COMMON RESPIRATORY TRACT INFECTION IN CHILDREN RINA TRIASIH


- Slides: 49
COMMON RESPIRATORY TRACT INFECTION IN CHILDREN RINA TRIASIH Department of Child Health Medical School, Gadjah Mada University Sardjito Hospital YOGYAKARTA
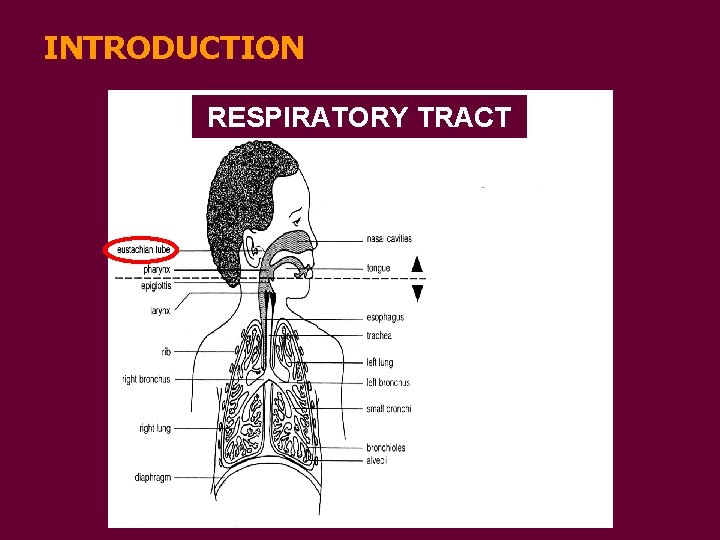
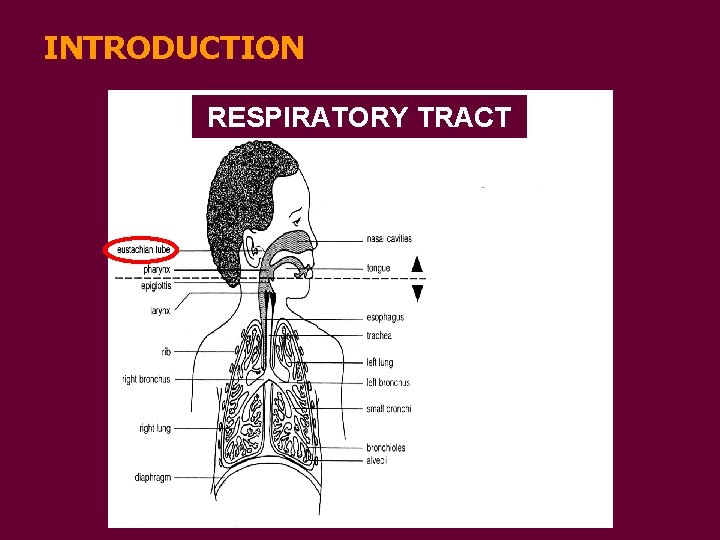
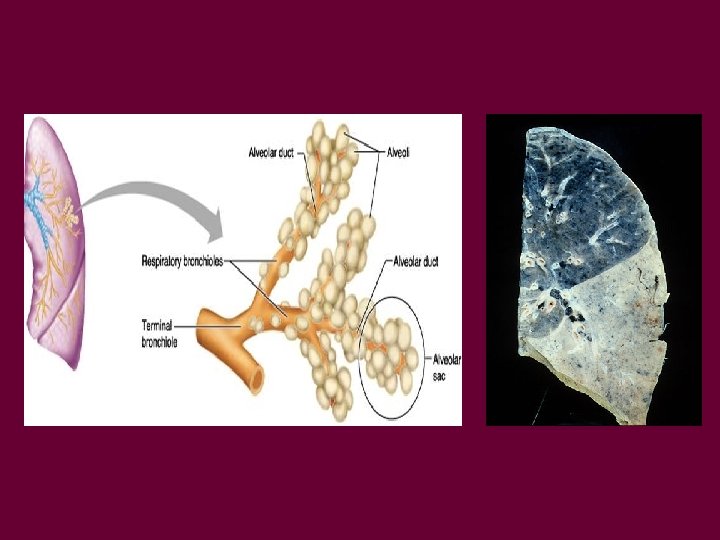
INTRODUCTION RESPIRATORY TRACT sinusitis
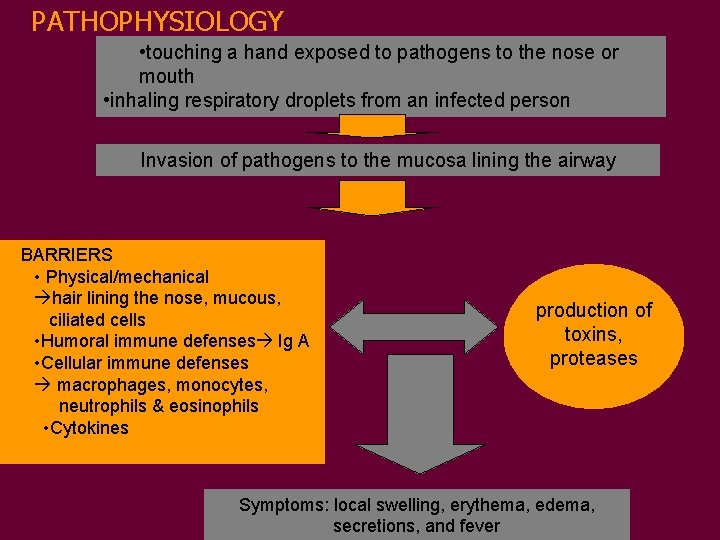
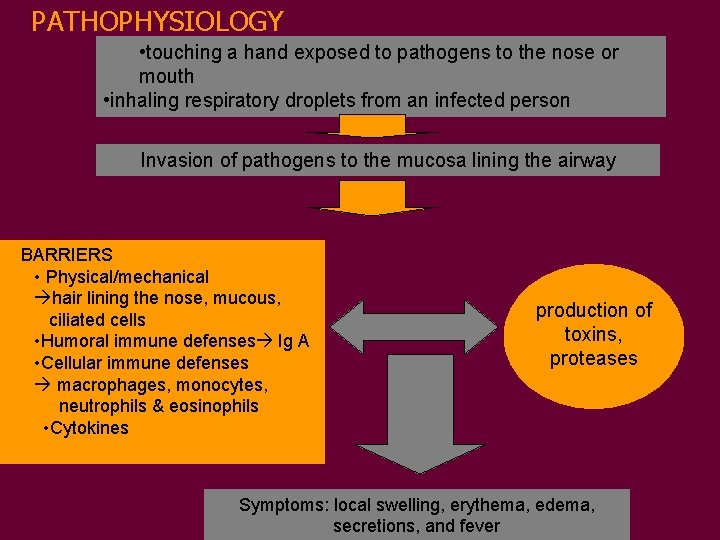
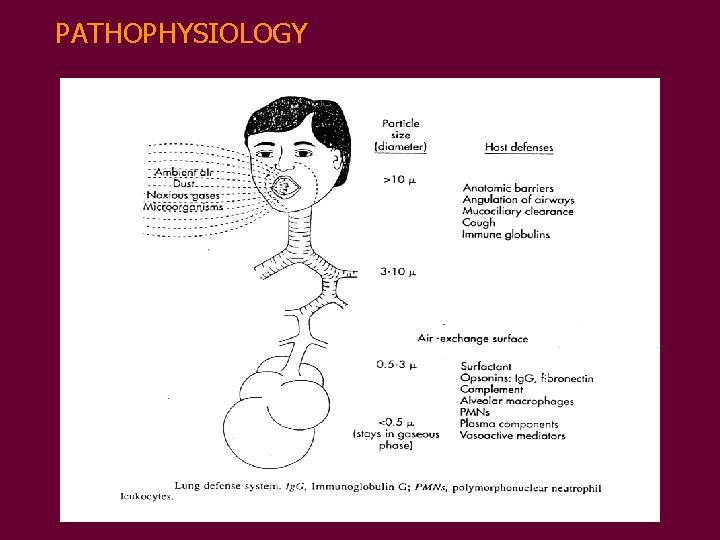
PATHOPHYSIOLOGY • touching a hand exposed to pathogens to the nose or mouth • inhaling respiratory droplets from an infected person Invasion of pathogens to the mucosa lining the airway BARRIERS • Physical/mechanical hair lining the nose, mucous, ciliated cells • Humoral immune defenses Ig A • Cellular immune defenses macrophages, monocytes, neutrophils & eosinophils • Cytokines production of toxins, proteases Symptoms: local swelling, erythema, edema, secretions, and fever
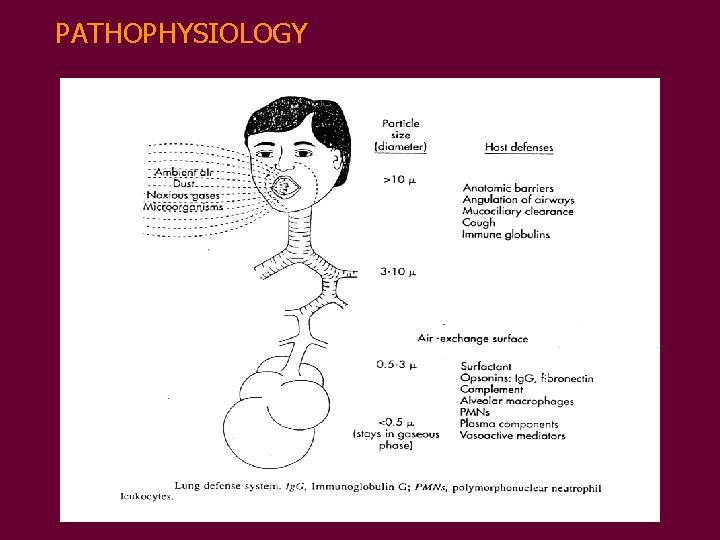
PATHOPHYSIOLOGY
RESPIRATORY TRACT INFECTION CLASSIFICATION Based on time: § ACUTE RESPIRATORY INFECTIONS Less than 14 days § CHRONIC RESPIRATORY INFECTIONS More than 14 days
ACUTE RESPIRATORY INFECTION (ARI)
EPIDEMIOLOGY • MORBIDITY • 50% of all illness diseases in children under 5 years • 30% in children 5 -12 years • EPISODE IN URBAN AREA: 5 -8/YEAR RURAL AREA: 3 -5/YEAR ( WHO, 1992) • Most infections are limited to upper tract, about 5% involved lower tract (Phelan, 1994)
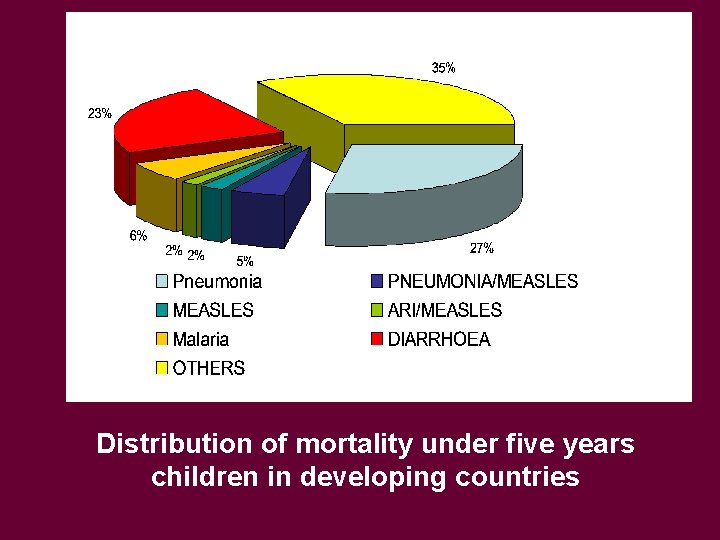
