Common Medication Errors in Pediatric Patients Presentation Pourmirzaee

- Slides: 43
Common Medication Errors in Pediatric Patients Presentation: Pourmirzaee ( Md)
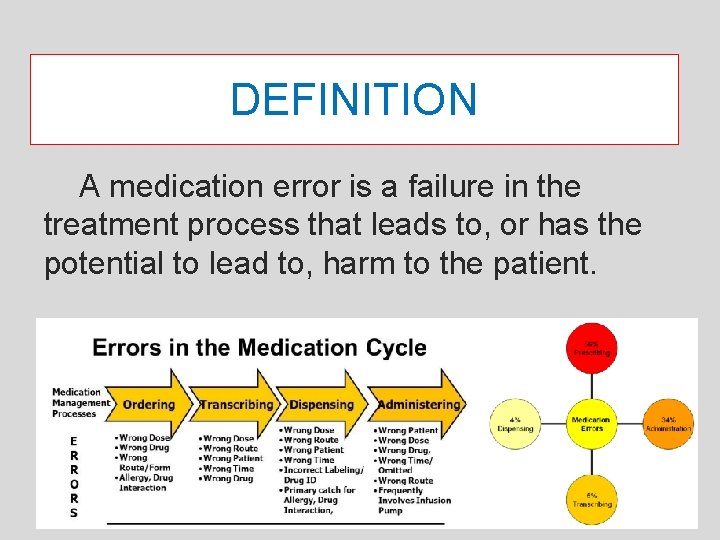
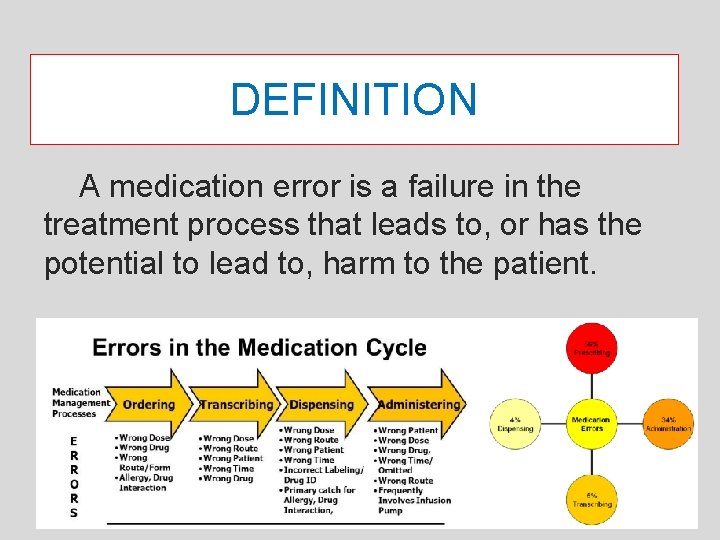
DEFINITION A medication error is a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient.
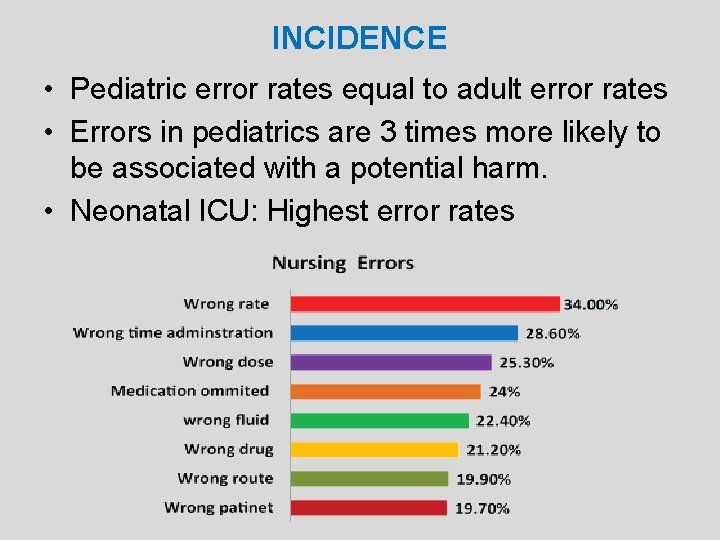
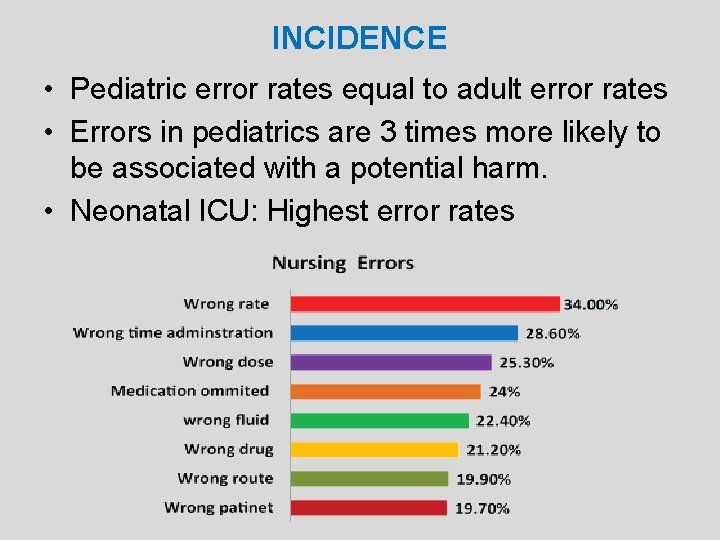
INCIDENCE • Pediatric error rates equal to adult error rates • Errors in pediatrics are 3 times more likely to be associated with a potential harm. • Neonatal ICU: Highest error rates
Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems
Pediatric and Neonatal Pharmacokinetics • One size doesn’t fit all – Preterm neonates (<36 weeks’ gestation) – Full-term neonates (birth to 30 days) – Infants (1– 12 months) – Toddlers (1– 4 years) – Children (5– 12 years) – Adolescents (>12 years)
Pediatric and Neonatal Pharmacokinetics • Do not use the terms interchangeably • Discuss patients in terms of age and weight to provide more accurate kinetic profile • Difference between adolescent and preterm neonate drug dose: potentially 100 -fold
Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems
