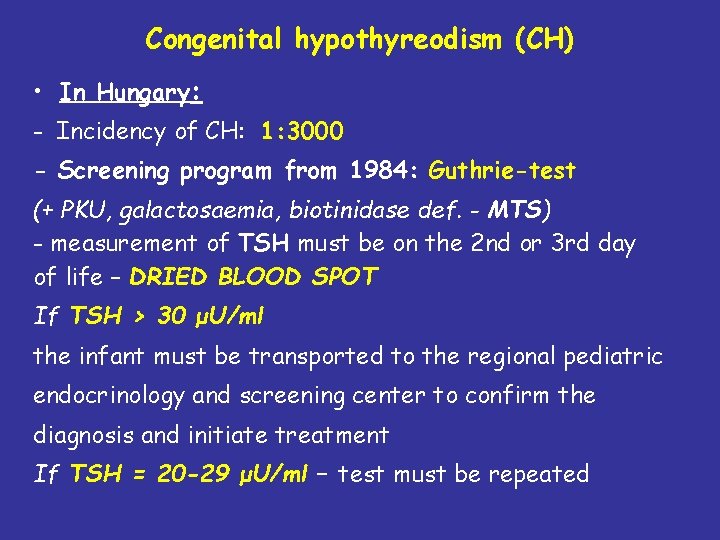
• • ETIOLOGY of CH 85% thyreoid gland dysgenesis organification def. agenesia, hypoplasia, ectopia 10% dyshormongenesis - defects of thyroxine or triiodothyronine synthesis within a structurally normal gland - nongoitrous CH TRH, TSHR def. , TSH resistance, iodine trapping and transport def. , thyroglobulin def. , deiodinase, peroxydase def. , G-protein def. 2% transcription factor gene mutation TTF 1, TTF 2, PAX 8 3% others – maternal radio-iodine therapy during pregnancy etc.
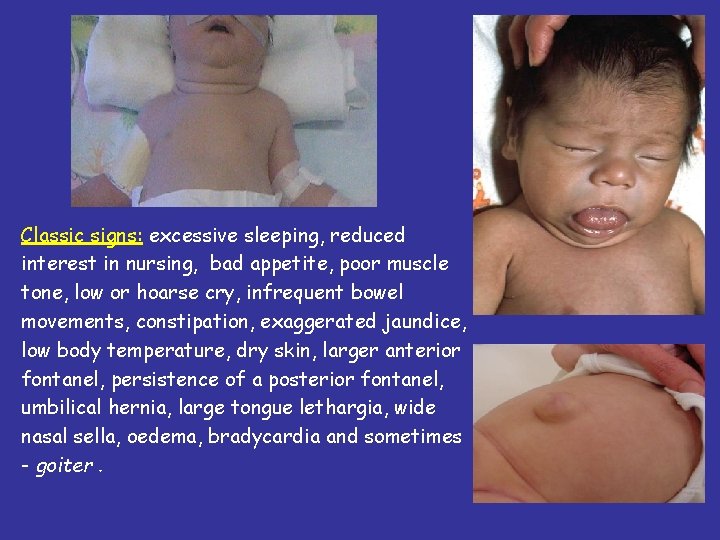
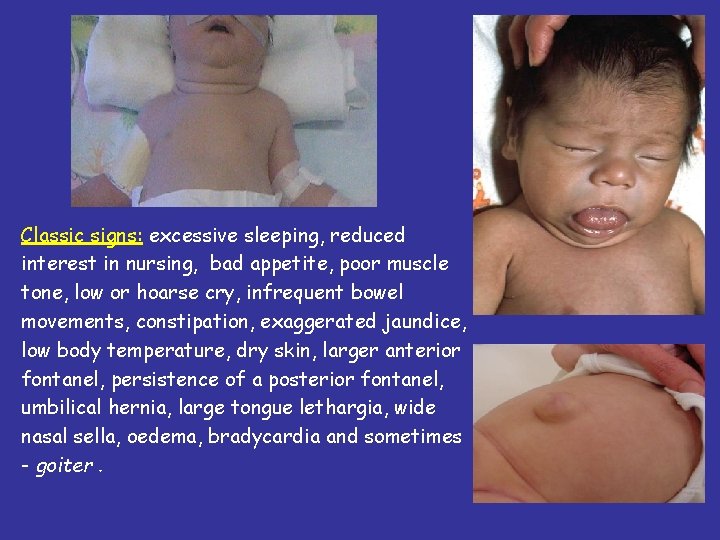
Classic signs: excessive sleeping, reduced interest in nursing, bad appetite, poor muscle tone, low or hoarse cry, infrequent bowel movements, constipation, exaggerated jaundice, low body temperature, dry skin, larger anterior fontanel, persistence of a posterior fontanel, umbilical hernia, large tongue lethargia, wide nasal sella, oedema, bradycardia and sometimes - goiter.
