COMMON OPHTHALMIC CONDITIONS IN A GP PRACTICE BY
COMMON OPHTHALMIC CONDITIONS IN A GP PRACTICE BY : DR RK SYDNEY SEBILOANE
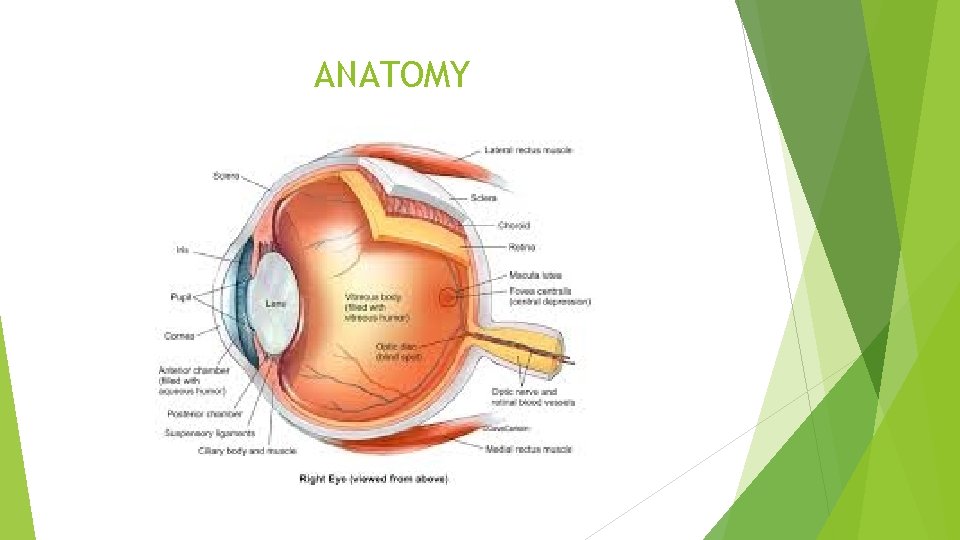
ANATOMY
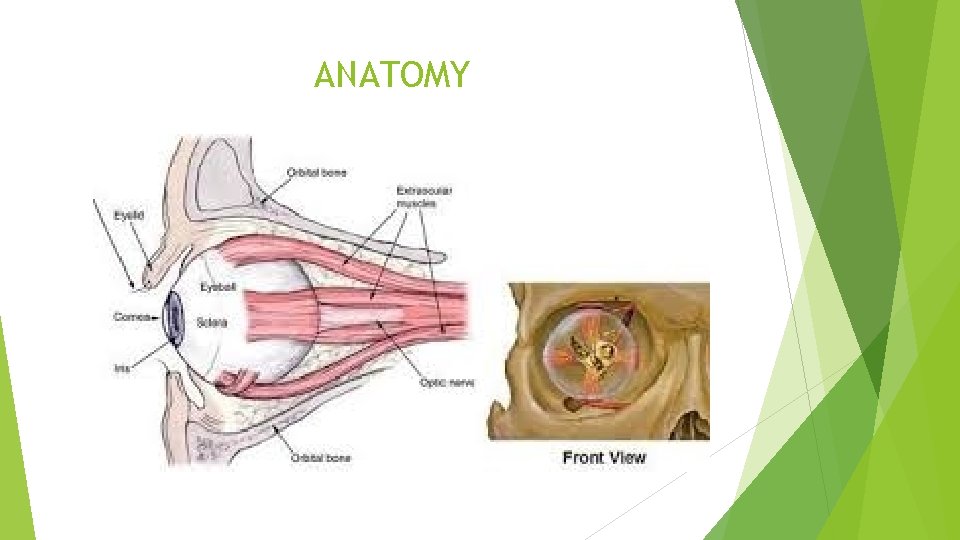
ANATOMY
CLINICAL EVALUATION Look at the patient as a whole Greet the patient – Introduce yourself Look at the appearance Can the patient use all four limbs ALL THIS ARE IMMEDIATE IMPRESSIONS YOU GET WHEN THE PATIENT WALKS INTO YOUR ROOM
OPHTHALMOLOGY EVALUATION Main complaint History of the main complaint Any previous surgery, co-morbidities, current treatment Systemic enquiry Summary of all relevant factors
OPHTHALMOLOGY EVALUATION (CONTINUED) Visual acuity including pinhole Ocular motility Slit-lamp bio-microscopy Summary of clinical findings including differential diagnosis Relevant investigations
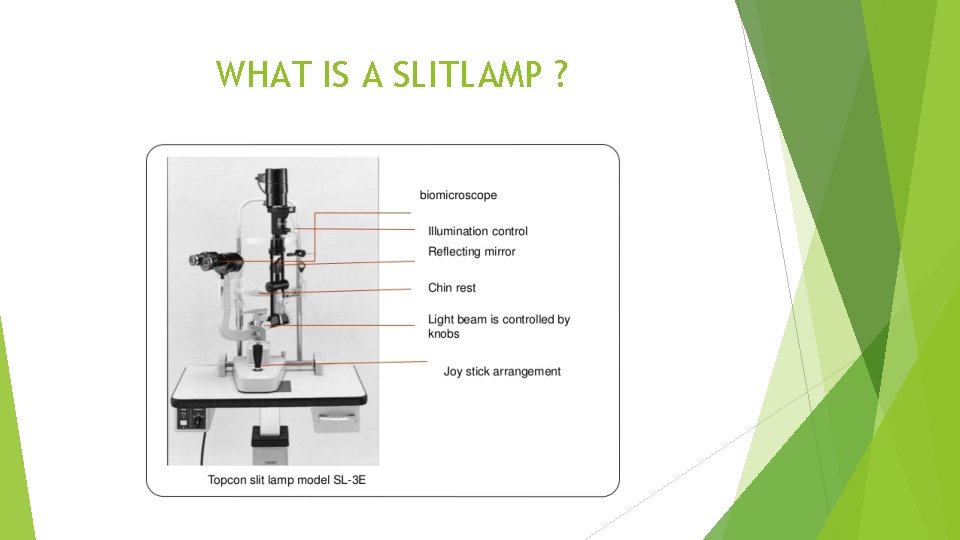
WHAT IS A SLITLAMP ?
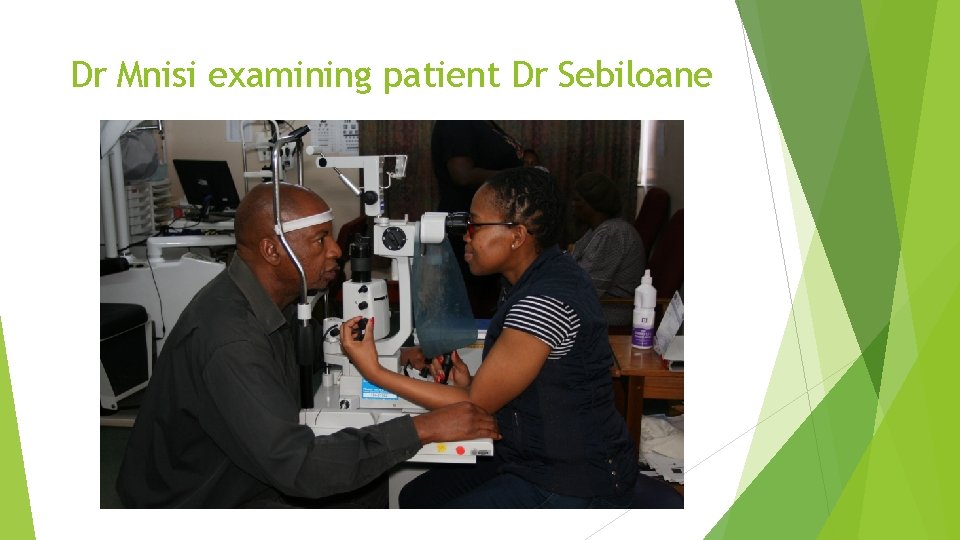
Dr Mnisi examining patient Dr Sebiloane
CLINICAL APPROACH Patients appearance and mobility, any head tilt, obvious abnormalities Facial appearance Orbit and Peri-orbita Eyelids Position of eyes in primary gaze and ocular motility Conjunctiva and Sclera Cornea Anterior Chamber Iris and Pupil Lens Vitreous Humour Retina and Optic nerve Neuro-Ophthalmolgy

ORBIT
Pre-Septal Cellulitis Very common Young children Follows insect bite Swelling of eyelid Visual acuity is normal Ocular motility is normal Eye ball is normal Imaging e. g. CT-scan, MRI is normal Treatment systemic antibiotics e. g. Augmentin, Ampicloxacillin

Pre-Septal Cellulitis
ORBITAL CELLULITIS Much less common May follow slight trauma 85% of cases follows extension from the sinuses, ethmoid sinus in particular Ocular motility is limited Visual acuity is decreased NB. Proptosis Treatment urgent referral
ORBITAL CELLULITIS - complications Exposure keratoplasty Central retinal artery occlusion Optic neuritis Meningitis Brain abscess Cavernous sinus thrombosis NB. Can cause severe morbidity and mortality
ORBITAL CELLULITIS - Treatment Urgent referral – Admission to hospital Broad-spectrum Intravenous antibiotics including anaerobic cover Cover haemophilus in children Four hourly optic nerve functioning i. e. Visual acuity, pupillary reaction, colour perception, light brightness sensitivity Imaging CT scan of orbit and sinuses is adequate Multi disciplinary approach including ENT and Neurosurgery
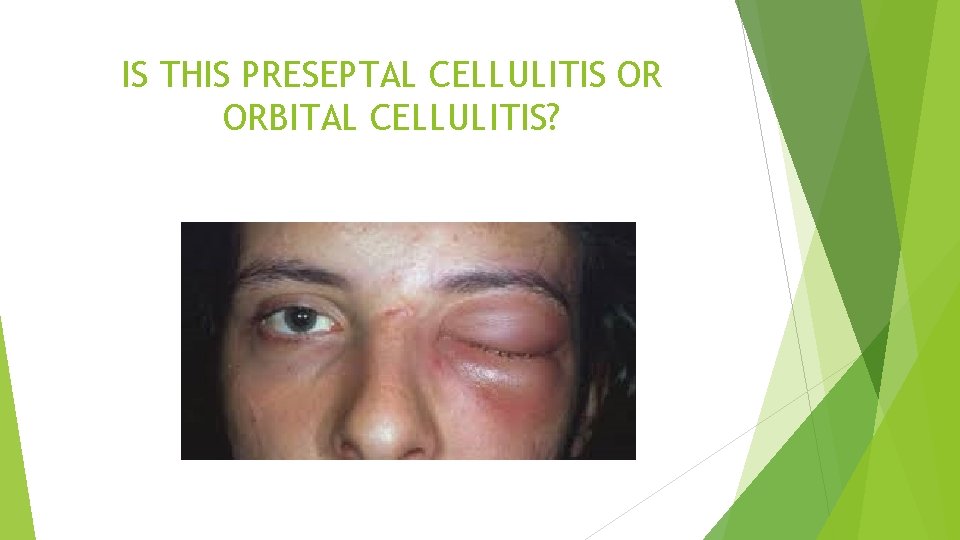
IS THIS PRESEPTAL CELLULITIS OR ORBITAL CELLULITIS?