• MORTALITY – One of the commonest cause of death in children – Cause around 3 million child deaths worldwide each year: • Most are caused by PNEUMONIA • 99% occur in developing countries (WHO, 1999)
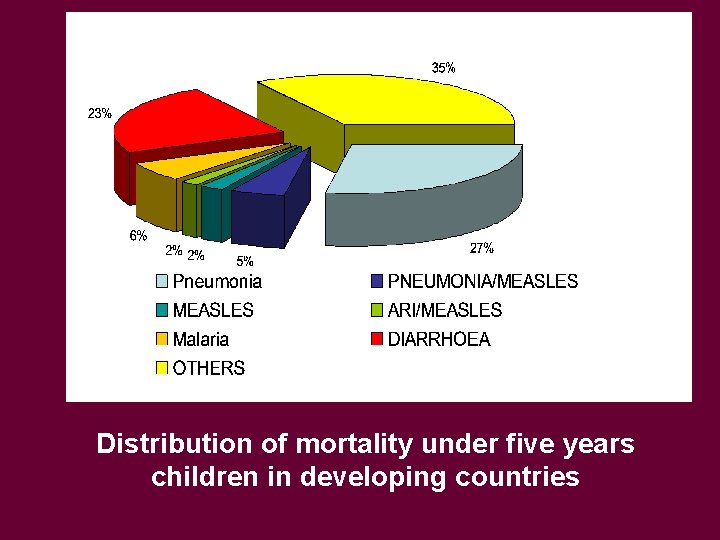
Distribution of mortality under five years children in developing countries

IN INDONESIA • MORBIDITY in children 5 years of age: 10 -20% (2. 33 - 4. 66 million) • MORTALITY >> PNEUMONIA MORTALITY RATE IN 1992 : 2. 7/ 1000 (National Household Survey=SKRT, 1992)
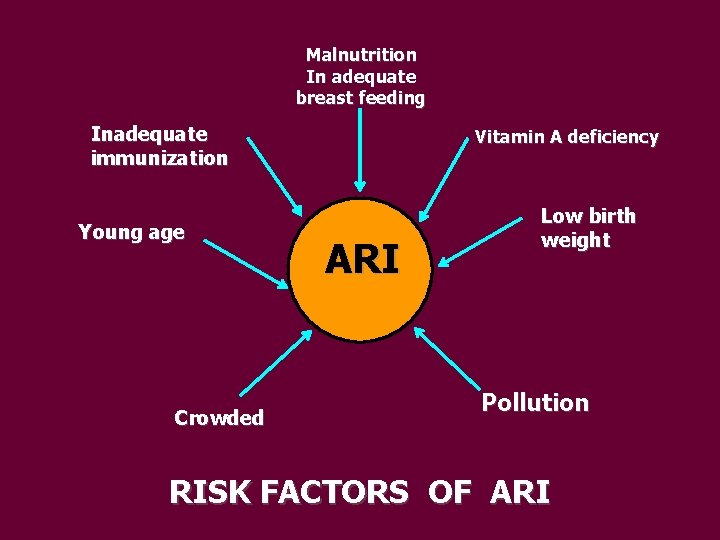
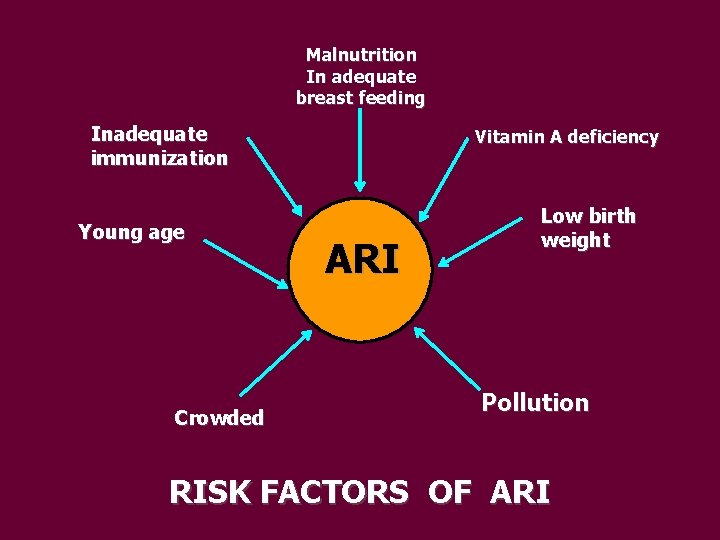
Malnutrition In adequate breast feeding Inadequate immunization Young age Crowded Vitamin A deficiency ARI Low birth weight Pollution RISK FACTORS OF ARI
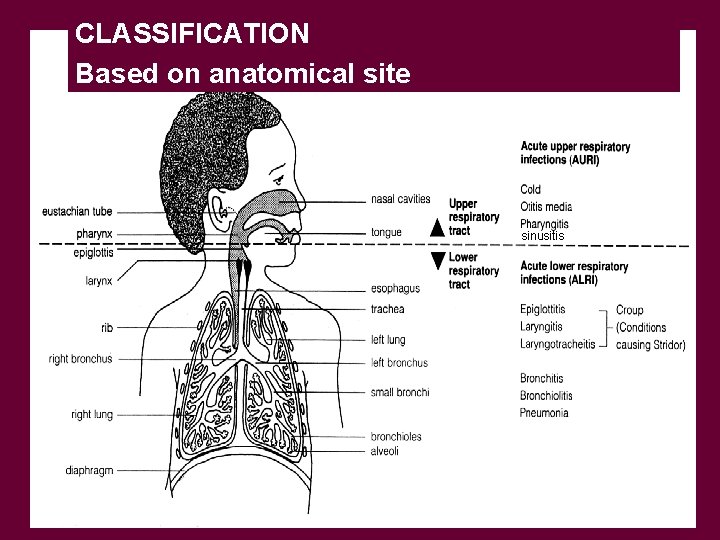
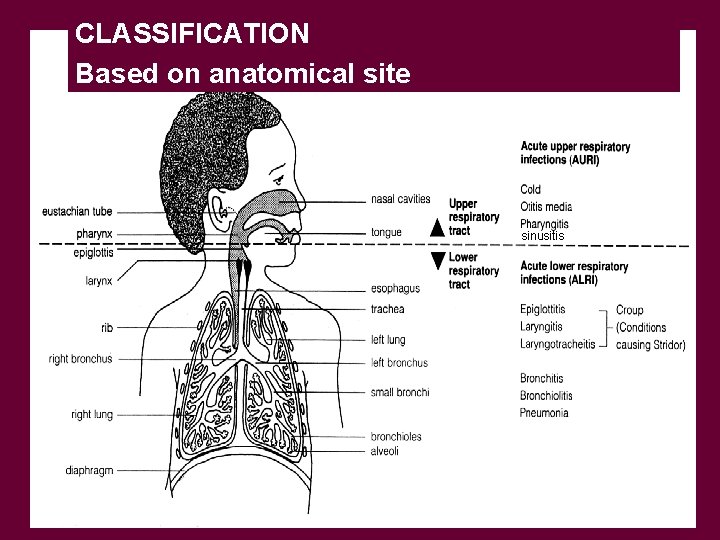
CLASSIFICATION Based on anatomical site sinusitis
• AURI: • common cold (rhinitis) • pharyngitis-nasopharyngitis-tonsilopharyngitis • sinusitis • otitis media • ALRI : • epiglotitis • • laryngo-tracheobronchitis bronchiolitis pneumonia
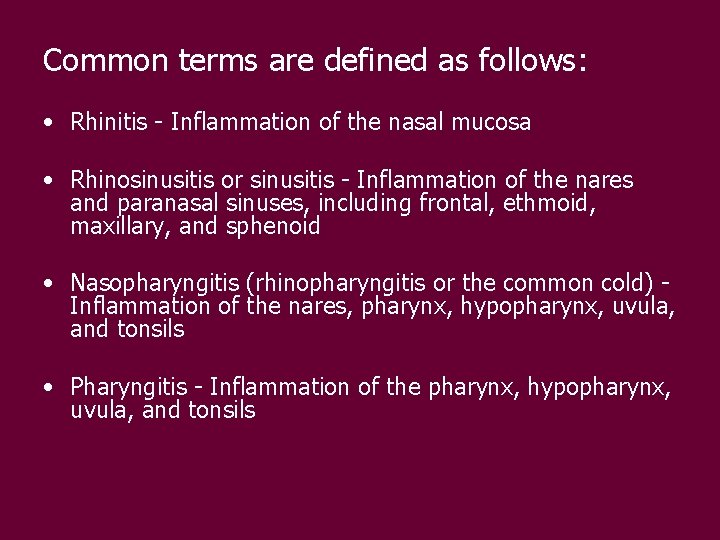
Common terms are defined as follows: • Rhinitis - Inflammation of the nasal mucosa • Rhinosinusitis or sinusitis - Inflammation of the nares and paranasal sinuses, including frontal, ethmoid, maxillary, and sphenoid • Nasopharyngitis (rhinopharyngitis or the common cold) Inflammation of the nares, pharynx, hypopharynx, uvula, and tonsils • Pharyngitis - Inflammation of the pharynx, hypopharynx, uvula, and tonsils
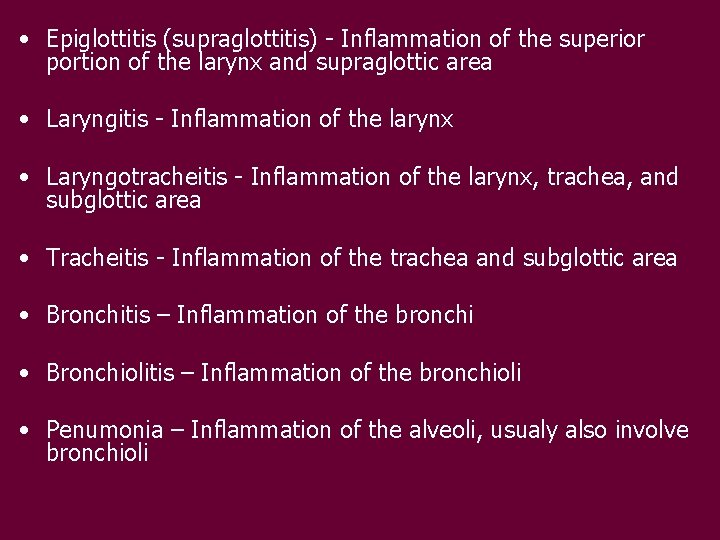
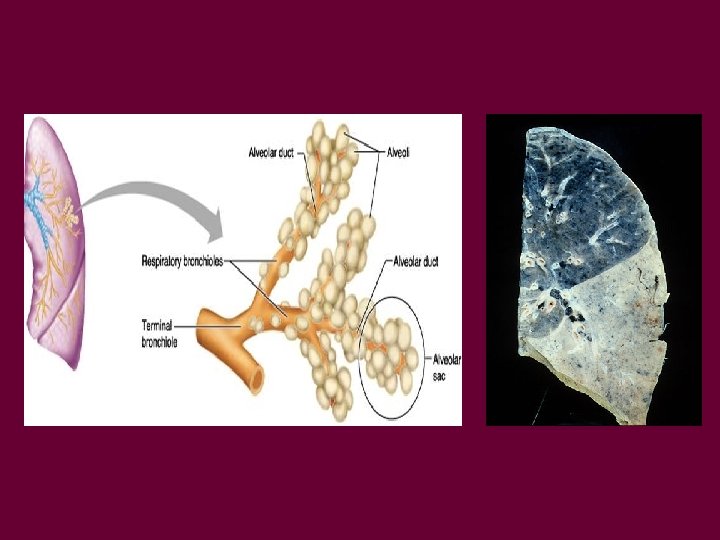