Lack of Pediatric Formulations • May lead to: – Crushing tablets – Opening capsules and adding to food or beverage – Utilizing IV formulations for oral use – Using ophthalmic preparations in the ear – Giving IV anticonvulsants rectally

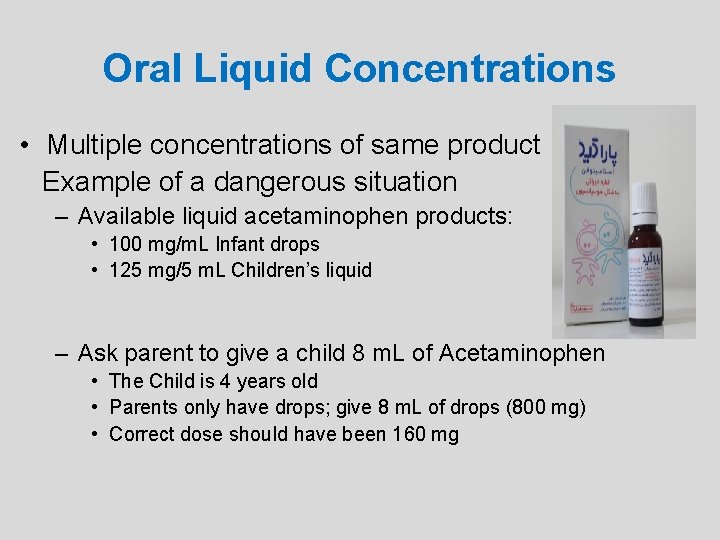
Oral Liquid Concentrations • Multiple concentrations of same product Example of a dangerous situation – Available liquid acetaminophen products: • 100 mg/m. L Infant drops • 125 mg/5 m. L Children’s liquid – Ask parent to give a child 8 m. L of Acetaminophen • The Child is 4 years old • Parents only have drops; give 8 m. L of drops (800 mg) • Correct dose should have been 160 mg
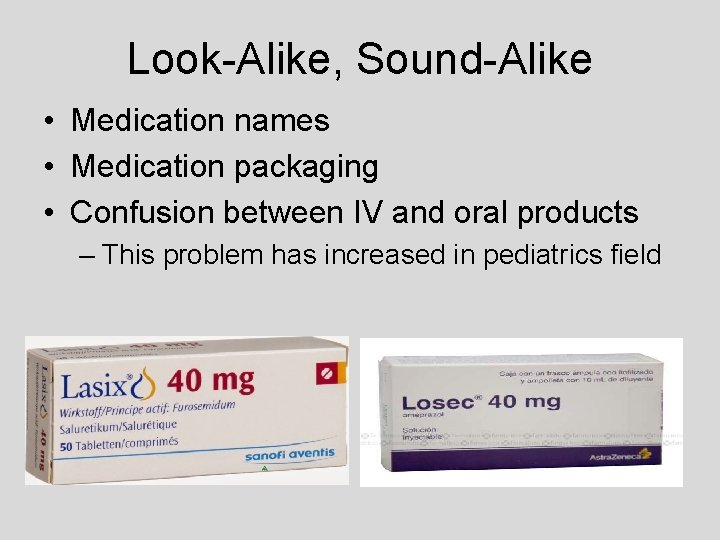
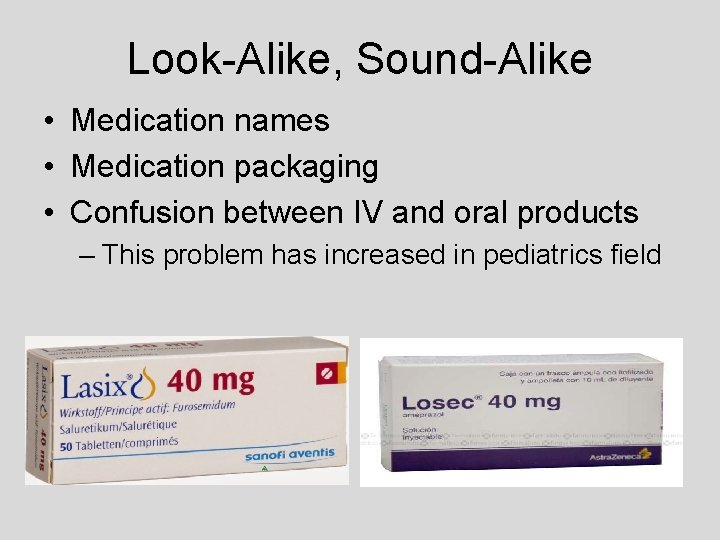
Look-Alike, Sound-Alike • Medication names • Medication packaging • Confusion between IV and oral products – This problem has increased in pediatrics field
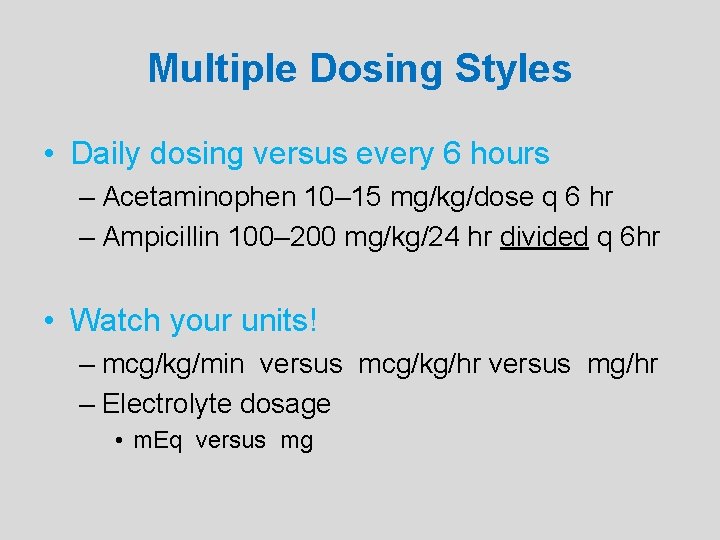
Multiple Dosing Styles • Daily dosing versus every 6 hours – Acetaminophen 10– 15 mg/kg/dose q 6 hr – Ampicillin 100– 200 mg/kg/24 hr divided q 6 hr • Watch your units! – mcg/kg/min versus mcg/kg/hr versus mg/hr – Electrolyte dosage • m. Eq versus mg
Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems
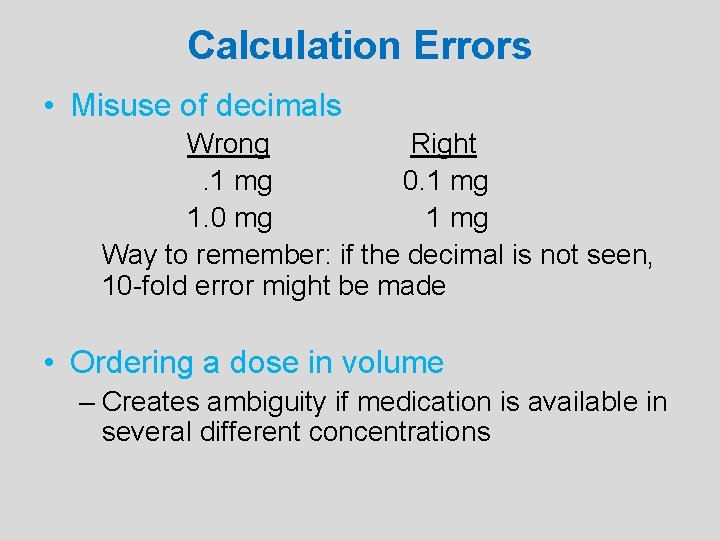
