Colorectal Cancer Anatomy of the Colon and Rectum
- Slides: 51
Colorectal Cancer
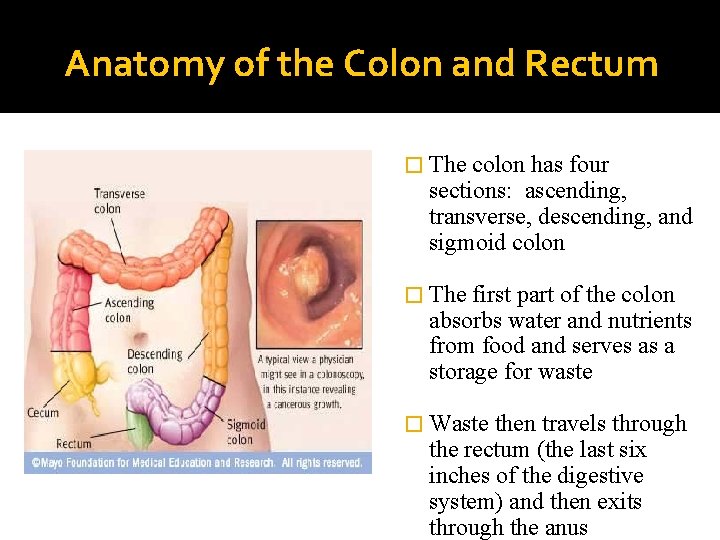
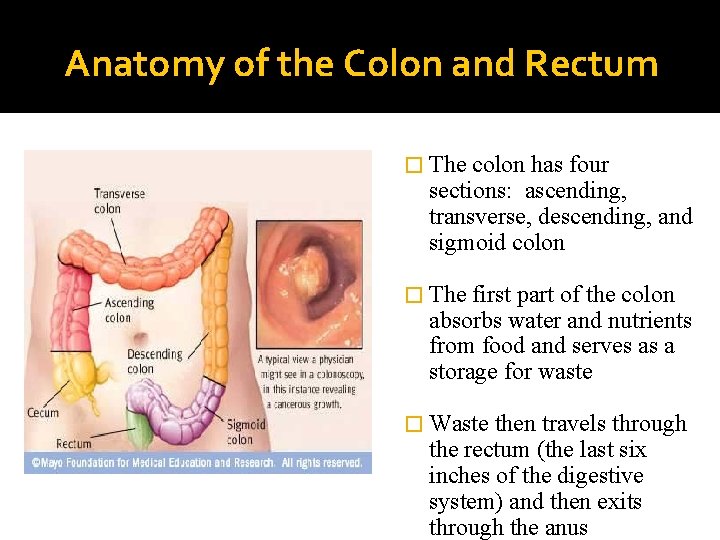
Anatomy of the Colon and Rectum � The colon has four sections: ascending, transverse, descending, and sigmoid colon � The first part of the colon absorbs water and nutrients from food and serves as a storage for waste � Waste then travels through the rectum (the last six inches of the digestive system) and then exits through the anus
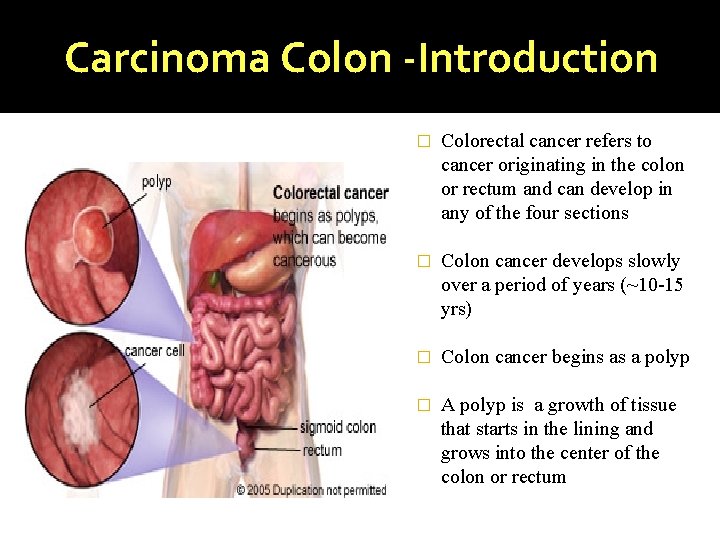
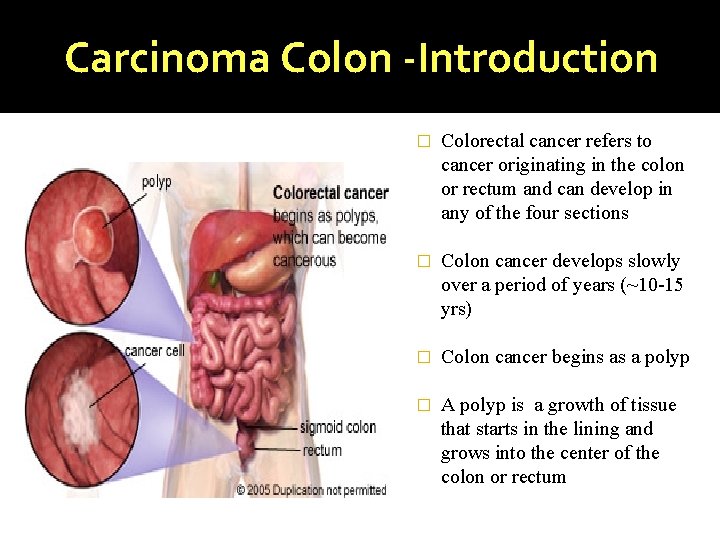
Carcinoma Colon -Introduction � Colorectal cancer refers to cancer originating in the colon or rectum and can develop in any of the four sections � Colon cancer develops slowly over a period of years (~10 -15 yrs) � Colon cancer begins as a polyp � A polyp is a growth of tissue that starts in the lining and grows into the center of the colon or rectum
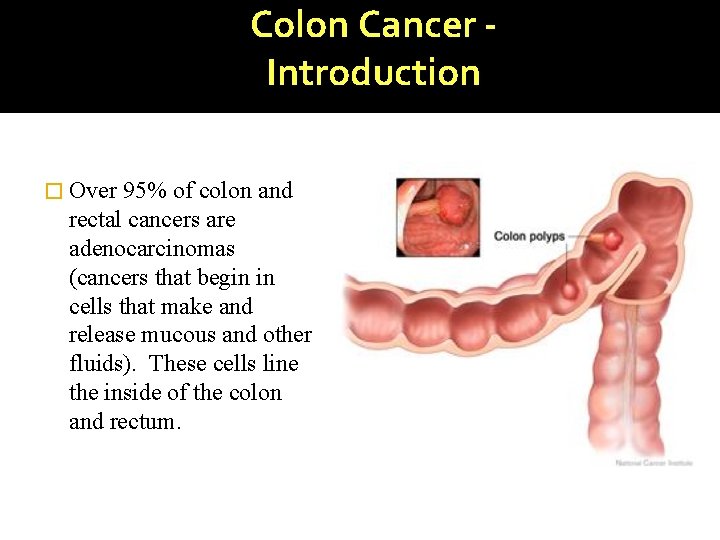
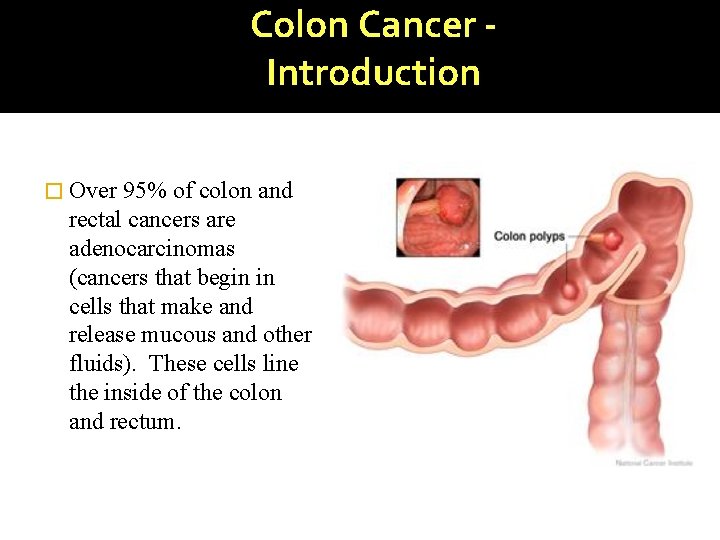
Colon Cancer Introduction � Over 95% of colon and rectal cancers are adenocarcinomas (cancers that begin in cells that make and release mucous and other fluids). These cells line the inside of the colon and rectum.
