Community Learning Disability Teams Debra Moore Managing Director
Community Learning Disability Teams Debra Moore Managing Director Debra Moore Associates www. debramooreassociates. com 01723 371446 07950 333884 debra@debramooreassociates. com
Mission impossible?
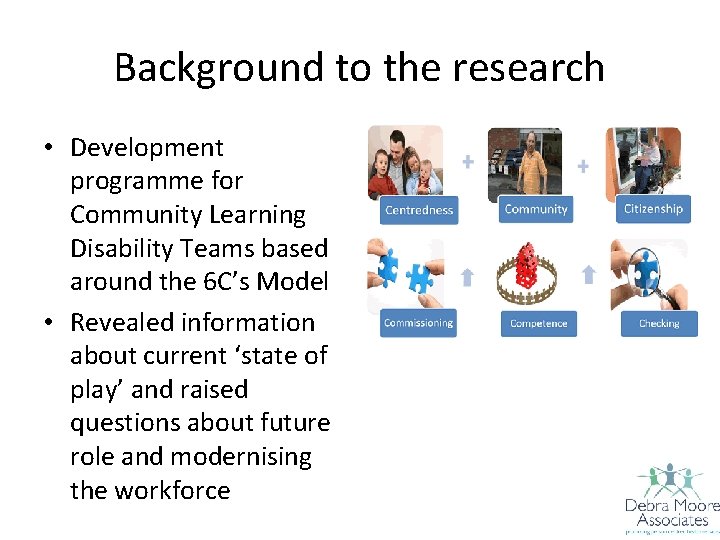
Background to the research • Development programme for Community Learning Disability Teams based around the 6 C’s Model • Revealed information about current ‘state of play’ and raised questions about future role and modernising the workforce
Background to the research …what people were saying…. • Need to reduce health inequalities and supporting the delivery of VP objectives e. g. HAP’s etc • Need to support mainstream NHS including mental health • Reducing out of area placements • ‘Personalisation’ • Safeguarding • Changes in demography • ‘Boundaries’ between teams e. g. children & older people • Supporting criminal justice system • Workforce issues • Financial pressures • Some concerns about choice and quality of provision
Pressure to ‘rescue’ • In some localities the community based team are increasingly ‘rescuing’ situations created by ‘specialist’ social care providers (often ‘importers’) • Also ‘recovering’ problems created by changes in other parts of the system e. g. day services - the ‘buck stops here’ position • Safeguarding