ORBITAL CELLULITIS

ORBITAL CELLULITIS

ORBITAL CELLULITIS
CHALAZION Also called Meibomian cyst Granulomatous inflammatory lesion commonly in the upper eyelid Painless nodule within the tarsal plate Called marginal chalazion if on the anterior lid margin Usually in patients with meibomian gland disease or rosacea and may be multiple If secondary infected it is referred to an internal hordeolum.

CHALAZION UPPER EYE LID

CHALAZION LOWER EYELID

CHALAZION TREATMENT – Incision and drainage

HORDEOLUM INTERNAL
HORDEOLUM EXTERNAL Acute staphylococcal abscess of a lash follicle A tender swelling in the lid margin pointing anteriorly through the skin with a lash at the apex. Treatment involves topical antibiotics, hot compresses and epilation of the associated lash

HORDEOLUM EXTERNAL
BLEPHARITIS Chronic condition, very common cause of ocular discomfort and irritation. Usually bilateral and symmetrical, maybe anterior or posterior. Anterior Blepharitis sub-divided into Staphylococcal and Seborrhoeic. Hard scales and crusting mainly located around the bases of the lashes. DANDRUFF on the lashes Mild papillary conjunctivitis and chronic conjunctivitis Treatment– Lid hygiene, Antibiotics and weak steroids eye drops Treat associated dry eye
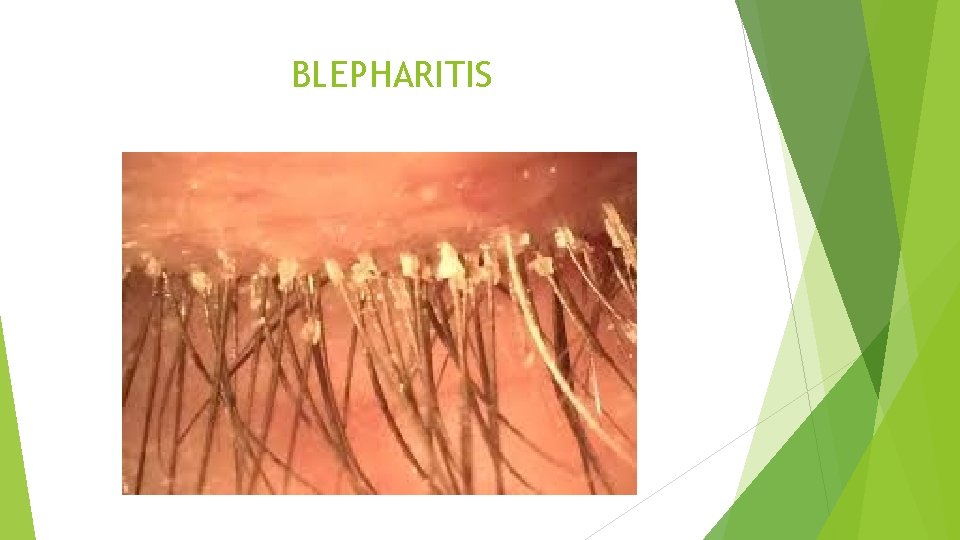
BLEPHARITIS
ALLERGIC DISORDERS Caused by pollen or by insect bites Sudden onset of bilateral pitting peri-orbital oedema, often accompanied by chemosis Treatment with systemic antihistamines

ALLERGIC DERMATITIS

ALLERGIC DERMATITIS
ATOPIC DERMATITIS Eczema, very common idiopathic condition Thickening, crusting and hyperpigmentation of the skin of the eyelid Can be associated with vernal disease in children and chronic keratoconjunctivitis in adults. Uncommon associations include keratoconus, pre-senile cataract and retinal detachment. Treatment – emollients to hydrate the skin and judicious use of mild topical steroids like hydrocortisone 1%.
ATOPIC DERMATITIS
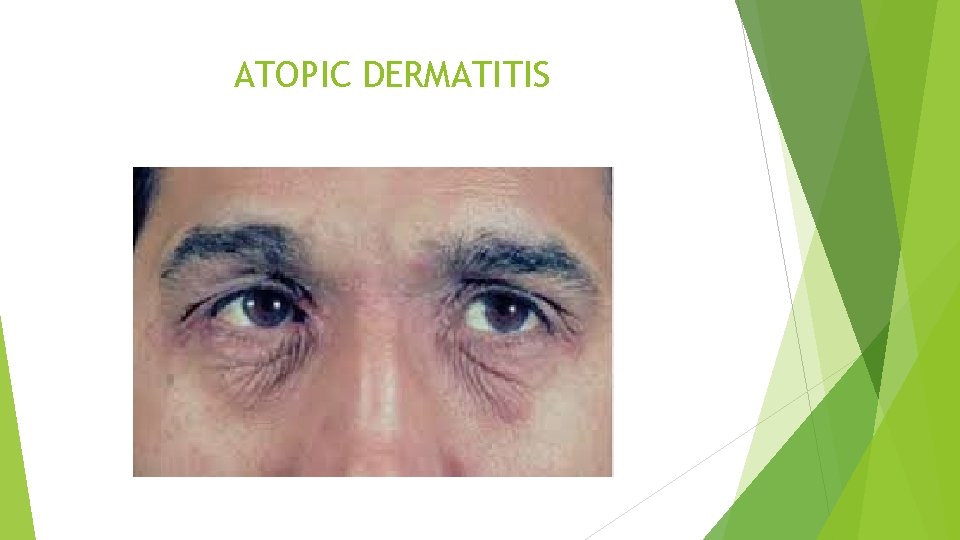
ATOPIC DERMATITIS

Dry Eye Syndrome Chronic lack of sufficient lubrication on the surface of the eye Consequences range from subtle but constant eye irritation to significant inflammation and even scarring of the conjunctiva and cornea. Prevalence range from 5% to as high as 50%. Symptoms: burning sensation, Itchy eye, aching sensations, heavy eyes, fatigued eyes, sore eyes, dryness sensation, red eyes, photophobia, blurred vision, foreign body sensation/grittiness Components of the normal tear film: oily/lipid, watery/aqueous and a mucouslike/mucin Contributing factors: computer use, contact lens wear, aging, menopause, indoor/outdoor environment, smoking, certain systemic diseases like diabetes, medications (antihistamines, antidepressants, antihypertensives, oral contraceptives, eyelid problems, refractive surgery Dietary factors: Omega-3, quercitin and other natural anti-inflammatories Treatment: address risk factors and life style modification, artificial tears and lubricants

DRY EYE SYNDROME TEAR DRAINAGE

DRY EYE SYNDROME MILD
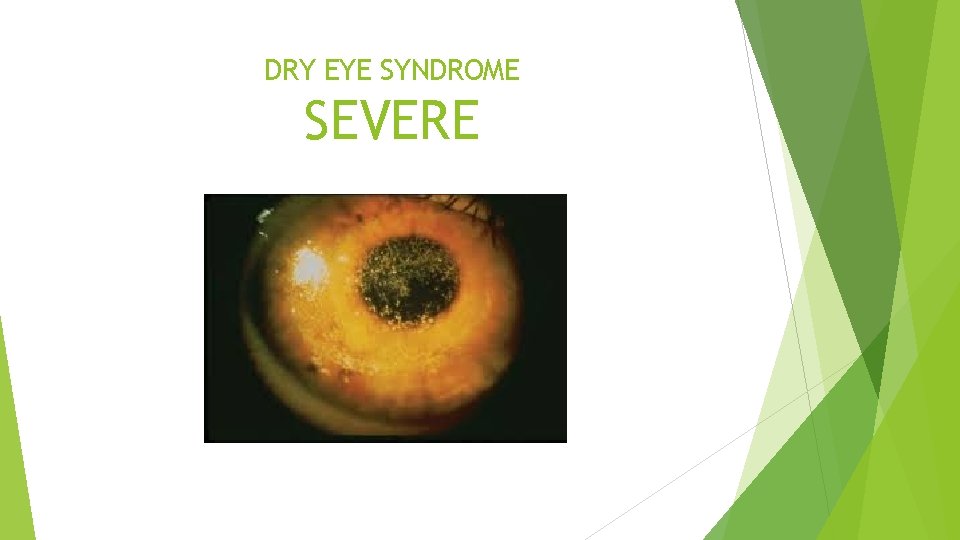
DRY EYE SYNDROME SEVERE

DRY EYE SYNDROME

MASCARA IN THE EYE
MASCARA IN THE EYE

MASCARA IN THE EYE

MASCARA IN THE EYE CONJUNCTIVA
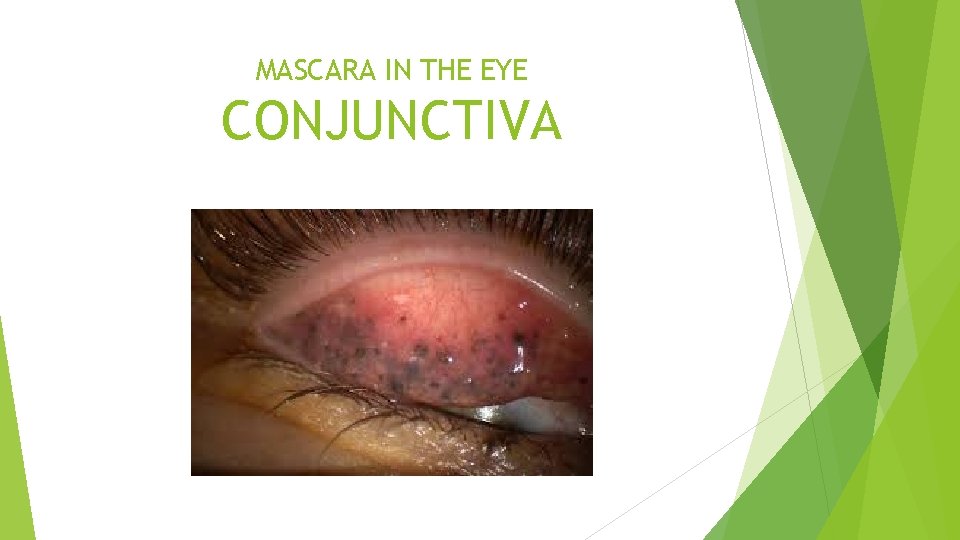
MASCARA IN THE EYE CONJUNCTIVA
ACUTE BACTERIAL CONJUNCTIVITIS Common and usually self-limiting condition caused by direct eye contact with infected secretions Most common isolates are S. pneumoniae, S. aureus, H. influenza and Moraxella catarrhalis. Minority of cases, severe caused by sexually transmitted organism Neisseria gonorrhoeae. May be acute onset of redness, grittiness, burning and discharge to hyperacute purulent discharge which may signify GONOCCOCAL or MENINGOCCOCAL CONJUNCTIVITIS Peripheral corneal ulceration may occur in gonococcal and meningococcal infection.
ACUTE BACTERIAL CONJUNCTIVITS TREATMENT 60% resolve within 5 days without treatment Topical antibiotics q. i. d. for up to 1 week are frequently administered to speed recovery and prevent re-infection. Gonococcal, H. influenza, Meningococcal require obligate systemic antibiotics

