Combined hormonal contraception Dr Caroline Marfleet Consultant in
Combined hormonal contraception Dr Caroline Marfleet Consultant in Sexual and Reproductive Healthcare Colchester Hospital University Foundation Trust Nov 2016
2010 ‘ 50 th anniversary of the pill’ ENOVID – 75 mcg mestranol + 5 mgm norethynodrel Approved for use as a contraceptive in 1960 Approved for use in Japan in 1999 1961 – 1 st case of Pulmonary embolus in Suffolk, England
1960 -2016 • Dose of EE has • New, more specific progestogens • OCs containing Oestradiol as valerate/hemihydrate • New methods of delivery of CHC – patches, rings • Better knowledge and clinical evidence! • Improved QOL and better health for women
Use of the OCP • Most commonly used method of contraception for women in UK • Used by 1 million women in 1969 • Used by 3 and a quarter million women in 2000 • Use decreases with age • 2/3 of women use ocp age 20 -24 • 11% of women use ocp in late 40 s FPA Fact sheet 2007
2016 – 3 methods of delivery of combined hormonal contraception
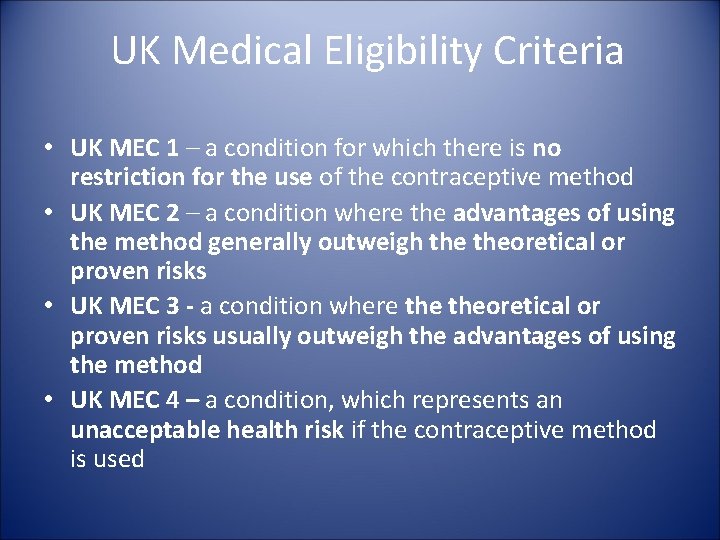
UK Medical Eligibility Criteria • UK MEC 1 – a condition for which there is no restriction for the use of the contraceptive method • UK MEC 2 – a condition where the advantages of using the method generally outweigh theoretical or proven risks • UK MEC 3 - a condition where theoretical or proven risks usually outweigh the advantages of using the method • UK MEC 4 – a condition, which represents an unacceptable health risk if the contraceptive method is used
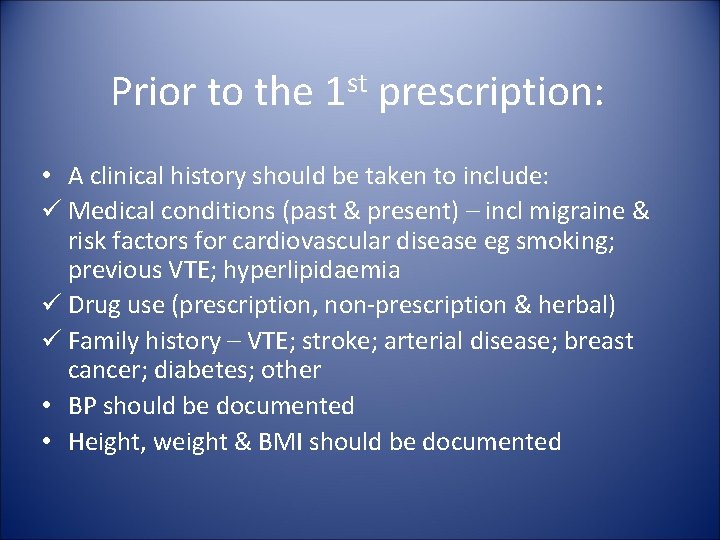
