COMA BRAIN DEATH Anesthesia and Intensive Care chair
COMA BRAIN DEATH Anesthesia and Intensive Care chair nr. 1 “Valeriu Ghereg” Coordinator of Anesthesia and Intensive Care programs CUSIM Svetlana Plamadeala, MD, Ph. D, associate professor
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
Aim of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
Reticular activating system Wakefulness Sleep state
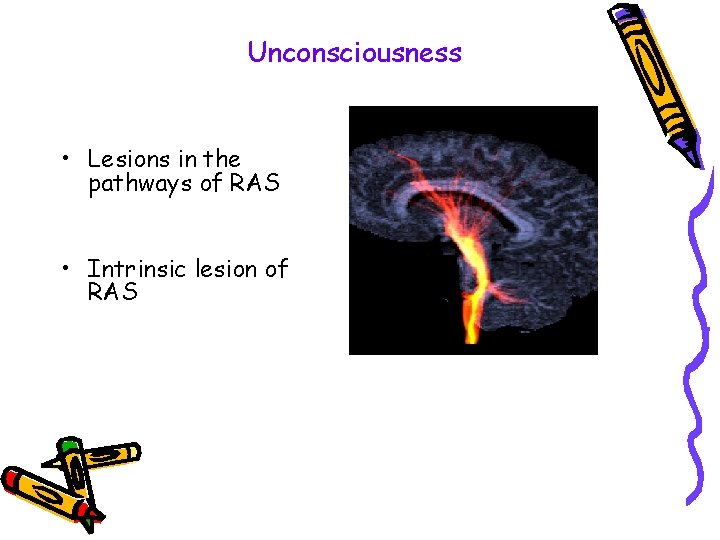
Unconsciousness • Lesions in the pathways of RAS • Intrinsic lesion of RAS
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
Levels of consciousness disturbance • Drowsiness (lethargy) • Stupor • Coma
Coma • State of unresponsiveness • Lack of alertness
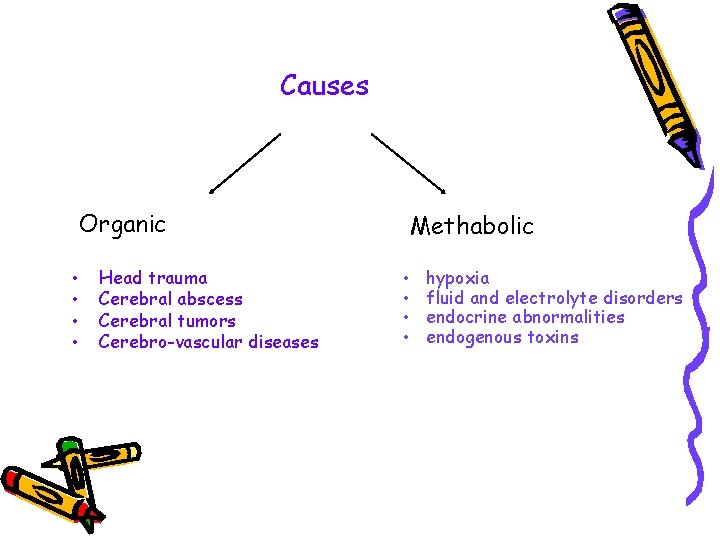
Causes Organic • • Head trauma Cerebral abscess Cerebral tumors Cerebro-vascular diseases Methabolic • • hypoxia fluid and electrolyte disorders endocrine abnormalities endogenous toxins