Introduction • The optimal dose of LT 4 during infancy is controversial • Advocates of high doses claim that intellectual outcome is improved • Others consider that high dose LT 4 in infancy may cause behaviour and concentration difficulties in later childhood
Hypothesis Initial high dose (50 µg/day) of LT 4 normalises thyroid function more quickly than low dose (25 µg/day), with no evidence of somatic overgrowth – a surrogate index of overtreatment between birth and 3 years of age.
Background • From 1979, when the Scottish newborn screening programme for CH began, the standard initial dose of LT 4 in most centres was 25 µg daily • From 1997 a high dose LT 4 regime has been increasingly used in the West of Scotland: 50 µg daily for the first 10 days followed by 37. 5 µg daily thereafter, titrating subsequent doses according to thyroid biochemistry
Patients and Methods 1 A retrospective study of patients referred between 1979 and 2005 in Scotland. Patients divided into 3 groups according to initial daily LT 4 dose (µg) • 25 (Group 1) • 30 -40 (Group 2) • 50 (Group 3)
Patients and Methods 2 Patients were excluded from the study if: • they did not conform to one of the three initial LT 4 treatment groups • the diagnosis was either transient elevated TSH or uncertain • there were less than two useable data points after birth
Patients and Methods 3 Differences in thyroid biochemistry (serum f. T 4 and TSH) between the 3 groups were compared at: • diagnosis • 7 -21 days after the start of treatment (7 -21 d. T 4) • 3, 6, 12, 18, 24 and 36 months of age Differences in somatic growth - length, weight and head circumference - were examined at 3, 6, 12, 18, 24 and 36 months of age SD scores were calculated vs. Cole, Freeman & Preece (Stat Med 1998, 17; 407 -09)
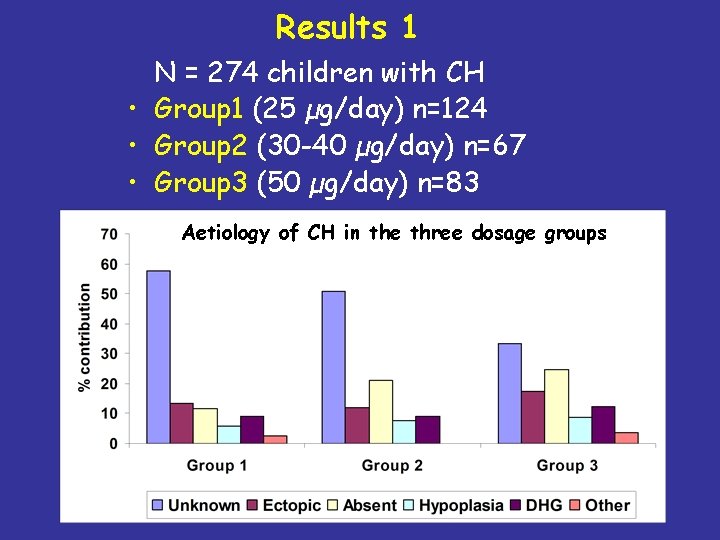
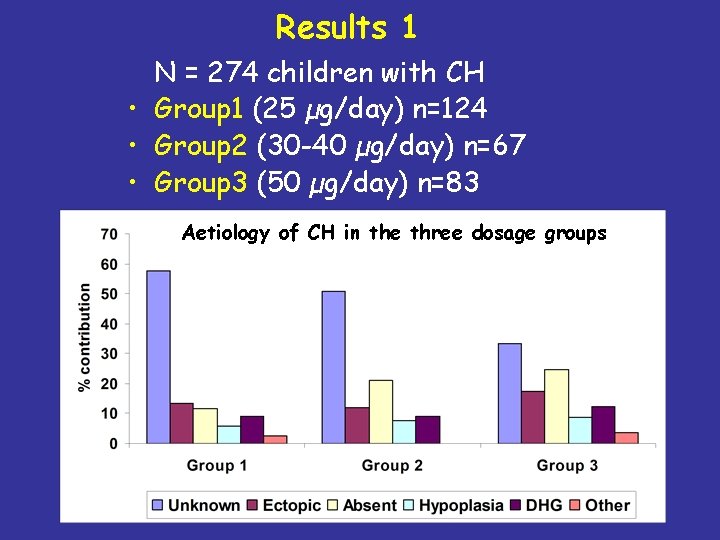
