Common Worm Infestations in Children Dr Nishant Verma
- Slides: 25
Common Worm Infestations in Children Dr Nishant Verma Department of Pediatrics
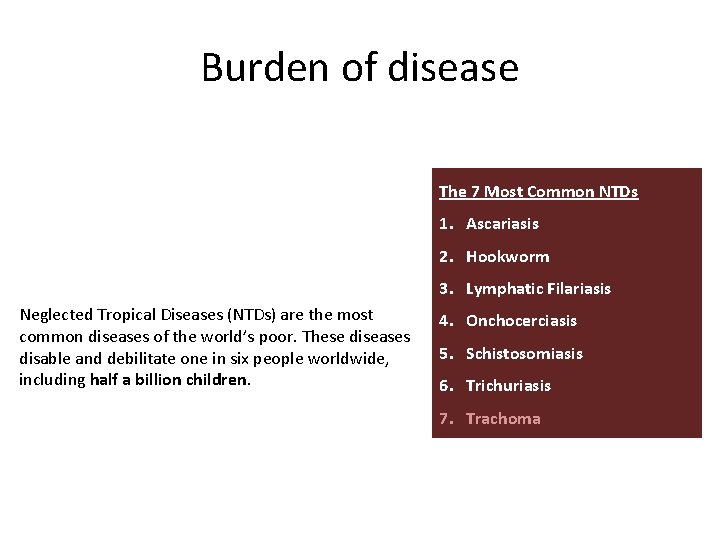
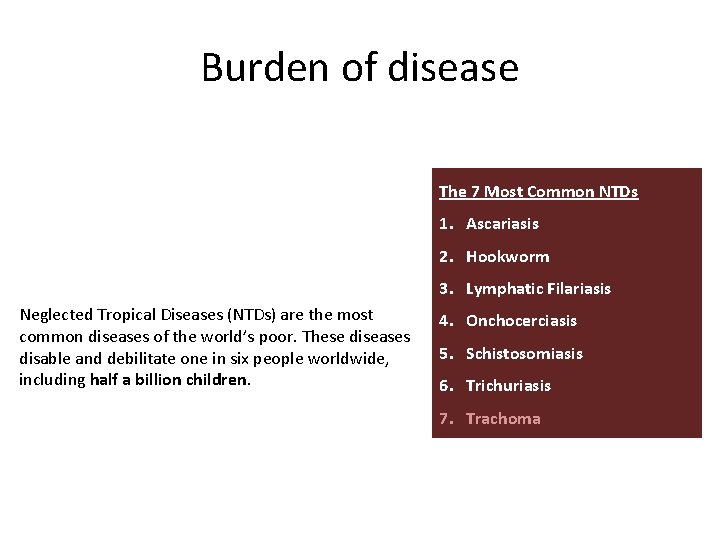
Burden of disease The 7 Most Common NTDs 1. Ascariasis 2. Hookworm 3. Lymphatic Filariasis Neglected Tropical Diseases (NTDs) are the most common diseases of the world’s poor. These diseases disable and debilitate one in six people worldwide, including half a billion children. 4. Onchocerciasis 5. Schistosomiasis 6. Trichuriasis 7. Trachoma
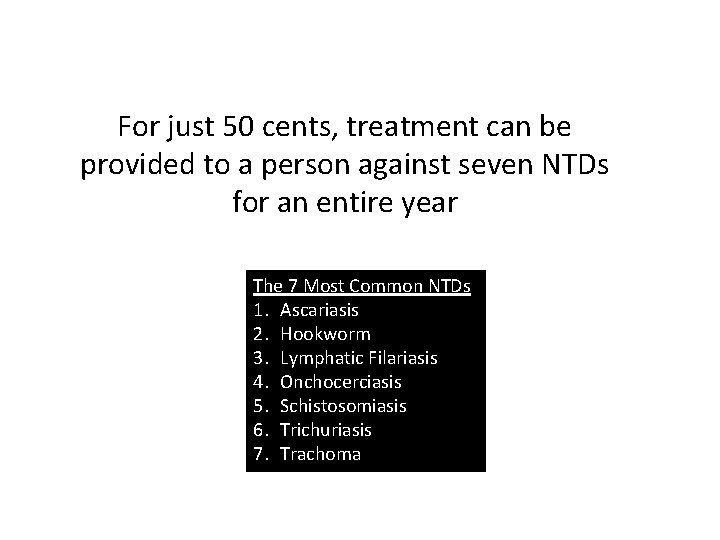