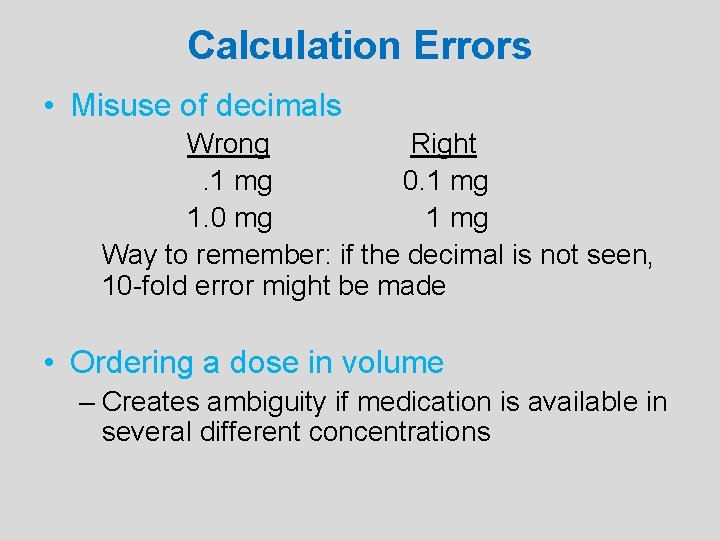
Calculation Errors • Misuse of decimals Wrong Right. 1 mg 0. 1 mg 1. 0 mg 1 mg Way to remember: if the decimal is not seen, 10 -fold error might be made • Ordering a dose in volume – Creates ambiguity if medication is available in several different concentrations
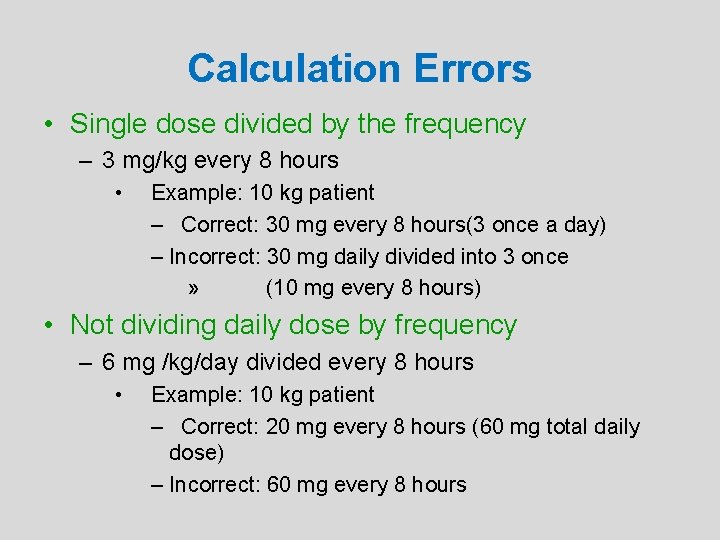
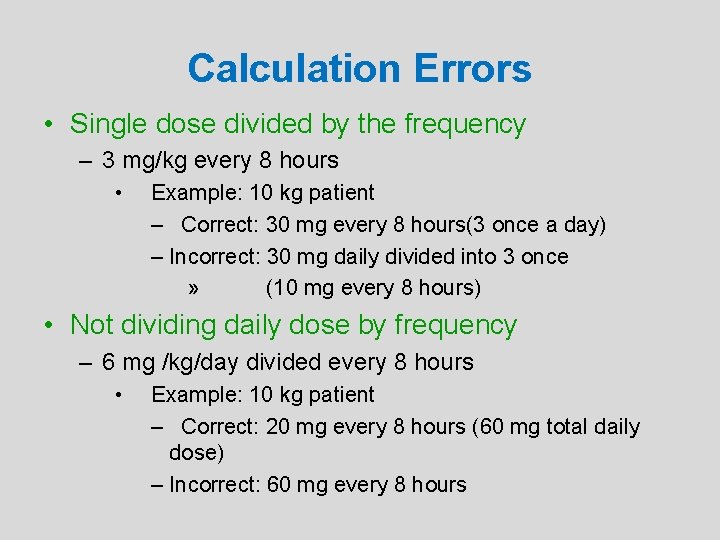
Calculation Errors • Single dose divided by the frequency – 3 mg/kg every 8 hours • Example: 10 kg patient – Correct: 30 mg every 8 hours(3 once a day) – Incorrect: 30 mg daily divided into 3 once » (10 mg every 8 hours) • Not dividing daily dose by frequency – 6 mg /kg/day divided every 8 hours • Example: 10 kg patient – Correct: 20 mg every 8 hours (60 mg total daily dose) – Incorrect: 60 mg every 8 hours
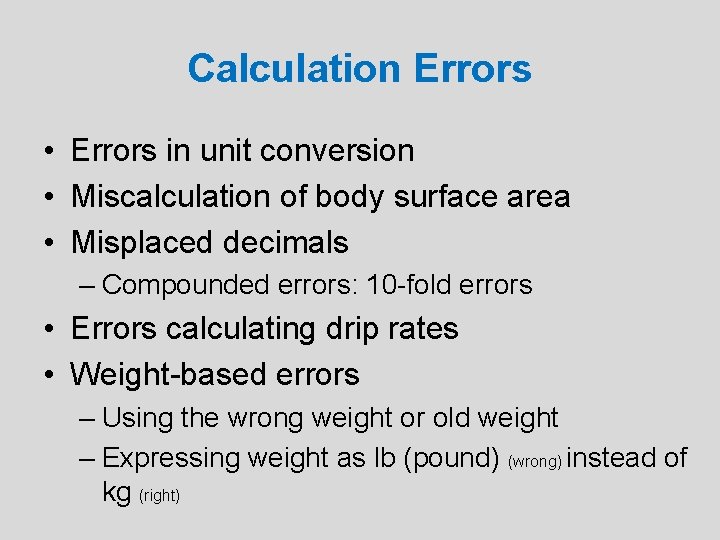
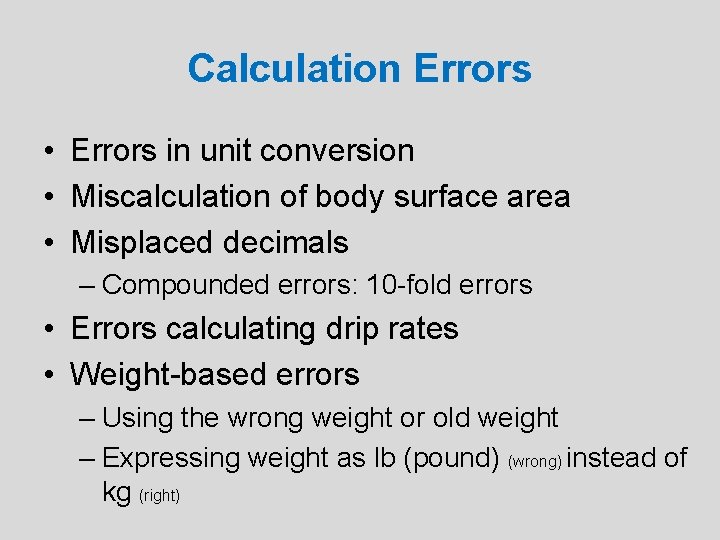
Calculation Errors • Errors in unit conversion • Miscalculation of body surface area • Misplaced decimals – Compounded errors: 10 -fold errors • Errors calculating drip rates • Weight-based errors – Using the wrong weight or old weight – Expressing weight as lb (pound) (wrong) instead of kg (right)
Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems
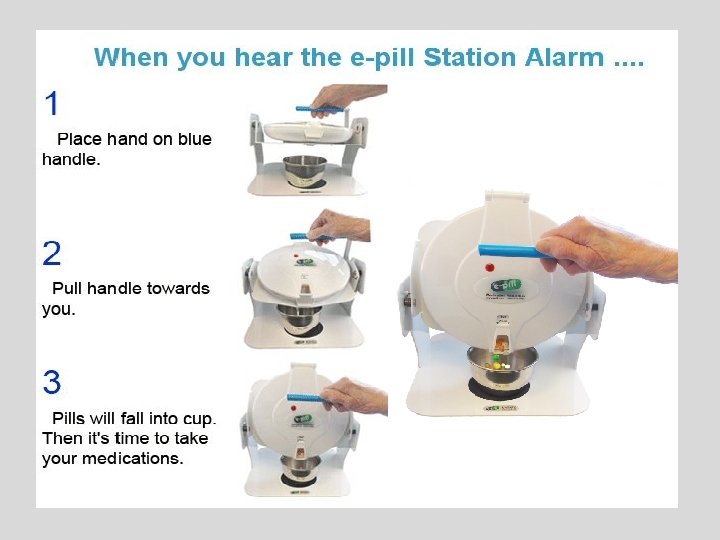
Oral Measuring Devices • Oral medications more likely to be dispensed in bulk and not in the unit of use • 75% of households still use kitchen teaspoons for measuring • Various calibration units on syringes – Varies on different syringe sizes
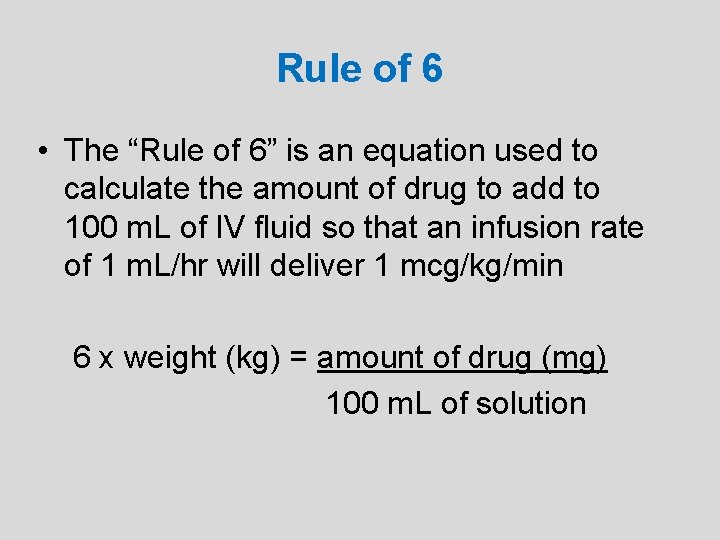
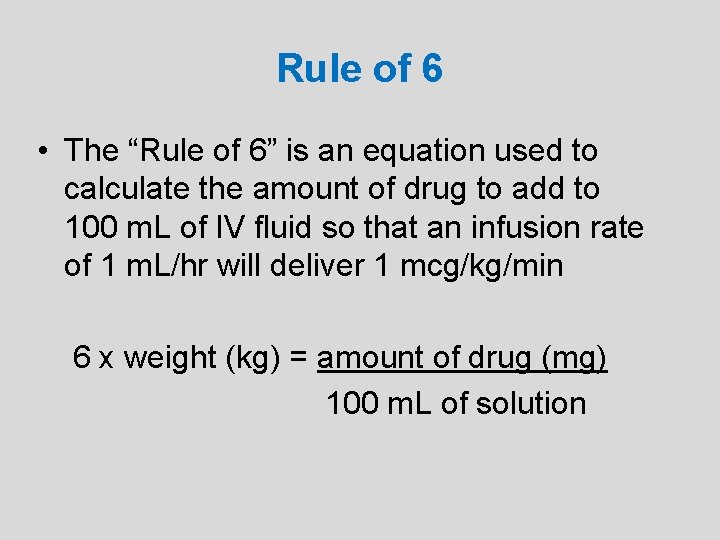
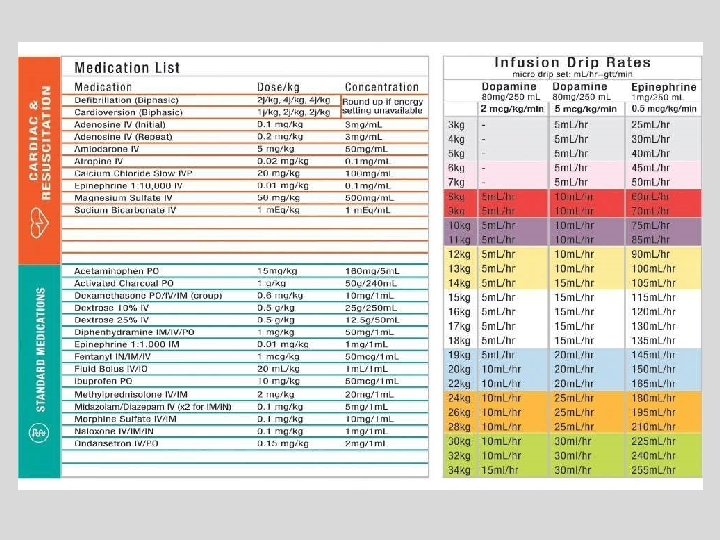
Rule of 6 • The “Rule of 6” is an equation used to calculate the amount of drug to add to 100 m. L of IV fluid so that an infusion rate of 1 m. L/hr will deliver 1 mcg/kg/min 6 x weight (kg) = amount of drug (mg) 100 m. L of solution
Concerns With Rule of 6 • Calculations and mixing may be completed at the bedside without pharmacy double check • Typically done with critical care, high-risk drugs • Dosage adjustments can result in fluid overload – Error risk compounded when double or triple concentrating infusions • Drug waste
Reasons for Increased Risk • Different and changing pharmacokinetic parameters • Lack of pediatric formulations, dosage forms, guidelines • Calculation errors • Inconsistent measurement of preparations • Problems with drug delivery systems
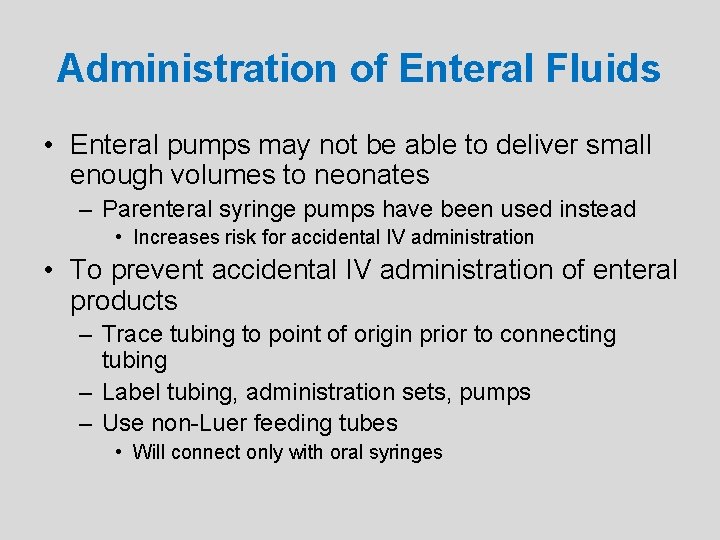