Results 1 N = 274 children with CH • Group 1 (25 µg/day) n=124 • Group 2 (30 -40 µg/day) n=67 • Group 3 (50 µg/day) n=83 Aetiology of CH in the three dosage groups
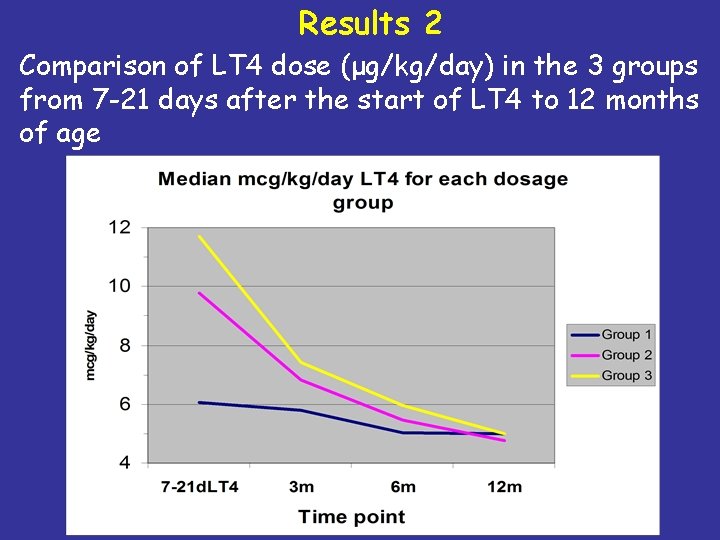
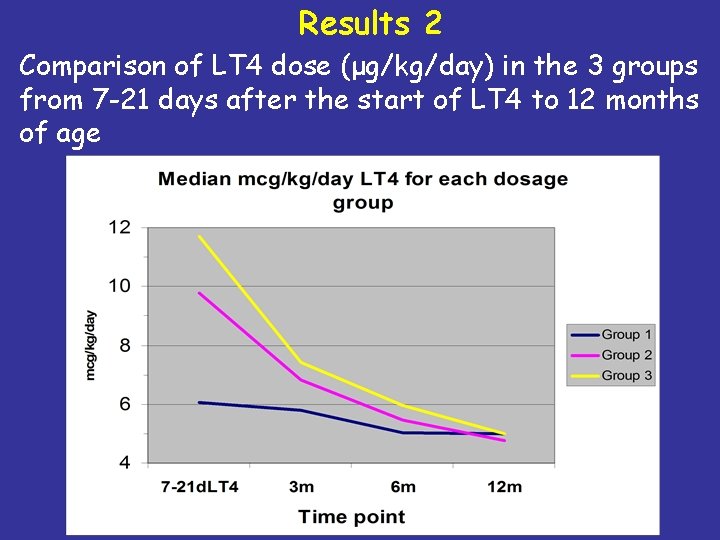
Results 2 Comparison of LT 4 dose (μg/kg/day) in the 3 groups from 7 -21 days after the start of LT 4 to 12 months of age
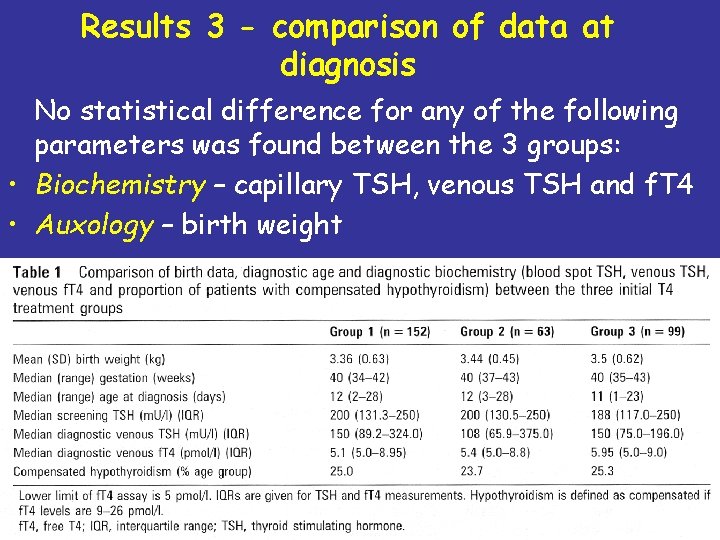
Results 3 - comparison of data at diagnosis No statistical difference for any of the following parameters was found between the 3 groups: • Biochemistry – capillary TSH, venous TSH and f. T 4 • Auxology – birth weight
![Results 4 median TSH values TIME OF VISIT TSH median IQR in m Results 4 – median TSH values TIME OF VISIT TSH median [IQR] in m.](https://slidetodoc.com/presentation_image_h/376ee4f99c2c4fe5399f245799726ee4/image-14.jpg)
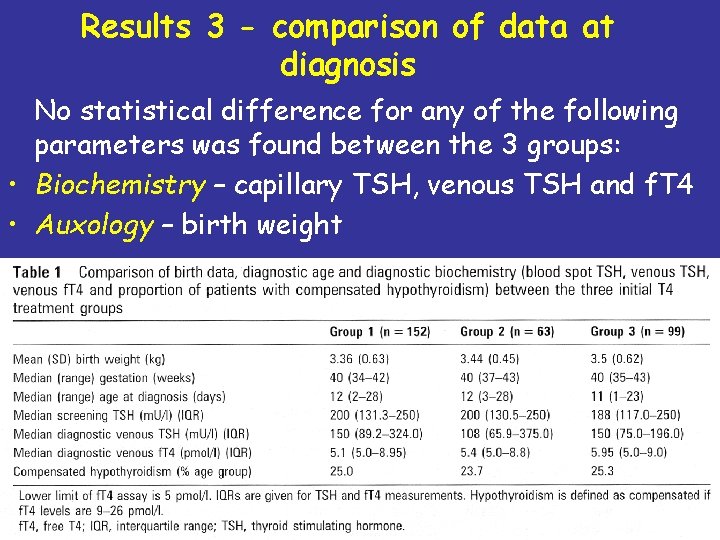