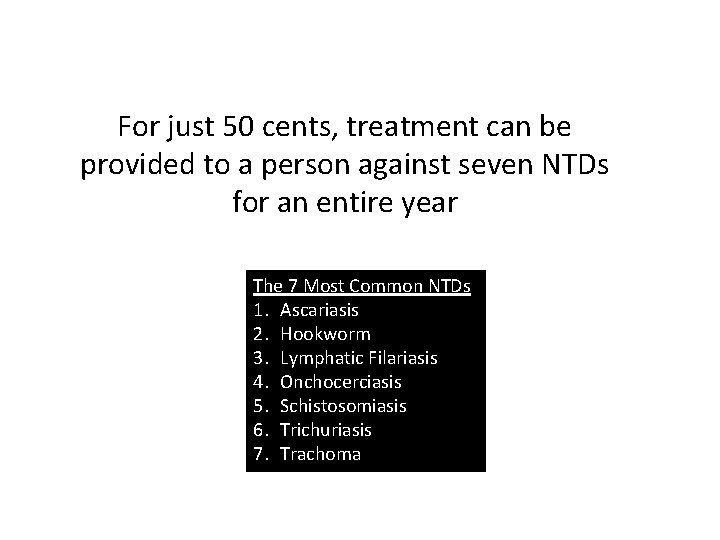
For just 50 cents, treatment can be provided to a person against seven NTDs for an entire year The 7 Most Common NTDs 1. Ascariasis 2. Hookworm 3. Lymphatic Filariasis 4. Onchocerciasis 5. Schistosomiasis 6. Trichuriasis 7. Trachoma
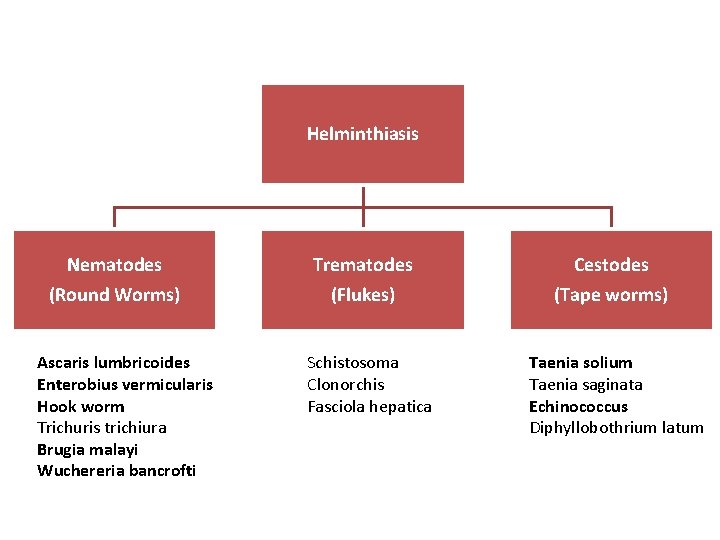
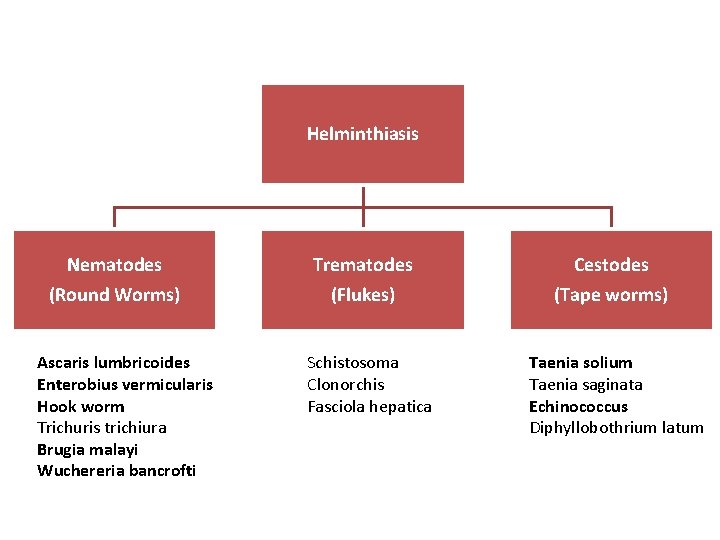
Helminthiasis Nematodes (Round Worms) Ascaris lumbricoides Enterobius vermicularis Hook worm Trichuris trichiura Brugia malayi Wuchereria bancrofti Trematodes (Flukes) Schistosoma Clonorchis Fasciola hepatica Cestodes (Tape worms) Taenia solium Taenia saginata Echinococcus Diphyllobothrium latum
