Common Skin Diseases for Internists Content Drug reaction



- Slides: 49

Common Skin Diseases for Internists
Content Drug reaction n Scabies n Infectious diseases n Generalized pruritus n
Drug reaction Incidence: 6 -30% n Classification of drug reaction n – non-immunological reaction – Immunological reaction
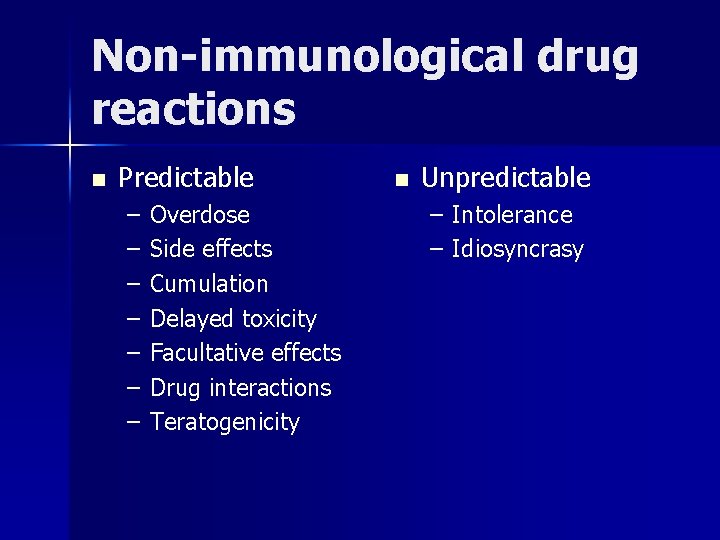
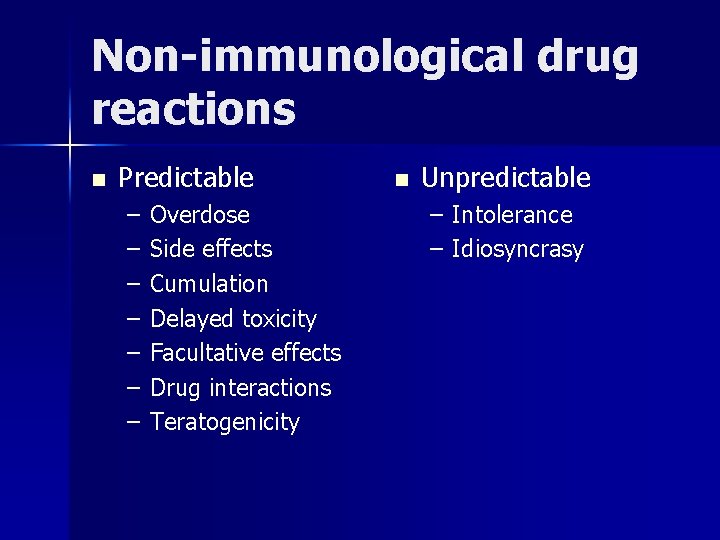
Non-immunological drug reactions n Predictable – – – – Overdose Side effects Cumulation Delayed toxicity Facultative effects Drug interactions Teratogenicity n Unpredictable – Intolerance – Idiosyncrasy
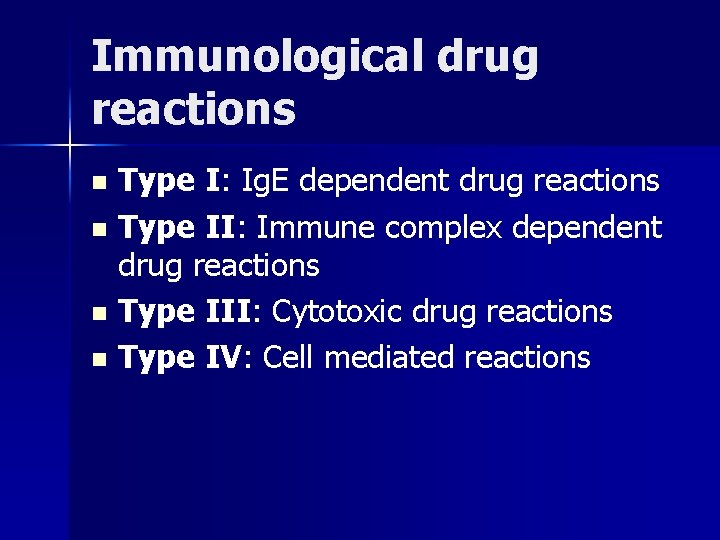
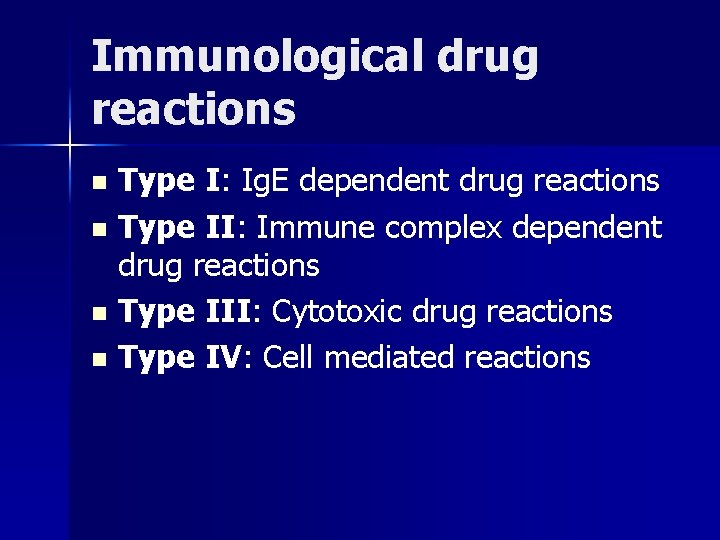
Immunological drug reactions Type I: Ig. E dependent drug reactions n Type II: Immune complex dependent drug reactions n Type III: Cytotoxic drug reactions n Type IV: Cell mediated reactions n
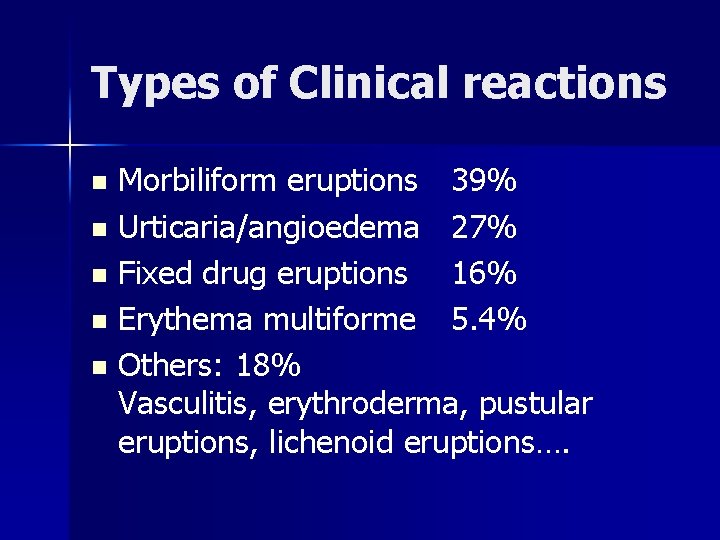
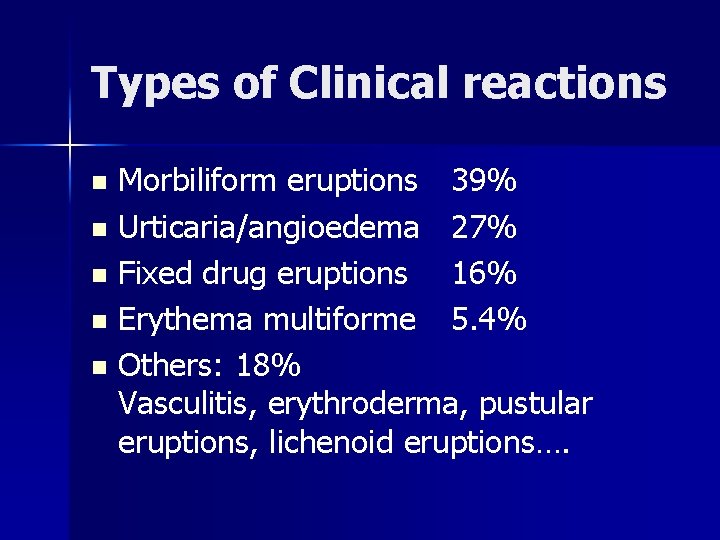
Types of Clinical reactions Morbiliform eruptions 39% n Urticaria/angioedema 27% n Fixed drug eruptions 16% n Erythema multiforme 5. 4% n Others: 18% Vasculitis, erythroderma, pustular eruptions, lichenoid eruptions…. n
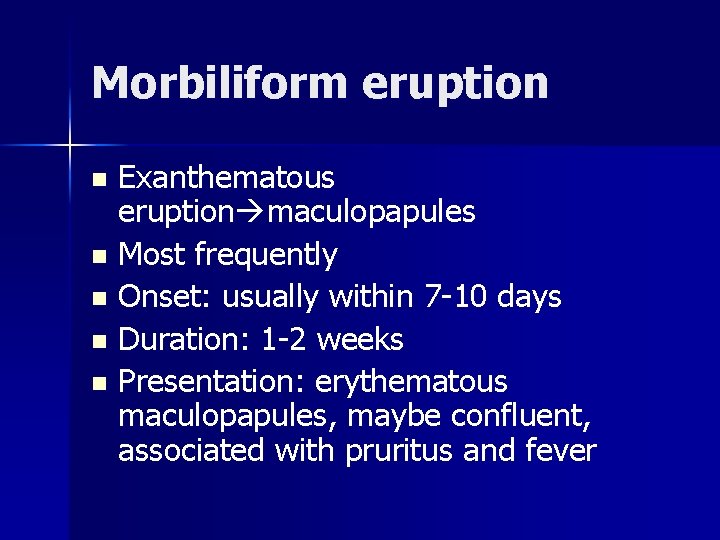
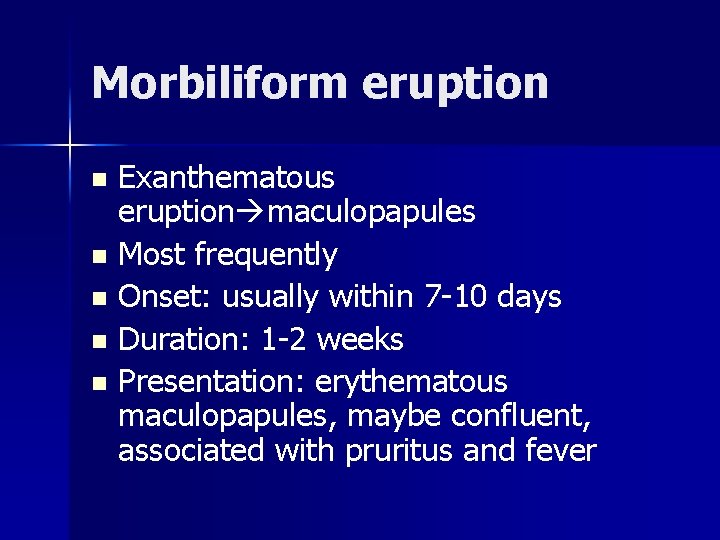
Morbiliform eruption Exanthematous eruption maculopapules n Most frequently n Onset: usually within 7 -10 days n Duration: 1 -2 weeks n Presentation: erythematous maculopapules, maybe confluent, associated with pruritus and fever n
