Community Health Needs Assessment Setting Priorities Building Leaders

Community Health Needs Assessment Setting Priorities Building Leaders – Transforming Hospitals – Improving Care © HTS 3 2016 | Page 1
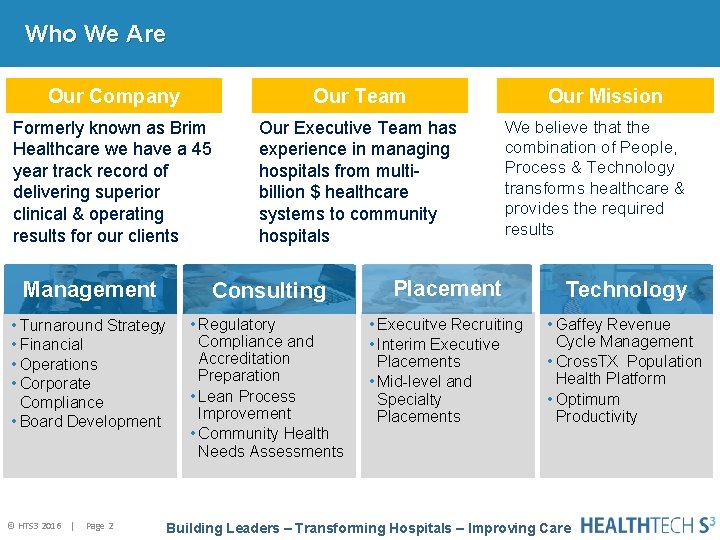
Who We Are Our Company Our Team Formerly known as Brim Healthcare we have a 45 year track record of delivering superior clinical & operating results for our clients Our Executive Team has experience in managing hospitals from multibillion $ healthcare systems to community hospitals Our Mission We believe that the combination of People, Process & Technology transforms healthcare & provides the required results Management Consulting Placement Technology • Turnaround Strategy • Financial • Operations • Corporate Compliance • Board Development • Regulatory Compliance and Accreditation Preparation • Lean Process Improvement • Community Health Needs Assessments • Execuitve Recruiting • Interim Executive Placements • Mid-level and Specialty Placements • Gaffey Revenue Cycle Management • Cross. TX Population Health Platform • Optimum Productivity © HTS 3 2016 | Page 2 Building Leaders – Transforming Hospitals – Improving Care
Instructions for Today’s Webinar • You may type a question in the text box if you have a question during the presentation • We will try to cover all of your questions – but if we don’t get to them during the webinar we will follow-up with you by e-mail • You may also send questions after the webinar to Carolyn St. Charles (contact information is included at the end of the presentation) • The webinar will be recorded and the recording will be available on the Health. Tech. S 3 web site www. healthtechs 3. com Health. Tech. S 3 hopes that the information contained herein will be informative and helpful on industry topics. However, please note that this information is not intended to be definitive. Health. Tech. S 3 and its affiliates expressly disclaim any and all liability, whatsoever, for any such information and for any use made thereof. Health. Tech. S 3 does not and shall not have any authority to develop substantive billing or coding policies for any hospital, clinic or their respective personnel, and any such final