Prior to the st 1 prescription: • A clinical history should be taken to include: ü Medical conditions (past & present) – incl migraine & risk factors for cardiovascular disease eg smoking; previous VTE; hyperlipidaemia ü Drug use (prescription, non-prescription & herbal) ü Family history – VTE; stroke; arterial disease; breast cancer; diabetes; other • BP should be documented • Height, weight & BMI should be documented

WHICH CHC? • Types of OCPs – combined and progestogen-only • Ethinyl oestradiol and progestogens • Oestradiol valerate /hemihydrate(body-identical oestrogen) and progestogen • Routes of administration -pill. patch, ring • Risks and benefits to individuals • Side effects relating to oestrogens/progestogens • Which pill and managing side effects
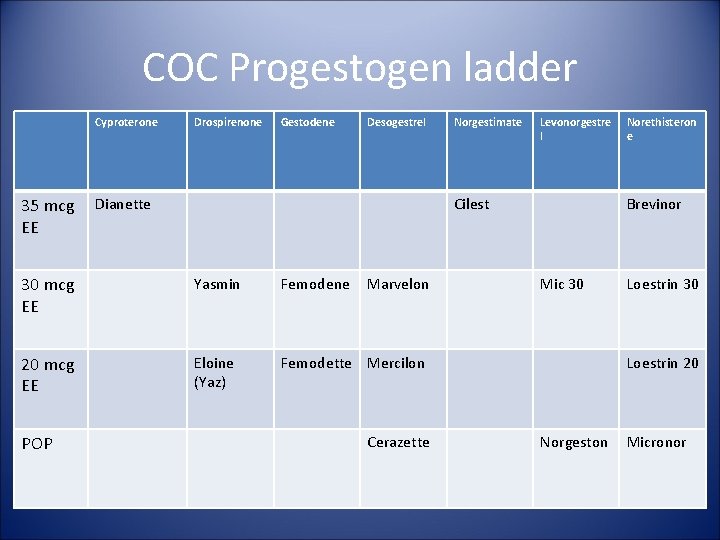
COC Progestogen ladder Cyproterone 35 mcg EE Drospirenone Gestodene Desogestrel Dianette Levonorgestre l Cilest 30 mcg EE Yasmin Femodene 20 mcg EE Eloine (Yaz) Femodette Mercilon POP Norgestimate Marvelon Cerazette Norethisteron e Brevinor Mic 30 Loestrin 20 Norgeston Micronor
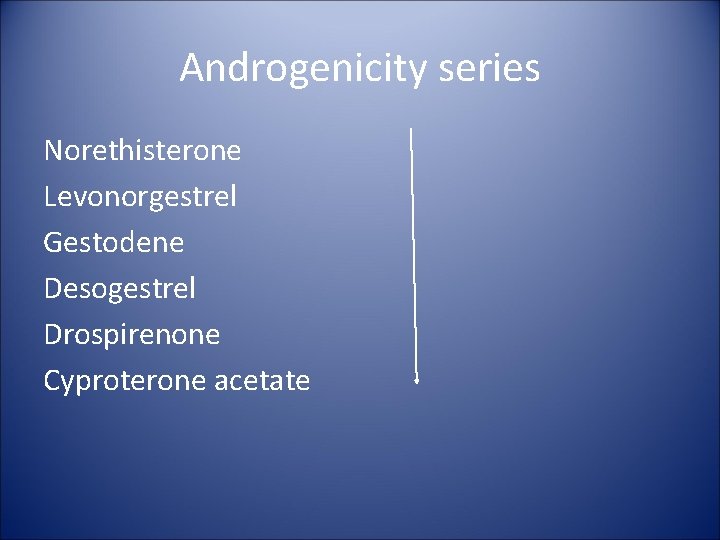
Androgenicity series Norethisterone Levonorgestrel Gestodene Desogestrel Drospirenone Cyproterone acetate
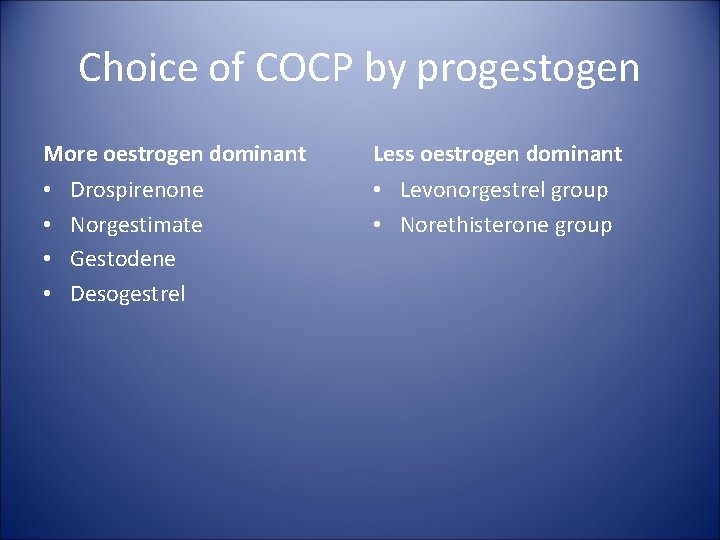
Choice of COCP by progestogen More oestrogen dominant • • Drospirenone Norgestimate Gestodene Desogestrel Less oestrogen dominant • Levonorgestrel group • Norethisterone group
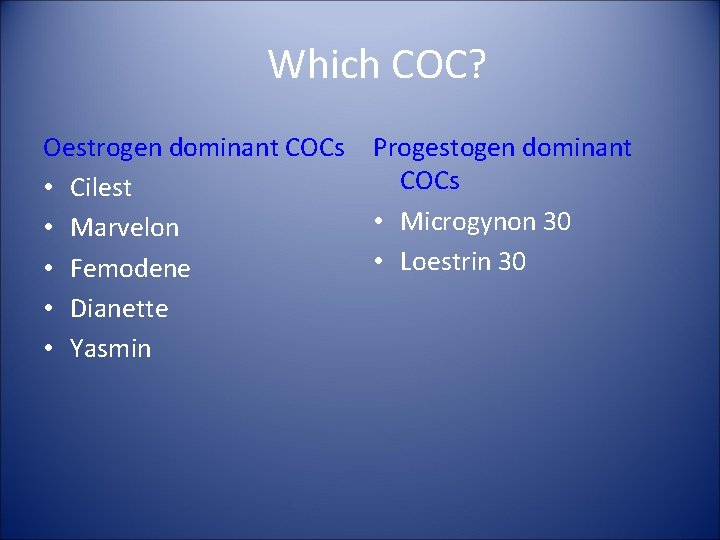
Which COC? Oestrogen dominant COCs • Cilest • Marvelon • Femodene • Dianette • Yasmin Progestogen dominant COCs • Microgynon 30 • Loestrin 30
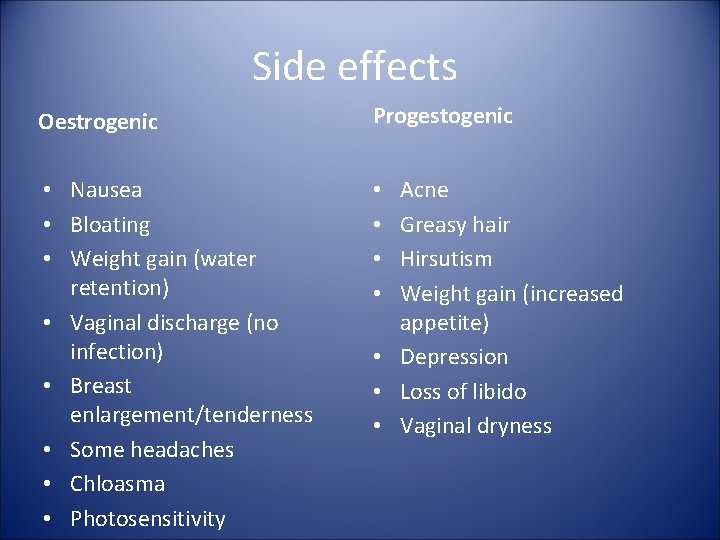
Side effects Oestrogenic Progestogenic • Nausea • Bloating • Weight gain (water retention) • Vaginal discharge (no infection) • Breast enlargement/tenderness • Some headaches • Chloasma • Photosensitivity • • Acne Greasy hair Hirsutism Weight gain (increased appetite) • Depression • Loss of libido • Vaginal dryness
