Community Family Health and Equity Achieving Health Equity





- Slides: 24

Community, Family Health and Equity Achieving Health Equity Ana P. Novais, MA, Executive Director of Health RI Department of Health August 2, 2010
Community, Family Health & Equity • Community- because all health is local • Family- because families are our key partners in health • Equity- because our mission is to assure that all Rhode Islanders will achieve optimal health
Who we are? • CFHE works to eliminate health disparities by assuring healthy child development, preventing and controlling disease and disability. • CHFE plans, develops, and evaluates programs and systems, which are comprehensive, community-based, culturally competent, coordinated and effective.
Who we are? • CFHE uses a life course developmental approach and addresses the determinants of health as a framework for health planning. • CFHE recognizes that social, political and economic policies and conditions determine health outcomes.
Community, Family Health & Equity • Our values guide us in the work we do internally and with our key partners. • Our six teams represent priority areas that promote synergy, collaboration, integration and coordination among programs.
Community, Family Health & Equity • • • Health Disparities and Access to Care Healthy Homes and Environments Chronic Care and Disease Management Health Promotion and Wellness Perinatal and Early Childhood Health Preventive Services and Community Practices
Community, Family Health & Equity • Social, physical and economic determinants of health • Program integration • Life course approach • Across the lifespan
Social Environments as Determinants of Health • Social determinants of health include interactions with family, friends, co-workers in settings like schools, neighborhoods, workplaces, businesses, places of worship; health care settings, recreational facilities. • Institutions such as law enforcement agencies, governmental and non-governmental agencies; and economic policy influence individual health and health behavior.
Social Environments as Determinants of Health • Social attitudes such as discrimination, prejudices and stereotypes; • as well as culture, language, political and religious beliefs also play a role.
Community and Physical Environments • Language, beliefs, social norms and attitudes (for example, discriminatory or stigmatizing attitudes to minorities) in a community influence health. • Socioeconomic conditions (e. g. Poverty, exposure to crime and violence, signs of social disorder such as trash and grafitti) are reflected in the social environment.
Community and Physical Environments • Policies made in governmental, corporate and nongovernmental sectors can impact health and health behaviors in whole populations both positively and negatively. • Physical environment- including the natural and built environments- can harm individual and community health when individuals and communities are exposed to toxic substances, irritants, infectious agents, and noise.
SDH: Education • Education influences the type of jobs one has, how much money one earns, the opportunities one has for access to health care… – 2008 RI four-year graduation rate for all high school students was 74% (69% for males and 79% for females) – 2008 RI drop out rate was 16%

SDH: Poverty • Poor individuals are less likely to have access to health coverage, a usual source of care, routine screenings and check-ups, healthy food, safe opportunities for physical activity. In RI (2007 -2008) – – 13. 9% of the population 21. 5% of children 18 and under 13. 9% of adults 19 to 64 11% of elderly 65 and older lived below poverty
SDH: Poverty & Race • In RI (2007 -2008) – 10. 7% of Whites – 31. 2% of Blacks – 36. 6% of Hispanics – 28. 2% of other groups lived below poverty

CFHE Integration Initiative • Creates a common vision of a healthy community that will increase HEALTH’s impact • Mobilizes and leverages resources efficiently across categorical diseases, programs, data and analysis, and community level interest and activity