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
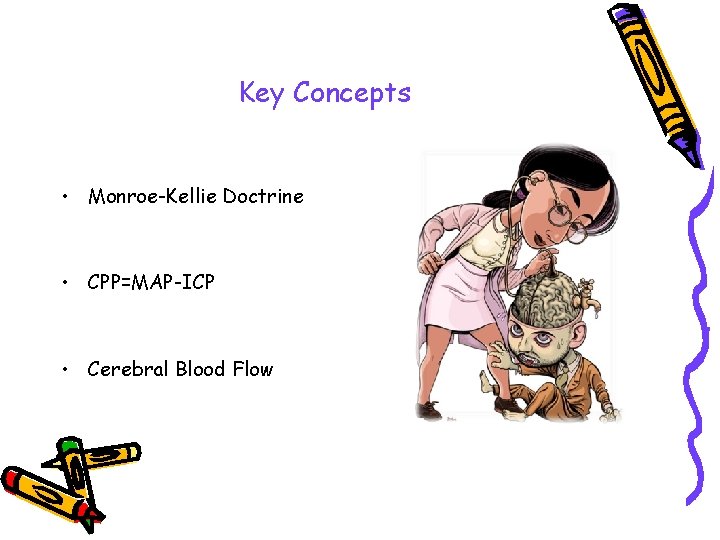
Key Concepts • Monroe-Kellie Doctrine • CPP=MAP-ICP • Cerebral Blood Flow
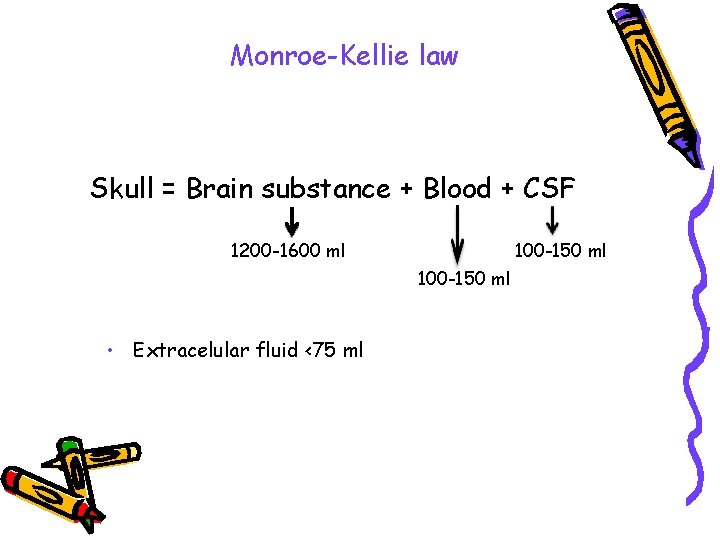
Monroe-Kellie law Skull = Brain substance + Blood + CSF 1200 -1600 ml 100 -150 ml • Extracelular fluid <75 ml
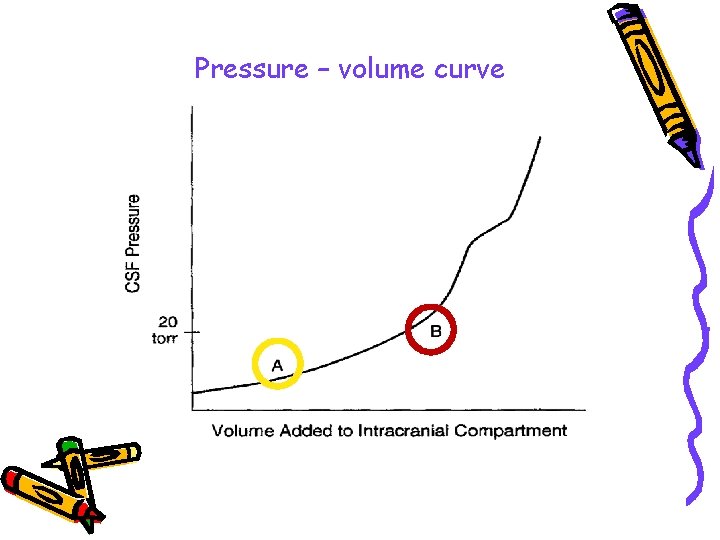
Pressure – volume curve
CPP = MAP - ICP • MAP = (s. BP + 2 d. BP)/3 • ICP keep < 20 mm. Hg • CPP > 60 mm. Hg (50 -70 mm. Hg)
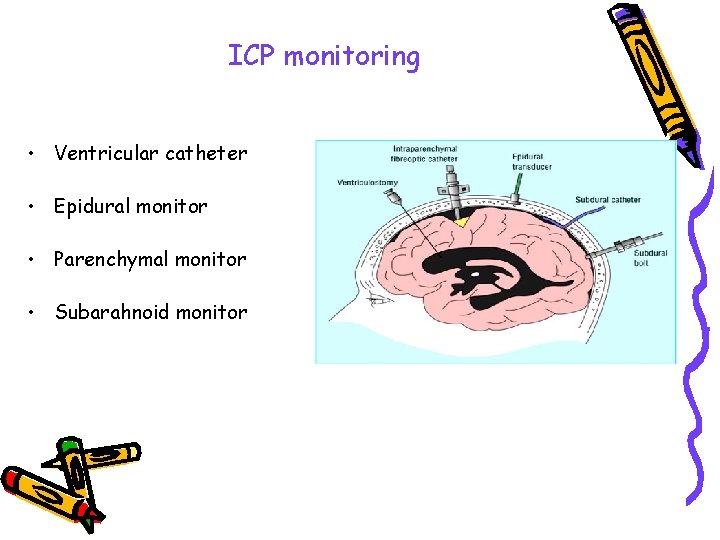
ICP monitoring • Ventricular catheter • Epidural monitor • Parenchymal monitor • Subarahnoid monitor
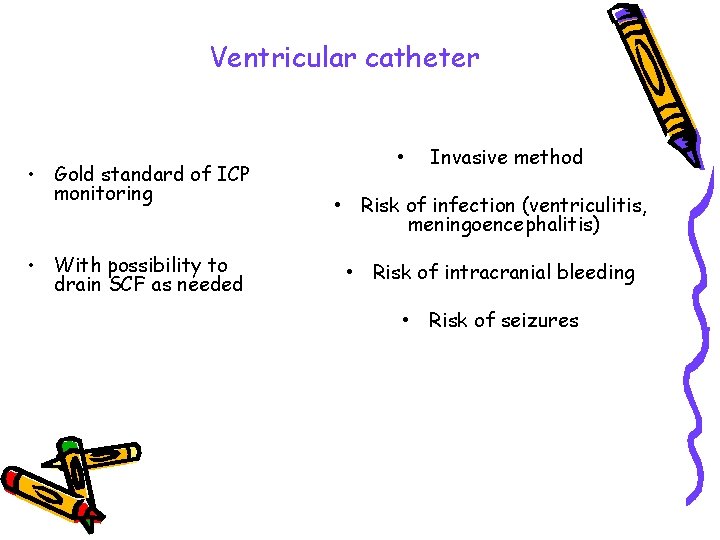
