Common pediatric rashes Discussion outline Dermatology terminology Common

















- Slides: 46
Common pediatric rashes
Discussion outline • • Dermatology terminology Common benign newborn rashes Common infectious newborn rashes Newborn vascular lesions • Various other pediatric rashes
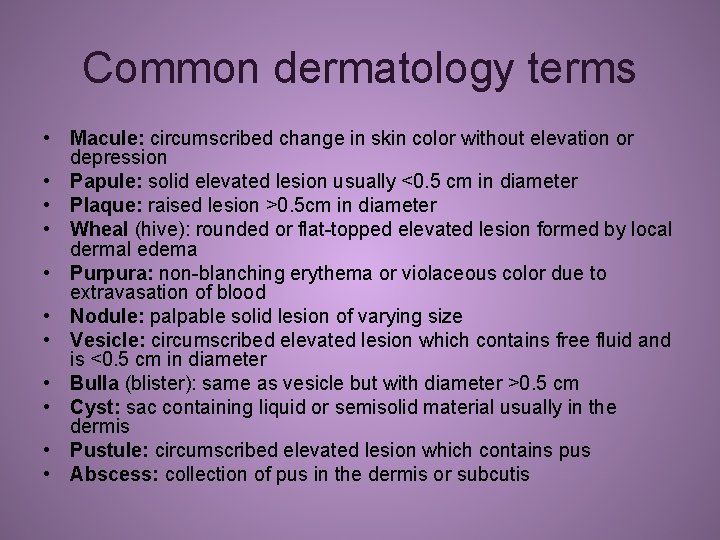
Common dermatology terms • Macule: circumscribed change in skin color without elevation or depression • Papule: solid elevated lesion usually <0. 5 cm in diameter • Plaque: raised lesion >0. 5 cm in diameter • Wheal (hive): rounded or flat-topped elevated lesion formed by local dermal edema • Purpura: non-blanching erythema or violaceous color due to extravasation of blood • Nodule: palpable solid lesion of varying size • Vesicle: circumscribed elevated lesion which contains free fluid and is <0. 5 cm in diameter • Bulla (blister): same as vesicle but with diameter >0. 5 cm • Cyst: sac containing liquid or semisolid material usually in the dermis • Pustule: circumscribed elevated lesion which contains pus • Abscess: collection of pus in the dermis or subcutis
Benign newborn rashes • • Erythema toxicum neonatorum Miliaria Neonatal acne Milia Seborrheic dermatitis Benign pustular melanosis of the newborn Sucking blisters Presented in random order….

Miliaria • Due to obstruction and rupture of exocrine sweat duct • Commonly seen secondary to thermal stress, particularly with crops of lesions over face, scalp, and trunk – Important to ensure infant is not over-wrapped – Once heat stress is removed, lesions usually resolve quickly

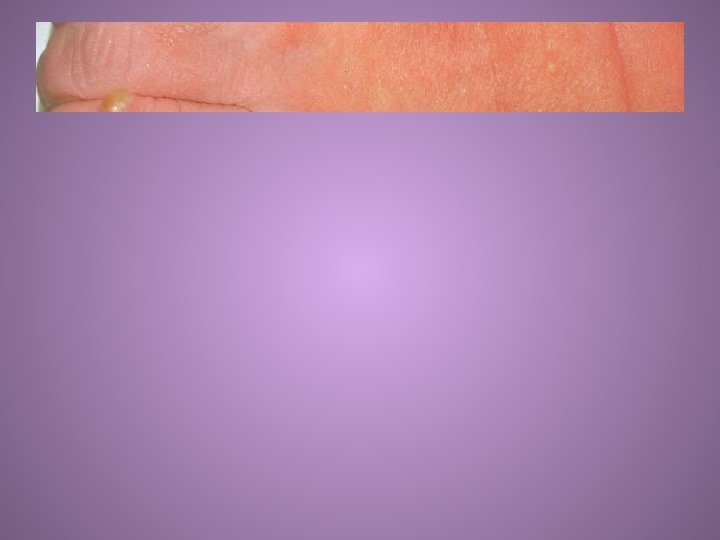
Neonatal acne • Can be present at birth or develop in first 2 -4 weeks of life • Consists of pustules over the cheeks primarily, but also involves other areas of face and scalp • No comedones in neonatal form • Resolves spontaneously and without scarring

