Colposcopy and Pap Smear Triage Guidelines September 5
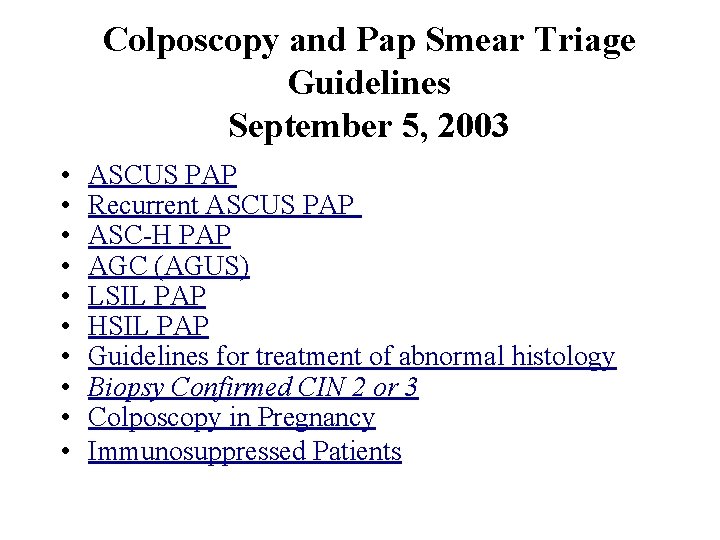
Colposcopy and Pap Smear Triage Guidelines September 5, 2003 • • • ASCUS PAP Recurrent ASCUS PAP ASC-H PAP AGC (AGUS) LSIL PAP HSIL PAP Guidelines for treatment of abnormal histology Biopsy Confirmed CIN 2 or 3 Colposcopy in Pregnancy Immunosuppressed Patients
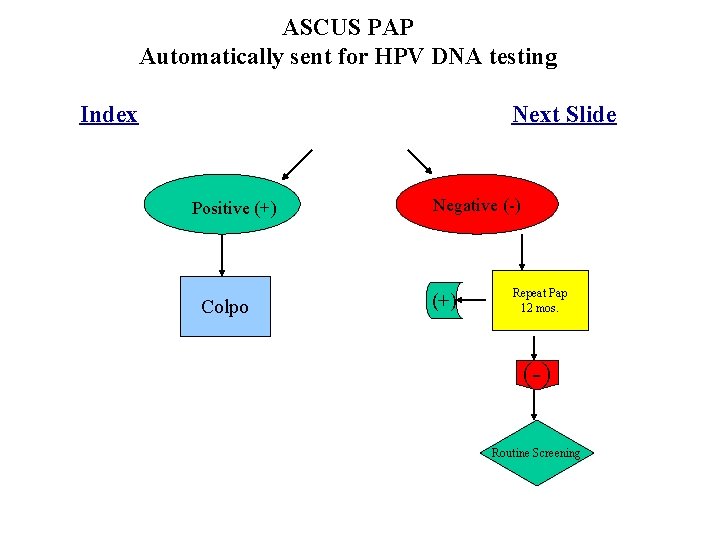
ASCUS PAP Automatically sent for HPV DNA testing Index Next Slide Positive (+) Colpo Negative (-) (+) Repeat Pap 12 mos. (-) Routine Screening

Colpo Normal CIN/CA Per ASCCP Guidelines HPV DNA 12 Mos. (-) Routine Screening =ACS or HPV+ Repeat Colpo For recurrent ASCUS with apparently normal colpo – bring in for colpo of vagina and vulva, as well as looking carefully for vaginitis. Empiric treatment of vaginitis is not recommended. For postmenopausal women (even on HRT) with ASCUS can consider treating with estrogen vaginal cream for two weeks, then discontinuing one week prior to repeat pap smear. If negative, repeat pap again after estrogen treatment in 4 -6 months. If negative again can resume routine screening. If>=ASC must send for colposcopy. Index Next Slide

ASC-H Pap Index Next Slide Colposcopy with ECC for all patients. Biopsy confirmed CIN No lesion identified Ask pathologist to review all specimens See following Guidelines No change HPV DNA @ 12 mos. Change in Dx: As per guidelines
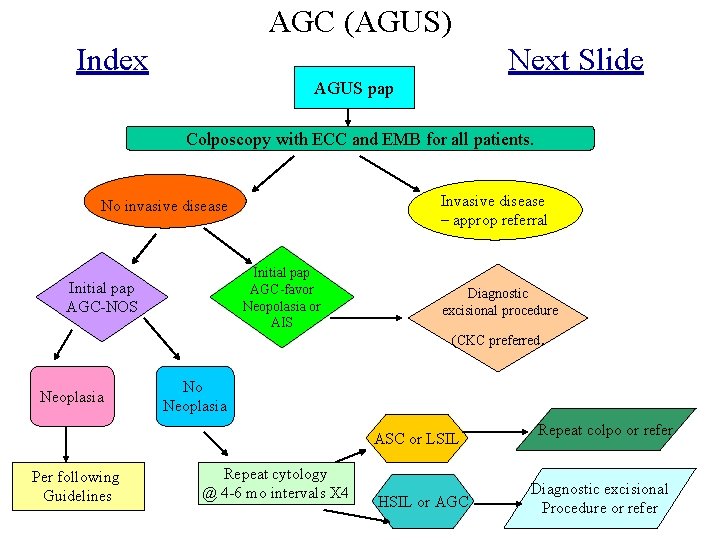