‘Being painted into a corner’
Background to the research ‘old chestnuts’ • Issues raised about time spent on health related activities and social work activities as opposed to ‘care management’ • Questions about the content of the work of individual CTLD members & blurring of roles within the team • Concern about capacity for ‘face to face’ contact and time spent on admin/IT and in meetings • Concern to make sure that the CTLD is part of a wider care pathway
Methodology • A brief electronic survey • A number of key questions generated by emergent themes from work with CTLD’s • Self selecting participants • Survey link posted on various professional websites and out via networking groups etc • 500+ responses
What percentage of your working week is spent across the following 4 areas? • Care Management • Admin & IT • Face to face contact with service users • Review meetings
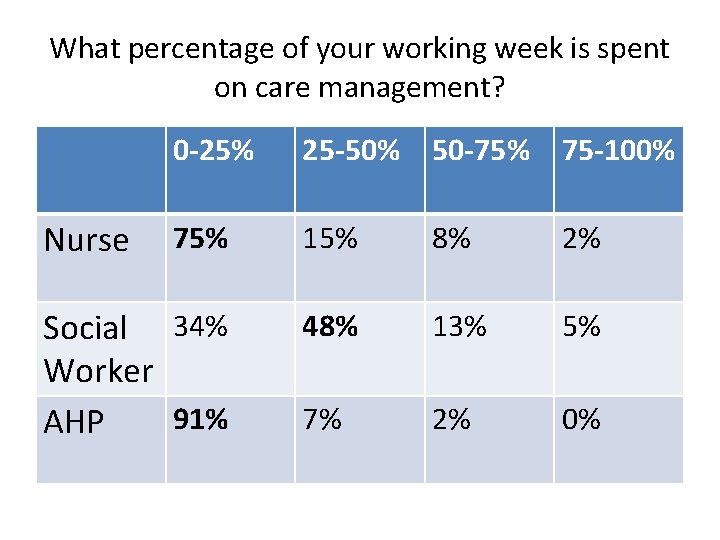
What percentage of your working week is spent on care management? 0 -25% 25 -50% 50 -75% 75 -100% 75% 15% 8% 2% Social 34% Worker 91% AHP 48% 13% 5% 7% 2% 0% Nurse
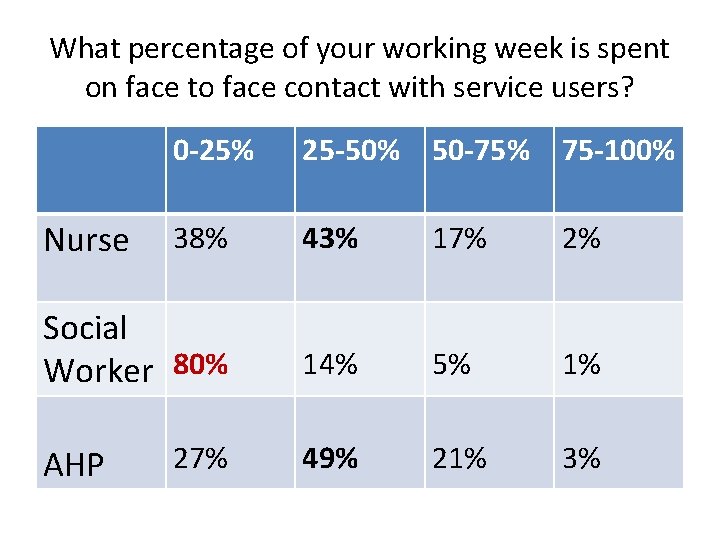
What percentage of your working week is spent on face to face contact with service users? 0 -25% 25 -50% 50 -75% 75 -100% 38% 43% 17% 2% Social Worker 80% 14% 5% 1% 27% 49% 21% 3% Nurse AHP