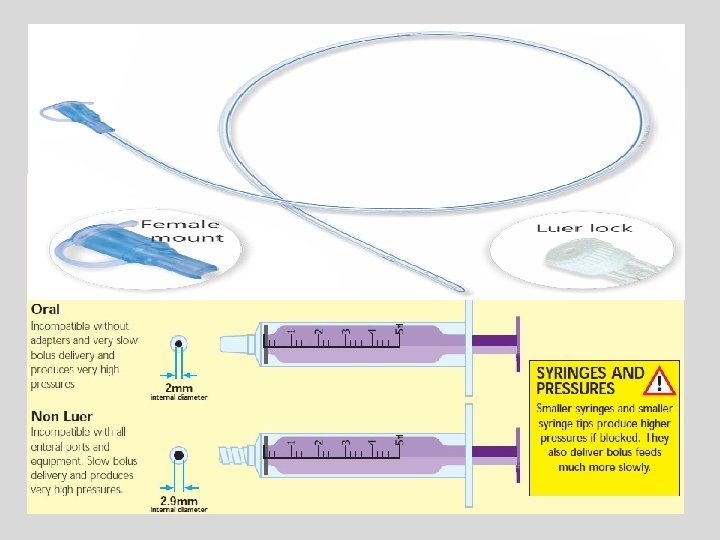
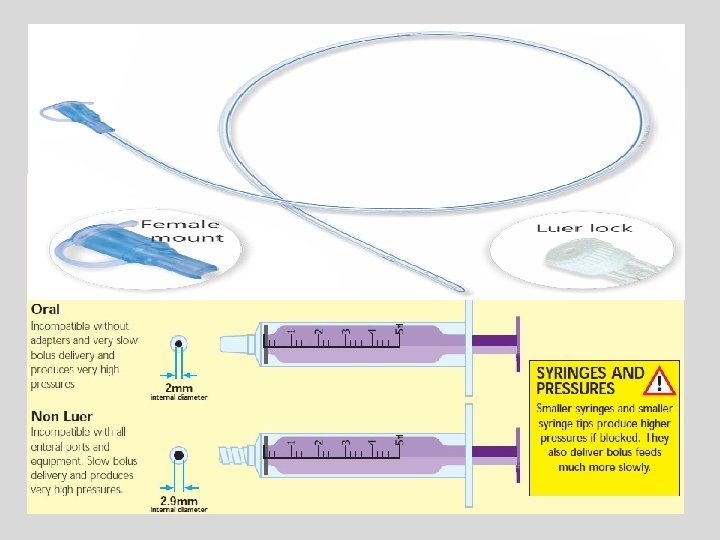
Administration of Enteral Fluids • Enteral pumps may not be able to deliver small enough volumes to neonates – Parenteral syringe pumps have been used instead • Increases risk for accidental IV administration • To prevent accidental IV administration of enteral products – Trace tubing to point of origin prior to connecting tubing – Label tubing, administration sets, pumps – Use non-Luer feeding tubes • Will connect only with oral syringes
Strategies for Medication Error Reduction
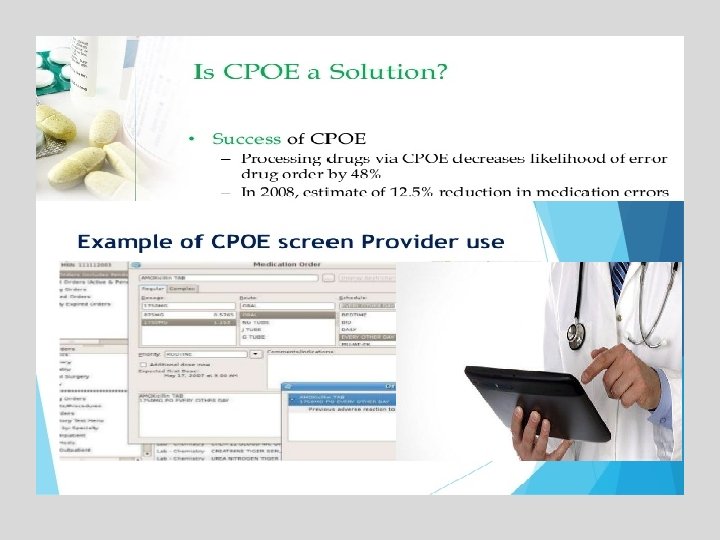
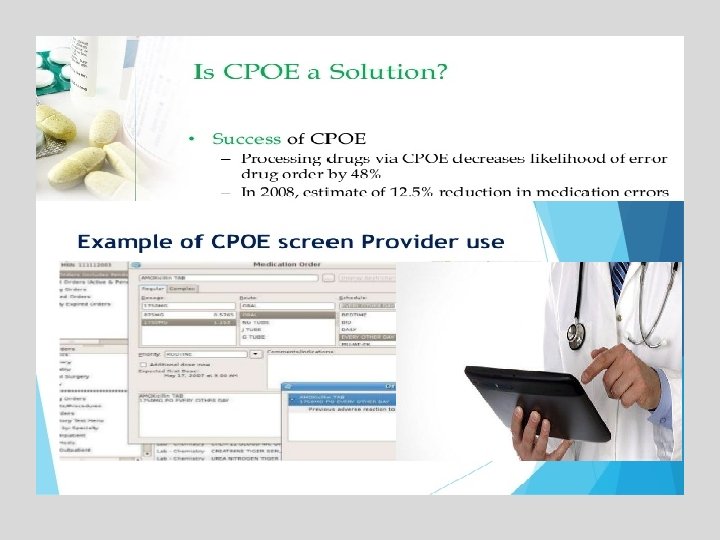
Strategies With Highest Error Prevention Potential in Pediatric Patients • Improved communication among physicians, nurses, and pharmacists • Clinical pharmacists making rounds with the healthcare team • Use of computerized prescriber order entry (CPOE)
Patient Information • Provide patient age (in years)and date of birth • Weight and height in Kg and meter • Patient’s medication history – Include concentration of all medications – Record doses in milligrams, not in volume – Specifically ask about common OTCs • Acetaminophen, ibuprofen, vitamins