AGC (AGUS) Index Next Slide AGUS pap Colposcopy with ECC and EMB for all patients. Invasive disease – approp referral No invasive disease Initial pap AGC-favor Neopolasia or AIS Initial pap AGC-NOS Diagnostic excisional procedure (CKC preferred Neoplasia No Neoplasia ASC or LSIL Per following Guidelines . Repeat cytology @ 4 -6 mo intervals X 4 HSIL or AGC Repeat colpo or refer Diagnostic excisional Procedure or refer
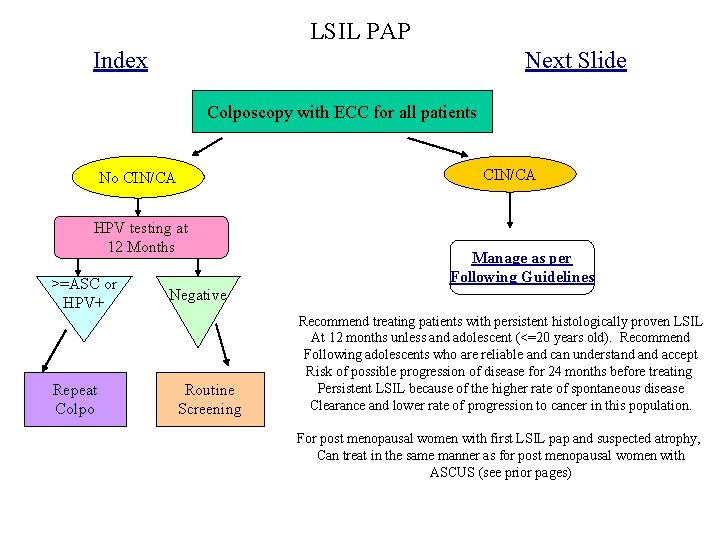
LSIL PAP Index Next Slide Colposcopy with ECC for all patients CIN/CA No CIN/CA HPV testing at 12 Months >=ASC or HPV+ Repeat Colpo Negative Routine Screening Manage as per Following Guidelines Recommend treating patients with persistent histologically proven LSIL At 12 months unless and adolescent (<=20 years old). Recommend Following adolescents who are reliable and can understand accept Risk of possible progression of disease for 24 months before treating Persistent LSIL because of the higher rate of spontaneous disease Clearance and lower rate of progression to cancer in this population. For post menopausal women with first LSIL pap and suspected atrophy, Can treat in the same manner as for post menopausal women with ASCUS (see prior pages)
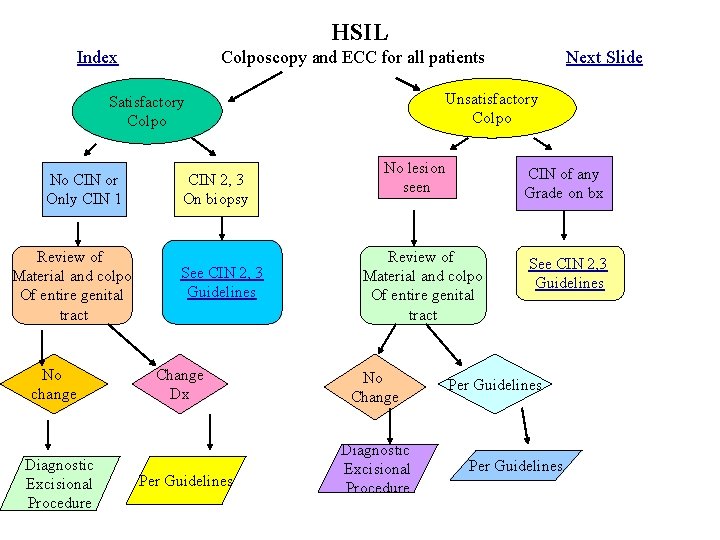
HSIL Index Colposcopy and ECC for all patients Unsatisfactory Colpo Satisfactory Colpo No CIN or Only CIN 1 Review of Material and colpo Of entire genital tract No change Diagnostic Excisional Procedure CIN 2, 3 On biopsy See CIN 2, 3 Guidelines Change Dx Per Guidelines Next Slide No lesion seen CIN of any Grade on bx Review of Material and colpo Of entire genital tract No Change Diagnostic Excisional Procedure See CIN 2, 3 Guidelines Per Guidelines
