COMMON FOOT ABNORMALITIES 3 RD ANNUAL ART PRACTICE
COMMON FOOT ABNORMALITIES 3 RD ANNUAL ART & PRACTICE OF PEDIATRIC ORTHOPEDICS FOR THE PCP FRIDAY, OCTOBER 26, 2018 JEANA SUMMERS, DO Jeana Lyn Summers, DO Pediatric Orthopaedic Fellow http: //www. phoenixchildrens. org jsummers 1@phoenixchildrens. com

OBJECTIVES Discuss normal pediatric foot anatomy/imaging Identify commonly seen conditions of the pediatric foot and recognize abnormalities Discuss non-operative treatment options in the primary care setting Identify when to refer to an orthopedist and what studies to obtain prior to referral
OUTLINE Foot anatomy Xray analysis Common terms Common pediatric foot conditions Metatarsus adductus Cavus deformities Planus deformities Osteochondroses Toe conditions
Shock absorption at heel strike Stability during weight bearing Level arm force generation
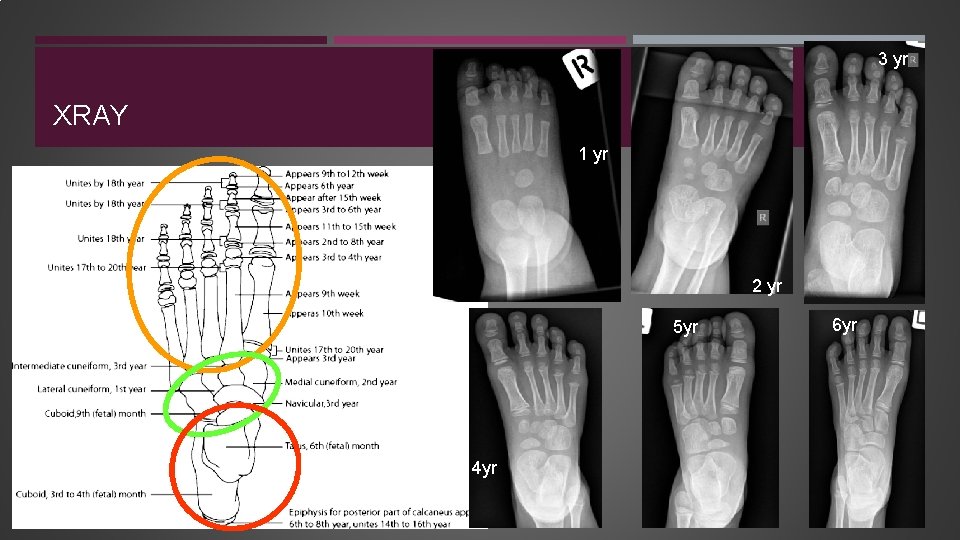
3 yr XRAY 1 yr 2 yr 5 yr 4 yr 6 yr
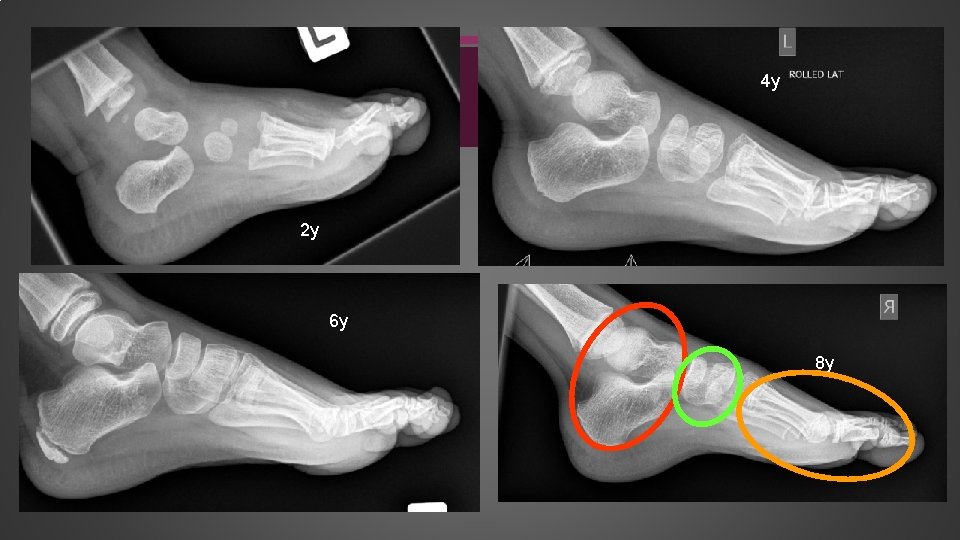
4 y 2 y 6 y 8 y

Equinus Calcaneal valgus Varus Equino varus Valgus Equino cavo varus Pronation/supination Plano valgus Cavus Abducto plano valgus Calcaneus Equino plano valgus Abduction Calcaneal cavus Adduction Cavo varus

EQUINUS: LATIN – RELATING TO HORSES