• Epiglottitis (supraglottitis) - Inflammation of the superior portion of the larynx and supraglottic area • Laryngitis - Inflammation of the larynx • Laryngotracheitis - Inflammation of the larynx, trachea, and subglottic area • Tracheitis - Inflammation of the trachea and subglottic area • Bronchitis – Inflammation of the bronchi • Bronchiolitis – Inflammation of the bronchioli • Penumonia – Inflammation of the alveoli, usualy also involve bronchioli
EPIDEMIOLOGY ASPECT : • Community acquired ARI • Hospital acquired ARI (Nosocomial infection) (Torres, 1997)
ETIOLOGY • AURI : VIRUS ( 90%) • COMMON VIRUSES AURI : Rhinovirus, Coronavirus, Adenovirus, Enterovirus ALRI : RSV, Para influenza 1, 2, 3; Coronavirus, Adenovirus, Enterovirus
PNEUMONIA
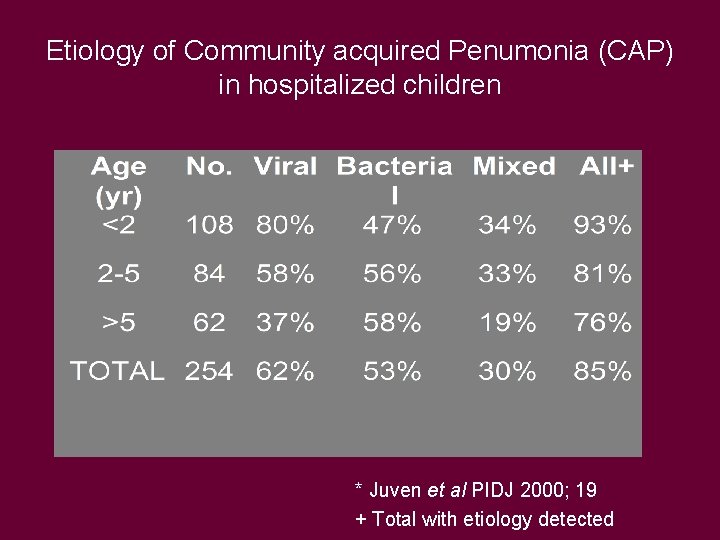
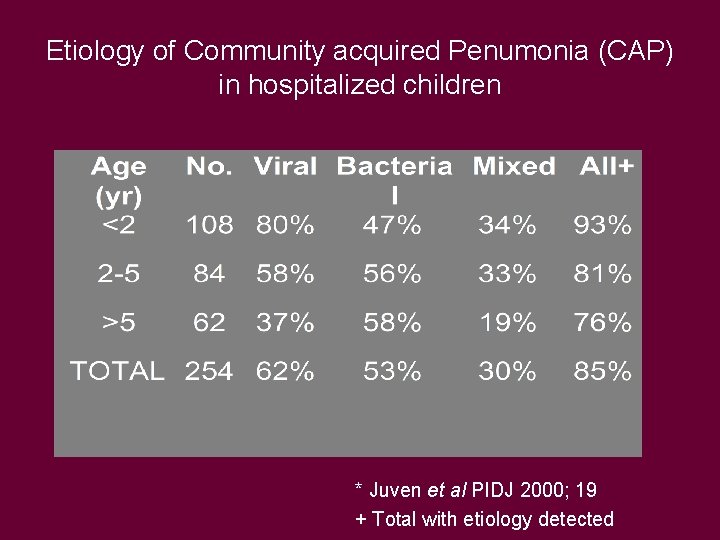
Etiology of Community acquired Penumonia (CAP) in hospitalized children * Juven et al PIDJ 2000; 19 + Total with etiology detected
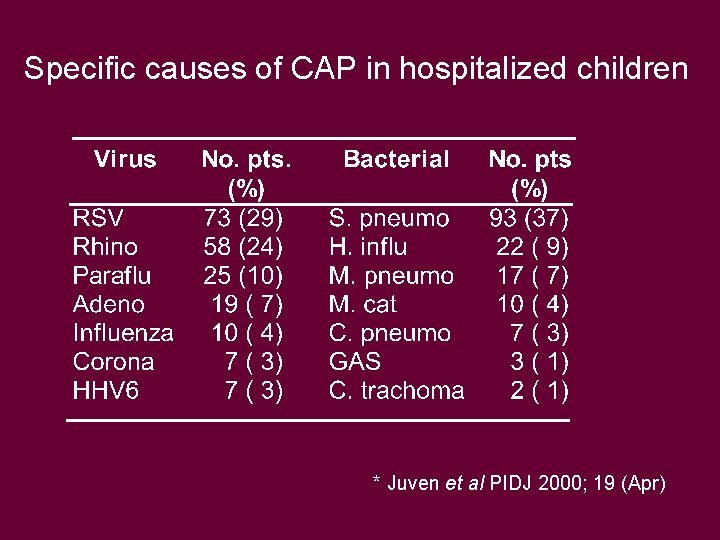
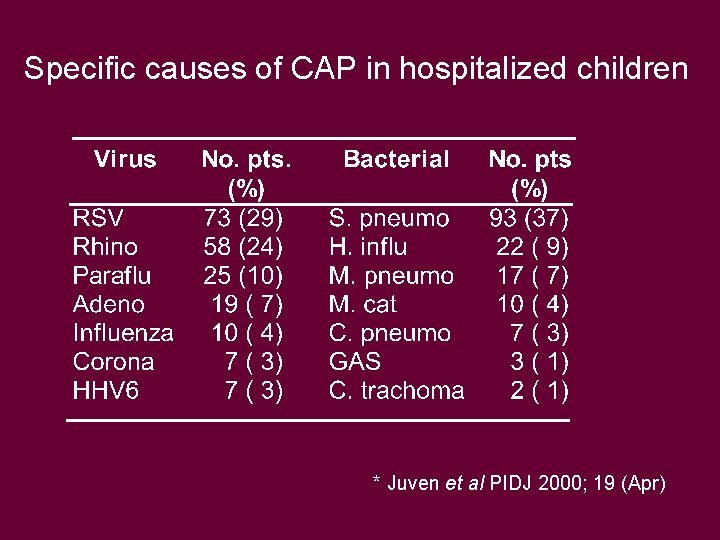
Specific causes of CAP in hospitalized children * Juven et al PIDJ 2000; 19 (Apr)
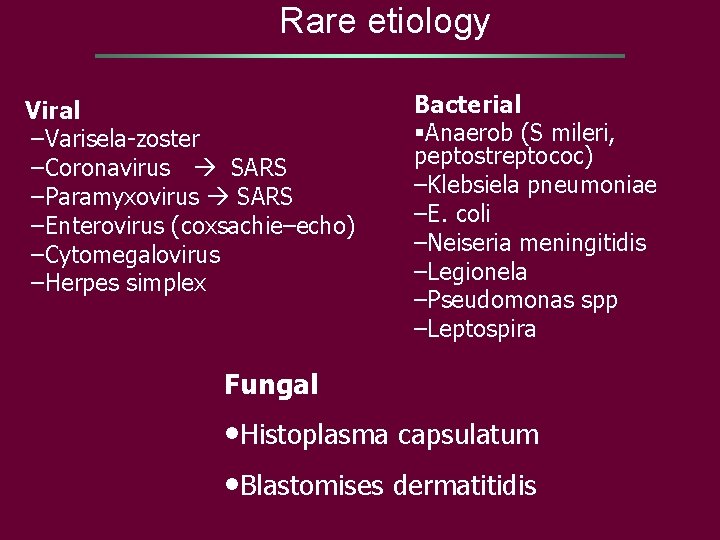
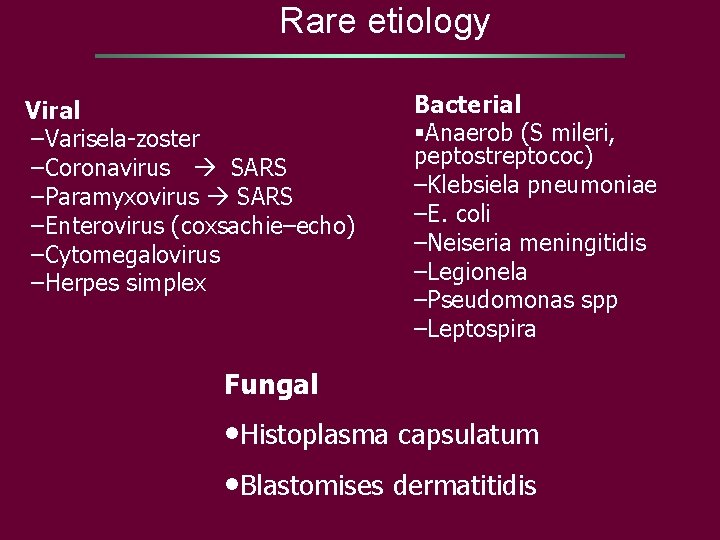
Rare etiology Viral –Varisela-zoster –Coronavirus SARS –Paramyxovirus SARS –Enterovirus (coxsachie–echo) –Cytomegalovirus –Herpes simplex Bacterial §Anaerob (S mileri, peptostreptococ) –Klebsiela pneumoniae –E. coli –Neiseria meningitidis –Legionela –Pseudomonas spp –Leptospira Fungal • Histoplasma capsulatum • Blastomises dermatitidis
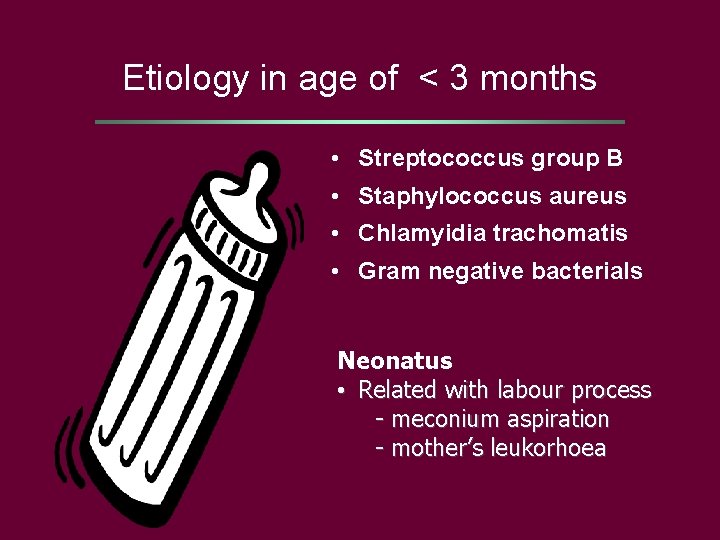
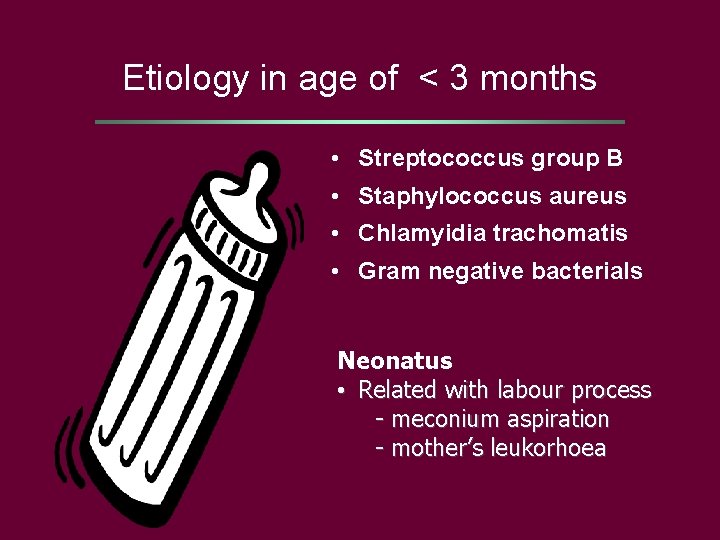