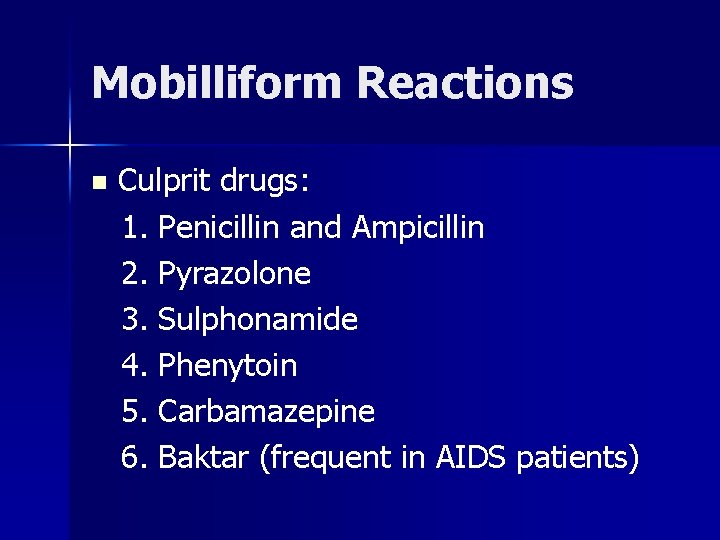
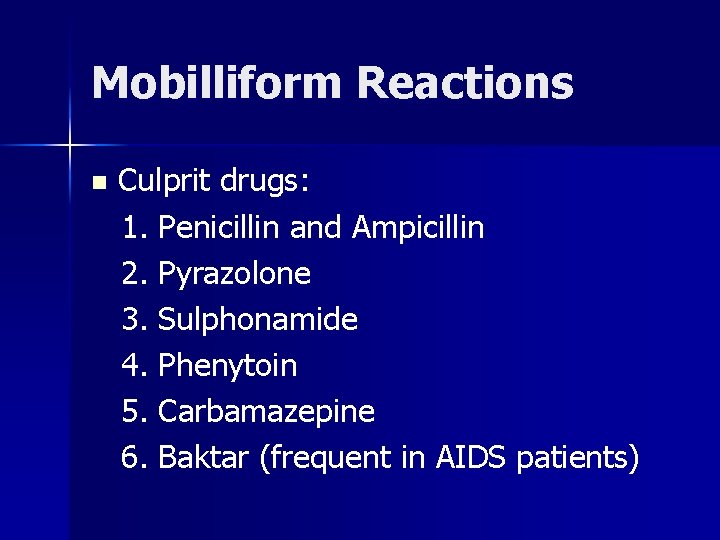
Mobilliform Reactions n Culprit drugs: 1. Penicillin and Ampicillin 2. Pyrazolone 3. Sulphonamide 4. Phenytoin 5. Carbamazepine 6. Baktar (frequent in AIDS patients)
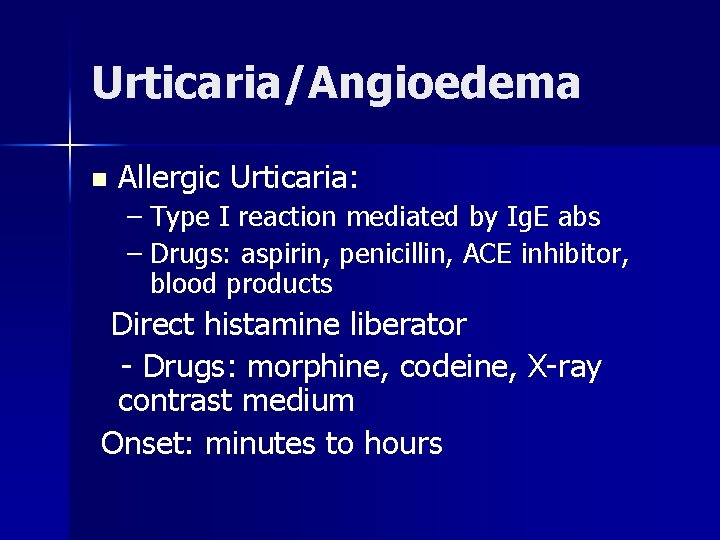
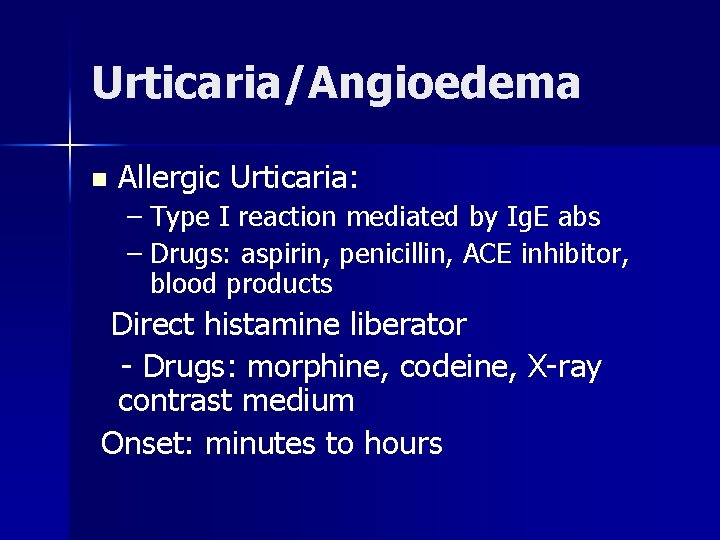
Urticaria/Angioedema n Allergic Urticaria: – Type I reaction mediated by Ig. E abs – Drugs: aspirin, penicillin, ACE inhibitor, blood products Direct histamine liberator - Drugs: morphine, codeine, X-ray contrast medium Onset: minutes to hours
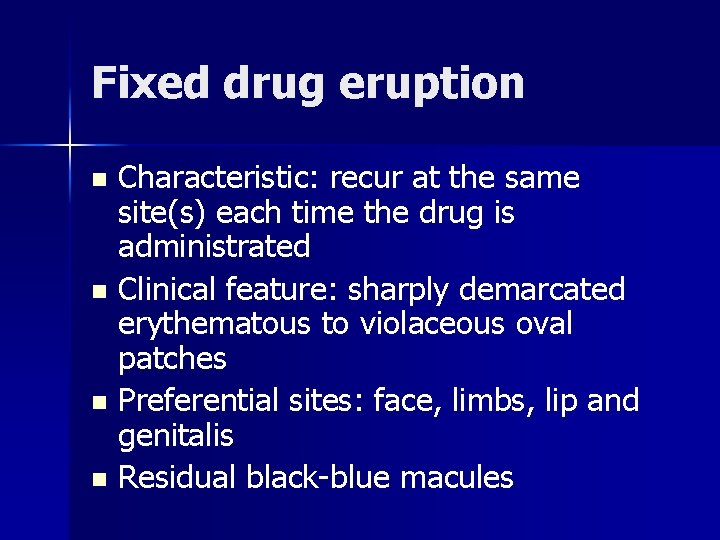
Fixed drug eruption Characteristic: recur at the same site(s) each time the drug is administrated n Clinical feature: sharply demarcated erythematous to violaceous oval patches n Preferential sites: face, limbs, lip and genitalis n Residual black-blue macules n
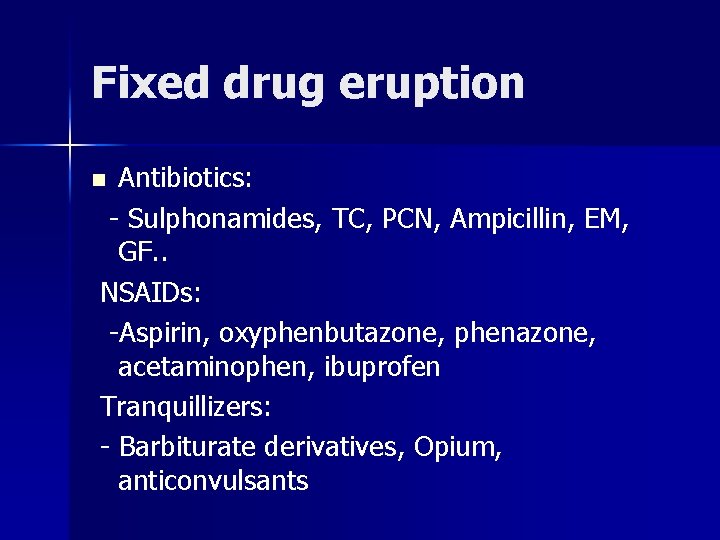
Fixed drug eruption Antibiotics: - Sulphonamides, TC, PCN, Ampicillin, EM, GF. . NSAIDs: -Aspirin, oxyphenbutazone, phenazone, acetaminophen, ibuprofen Tranquillizers: - Barbiturate derivatives, Opium, anticonvulsants n
Erythema Multiforme Clinical features: macules, papules, target lesions with central vesicles n Distribution: distal limbs, palm and sole n Etiology: drugs, HSV infections n Erythema multiforme, major type Stevens - ohnson Syndrome(SJS) Toxic epidermal necrolysis (TEN) n