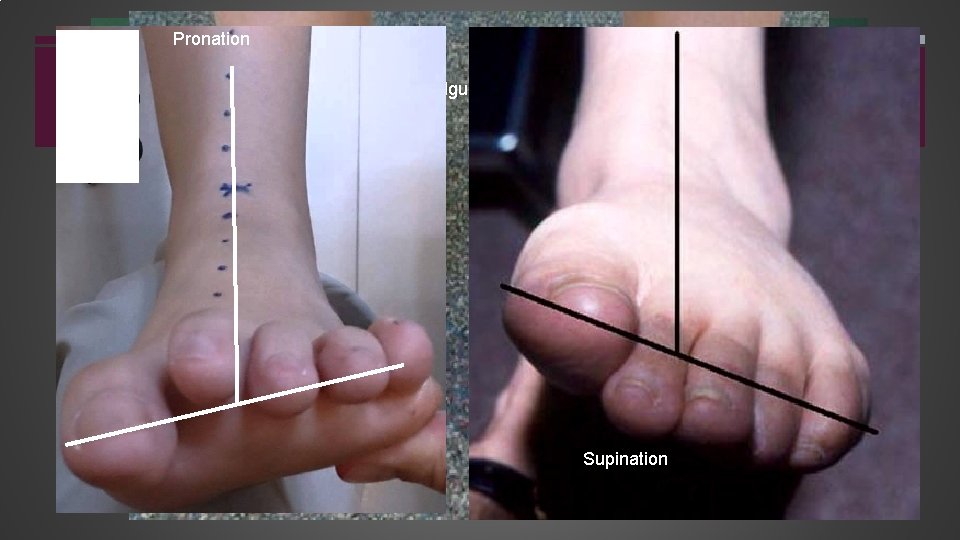
Pronation Valgus = Eversion Supination Varus = Inversion
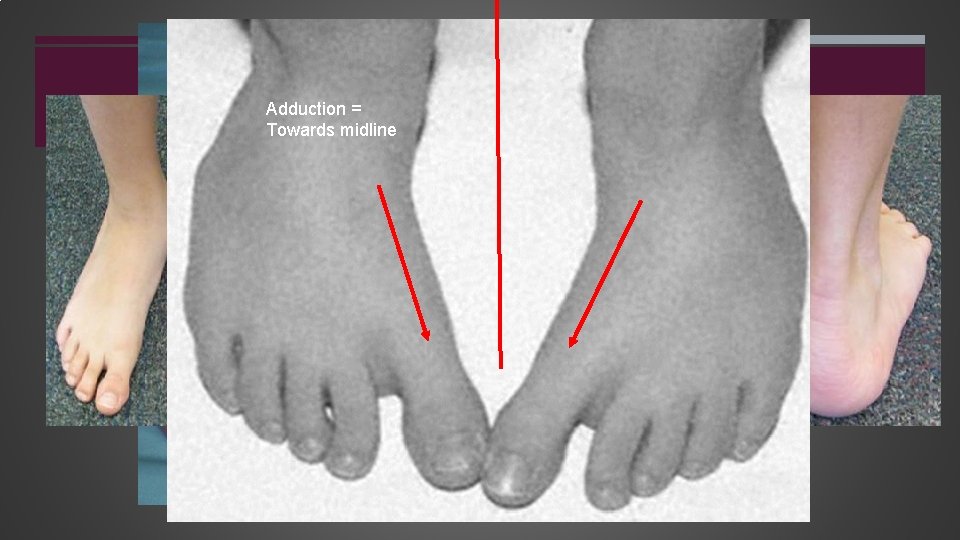
Adduction = Cavus = hollow arch Towards midline Abduction = away from midline
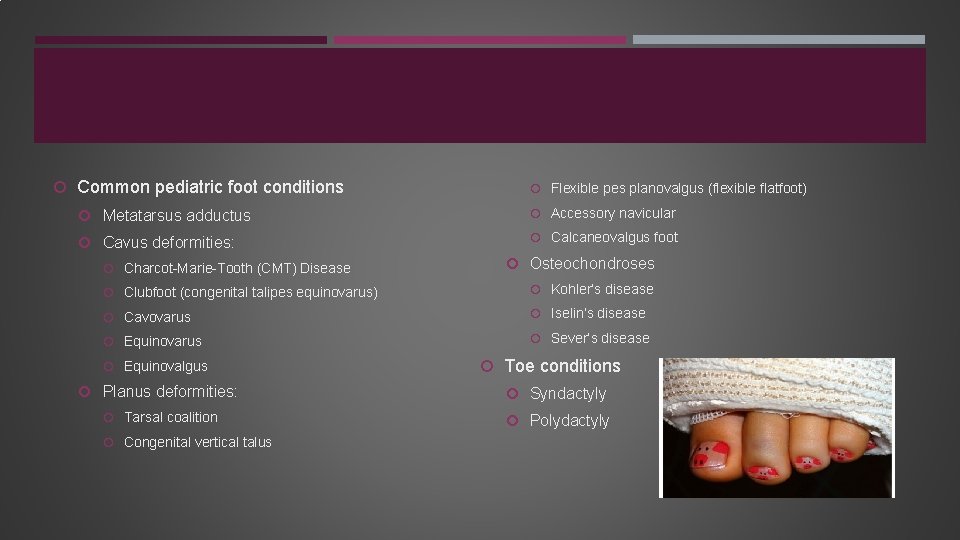
Common pediatric foot conditions Flexible pes planovalgus (flexible flatfoot) Metatarsus adductus Accessory navicular Cavus deformities: Calcaneovalgus foot Charcot-Marie-Tooth (CMT) Disease Osteochondroses Clubfoot (congenital talipes equinovarus) Kohler’s disease Cavovarus Iselin’s disease Equinovarus Sever’s disease Equinovalgus Toe conditions Planus deformities: Syndactyly Tarsal coalition Polydactyly Congenital vertical talus
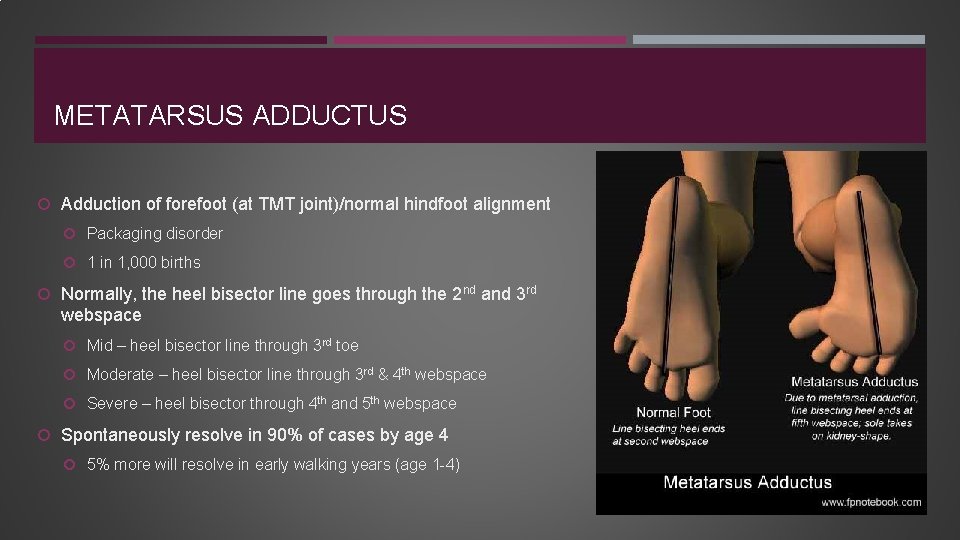
METATARSUS ADDUCTUS Adduction of forefoot (at TMT joint)/normal hindfoot alignment Packaging disorder 1 in 1, 000 births Normally, the heel bisector line goes through the 2 nd and 3 rd webspace Mid – heel bisector line through 3 rd toe Moderate – heel bisector line through 3 rd & 4 th webspace Severe – heel bisector through 4 th and 5 th webspace Spontaneously resolve in 90% of cases by age 4 5% more will resolve in early walking years (age 1 -4)
CAVUS DEFORMITIES Charcot-Marie-Tooth (CMT) Disease Clubfoot (congenital talipes equinovarus) Cavovarus Equinovalgus