Etiology in age of < 3 months • Streptococcus group B • Staphylococcus aureus • Chlamyidia trachomatis • Gram negative bacterials Neonatus • Related with labour process - meconium aspiration - mother’s leukorhoea
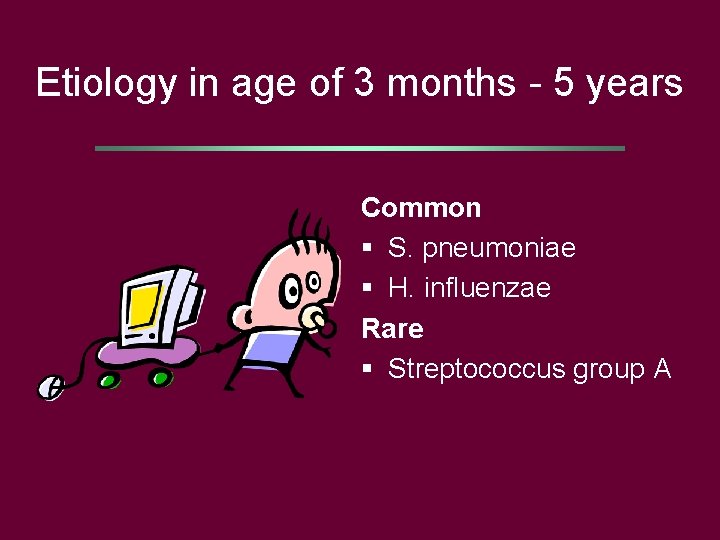
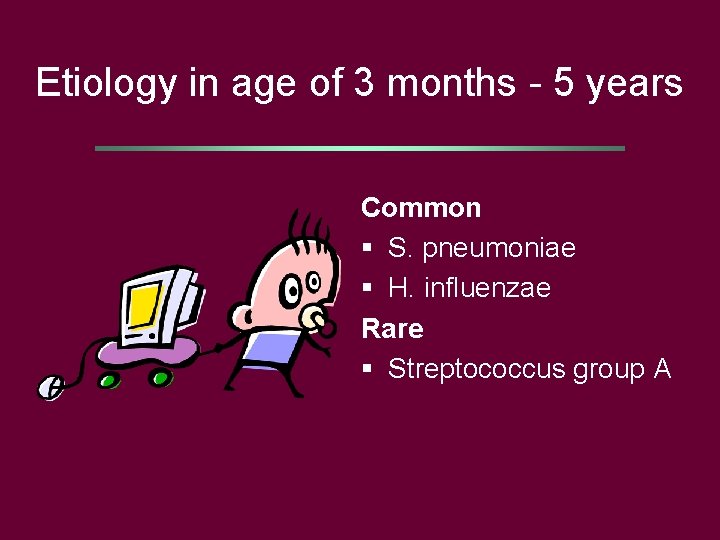
Etiology in age of 3 months - 5 years Common § S. pneumoniae § H. influenzae Rare § Streptococcus group A
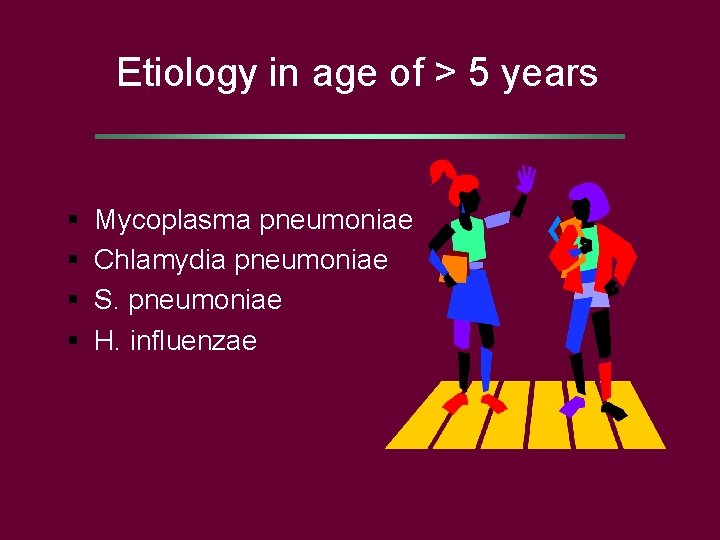
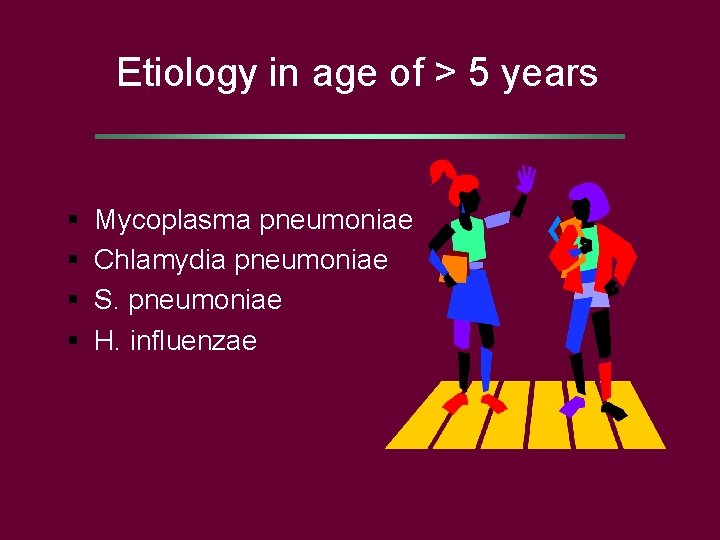
Etiology in age of > 5 years § § Mycoplasma pneumoniae Chlamydia pneumoniae S. pneumoniae H. influenzae
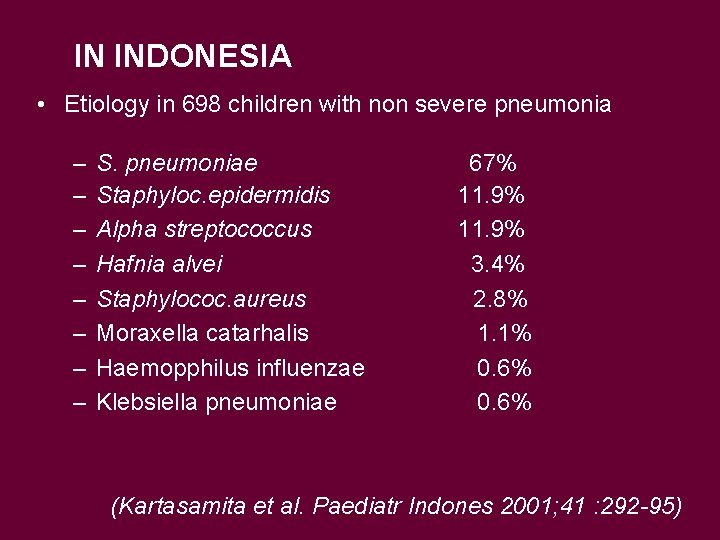
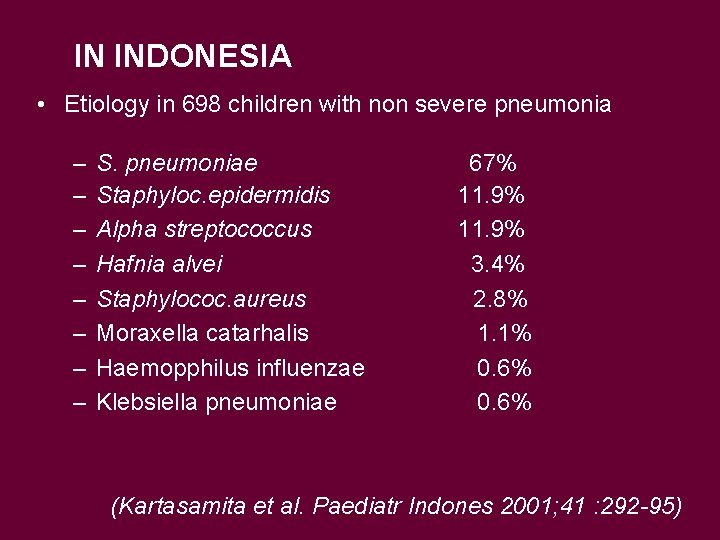
IN INDONESIA • Etiology in 698 children with non severe pneumonia – – – – S. pneumoniae Staphyloc. epidermidis Alpha streptococcus Hafnia alvei Staphylococ. aureus Moraxella catarhalis Haemopphilus influenzae Klebsiella pneumoniae 67% 11. 9% 3. 4% 2. 8% 1. 1% 0. 6% (Kartasamita et al. Paediatr Indones 2001; 41 : 292 -95)
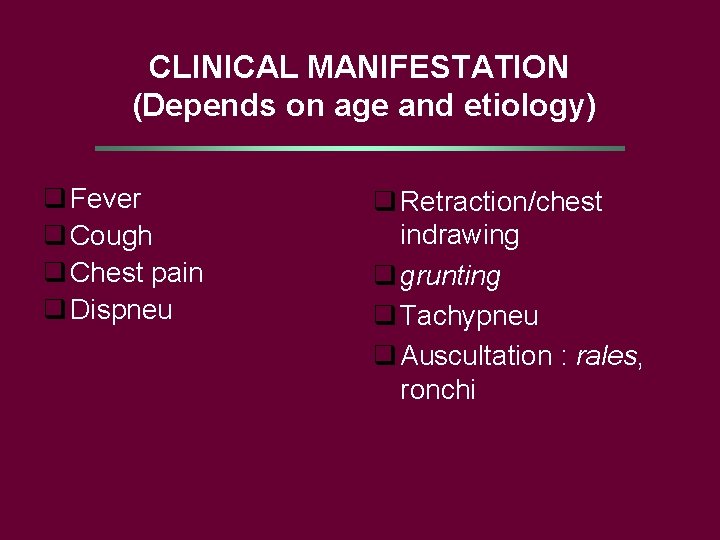
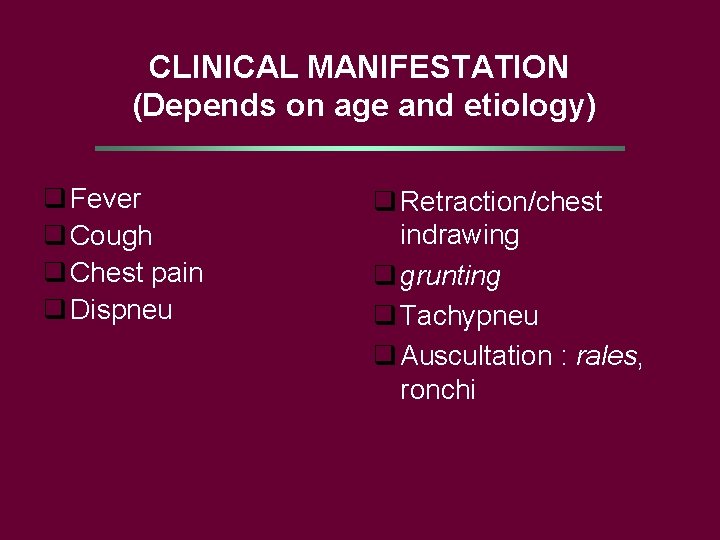
CLINICAL MANIFESTATION (Depends on age and etiology) q Fever q Cough q Chest pain q Dispneu q Retraction/chest indrawing q grunting q Tachypneu q Auscultation : rales, ronchi
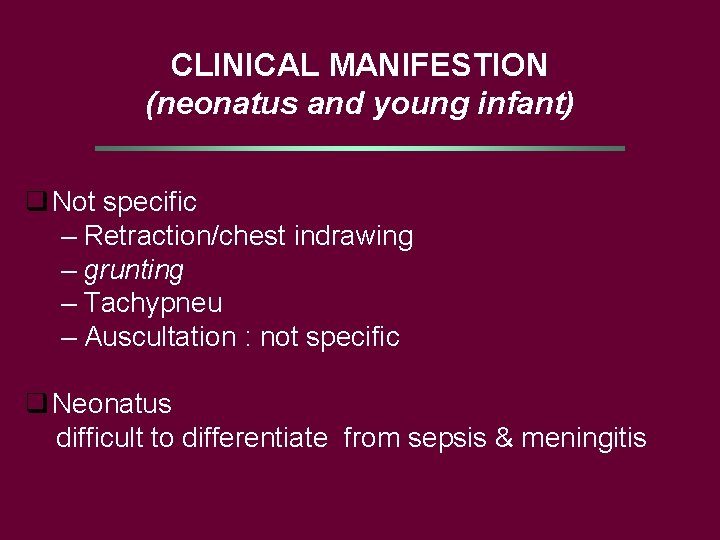
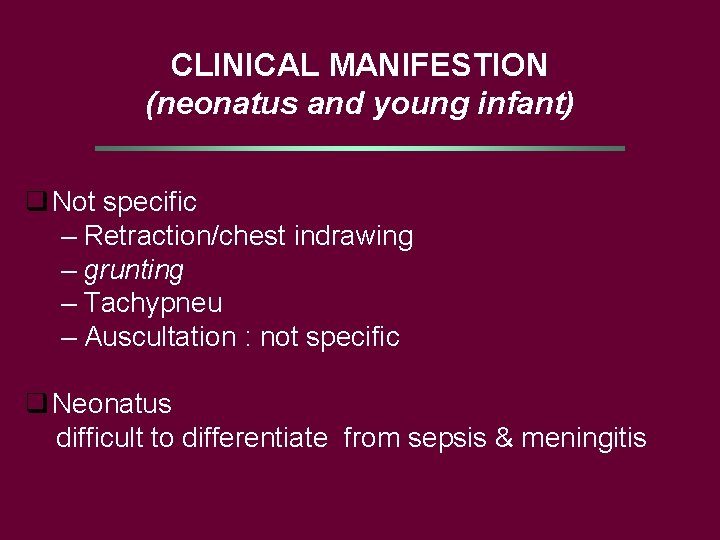
CLINICAL MANIFESTION (neonatus and young infant) q Not specific – Retraction/chest indrawing – grunting – Tachypneu – Auscultation : not specific q Neonatus difficult to differentiate from sepsis & meningitis
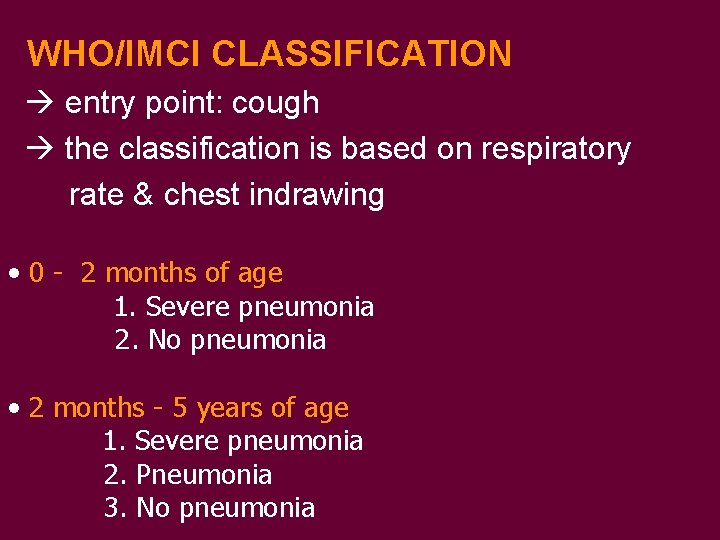
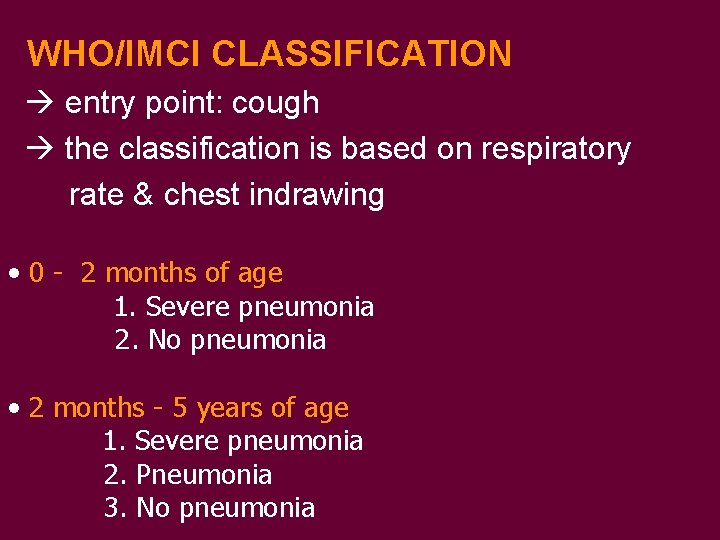
