Common Sense and Crisis Management Marsha Holton CCRN







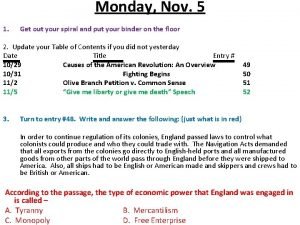
- Slides: 30
Common Sense and Crisis Management Marsha Holton, CCRN, RCIS, FSICP
Marsha Holton, CCRN, RCIS I have no real or apparent conflicts of interest to report.
Objectives • Discuss common sense approach to decision making • • Identify the components of a 90 second patient assessment during crisis management • Identify the basic team members and approaches to crisis management in the lab – Rapid Response Teams – CODE BLUE Teams
• Common sense and crisis management are not diametrically opposing thoughts. – You can approach a crisis with common sense – You can even control a crisis with common sense • You just need to have a plan. Common Sense Starts with a Plan for Emergencies
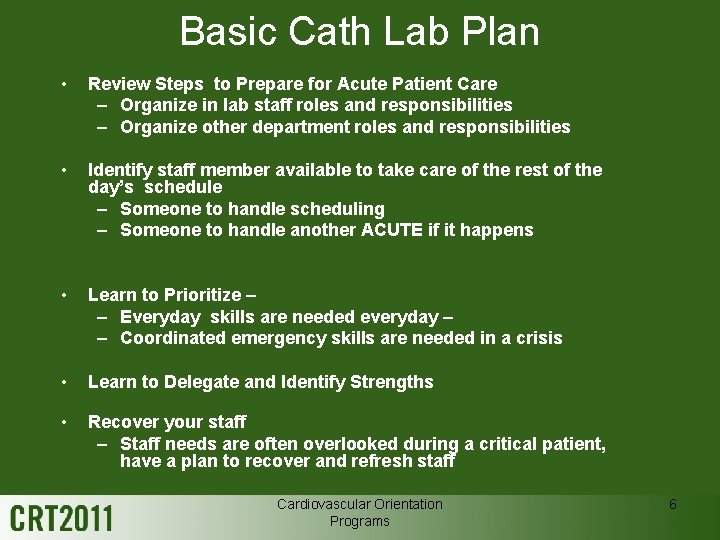
Basic Cath Lab Plan • Review Steps to Prepare for Acute Patient Care – Organize in lab staff roles and responsibilities – Organize other department roles and responsibilities • Identify staff member available to take care of the rest of the day’s schedule – Someone to handle scheduling – Someone to handle another ACUTE if it happens • Learn to Prioritize – – Everyday skills are needed everyday – – Coordinated emergency skills are needed in a crisis • Learn to Delegate and Identify Strengths • Recover your staff – Staff needs are often overlooked during a critical patient, have a plan to recover and refresh staff Cardiovascular Orientation Programs 6
Rapid Response Teams • Team leader – ICU Charge, or Doc in ER or Anesthesia… • The team may include – Critical care nurses, respiratory therapists, fellows if at a teaching hospital, anesthesia, • This sounds like a lot of people and it is… – but it works if you have a plan for the crisis. • www. IHI. org. Establish a Rapid Response Team.
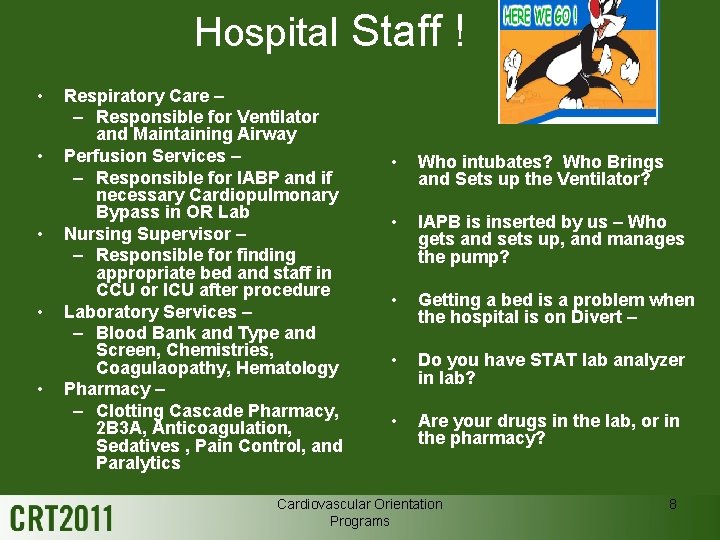
Hospital Staff ! • • • Respiratory Care – – Responsible for Ventilator and Maintaining Airway Perfusion Services – – Responsible for IABP and if necessary Cardiopulmonary Bypass in OR Lab Nursing Supervisor – – Responsible for finding appropriate bed and staff in CCU or ICU after procedure Laboratory Services – – Blood Bank and Type and Screen, Chemistries, Coagulaopathy, Hematology Pharmacy – – Clotting Cascade Pharmacy, 2 B 3 A, Anticoagulation, Sedatives , Pain Control, and Paralytics • Who intubates? Who Brings and Sets up the Ventilator? • IAPB is inserted by us – Who gets and sets up, and manages the pump? • Getting a bed is a problem when the hospital is on Divert – • Do you have STAT lab analyzer in lab? • Are your drugs in the lab, or in the pharmacy? Cardiovascular Orientation Programs 8
So, What Do You Think? Did You Make Your Plan? Do You Have a Plan? Will You Share Your Plan if Asked? Is you plan based on good outcomes and research? SHOCK info.