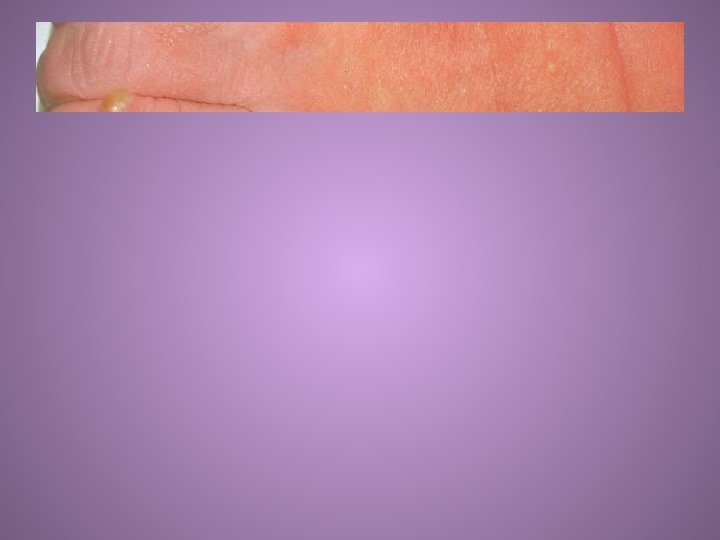
Benign pustular melanosis of the newborn • Lesions present at birth • Superficial pustules which rupture easily without pus content, leaving spot of hyperpigmentation • Pustules last 1 -2 days but pigmented spots may persist for a while • Any area of the body may be involved • Smears from pustules reveal polymorphonuclear leukocytes with absence of organisms

Seborrheic dermatitis • Primarily affects scalp and intertriginous areas – Involvement of scalp is frequently termed "cradle cap“ and manifests as greasy, yellow plaques on scalp • Most common in first 6 weeks of life, but can occur in children up to 12 months of age • Usually clears up without treatment in 3 -4 weeks – If needed, treatment can include mild tar shampoo, oatmeal baths, avoidance of soaps, and occasional use of mild topical steroid – Involvement of skin creases can lead to secondary candidal infections • Etiology unknown

Erythema toxicum neonatorum • Onset on day 2 -3 of life, mostly in term babies – Lesions wax and wane over ensuing 3 -6 days – Lesions may intensify or coalesce particularly in response to local heat • Central white-yellow papule surrounded by a halo of erythema, mainly over trunk (but also on limbs and face) • Scrapings of lesions would reveal eosinophils • Etiology unknown


Milia • Tiny, white, usually discrete papules – Inclusion cysts that contain trapped keratinised stratum corneum • Commonly occur on face and scalp • Usually resolve within a few months without treatment • Rarely associated with dermatologic syndromes – Epidermolysis bullosa, oro-facial-digital syndrome (type 1) • Similar lesions may occasionally be seen in mouth – When on hard palate, called Epstein's pearls – When on alveolar ridges, called alveolar cysts or Bohn's nodules

Sucking blisters • Present at birth, most often over dorsal and lateral aspect of wrist – Either bilateral or unilateral • May appear like well-demarcated bruises or vesicles • Infant is noted to exhibit excessive sucking activity
Infectious newborn lesions • • Staphylococcal pustules Herpes simplex Generalized in utero infection Paronychia Bullous impetigo Omphalitis Congenital syphilis Candida Dermatitis Presented in random order….

Paronychia • Localized inflammation with infection of nail fold • Relatively common in infants • Treat most infections with oral antibiotics and severe cases with IV antibiotics – First line treatment is usually flucloxacillin/floxacillin for Staphylococcus aureus or Streptococcus pyogenes – For chronic lesions, consider Gram-negative organisms or Candida as potential causes

Bullous impetigo • Skin infection typically caused by Staphylococcus aureus • Lesions tend to appear DOL 5 -10 • Any body site may be involved, with predilection to diaper area • Bullae are flaccid, containing straw colored or turbid fluid – Rupture easily leaving moist denuded area (“honeycrusted lesions”) • Treatment with systemic antibiotics, particularly for lesions around umbilicus

Staphylococcal pustule • • Typically seen first few days of life Predilection to neck, axilla, and inguinal areas Nearly always caused by Staphylococcus aureus If one lesion, may be treated "expectantly" with application of chlorhexidine (mainly to prevent spread) – However, if more than one lesion, oral antibiotics are indicated after culture is taken – For pustules in periumbilical area, consider systemic antibiotics