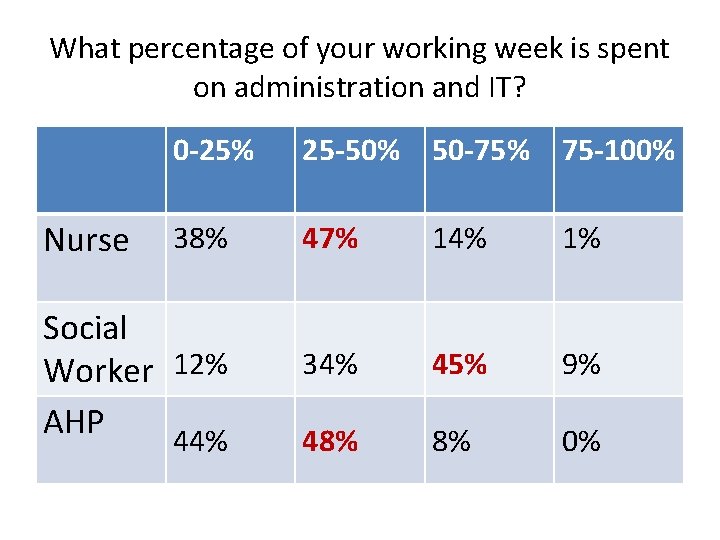
What percentage of your working week is spent on administration and IT? Nurse 0 -25% 25 -50% 50 -75% 75 -100% 38% 47% 14% 1% 34% 45% 9% 48% 8% 0% Social Worker 12% AHP 44%
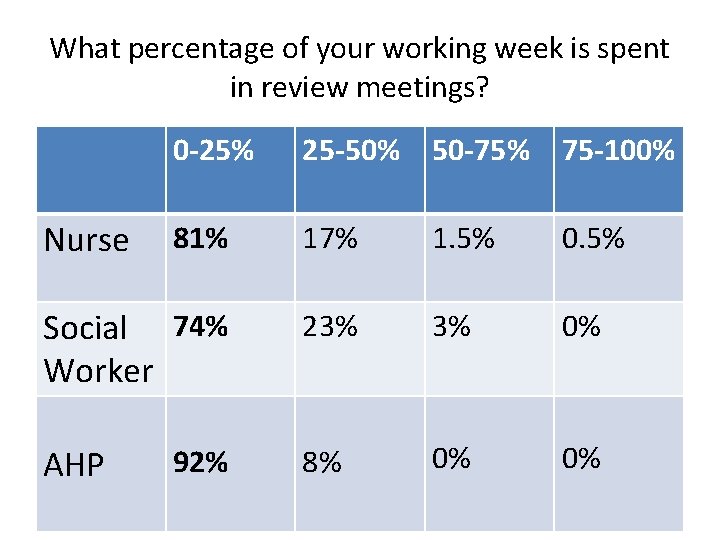
What percentage of your working week is spent in review meetings? 0 -25% 25 -50% 50 -75% 75 -100% 81% 17% 1. 5% 0. 5% Social 74% Worker 23% 3% 0% AHP 8% 0% 0% Nurse 92%
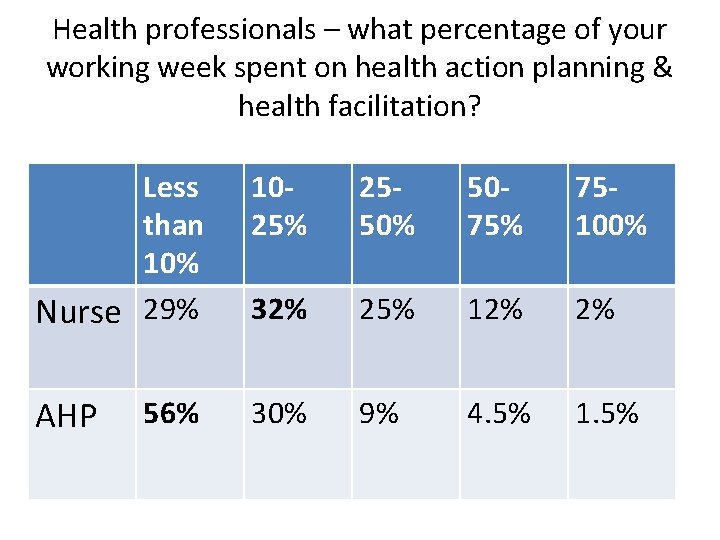
Health professionals – what percentage of your working week spent on health action planning & health facilitation? Less than 10% Nurse 29% 1025% 2550% 5075% 75100% 32% 25% 12% 2% AHP 30% 9% 4. 5% 1. 5% 56%
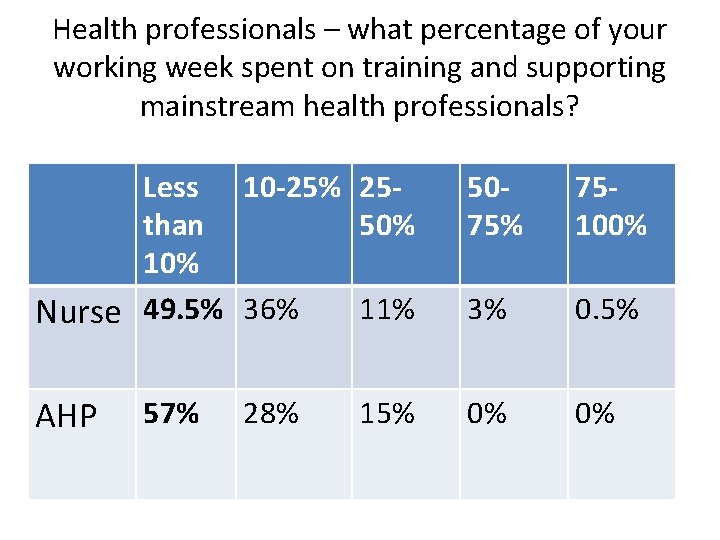
Health professionals – what percentage of your working week spent on training and supporting mainstream health professionals? Less 10 -25% 25 than 50% 11% Nurse 49. 5% 36% 5075% 75100% 3% 0. 5% AHP 0% 0% 57% 28% 15%
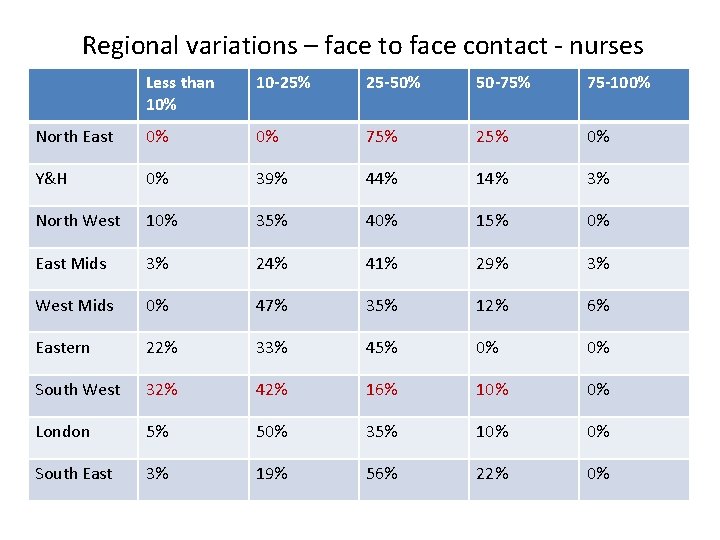
Regional variations – face to face contact - nurses Less than 10% 10 -25% 25 -50% 50 -75% 75 -100% North East 0% 0% 75% 25% 0% Y&H 0% 39% 44% 14% 3% North West 10% 35% 40% 15% 0% East Mids 3% 24% 41% 29% 3% West Mids 0% 47% 35% 12% 6% Eastern 22% 33% 45% 0% 0% South West 32% 42% 16% 10% 0% London 5% 50% 35% 10% 0% South East 3% 19% 56% 22% 0%
