Coma and Glasgow coma scale Critical care medicine

- Slides: 15
Coma and Glasgow coma scale Critical care medicine 2 ed year Dr. Warda Ramadan Lecturer of Critical care& Emergency Nursing
Coma and Glasgow coma scale n Def : Coma is unarousable unresponsiveness. Quantify using Glasgow coma scale.
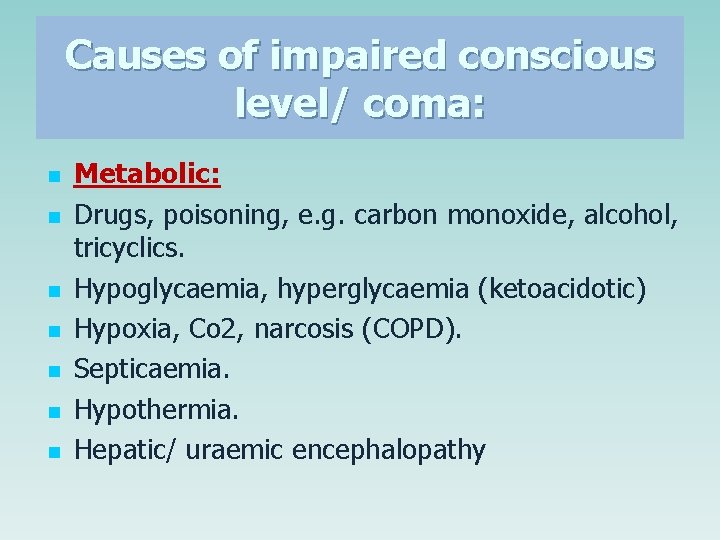
Causes of impaired conscious level/ coma: n n n n Metabolic: Drugs, poisoning, e. g. carbon monoxide, alcohol, tricyclics. Hypoglycaemia, hyperglycaemia (ketoacidotic) Hypoxia, Co 2, narcosis (COPD). Septicaemia. Hypothermia. Hepatic/ uraemic encephalopathy
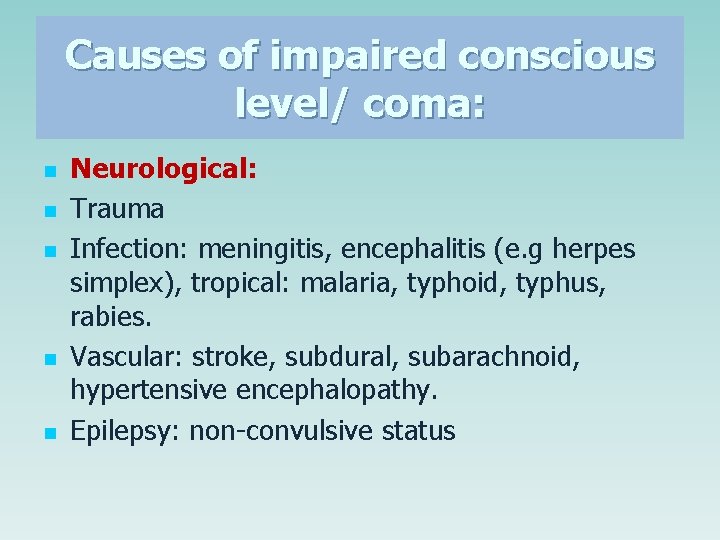
Causes of impaired conscious level/ coma: n n n Neurological: Trauma Infection: meningitis, encephalitis (e. g herpes simplex), tropical: malaria, typhoid, typhus, rabies. Vascular: stroke, subdural, subarachnoid, hypertensive encephalopathy. Epilepsy: non-convulsive status
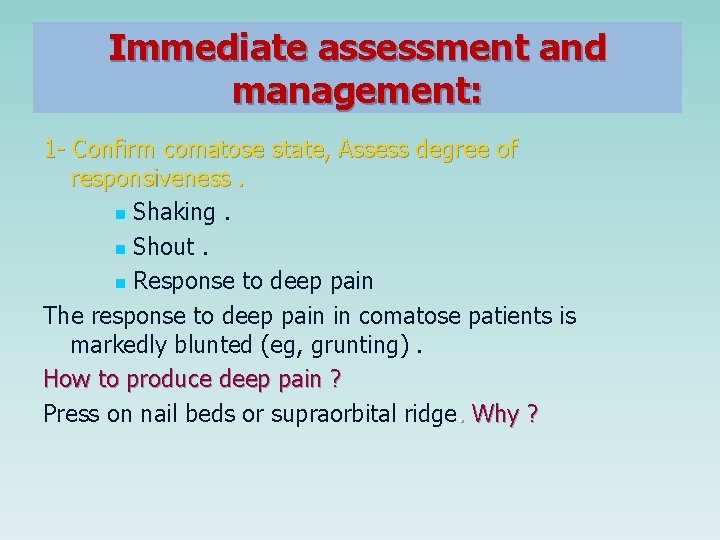
Immediate assessment and management: 1 - Confirm comatose state, Assess degree of responsiveness. n Shaking. n Shout. n Response to deep pain The response to deep pain in comatose patients is markedly blunted (eg, grunting). How to produce deep pain ? Press on nail beds or supraorbital ridge. Why ?