SJS-Clinical features n n Skin: extensive EM with skin blisters and erosions (<10%), face, neck and chest Nikolski sign(+) Mucosa: oral cavity, bulbar conjunctiva and anogenital, pharyx, GI tract Systemic: fever, malaise, headache, rhinitis, cough, sore throat, myalgia, arthralgia
TEN- Clinical feature Identical to SJS but differ in severity? n Developed from SJS or occurred de novo n Skin: sheet-like erosions>30% of TBSA n Initial “Burning” morbilliform eruptions with flu-like syndrome n Culprit drugs: same as SJS n
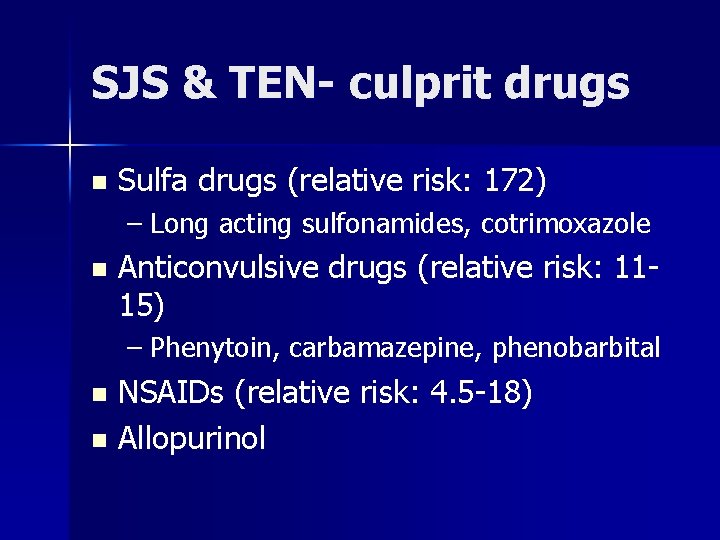
SJS & TEN- culprit drugs n Sulfa drugs (relative risk: 172) – Long acting sulfonamides, cotrimoxazole n Anticonvulsive drugs (relative risk: 1115) – Phenytoin, carbamazepine, phenobarbital NSAIDs (relative risk: 4. 5 -18) n Allopurinol n
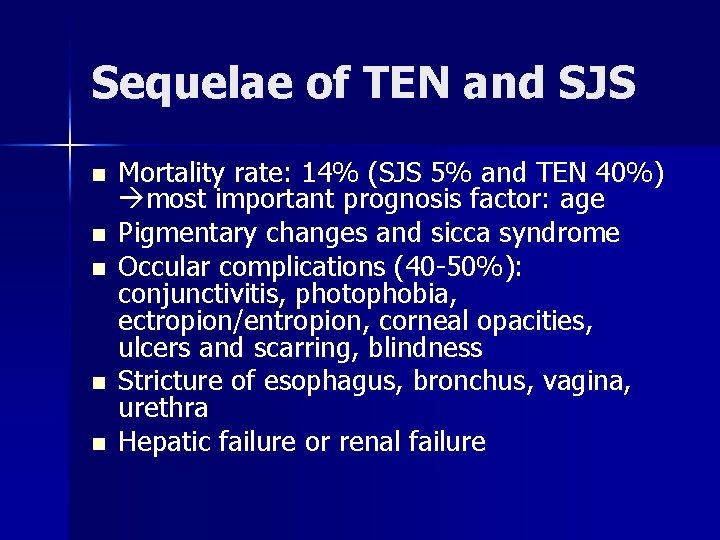
Sequelae of TEN and SJS n n n Mortality rate: 14% (SJS 5% and TEN 40%) most important prognosis factor: age Pigmentary changes and sicca syndrome Occular complications (40 -50%): conjunctivitis, photophobia, ectropion/entropion, corneal opacities, ulcers and scarring, blindness Stricture of esophagus, bronchus, vagina, urethra Hepatic failure or renal failure
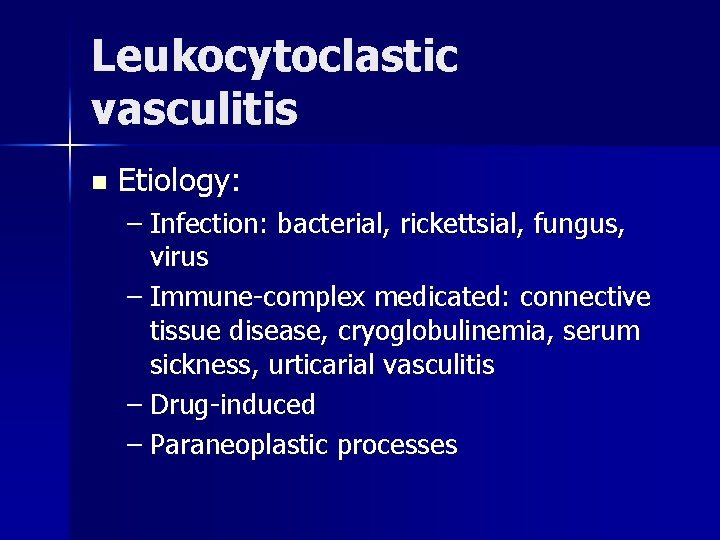
Leukocytoclastic vasculitis n Etiology: – Infection: bacterial, rickettsial, fungus, virus – Immune-complex medicated: connective tissue disease, cryoglobulinemia, serum sickness, urticarial vasculitis – Drug-induced – Paraneoplastic processes
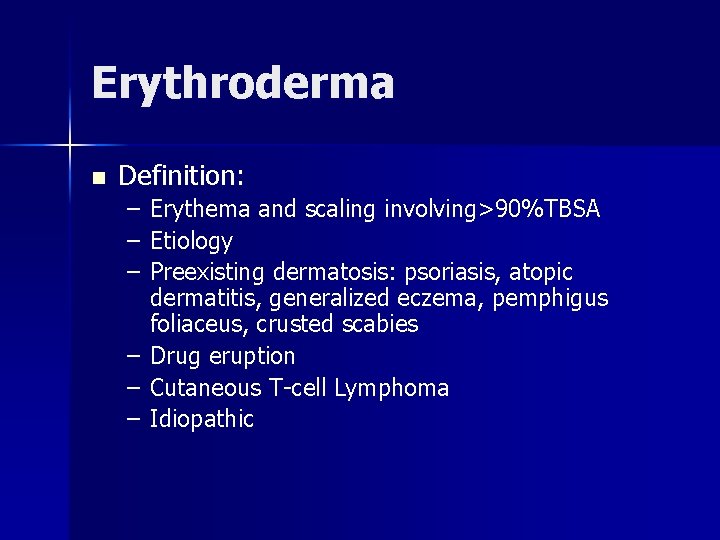