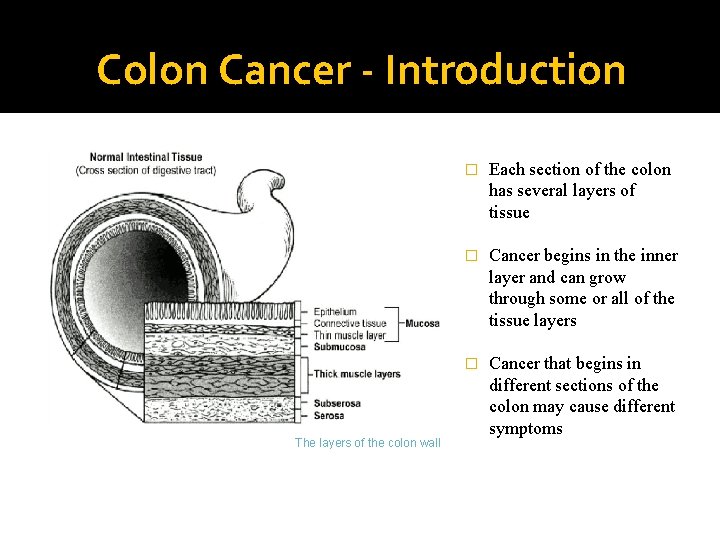
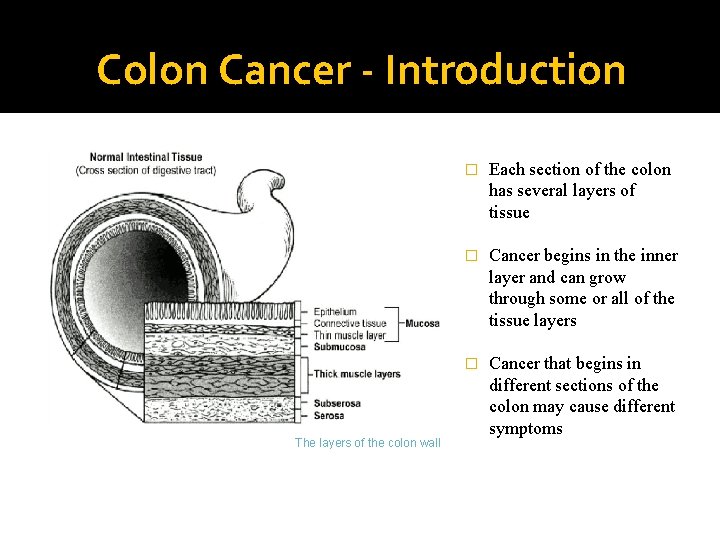
Colon Cancer - Introduction The layers of the colon wall � Each section of the colon has several layers of tissue � Cancer begins in the inner layer and can grow through some or all of the tissue layers � Cancer that begins in different sections of the colon may cause different symptoms
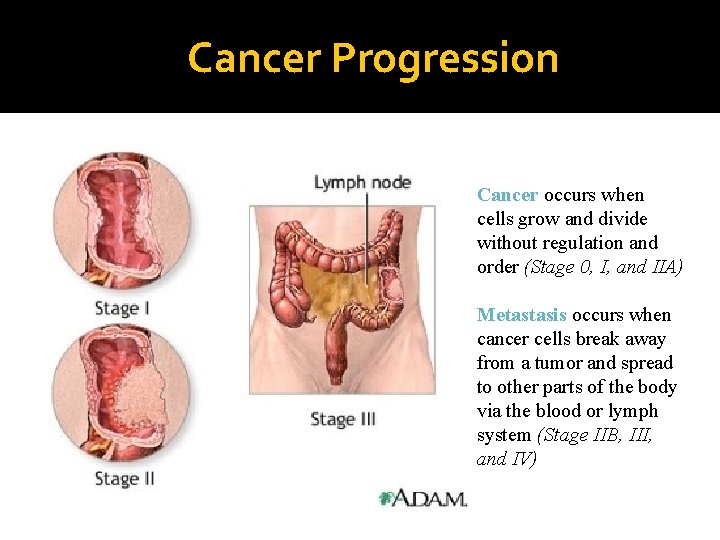
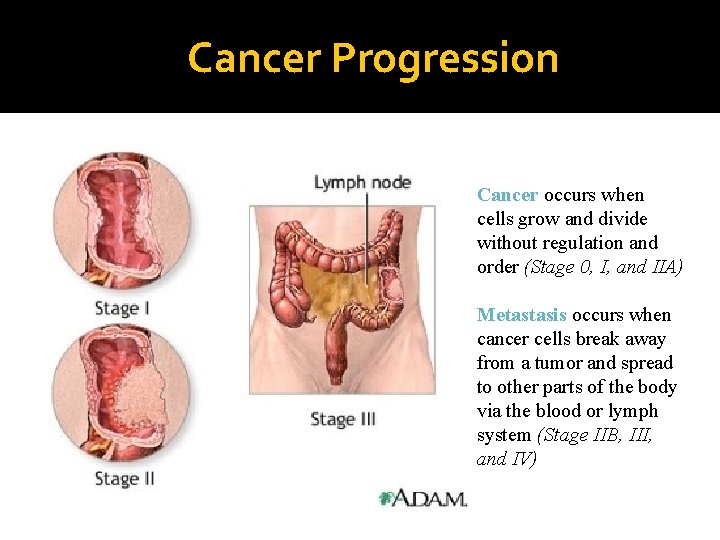
Cancer Progression � Cancer occurs when cells grow and divide without regulation and order (Stage 0, I, and IIA) � Metastasis occurs when cancer cells break away from a tumor and spread to other parts of the body via the blood or lymph system (Stage IIB, III, and IV)
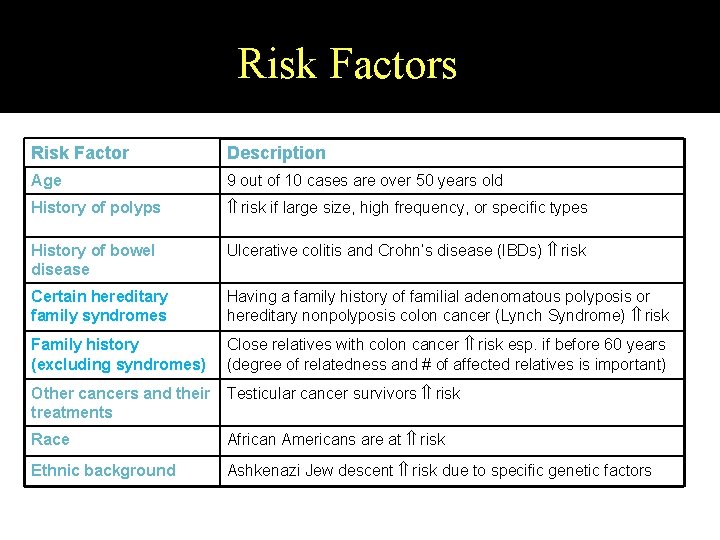
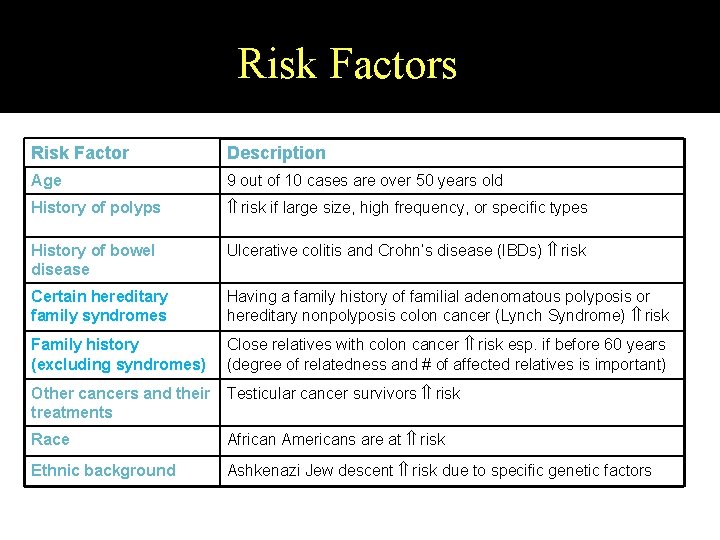
Risk Factors Risk Factor Description Age 9 out of 10 cases are over 50 years old History of polyps risk if large size, high frequency, or specific types History of bowel disease Ulcerative colitis and Crohn’s disease (IBDs) risk Certain hereditary family syndromes Having a family history of familial adenomatous polyposis or hereditary nonpolyposis colon cancer (Lynch Syndrome) risk Family history (excluding syndromes) Close relatives with colon cancer risk esp. if before 60 years (degree of relatedness and # of affected relatives is important) Other cancers and their treatments Testicular cancer survivors risk Race African Americans are at risk Ethnic background Ashkenazi Jew descent risk due to specific genetic factors