Results 4 – median TSH values TIME OF VISIT TSH median [IQR] in m. U/L (number of patients) Group 1 (25 μg) Group 2 (30 -40 μg) Group 3 (50 μg) At diagnosis 150 [89. 2 -324] (152) 108 [65. 9 -375] (63) 150 [75 -196] (99) 7 -21 days after the start of LT 4 58 [21 -100] 29 [11 -56] 4. 1 [1. 3 -9. 5] 3 months of age 10 [2. 7 -25. 3] 8 [2. 8 -16] 1. 5 [0. 6 -4. 6] 6 months of age 5. 2 [1 -16. 4] 7. 8 [0. 9 -20] 2. 7 [0. 5 -7. 6] 12 months of age 3. 5 [1. 1 -8. 4] 6. 3 [1. 2 -15. 6] 4. 3 [1 -10. 4] 18 months of age 2. 5 [0. 6 -8. 9] 2. 3 [1. 4 -13. 1] 2. 4 [0. 5 -8. 3] 24 months of age 3. 3 [1 -5. 6] 4. 7 [1. 5 -10. 2] 1. 0 [0. 3 -6. 1] 36 months of age 2. 4 [0. 4 -5. 6] 3. 3 [1. 6 -14. 3] 4. 5 [1. 4 -7. 4] TSH values 5 m. U/L are highlighted for comparison
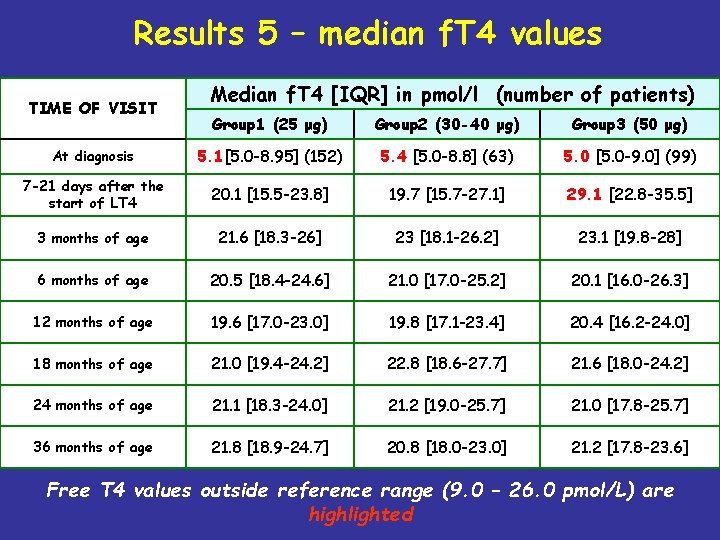
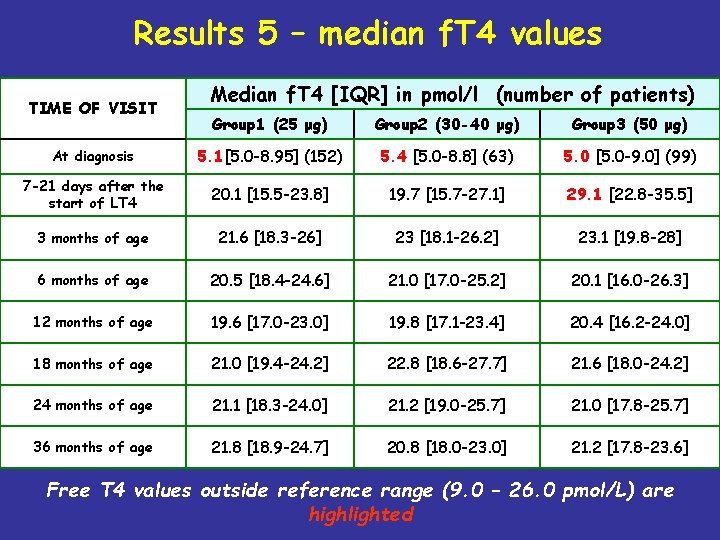
Results 5 – median f. T 4 values TIME OF VISIT Median f. T 4 [IQR] in pmol/l (number of patients) Group 1 (25 μg) Group 2 (30 -40 μg) Group 3 (50 μg) At diagnosis 5. 1[5. 0 -8. 95] (152) 5. 4 [5. 0 -8. 8] (63) 5. 0 [5. 0 -9. 0] (99) 7 -21 days after the start of LT 4 20. 