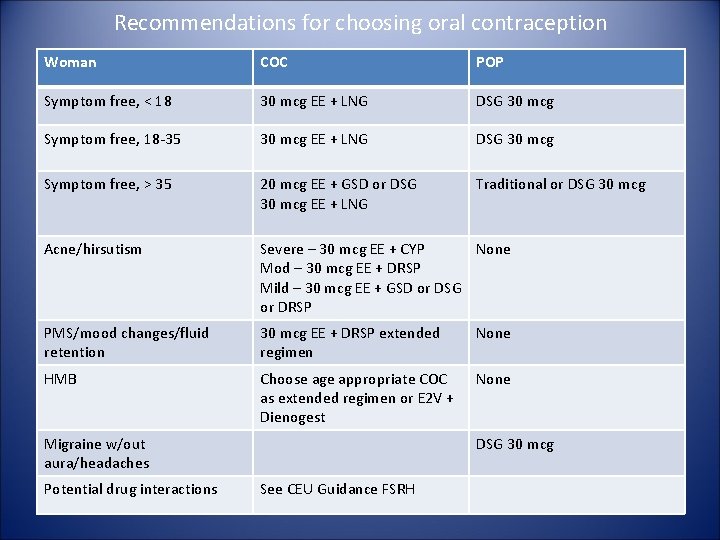
Recommendations for choosing oral contraception Woman COC POP Symptom free, < 18 30 mcg EE + LNG DSG 30 mcg Symptom free, 18 -35 30 mcg EE + LNG DSG 30 mcg Symptom free, > 35 20 mcg EE + GSD or DSG 30 mcg EE + LNG Traditional or DSG 30 mcg Acne/hirsutism Severe – 30 mcg EE + CYP None Mod – 30 mcg EE + DRSP Mild – 30 mcg EE + GSD or DSG or DRSP PMS/mood changes/fluid retention 30 mcg EE + DRSP extended regimen None HMB Choose age appropriate COC as extended regimen or E 2 V + Dienogest None Migraine w/out aura/headaches Potential drug interactions DSG 30 mcg See CEU Guidance FSRH
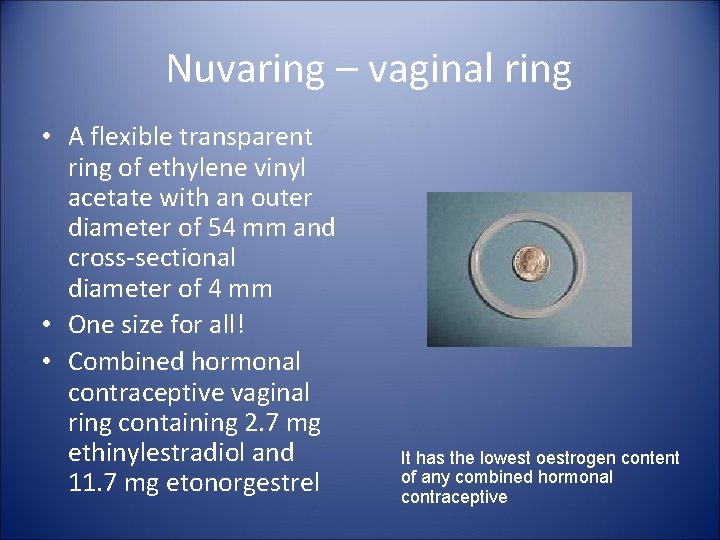
Nuvaring – vaginal ring • A flexible transparent ring of ethylene vinyl acetate with an outer diameter of 54 mm and cross-sectional diameter of 4 mm • One size for all! • Combined hormonal contraceptive vaginal ring containing 2. 7 mg ethinylestradiol and 11. 7 mg etonorgestrel It has the lowest oestrogen content of any combined hormonal contraceptive
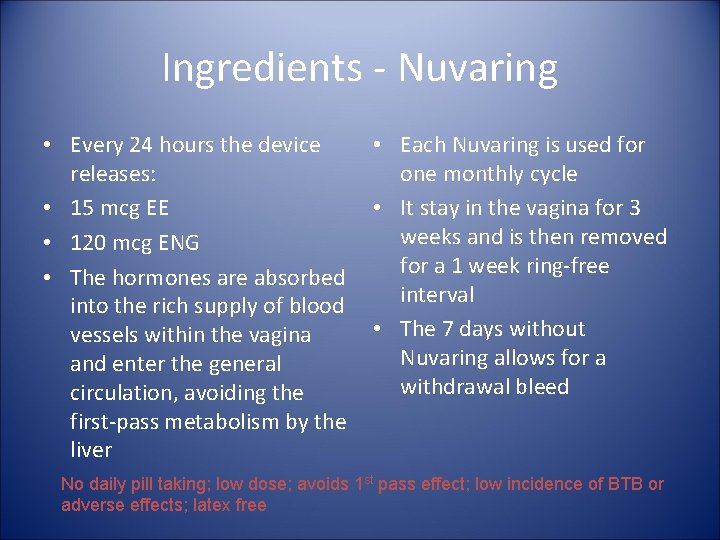
Ingredients - Nuvaring • Every 24 hours the device releases: • 15 mcg EE • 120 mcg ENG • The hormones are absorbed into the rich supply of blood vessels within the vagina and enter the general circulation, avoiding the first-pass metabolism by the liver • Each Nuvaring is used for one monthly cycle • It stay in the vagina for 3 weeks and is then removed for a 1 week ring-free interval • The 7 days without Nuvaring allows for a withdrawal bleed No daily pill taking; low dose; avoids 1 st pass effect; low incidence of BTB or adverse effects; latex free
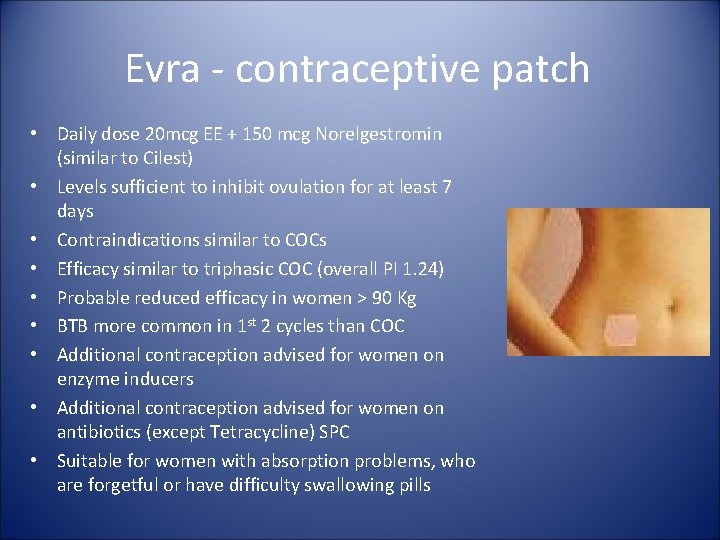