Ascaris lumbricoides – Life cycle
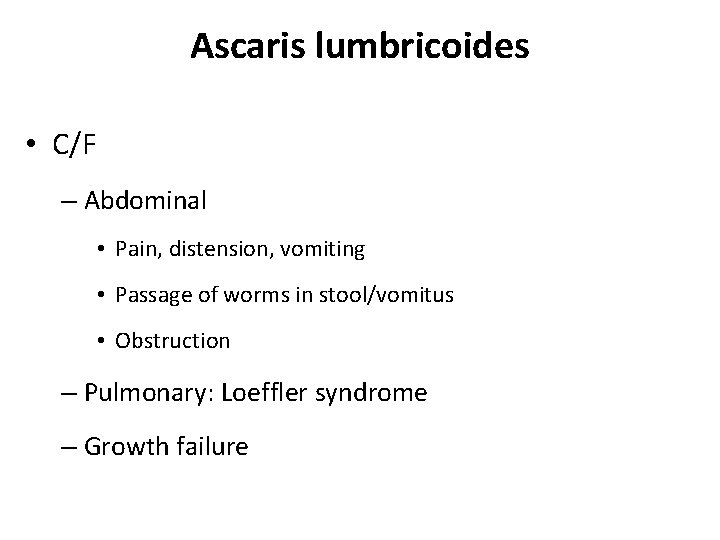
Ascaris lumbricoides • C/F – Abdominal • Pain, distension, vomiting • Passage of worms in stool/vomitus • Obstruction – Pulmonary: Loeffler syndrome – Growth failure
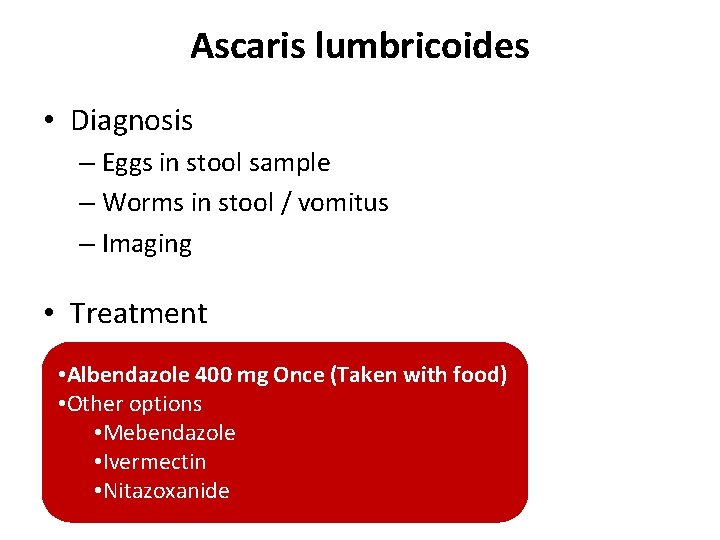
Ascaris lumbricoides • Diagnosis – Eggs in stool sample – Worms in stool / vomitus – Imaging • Treatment • Albendazole 400 mg Once (Taken with food) • Other options • Mebendazole • Ivermectin • Nitazoxanide
Enterobius vermicularis (Pin Worm) • Peri-anal itching • More at night