BACTERIAL CONJUNCTIVITIS

GONOCOCCAL CONJUNCTIVITIS
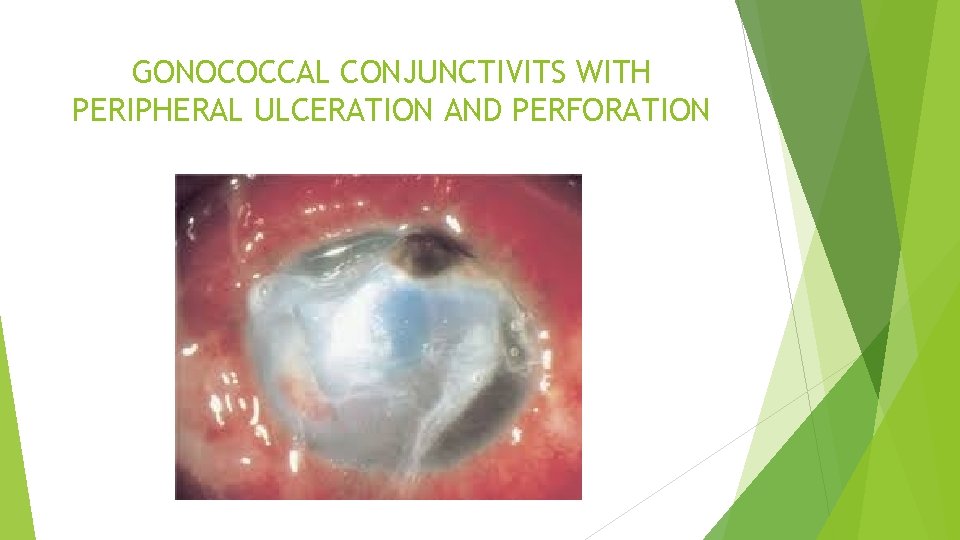
GONOCOCCAL CONJUNCTIVITS WITH PERIPHERAL ULCERATION AND PERFORATION
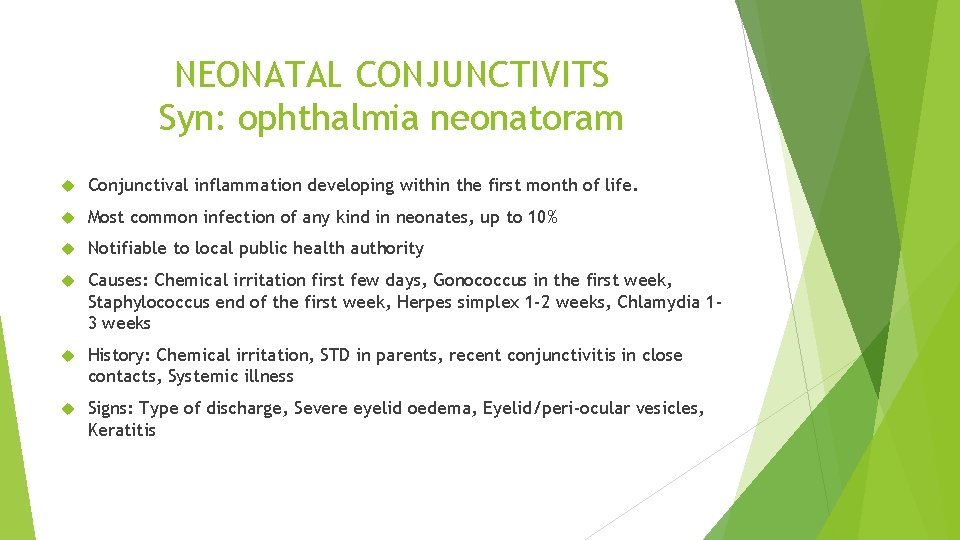
NEONATAL CONJUNCTIVITS Syn: ophthalmia neonatoram Conjunctival inflammation developing within the first month of life. Most common infection of any kind in neonates, up to 10% Notifiable to local public health authority Causes: Chemical irritation first few days, Gonococcus in the first week, Staphylococcus end of the first week, Herpes simplex 1 -2 weeks, Chlamydia 13 weeks History: Chemical irritation, STD in parents, recent conjunctivitis in close contacts, Systemic illness Signs: Type of discharge, Severe eyelid oedema, Eyelid/peri-ocular vesicles, Keratitis
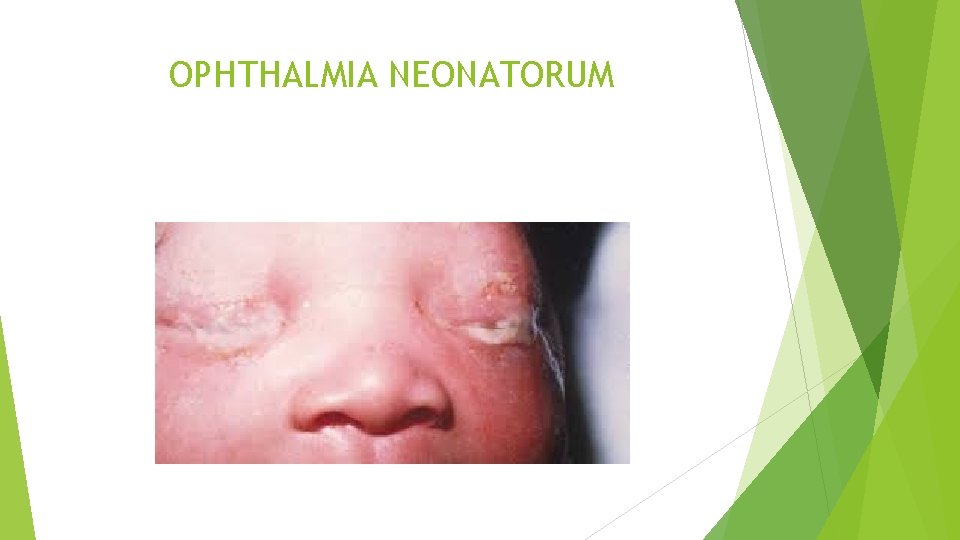
OPHTHALMIA NEONATORUM

TREATMENT Prophylaxis: Povidine-iodine 2. 5%, Erythromycin 0. 5%, Silver nitrate 1% Mild Conjunctivitis: Topical antibiotic like chloramphenicol Moderate to severe cases: Should be investigated Severe conjunctivitis or when systemic illness is suspected requires hospital admission Genitourinary specialist referral for the mother and her sexual contacts is important when a STI is diagnosed and the neonate should be screened for other STI’s
ADENOVIRAL CONJUNCTIVITIS Highly contagious disease and viral particles have the ability to survive on dry surfaces for weeks Very Viral shedding may occur for may days before clinical features became apparent Infection may be sporadic or it may occur in epidemics in workplaces including hospitals, doctor’s consulting rooms and schools Transmission is generally by contact with respiratory or ocular secretions NB

CLINICAL PRESENTATION History of close contact Clinical spectrum varies from mild sub-clinical disease to severe inflammation with significant mobility. Eyelid oedema and tender pre-auricular lymphadenopathy Prominent conjunctival hyperaemia and follicles Conjunctival haemorrhages, Chemosis, Pseudomembranes Keratitis Anterior uveitis is uncommon

ADENOVIRAL CONJUNCTIVITUS

ADENOVIRUS CONJUNCTIVITIS LID OEDEMA
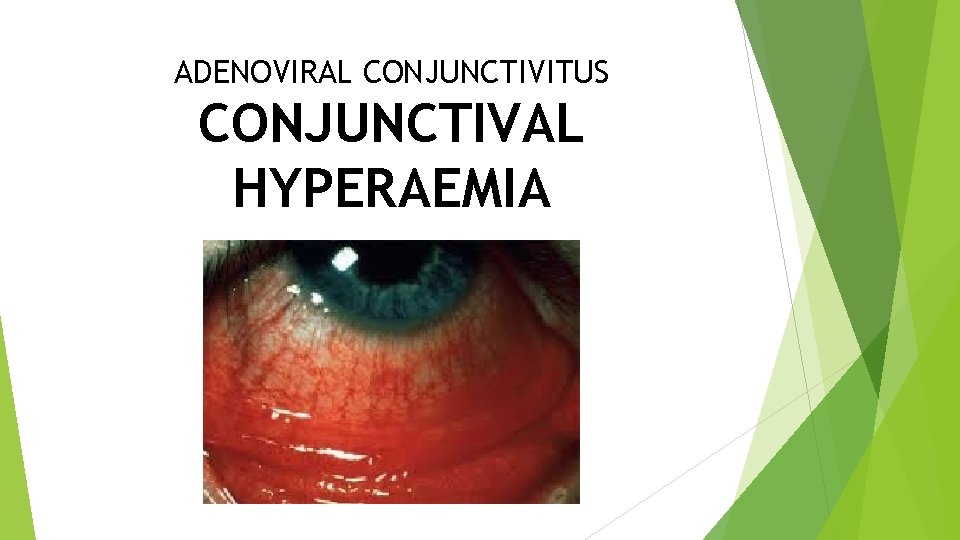
ADENOVIRAL CONJUNCTIVITUS CONJUNCTIVAL HYPERAEMIA
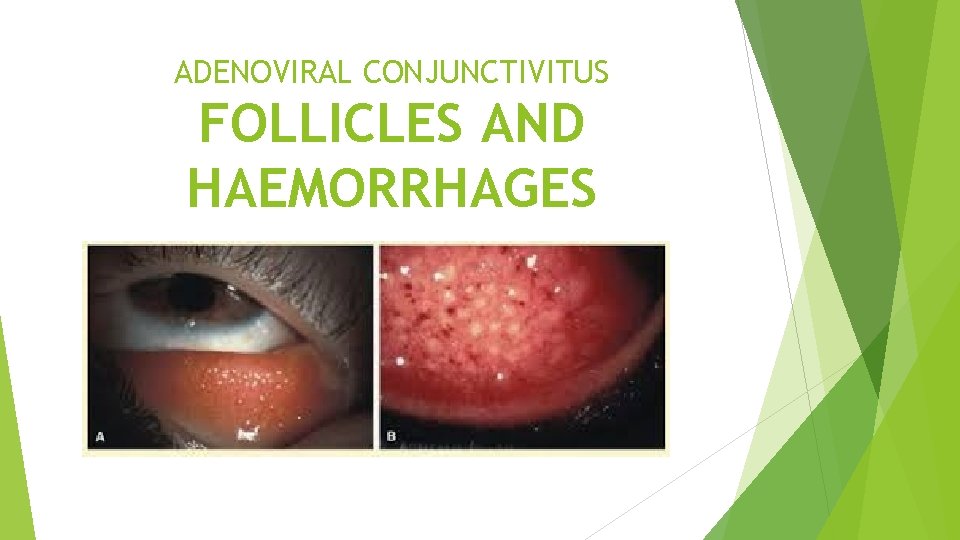
ADENOVIRAL CONJUNCTIVITUS FOLLICLES AND HAEMORRHAGES