CFHE Integration Initiative • • • Joint leadership Joint planning and quality initiatives Common outcomes Common policies Common financing and implementation at the state and local level
Lifecourse Health Development • Health accumulates across the lifespan • Results from multiple risks, protective and promoting factors • Represented by “trajectory” • Critical/Sensitive periods: weathering, how poverty gets “under the skin” • Factors influencing disparities vs disease
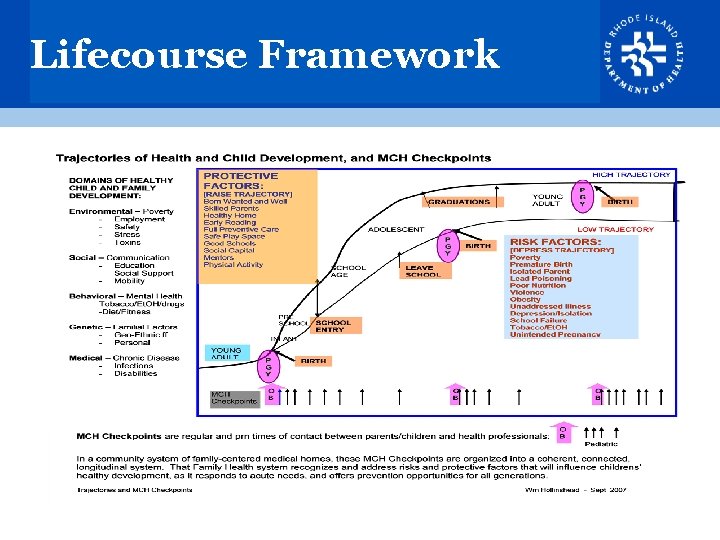
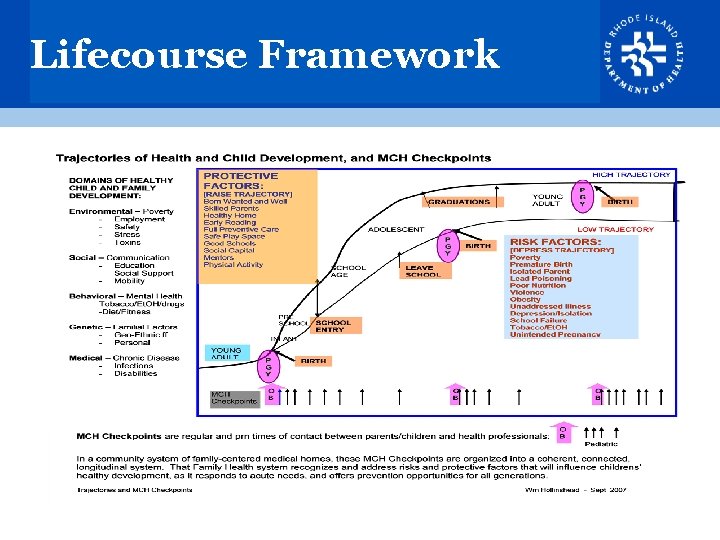
Lifecourse Framework
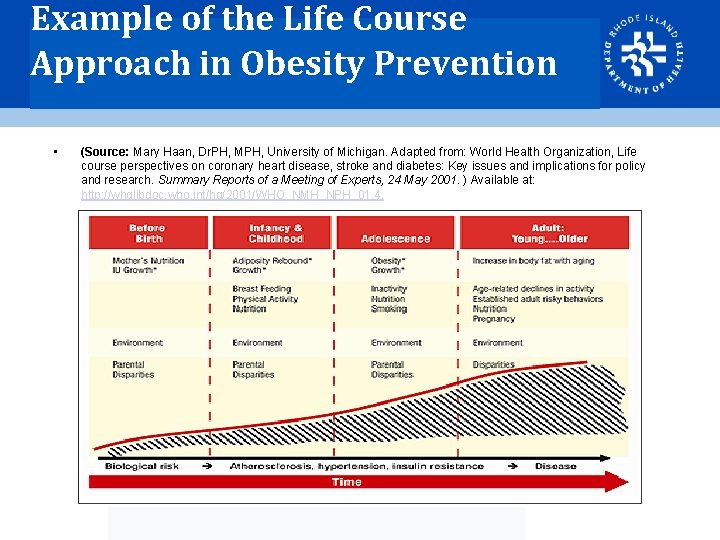
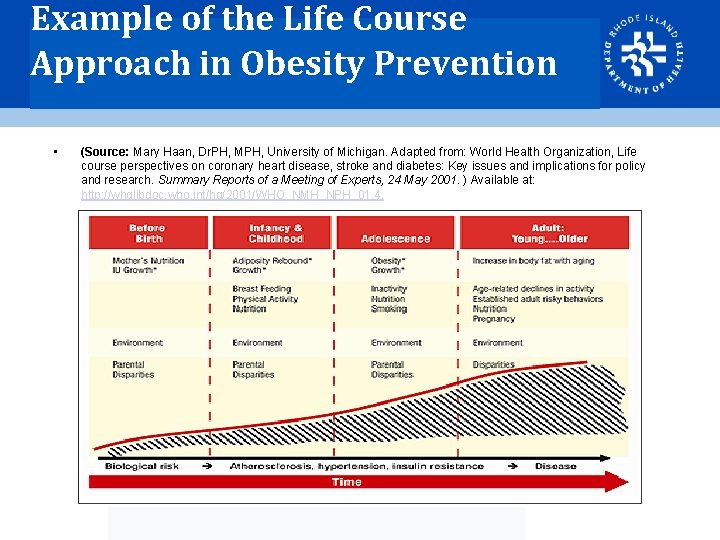
Example of the Life Course Approach in Obesity Prevention • (Source: Mary Haan, Dr. PH, MPH, University of Michigan. Adapted from: World Health Organization, Life course perspectives on coronary heart disease, stroke and diabetes: Key issues and implications for policy and research. Summary Reports of a Meeting of Experts, 24 May 2001. ) Available at: http: //whqlibdoc. who. int/hq/2001/WHO_NMH_NPH_01. 4.
Community, Family Health & Equity • Social, physical and economic determinants of health • Life course approach • Program integration • Across the lifespan