Smile, you know that’s funny.
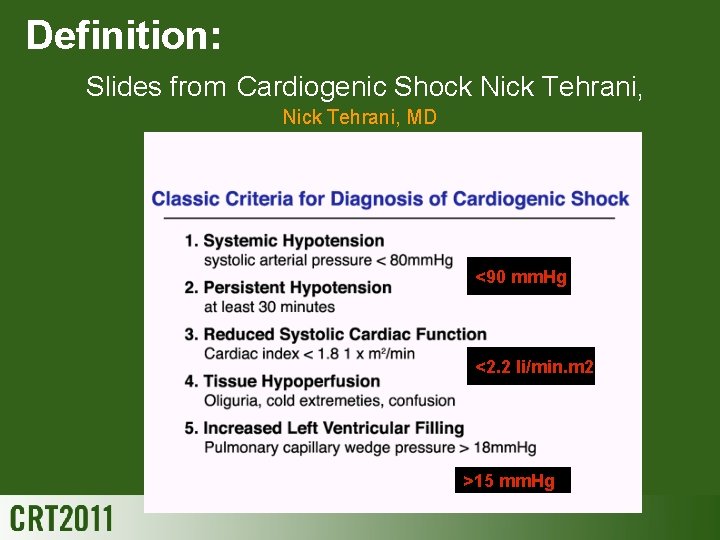
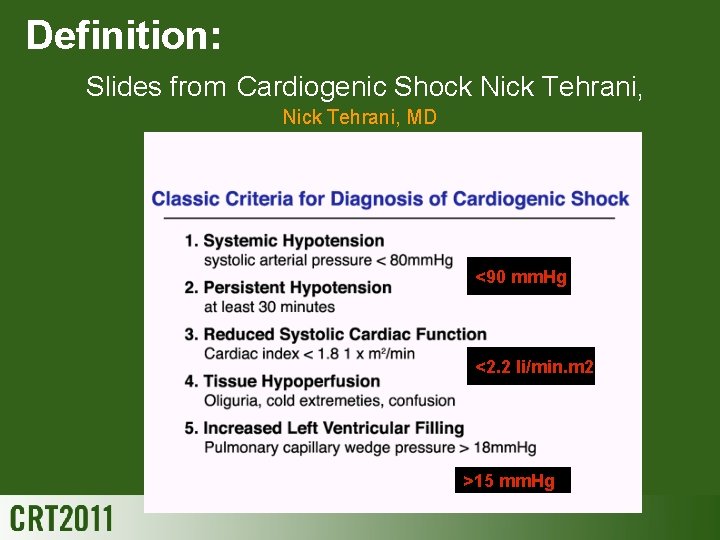
Definition: Slides from Cardiogenic Shock Nick Tehrani, MD <90 mm. Hg <2. 2 li/min. m 2 >15 mm. Hg
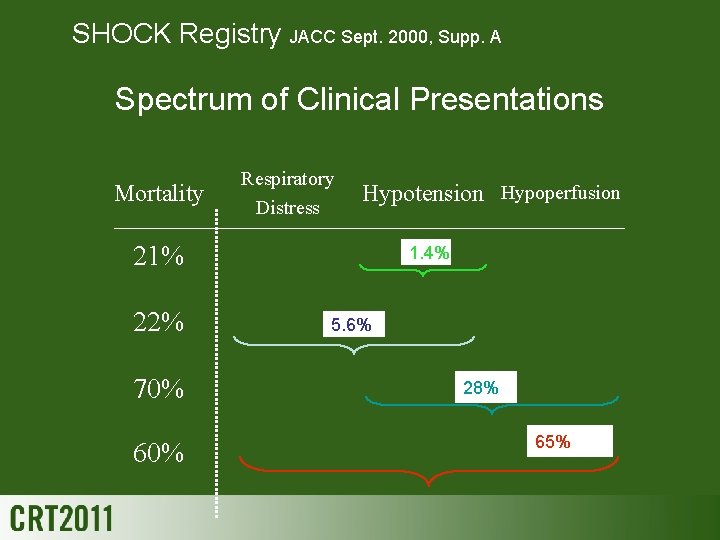
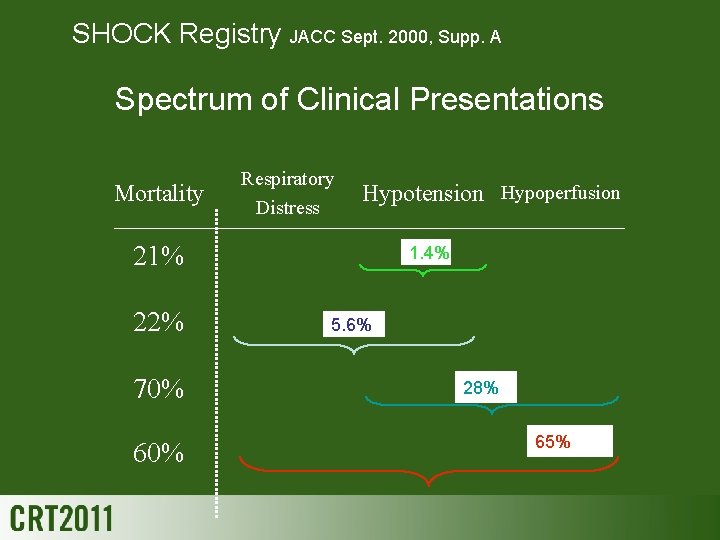
SHOCK Registry JACC Sept. 2000, Supp. A Spectrum of Clinical Presentations Mortality Respiratory Distress Hypotension Hypoperfusion 21% 22% 70% 60% 1. 4% 5. 6% 28% 65%
Risk Factors for Cardiogenic Shock Due to AMI-mediated LV Dysfunction… • • Age > 65 Female gender Large infarction Anterior infarction Prior infarction DM Prior HTN
Outcomes of Cardiogenic Shock • Historic mortality 60 -80% • More recently reported mortality numbers – 67% in the SHOCK trial registry – 56% in GUSTO-I (v. s. 3% in Pts. without shock)
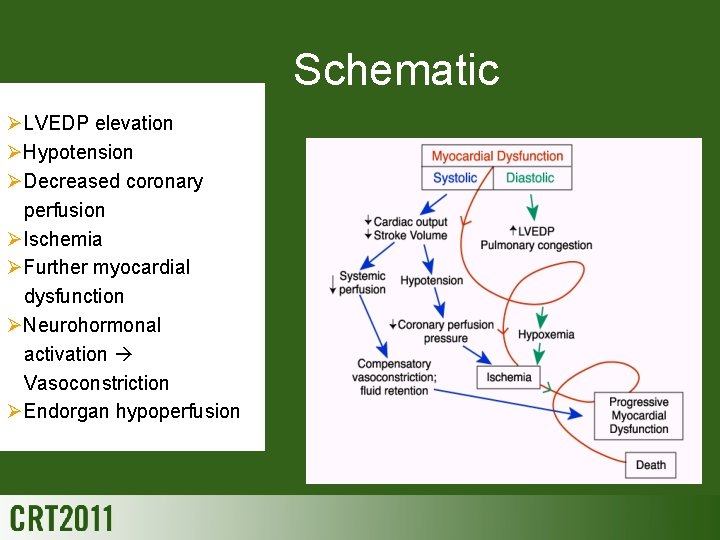
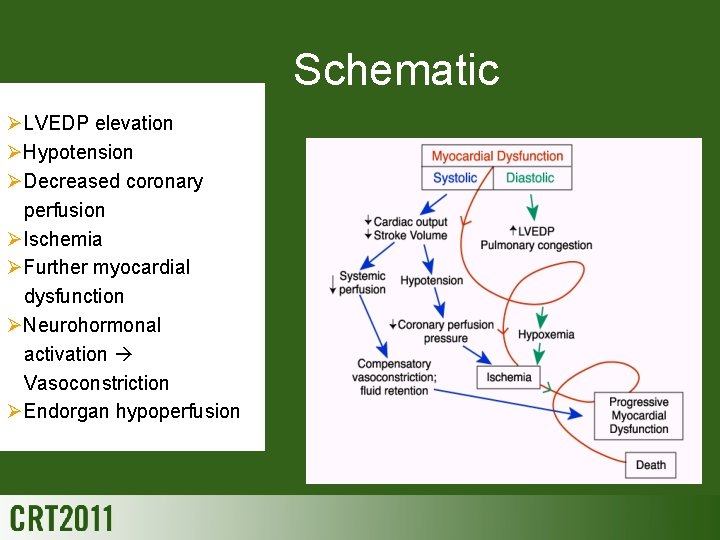
Schematic ØLVEDP elevation ØHypotension ØDecreased coronary perfusion ØIschemia ØFurther myocardial dysfunction ØNeurohormonal activation Vasoconstriction ØEndorgan hypoperfusion
Common Sense Patient Care • 5 minute patient eval. • Yes someone has to assess the patient • An it may be while you are running a code • Delegate,