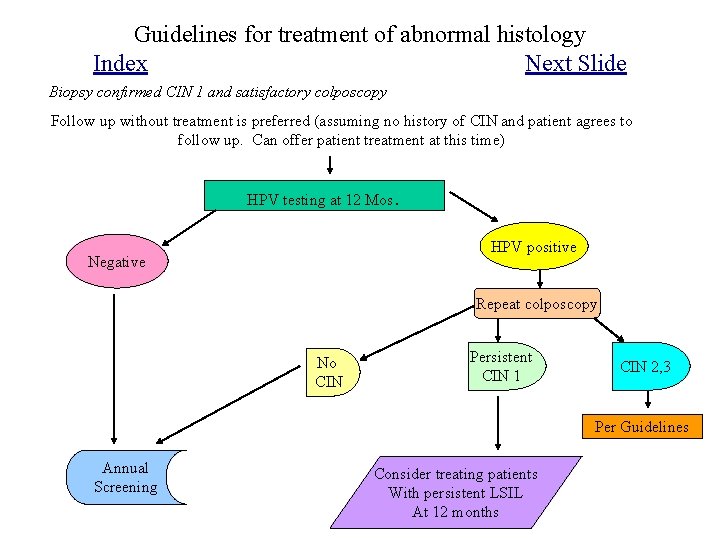
Guidelines for treatment of abnormal histology Index Next Slide Biopsy confirmed CIN 1 and satisfactory colposcopy Follow up without treatment is preferred (assuming no history of CIN and patient agrees to follow up. Can offer patient treatment at this time) HPV testing at 12 Mos . HPV positive Negative Repeat colposcopy No CIN Persistent CIN 1 CIN 2, 3 Per Guidelines Annual Screening Consider treating patients With persistent LSIL At 12 months
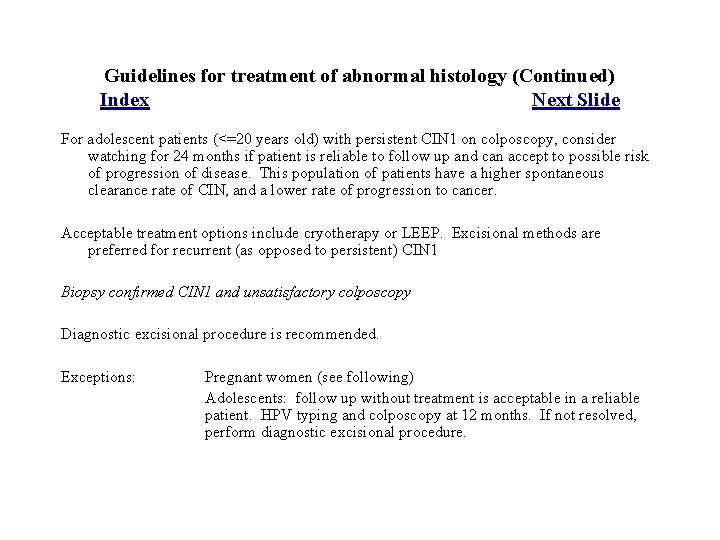
Guidelines for treatment of abnormal histology (Continued) Index Next Slide For adolescent patients (<=20 years old) with persistent CIN 1 on colposcopy, consider watching for 24 months if patient is reliable to follow up and can accept to possible risk of progression of disease. This population of patients have a higher spontaneous clearance rate of CIN, and a lower rate of progression to cancer. Acceptable treatment options include cryotherapy or LEEP. Excisional methods are preferred for recurrent (as opposed to persistent) CIN 1 Biopsy confirmed CIN 1 and unsatisfactory colposcopy Diagnostic excisional procedure is recommended. Exceptions: Pregnant women (see following) Adolescents: follow up without treatment is acceptable in a reliable patient. HPV typing and colposcopy at 12 months. If not resolved, perform diagnostic excisional procedure.