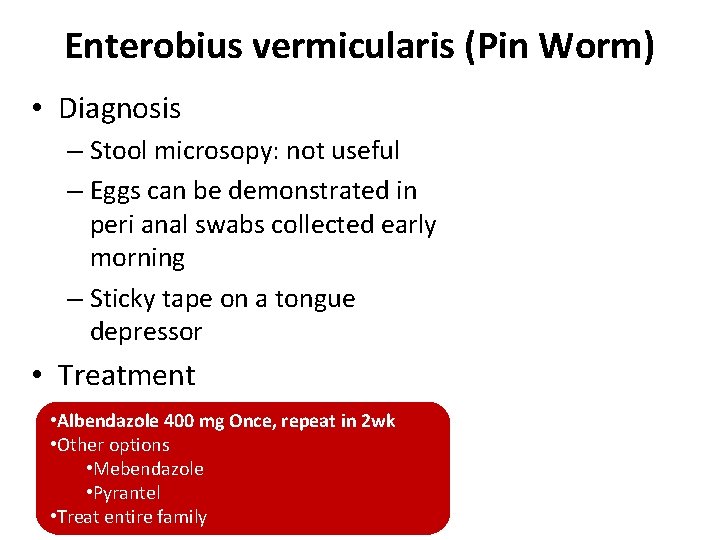
Enterobius vermicularis (Pin Worm) • Diagnosis – Stool microsopy: not useful – Eggs can be demonstrated in peri anal swabs collected early morning – Sticky tape on a tongue depressor • Treatment • Albendazole 400 mg Once, repeat in 2 wk • Other options • Mebendazole • Pyrantel • Treat entire family
Hook worm Ancylostoma duodenale / Necator americanus
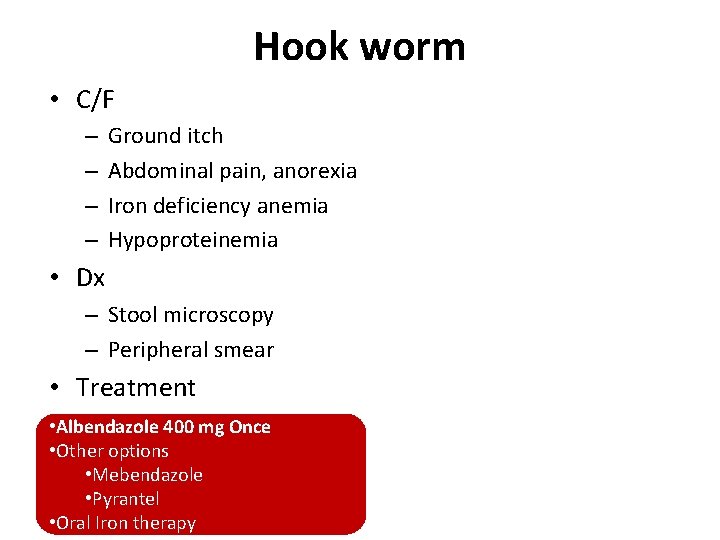
Hook worm • C/F – – Ground itch Abdominal pain, anorexia Iron deficiency anemia Hypoproteinemia • Dx – Stool microscopy – Peripheral smear • Treatment • Albendazole 400 mg Once • Other options • Mebendazole • Pyrantel • Oral Iron therapy