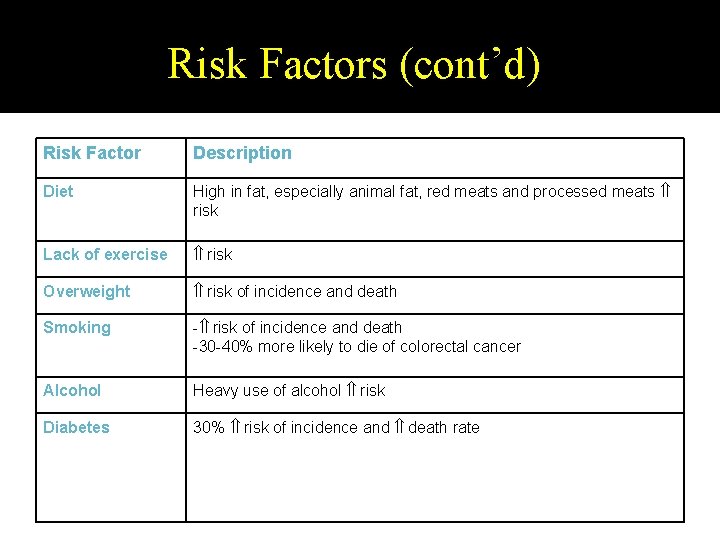
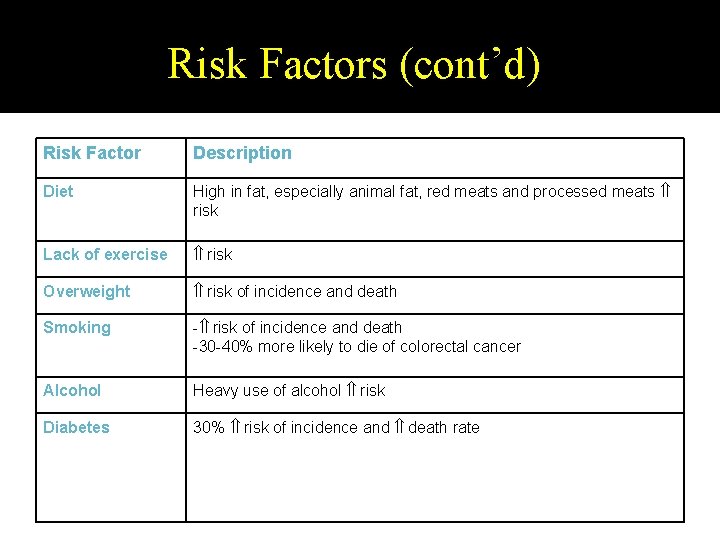
Risk Factors (cont’d) Risk Factor Description Diet High in fat, especially animal fat, red meats and processed meats risk Lack of exercise risk Overweight risk of incidence and death Smoking - risk of incidence and death -30 -40% more likely to die of colorectal cancer Alcohol Heavy use of alcohol risk Diabetes 30% risk of incidence and death rate
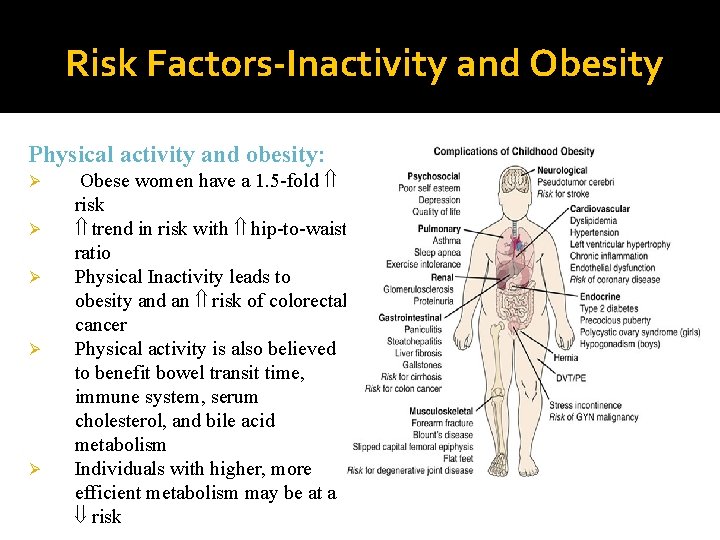
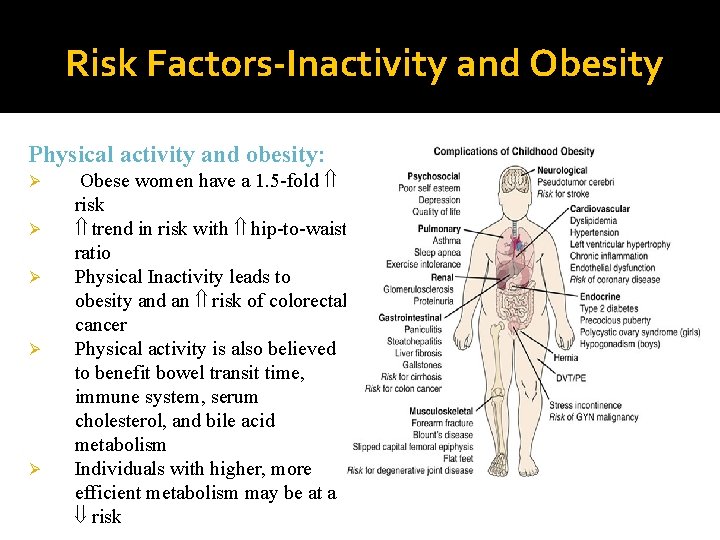
Risk Factors-Inactivity and Obesity Physical activity and obesity: Ø Ø Ø Obese women have a 1. 5 -fold risk trend in risk with hip-to-waist ratio Physical Inactivity leads to obesity and an risk of colorectal cancer Physical activity is also believed to benefit bowel transit time, immune system, serum cholesterol, and bile acid metabolism Individuals with higher, more efficient metabolism may be at a risk
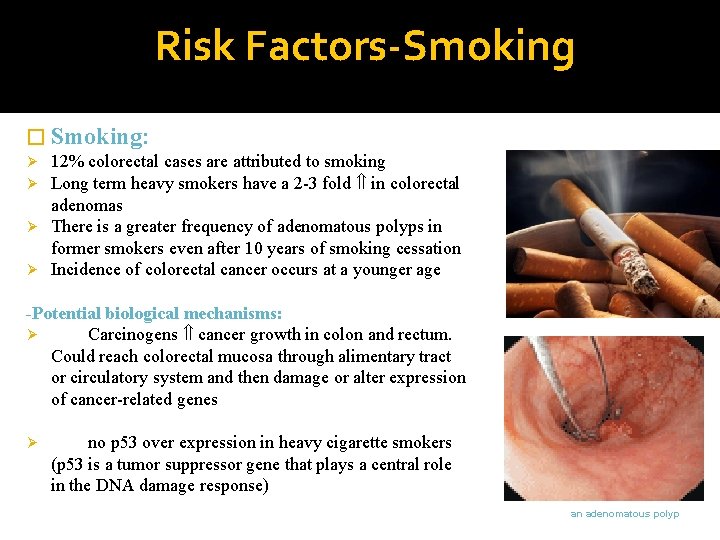
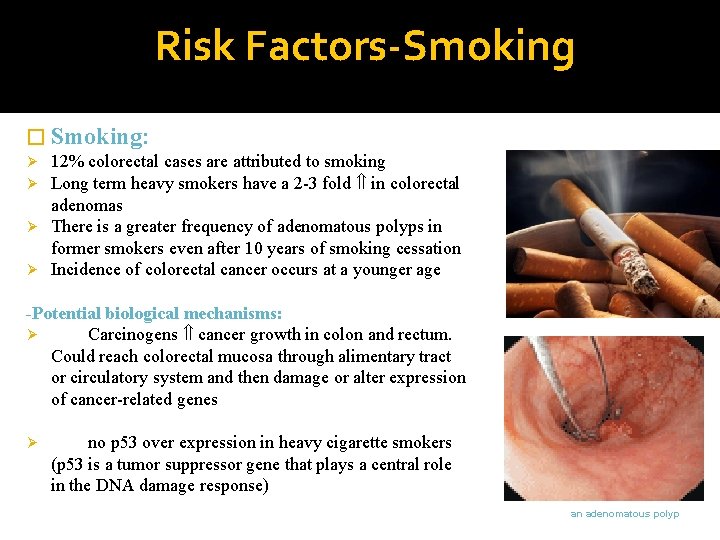
Risk Factors-Smoking � Smoking: 12% colorectal cases are attributed to smoking Long term heavy smokers have a 2 -3 fold in colorectal adenomas Ø There is a greater frequency of adenomatous polyps in former smokers even after 10 years of smoking cessation Ø Incidence of colorectal cancer occurs at a younger age Ø Ø -Potential biological mechanisms: Ø Carcinogens cancer growth in colon and rectum. Could reach colorectal mucosa through alimentary tract or circulatory system and then damage or alter expression of cancer-related genes Ø no p 53 over expression in heavy cigarette smokers (p 53 is a tumor suppressor gene that plays a central role in the DNA damage response) an adenomatous polyp