Ventricular catheter • Gold standard of ICP monitoring • With possibility to drain SCF as needed • Invasive method • Risk of infection (ventriculitis, meningoencephalitis) • Risk of intracranial bleeding • Risk of seizures
Cerebral blood flow • Blood pressure • Pa. CO 2 • Pa. O 2
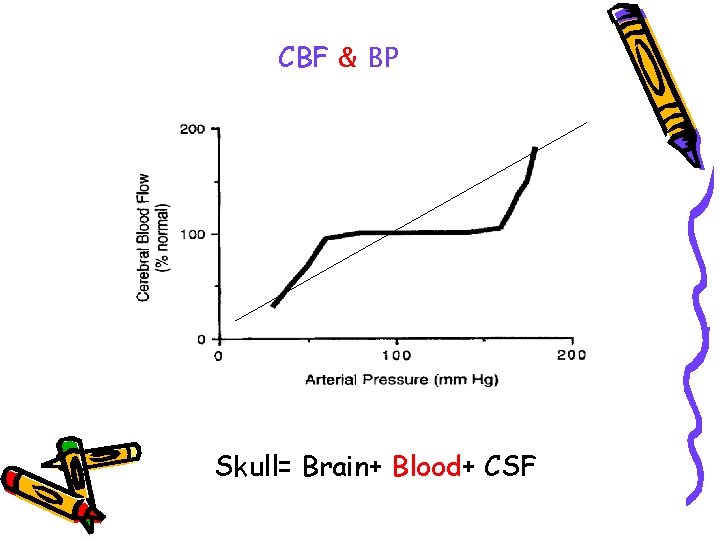
CBF & BP Skull= Brain+ Blood+ CSF
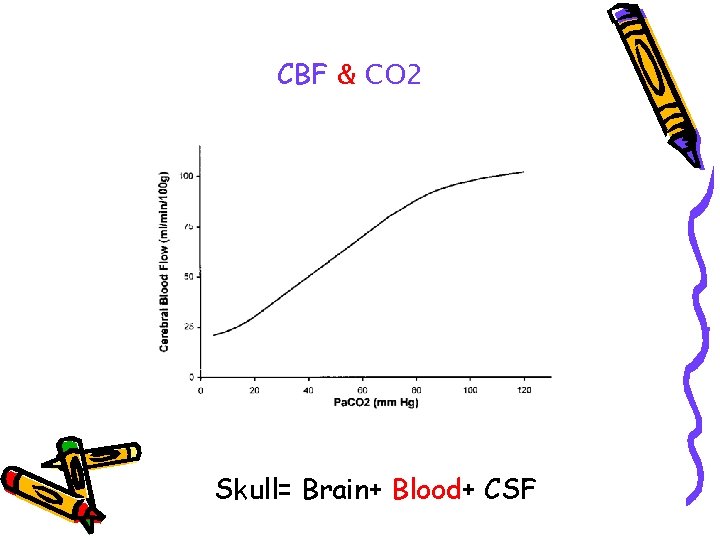
CBF & CO 2 Skull= Brain+ Blood+ CSF
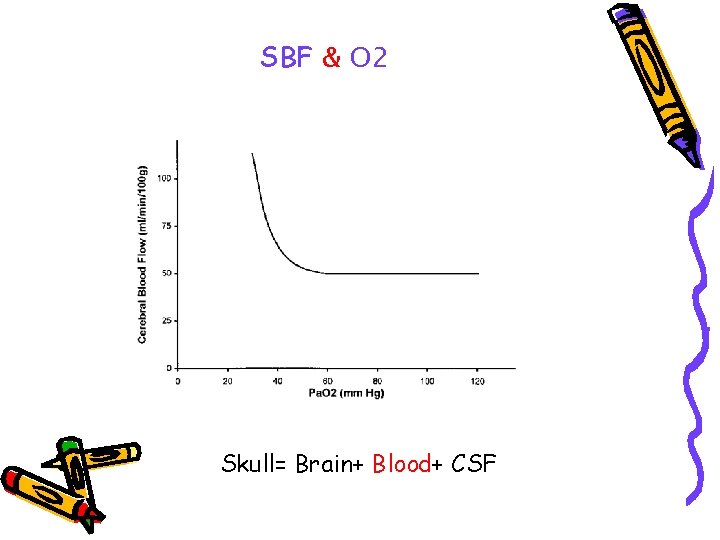
SBF & O 2 Skull= Brain+ Blood+ CSF
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
Cerebral edema increases in brain of water content • Vazogenic edema • Cytotoxic edema
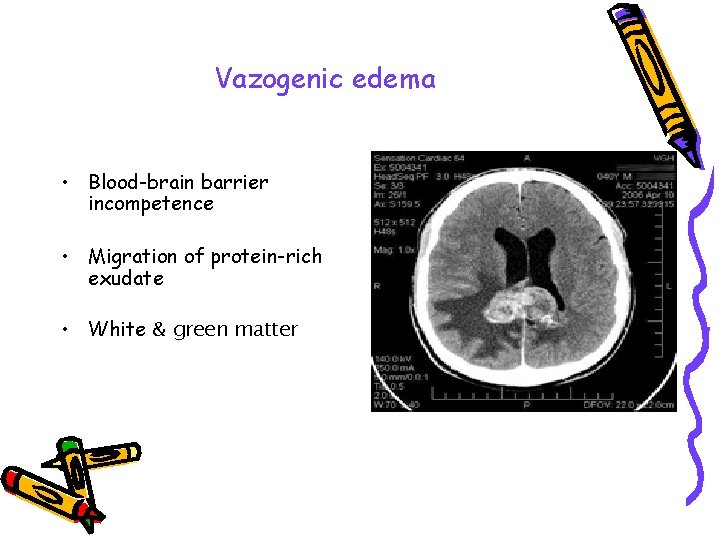
Vazogenic edema • Blood-brain barrier incompetence • Migration of protein-rich exudate • White & green matter
Vazogenic edema • Cerebral tumors • Abscess • Head trauma • Meningitis • Cerebral stroke (ischemic, hemorrhagic) NB. Corticosteroids demonstrate effectiveness