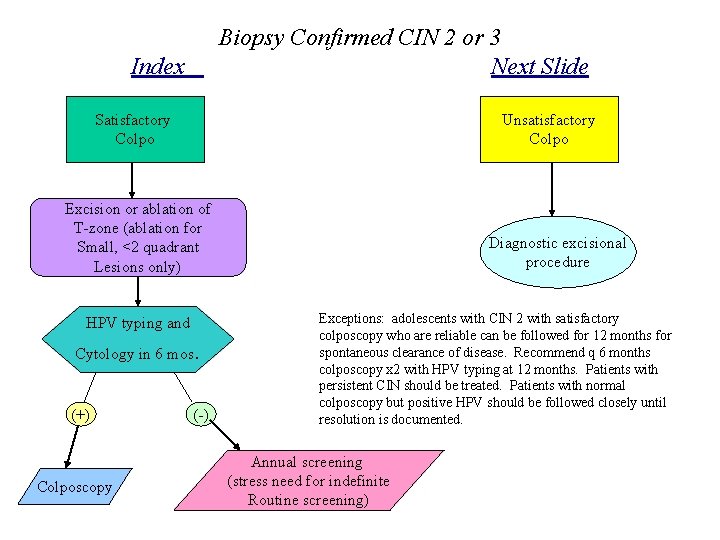
Biopsy Confirmed CIN 2 or 3 Next Slide Index Satisfactory Colpo Unsatisfactory Colpo Excision or ablation of T-zone (ablation for Small, <2 quadrant Lesions only) HPV typing and Cytology in 6 mos (+) Colposcopy . (-) Diagnostic excisional procedure Exceptions: adolescents with CIN 2 with satisfactory colposcopy who are reliable can be followed for 12 months for spontaneous clearance of disease. Recommend q 6 months colposcopy x 2 with HPV typing at 12 months. Patients with persistent CIN should be treated. Patients with normal colposcopy but positive HPV should be followed closely until resolution is documented. Annual screening (stress need for indefinite Routine screening)
Colposcopy in Pregnancy Index Next Slide Repeat colposcopy every three months in pregnancy, and again 8 weeks after delivery. Treatment of lesion should be based on post partum colposcopy and histology. If colposcopic impression or pathology during pregnancy suggests CIS, patient needs to be referred to an OB/GYN for possible excisional procedure while pregnant. Cervical biopsies are considered safe in pregnancy, although there is an increased risk of bleeding. ECC IS CONTRAINDICATED.
Immunosuppressed Patients (HIV, immunosuppressive therapy including chronic steroid use) Index Treatment of low grade lesions in immunosuppressed women results in poor clearance rates and no observable decrease in the rate of progression to high grade disease. The literature therefore supports observational management of immunosuppressed women with low grade disease. Treatment of CIN 2, 3 results in high rates of recurrence for CIN , but does appear to be effective in preventing progression to invasive cancer. The addition of 5 -FU after treatment of CIN 2, 3 halved the reoccurrence rate in one study. In HIV positive women, the administration of highly active antiretroviral therapy (HAART) at the time of treatment may help to clear disease. Consider OB/GYN and ID consultation prior to treating this group of women.
- Slides: 12