1 [15. 5 -23. 8] 19. 7 [15. 7 -27. 1] 29. 1 [22. 8 -35. 5] 3 months of age 21. 6 [18. 3 -26] 23 [18. 1 -26. 2] 23. 1 [19. 8 -28] 6 months of age 20. 5 [18. 4 -24. 6] 21. 0 [17. 0 -25. 2] 20. 1 [16. 0 -26. 3] 12 months of age 19. 6 [17. 0 -23. 0] 19. 8 [17. 1 -23. 4] 20. 4 [16. 2 -24. 0] 18 months of age 21. 0 [19. 4 -24. 2] 22. 8 [18. 6 -27. 7] 21. 6 [18. 0 -24. 2] 24 months of age 21. 1 [18. 3 -24. 0] 21. 2 [19. 0 -25. 7] 21. 0 [17. 8 -25. 7] 36 months of age 21. 8 [18. 9 -24. 7] 20. 8 [18. 0 -23. 0] 21. 2 [17. 8 -23. 6] Free T 4 values outside reference range (9. 0 – 26. 0 pmol/L) are highlighted
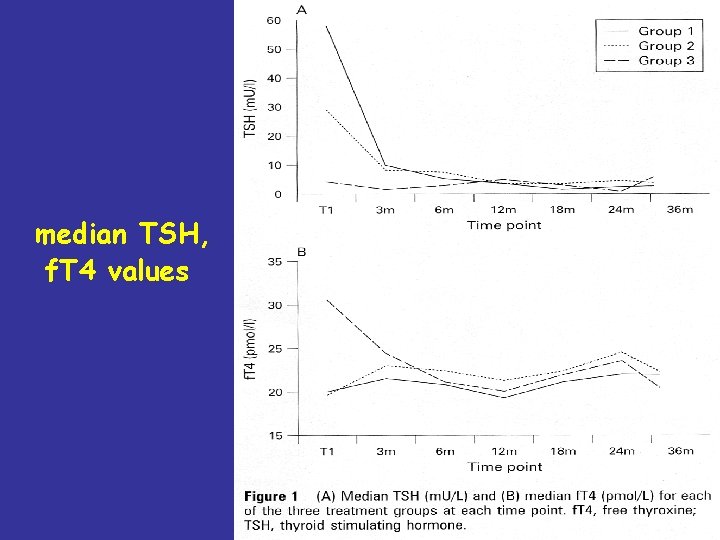
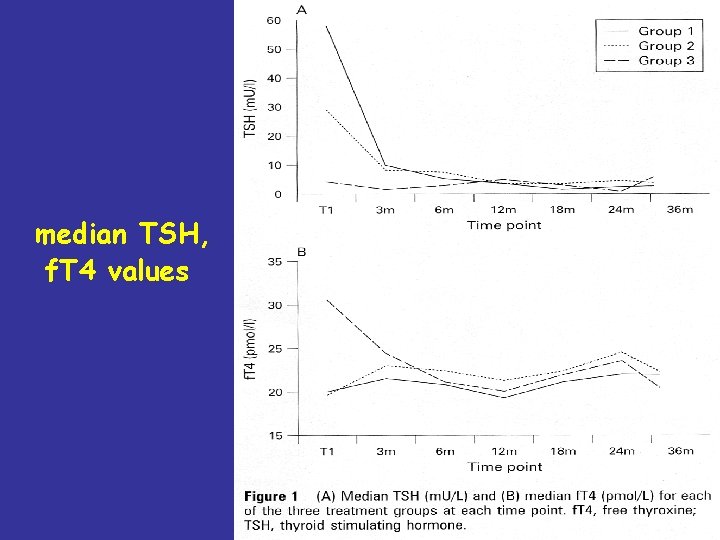
median TSH, f. T 4 values
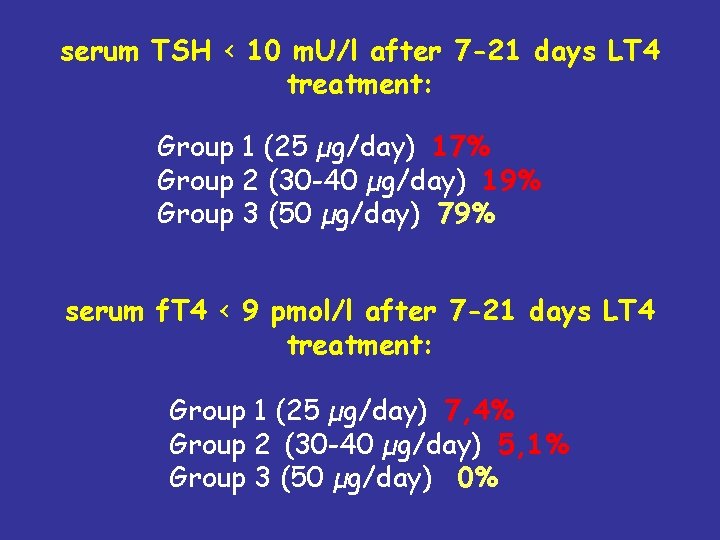
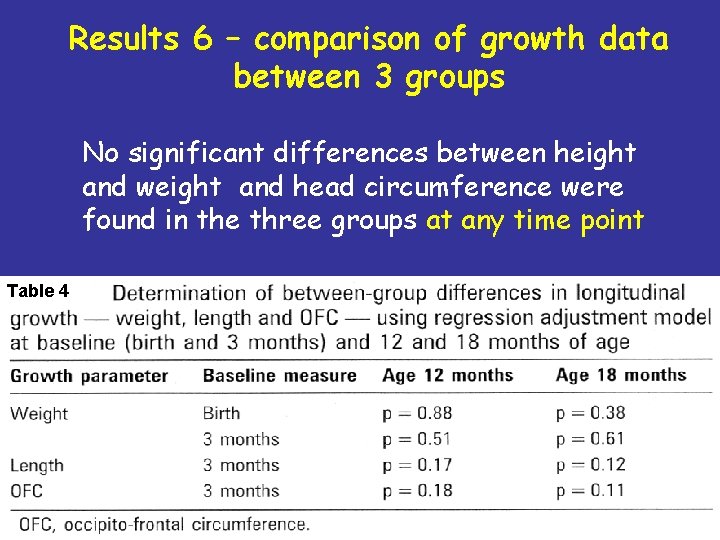
serum TSH < 10 m. U/l after 7 -21 days LT 4 treatment: Group 1 (25 µg/day) 17% Group 2 (30 -40 µg/day) 19% Group 3 (50 µg/day) 79% serum f. T 4 < 9 pmol/l after 7 -21 days LT 4 treatment: Group 1 (25 µg/day) 7, 4% Group 2 (30 -40 µg/day) 5, 1% Group 3 (50 µg/day) 0%