Erythroderma n Definition: – Erythema and scaling involving>90%TBSA – Etiology – Preexisting dermatosis: psoriasis, atopic dermatitis, generalized eczema, pemphigus foliaceus, crusted scabies – Drug eruption – Cutaneous T-cell Lymphoma – Idiopathic

Acute generalized exanthumatous pustulosis (AGEP) Onset within 24 hrs after taking medication n Course: started on face and flexural area, disseminated with fever and settled spontaneously with desquamation n Drugs: >80% is antibiotics n
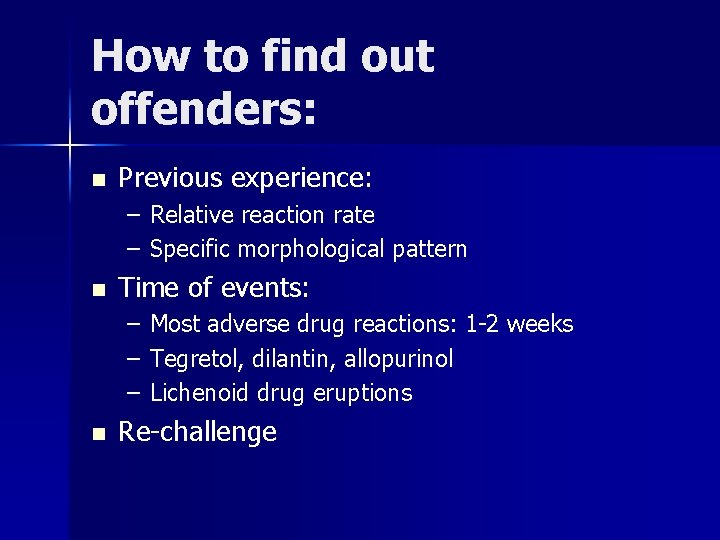
How to find out offenders: n Previous experience: – Relative reaction rate – Specific morphological pattern n Time of events: – Most adverse drug reactions: 1 -2 weeks – Tegretol, dilantin, allopurinol – Lichenoid drug eruptions n Re-challenge
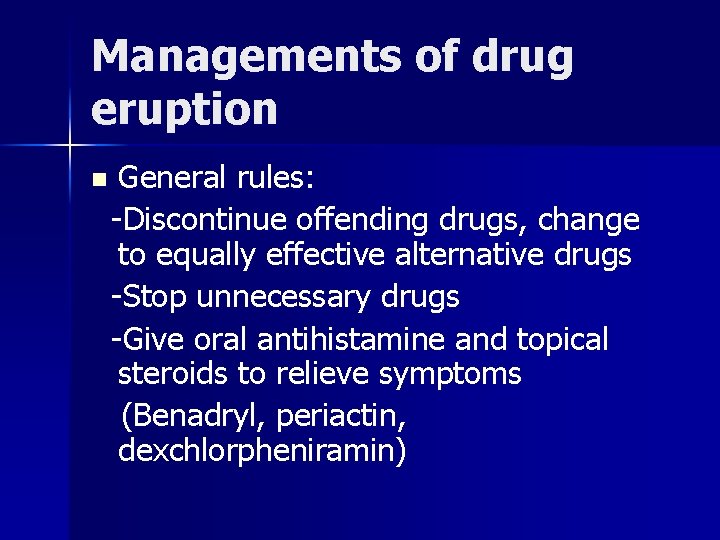
Managements of drug eruption n General rules: -Discontinue offending drugs, change to equally effective alternative drugs -Stop unnecessary drugs -Give oral antihistamine and topical steroids to relieve symptoms (Benadryl, periactin, dexchlorpheniramin)
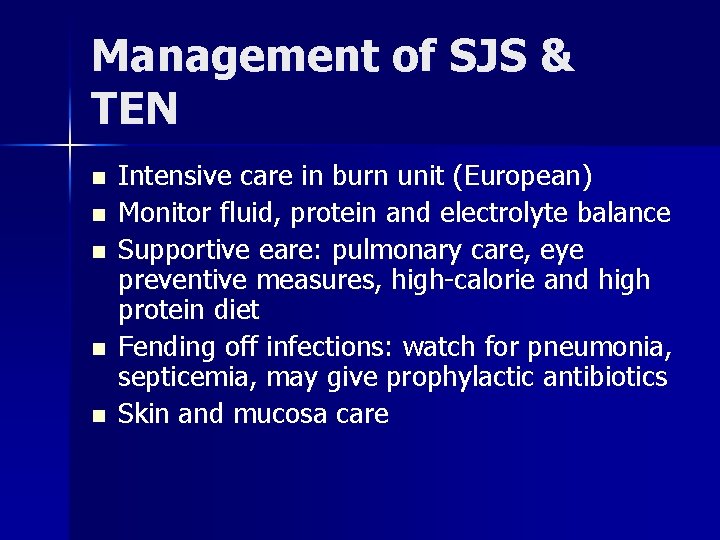
Management of SJS & TEN n n n Intensive care in burn unit (European) Monitor fluid, protein and electrolyte balance Supportive eare: pulmonary care, eye preventive measures, high-calorie and high protein diet Fending off infections: watch for pneumonia, septicemia, may give prophylactic antibiotics Skin and mucosa care
Scabies Etiology: Sarcoptes scabiei var. hominis n Burrow: n – fertilized female excavate burrows and begin egg laying – Inclined downward the epidermis n 40 -50 eggs are laid by each female during a lifespan of 4 -6 weeks