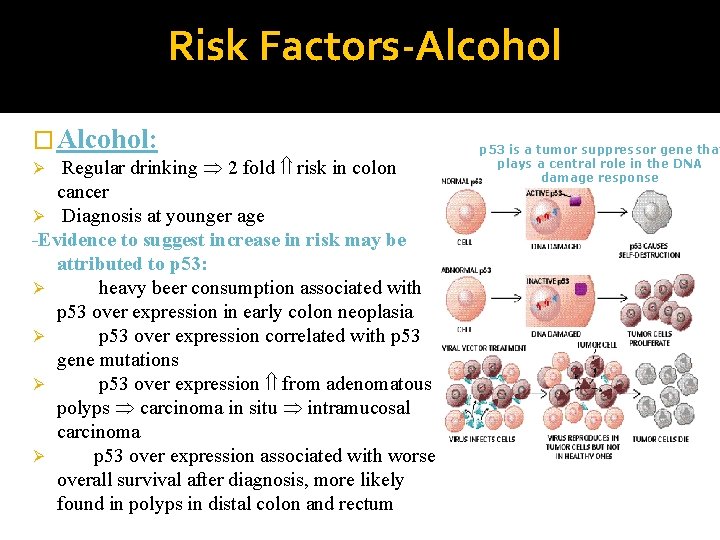
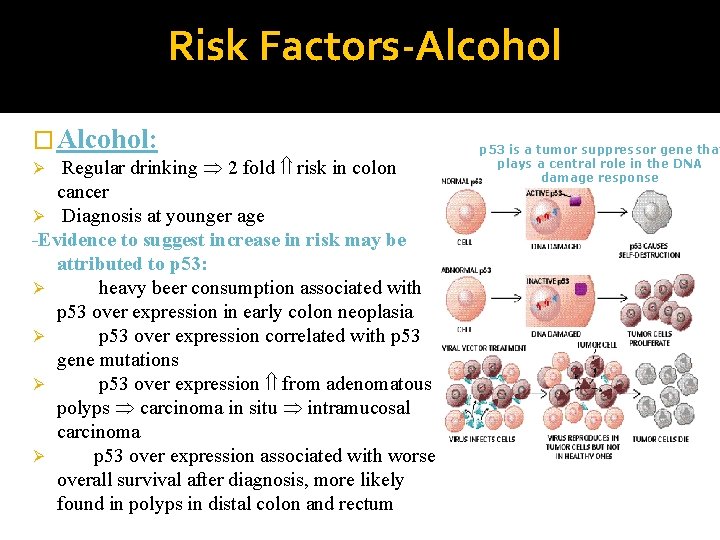
Risk Factors-Alcohol � Alcohol: Regular drinking 2 fold risk in colon cancer Ø Diagnosis at younger age -Evidence to suggest increase in risk may be attributed to p 53: Ø heavy beer consumption associated with p 53 over expression in early colon neoplasia Ø p 53 over expression correlated with p 53 gene mutations Ø p 53 over expression from adenomatous polyps carcinoma in situ intramucosal carcinoma Ø p 53 over expression associated with worse overall survival after diagnosis, more likely found in polyps in distal colon and rectum Ø p 53 is a tumor suppressor gene that plays a central role in the DNA damage response
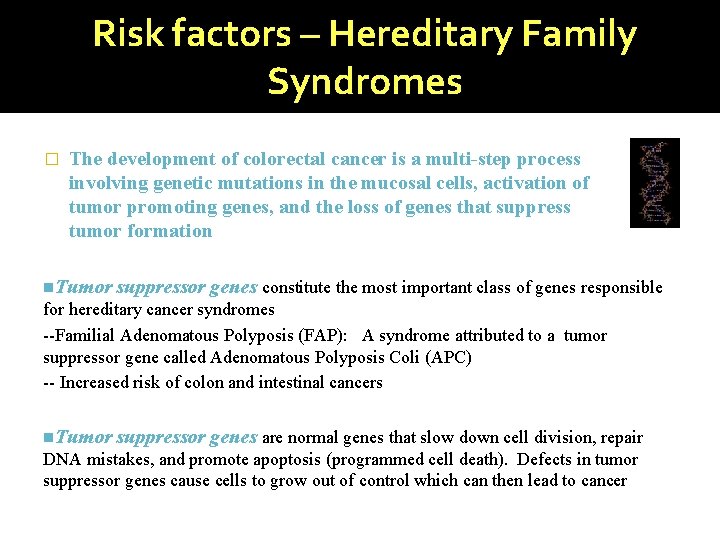
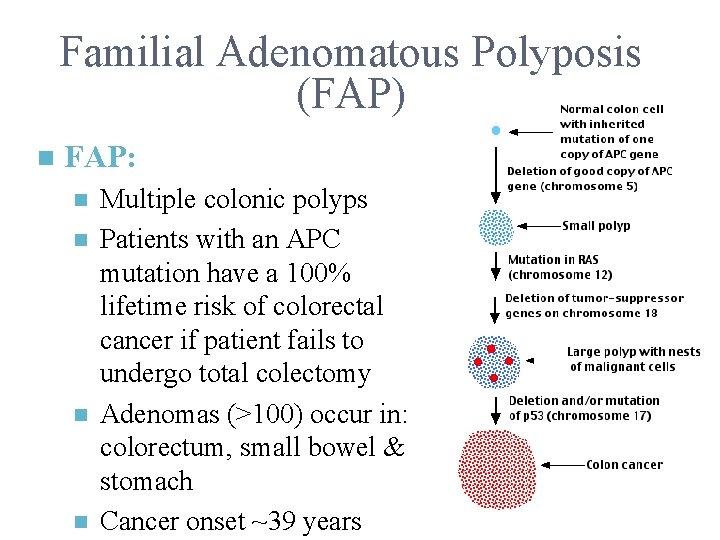
Risk factors – Hereditary Family Syndromes � The development of colorectal cancer is a multi-step process involving genetic mutations in the mucosal cells, activation of tumor promoting genes, and the loss of genes that suppress tumor formation n. Tumor suppressor genes constitute the most important class of genes responsible for hereditary cancer syndromes --Familial Adenomatous Polyposis (FAP): A syndrome attributed to a tumor suppressor gene called Adenomatous Polyposis Coli (APC) -- Increased risk of colon and intestinal cancers n. Tumor suppressor genes are normal genes that slow down cell division, repair DNA mistakes, and promote apoptosis (programmed cell death). Defects in tumor suppressor genes cause cells to grow out of control which can then lead to cancer