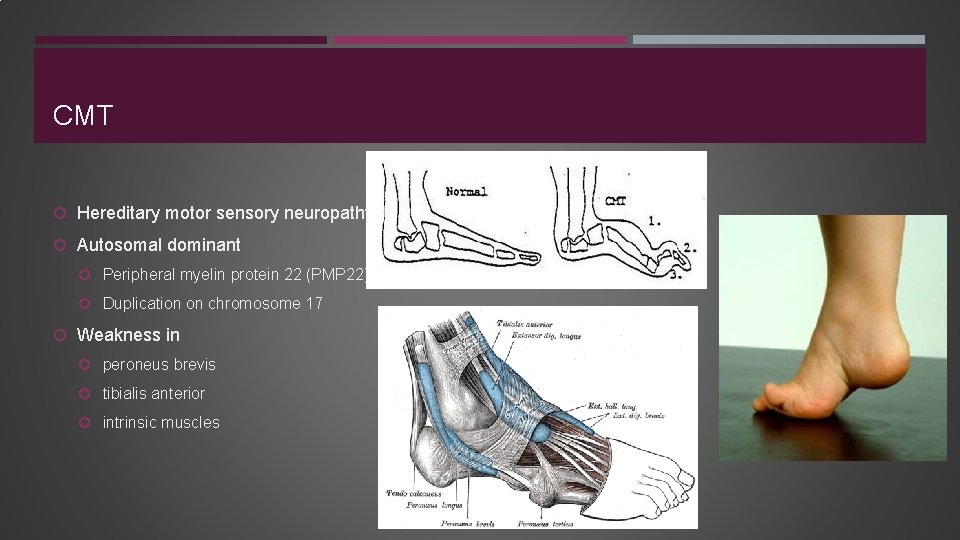
CMT Hereditary motor sensory neuropathy Autosomal dominant Peripheral myelin protein 22 (PMP 22) Duplication on chromosome 17 Weakness in peroneus brevis tibialis anterior intrinsic muscles
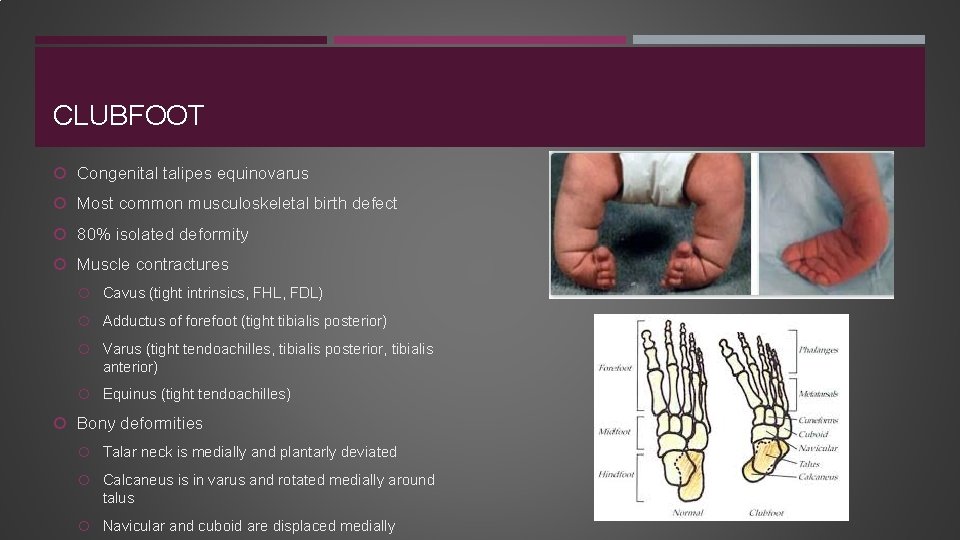
CLUBFOOT Congenital talipes equinovarus Most common musculoskeletal birth defect 80% isolated deformity Muscle contractures Cavus (tight intrinsics, FHL, FDL) Adductus of forefoot (tight tibialis posterior) Varus (tight tendoachilles, tibialis posterior, tibialis anterior) Equinus (tight tendoachilles) Bony deformities Talar neck is medially and plantarly deviated Calcaneus is in varus and rotated medially around talus Navicular and cuboid are displaced medially
Sometimes diagnosed in utero Seen on ultrasound Get established with orthopedist so parents can discuss treatment prior to birth Associated anomalies very common when diagnosed in 1 st trimester True clubfeet normally diagnosed during 2 nd trimester (anomalies are less common) False positive rate is higher due to higher probability of intrauterine crowding in 3 rd trimester