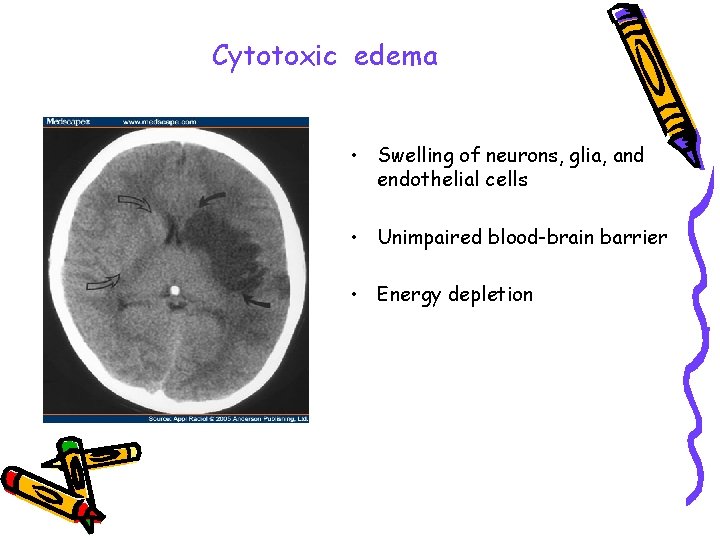
Cytotoxic edema • Swelling of neurons, glia, and endothelial cells • Unimpaired blood-brain barrier • Energy depletion
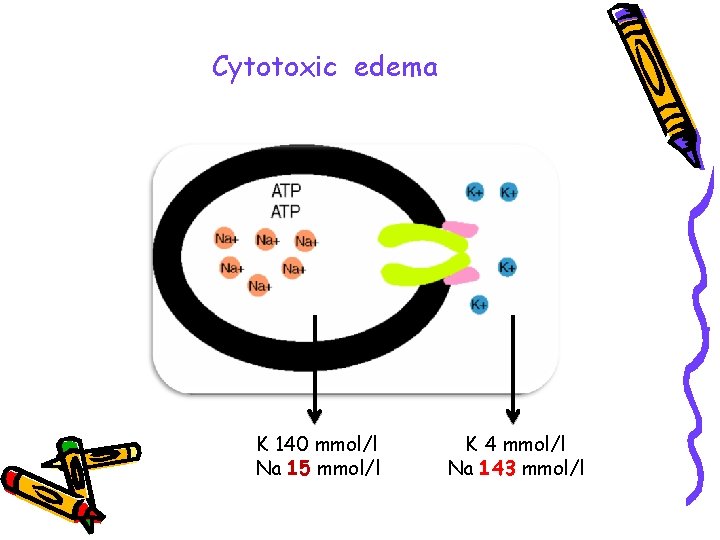
Cytotoxic edema K 140 mmol/l Na 15 mmol/l K 4 mmol/l Na 143 mmol/l
Cytotoxic edema Hypoperfusion - the first cause NB. Effective – osmotic agents
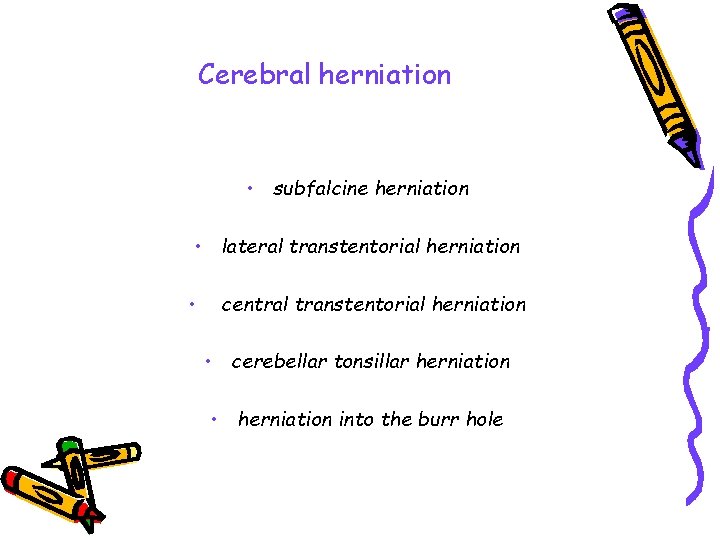
Cerebral herniation • subfalcine herniation • lateral transtentorial herniation • central transtentorial herniation • cerebellar tonsillar herniation • herniation into the burr hole
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
Acute depression in level of consciousness is a critical, lifethreatening emergency that requires a complex systemic aproach
Coma-patient examination ABCDE approach: A –airway B – breathing C – circulation D – disability E – exposure Neurologic examination (advanced)