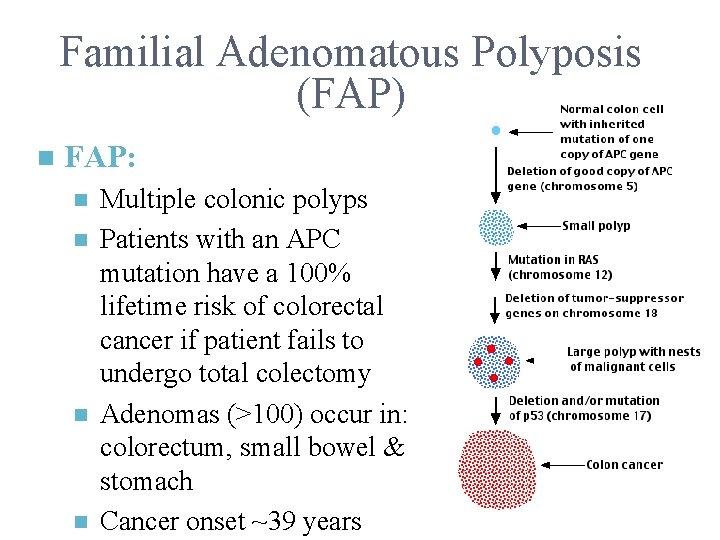
Familial Adenomatous Polyposis (FAP) n FAP: n n Multiple colonic polyps Patients with an APC mutation have a 100% lifetime risk of colorectal cancer if patient fails to undergo total colectomy Adenomas (>100) occur in: colorectum, small bowel & stomach Cancer onset ~39 years
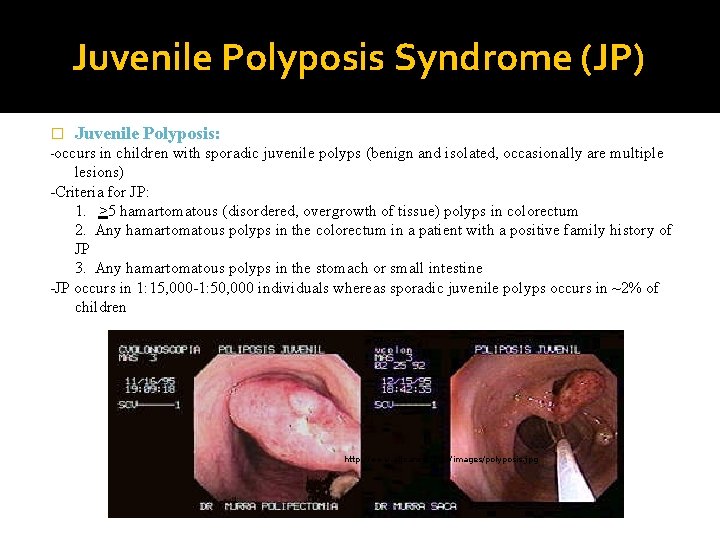
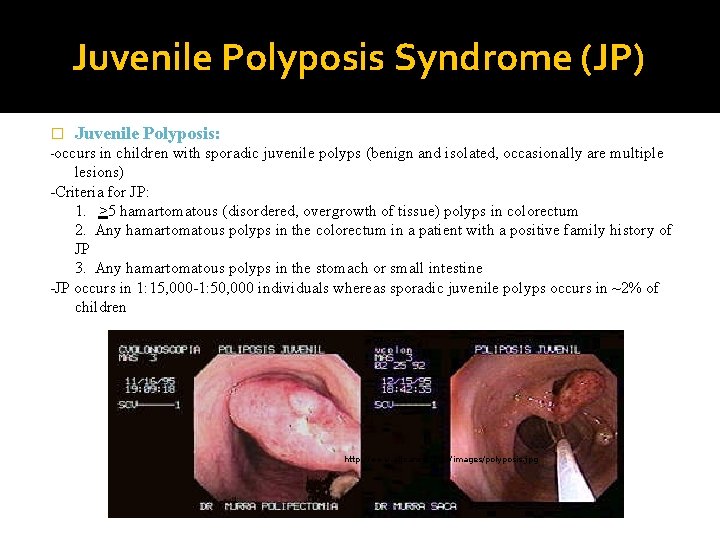
Juvenile Polyposis Syndrome (JP) � Juvenile Polyposis: -occurs in children with sporadic juvenile polyps (benign and isolated, occasionally are multiple lesions) -Criteria for JP: 1. >5 hamartomatous (disordered, overgrowth of tissue) polyps in colorectum 2. Any hamartomatous polyps in the colorectum in a patient with a positive family history of JP 3. Any hamartomatous polyps in the stomach or small intestine -JP occurs in 1: 15, 000 -1: 50, 000 individuals whereas sporadic juvenile polyps occurs in ~2% of children http: //www. altcancer. com/images/polyposis. jpg
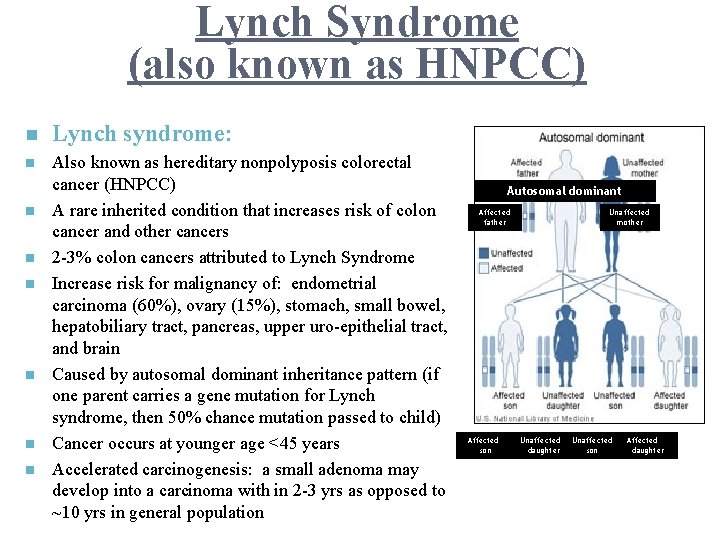
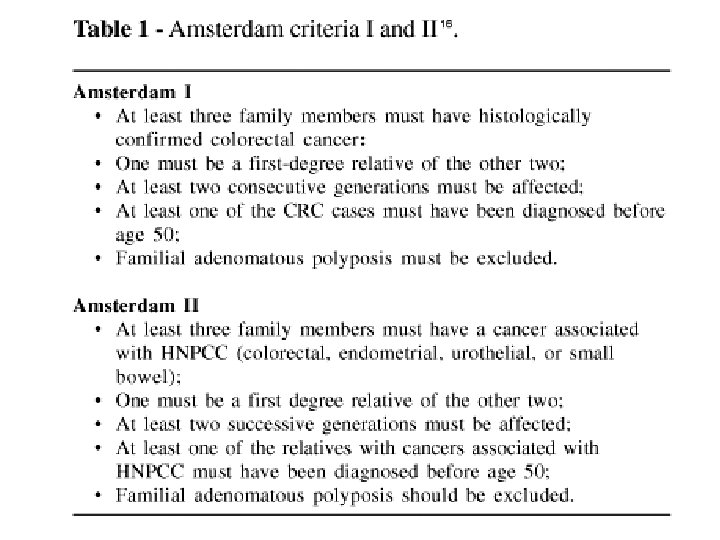
Lynch Syndrome (also known as HNPCC) n Lynch syndrome: n Also known as hereditary nonpolyposis colorectal cancer (HNPCC) A rare inherited condition that increases risk of colon cancer and other cancers 2 -3% colon cancers attributed to Lynch Syndrome Increase risk for malignancy of: endometrial carcinoma (60%), ovary (15%), stomach, small bowel, hepatobiliary