ADENOVIRAL CONJUNCTIVITUS PSEUDOMEMBRANES

ADENOVIRAL CONJUNCTIVITUS KERATITIS
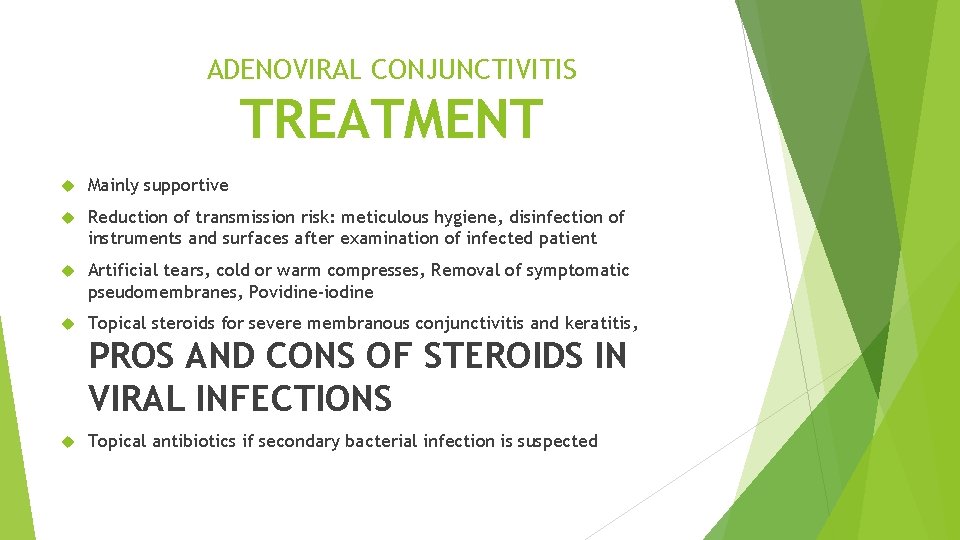
ADENOVIRAL CONJUNCTIVITIS TREATMENT Mainly supportive Reduction of transmission risk: meticulous hygiene, disinfection of instruments and surfaces after examination of infected patient Artificial tears, cold or warm compresses, Removal of symptomatic pseudomembranes, Povidine-iodine Topical steroids for severe membranous conjunctivitis and keratitis, PROS AND CONS OF STEROIDS IN VIRAL INFECTIONS Topical antibiotics if secondary bacterial infection is suspected

NB TO DOCTORS Incubation period of the virus is 10 -14 days Once you have the virus, you will shed it for up to 14 days potentially infecting others May have to book off-sick for up to 2 weeks
VERNAL KERATOCONJUNCTIVITIS syn VERNAL CATARRH Probably most common eye condition in general practice Recurrent bilateral disorder in which both Ig. E- and cell-mediated immune mechanisms play important roles Onset generally from 2 years, mean 7 years, common in males Can involve upper tarsal conjunctiva (Palpebral VKC) leading to corneal disease, or limbal disease Mixed VKC has features of both palpebral and limbal disease
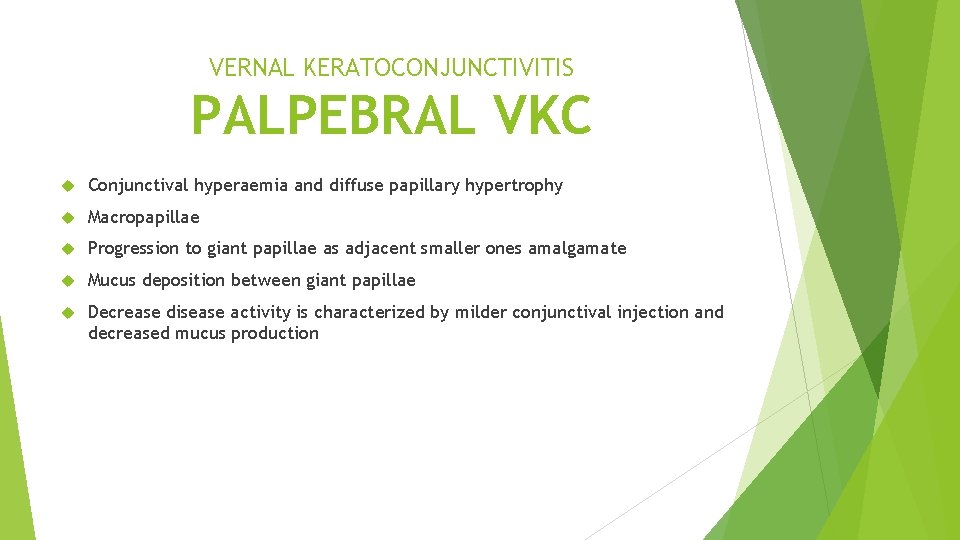
VERNAL KERATOCONJUNCTIVITIS PALPEBRAL VKC Conjunctival hyperaemia and diffuse papillary hypertrophy Macropapillae Progression to giant papillae as adjacent smaller ones amalgamate Mucus deposition between giant papillae Decrease disease activity is characterized by milder conjunctival injection and decreased mucus production
VERNAL KERATOCONJUNCTIVITIS LIMBAL DISEASE Gelatinous limbal papillae with transient apically-located white cellular collections

VERNAL KERATOCONJUNCTIVITIS KERATOPATHY Superior punctate epithelial erosions Epithelial macroerosions Plaques and shield’ ulcers Subepithelial scars Pseudogerontoxon resembles arcus senilis Corneal vascularization Keratoconus probably due to chronic rubbing of eyes Herpes simplex keratitis is more common than average? ? ? ?
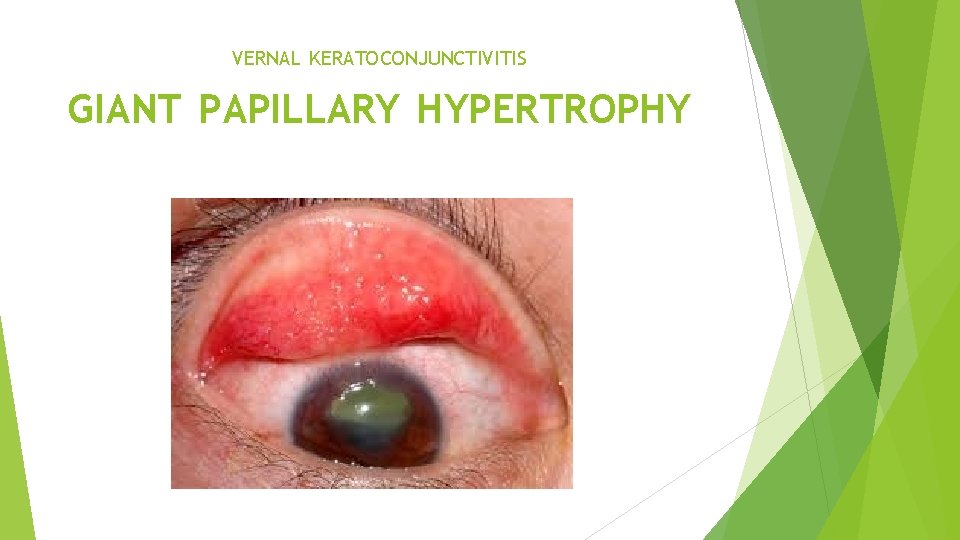
VERNAL KERATOCONJUNCTIVITIS GIANT PAPILLARY HYPERTROPHY

VERNAL KERATOCONJUNCTIVITIS TECHNIQUE OF UPPER LID EVERSION TO DEMONSTRATE GIANT PAPILLAE
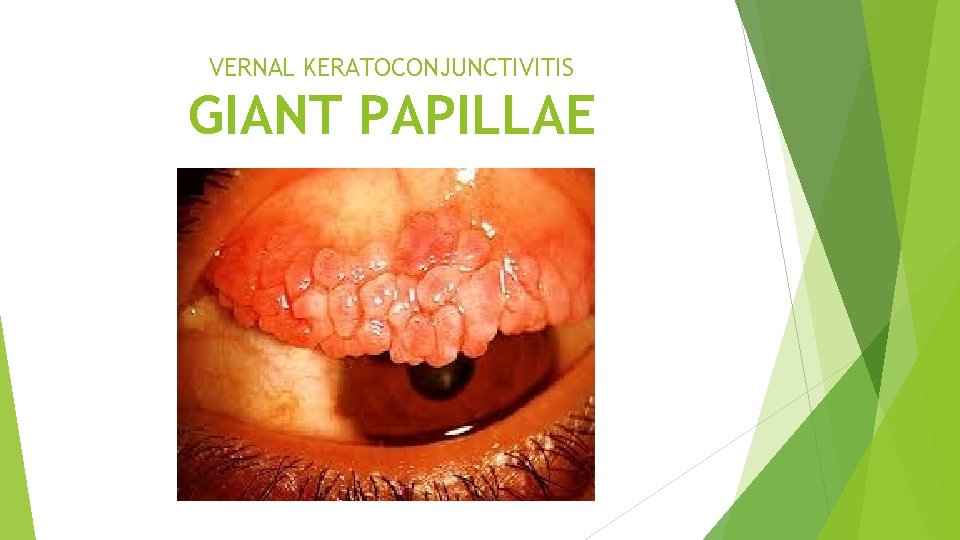
VERNAL KERATOCONJUNCTIVITIS GIANT PAPILLAE
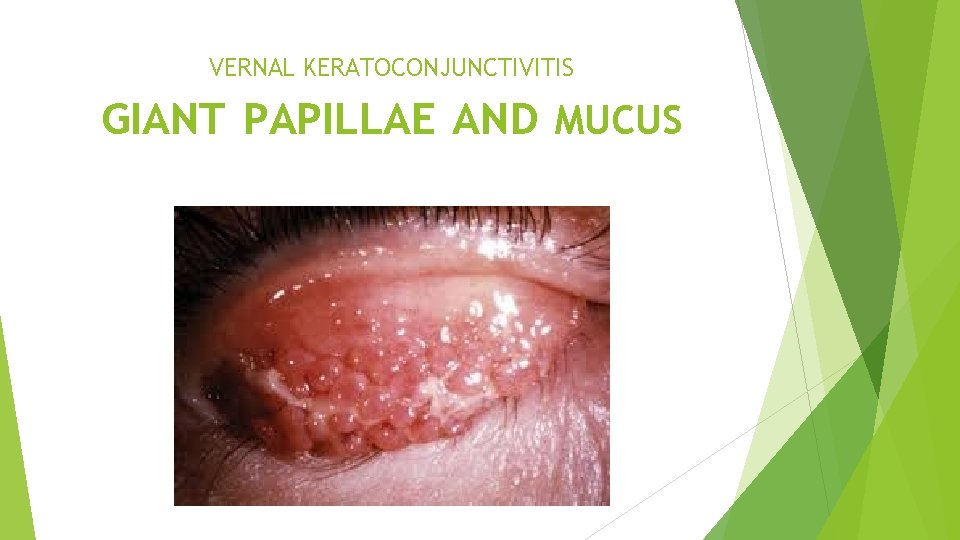
VERNAL KERATOCONJUNCTIVITIS GIANT PAPILLAE AND MUCUS
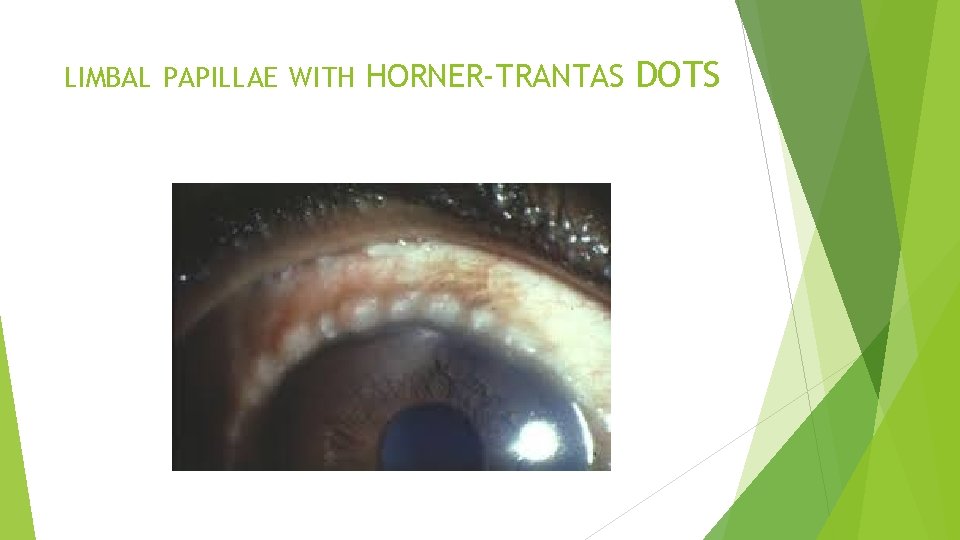
LIMBAL PAPILLAE WITH HORNER-TRANTAS DOTS
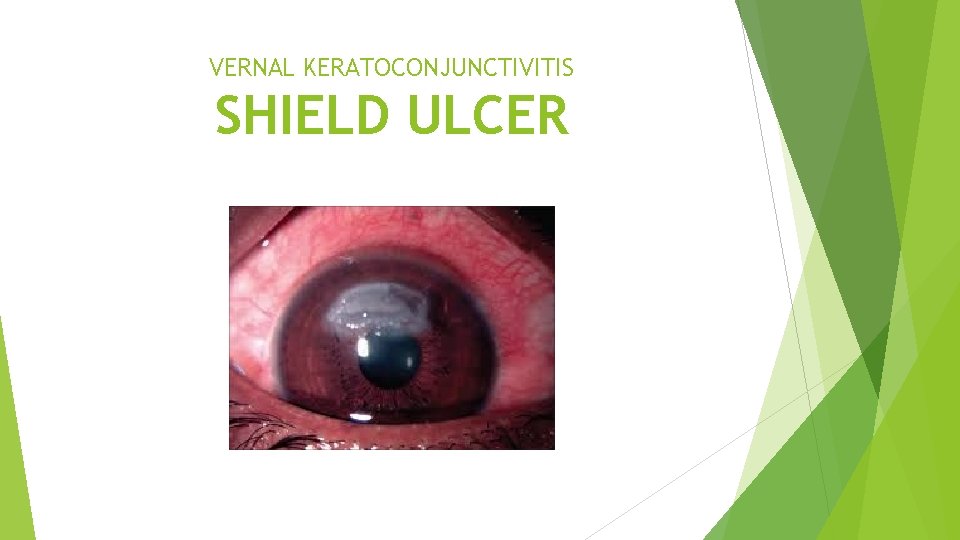
VERNAL KERATOCONJUNCTIVITIS SHIELD ULCER