*Immediate management: n n Assess airway, breathing, and circulation. Consider intubation if GCS < 8. Support the circulation if required (i. e. IV fluids).
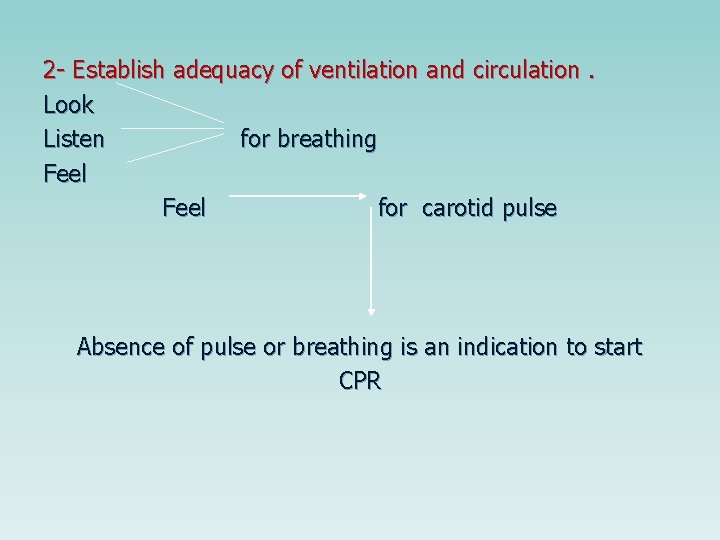
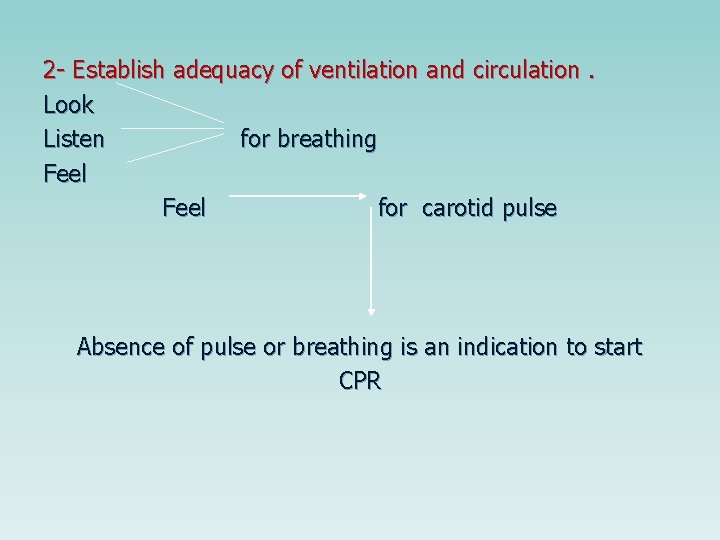
2 - Establish adequacy of ventilation and circulation. Look Listen for breathing Feel for carotid pulse Absence of pulse or breathing is an indication to start CPR
3 - Secure airway. Even if adequate spontaneous ventilation is occurring, it is usually wise to safeguard the airway by rolling the patient onto one side or inserting a nasal or oral airway. 4 - Insert intravenous cannula into upper extremity. n Large – bore cannula (≥ 16 gauze) or use a large – bore needle secure it in place for later us n obtain sufficient blood samples
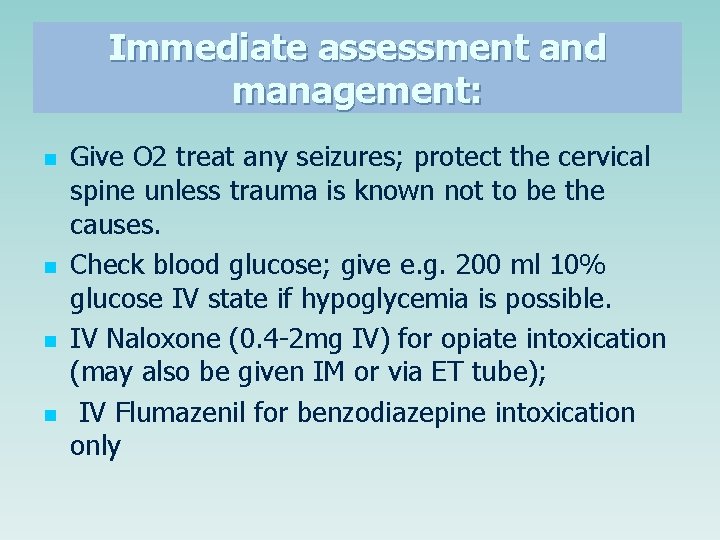
Immediate assessment and management: n n Give O 2 treat any seizures; protect the cervical spine unless trauma is known not to be the causes. Check blood glucose; give e. g. 200 ml 10% glucose IV state if hypoglycemia is possible. IV Naloxone (0. 4 -2 mg IV) for opiate intoxication (may also be given IM or via ET tube); IV Flumazenil for benzodiazepine intoxication only
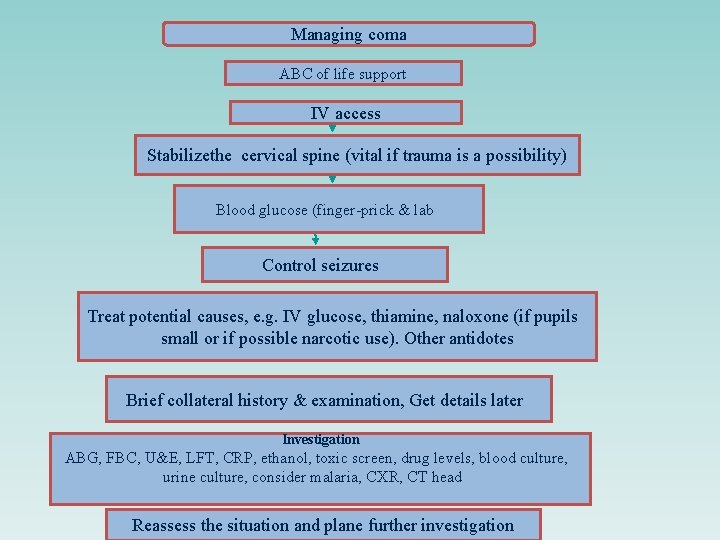
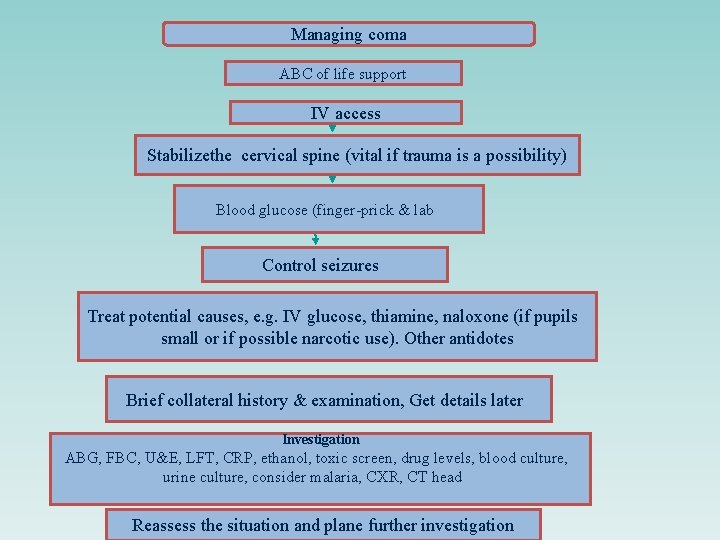