tract, pancreas, upper uro-epithelial tract, and brain Caused by autosomal dominant inheritance pattern (if one parent carries a gene mutation for Lynch syndrome, then 50% chance mutation passed to child) Cancer occurs at younger age <45 years Accelerated carcinogenesis: a small adenoma may develop into a carcinoma with in 2 -3 yrs as opposed to ~10 yrs in general population n n n Autosomal dominant Affected father Affected son Unaffected mother Unaffected daughter Unaffected son Affected daughter
TYPES �Synchronous : - Multiple primary carcinomas in different parts of the colon at the same time �Metachronous : - growth in different parts of the colon in different periods Gross Types : - Annular, tubular, ulcerative, cauliflower like
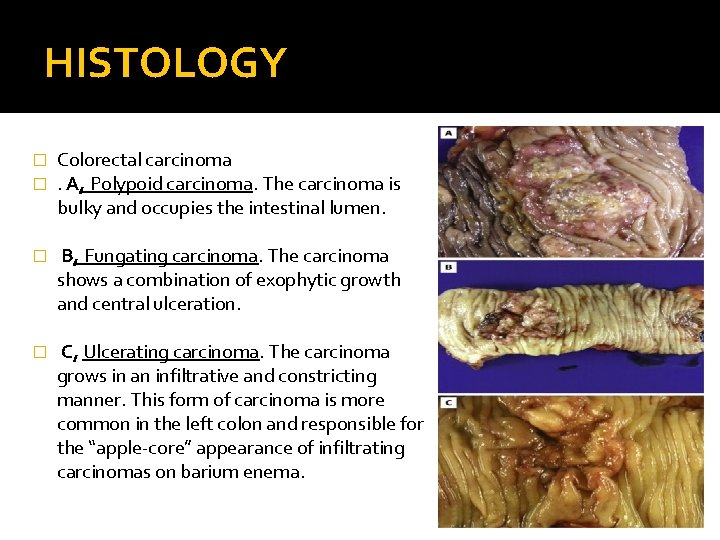
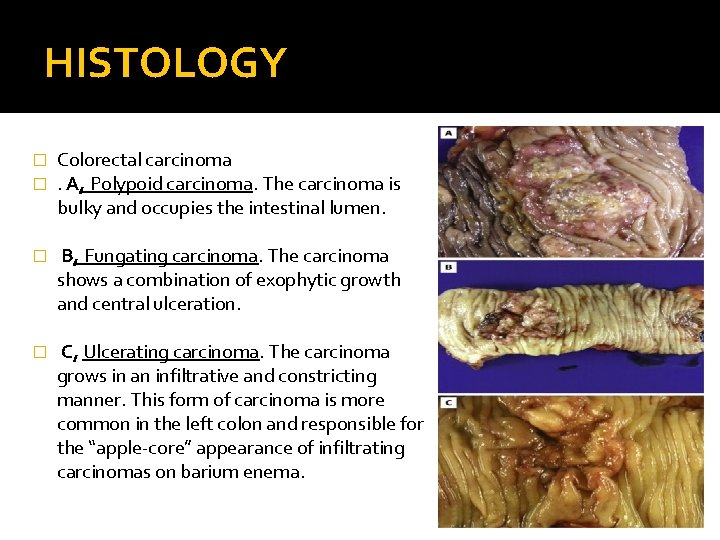
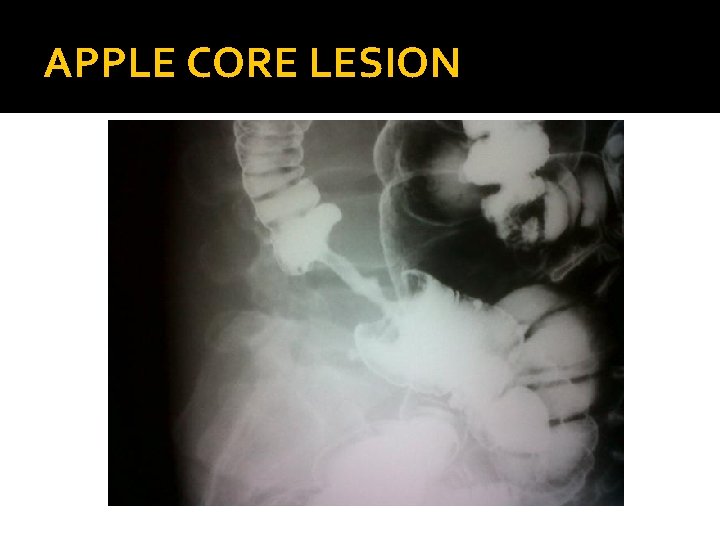
HISTOLOGY � � Colorectal carcinoma. A, Polypoid carcinoma. The carcinoma is bulky and occupies the intestinal lumen. � B, Fungating carcinoma. The carcinoma shows a combination of exophytic growth and central ulceration. � C, Ulcerating carcinoma. The carcinoma grows in an infiltrative and constricting manner. This form of carcinoma is more common in the left colon and responsible for the “apple-core” appearance of infiltrating carcinomas on barium enema.
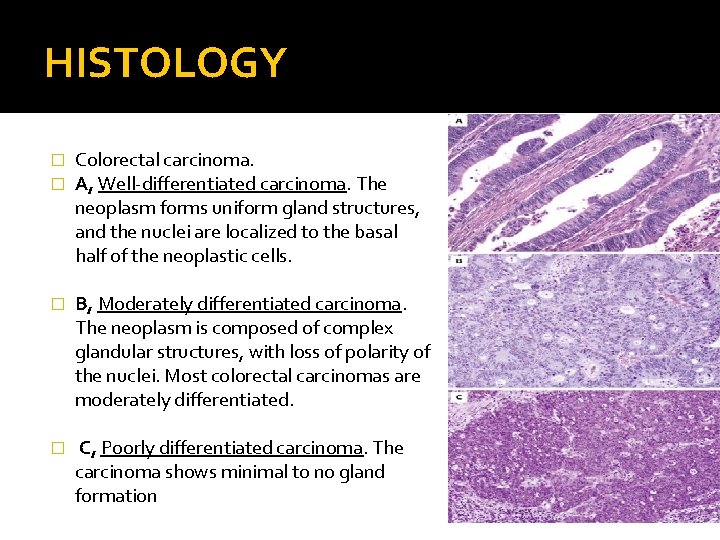
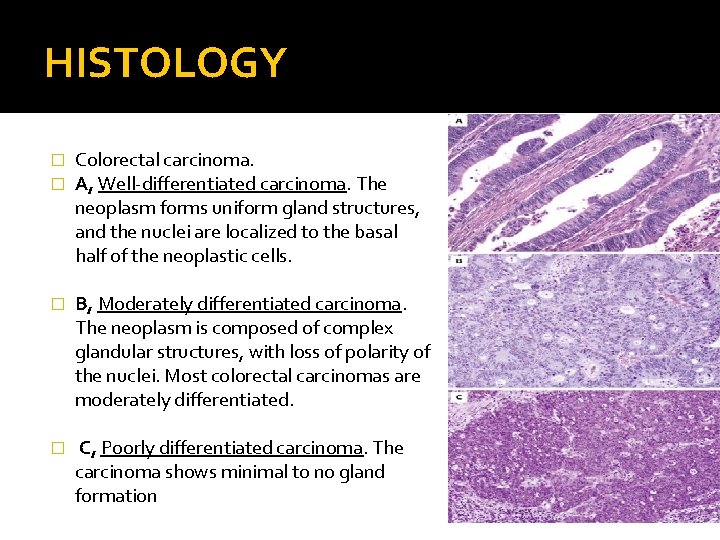