So Start with the Basics • • • Vital Signs Lines at least one big one, two if time Labs EKG Physical Examination • Consents • Sometimes Drugs come first. (different session) • Research Protocols • Send someone to be with the family.
Head to toe Assessment in 5 Minutes or less

Neuro • • • Are they talking? Are they anxious or restless? Are they making sense? Can they read the consent forms? Are they moving everything? Vitals including temp done? • Neuro: Anxious, restless, and still has chest pain. AAO x 3, MAE, no Hx of CVA or TIA. Temp 98. 8 • Done. Move south to the heart.

Cardiovascular • • • Skin warm dry and pink or not? Chest pain? Scale of 1 -10 Pulses all present or not? RRR or not? BP OK or not? Murmurs? Rubs? Hx of CABG or not? Hx of previous CV adventure? Personally or family? • CV: Chest pain is 5/10, skin cool, damp, pale. Pulses present, but irregular, Bp 90/66. No murmurs, or rubs, no history of prior event, positive family history, brother had MI at age 51.

Respiratory • Respirations normal or labored? • O 2 on at what flow • Listen to lungs front and back, rales or wheezes need to be noted • History of smoking, cancer, toxic chemicals, pneumonias or not • Resp: 02 at 3 L NC. Mild SOB, Rales bilaterally at bases, no wheezing. No history of pneumonias, smoking, or toxic chemical exposure.
Gastrointestional • When did they eat or drink? What and how much. Any ETOH in last 6 hours? • History of ulcers, surgeries, what and when. • Vomiting? • GI: Last meal 5 hours ago, full breakfast, eggs and bacon and coffee and toast. Coffee 30 minutes ago, 3 beers with dinner last night. History of ulcer, no treatment, no surgeries except appendectomy as child. Feels like throwing up right now.

Urinary • History of renal disease or renal stones? History of frequent urinary infections? Blood in urine? Under the age of 55 and intact and sexually active and not protected? Any other high risk history? • GU: Had kidney stones 20 years ago with blood in urine, no infections for years. No high risk behaviors, but thinks he had hepatitis as a child.
Skeletal • Any musculoskeletal surgeries? • Any history of fractures, back, neck, etc? When and where • Any chronic pain that requires pain medication regularly? What and how much and when was the last hit? • Skeletal: Patient fell last winter, sprained back and neck, takes Motrin and occasionally Percocet. No Rx. for a few weeks.