CLUBFOOT TREATMENT Ponseti method >90% success rate to avoid comprehensive surgical release Expect to walk, run, and be fully active Goal is to correct in the following order: Cavus Adductus Varus Equinus Foot abduction orthosis critical for longterm success Use full time x 3 mos and then at night (=/- naps) for 2 -4 years
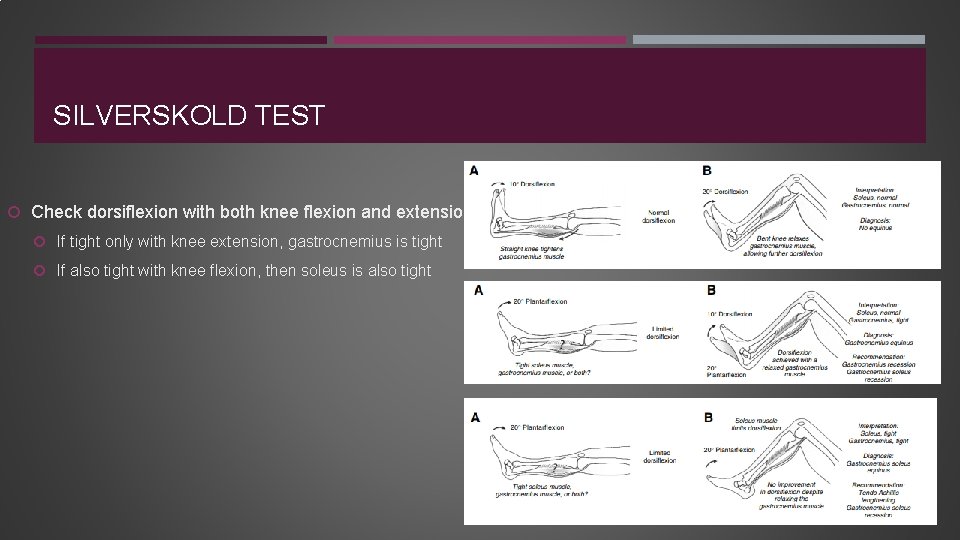
SILVERSKOLD TEST Check dorsiflexion with both knee flexion and extension If tight only with knee extension, gastrocnemius is tight If also tight with knee flexion, then soleus is also tight
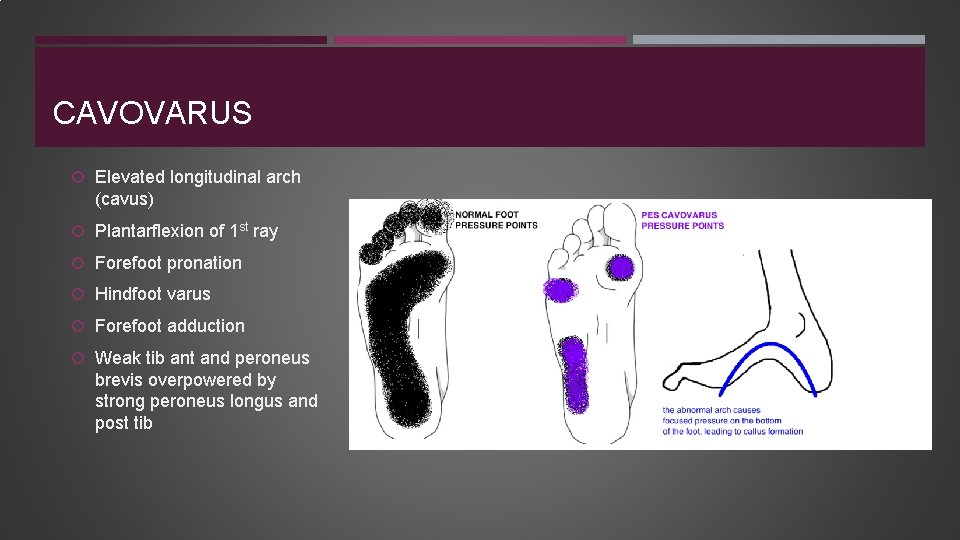
CAVOVARUS Elevated longitudinal arch (cavus) Plantarflexion of 1 st ray Forefoot pronation Hindfoot varus Forefoot adduction Weak tib ant and peroneus brevis overpowered by strong peroneus longus and post tib
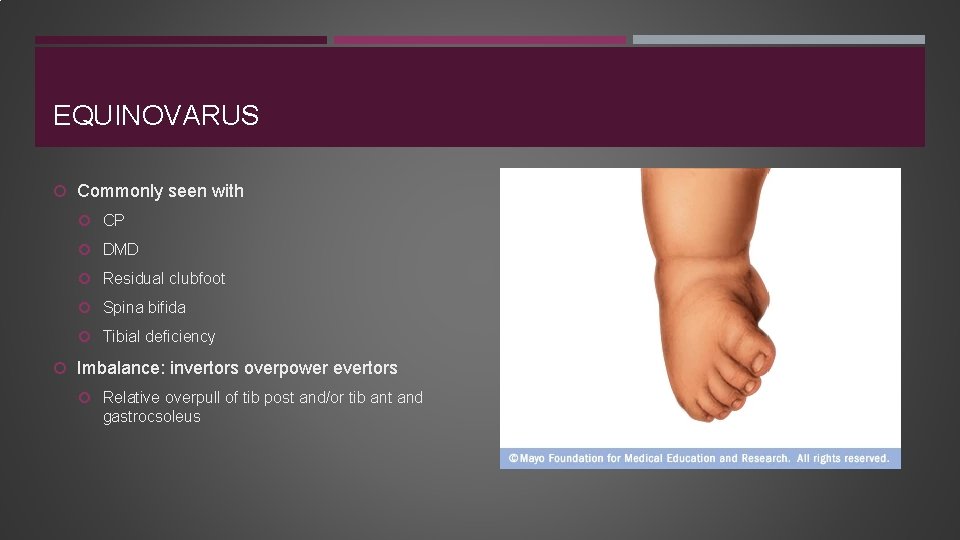
EQUINOVARUS Commonly seen with CP DMD Residual clubfoot Spina bifida Tibial deficiency Imbalance: invertors overpower evertors Relative overpull of tib post and/or tib ant and gastrocsoleus
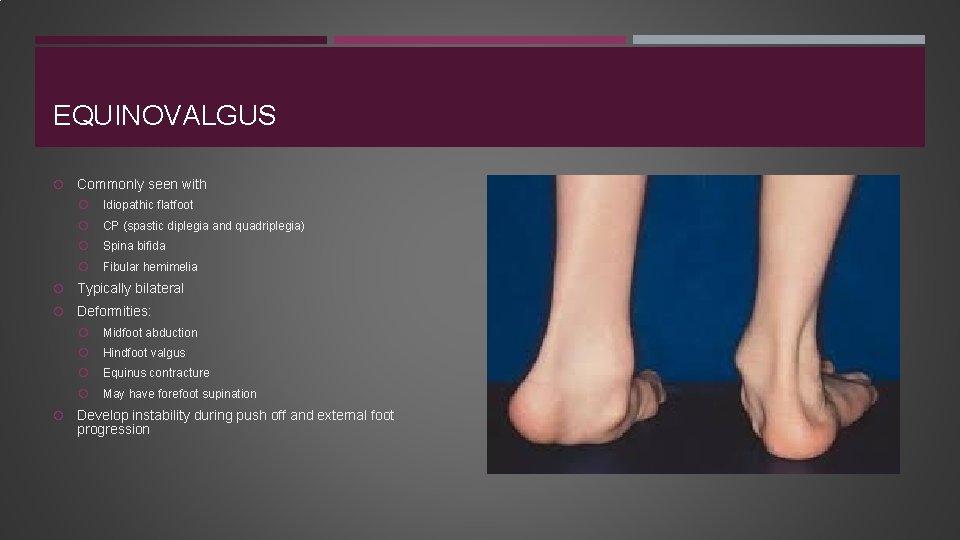
EQUINOVALGUS Commonly seen with Idiopathic flatfoot CP (spastic diplegia and quadriplegia) Spina bifida Fibular hemimelia Typically bilateral Deformities: Midfoot abduction Hindfoot valgus Equinus contracture May have forefoot supination Develop instability during push off and external foot progression