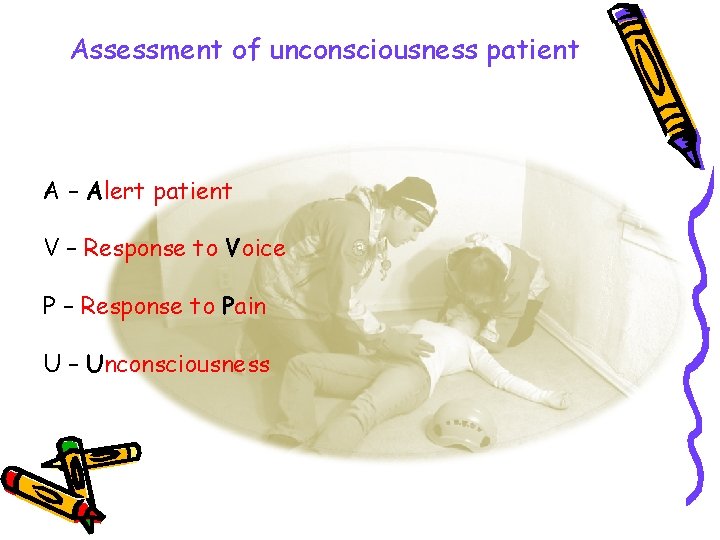
Assessment of unconsciousness patient A – Alert patient V – Response to Voice P – Response to Pain U – Unconsciousness

HILTON GARDEN IN GLASGOW SITY
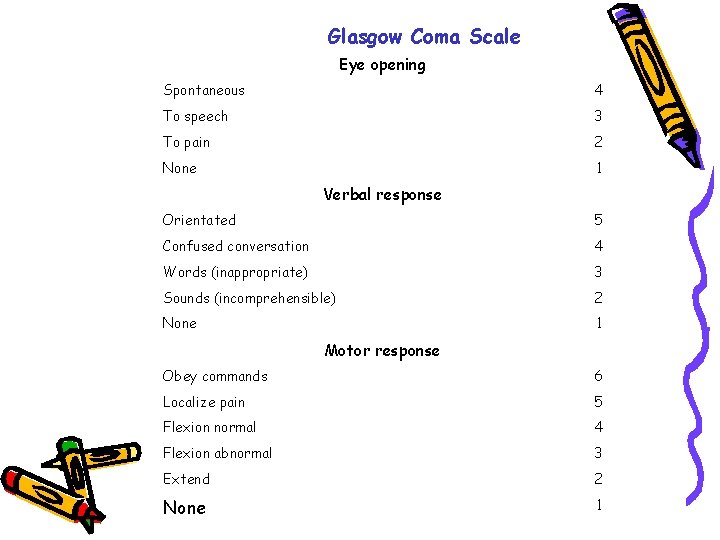
Glasgow Coma Scale Eye opening Spontaneous 4 To speech 3 To pain 2 None 1 Verbal response Orientated 5 Confused conversation 4 Words (inappropriate) 3 Sounds (incomprehensible) 2 None 1 Motor response Obey commands 6 Localize pain 5 Flexion normal 4 Flexion abnormal 3 Extend 2 None 1
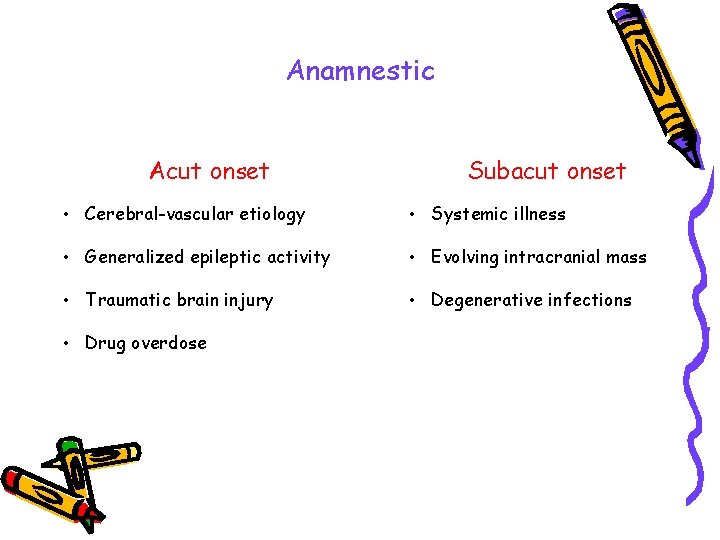
Anamnestic Acut onset Subacut onset • Cerebral-vascular etiology • Systemic illness • Generalized epileptic activity • Evolving intracranial mass • Traumatic brain injury • Degenerative infections • Drug overdose
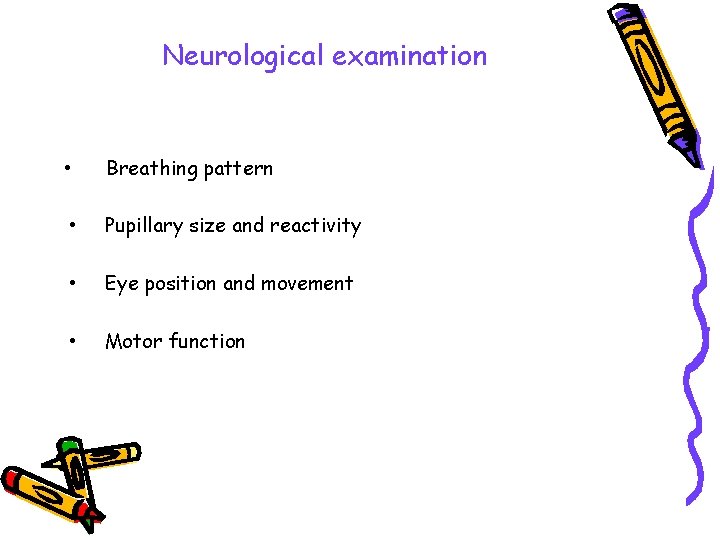