responsibility remains exclusively with the hospital, clinic or their respective personnel. Health. Tech. S 3 recommends that hospitals, clinics, their respective personnel, and all other third party recipients of this information consult original source materials and qualified healthcare regulatory counsel for specific guidance in healthcare reimbursement and regulatory matters. © HTS 3 2016 | Page 3

Speaker Carolyn St. Charles, RN, BSN, MBA Regional Chief Clinical Officer Carolyn began her healthcareer as a staff nurse in Intensive Care. She has worked in a variety of staff, administrative and consulting roles and has been in her current position as Regional Chief Clinical Officer with Health. Tech. S 3 for the last fifteen years. In her role as Regional Chief Clinical Officer, Carolyn St. Charles is the lead consultant for development of Community Health Needs Assessments. She also conducts mock surveys for Critical Access Hospitals, Acute Care Hospitals, Long Term Care, Rural Health Clinics, Home Health and Hospice. Healthcare Focus © HTS 3 2016 | Page 4 45 Year Company History Experienced Consultants Building Leaders – Transforming Hospitals – Improving Care Technology Partnerships
The Affordable Care Act added 501(r) to the Internal Revenue Code. This provided that hospital organizations will not be treated as tax-exempt under 501(c)(3) unless they meet certain requirements. All of the provisions apply to taxable years beginning after March 23, 2010, except the Community Health Needs Assessment (CHNA). 1. Establish written financial assistance and emergency medical care policies. 2. Limit amounts charged for emergency or other medically necessary care to individuals eligible for assistance under the hospital's financial assistance policy. 3. Make reasonable efforts to determine whether an individual is eligible for assistance under the hospital’s financial assistance policy before engaging in extraordinary collection actions against the individual. 4. Conduct a community health needs assessment (CHNA) and adopt an implementation strategy at least once every three years. – A $50, 000 excise tax will be imposed on a hospital that fails to meet the CHNA requirements with respect to any taxable year. © HTS 3 2016 | Page 5