PLANUS DEFORMITIES Tarsal coalition Congenital vertical talus Flexible pes planovalgus (flexible flatfoot) Accessory navicular Calcaneovalgus foot
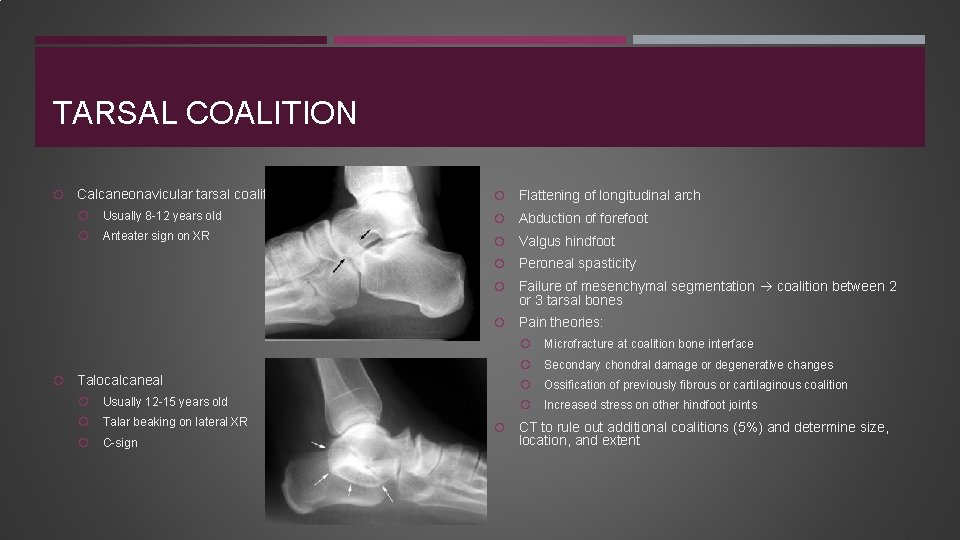
TARSAL COALITION Calcaneonavicular tarsal coalition Flattening of longitudinal arch Usually 8 -12 years old Abduction of forefoot Anteater sign on XR Valgus hindfoot Peroneal spasticity Failure of mesenchymal segmentation coalition between 2 or 3 tarsal bones Pain theories: Talocalcaneal Usually 12 -15 years old Talar beaking on lateral XR C-sign Microfracture at coalition bone interface Secondary chondral damage or degenerative changes Ossification of previously fibrous or cartilaginous coalition Increased stress on other hindfoot joints CT to rule out additional coalitions (5%) and determine size, location, and extent
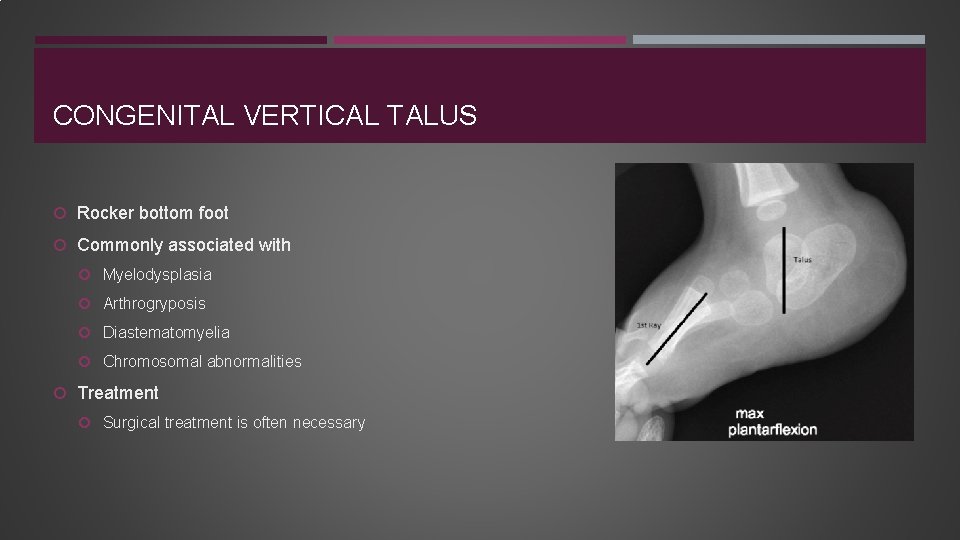
CONGENITAL VERTICAL TALUS Rocker bottom foot Commonly associated with Myelodysplasia Arthrogryposis Diastematomyelia Chromosomal abnormalities Treatment Surgical treatment is often necessary
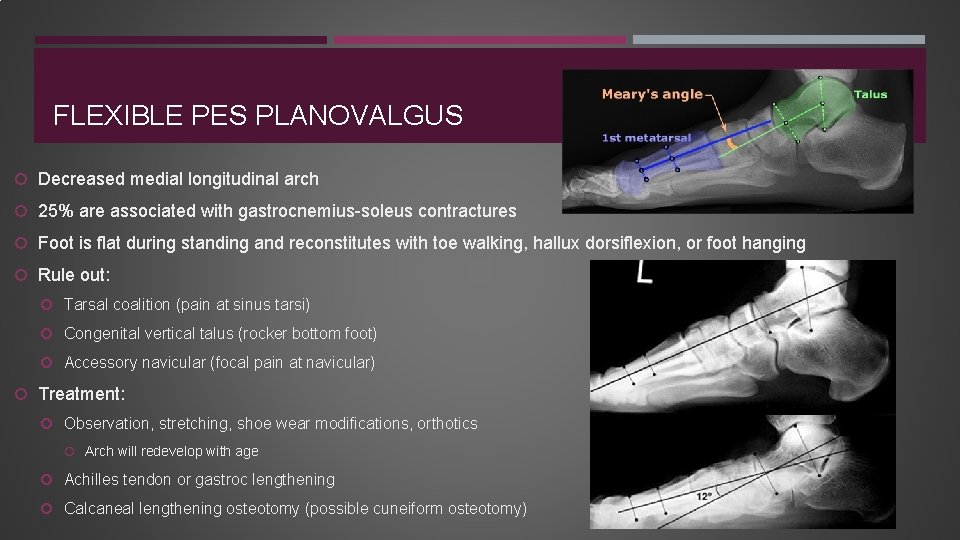