HISTOLOGY � � Colorectal carcinoma. A, Well-differentiated carcinoma. The neoplasm forms uniform gland structures, and the nuclei are localized to the basal half of the neoplastic cells. � B, Moderately differentiated carcinoma. The neoplasm is composed of complex glandular structures, with loss of polarity of the nuclei. Most colorectal carcinomas are moderately differentiated. � C, Poorly differentiated carcinoma. The carcinoma shows minimal to no gland formation
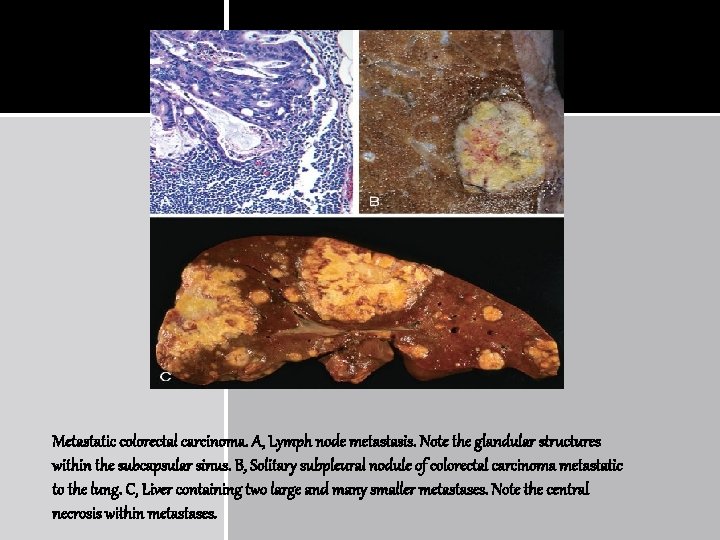
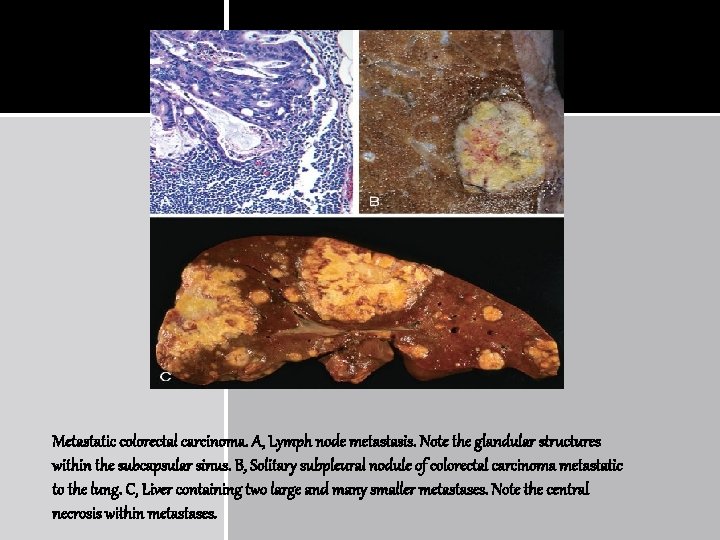
Metastatic colorectal carcinoma. A, Lymph node metastasis. Note the glandular structures within the subcapsular sinus. B, Solitary subpleural nodule of colorectal carcinoma metastatic to the lung. C, Liver containing two large and many smaller metastases. Note the central necrosis within metastases.
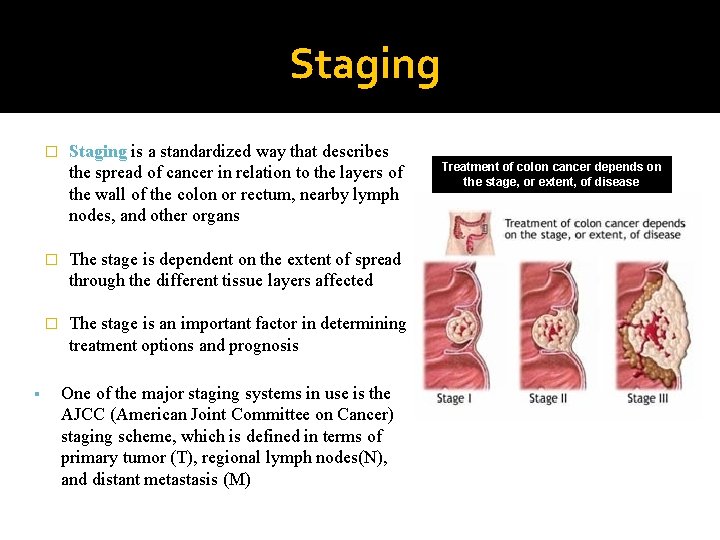
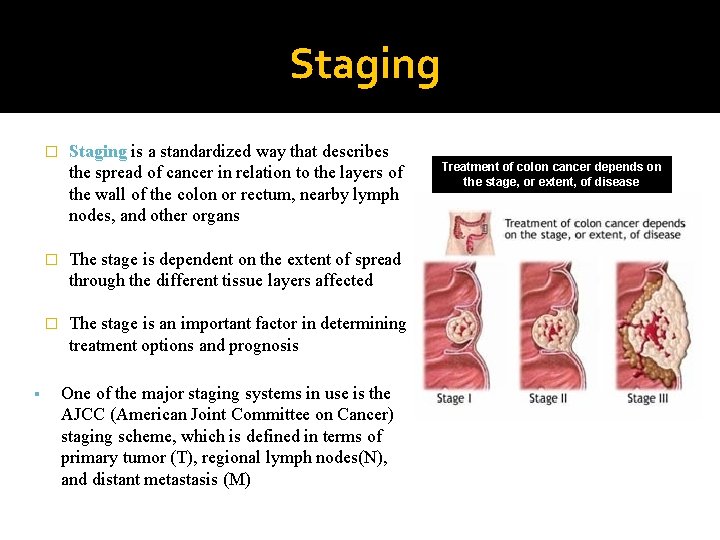
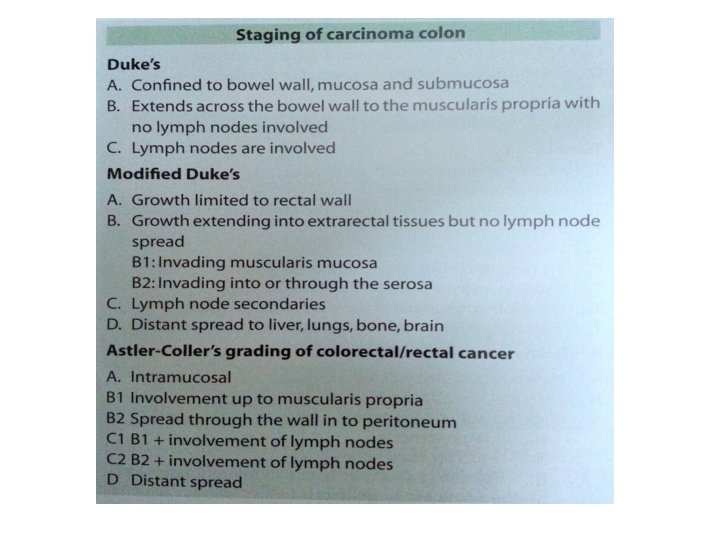
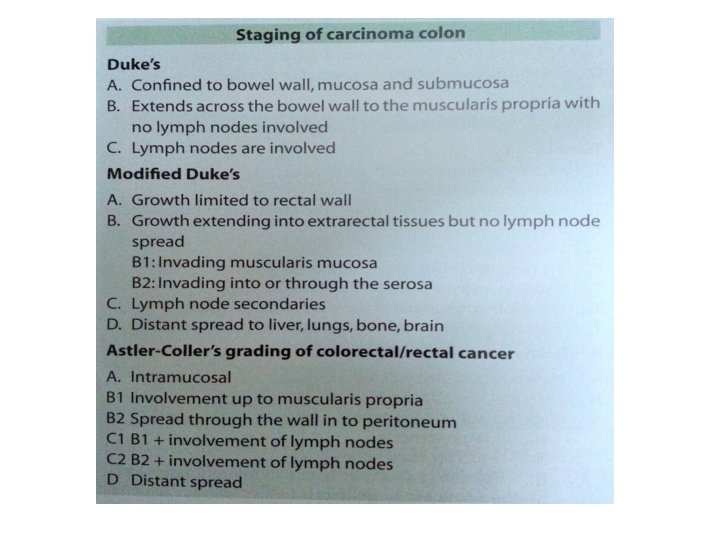
Staging � Staging is a standardized way that describes the spread of cancer in relation to the layers of the wall of the colon or rectum, nearby lymph nodes, and other organs � The stage is dependent on the extent of spread through the different tissue layers affected � The stage is an important factor in determining treatment options and prognosis One of the major staging systems in use is the AJCC (American Joint Committee on Cancer) staging scheme, which is defined in terms of primary tumor (T), regional lymph nodes(N), and distant metastasis (M) Treatment of colon cancer depends on the stage, or extent, of disease
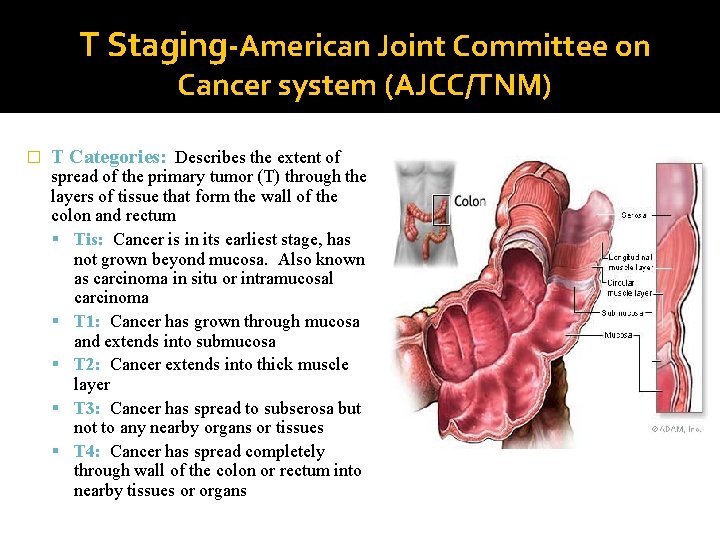
