Communication Assessment Chapter 3 Perry C Hanavan Au
- Slides: 22
Communication Assessment Chapter 3 Perry C. Hanavan, Au. D.
Goals of Initial Assessment ODetermine communication demands in everyday life OEvaluate impact of hearing loss OIdentify settings where problems arise ODocument social activities in which person engages OAssess effective use of communication strategies OChronicle employment responsibilities
Conversational Fluency ODefinition: – how smoothly conversation unfolds
Conversational Fluency Factors OTime spent repairing communication breakdowns – if need for clarification is low, then fluency is high OExchange of information and ideas – is conversation easily and successfully share information, then fluency is high OSpeaking time shared – equal time, few silences, few interruptions, then fluency is high
Index of Sharing Speaking Time OConversational turn: – period participant delivers a contribution to a conversation OMean length (speaking) turn (MLT) – average number of words spoken during a set number of conversational turns OMean length turn ratio (MLT ratio) – ratio of two speakers in a conversation
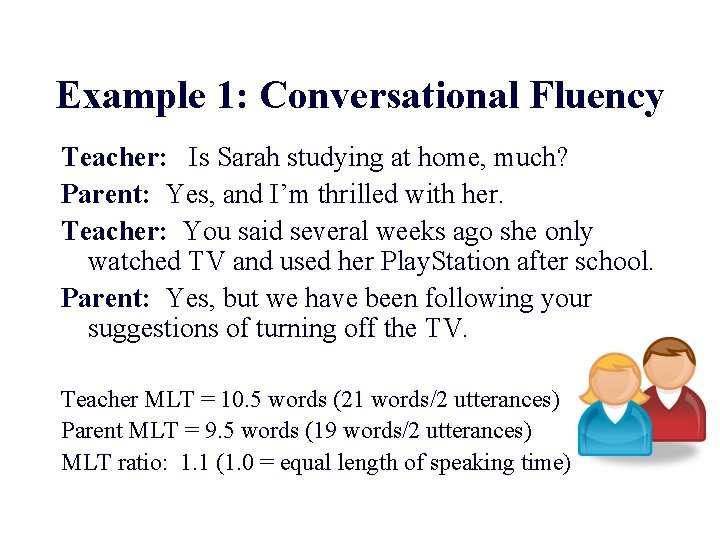
Example 1: Conversational Fluency Teacher: Is Sarah studying at home, much? Parent: Yes, and I’m thrilled with her. Teacher: You said several weeks ago she only watched TV and used her Play. Station after school. Parent: Yes, but we have been following your suggestions of turning off the TV. Teacher MLT = 10. 5 words (21 words/2 utterances) Parent MLT = 9. 5 words (19 words/2 utterances) MLT ratio: 1. 1 (1. 0 = equal length of speaking time)
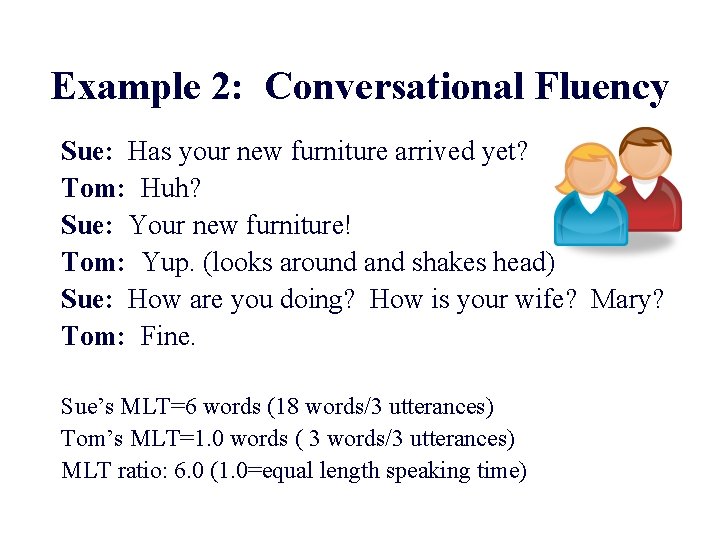
Example 2: Conversational Fluency Sue: Has your new furniture arrived yet? Tom: Huh? Sue: Your new furniture! Tom: Yup. (looks around and shakes head) Sue: How are you doing? How is your wife? Mary? Tom: Fine. Sue’s MLT=6 words (18 words/3 utterances) Tom’s MLT=1. 0 words ( 3 words/3 utterances) MLT ratio: 6. 0 (1. 0=equal length speaking time)
Traditional Audiologic vs Conversational Fluency Measures OMost audiologic test lists present unrelated speech stimuli (spondees, PB words, etc. ) OClients usually must repeat what they hear verbatim (Say the word _____) ONo interaction with communication partners
Problems Measuring Conversational Fluency OVaries with the conversational setting, situation, and communication partner OVaries with the topic of discussion OCommunication breakdowns may not arise in the clinical setting ONo one evaluation adequately measures conversational fluency
Assessment Procedures OInterview OQuestionnaire ODaily Log OGroup Discussion OStructured Communication Interaction OUnstructured Communication Interaction
Interviews OThe client provides subjective impressions of conversational fluency in various settings OAdvantages – client specific information ODisadvantages – difficult to quantify information OExample interview
Questionnaire O Questions that probe subjective information about conversational fluency O Advantages – quick, easy to administer O Disadvantages – may miss client-specific information
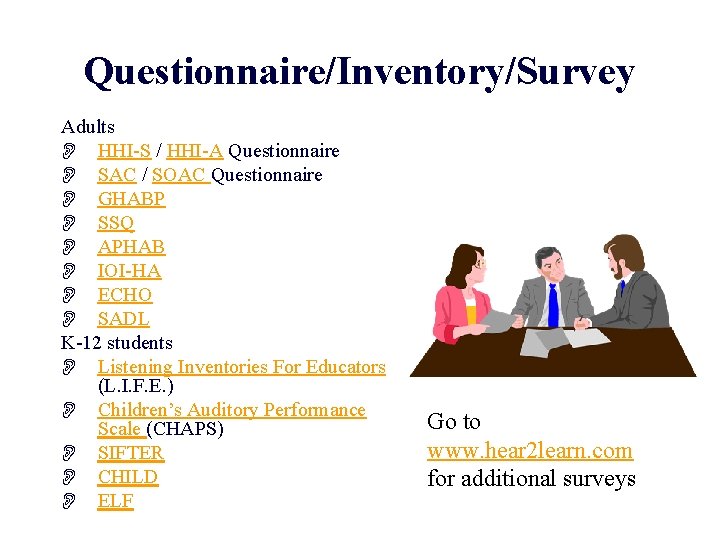
Questionnaire/Inventory/Survey Adults O HHI-S / HHI-A Questionnaire O SAC / SOAC Questionnaire O GHABP O SSQ O APHAB O IOI-HA O ECHO O SADL K-12 students O Listening Inventories For Educators (L. I. F. E. ) O Children’s Auditory Performance Scale (CHAPS) O SIFTER O CHILD O ELF Go to www. hear 2 learn. com for additional surveys