FLEXIBLE PES PLANOVALGUS Decreased medial longitudinal arch 25% are associated with gastrocnemius-soleus contractures Foot is flat during standing and reconstitutes with toe walking, hallux dorsiflexion, or foot hanging Rule out: Tarsal coalition (pain at sinus tarsi) Congenital vertical talus (rocker bottom foot) Accessory navicular (focal pain at navicular) Treatment: Observation, stretching, shoe wear modifications, orthotics Arch will redevelop with age Achilles tendon or gastroc lengthening Calcaneal lengthening osteotomy (possible cuneiform osteotomy)
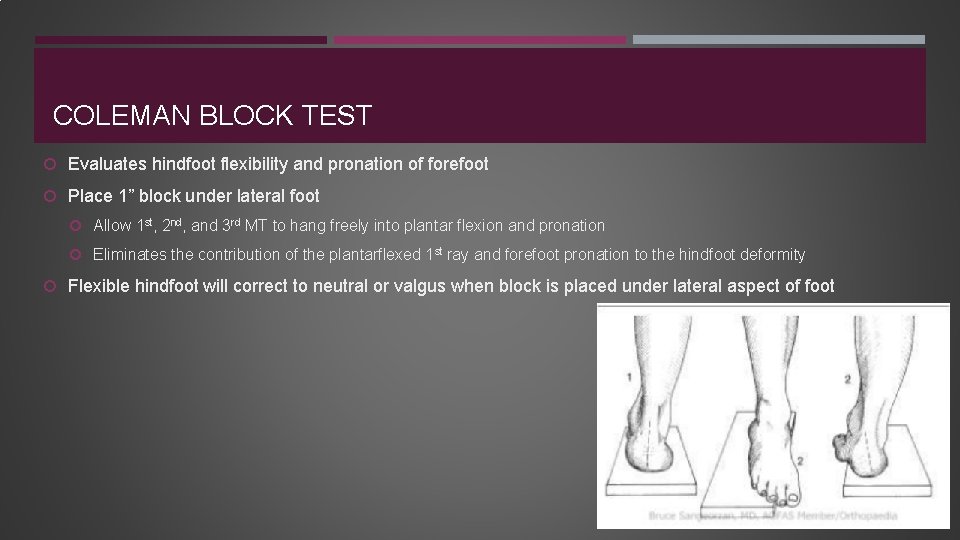
COLEMAN BLOCK TEST Evaluates hindfoot flexibility and pronation of forefoot Place 1” block under lateral foot Allow 1 st, 2 nd, and 3 rd MT to hang freely into plantar flexion and pronation Eliminates the contribution of the plantarflexed 1 st ray and forefoot pronation to the hindfoot deformity Flexible hindfoot will correct to neutral or valgus when block is placed under lateral aspect of foot
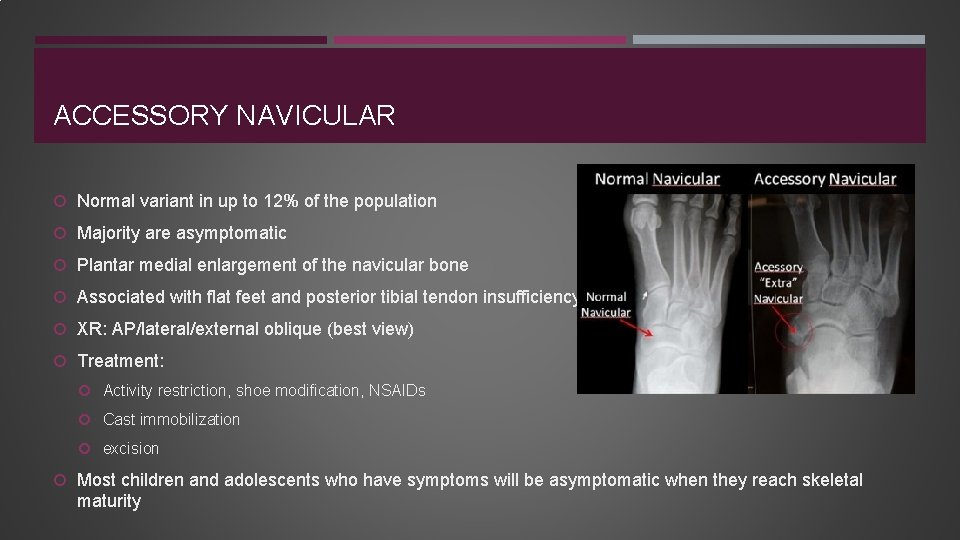
ACCESSORY NAVICULAR Normal variant in up to 12% of the population Majority are asymptomatic Plantar medial enlargement of the navicular bone Associated with flat feet and posterior tibial tendon insufficiency XR: AP/lateral/external oblique (best view) Treatment: Activity restriction, shoe modification, NSAIDs Cast immobilization excision Most children and adolescents who have symptoms will be asymptomatic when they reach skeletal maturity