Equity Pyramid Lowest Impact (1) 1. Education & Counseling e. g. Eat Right 2. Clinical Interventions e. g. diabetes control; pediatric weight management counseling 3. Long Lasting Protective Public Health Interventions e. g. immunizations; HIV testing; BMI screening? 4. Changing the Context-Healthy Choices as Default Options e. g. smoke free laws; healthy food in schools law Highest Impact (5) 5. Social and Environmental Determinants of Health e. g. housing, education, inequalities; community garden This pyramid is adapted from Thomas Frieden, MD, MPH presentation at the Weight of the Nation conference, Washington D. C. , July 27, 2009
Healthy Rhode Island 2010 banners
Questions? Ana P. Novais (401) 222 -1171 ana. novais@health. ri. gov Peter Simon, MD, MPH 401. 222. 5928 peter. simon@health. ri. gov Resources: www. health. ri. gov
 The intentional use of unfriendly or offensive behavior
The intentional use of unfriendly or offensive behavior Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 mental and emotional health
Chapter 3 mental and emotional health Chapter 15 achieving mental and emotional health answer key
Chapter 15 achieving mental and emotional health answer key Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 15 achieving mental and emotional health answer key
Chapter 15 achieving mental and emotional health answer key Achieving mental and emotional health
Achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 15 achieving mental and emotional health
Chapter 15 achieving mental and emotional health Family and community health advisor
Family and community health advisor Duke family medicine and community health
Duke family medicine and community health Family care plan in community health nursing
Family care plan in community health nursing Occupational health nurse roles and responsibilities
Occupational health nurse roles and responsibilities Achieving operational excellence and customer intimacy
Achieving operational excellence and customer intimacy Strategic fit
Strategic fit Customer intimacy operational excellence
Customer intimacy operational excellence Implied uncertainty spectrum
Implied uncertainty spectrum Includes the individual and the family community is
Includes the individual and the family community is Nogdawindamin sault ste marie
Nogdawindamin sault ste marie Conjugal family
Conjugal family The role of project management in achieving project success
The role of project management in achieving project success Achieving cardiorespiratory fitness can
Achieving cardiorespiratory fitness can