WHO/IMCI CLASSIFICATION entry point: cough the classification is based on respiratory rate & chest indrawing • 0 - 2 months of age 1. Severe pneumonia 2. No pneumonia • 2 months - 5 years of age 1. Severe pneumonia 2. Pneumonia 3. No pneumonia
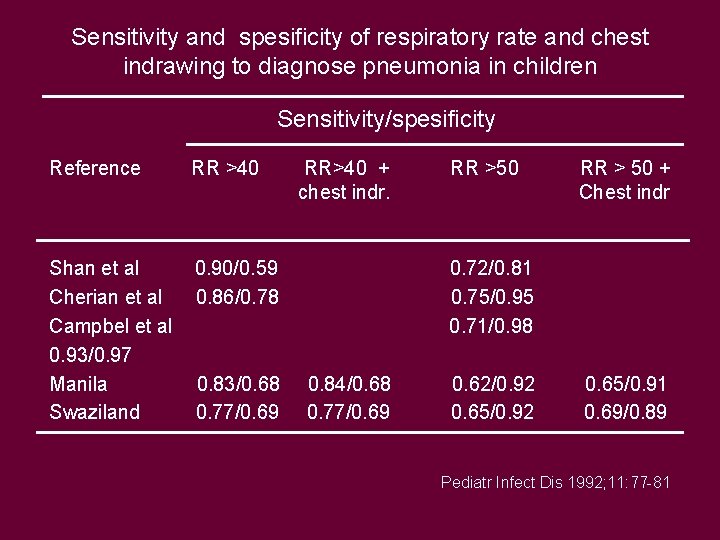
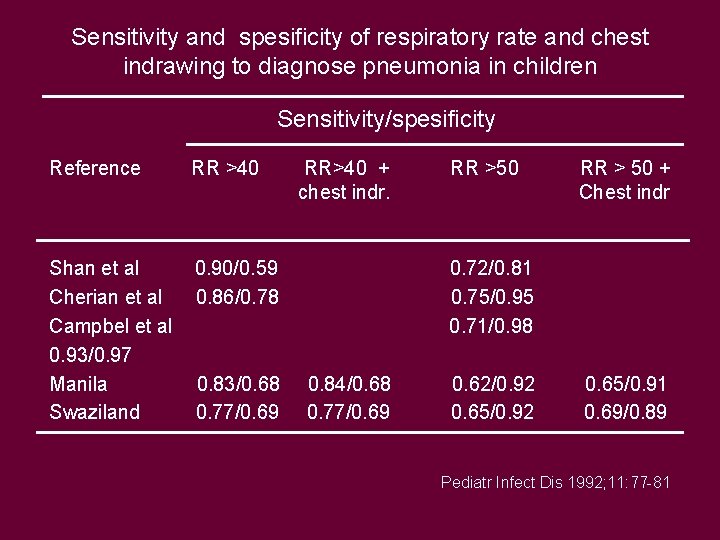
Sensitivity and spesificity of respiratory rate and chest indrawing to diagnose pneumonia in children Sensitivity/spesificity Reference RR >40 Shan et al Cherian et al Campbel et al 0. 93/0. 97 Manila Swaziland 0. 90/0. 59 0. 86/0. 78 0. 83/0. 68 0. 77/0. 69 RR>40 + chest indr. RR >50 RR > 50 + Chest indr 0. 72/0. 81 0. 75/0. 95 0. 71/0. 98 0. 84/0. 68 0. 77/0. 69 0. 62/0. 92 0. 65/0. 91 0. 69/0. 89 Pediatr Infect Dis 1992; 11: 77 -81
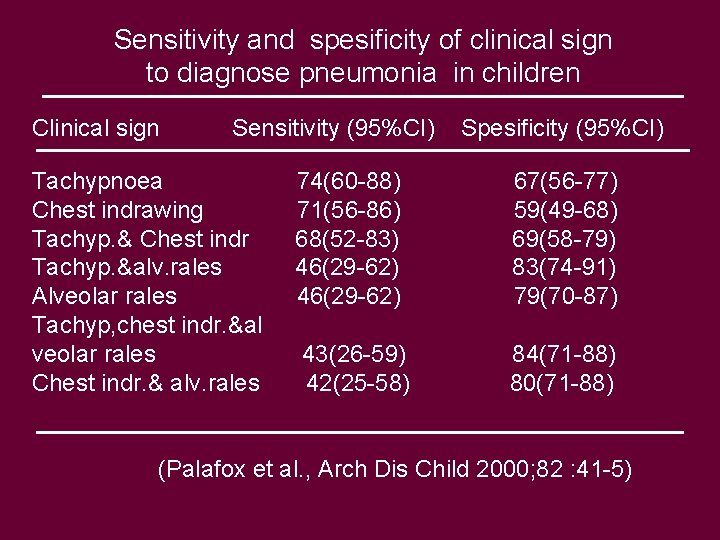
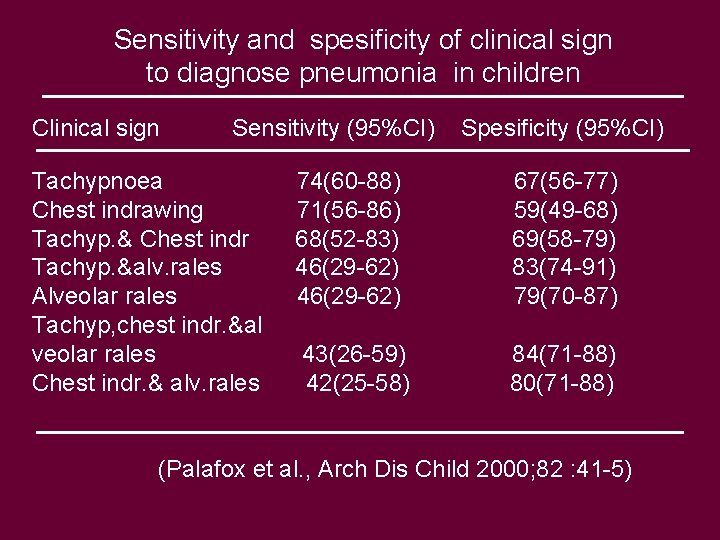
Sensitivity and spesificity of clinical sign to diagnose pneumonia in children Clinical sign Sensitivity (95%CI) Tachypnoea Chest indrawing Tachyp. & Chest indr Tachyp. &alv. rales Alveolar rales Tachyp, chest indr. &al veolar rales Chest indr. & alv. rales Spesificity (95%CI) 74(60 -88) 71(56 -86) 68(52 -83) 46(29 -62) 67(56 -77) 59(49 -68) 69(58 -79) 83(74 -91) 79(70 -87) 43(26 -59) 42(25 -58) 84(71 -88) 80(71 -88) (Palafox et al. , Arch Dis Child 2000; 82 : 41 -5)
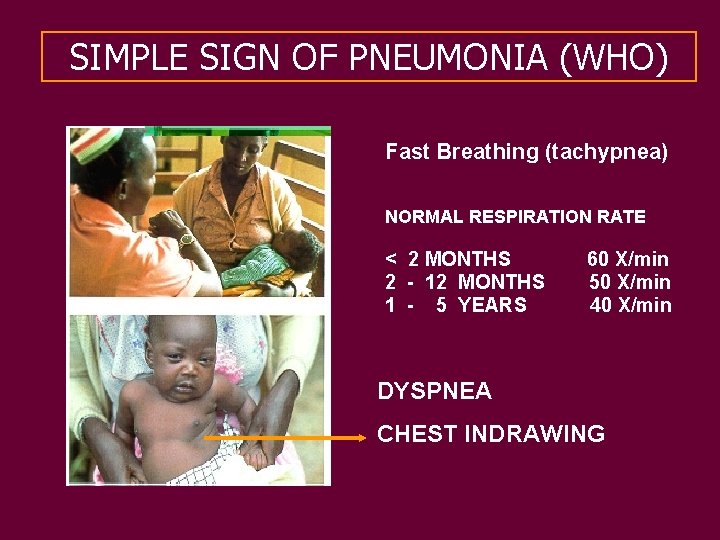
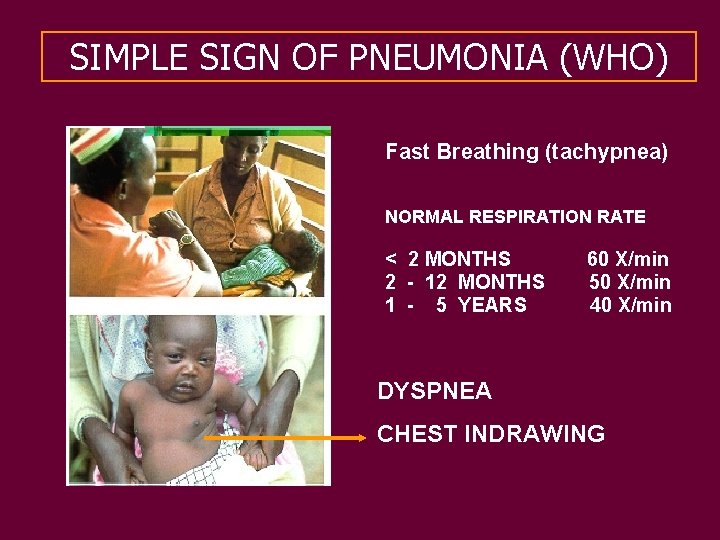
SIMPLE SIGN OF PNEUMONIA (WHO) Fast Breathing (tachypnea) NORMAL RESPIRATION RATE < 2 MONTHS 2 - 12 MONTHS 1 - 5 YEARS 60 X/min 50 X/min 40 X/min DYSPNEA CHEST INDRAWING
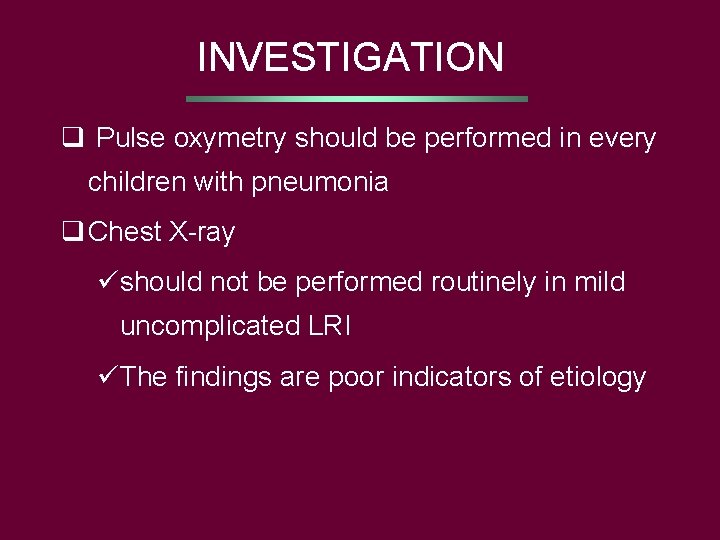
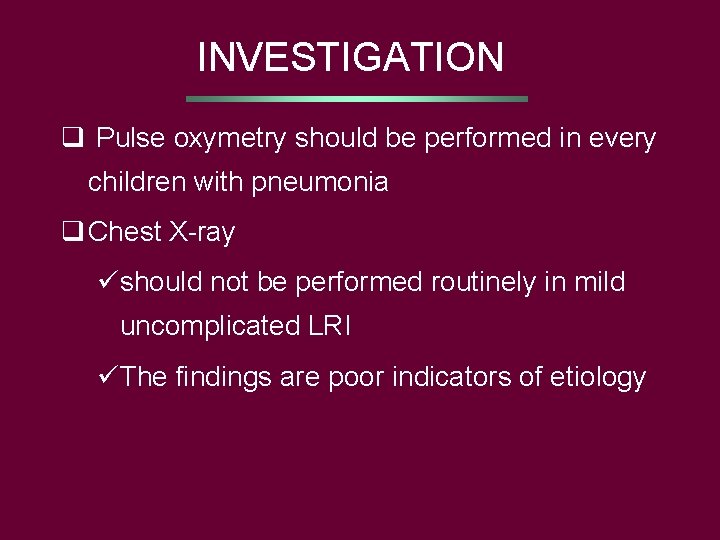
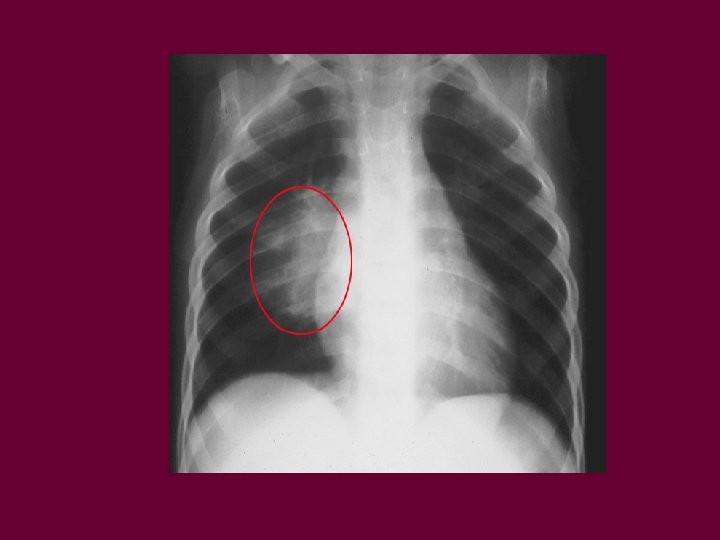
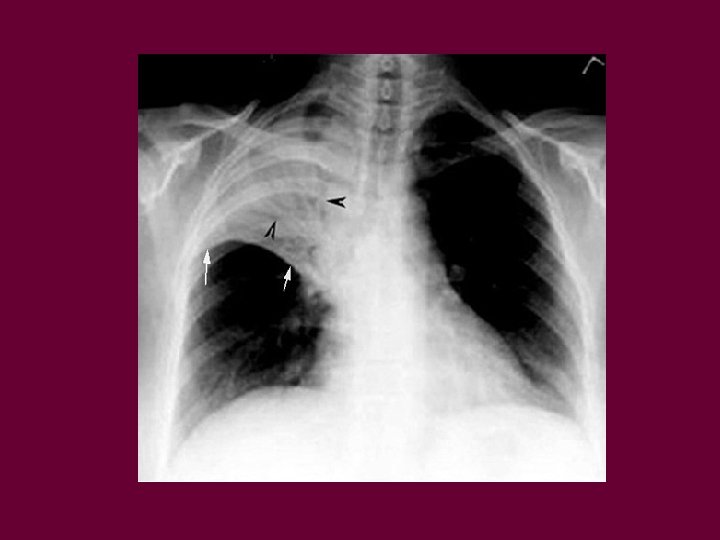