Evra - contraceptive patch • Daily dose 20 mcg EE + 150 mcg Norelgestromin (similar to Cilest) • Levels sufficient to inhibit ovulation for at least 7 days • Contraindications similar to COCs • Efficacy similar to triphasic COC (overall PI 1. 24) • Probable reduced efficacy in women > 90 Kg • BTB more common in 1 st 2 cycles than COC • Additional contraception advised for women on enzyme inducers • Additional contraception advised for women on antibiotics (except Tetracycline) SPC • Suitable for women with absorption problems, who are forgetful or have difficulty swallowing pills
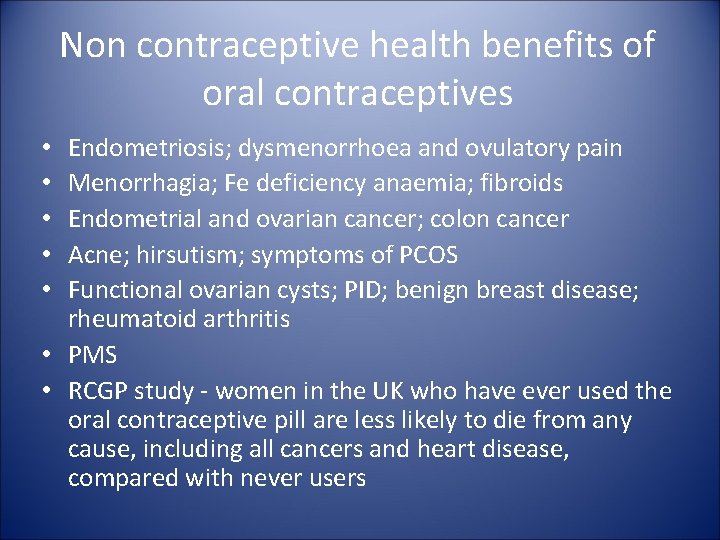
Non contraceptive health benefits of oral contraceptives Endometriosis; dysmenorrhoea and ovulatory pain Menorrhagia; Fe deficiency anaemia; fibroids Endometrial and ovarian cancer; colon cancer Acne; hirsutism; symptoms of PCOS Functional ovarian cysts; PID; benign breast disease; rheumatoid arthritis • PMS • RCGP study - women in the UK who have ever used the oral contraceptive pill are less likely to die from any cause, including all cancers and heart disease, compared with never users • • •
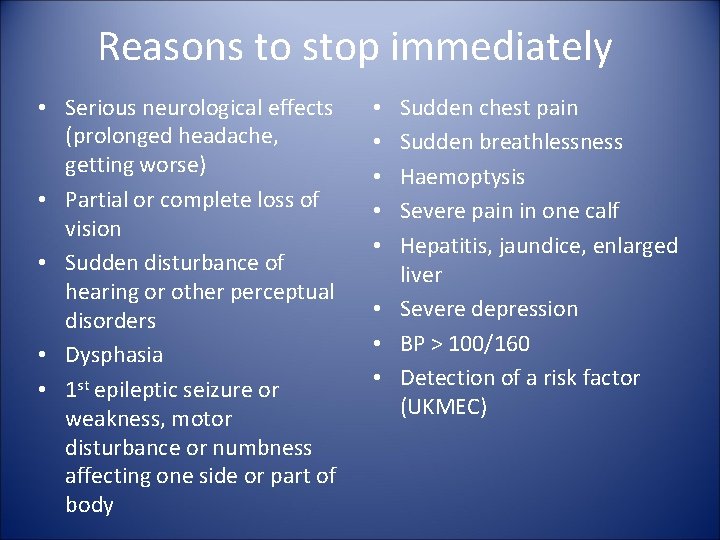
Reasons to stop immediately • Serious neurological effects (prolonged headache, getting worse) • Partial or complete loss of vision • Sudden disturbance of hearing or other perceptual disorders • Dysphasia • 1 st epileptic seizure or weakness, motor disturbance or numbness affecting one side or part of body Sudden chest pain Sudden breathlessness Haemoptysis Severe pain in one calf Hepatitis, jaundice, enlarged liver • Severe depression • BP > 100/160 • Detection of a risk factor (UKMEC) • • •
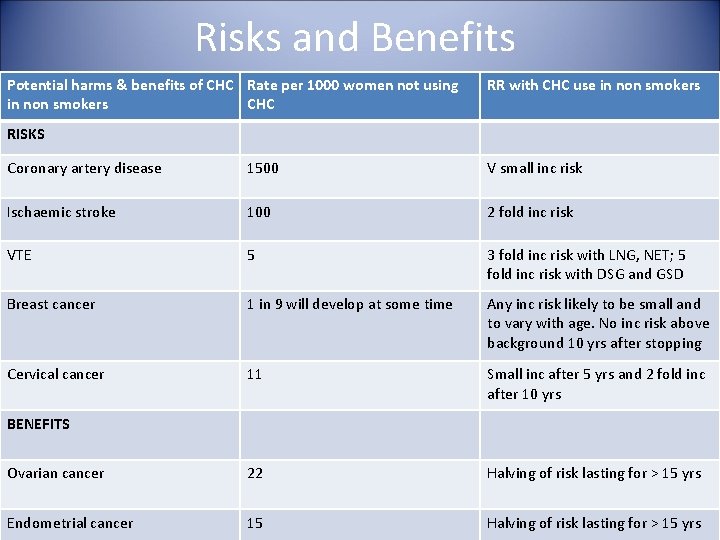