Scabies-Transmission Direct skin-to-skin contact: prolonged hand holding or sharing beds & clothes n Scabies from patients of crusted scabies n Bed sheets and linen: controversial n Away from host, scabies can still survive for 24 -36 hrs (or 2 wks) n
Scabies n Incubation period for itching sensation: – For first time infestation: 2 wks-1 month – For repetitive infestation: immediate Allergic reaction to the mite or its products (eg. Stool, but not the burrows) n Immunology: cell mediated immunity, elevated Ig. E n
Scabies- clinical features Scabies in adults with good hygiene n Scabies in infants and young children n Crusted scabies (Norwegian’s scabies) n Scabies granuloma n
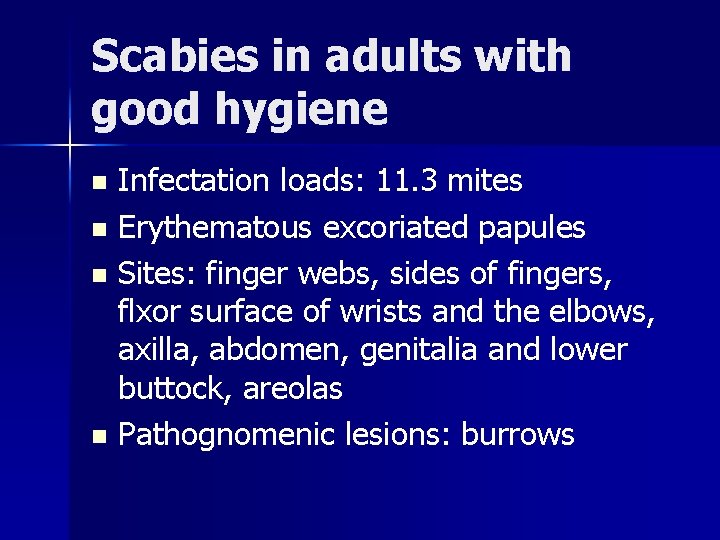
Scabies in adults with good hygiene Infectation loads: 11. 3 mites n Erythematous excoriated papules n Sites: finger webs, sides of fingers, flxor surface of wrists and the elbows, axilla, abdomen, genitalia and lower buttock, areolas n Pathognomenic lesions: burrows n
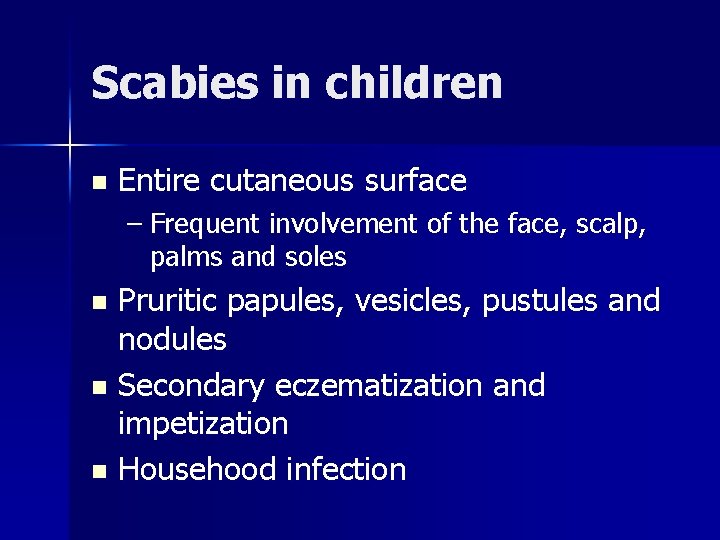
Scabies in children n Entire cutaneous surface – Frequent involvement of the face, scalp, palms and soles Pruritic papules, vesicles, pustules and nodules n Secondary eczematization and impetization n Househood infection n
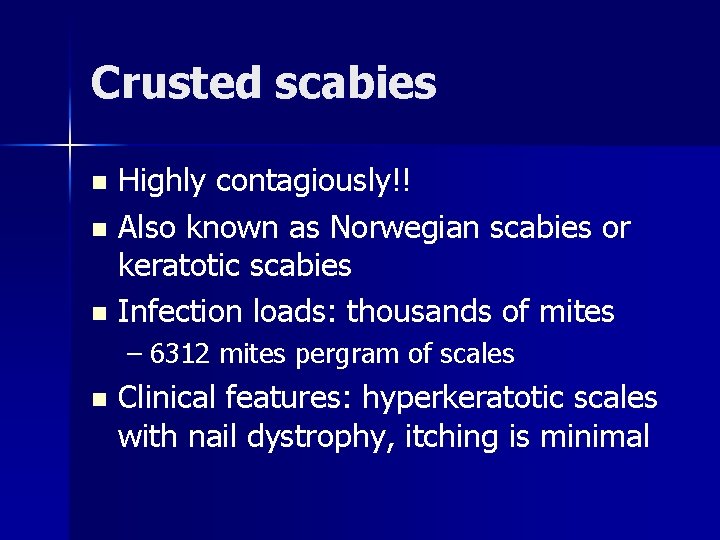