Managing coma ABC of life support IV access Stabilizethe cervical spine (vital if trauma is a possibility) Blood glucose (finger-prick & lab Control seizures Treat potential causes, e. g. IV glucose, thiamine, naloxone (if pupils small or if possible narcotic use). Other antidotes Brief collateral history & examination, Get details later Investigation ABG, FBC, U&E, LFT, CRP, ethanol, toxic screen, drug levels, blood culture, urine culture, consider malaria, CXR, CT head Reassess the situation and plane further investigation
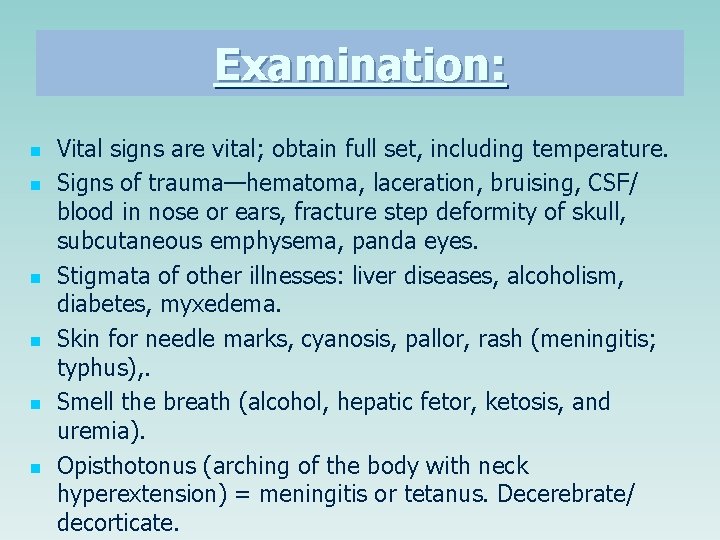
Examination: n n n Vital signs are vital; obtain full set, including temperature. Signs of trauma—hematoma, laceration, bruising, CSF/ blood in nose or ears, fracture step deformity of skull, subcutaneous emphysema, panda eyes. Stigmata of other illnesses: liver diseases, alcoholism, diabetes, myxedema. Skin for needle marks, cyanosis, pallor, rash (meningitis; typhus), . Smell the breath (alcohol, hepatic fetor, ketosis, and uremia). Opisthotonus (arching of the body with neck hyperextension) = meningitis or tetanus. Decerebrate/ decorticate.
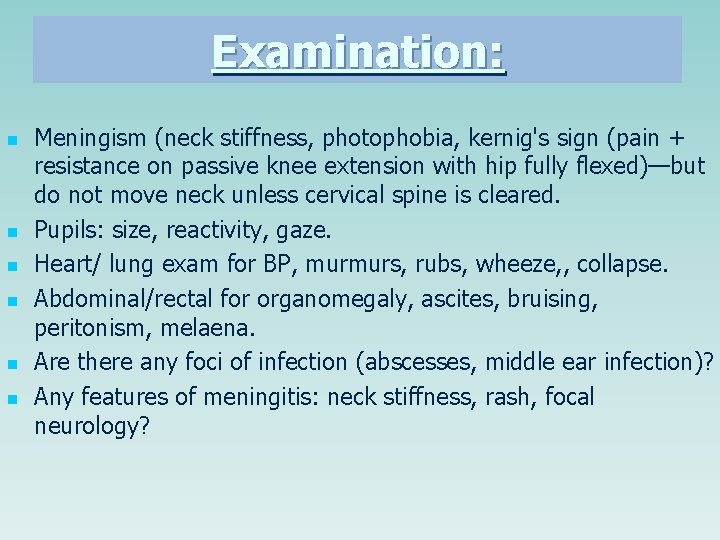