Risks and Benefits Potential harms & benefits of CHC Rate per 1000 women not using in non smokers CHC RR with CHC use in non smokers RISKS Coronary artery disease 1500 V small inc risk Ischaemic stroke 100 2 fold inc risk VTE 5 3 fold inc risk with LNG, NET; 5 fold inc risk with DSG and GSD Breast cancer 1 in 9 will develop at some time Any inc risk likely to be small and to vary with age. No inc risk above background 10 yrs after stopping Cervical cancer 11 Small inc after 5 yrs and 2 fold inc after 10 yrs Ovarian cancer 22 Halving of risk lasting for > 15 yrs Endometrial cancer 15 Halving of risk lasting for > 15 yrs BENEFITS
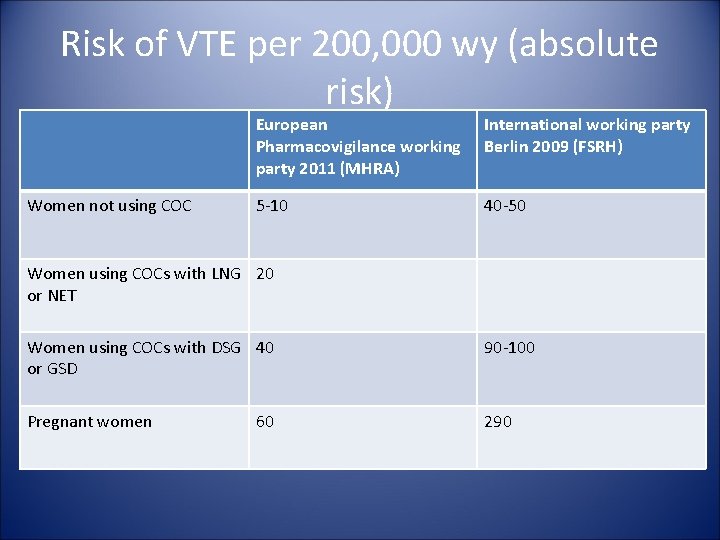
Risk of VTE per 200, 000 wy (absolute risk) Women not using COC European Pharmacovigilance working party 2011 (MHRA) International working party Berlin 2009 (FSRH) 5 -10 40 -50 Women using COCs with LNG 20 or NET Women using COCs with DSG 40 or GSD 90 -100 Pregnant women 290 60
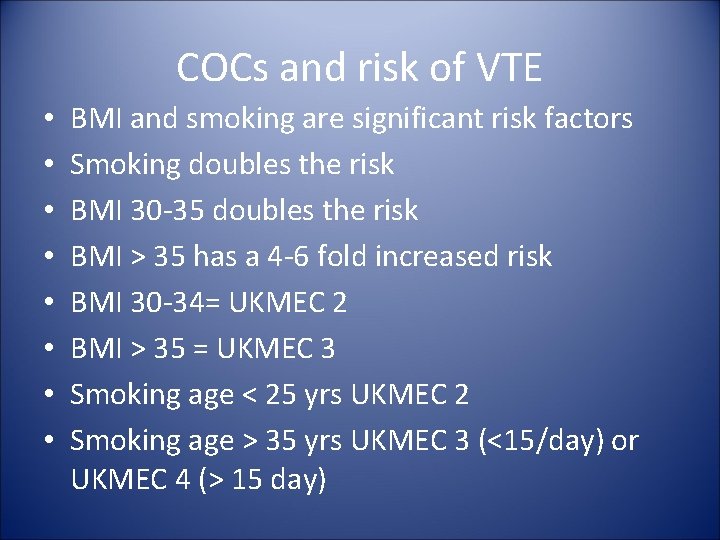
COCs and risk of VTE • • BMI and smoking are significant risk factors Smoking doubles the risk BMI 30 -35 doubles the risk BMI > 35 has a 4 -6 fold increased risk BMI 30 -34= UKMEC 2 BMI > 35 = UKMEC 3 Smoking age < 25 yrs UKMEC 2 Smoking age > 35 yrs UKMEC 3 (<15/day) or UKMEC 4 (> 15 day)
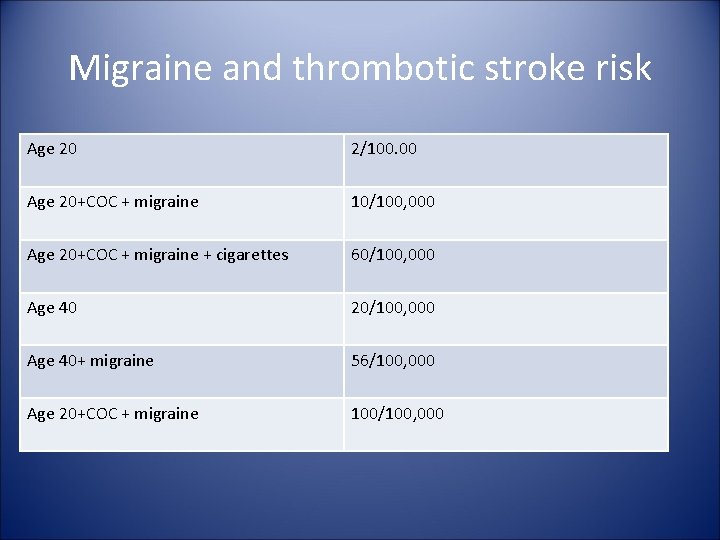
Migraine and thrombotic stroke risk Age 20 2/100. 00 Age 20+COC + migraine 10/100, 000 Age 20+COC + migraine + cigarettes 60/100, 000 Age 40 20/100, 000 Age 40+ migraine 56/100, 000 Age 20+COC + migraine 100/100, 000
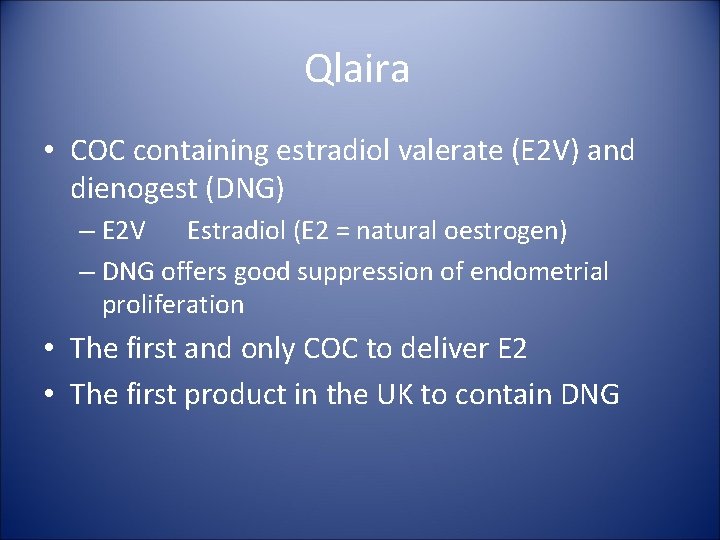
Qlaira • COC containing estradiol valerate (E 2 V) and dienogest (DNG) – E 2 V Estradiol (E 2 = natural oestrogen) – DNG offers good suppression of endometrial proliferation • The first and only COC to deliver E 2 • The first product in the UK to contain DNG