Crusted scabies Highly contagiously!! n Also known as Norwegian scabies or keratotic scabies n Infection loads: thousands of mites n – 6312 mites pergram of scales n Clinical features: hyperkeratotic scales with nail dystrophy, itching is minimal
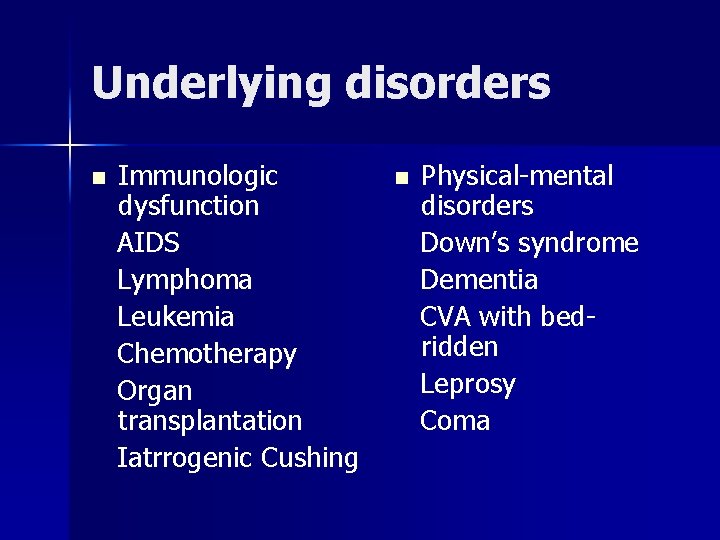
Underlying disorders n Immunologic dysfunction AIDS Lymphoma Leukemia Chemotherapy Organ transplantation Iatrrogenic Cushing n Physical-mental disorders Down’s syndrome Dementia CVA with bedridden Leprosy Coma
Scabies granuloma Reddish-brown, purpuric nodules n Most frequently the male genitalia, groin, and axillary regions n Hypersensitivity reaction to retained mite parts or antigens n
Scabies-treatment BB (benzyl benzoate) lotion or lindane lotion: apply behind the ear and from the neck down to all areas for 3 days n Undergarments, bed linens, towels and clothes should be washed with hot cycles (Temp>60℃) n Isolated contact pillow, futon or coats for more than 2 weeks n
Persistent pruritus Incomplete treatment n Inter-infection through family members n Contact dermatitis due to over treatment n Scabies granuloma n Parasite delusion n
Infectious diseases n Fungus infection Dermatophytes Candidiasis Malassezia furfur Tinea vesicolor Folliculitis n Viral infection Herpes simplex HSV 1 HSV 2 Eczem herpeticum Herpetic whitlow Herpes zoster
Dermatophyte infeciton Fungus infection due to Microsporum, Trichophyton and Epidermophyton n Survive on corneal layer especially warm and moisture area n Active border: characteristic pattern of inflammation n