Neurological examination • Breathing pattern • Pupillary size and reactivity • Eye position and movement • Motor function
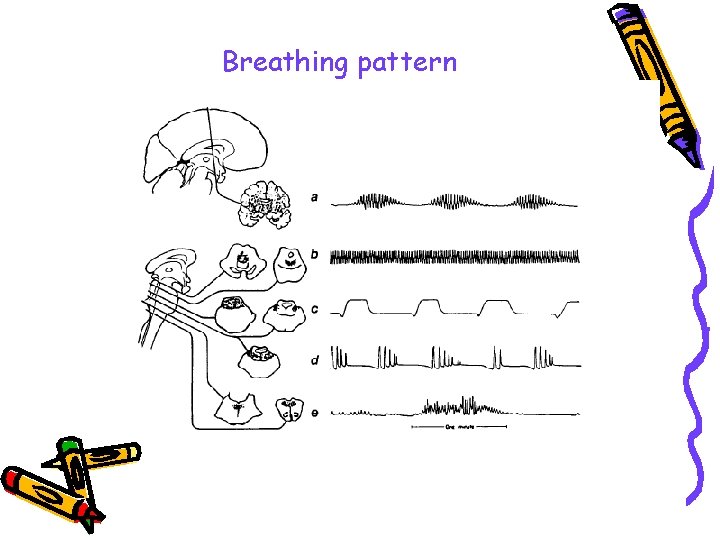
Breathing pattern
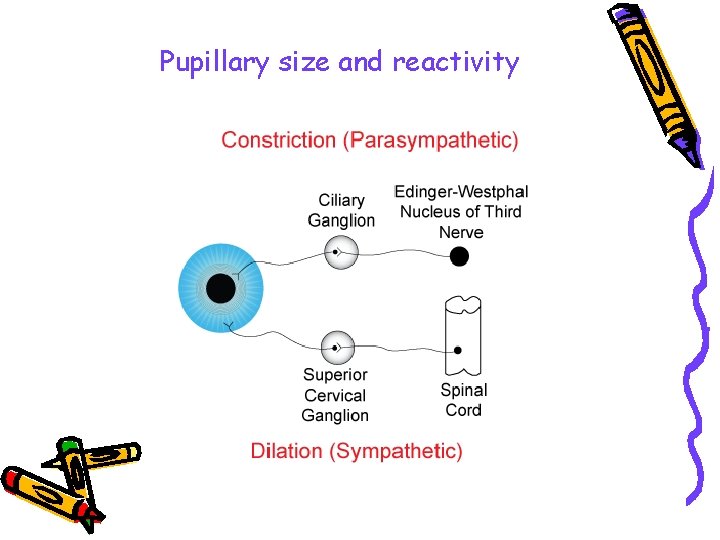
Pupillary size and reactivity
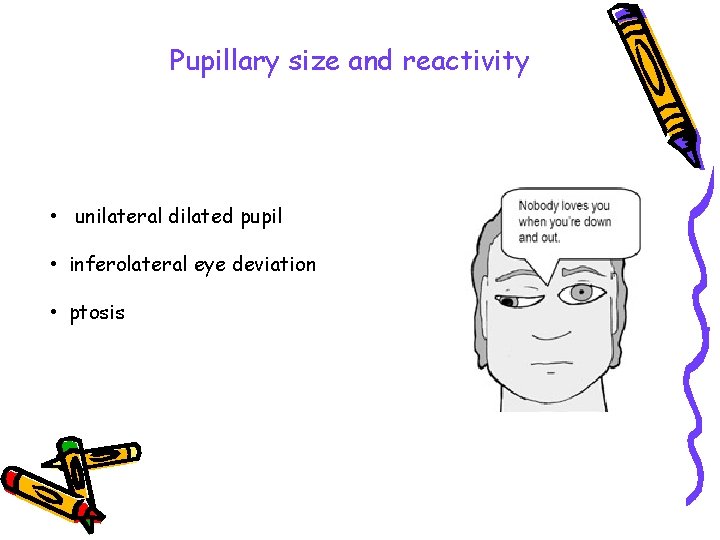
Pupillary size and reactivity • unilateral dilated pupil • inferolateral eye deviation • ptosis
Eye position and movement • Oculocephalic reflex • Oculovestibular reflex
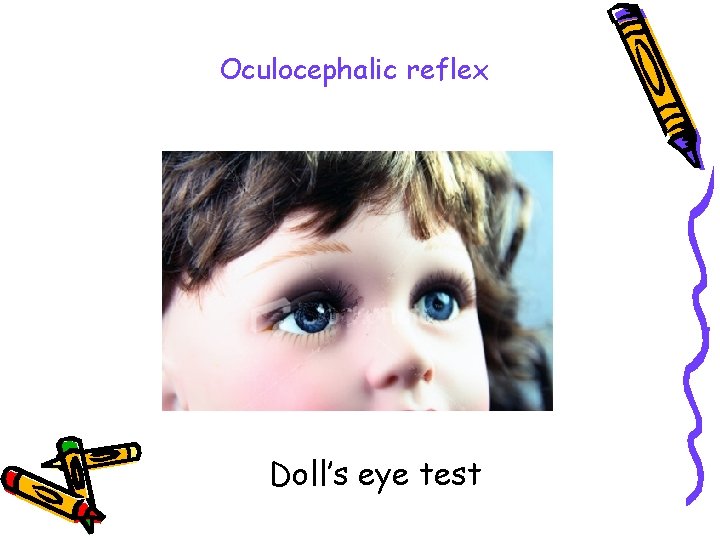
Oculocephalic reflex Doll’s eye test
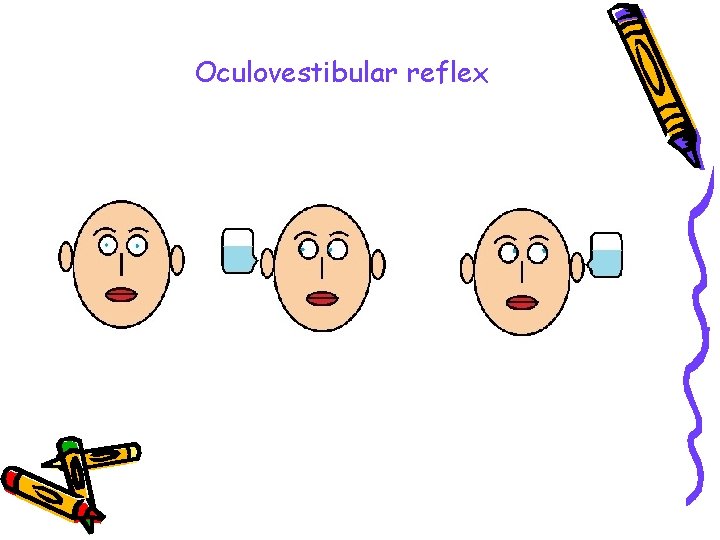
Oculovestibular reflex

Motor function
Paraclinical tests • CT scan • MRI • Lumbar puncture • EEG • Evoked potentials
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
Principles of neuro-intensive care Skull= Brain + Blood + CSF Control of cerebral metabolism