O There a variety of outcome measures used by audiologists. An outcome measure may be address one or more outcome domains: impairment, activity, participation, satisfaction, and health-related quality of life. Some outcome measures such as pure tone thresholds, insertion gain, and audibility index (AI) are used every day and provide objective evidence of patient status. These are outcome measures in the impairment domain. Speech recognition scores (W-22, NU-6, SPIN, HINT, etc. ), the Abbreviated Profile of Hearing Aid Benefit (APHAB; Cox and Alexander, 1995), Client Oriented Scale of Improvement (COSI; Dillon et al. 1997), and the Glasgow Hearing Aid Benefit Profile (Gatehouse, 1999) are examples of outcome measures in the activity domain. The APHAB, for example, asks the patient to rate the frequency he/she has problems in a specific situation: 'I have difficulty hearing a conversation when I’m with one of my family at home. ' The Hearing Handicap Inventory for the Elderly (HHIE; Ventry and Weinstein, 1982), the Hearing Handicap Inventory for Adults (HHIA; Newman et al. 1991), the Abbreviated Profile of Hearing Aid Benefit (APHAB; Cox and Alexander, 1995), the Client Oriented Scale of Improvement (COSI; Dillon et al. 1997), and the Glasgow Hearing Aid Benefit Profile (Gatehouse, 1999) are outcome measures in the participation domain. For example, the HHIE asks the question 'Does a hearing problem cause you to avoid groups of people? ' The Satisfaction with Amplification in Daily Life (SADL) and the ASHA Consumer Satisfaction Measure are examples of outcome measures in the satisfaction domain. For example, the SADL asks the question 'Does wearing your hearing aid(s) improve your self-confidence? ' The HHIE, the Communication Profile for the Hearing Impaired (CPHI; Demorest and Erdman, 1986), the Sickness Impact Profile (SIP; Bergner et al. 1981), the MOS-36 Short Form Health Survey (Ware and Sherbourne, 1992), and the Health Utilities Index (HUI; Feeney et al. 1995) are examples of outcomes measures in the health-related quality of life domain. For example, the SF-36 asks the question 'Compared to a year ago, how would you rate your health in general now? ' There also a number of outcome measures that address the economic aspects of clinical treatment choices. Cost analysis simply measures the cost of treatment (e. g. labor, equipment, supplies, space, utilities, depreciation, overhead). It does not measure 'benefit'. Cost-benefit analysis compares dollars spent against dollars gained or saved by a treatment option. Dollar values are assigned to both the cost of treatment (cost analysis) and the costs saved, or avoided, by the treatment. For example, improved quality of life, reduced family strife, and improved employability are economic benefits to the patient. Willingness to pay analysis is a special category of cost-benefit analysis. Willingness to pay analysis obtains data on the amount individuals are willing to pay for treatment (with or without benefit). Cost effectiveness measures the cost per unit of outcome. For example, how much it cost for each percent change on the APHAB? Cost-utility analysis relates cost to changes in quality of life. One costutility measure is the cost per quality-adjusted life year. This measure compares cost against benefit calculated over a patient’s life expectancy.