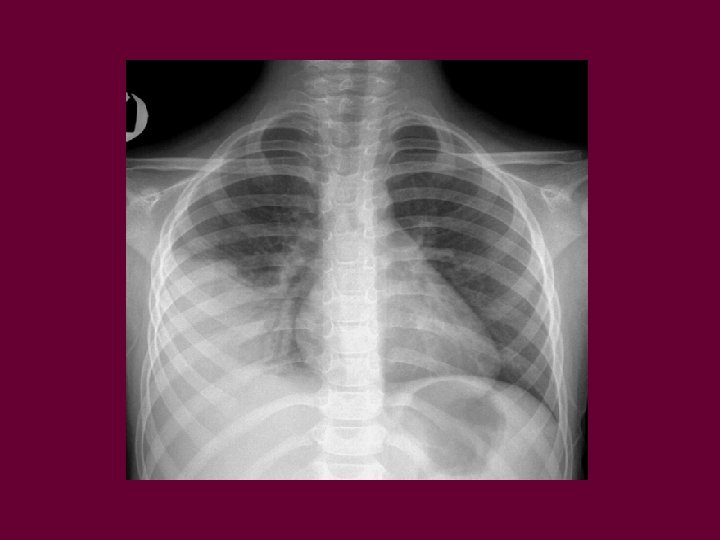
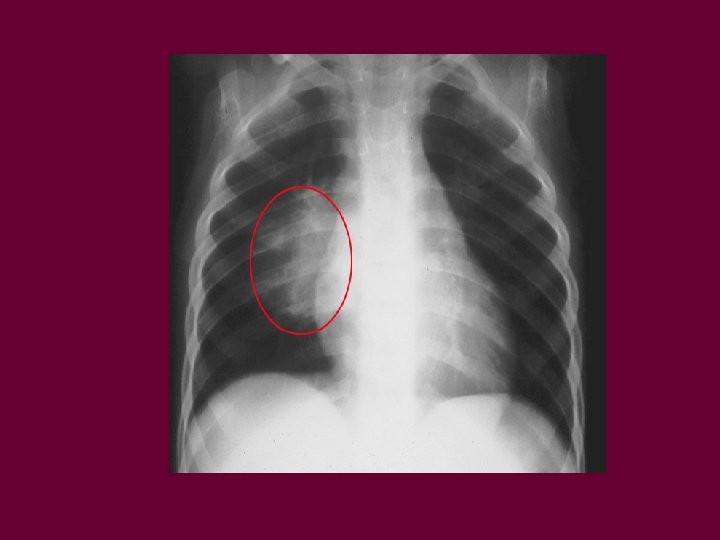
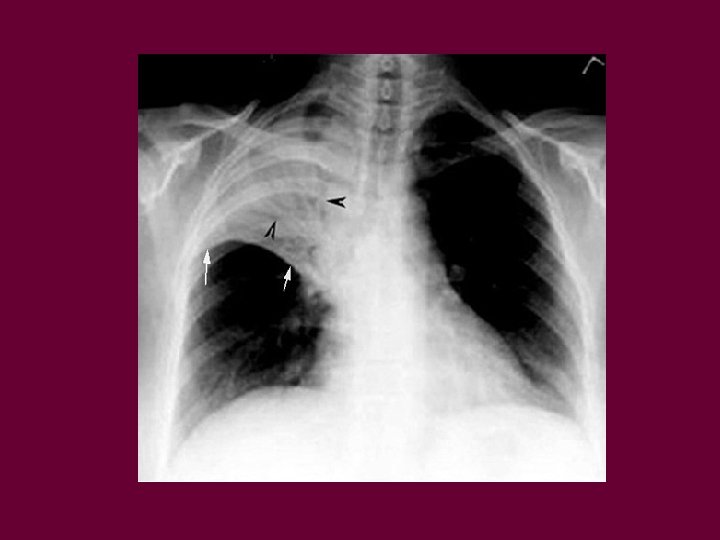
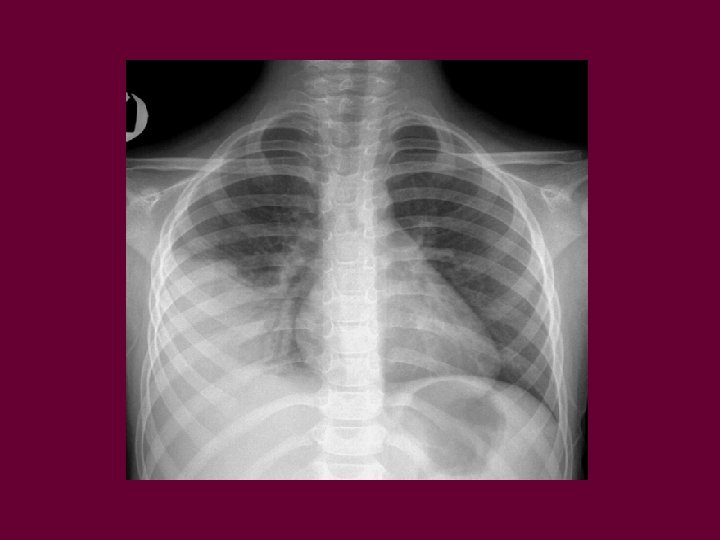
INVESTIGATION q Pulse oxymetry should be performed in every children with pneumonia q Chest X-ray üshould not be performed routinely in mild uncomplicated LRI üThe findings are poor indicators of etiology
INVESTIGATION q Blood culture q Nasopharyngeal aspirates üFrom all children under the age of 18 months should be sent for viral antigen detection q Sputum culture bronchoalveolar lavage q Pleural fluid culture if significant pleural efussion present
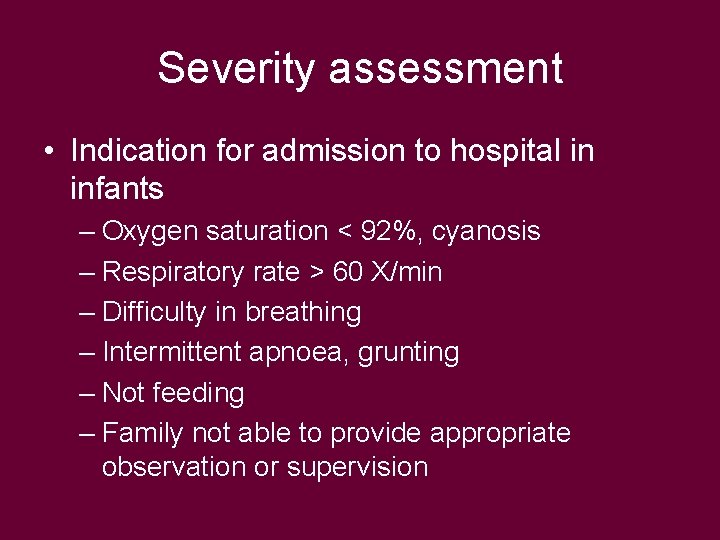
Severity assessment • Indication for admission to hospital in infants – Oxygen saturation < 92%, cyanosis – Respiratory rate > 60 X/min – Difficulty in breathing – Intermittent apnoea, grunting – Not feeding – Family not able to provide appropriate observation or supervision
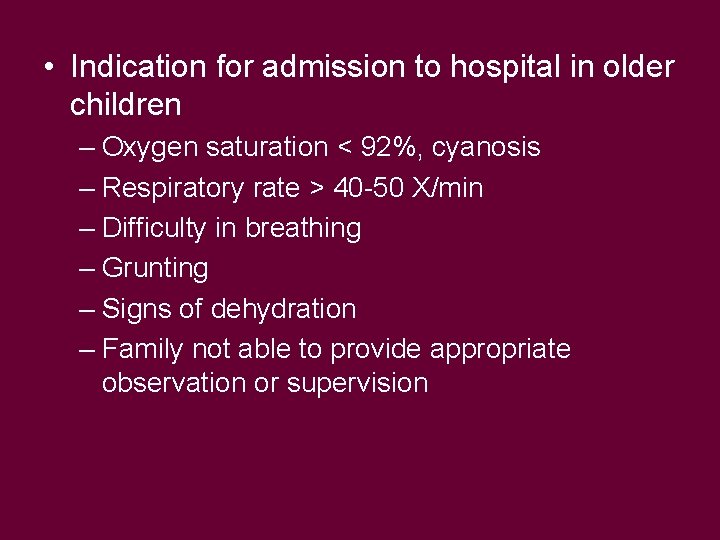
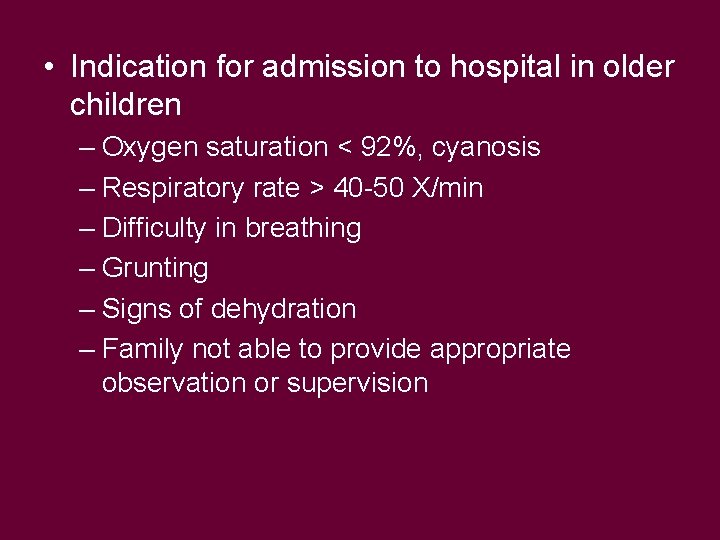
• Indication for admission to hospital in older children – Oxygen saturation < 92%, cyanosis – Respiratory rate > 40 -50 X/min – Difficulty in breathing – Grunting – Signs of dehydration – Family not able to provide appropriate observation or supervision
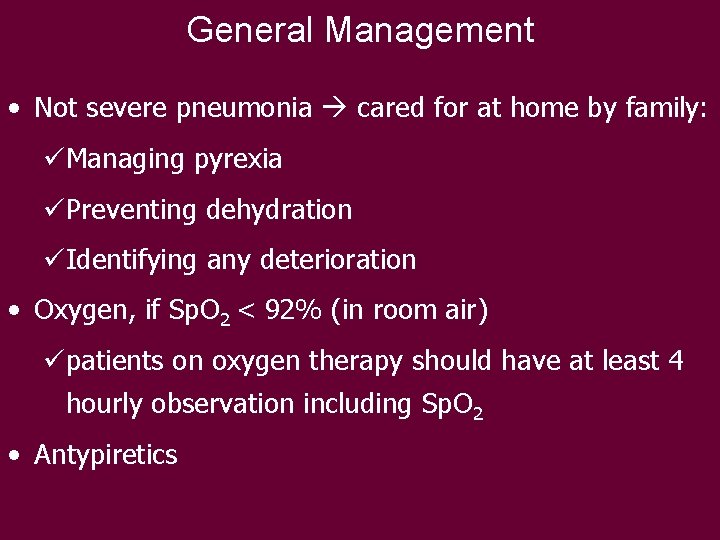
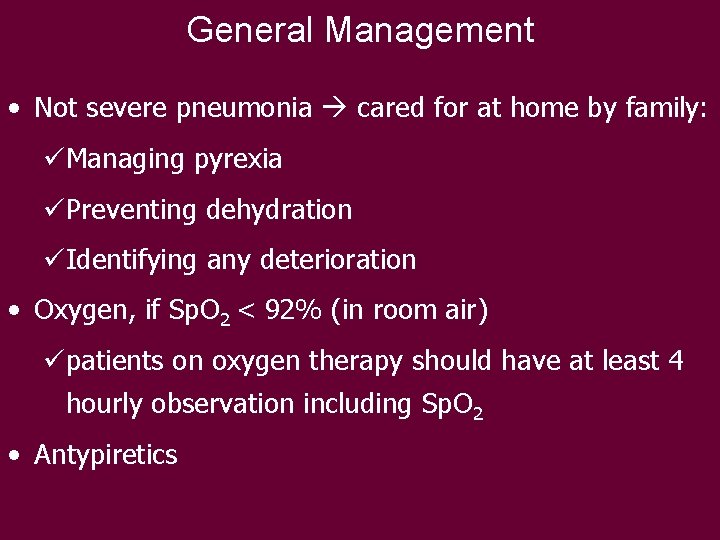
General Management • Not severe pneumonia cared for at home by family: üManaging pyrexia üPreventing dehydration üIdentifying any deterioration • Oxygen, if Sp. O 2 < 92% (in room air) üpatients on oxygen therapy should have at least 4 hourly observation including Sp. O 2 • Antypiretics