Cutaneous Candidiasis n n Predisopsing factors: DM, use of corticosteroids, broad-spectrum Abx or chemotherapy, AIDS Mucosa: red and swellon mucosa with firmly adherent whitish plaques Skin: intertriginous area, shinny reddish patches with satellite pustules or plaques Disseminated candidiasis
Disseminated Candidiasis n n Predisposing factors: using steroid or multiple antibiotics, neutropenia, retained IV catheter, TPN, urinary catheter Clinical manifestations: 1. Triads: fever, papular rash, diffuse muscle tenderness 2. Most common sites: kidney, lung, GI tract 3. Characterisitc skin lesions (13%): red to purpuric papulonodules with pale center, on trunk and proximal extremities n B/C rate of candida: 25%
Malassezia furfur n Tinea vesicolor – Hypo/hyper-pigmented macules on occlusive area – Upper trunk>upper limbs, neck> abdomen n Pityrosporum folliculitis – Itchy follicular papules and pustules over upper back and chest, upper arms and neck – Predisposing factor: DM, use of broad spectrum antibiotics, use of steroids, occulsive and greay skin
Herpes simplex n n Caused by herpes simples virus-1 and – 2 Clinical manifestiotions: – – – n Grouped vesicles- umbilicated-crusted Lesions over lips or genital area Specific forms: herpetic whitlow, eczema herpeticu Predisposing factors: – Immunosuppressive patients, life stress
Herpes Zoster n n Caused by Varicella-zoster virus Clinical manifestations: 1. Prodrome: pain, itching or burning localized to a single(or adjacent) dermatomes 2. Zoster sine herpete 3. Grouped vesicles appeared 4 -5 days later n Treatment: acyclovir(IV) or Valtrex(PO), topical treatment is ineffective!