Skull= Brain + Blood + CSF Osmotic therapy • Manitol • 3% Na. Cl
Skull= Brain + Blood + CSF • Patient position • Temperature control • Control of Blood Pressure • Sedation/analgezia/ventilation • Control of (PEEP)
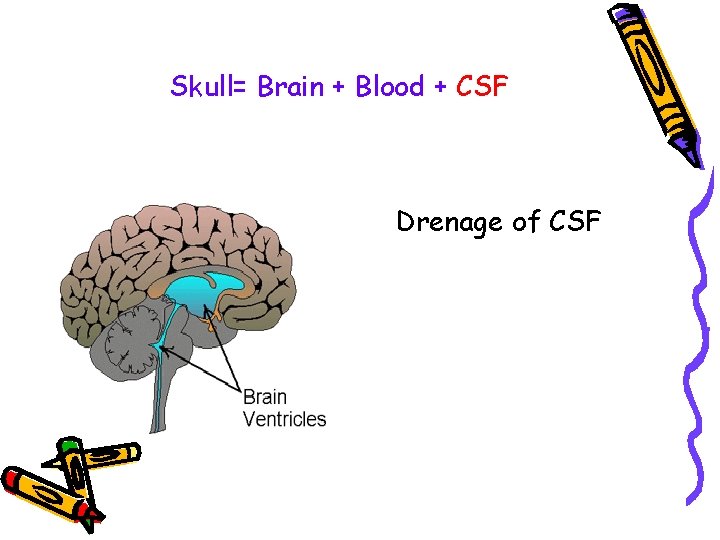
Skull= Brain + Blood + CSF Drenage of CSF
Loop diuretic • Potentiates osmotic effect • Reduces ICP by means of the flowing effects: • Increasing of osmotic gradient • Reducing of CSF production • Reducing of the cerebral water compartment Skull= Brain + Blood + CSF
Control of cerebral metabolism • Control of seizure activity • Barbituric coma • Hipothermia
Uncontrolled ICP
Aims of the course • • Neurophysiology of coma Causes and levels of consciousness disturbances Key concepts of neuro-intensive care Cerebral edema Assessment of unconsciousness patient Principles of neuro-intensive care State into which coma resolve Brain death