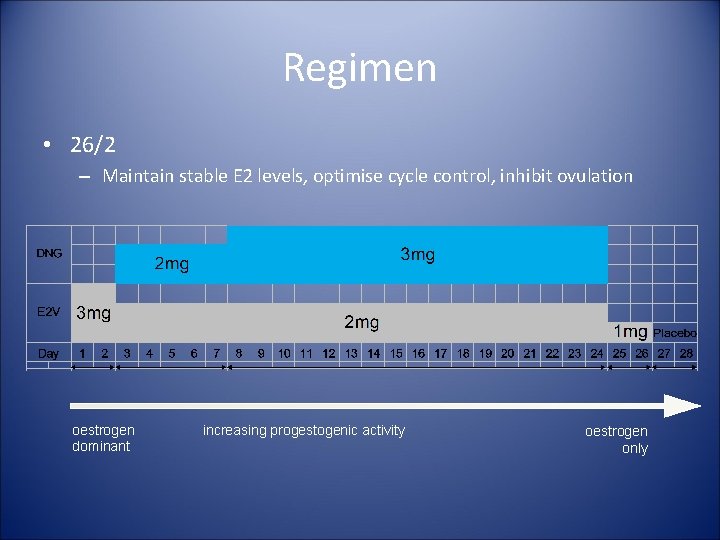
Regimen • 26/2 – Maintain stable E 2 levels, optimise cycle control, inhibit ovulation oestrogen dominant increasing progestogenic activity oestrogen only
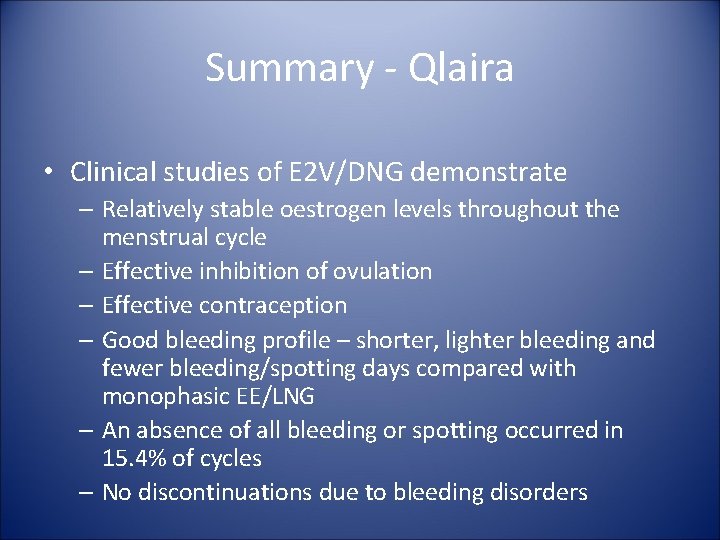
Summary - Qlaira • Clinical studies of E 2 V/DNG demonstrate – Relatively stable oestrogen levels throughout the menstrual cycle – Effective inhibition of ovulation – Effective contraception – Good bleeding profile – shorter, lighter bleeding and fewer bleeding/spotting days compared with monophasic EE/LNG – An absence of all bleeding or spotting occurred in 15. 4% of cycles – No discontinuations due to bleeding disorders
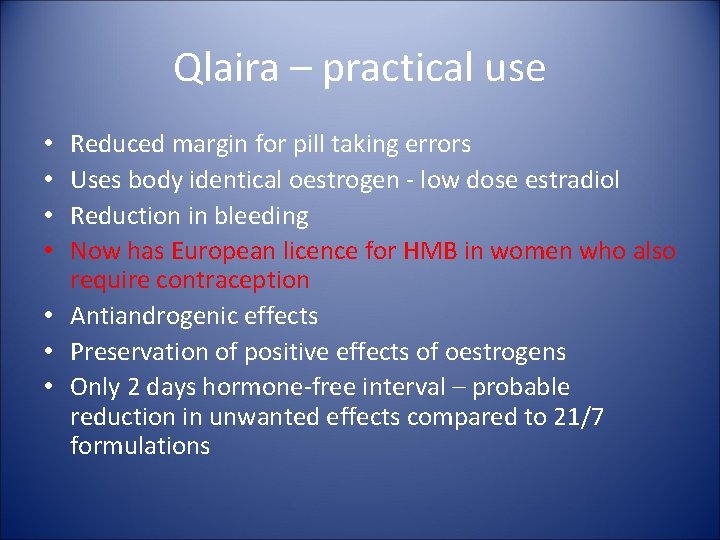
Qlaira – practical use Reduced margin for pill taking errors Uses body identical oestrogen - low dose estradiol Reduction in bleeding Now has European licence for HMB in women who also require contraception • Antiandrogenic effects • Preservation of positive effects of oestrogens • Only 2 days hormone-free interval – probable reduction in unwanted effects compared to 21/7 formulations • •
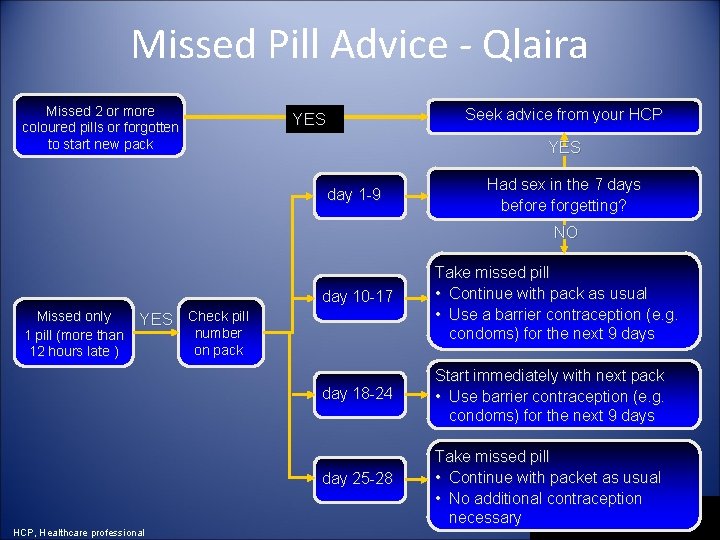
Missed Pill Advice - Qlaira Missed 2 or more coloured pills or forgotten to start new pack Seek advice from your HCP YES day 1 -9 Had sex in the 7 days before forgetting? NO Missed only 1 pill (more than 12 hours late ) day 10 -17 Take missed pill • Continue with pack as usual • Use a barrier contraception (e. g. condoms) for the next 9 days day 18 -24 Start immediately with next pack • Use barrier contraception (e. g. condoms) for the next 9 days YES Check pill number on pack day 25 -28 HCP, Healthcare professional Take missed pill • Continue with packet as usual • No additional contraception necessary