Final Regulations December 2014 The final rules issued December of 2014 are consistent with earlier guidance issued by the IRS in April of 2013. However, they include the following clarifications: 1. 2. 3. 4. 5. Expands examples of health needs to include preventing illness and addressing the social determinants of health Gives hospitals flexibility if they are unable to obtain required community input Adds requirement to use community input in setting priorities as well as in the assessment process Requires that CHNA documentation must include evaluation of impact of any actions that were taken to address significant health needs since the previous assessment The requirement that implementation strategies include a plan to evaluate planned actions was deleted from the final rule but the strategy still must include anticipated impact of planned actions Source: • “Additional Requirements for Charitable Hospitals; Community Health Needs Assessments for Charitable Hospitals; Requirement of a Section 4959 Excise Tax Return and Time for Filing the Return; Final Rule, ” 79 FR 78953 [December 31, 2014], pp. 78953 -79016) • “Community Health Needs Assessments for Charitable Hospitals, ” 78 FR 20523 [April 2, 2013], pp. 20523 -20544 • Catholic Health Association: Assessing & Addressing Community Health Needs 2015 EDITION I I © HTS 3 2016 | Page 6
Exempt or Not? Governmental entities, which means that they are exempt under IRC Section 115 instead of IRC 501 C 3, do not have to file a Form 990 tax return AND they are not subject to the 501 R tax regulations and therefore is not required to complete a CHNA. Some governmental hospitals that are referred to as “dual status” hospitals. A “dual status” hospital is a governmental hospital that has received 501 C 3 status in order to participate in certain employee benefits, which is typically a 403 b pension plan. These hospitals are not required to file a Form 990; however, since they do have 501 C 3 tax status, they are subject to the 501 R tax regulations and thus required to complete a CHNA. © HTS 3 2016 | Page 7