Daily Log/Diary OSelf-reports of behavior used by respondents for self-monitoring OAdvantages – quantitative information ODisadvantages – can be a reactive process OExample daily diary
Group Discussion OA forum for members to discuss communication issues OAdvantages – introspection and reflection ODisadvantages – reluctance to participate OExamples: Active Communication Education – discussion topics
Structured Communication Interaction OSimulated communication interactions OAdvantage – good face validity ODisadvantage – can be time consuming to score
Structured Communication Interaction TOPICON O Each participant independently examinees a list of topics and indicates topics of personal interest or familiarity O One participant selects a topic for conversation from the list– reflecting personal interest, that of the other participant, or both O The client and the partner conduct a brief conversation on the chosen topic--2 to 5 minutes while the clinician evaluates the conversation (example) – Background noise, visual distractions, and/or speech and language difficulties may be introduced during the conversation, while the clinician monitors and assesses events O The participants and the clinician discuss the content and fluency of the conversation, considering avoidance or resolution of difficulties. – (Erber, 1996)
Structured Communication Interaction Quest? AR O Conversation-based communication therapy procedure that provides interactive practice with common question-answer sequences. O The client asks a series of questions and learns to anticipate and accurately receive spoken messages O Provides person with hearing loss confidence in asking response-limiting questions ASQUE (yes/no; choice; wh questions, etc. ) – (in Erber, 1996)
Unstructured Communication Interaction O Spontaneous interaction with few external constraints O Free flowing conversation between patient and communication partner O Advantage – good ecological validity—mimics real-world interaction O Disadvantage – results may vary as a function of the communication partner – Example: Dyalog, ratings, transcription analysis
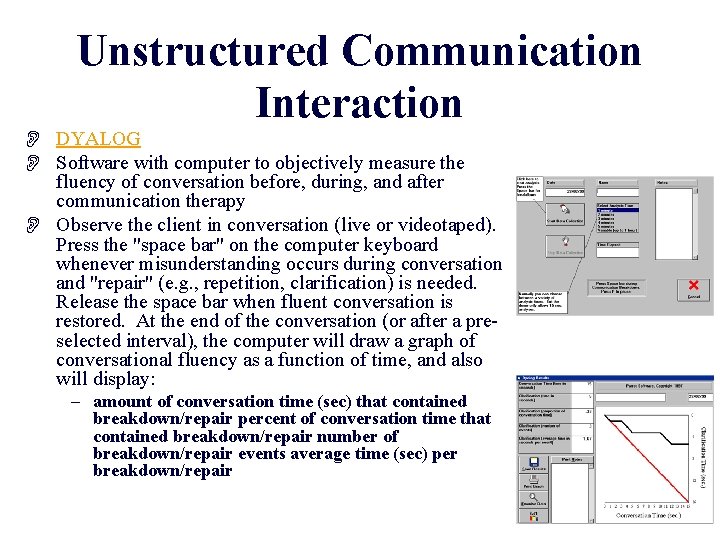
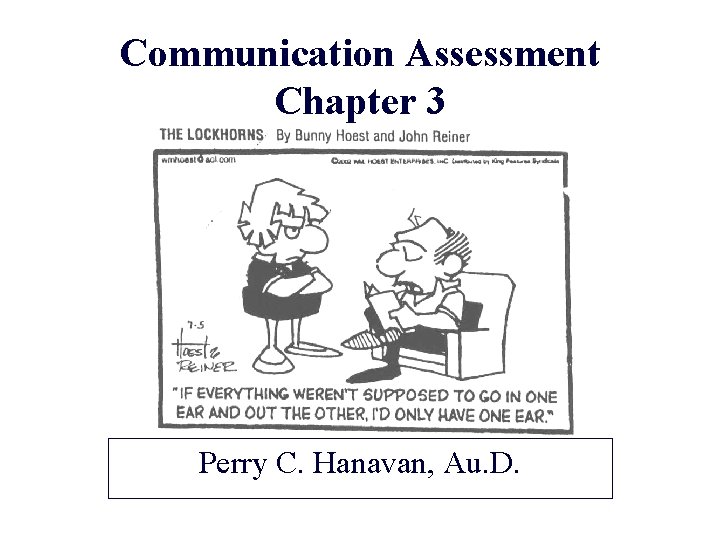
Unstructured Communication Interaction O DYALOG O Software with computer to objectively measure the fluency of conversation before, during, and after communication therapy O Observe the client in conversation (live or videotaped). Press the "space bar" on the computer keyboard whenever misunderstanding occurs during conversation and "repair" (e. g. , repetition, clarification) is needed. Release the space bar when fluent conversation is restored. At the end of the conversation (or after a preselected interval), the computer will draw a graph of conversational fluency as a function of time, and also will display: – amount of conversation time (sec) that contained breakdown/repair percent of conversation time that contained breakdown/repair number of breakdown/repair events average time (sec) per breakdown/repair
Unstructured Communication Interaction ORatings of conversations OTranscription analysis of conversations