VERNAL KERATOCONJUNCTIVITIS PLAQUE FORMATION IN THE LEFT EYE
VERNAL KERATOCONJUNCTIVITIS TREATMENT Mast cell stabilizers Antihistamines Steroids for severe exacerbations of conjunctivitis and significant keratopathy Immune modulators eg. Ciclosporin 0. 05% if steroids are ineffective or poorly tolerated Tacrolimus 0. 03% ointment is an option to Ciclosporin Acetylcysteine a mucolytic agent Antibiotics if there is associated bacterial infection
VERNAL KERATOCONJUNCTIVITIS SURGERY Bandage contact lenses for persistent epithelial defects Superficial keratectomy to remove plaques or debride shield’ ulcers and allow epithelialization Surface maintenance-restoration surgery such as amniotic membrane overlay grafting or lamellar keratoplasty Eyelid procedures such as botulinum toxin-induced ptosis or lateral tarsorrhaphy may be required for severe persistent epithelial defects or ulceration. Gluing may be appropriate for punched-out corneal perforations
PTERYGIUM A triangular fibrovascular subepithelial ingrowth of the degenerative bulbar conjunctival tissue over the limbus onto the cornea. Patients living in hot climates may represent a response to ultraviolet exposure and possibly other factors such as chronic dryness. Histologically shows elastotic degenerative changes in vascularized subepithelial stromal collagen Can be graded into Type 1, Type 2 and Type 3 depending on corneal encroachment. Treatment: Pterygium excision combined with conjunctiva autografting to reduce recurrence.
PINGUECULUM Extremely common, innocuous usually bilateral A yellow-white mound or aggregation of smaller mounds on the bulbar conjunctiva adjacent to the limbus. Asymptomatic ‘elastotic’ degeneration of the collagen fibres of conjuntival stroma. Actinic damage similar to the aetiology of pterygium Treatment is usually unnecessary because growth is very slow or absent. Excision is performed for cosmetic reasons or if a lesion is causing irritation Occasionally may become inflamed and require a short course of a weak steroid such as fluorometholone
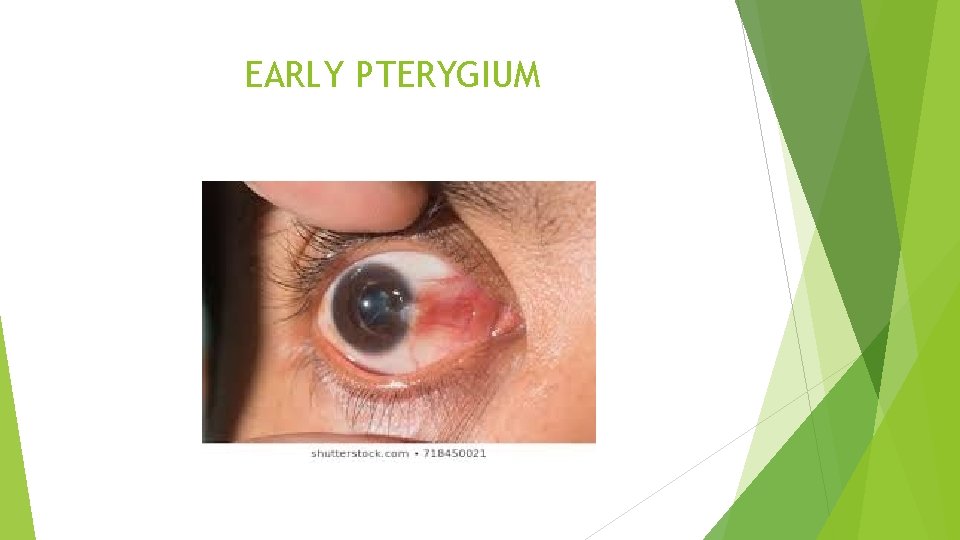
EARLY PTERYGIUM

ADVANCED PTERYGIUM
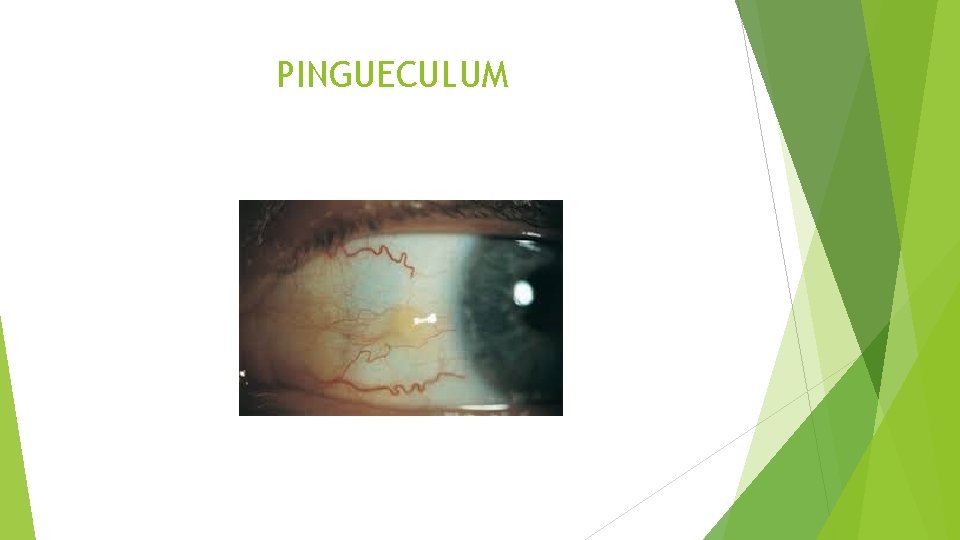
PINGUECULUM

INFLAMED PINGUECULUM
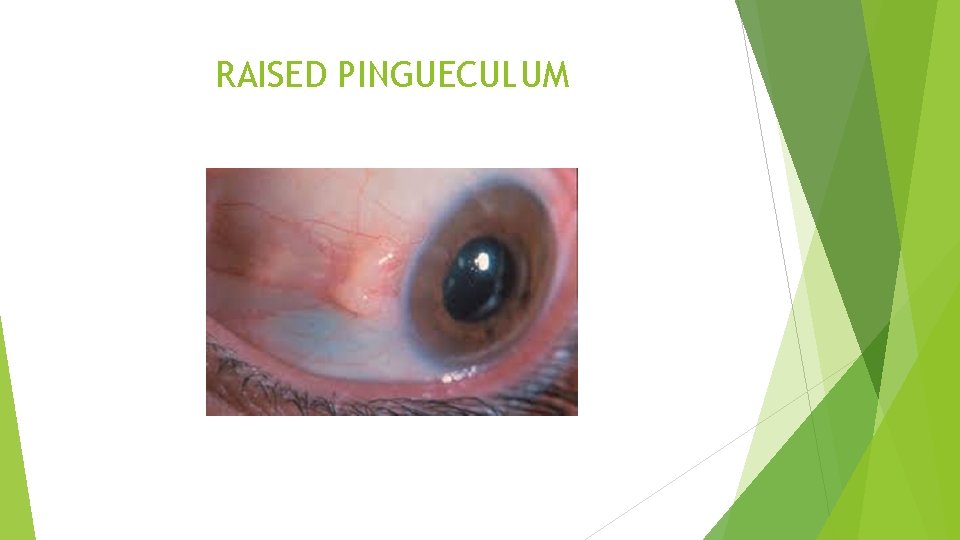
RAISED PINGUECULUM
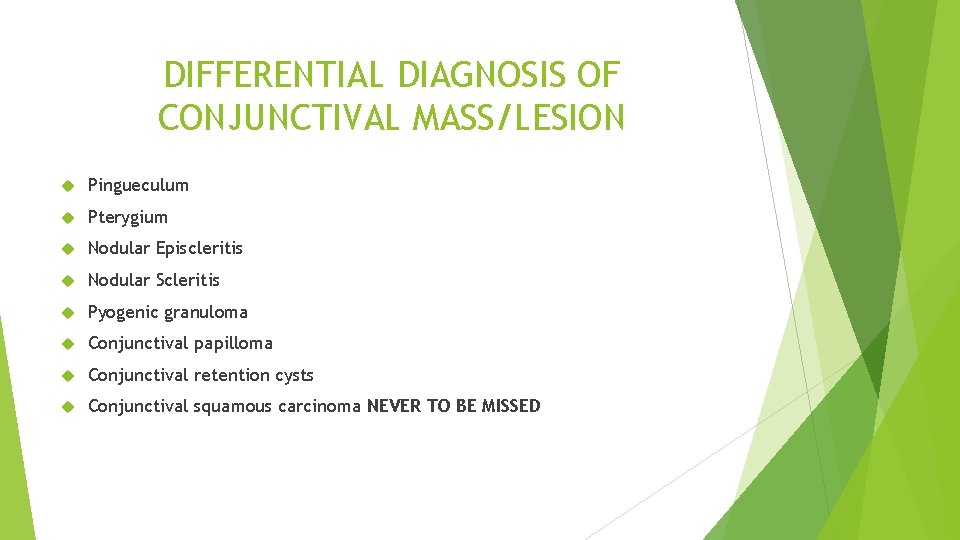
DIFFERENTIAL DIAGNOSIS OF CONJUNCTIVAL MASS/LESION Pingueculum Pterygium Nodular Episcleritis Nodular Scleritis Pyogenic granuloma Conjunctival papilloma Conjunctival retention cysts Conjunctival squamous carcinoma NEVER TO BE MISSED