Steps for Identifying Priority Community Health Needs 1. Understand interpret the indicator data you have gathered from primary and secondary sources 2. Identify major community health needs 3. Develop priorities 4. Incorporate community health priorities in your Community Health Needs Assessment © HTS 3 2016 | Page 8
Step 1 Understand Interpret the Data © HTS 3 2016 | Page 9
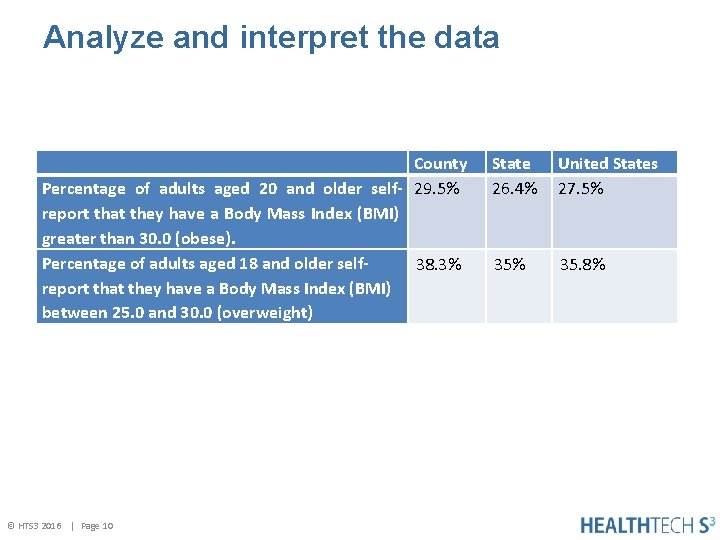
Analyze and interpret the data County Percentage of adults aged 20 and older self- 29. 5% report that they have a Body Mass Index (BMI) greater than 30. 0 (obese). Percentage of adults aged 18 and older self 38. 3% report that they have a Body Mass Index (BMI) between 25. 0 and 30. 0 (overweight) © HTS 3 2016 | Page 10 State 26. 4% United States 27. 5% 35. 8%
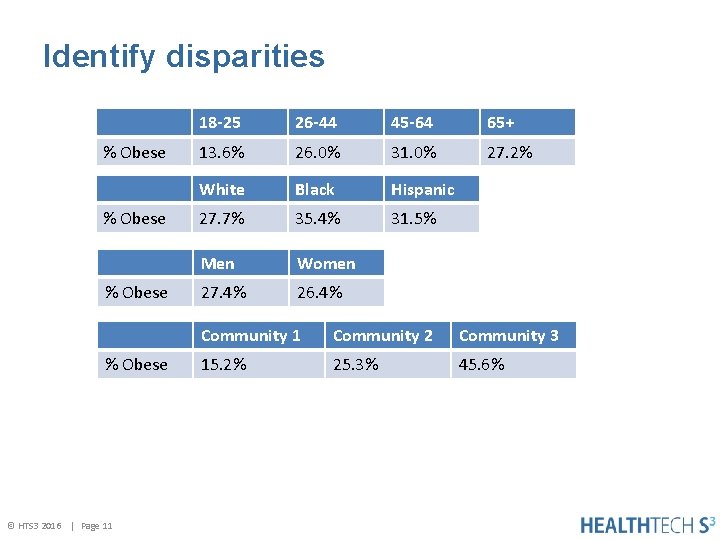
Identify disparities % Obese © HTS 3 2016 | Page 11 18 -25 26 -44 45 -64 65+ 13. 6% 26. 0% 31. 0% 27. 2% White Black Hispanic 27. 7% 35. 4% 31. 5% Men Women 27. 4% 26. 4% Community 1 Community 2 Community 3 15. 2% 25. 3% 45. 6%
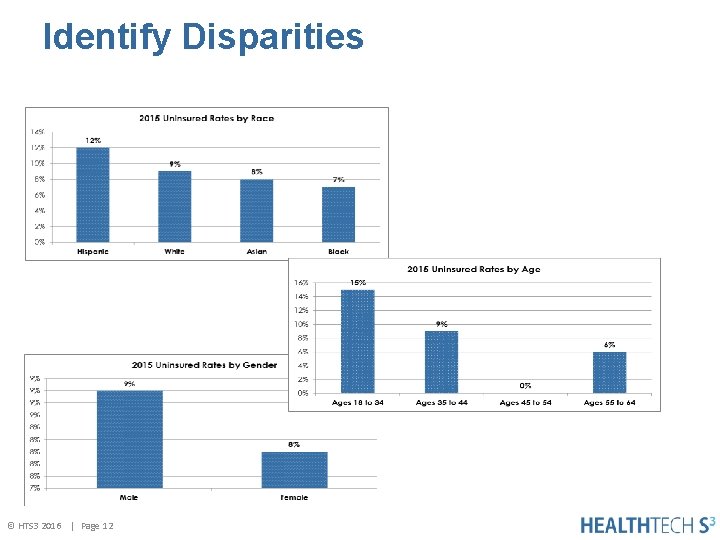
Identify Disparities © HTS 3 2016 | Page 12
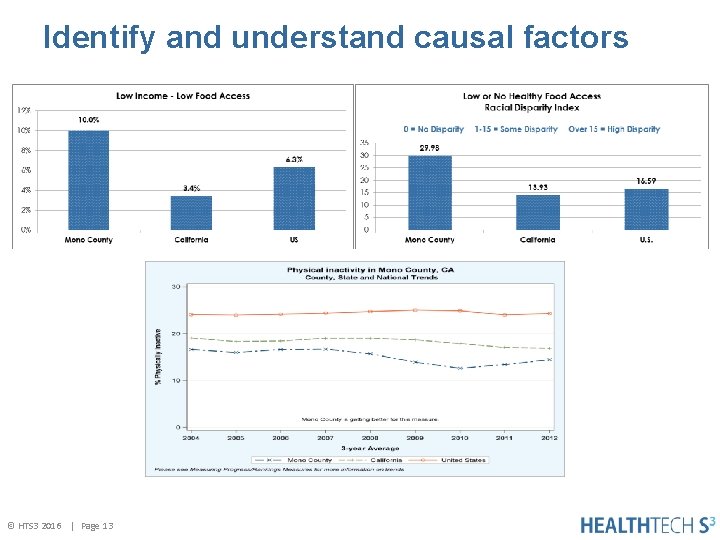
Identify and understand causal factors © HTS 3 2016 | Page 13
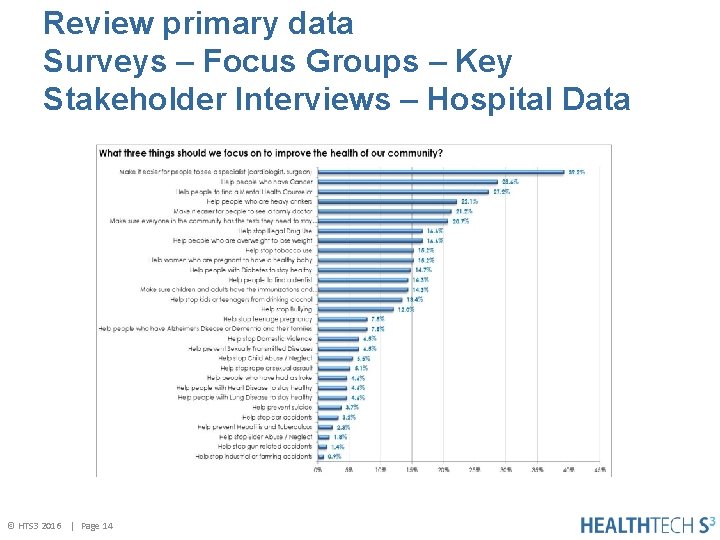
Review primary data Surveys – Focus Groups – Key Stakeholder Interviews – Hospital Data © HTS 3 2016 | Page 14
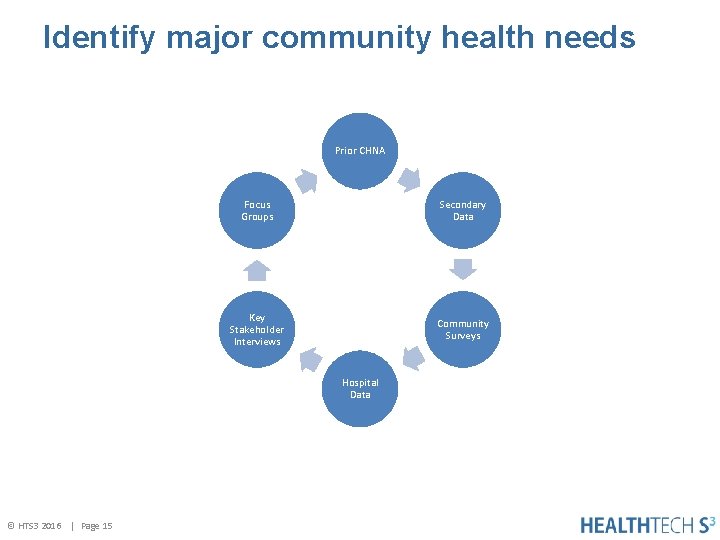
Identify major community health needs Prior CHNA Focus Groups Secondary Data Key Stakeholder Interviews Community Surveys Hospital Data © HTS 3 2016 | Page 15
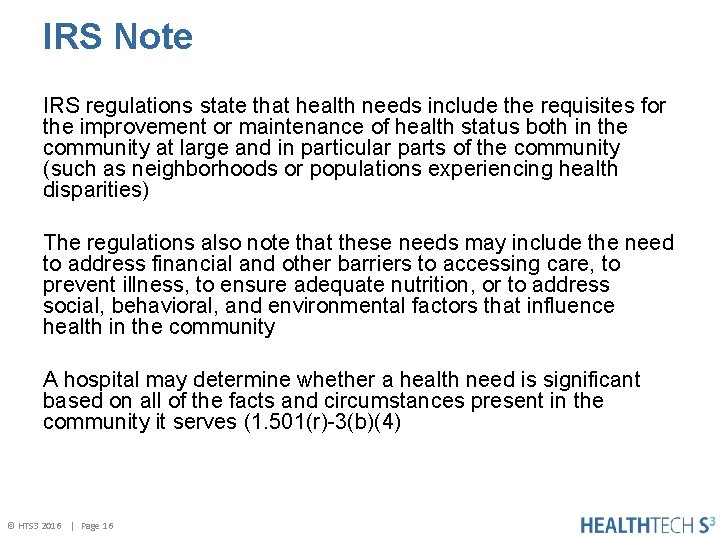
IRS Note IRS regulations state that health needs include the requisites for the improvement or maintenance of health status both in the community at large and in particular parts of the community (such as neighborhoods or populations experiencing health disparities) The regulations also note that these needs may include the need to address financial and other barriers to accessing care, to prevent illness, to ensure adequate nutrition, or to address social, behavioral, and environmental factors that influence health in the community A hospital may determine whether a health need is significant based on all of the facts and circumstances present in the community it serves (1. 501(r)-3(b)(4) © HTS 3 2016 | Page 16