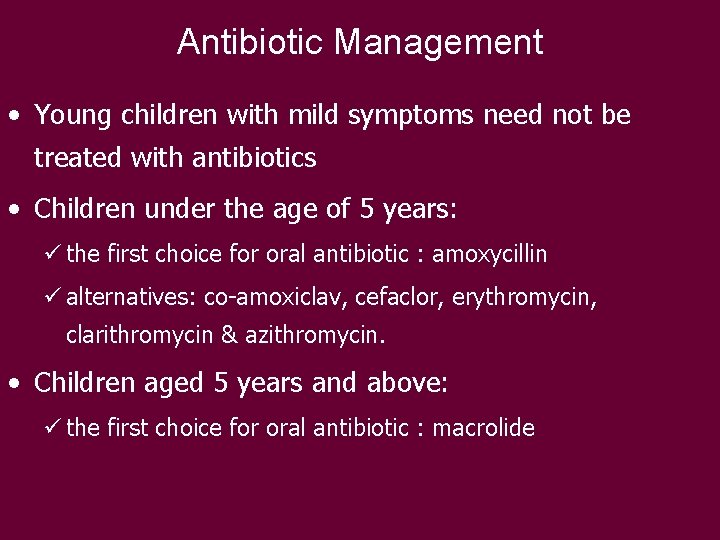
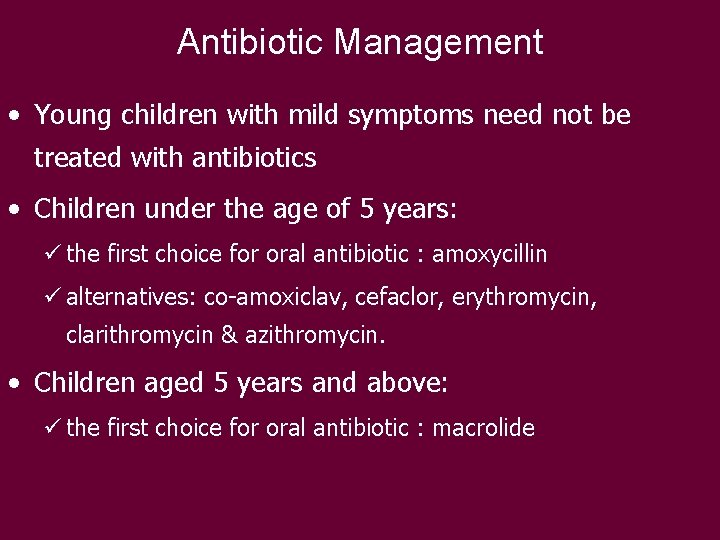
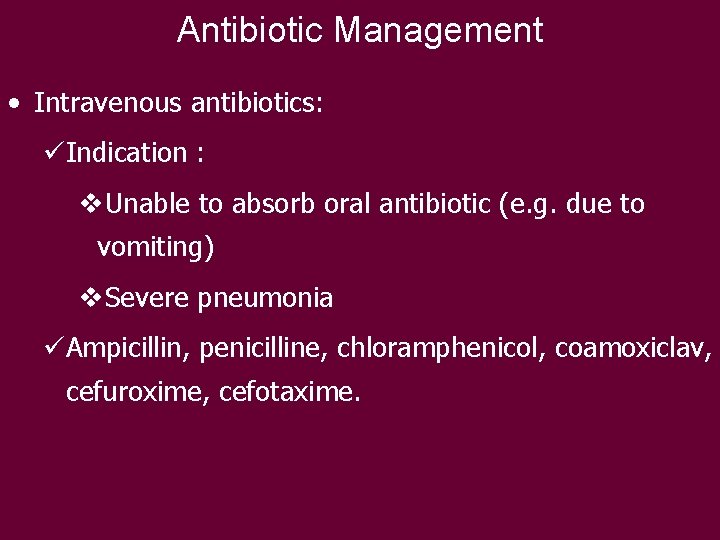
Antibiotic Management • Young children with mild symptoms need not be treated with antibiotics • Children under the age of 5 years: ü the first choice for oral antibiotic : amoxycillin ü alternatives: co-amoxiclav, cefaclor, erythromycin, clarithromycin & azithromycin. • Children aged 5 years and above: ü the first choice for oral antibiotic : macrolide
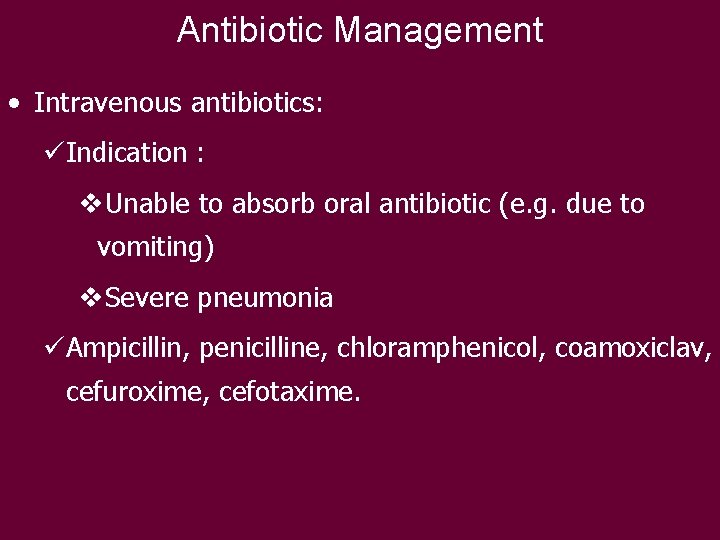
Antibiotic Management • Intravenous antibiotics: üIndication : v. Unable to absorb oral antibiotic (e. g. due to vomiting) v. Severe pneumonia üAmpicillin, penicilline, chloramphenicol, coamoxiclav, cefuroxime, cefotaxime.
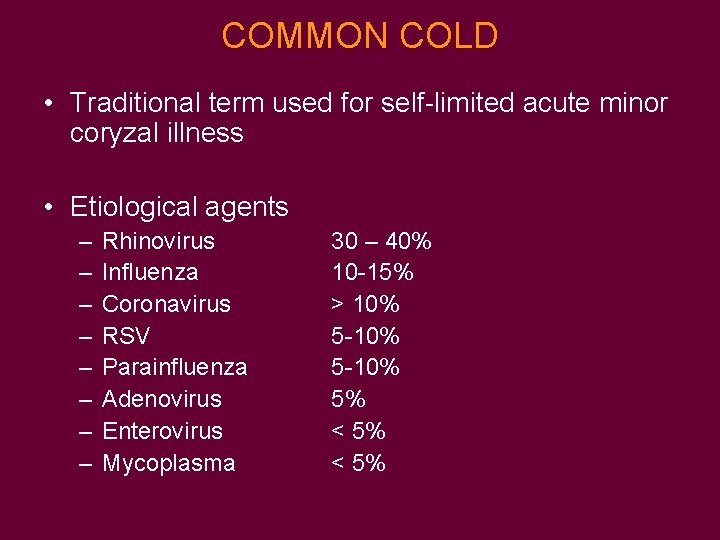
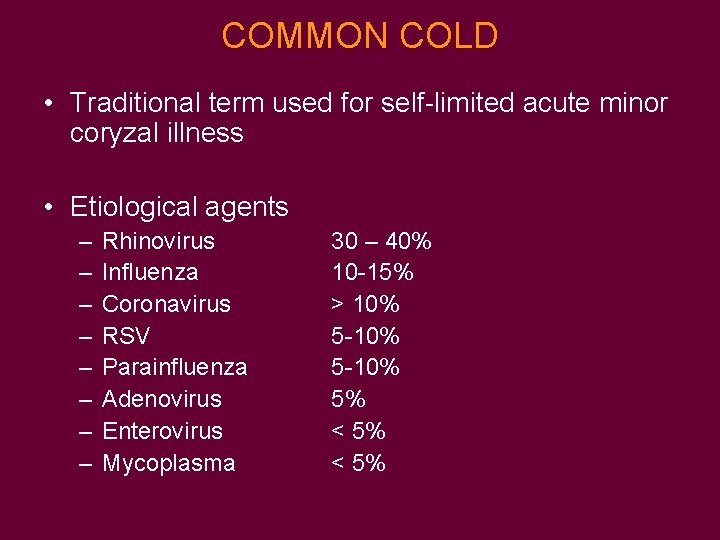
COMMON COLD • Traditional term used for self-limited acute minor coryzal illness • Etiological agents – – – – Rhinovirus Influenza Coronavirus RSV Parainfluenza Adenovirus Enterovirus Mycoplasma 30 – 40% 10 -15% > 10% 5 -10% 5% < 5%
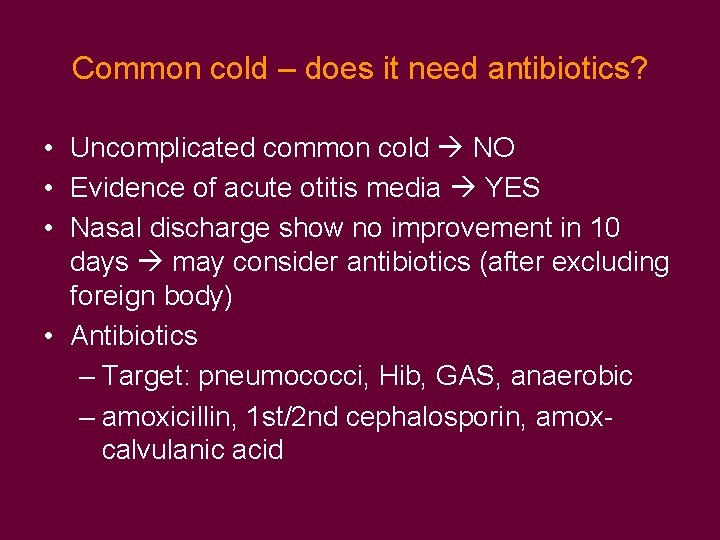
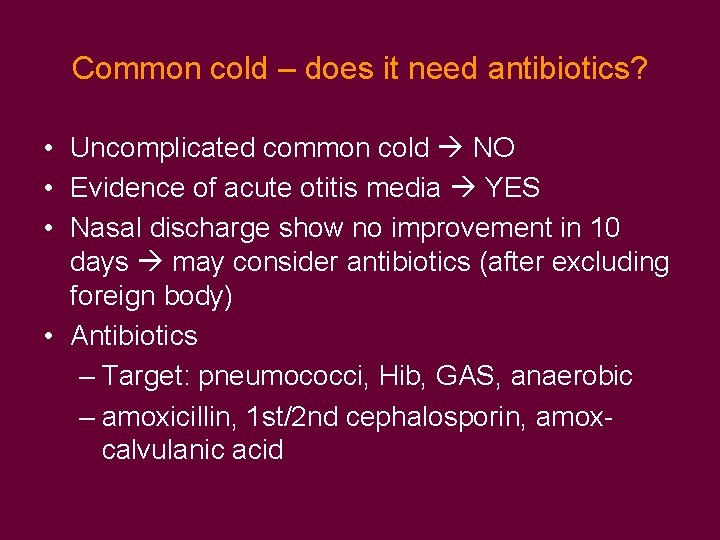
Common cold – does it need antibiotics? • Uncomplicated common cold NO • Evidence of acute otitis media YES • Nasal discharge show no improvement in 10 days may consider antibiotics (after excluding foreign body) • Antibiotics – Target: pneumococci, Hib, GAS, anaerobic – amoxicillin, 1 st/2 nd cephalosporin, amoxcalvulanic acid
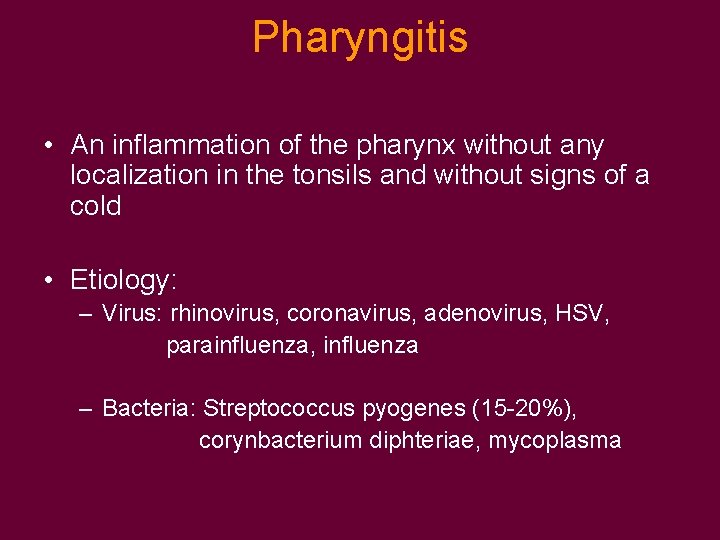
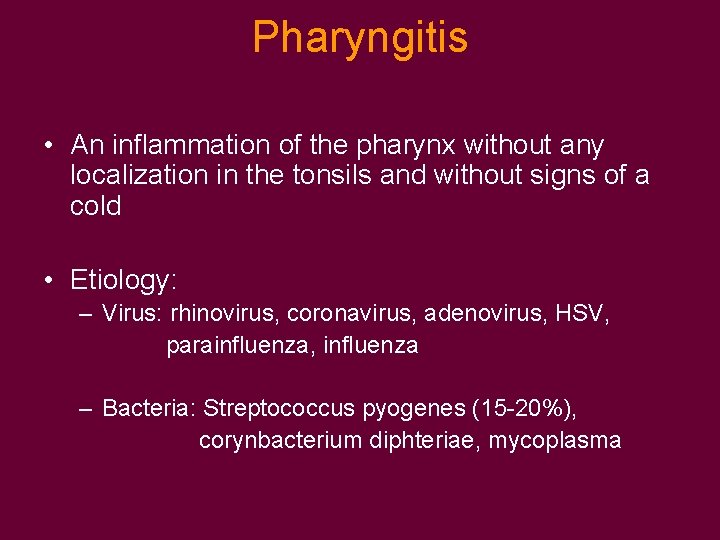