NODULAR EPISCLERITIS

PYOGENIC GRANULOMA OF THE CONJUNCTIVA
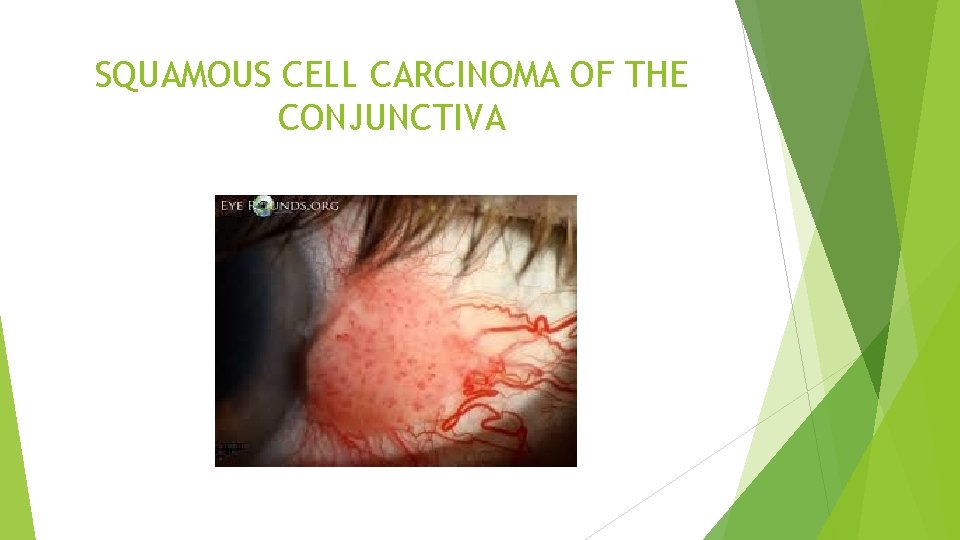
SQUAMOUS CELL CARCINOMA OF THE CONJUNCTIVA
THIS CONDITIONS MIMIC EACH OTHER HISTORY AND EXAMINATION PLUS HIGH INDEX OF SUSPICION IS KEY

BACTERIAL KERATITIS

BACTERIAL KERATITIS
BACTERIAL KERATITIS Ophthalmic emergency Not to be missed as it is potential litigator
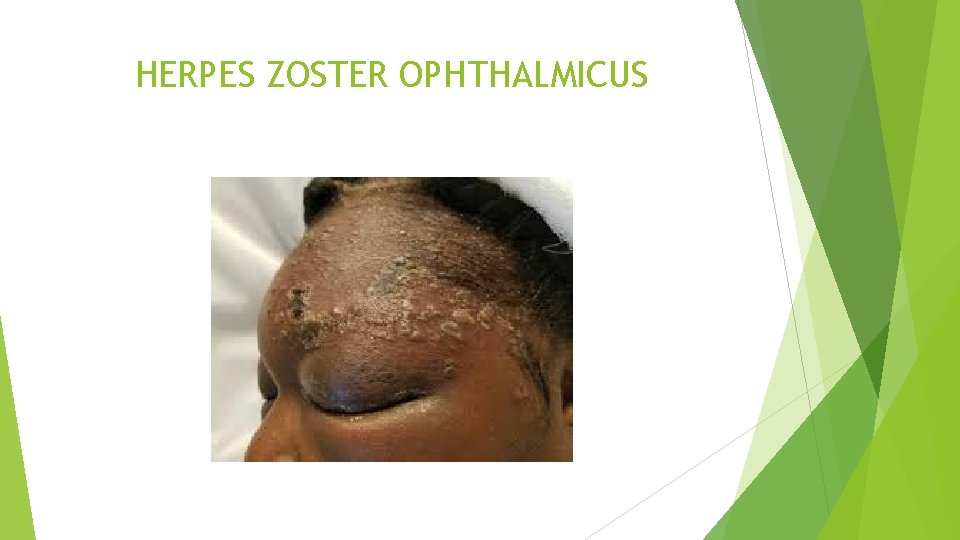
HERPES ZOSTER OPHTHALMICUS
KERATOCONUS Is a progressive disorder in which the cornea assumes a conical shape secondary to stromal thinning and protrusion Presentation is typically during puberty with unilateral impairment of vision due to progressive myopia and astigmatism Treatment initially glasses, as it progresses hard contact lenses Hallmark of treatment these days is Corneal collagen cross-linking Corneal graft surgery / Keratoplasty reserved for advanced cases
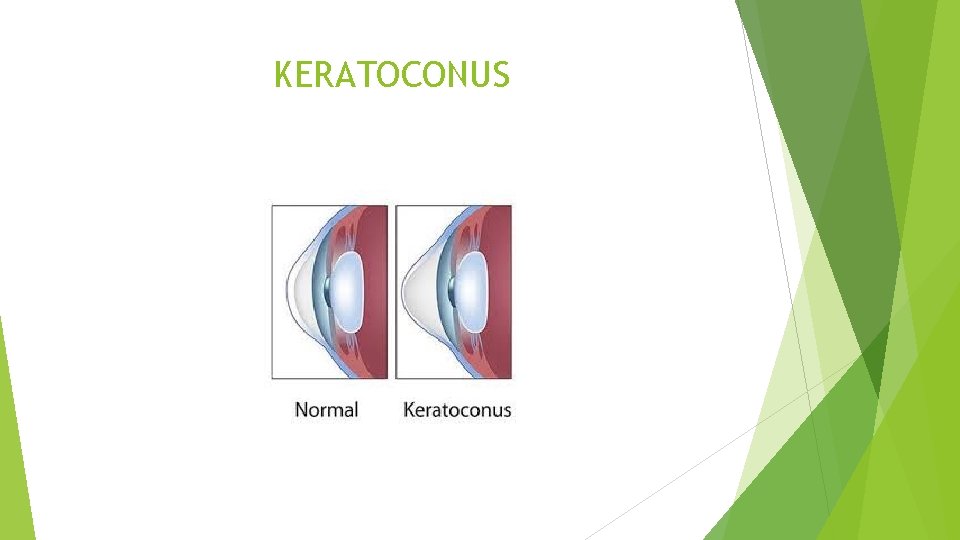
KERATOCONUS

KERATOCONUS
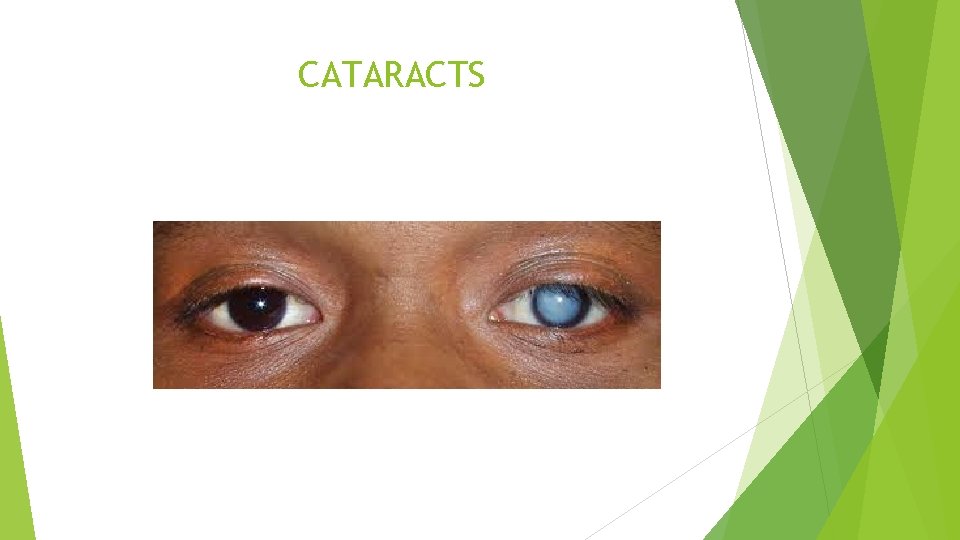
CATARACTS
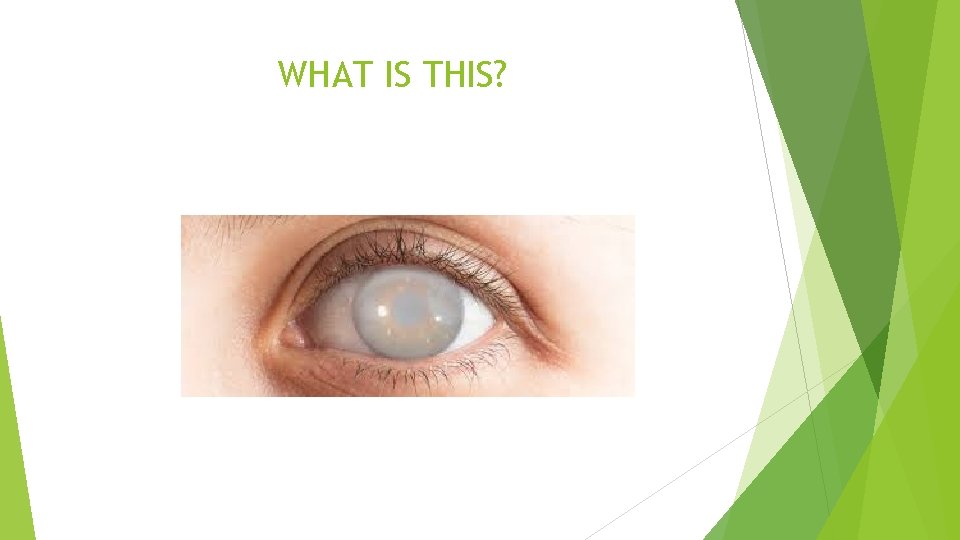
WHAT IS THIS?
PLEASE DO REMEMBER THAT OPHTHALMOLOGY IS NOT CATARACTS
GLAUCOMA Raised intraocular pressure leading to … Optic disc cupping Characteristic visual field changes