Reduction of Calculation Errors • Establish reliable method of providing current patient weight in kg to the healthcare team • Require calculated dose and dose per weight (i. e. , mg/kg) on each order Acetaminophen 100 mg(10 mg/kg)every 6 hours PO • Require independent double check of dosing calculations .
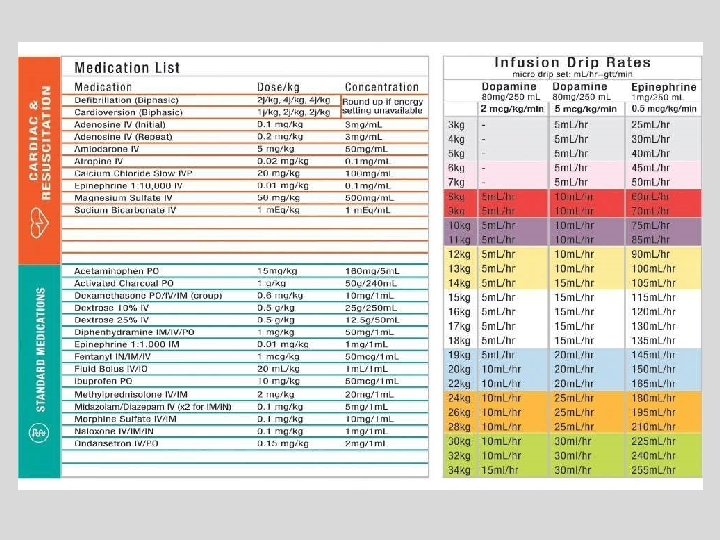
Reduction of Calculation Errors • Use pre-calculated dose sheets – Emergency medication sheets – Commonly used medications • Standardize dosing and concentrations – IV drip rates or concentrations • Provide pediatric references in ordering, dispensing, and administration • Encourage rounding to whole numbers when possible
Reduction of Calculation Errors • Include warnings for potentially low or high doses in the pharmacy • Appropriately use decimal points – Utilize leading zeros: – Do not use trailing zeros: 0. 1 (right) . 1 (wrong) 1. 0 (wrong)
Reduction of Prescribing Errors • Verbal (Phone) orders – Only for emergent/urgent situations – Not allowed when the prescriber and chart are available – Spell drug names and pronounce numeral digits • Fifty, Five Zero – Never accept verbal chemotherapy orders – Have order signed by prescriber as soon as possible