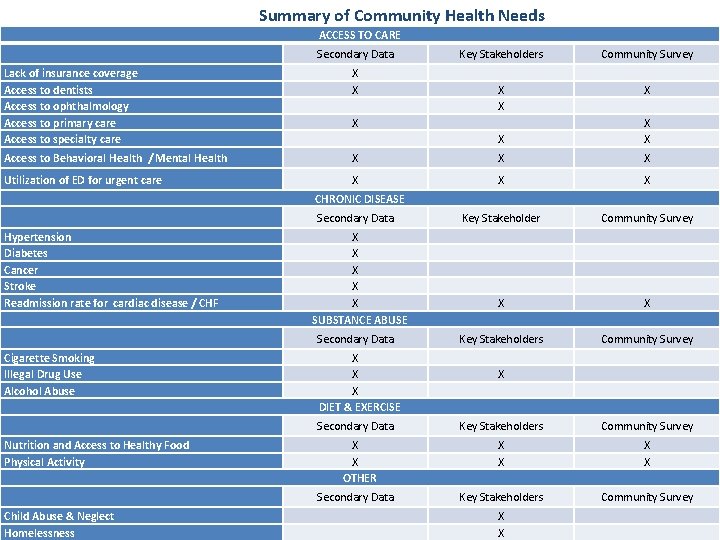
Summary of Community Health Needs ACCESS TO CARE Secondary Data Lack of insurance coverage Access to dentists Access to ophthalmology Access to primary care Access to specialty care X X Access to Behavioral Health / Mental Health Utilization of ED for urgent care Key Stakeholders Community Survey X X X X Key Stakeholder Community Survey X X Key Stakeholders Community Survey CHRONIC DISEASE Secondary Data Hypertension Diabetes Cancer Stroke Readmission rate for cardiac disease / CHF X X X SUBSTANCE ABUSE Secondary Data Cigarette Smoking Illegal Drug Use Alcohol Abuse X X X DIET & EXERCISE Secondary Data Nutrition and Access to Healthy Food Physical Activity X X OTHER Secondary Data Child Abuse & Neglect © HTS 3 2016 | Page 17 Homelessness X Key Stakeholders Community Survey X X
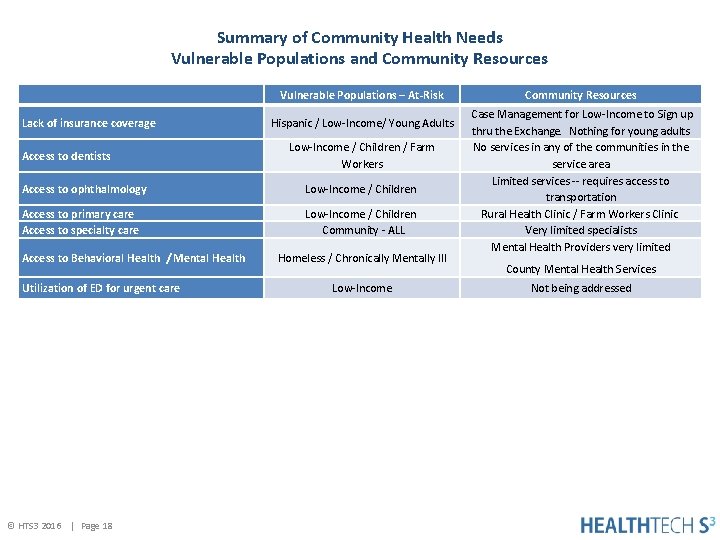
Summary of Community Health Needs Vulnerable Populations and Community Resources Vulnerable Populations – At-Risk Lack of insurance coverage Access to dentists Hispanic / Low-Income/ Young Adults Low-Income / Children / Farm Workers Access to ophthalmology Low-Income / Children Access to primary care Access to specialty care Low-Income / Children Community - ALL Access to Behavioral Health / Mental Health Utilization of ED for urgent care © HTS 3 2016 | Page 18 Homeless / Chronically Mentally Ill Low-Income Community Resources Case Management for Low-Income to Sign up thru the Exchange. Nothing for young adults No services in any of the communities in the service area Limited services -- requires access to transportation Rural Health Clinic / Farm Workers Clinic Very limited specialists Mental Health Providers very limited County Mental Health Services Not being addressed
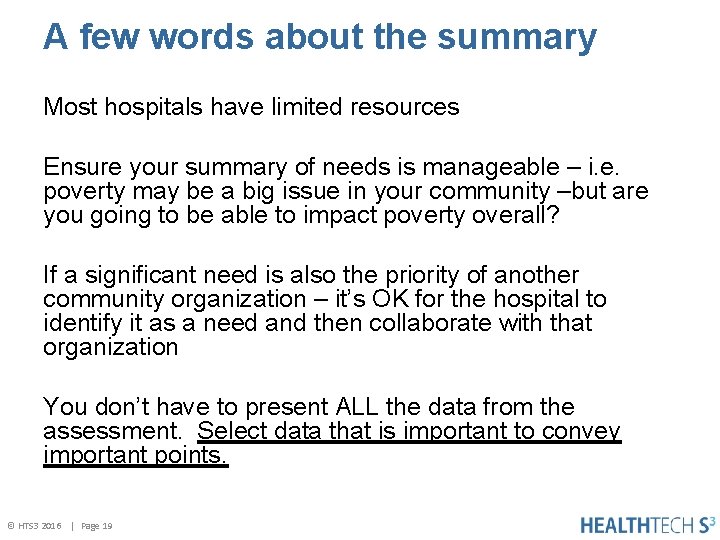
A few words about the summary Most hospitals have limited resources Ensure your summary of needs is manageable – i. e. poverty may be a big issue in your community –but are you going to be able to impact poverty overall? If a significant need is also the priority of another community organization – it’s OK for the hospital to identify it as a need and then collaborate with that organization You don’t have to present ALL the data from the assessment. Select data that is important to convey important points. © HTS 3 2016 | Page 19