Filariasis Wuchereria bancrofti, Brugia malayi, B. timori
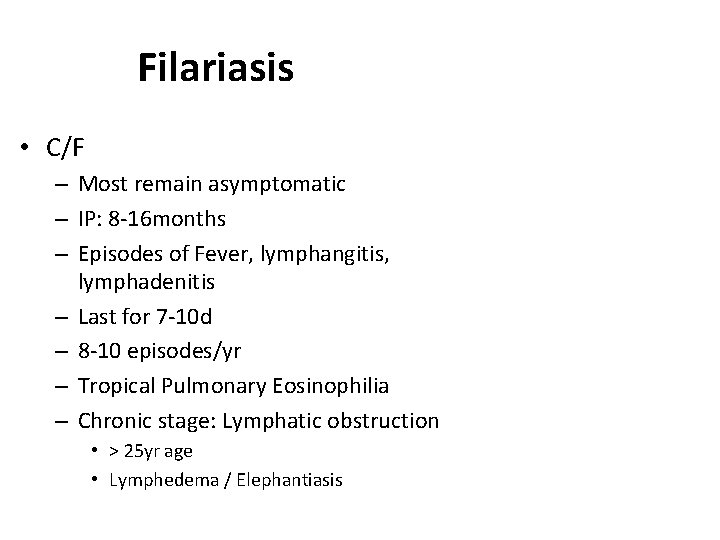
Filariasis • C/F – Most remain asymptomatic – IP: 8 -16 months – Episodes of Fever, lymphangitis, lymphadenitis – Last for 7 -10 d – 8 -10 episodes/yr – Tropical Pulmonary Eosinophilia – Chronic stage: Lymphatic obstruction • > 25 yr age • Lymphedema / Elephantiasis
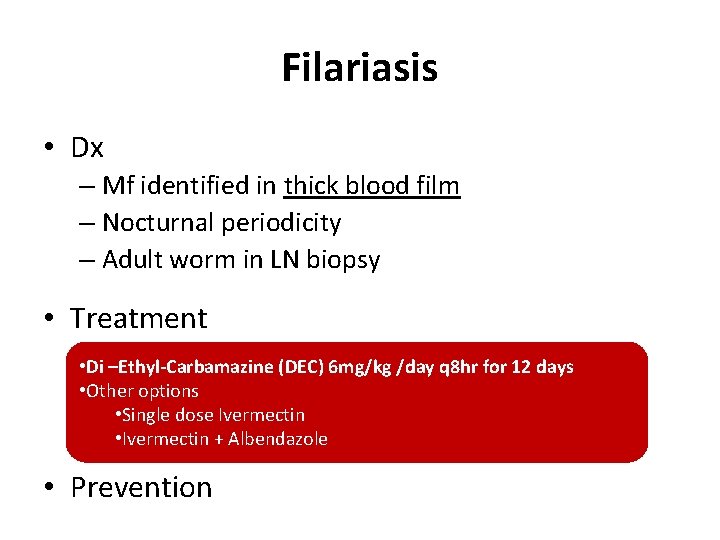
Filariasis • Dx – Mf identified in thick blood film – Nocturnal periodicity – Adult worm in LN biopsy • Treatment • Di –Ethyl-Carbamazine (DEC) 6 mg/kg /day q 8 hr for 12 days • Other options • Single dose Ivermectin • Ivermectin + Albendazole • Prevention
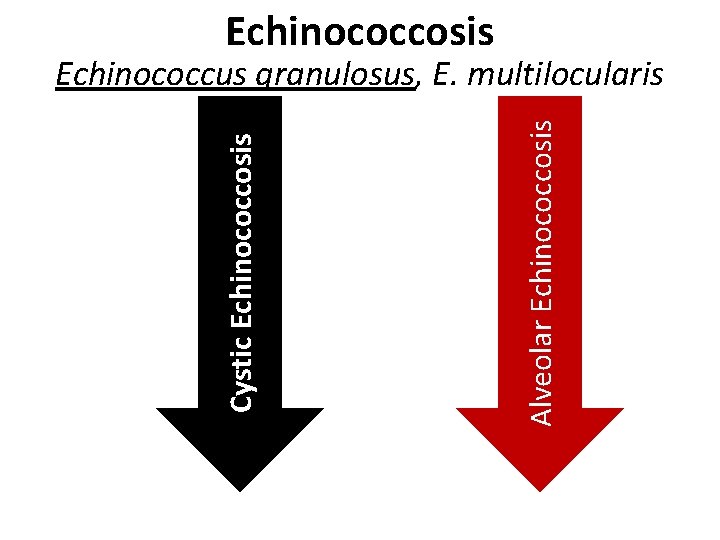
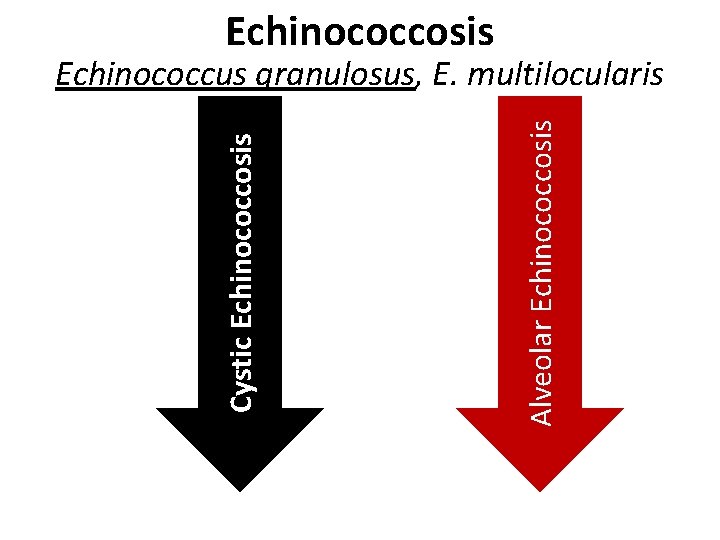
Echinococcosis Alveolar Echinococcosis Cystic Echinococcosis Echinococcus granulosus, E. multilocularis
Echinococcosis • C/F – Site and mass effect of the cyst – Rupture: fever, anaphylaxis
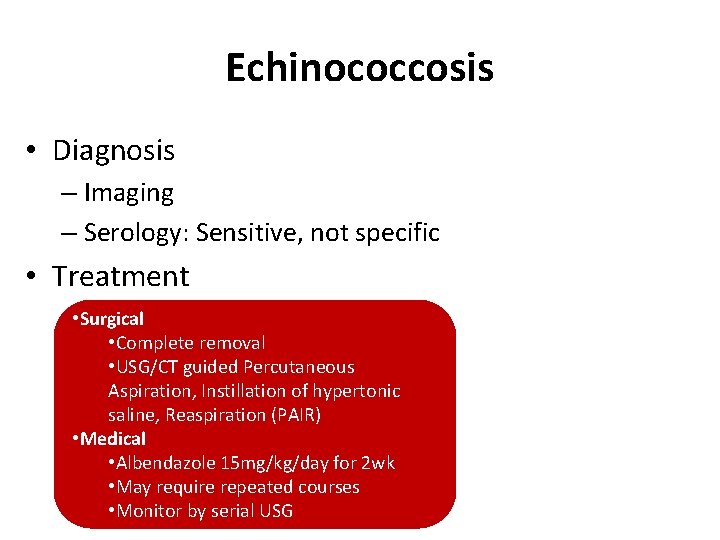
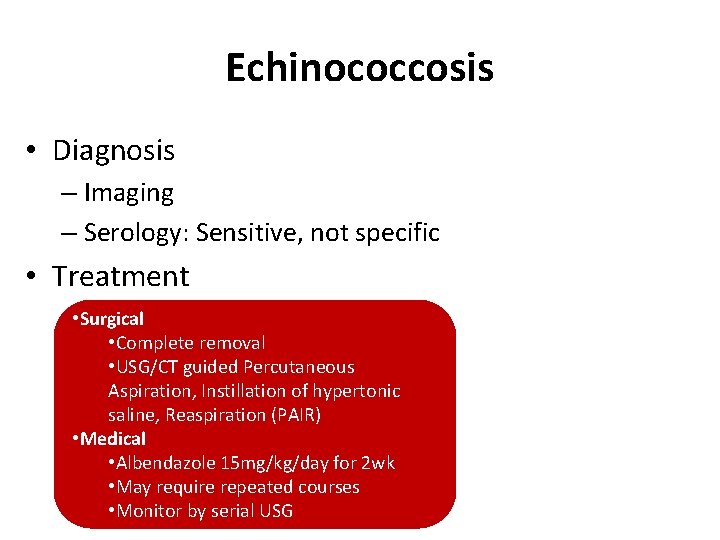
Echinococcosis • Diagnosis – Imaging – Serology: Sensitive, not specific • Treatment • Surgical • Complete removal • USG/CT guided Percutaneous Aspiration, Instillation of hypertonic saline, Reaspiration (PAIR) • Medical • Albendazole 15 mg/kg/day for 2 wk • May require repeated courses • Monitor by serial USG
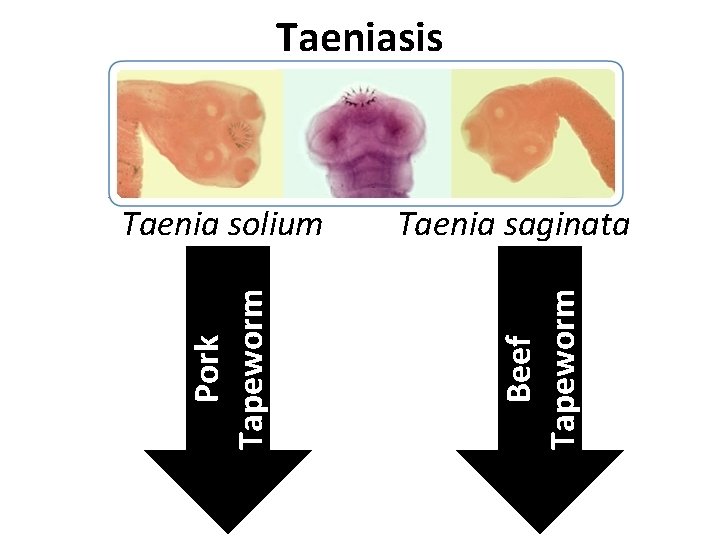
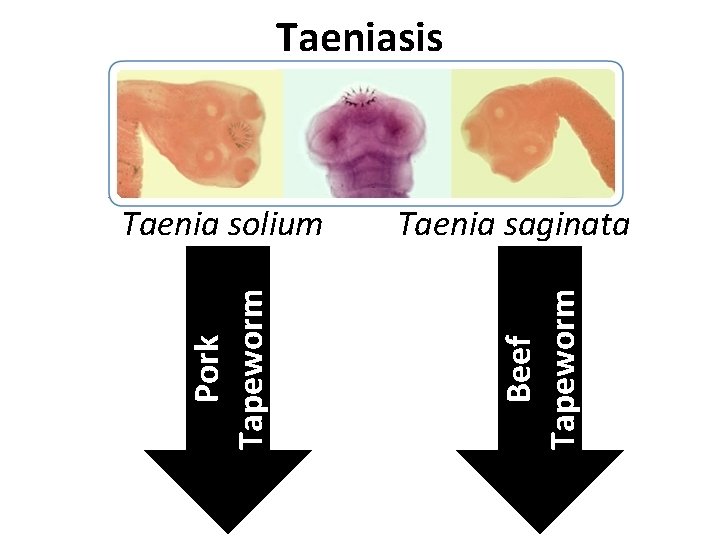
Taeniasis Taenia saginata Beef Tapeworm Pork Tapeworm Taenia solium
Taeniasis
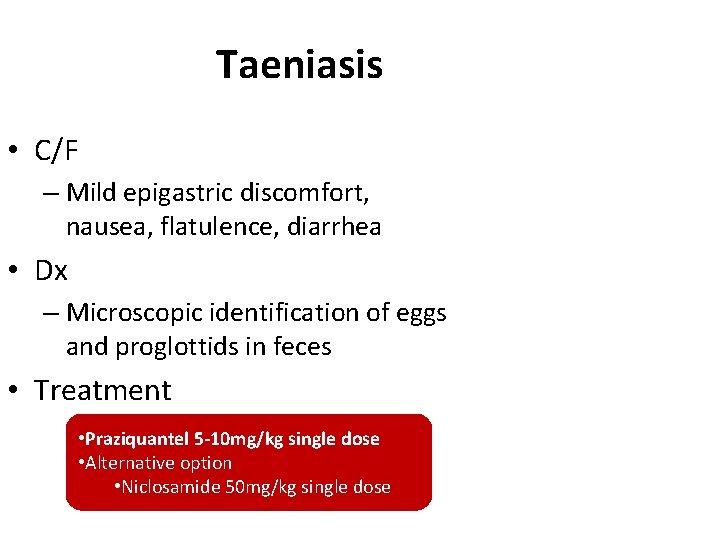
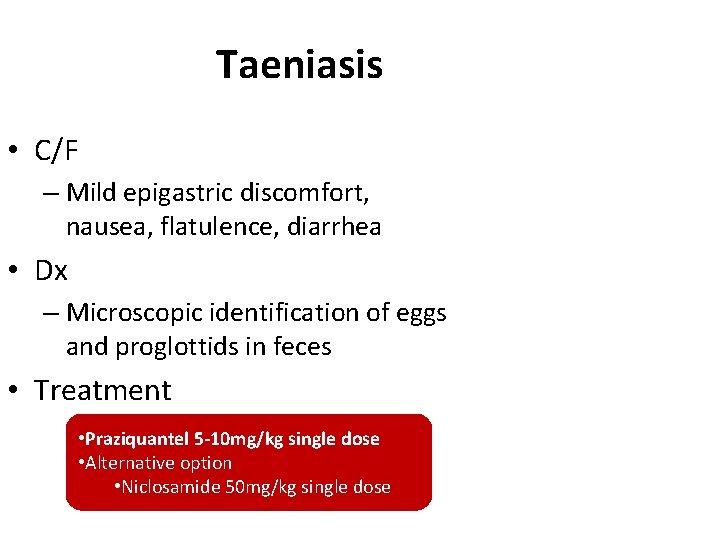
Taeniasis • C/F – Mild epigastric discomfort, nausea, flatulence, diarrhea • Dx – Microscopic identification of eggs and proglottids in feces • Treatment • Praziquantel 5 -10 mg/kg single dose • Alternative option • Niclosamide 50 mg/kg single dose