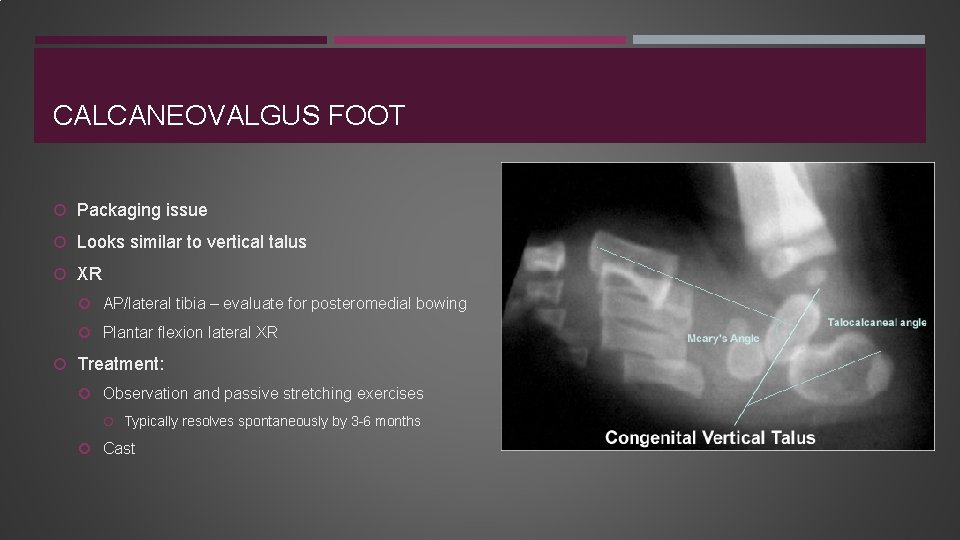
CALCANEOVALGUS FOOT Packaging issue Looks similar to vertical talus XR AP/lateral tibia – evaluate for posteromedial bowing Plantar flexion lateral XR Treatment: Observation and passive stretching exercises Typically resolves spontaneously by 3 -6 months Cast
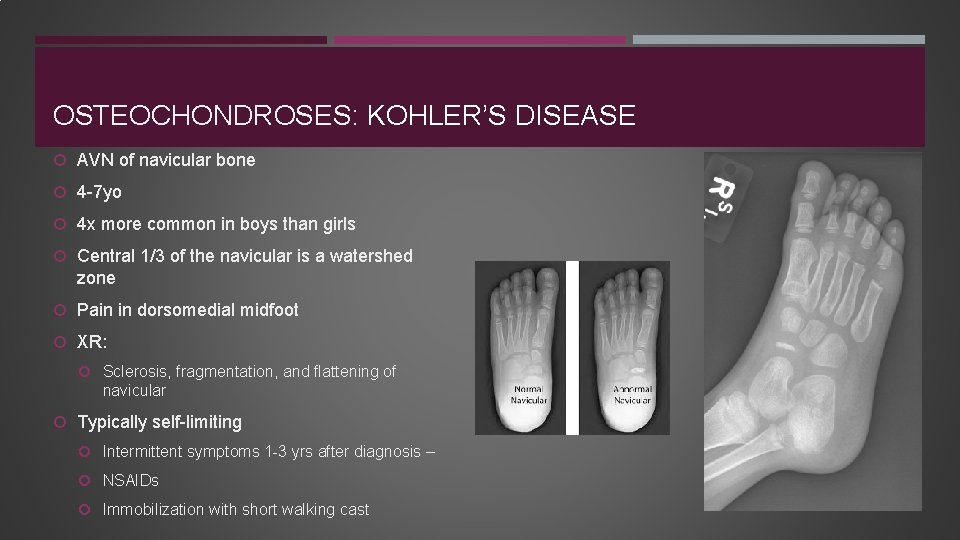
OSTEOCHONDROSES: KOHLER’S DISEASE AVN of navicular bone 4 -7 yo 4 x more common in boys than girls Central 1/3 of the navicular is a watershed zone Pain in dorsomedial midfoot XR: Sclerosis, fragmentation, and flattening of navicular Typically self-limiting Intermittent symptoms 1 -3 yrs after diagnosis – NSAIDs Immobilization with short walking cast
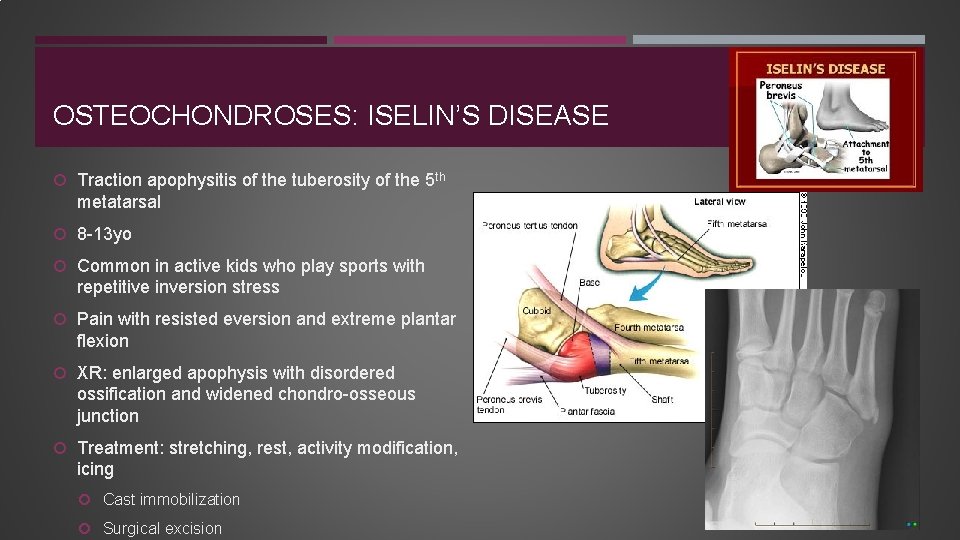
OSTEOCHONDROSES: ISELIN’S DISEASE Traction apophysitis of the tuberosity of the 5 th metatarsal 8 -13 yo Common in active kids who play sports with repetitive inversion stress Pain with resisted eversion and extreme plantar flexion XR: enlarged apophysis with disordered ossification and widened chondro-osseous junction Treatment: stretching, rest, activity modification, icing Cast immobilization Surgical excision
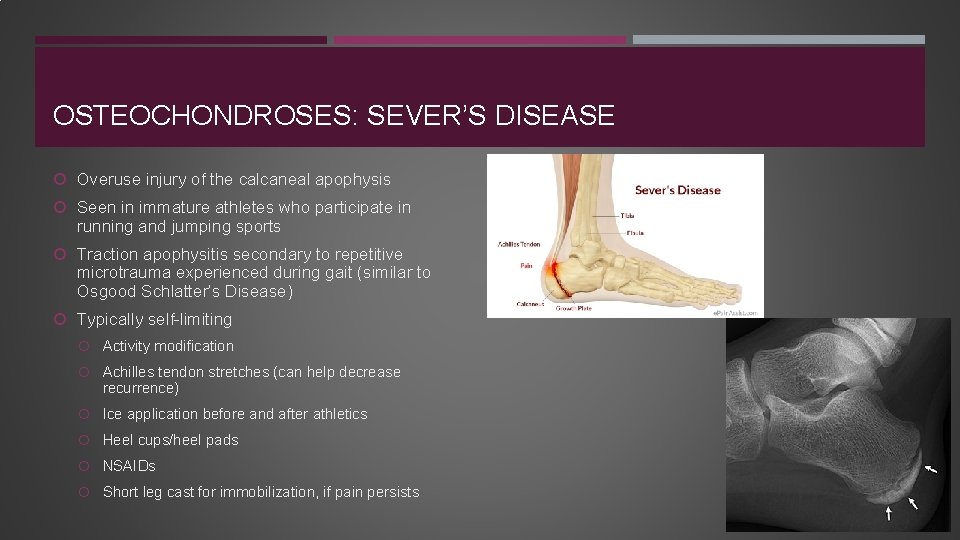