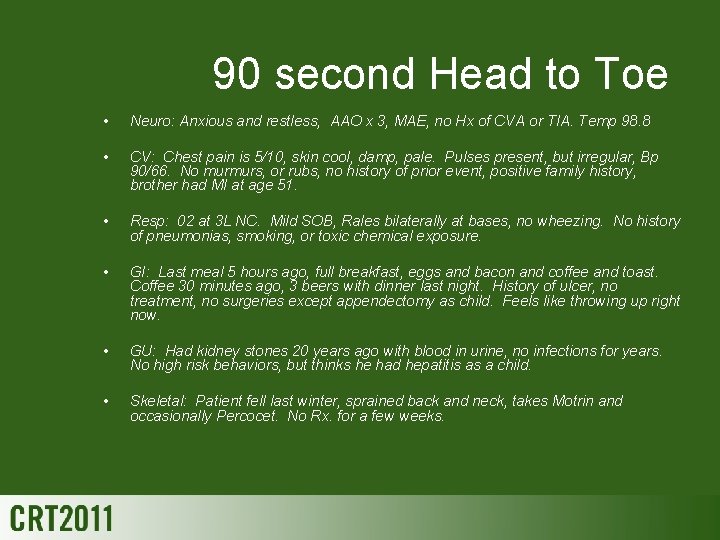
90 second Head to Toe • Neuro: Anxious and restless, AAO x 3, MAE, no Hx of CVA or TIA. Temp 98. 8 • CV: Chest pain is 5/10, skin cool, damp, pale. Pulses present, but irregular, Bp 90/66. No murmurs, or rubs, no history of prior event, positive family history, brother had MI at age 51. • Resp: 02 at 3 L NC. Mild SOB, Rales bilaterally at bases, no wheezing. No history of pneumonias, smoking, or toxic chemical exposure. • GI: Last meal 5 hours ago, full breakfast, eggs and bacon and coffee and toast. Coffee 30 minutes ago, 3 beers with dinner last night. History of ulcer, no treatment, no surgeries except appendectomy as child. Feels like throwing up right now. • GU: Had kidney stones 20 years ago with blood in urine, no infections for years. No high risk behaviors, but thinks he had hepatitis as a child. • Skeletal: Patient fell last winter, sprained back and neck, takes Motrin and occasionally Percocet. No Rx. for a few weeks.
Note : Medications • • List all drugs List all doses List all times List last dose taken • LIST ALLERGIES and SYMPTOMS
Note: Labs • • • Basic cardiac panel, Troponin, CKMB CBC PT/PTT Chem. 7 electrolytes, BUN, Creat. Type and screen • Something should be back before going into the lab. • But sometimes not.
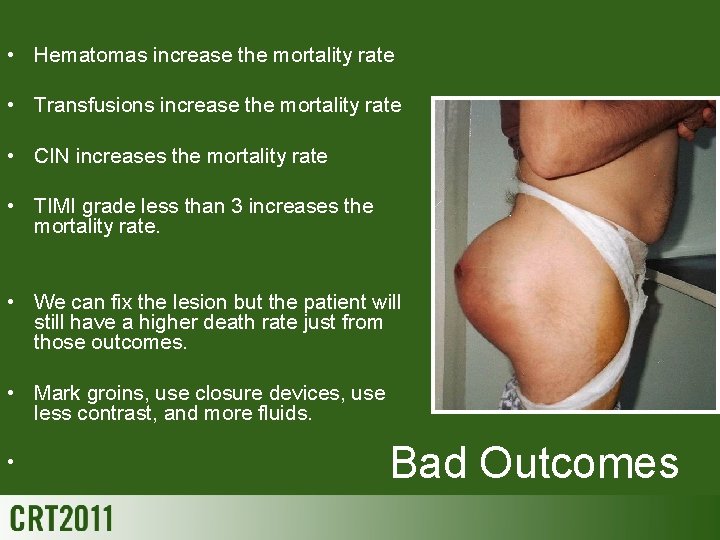
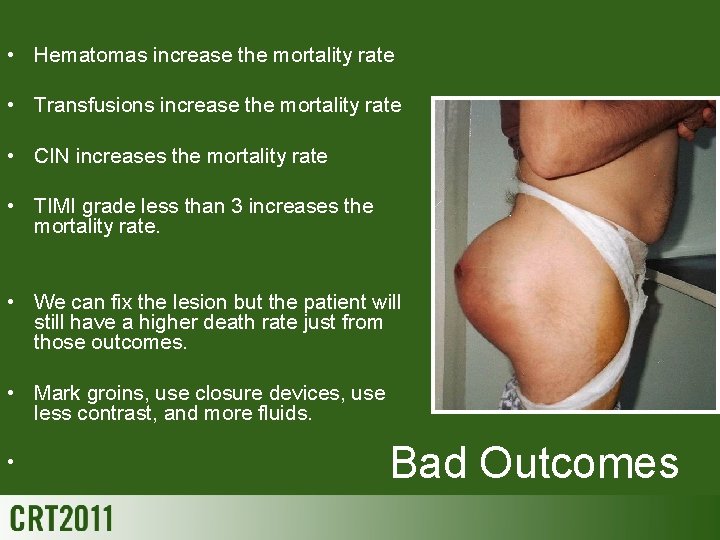
• Hematomas increase the mortality rate • Transfusions increase the mortality rate • CIN increases the mortality rate • TIMI grade less than 3 increases the mortality rate. • We can fix the lesion but the patient will still have a higher death rate just from those outcomes. • Mark groins, use closure devices, use less contrast, and more fluids. • Bad Outcomes

Quick Reminder • Drop of 2 -3 grams of hemoglobin is equivalent to a unit of blood • Drop of platelet count by 50% indicates heparin induced thrombocytopenia if patient is on heparin • Increase in serum creatinine of 25% can indicate contrast induced nephrotoxicity

Your 5 minutes are Up Time to Go to the Lab.