GLAUCOMATOUS OPTIC DISC
UVEITIS Acute anterior uveitis is the most common form of uveitis accounting for 75% of the cases Characterized by onset of unilateral pain, photophobia, redness which may be associated with lacrimation Always think of it when you see a red eye Visual acuity is usually good at presentation but it is decreased later
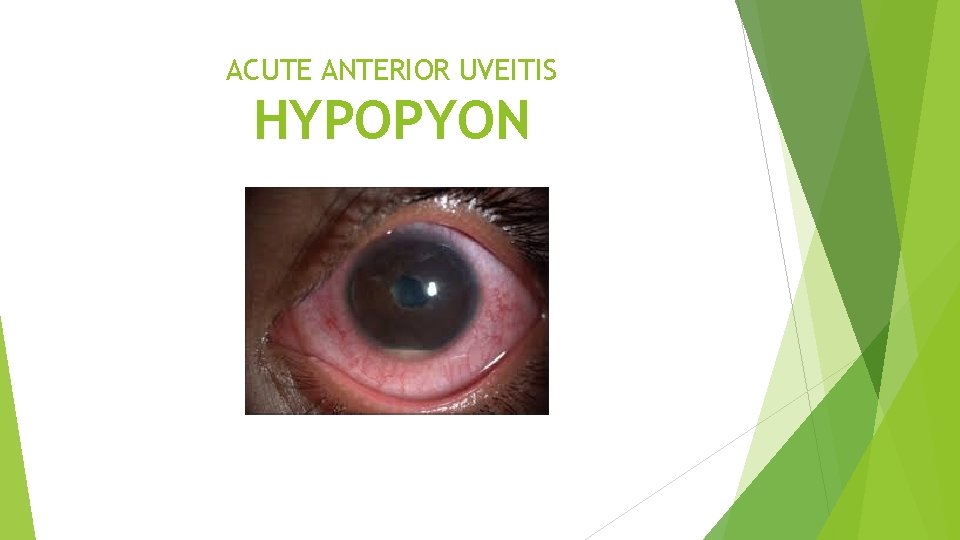
ACUTE ANTERIOR UVEITIS HYPOPYON

ACUTE ANTERIOR UVEITIS MUTTON-FAT KP

ACUTE ANTERIOR UVEITIS POSTERIOR SYNECHIAE
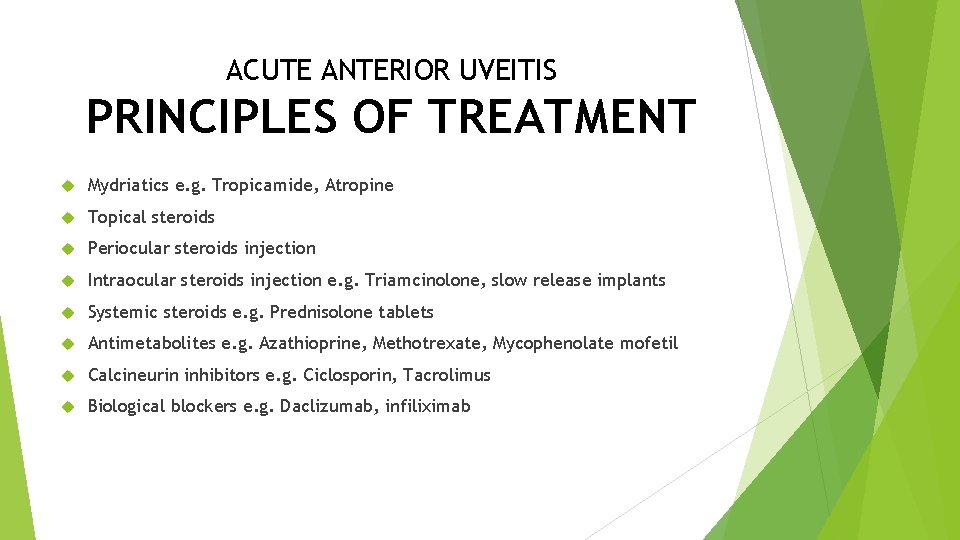
ACUTE ANTERIOR UVEITIS PRINCIPLES OF TREATMENT Mydriatics e. g. Tropicamide, Atropine Topical steroids Periocular steroids injection Intraocular steroids injection e. g. Triamcinolone, slow release implants Systemic steroids e. g. Prednisolone tablets Antimetabolites e. g. Azathioprine, Methotrexate, Mycophenolate mofetil Calcineurin inhibitors e. g. Ciclosporin, Tacrolimus Biological blockers e. g. Daclizumab, infiliximab
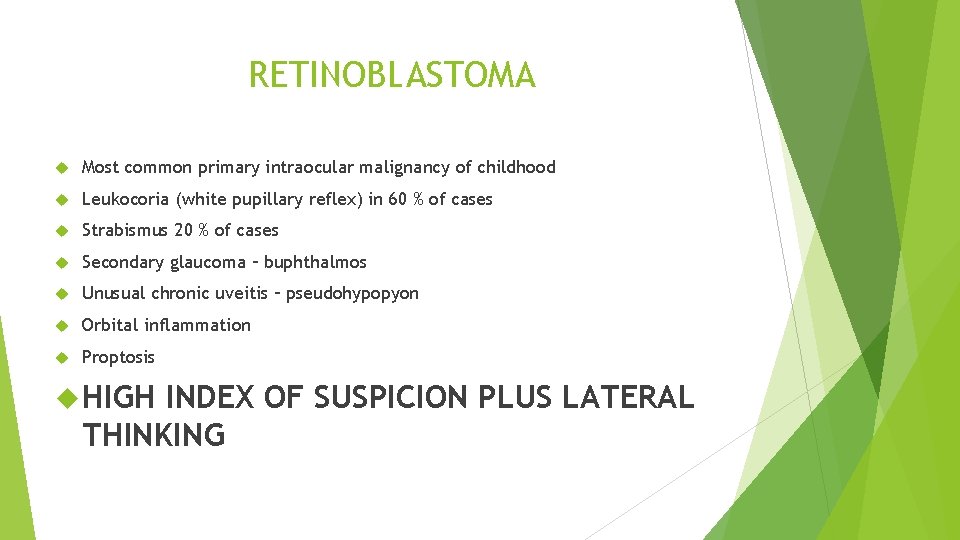
RETINOBLASTOMA Most common primary intraocular malignancy of childhood Leukocoria (white pupillary reflex) in 60 % of cases Strabismus 20 % of cases Secondary glaucoma – buphthalmos Unusual chronic uveitis – pseudohypopyon Orbital inflammation Proptosis HIGH INDEX OF SUSPICION PLUS LATERAL THINKING
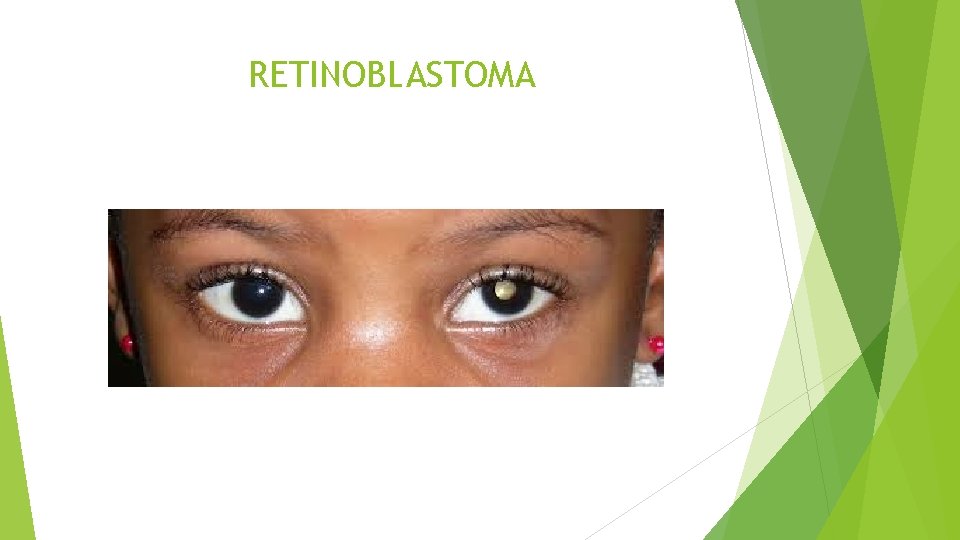
RETINOBLASTOMA
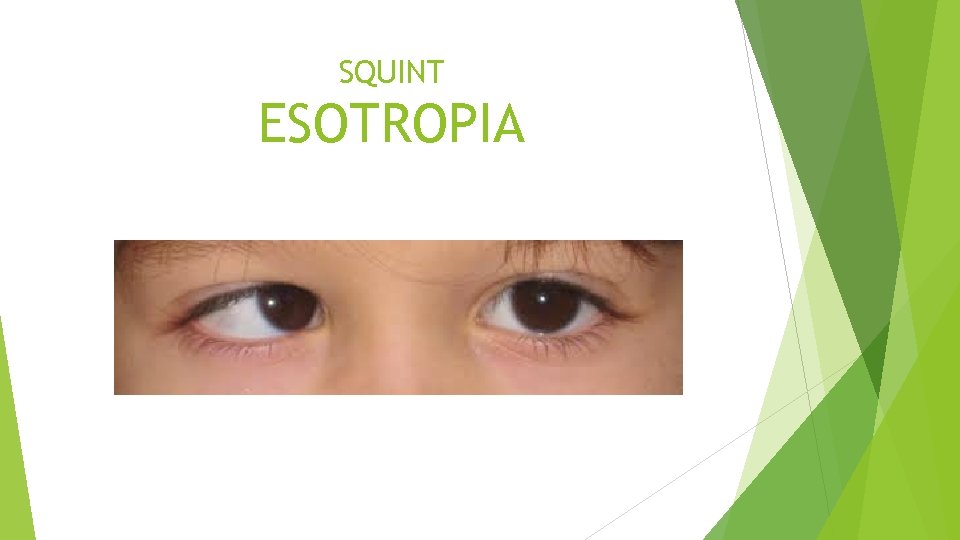
SQUINT ESOTROPIA
DIABETES Orbit: Orbital mucormycosis – Very rare Lids: Ptosis – Third nerve palsy, Poliosis Ocular surface: Episcleritis, Scleritis Cornea: Dry eyes, decrease sensation, Epithelial peeling Anterior Chamber: Open angle glaucoma, Neovascular glaucoma Lens: Cataracts Vitreous: Posterior vitreous detachment, Vitreous haemorrhage Retina: Retinopathy Neuro-ophthalmic manifestations: Papillitis/optic disc swelling, Third nerve palsy, Six nerve palsy
HYPERTENSION Dry eye syndrome: Due to side effects of medication Retinal venous occlusive disease: Branch retinal vein occlusion, Central retinal vein occlusion Hypertensive disease: Retinopathy, Choroidopathy Neuro-ophthalmic manifestations: Malignant Hypertension Third nerve palsy, Six nerve palsy, rarely Fourth nerve palsy
THIRD NERVE PALSY Metabolic versus Surgical, Pupil sparing versus Pupil involving Ptosis The eye will not look When the patient attempts to look down, there will be Pupil may be unaffected (metabolic condition) or affected (unreactive to light and semi dilated, surgical condition) In a primary position the affected eye will be turned outwards and slightly down wards due to unopposed abducent (6 th nerve) and trochlear (4 th nerve) UP nor IN nor DOWN intorsion of the eye
THIRD NERVE PALSY If the pupil is involved, acute emergency. This is suggestive of an aneurysm Uninvolved pupil is suggestive of a medical condition, commonly diabetes and hypertension BEWARE THIRD NERVE
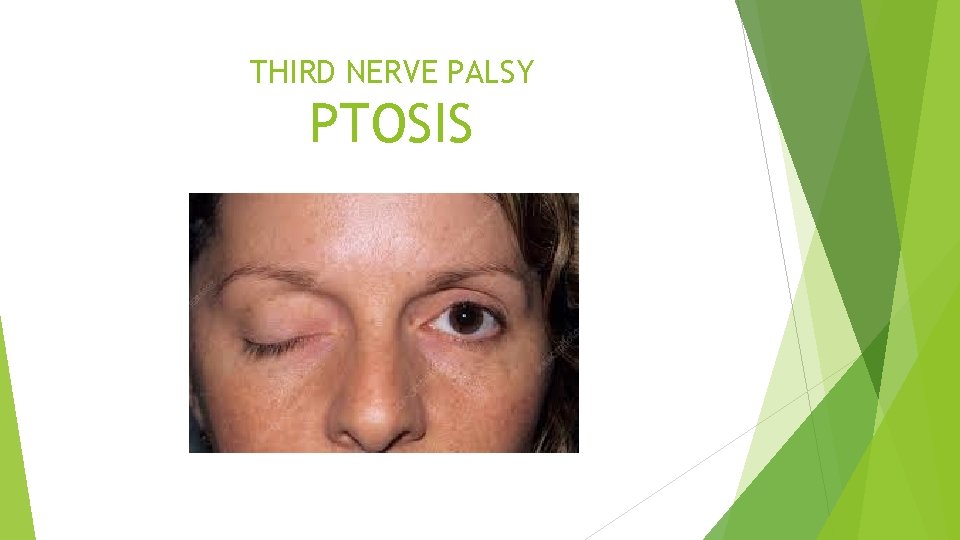
THIRD NERVE PALSY PTOSIS
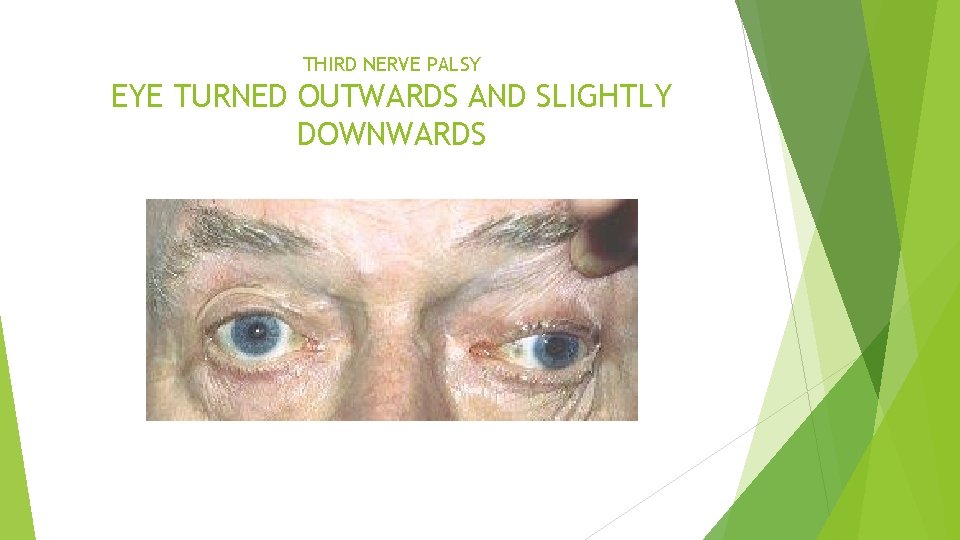
THIRD NERVE PALSY EYE TURNED OUTWARDS AND SLIGHTLY DOWNWARDS