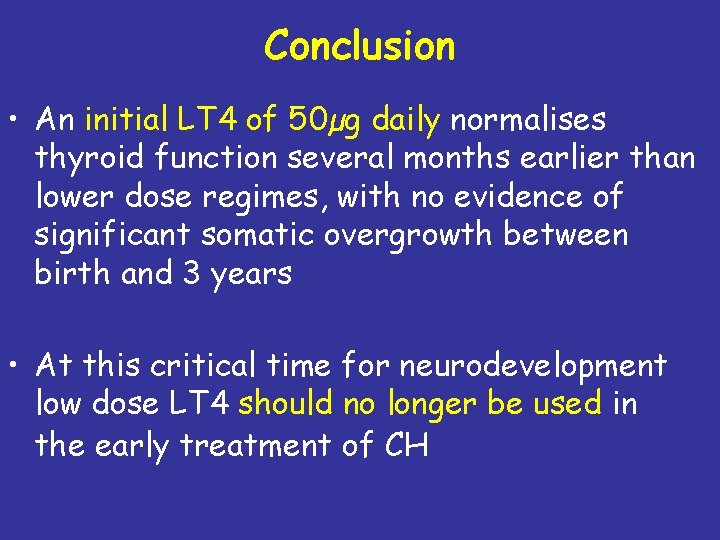
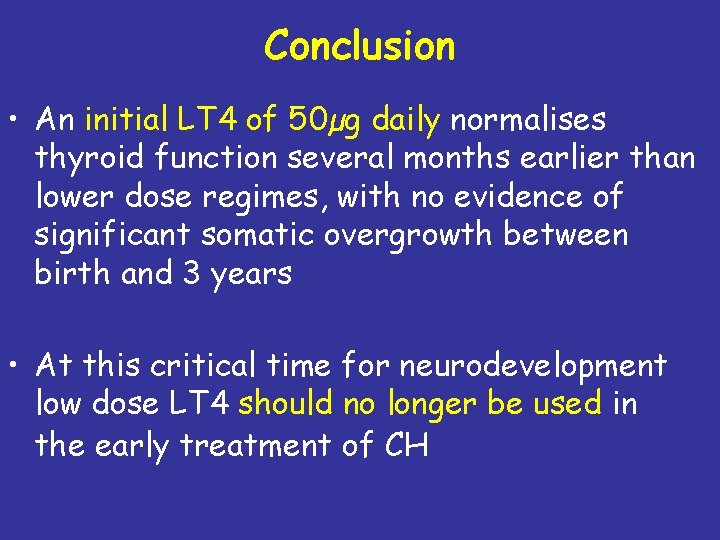
Results 6 – comparison of growth data between 3 groups No significant differences between height and weight and head circumference were found in the three groups at any time point Table 4
Conclusion • An initial LT 4 of 50µg daily normalises thyroid function several months earlier than lower dose regimes, with no evidence of significant somatic overgrowth between birth and 3 years • At this critical time for neurodevelopment low dose LT 4 should no longer be used in the early treatment of CH
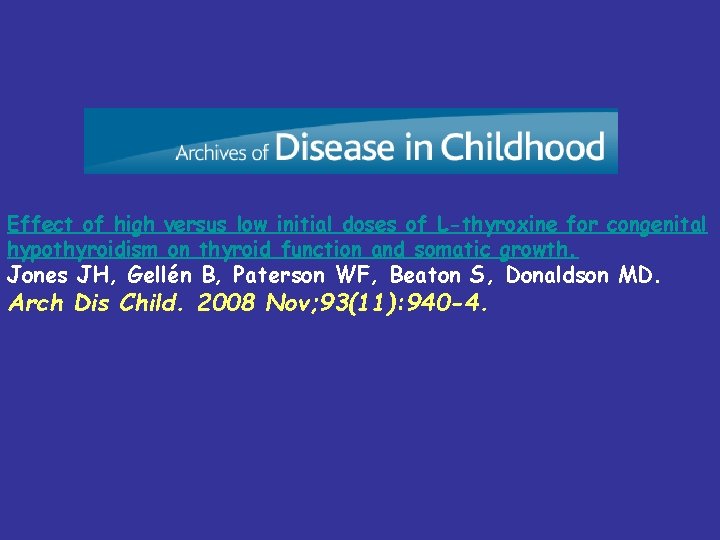
Effect of high versus low initial doses of L-thyroxine for congenital hypothyroidism on thyroid function and somatic growth. Jones JH, Gellén B, Paterson WF, Beaton S, Donaldson MD. Arch Dis Child. 2008 Nov; 93(11): 940 -4.