State into which coma resolve • Vegetative state • Akinetic mutism • “Locked in“ syndrome
Vegetative state • State of wakefulness • Undetectable awareness
Akinetic mutism A person with akinetic mutism has "sleep-waking cycles but, when apparently awake, with eyes open, lies mute, immobile and unresponsive
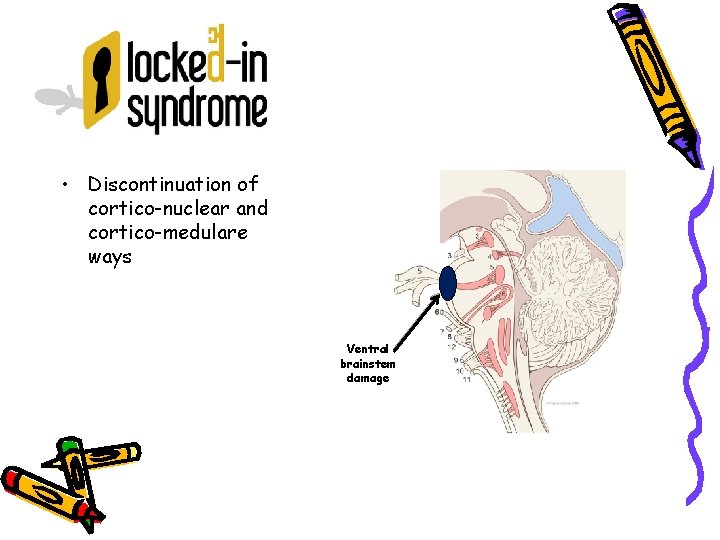
• Discontinuation of cortico-nuclear and cortico-medulare ways Ventral brainstem damage

“Locked in“ syndrome Le scaphandre et le papillion
Brain death Brain injury with unreversible cessation of the brain and brain stem functions
Brain death The medical and legal definitions of death: brain death & cardiac death are the same.
Summary • Cerebral injury primary/secondary • Secondary cerebral injuries – preventable • Skull= Brain + Blood + CSF • CPP > 60 mm. Hg
- Slides: 62