Step 3 Develop priorities © HTS 3 2016 | Page 20
Determine who will be involved in setting priorities • • Executive Team CHNA Steering Committee Board members Key stakeholders / partners There’s not a magic list ---- some hospitals have very large groups ---- others small groups At a minimum include the CHNA steering committee and Public Health © HTS 3 2016 | Page 21
IRS Note Current IRS regulations state that input from persons representing the broad interests of the community should be taken into account in prioritizing significant health needs and identifying resources potentially available to address those needs. © HTS 3 2016 | Page 22
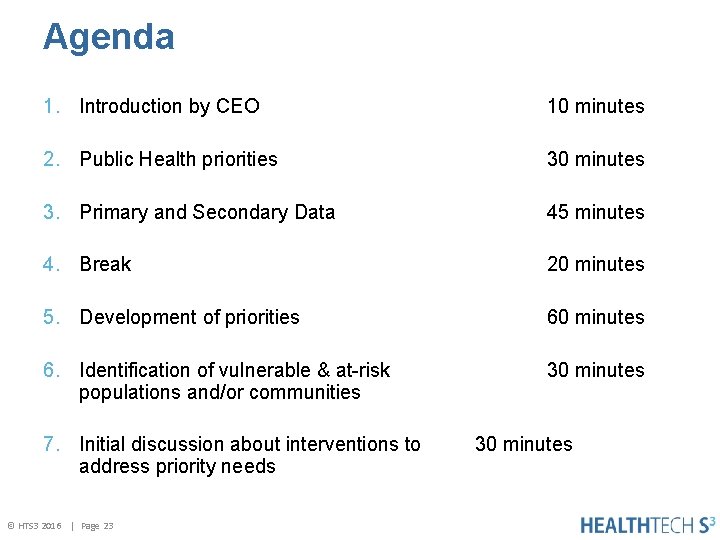
Agenda 1. Introduction by CEO 10 minutes 2. Public Health priorities 30 minutes 3. Primary and Secondary Data 45 minutes 4. Break 20 minutes 5. Development of priorities 60 minutes 6. Identification of vulnerable & at-risk populations and/or communities 30 minutes 7. Initial discussion about interventions to address priority needs © HTS 3 2016 | Page 23 30 minutes
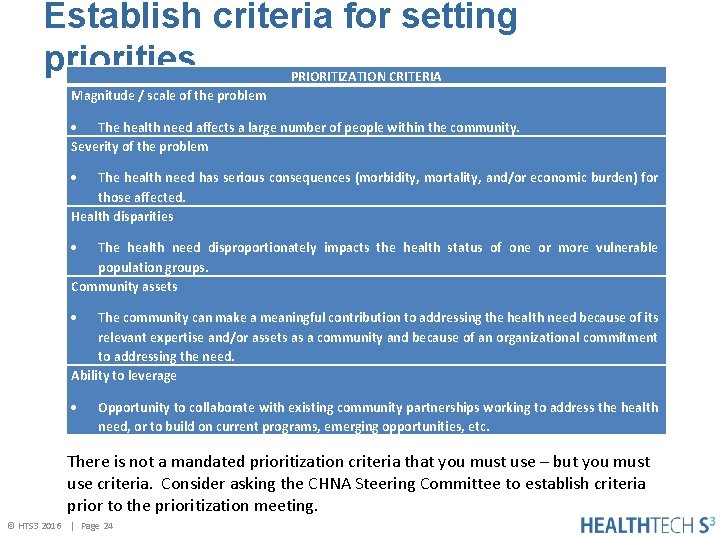
Establish criteria for setting priorities PRIORITIZATION CRITERIA Magnitude / scale of the problem The health need affects a large number of people within the community. Severity of the problem The health need has serious consequences (morbidity, mortality, and/or economic burden) for those affected. Health disparities The health need disproportionately impacts the health status of one or more vulnerable population groups. Community assets The community can make a meaningful contribution to addressing the health need because of its relevant expertise and/or assets as a community and because of an organizational commitment to addressing the need. Ability to leverage Opportunity to collaborate with existing community partnerships working to address the health need, or to build on current programs, emerging opportunities, etc. There is not a mandated prioritization criteria that you must use – but you must use criteria. Consider asking the CHNA Steering Committee to establish criteria prior to the prioritization meeting. © HTS 3 2016 | Page 24