Pharyngitis • An inflammation of the pharynx without any localization in the tonsils and without signs of a cold • Etiology: – Virus: rhinovirus, coronavirus, adenovirus, HSV, parainfluenza, influenza – Bacteria: Streptococcus pyogenes (15 -20%), corynbacterium diphteriae, mycoplasma
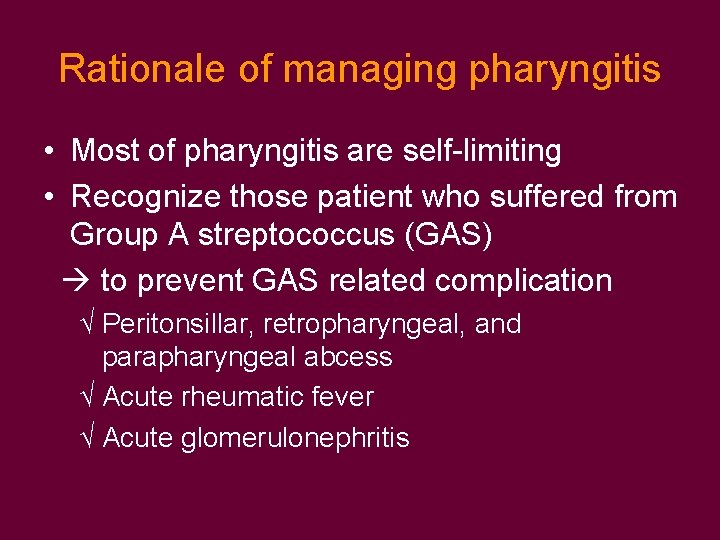
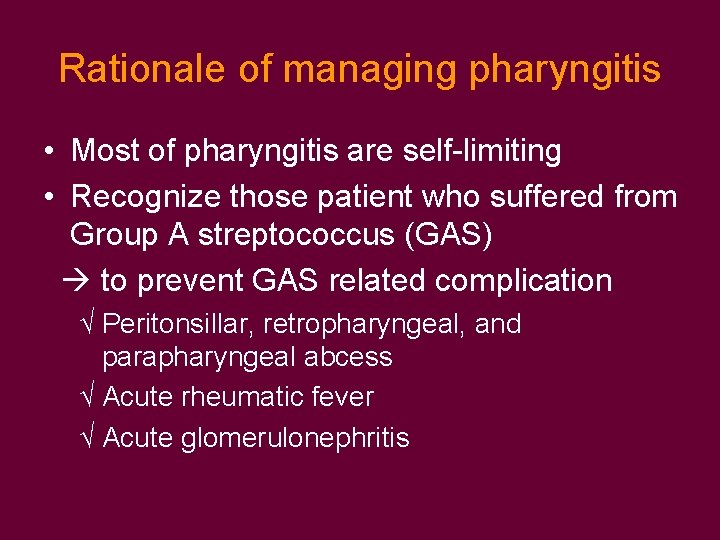
Rationale of managing pharyngitis • Most of pharyngitis are self-limiting • Recognize those patient who suffered from Group A streptococcus (GAS) to prevent GAS related complication √ Peritonsillar, retropharyngeal, and parapharyngeal abcess √ Acute rheumatic fever √ Acute glomerulonephritis
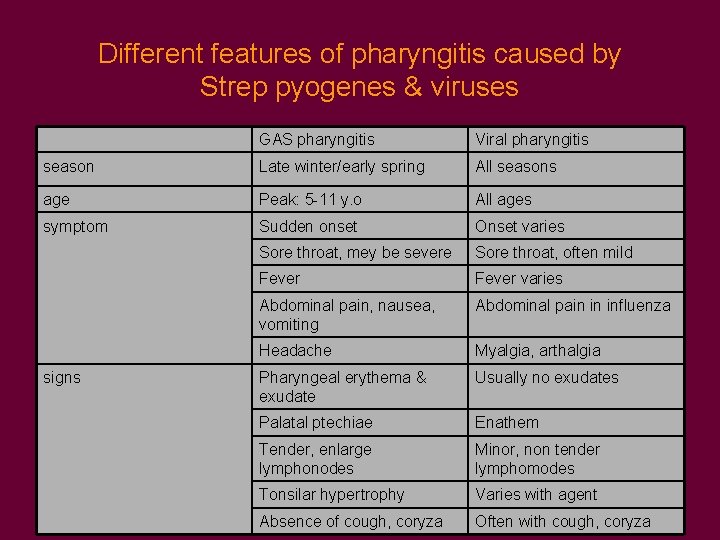
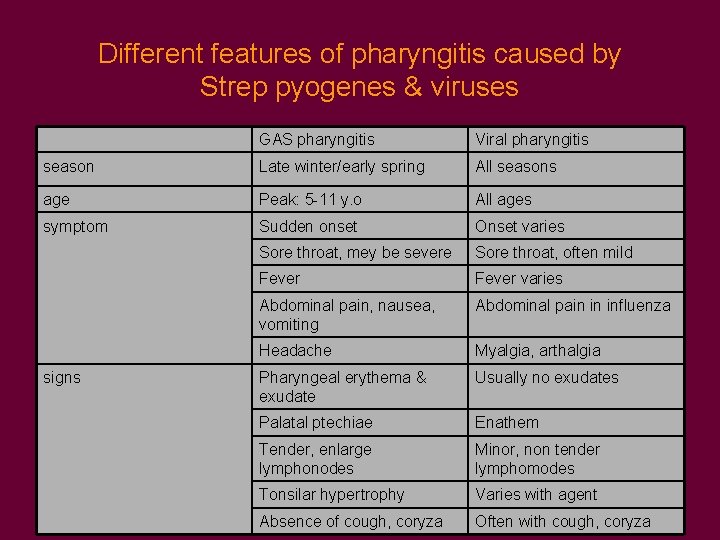
Different features of pharyngitis caused by Strep pyogenes & viruses GAS pharyngitis Viral pharyngitis season Late winter/early spring All seasons age Peak: 5 -11 y. o All ages symptom Sudden onset Onset varies Sore throat, mey be severe Sore throat, often mild Fever varies Abdominal pain, nausea, vomiting Abdominal pain in influenza Headache Myalgia, arthalgia Pharyngeal erythema & exudate Usually no exudates Palatal ptechiae Enathem Tender, enlarge lymphonodes Minor, non tender lymphomodes Tonsilar hypertrophy Varies with agent Absence of cough, coryza Often with cough, coryza signs
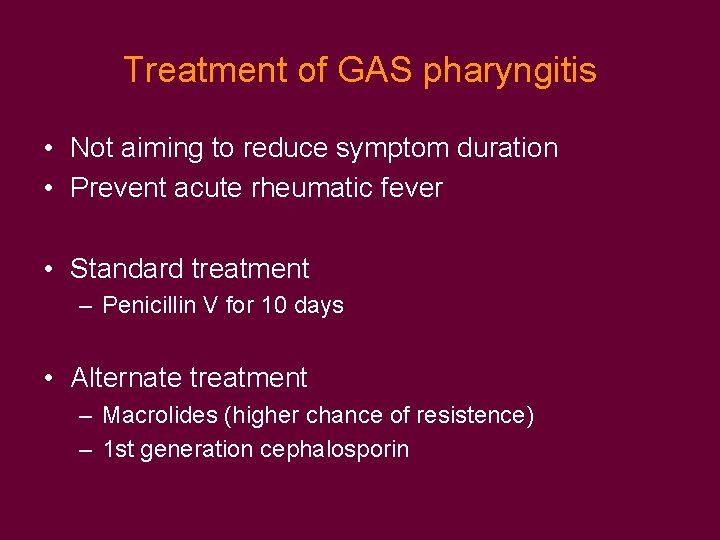
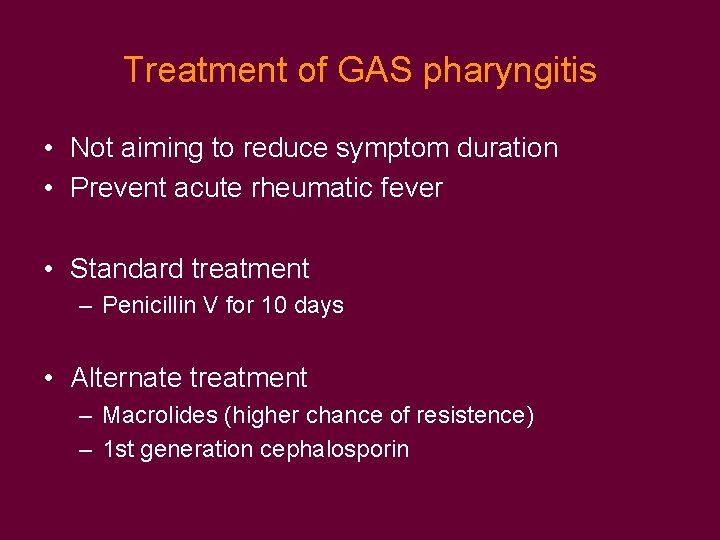
Treatment of GAS pharyngitis • Not aiming to reduce symptom duration • Prevent acute rheumatic fever • Standard treatment – Penicillin V for 10 days • Alternate treatment – Macrolides (higher chance of resistence) – 1 st generation cephalosporin

Thank you