Examination: n n n Meningism (neck stiffness, photophobia, kernig's sign (pain + resistance on passive knee extension with hip fully flexed)—but do not move neck unless cervical spine is cleared. Pupils: size, reactivity, gaze. Heart/ lung exam for BP, murmurs, rubs, wheeze, , collapse. Abdominal/rectal for organomegaly, ascites, bruising, peritonism, melaena. Are there any foci of infection (abscesses, middle ear infection)? Any features of meningitis: neck stiffness, rash, focal neurology?
Quick history: n n n n From family, ambulance staff, bystanders: abrupt or gradual onset? How found—suicide note, seizure? If injured, suspect cervical spinal injury and do not move spine. Recent complaints—headache, fever, depression? Recent medical history—sinusitis, otitis, neurosurgery, any procedure? Past medical history—diabetes, asthma, high blood pressure, cancer, epilepsy, psychiatric illness? Drug or toxin exposure (especially alcohol or other recreational drugs) Any travel?
If the diagnosis is unclear: n n n Treat the treatable: O 2; naloxone as above; glucose (200 ml of 10% IV); Septic specifics: cefotaxime 2 g/12 h IV (meningitis), artemether/ quinine (malaria), aciclovir (encephalitis). Do routine biochemistry, hematology, thick films, blood cultures, blood ethanol, drug screen, etc. Arrange urgent CT head, if normal and no CI, proceed to LP. The diagnosis should now be clear, e. g hypo/hyperglycemia, alcohol excess, poisoning, uremia, pneumonia, hepatic encephalopathy, etc.