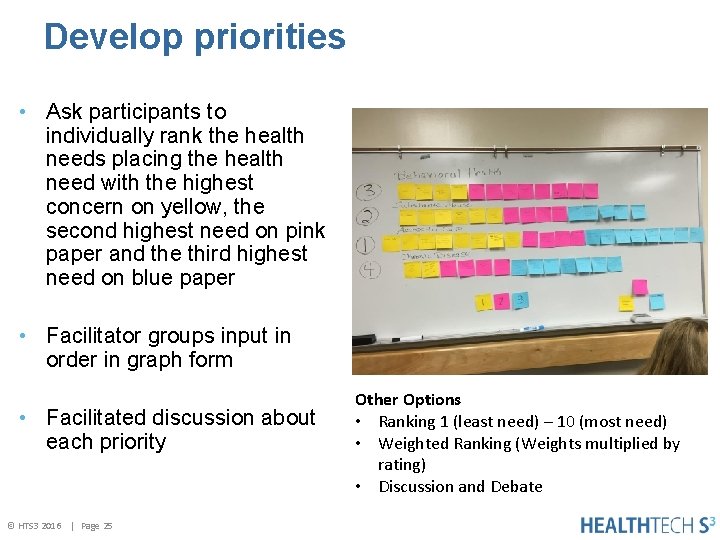
Develop priorities • Ask participants to individually rank the health needs placing the health need with the highest concern on yellow, the second highest need on pink paper and the third highest need on blue paper • Facilitator groups input in order in graph form • Facilitated discussion about each priority © HTS 3 2016 | Page 25 Other Options • Ranking 1 (least need) – 10 (most need) • Weighted Ranking (Weights multiplied by rating) • Discussion and Debate

Too Big Too Little Just Right © HTS 3 2016 | Page 26 Too Many Not Enough Just
Identify at-risk populations / groups / communities © HTS 3 2016 | Page 27

Begin discussions about community partners and implementation strategies © HTS 3 2016 | Page 28
Important Considerations Depending on who you invited to the meeting to determine priorities you will need to validate priorities with community members and key stakeholders including public health If you have completed a community survey or community focus groups --- that is one way to show community input © HTS 3 2016 | Page 29

Step 4 Governing Board Approval • Incorporate prioritized community health needs in your Community Health Needs Assessment • Request governing board approval of CHNA © HTS 3 2016 | Page 30
World Health Organization The context of people’s lives determine their health, and so blaming individuals for having poor health or crediting them for good health is inappropriate. © HTS 3 2016 | Page 31
If you would like to talk about your CHNA Please contact me Carolyn St. Charles Regional Chief Clinical Officer carolyn. stcharles@healthtech. S 3. com 360 -584 -9868 © HTS 3 2016 | Page 32
Upcoming Webinars November 4, 2016: A Deep Dive: Continuous Survey Readiness – Myth or Reality? Click here to register -- http: //bit. ly/2 e. KJm. Rt Continuous Survey Readiness is something every Hospital strives for – but how do you get there? Our webinar will discuss practical ways of ensuring continuous survey readiness for every Hospital – regardless of size 12: 00 – 1: 00 p. m. CDT Hosted By: Carolyn St. Charles, MBA, BSN Regional Chief Clinical Officer December 2, 2016: Community Health Needs Assessment: Developing an Action Plan Click here to register -- http: //bit. ly/2 e. KJTDb Hospitals have 4 ½ months after completion of the Community Health Needs Assessment to develop an action plan in collaboration with community partners. Join us and learn about how to develop a realistic, actionable plan. 12: 00 – 1: 00 p. m. CDT Hosted By: Carolyn St. Charles, MBA, BSN Regional Chief Clinical Officer November 10, 2016: Social Media and the Protection of Residents Click here to register -- http: //bit. ly/2 e. KLk. Br Helping your long-term care residents’ successfully return home requires planning, goal development and follow-up services. Additionally you must consider community and care giver resources as well as equipment and medication management. This webinar will include a discussion on patient-centered discharge planning that will help your residents achieve their goals. 12: 00 – 1: 00 p. m. CDT Hosted By: Cheri Benander, MSN, RN, NHA, CHC, NHCE-C December 12, 2016: Leading Change: Shifting to Population Health Management Click here to register -- http: //bit. ly/2 e. KM 8 Gk With the rapidly changing health care landscape, the goals for organizations are to assure better outcomes and lower costs. The challenge of shifting to a population health management model can be a daunting effort. 12: 00 – 1: 00 p. m. CDT Hosted By: Diane Bradley, Ph. D, RN, NEA-BC, CPHQ, FACHE, FACHCA Regional Chief Clinical Officer November 21, 2016: Clinical Integration and Care Coordination: A Means to Reducing Fragmentation Click here to register -- http: //bit. ly/2 e. KIWd. V Organizations actively pursuing population health management must focus their energy on providing efficient and effective care delivery in the best possible setting. This is accomplished through the development of a clinically integrated network. Clinical integration is only achieved by understanding the connection between data analytics and technology. 12: 00 – 1: 00 p. m. CDT Hosted By: Diane Bradley, Ph. D, RN, NEA-BC, CPHQ, FACHE, FACHCA Regional Chief Clinical Officer © HTS 3 2016 | Page 33
- Slides: 33