Generalized Pruritus n n Definition: a sensation that leads to a desire to scratch without apparently skin change Etiology Chronic renal disease Cholestasis Iron deficiency Endocrine disease A manifestation of malignant disease Polucythemia vera Aquagenic pruritus Aged skin
Chronic renal disease n n 80% patient on renal dialysis Pathogenesis Dryness Enhanced itching response to histamine Increase Mast cells Secondary hyperparathyroidism Increased vit A concentration Abnormal pattern of cutaneous nerve
Uremic pruritus n Treatment: – Frequent emollient use – Oral antihistamine – Mast cell stabilizer – Phototherapy
Pruritus in cholestasis n n Pathogenesis: High plasma level of bile salts Opioid peptides Treatments Plasmaphoresis Cholestyramine, phenobarbital, rifampicin Ursodeoxycholic acid Naloxone
Pruritus in Endocrine diseases Thryotoxicosis: Hot and moisture n Hypothyroidism: Dry and myxedematous n Diabetes melliutus n Postmenopausal pruritus: FSH and LH n
Pruritus as a manifestation of malignant disease Hodgkin’s disease n Polycycemia vera n Hypereosinophilic syndrome n Myelodysplasia n
Pruritus of aged skin 50% of persons aged over 70 n Reasons: Postmenopausal Scabies Low grade eczema Systemic disease Dry skin n
Sweat Retention syndrome Causes: excessive sweating and occlusions --Fever, bed-ridden, excessive clothing n Types: --Miliaria crystallina --Miliaria rubra --Miliaria pustulosa n