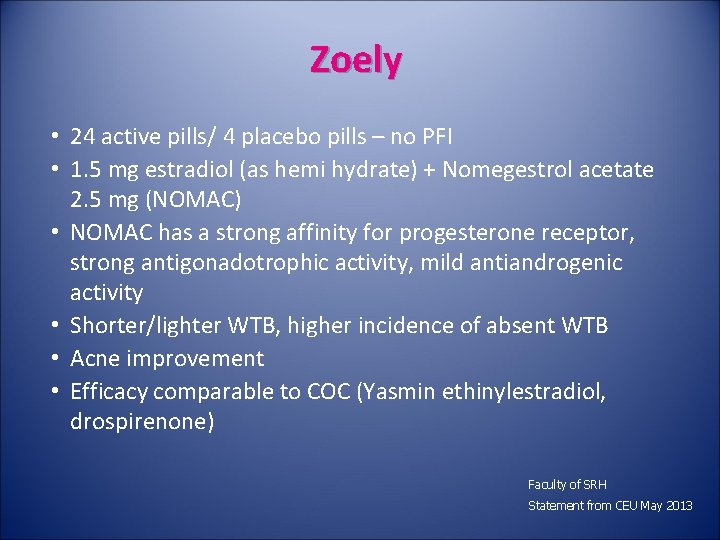
Zoely • 24 active pills/ 4 placebo pills – no PFI • 1. 5 mg estradiol (as hemi hydrate) + Nomegestrol acetate 2. 5 mg (NOMAC) • NOMAC has a strong affinity for progesterone receptor, strong antigonadotrophic activity, mild antiandrogenic activity • Shorter/lighter WTB, higher incidence of absent WTB • Acne improvement • Efficacy comparable to COC (Yasmin ethinylestradiol, drospirenone) Faculty of SRH Statement from CEU May 2013
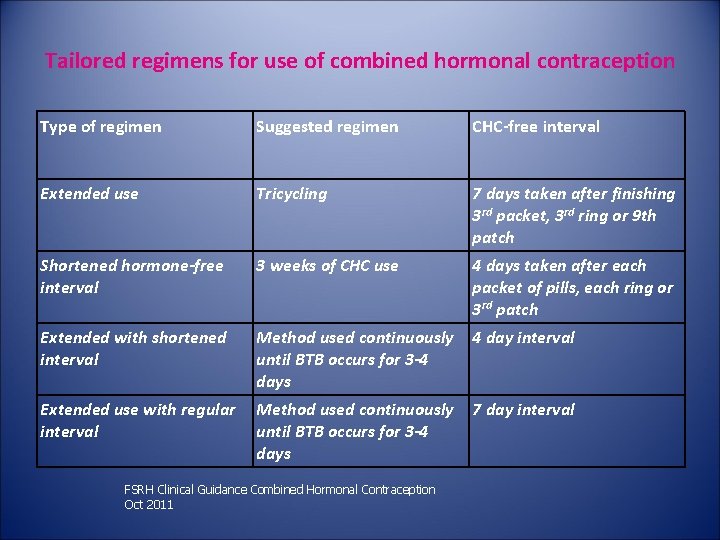
Tailored regimens for use of combined hormonal contraception Type of regimen Suggested regimen CHC-free interval Extended use Tricycling 7 days taken after finishing 3 rd packet, 3 rd ring or 9 th patch Shortened hormone-free interval 3 weeks of CHC use 4 days taken after each packet of pills, each ring or 3 rd patch Extended with shortened interval Method used continuously until BTB occurs for 3 -4 days 4 day interval Extended use with regular interval Method used continuously until BTB occurs for 3 -4 days 7 day interval FSRH Clinical Guidance Combined Hormonal Contraception Oct 2011
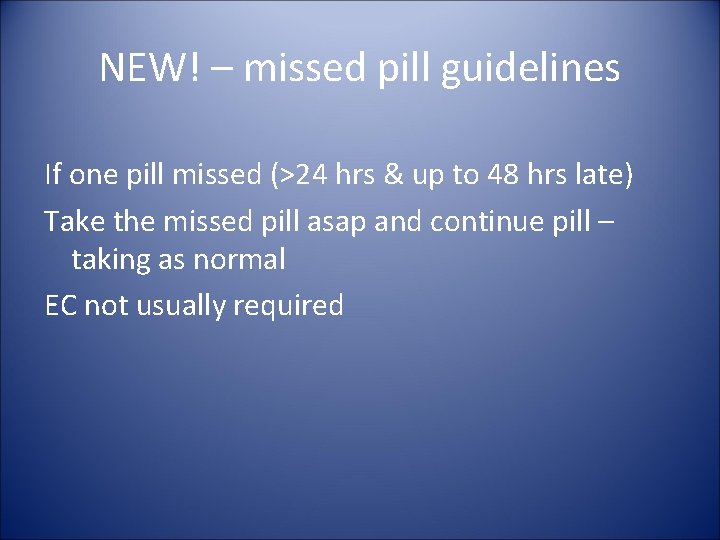
NEW! – missed pill guidelines If one pill missed (>24 hrs & up to 48 hrs late) Take the missed pill asap and continue pill – taking as normal EC not usually required
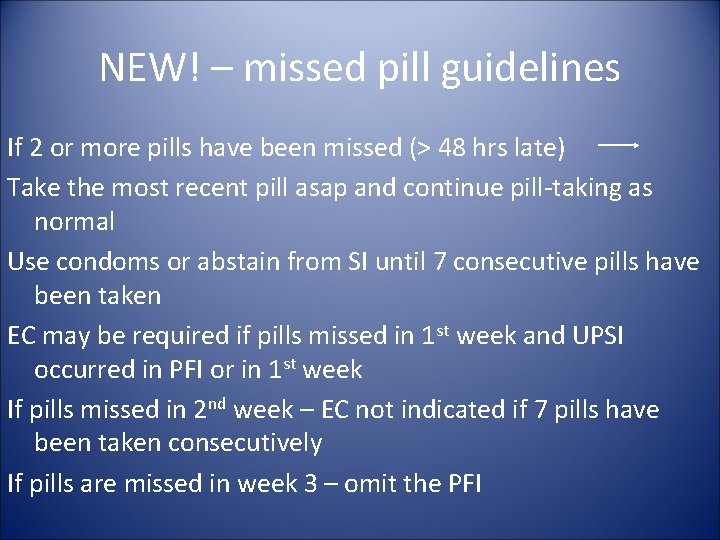
NEW! – missed pill guidelines If 2 or more pills have been missed (> 48 hrs late) Take the most recent pill asap and continue pill-taking as normal Use condoms or abstain from SI until 7 consecutive pills have been taken EC may be required if pills missed in 1 st week and UPSI occurred in PFI or in 1 st week If pills missed in 2 nd week – EC not indicated if 7 pills have been taken consecutively If pills are missed in week 3 – omit the PFI