OSTEOCHONDROSES: SEVER’S DISEASE Overuse injury of the calcaneal apophysis Seen in immature athletes who participate in running and jumping sports Traction apophysitis secondary to repetitive microtrauma experienced during gait (similar to Osgood Schlatter’s Disease) Typically self-limiting Activity modification Achilles tendon stretches (can help decrease recurrence) Ice application before and after athletics Heel cups/heel pads NSAIDs Short leg cast for immobilization, if pain persists
TOE CONDITIONS: SYNDACTYLY 1 in 2, 000 births Most frequently between 2 nd and 3 rd toe Due to incomplete or absent apoptosis during gestation Autosomal dominant Types: Simple – soft tissue only Complex – bony fusion Usually painless with cosmetic concerns only May perform digital release for complex syndactyly or for aesthetic reasons in simple forms
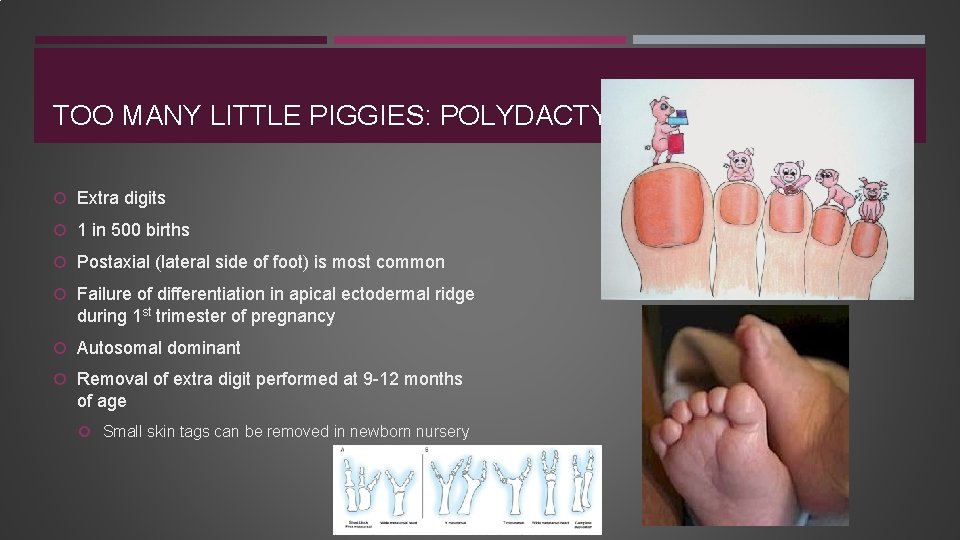
TOO MANY LITTLE PIGGIES: POLYDACTYLY Extra digits 1 in 500 births Postaxial (lateral side of foot) is most common Failure of differentiation in apical ectodermal ridge during 1 st trimester of pregnancy Autosomal dominant Removal of extra digit performed at 9 -12 months of age Small skin tags can be removed in newborn nursery
THANK YOU! Questions?
- Slides: 34