Reduction of Prescribing Errors • Write directly into patient’s chart • Avoid abbreviations – Do not use u for unit; spell out “unit” • U can be misread as a zero • 10 u can be misread as 100 – Do not use cc; use m. L • cc can be misread as 00 • 1 cc has been interpreted as 100 • Include patient weight in each order
Reduction of Dispensing Errors • Standardize concentrations • Use one consistent formula or standard concentration • Use the commercially available unit of use preparations whenever feasible • Have pharmacy prepare all IV admixtures and oral liquid preparations • Independently double check prior to dispensing
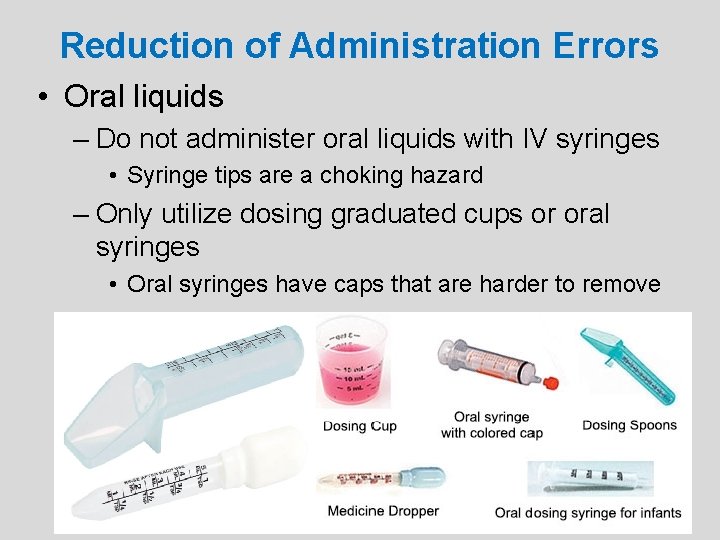
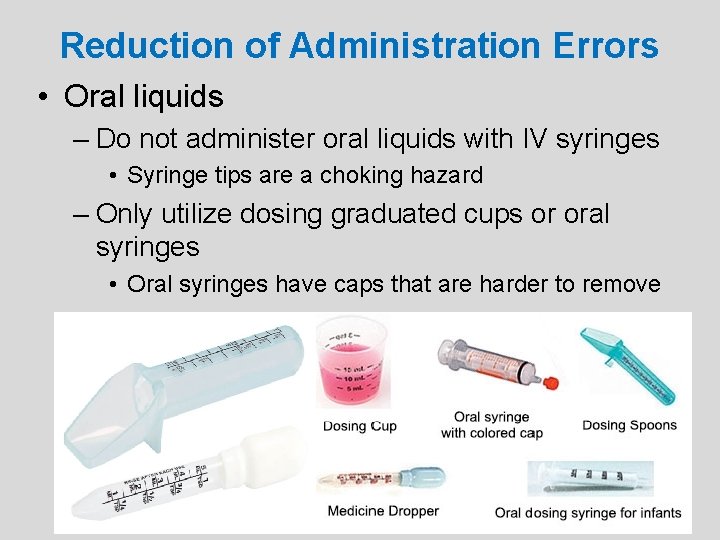
Reduction of Administration Errors • Oral liquids – Do not administer oral liquids with IV syringes • Syringe tips are a choking hazard – Only utilize dosing graduated cups or oral syringes • Oral syringes have caps that are harder to remove
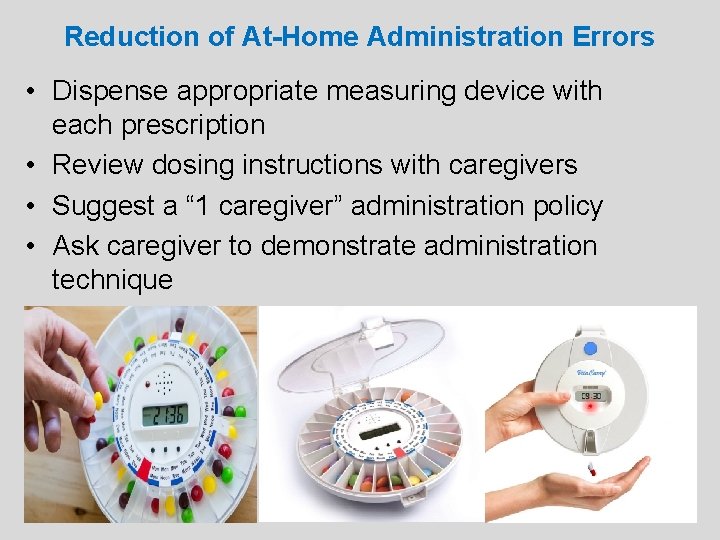
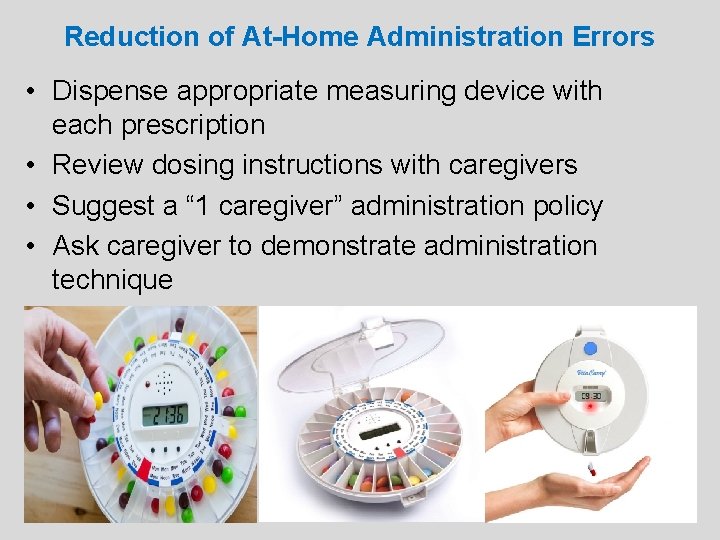
Reduction of At-Home Administration Errors • Dispense appropriate measuring device with each prescription • Review dosing instructions with caregivers • Suggest a “ 1 caregiver” administration policy • Ask caregiver to demonstrate administration technique
Reducing Errors in the Pediatric OR • Label all medications placed on and off sterile field including: – Drug name – Concentration/strength – Date and initials of person preparing • Segregate neuromuscular blocking agents from other medications
Reducing Errors in the Pediatric OR • Add required medications to surgeon’s preference cards or pre-printed order forms – Avoids verbal orders from OR • Standardize medications and concentrations for same procedures • Communicate information about perioperative medication use to postoperative care team
Pre-Procedure Sedation • Often prescribed for administration at home prior to arrival at physician’s office – Chloral hydrate and benzodiazepines most common • American Academy of Pediatrics – Children should not receive sedatives without supervision and monitoring by skilled medical personnel with appropriate resuscitation equipment
References Cohen MR. Medication Errors. Causes, Prevention, and Risk Management; 11. 1– 11. 16. Fortescue E, Kaushal R, Landrigan CP, et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2013; 111(4 pt 1): 722– 9. Institute for Safe Medication Practices. Safety briefs. ISMP Medication Safety Alert! February 26, 1997; 2: 1. Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2011; 285: 2114– 20.