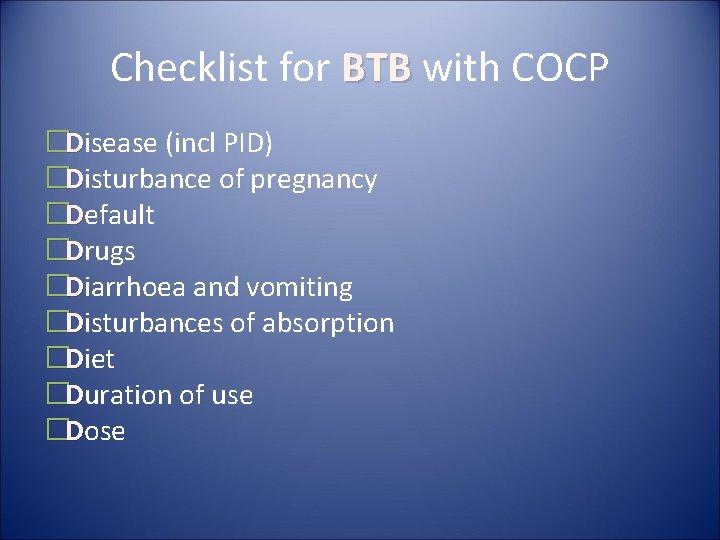
Checklist for BTB with COCP �Disease (incl PID) �Disturbance of pregnancy �Default �Drugs �Diarrhoea and vomiting �Disturbances of absorption �Diet �Duration of use �Dose
CEU 2011 Drug interactions and hormonal contraception • Additional precautions NO longer required when using nonenzyme inducing antibiotics with CHC • All women on enzyme inducing drugs should be advised to use methods unaffected by those drugs – Cu-IUD; IUS; Injectables • CHC not recommended in women on Lamotrigine monotherapy (inc risk of seizures) • UPA not recommended while using enzyme inducers or within 28 days • UPA not recommended while breast feeding • UPA may reduce efficacy of other hormonal contraception - so abstinence for 5 days and then additional contraception for 7 days (pill, ring, patch, implant, injectable); 9 days (Qlaira); 2 days POP
Quick starting contraception!!! Criteria for excluding pregnancy: • No SI since last menses • Is correctly and consistently using a reliable method • Is within 7 days of onset of menses • Is within 4 weeks postpartum and not breast feeding • Is fully or nearly fully breast feeding, amenorrhoeic and < 6 months postpartum
Conclusion - 2016 • In 2016, more choice than ever before! • Different combinations, doses and delivery systems may be associated with different effects • Choice of hormonal contraception can be tailored based on the patient’s previous experience and risk profile • Appropriate contraception can offer significant health benefits to women and improve QOL • Appropriate counselling is vital to encourage continuation
- Slides: 36