Credits and Acknowledgements • • • • www. ACC/NCDR PCI Risk Assessment, Wolfram Demonstration Project Rubric for Error Analysis, K. Mc. Canalley, San Diego www. images. com Neurologic complications of cardiovascular procedures, Kumar Rajamani MD , Seemant Chaturvedi MD , Steven R Levine MD. Reference from Neurology Med. Link. Cardiogenic Shock presentation, Nick Teherini Textbook of STEMI Interventions, Mehta, S. Lessons from the single community experience. Pg 97. ACC/AHA Guidelines. HMP Communications, Malvern, Pa Changing the Standard of Care in STEMI PCI, Dave, R. . Case Study. CLD, Vol 16, num. 9. Sept, 2008 Harrison's Principles of Internal Medicine, Isselbacher, et al. Part 7, Ch 202. Acute Myocardial Infarction, pgs 1066 -1067. 13 th ed. Mc. Graw Hill Publishers Merhan, Roxanna, TCT 2002 Contrast Induced Nephrotoxicity lectures. Levy, EM, et. al. JAMA 1996: 275. 1489 -1494. Table on CIN and mortality Invasive Cardiology, A Manual for Cath Lab Personnel, Watson, S. , Gorski, K Ch. 27 Emergencies in the Cardiac Catheterization Laboratory, Barbiere, C. Ch 17. Nursing Care of the Interventional Cardiac Procedure Patient. Holton, M. Orientation Manual, Greater Southeast Community Hospital, IMC Training for Staff. Patient Care and Assessment, RCIS Reviews. Interventions Sessions, Jeff Davis Edison College Lab picture.
 Marsha linehan daughter geraldine
Marsha linehan daughter geraldine Amateur revenge porn
Amateur revenge porn Myasthenia gravis sauna
Myasthenia gravis sauna Narrow sense heritability vs broad sense heritability
Narrow sense heritability vs broad sense heritability Narrow sense heritability vs broad sense heritability
Narrow sense heritability vs broad sense heritability Sociology and common sense
Sociology and common sense Examples of common sense and sociological explanations
Examples of common sense and sociological explanations Right attitude and common sense
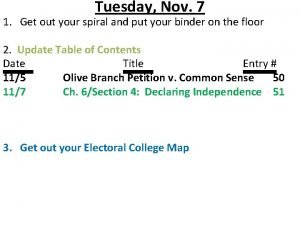
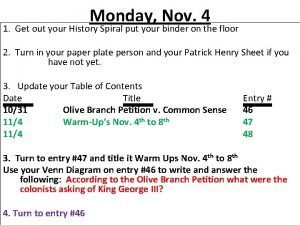
Right attitude and common sense Olive branch petition and common sense venn diagram
Olive branch petition and common sense venn diagram Venn diagram of olive branch petition and common sense
Venn diagram of olive branch petition and common sense Tischler sociology
Tischler sociology Olive branch petition and common sense venn diagram
Olive branch petition and common sense venn diagram Common sense education fair and square
Common sense education fair and square Social psychology vs sociology
Social psychology vs sociology Marsha vernoga
Marsha vernoga Marsha hentai
Marsha hentai Marsha colbey
Marsha colbey Marsha berger
Marsha berger Marsha slough
Marsha slough Marsha chan
Marsha chan Marsha faradina
Marsha faradina Marsha chechik
Marsha chechik How learning works
How learning works Marsha garrett middlesbrough
Marsha garrett middlesbrough Marsha garrett middlesbrough
Marsha garrett middlesbrough Introductions by marsha
Introductions by marsha Pauls friend moved here from manteca california
Pauls friend moved here from manteca california Polk county assessor gis
Polk county assessor gis Uselargefrs
Uselargefrs Marsha warren
Marsha warren Qqqnn
Qqqnn