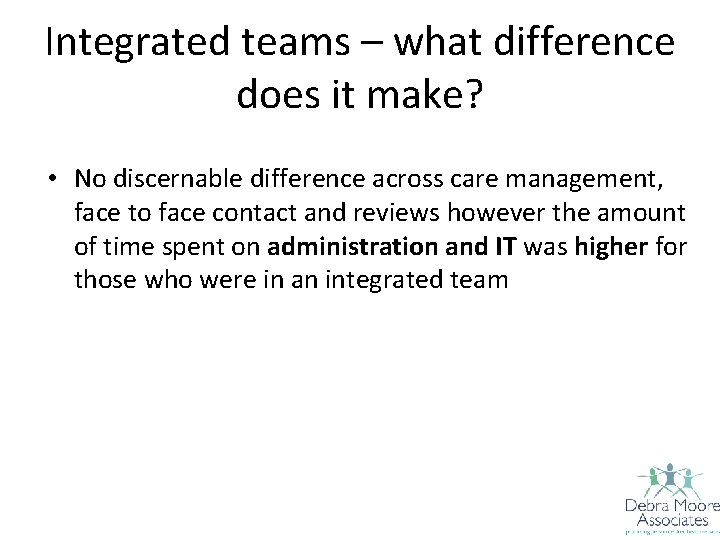
Integrated teams – what difference does it make? • No discernable difference across care management, face to face contact and reviews however the amount of time spent on administration and IT was higher for those who were in an integrated team
Probably raised as many questions as answers • Why are there such big variations between regions and how does this effect outcomes? • What does admin & IT consist of? • If health professionals reduce care management activity what will be the implications?
Next steps • More detailed analysis of survey • Drilling down on emergent themes • Examine patterns of provision e. g. A&T, Out of Area placements etc • Consider how we map against outcomes such as health checks, numbers of HAPs etc
Lessons for nurses • • Health related activity as a first priority Outcomes Person experience Universal and mainstream services Look after one another Don’t give up Use an appreciative eye – what do you want more of?
Don’t get the Dibley’s! • Strong leadership • Earn your place at the table • Ensure people who use services and their families are at the table • No piccalilli and tuna sandwiches!
Finally Keeping the message simple ensuring the ‘me and mine’ test is passed • http: //www. youtube. com/watch? v=LYPIx. Hz. X AJY
- Slides: 22