Herpes simplex • May involve skin, mouth, or eye • Lesions typically develop DOL 5 -10 • Grouped vesicles may be seen, often in linear distribution if affecting limbs (1 st slide) • If vesicle eroded, shallow ulcer with erythematous base may be seen (2 nd slide) • May have associated lesions on lips -- similar to those of "cold sore" in an adult
Herpes Simplex Cont’ • HSV infection develops in one of three patterns, with roughly equal frequency – Localized to the skin, eyes, and mouth (SEM) – Localized CNS disease – Disseminated disease involving multiple organs • Can develop anytime between birth and four weeks • Patients with disseminated disease present earliest, often within the first week after delivery, although CNS symptoms usually occur during the second or third week
Discussion point: How do you differentiate HSV from impetigo from staph from millia?

Omphalitis • Infection of umbilical stump – Erythematous, edematous, +/- exudative • Most commonly occurs after day 3 • Infective organisms are variable, but S. aureus, S. pyogenes, and Gram-negative organisms are common – If cultures available, swab affected area for Gram-stain and culture to guide treatment – Initiate IV antibiotics

Congenital syphilis • Dermatological findings quite variable – Classically involve palmar/plantar, perioral, and anogenital regions • Early lesions include petechiae, hemorrhagic vesicles, and bullae • Lesions extremely infectious • May have extracutaneous findings – Hepatomegaly, low birth weight, thrombocytopenia, anaemia, jaundice, respiratory distress, osteochondritis, hydrops fetalis, meningitis, chorioretinitis, and pseudoparalysis – Older infants may present with "snuffles" (syphylitic rhinitis) which, in early stages, may be mistaken for URI
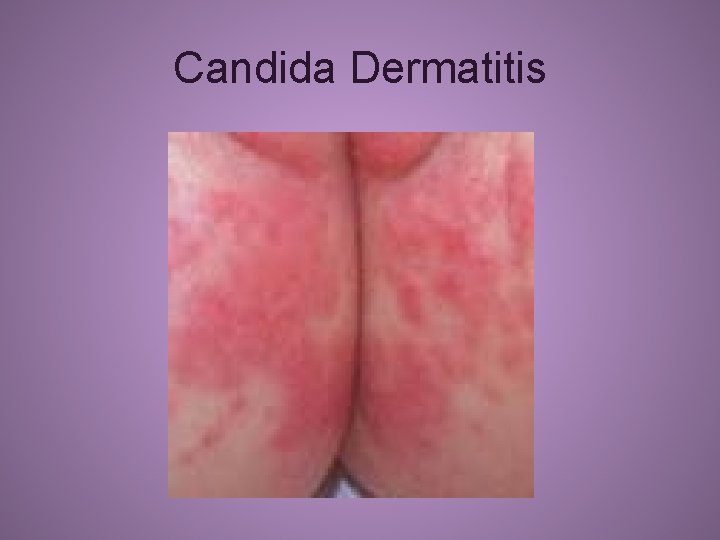
Candida Dermatitis • A common condition of young infants • Most commonly caused by C. albicans • Characteristically appears as an erythematous rash in the inguinal region • Classically has areas of confluent erythema with discrete erythematous papules and plaques with superficial scales • Satellite lesions are typically noted
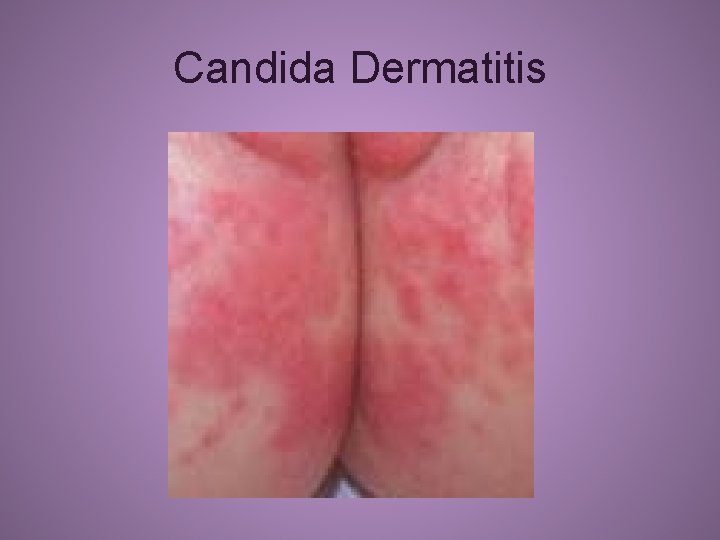
Candida Dermatitis
Newborn vascular lesions • Harlequin phenomenon • Cutis marmorata