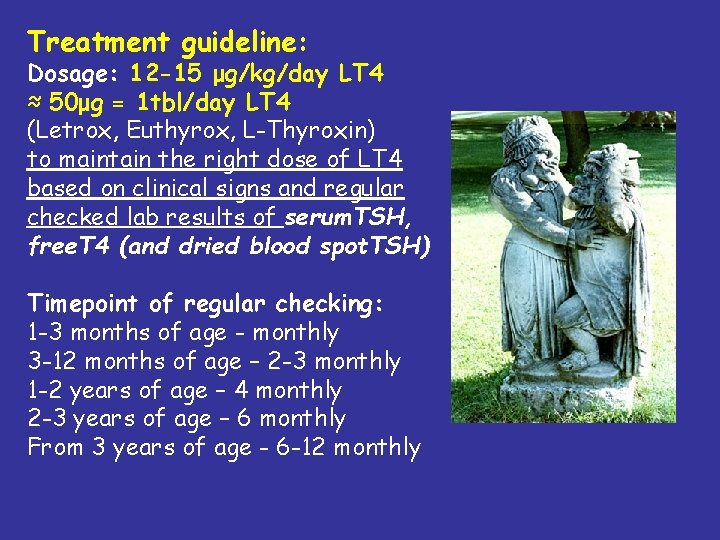
Treatment guideline: Dosage: 12 -15 μg/kg/day LT 4 ≈ 50μg = 1 tbl/day LT 4 (Letrox, Euthyrox, L-Thyroxin) to maintain the right dose of LT 4 based on clinical signs and regular checked lab results of serum. TSH, free. T 4 (and dried blood spot. TSH) Timepoint of regular checking: 1 -3 months of age - monthly 3 -12 months of age – 2 -3 monthly 1 -2 years of age – 4 monthly 2 -3 years of age – 6 monthly From 3 years of age - 6 -12 monthly
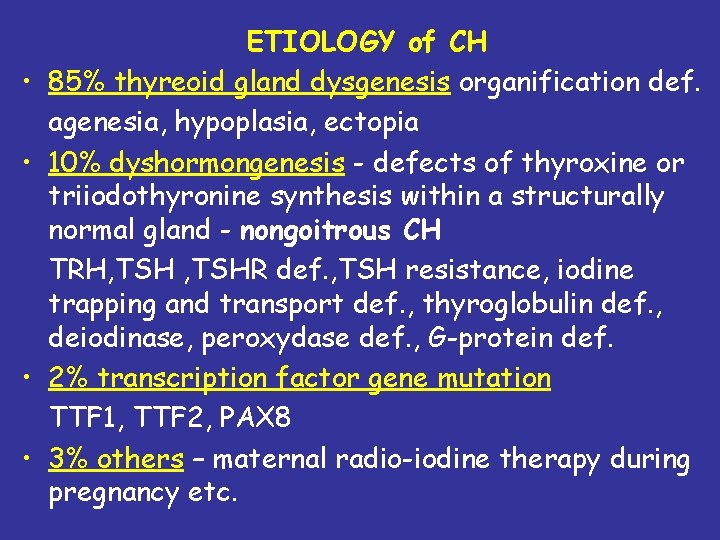
Prognosis • Most children born with congenital hypothyroidism and correctly treated with thyroxine grow and develop normally in all respects. • Congenital hypothyroidism is the most common preventable cause of mental retardation. • Few treatments in the practice of medicine provide as large a benefit for as small an effort.