THIRD NERVE PALSY CANNOT LOOK UP
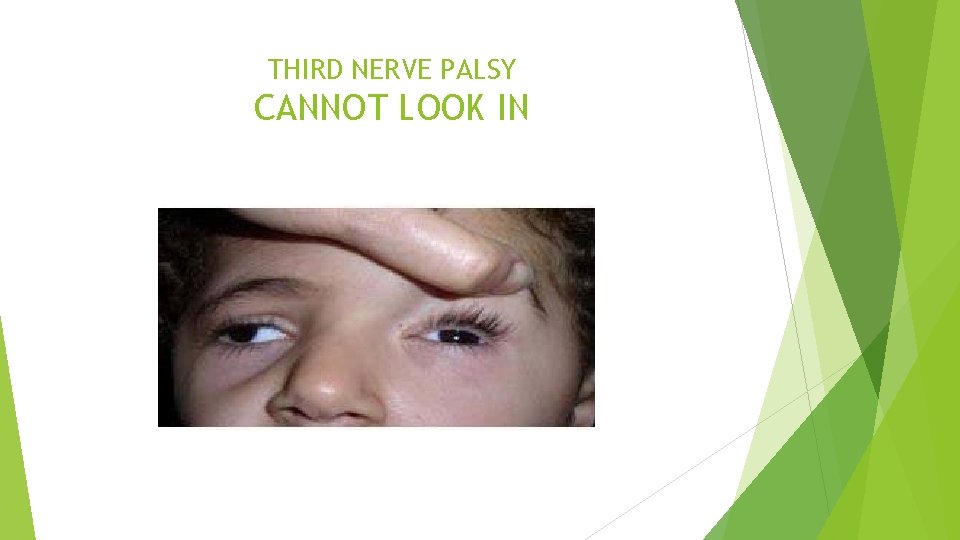
THIRD NERVE PALSY CANNOT LOOK IN
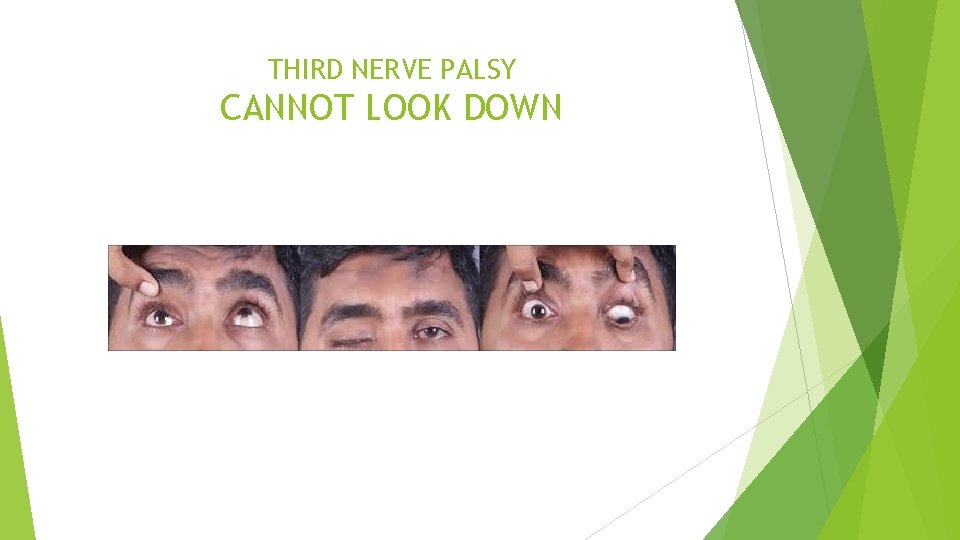
THIRD NERVE PALSY CANNOT LOOK DOWN
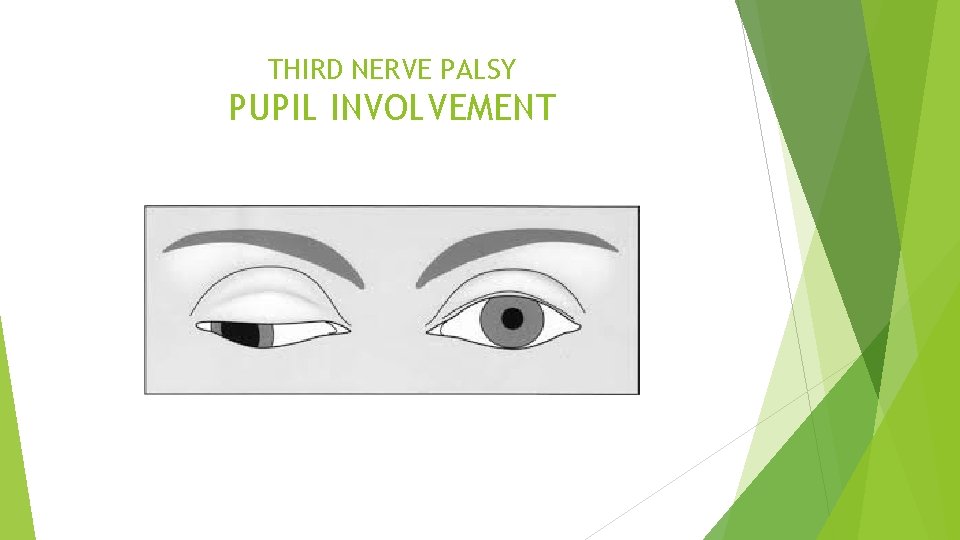
THIRD NERVE PALSY PUPIL INVOLVEMENT
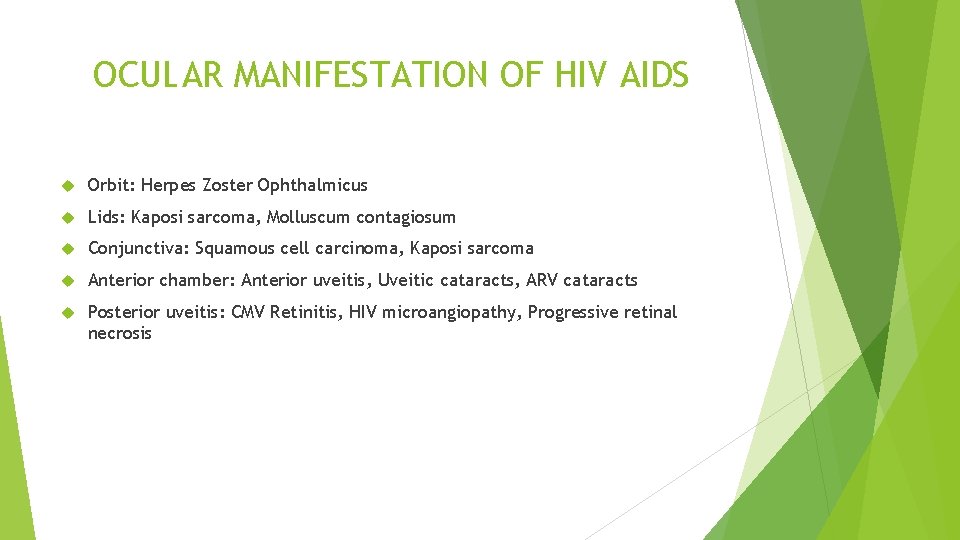
OCULAR MANIFESTATION OF HIV AIDS Orbit: Herpes Zoster Ophthalmicus Lids: Kaposi sarcoma, Molluscum contagiosum Conjunctiva: Squamous cell carcinoma, Kaposi sarcoma Anterior chamber: Anterior uveitis, Uveitic cataracts, ARV cataracts Posterior uveitis: CMV Retinitis, HIV microangiopathy, Progressive retinal necrosis
TO BE CONTINUED …
- Slides: 120