Cutis marmorata • Reticulated pattern of constricted capillaries and venules – Often called "mottling“ • Due to vasomotor instability in immature infants • Generally resolves with increasing age and for most infants is of no significance – However, may reflect underlying poor perfusion – Infants who develop mottling and are unwell need to be clinically evaluated for sepsis and other illnesses

Harlequin phenomenon • Striking reddening of one side of body and blanching of other half • Each episode may last from seconds to minutes • Episodes occur most often during first few days of life • Thought to be vascular manifestation of changes occurring in newborn’s autonomic system
Various other pediatric rashes Adapted from: Paul Geltman, MD, MPH and Johns Hopkins Derm. Atlas The following are ~80 slides to be used as time permits – possibly during a second lecture session. Some photos may contain nude anatomy and would not be appropriate for openly public display.
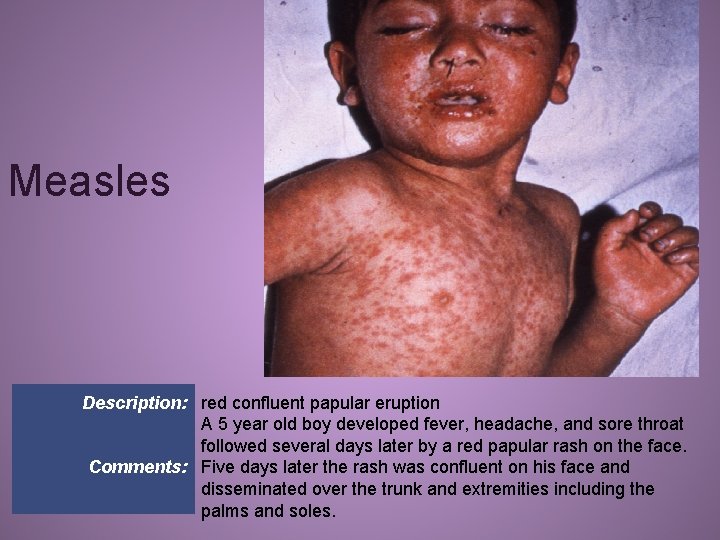
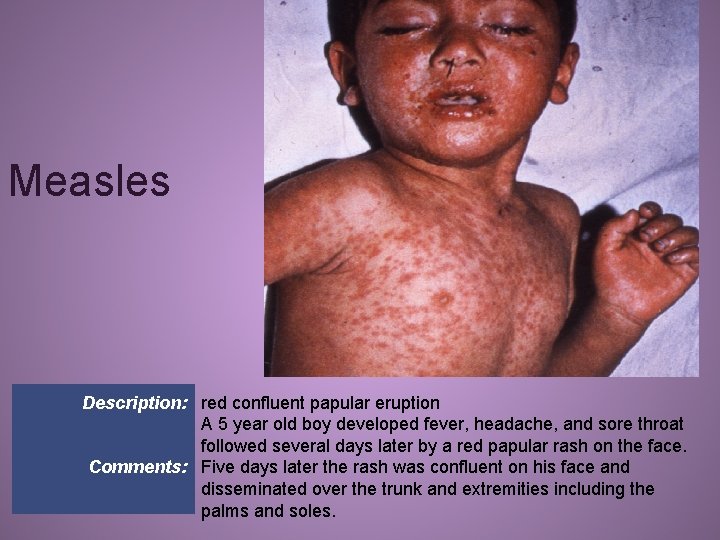
Measles Description: red confluent papular eruption A 5 year old boy developed fever, headache, and sore throat followed several days later by a red papular rash on the face. Comments: Five days later the rash was confluent on his face and disseminated over the trunk and extremities including the palms and soles.
[The remainder of these ~80 slides have been temporarily removed from this lecture due to space limitations. The full lecture (25 MB) is available from brett. d. nelson@gmail. com. ]