Cysticercosis
Cysticercosis
Cysticercosis
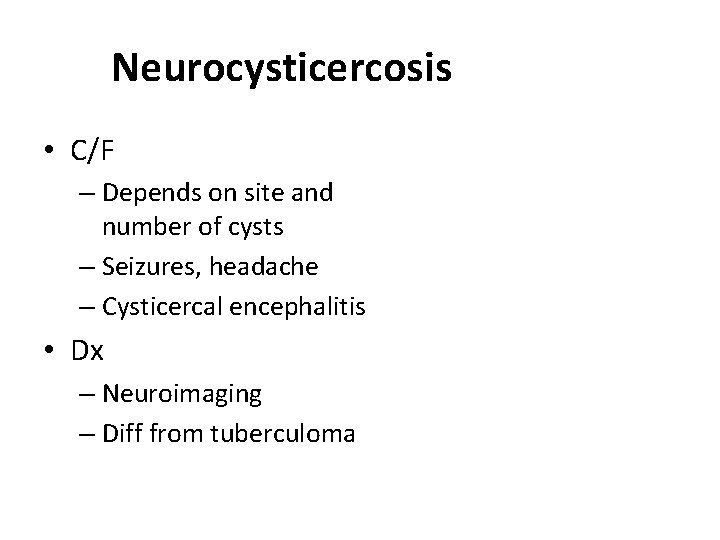
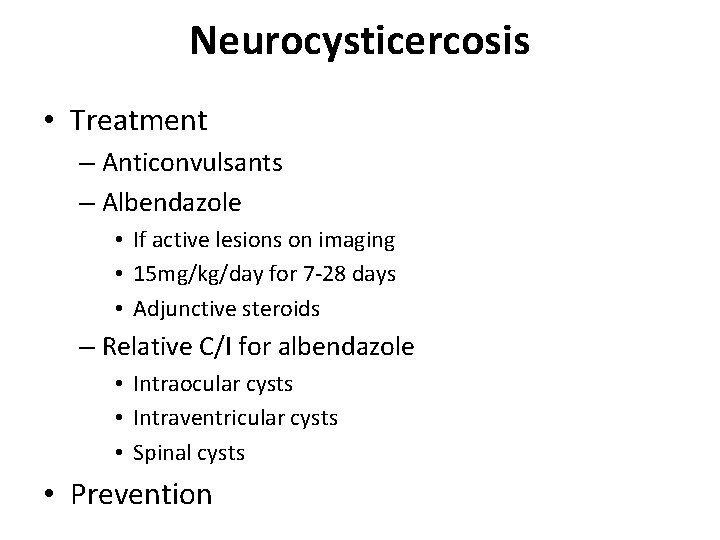
Neurocysticercosis • C/F – Depends on site and number of cysts – Seizures, headache – Cysticercal encephalitis • Dx – Neuroimaging – Diff from tuberculoma
Neurocysticercosis • Treatment – Anticonvulsants – Albendazole • If active lesions on imaging • 15 mg/kg/day for 7 -28 days • Adjunctive steroids – Relative C/I for albendazole • Intraocular cysts • Intraventricular cysts • Spinal cysts • Prevention