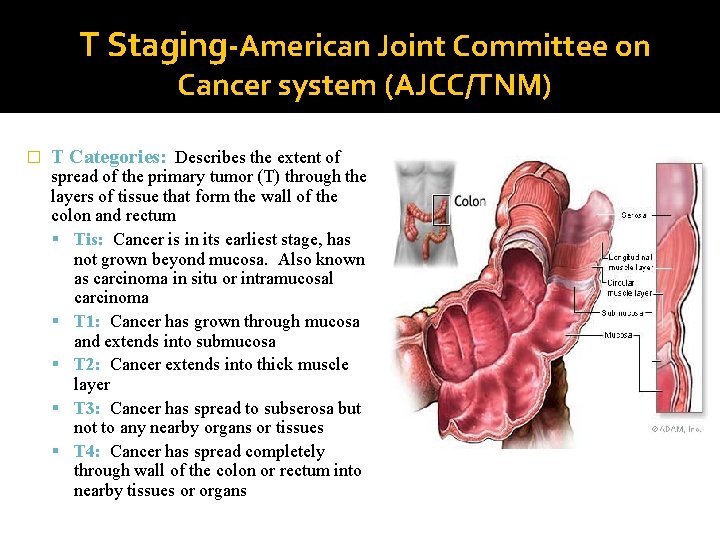
T Staging-American Joint Committee on Cancer system (AJCC/TNM) � T Categories: Describes the extent of spread of the primary tumor (T) through the layers of tissue that form the wall of the colon and rectum Tis: Cancer is in its earliest stage, has not grown beyond mucosa. Also known as carcinoma in situ or intramucosal carcinoma T 1: Cancer has grown through mucosa and extends into submucosa T 2: Cancer extends into thick muscle layer T 3: Cancer has spread to subserosa but not to any nearby organs or tissues T 4: Cancer has spread completely through wall of the colon or rectum into nearby tissues or organs
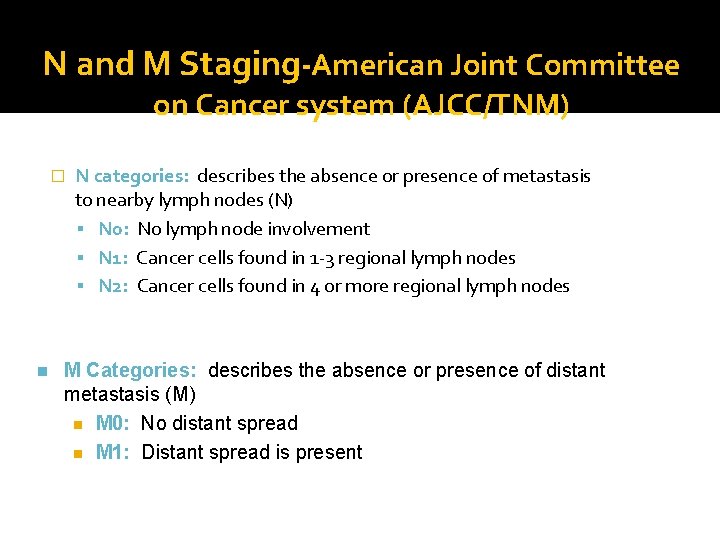
N and M Staging-American Joint Committee on Cancer system (AJCC/TNM) � n N categories: describes the absence or presence of metastasis to nearby lymph nodes (N) N 0: No lymph node involvement N 1: Cancer cells found in 1 -3 regional lymph nodes N 2: Cancer cells found in 4 or more regional lymph nodes M Categories: describes the absence or presence of distant metastasis (M) n M 0: No distant spread n M 1: Distant spread is present
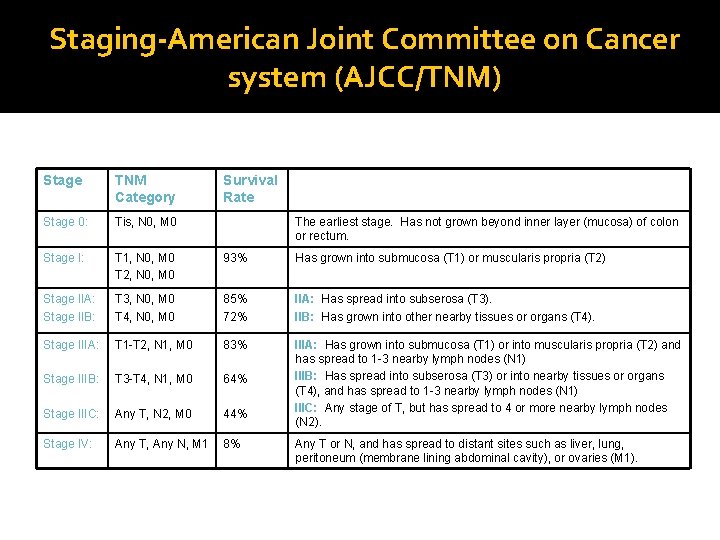
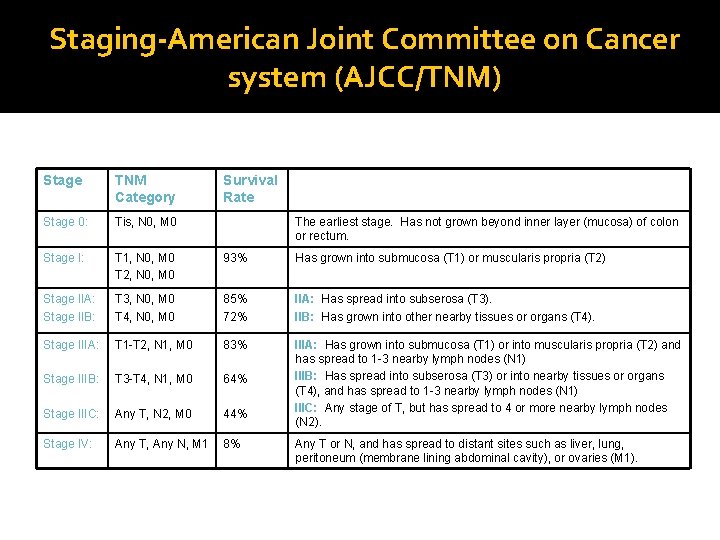
Staging-American Joint Committee on Cancer system (AJCC/TNM) Stage TNM Category Survival Rate Stage 0: Tis, N 0, M 0 Stage I: T 1, N 0, M 0 T 2, N 0, M 0 93% Has grown into submucosa (T 1) or muscularis propria (T 2) Stage IIA: Stage IIB: T 3, N 0, M 0 T 4, N 0, M 0 85% 72% IIA: Has spread into subserosa (T 3). IIB: Has grown into other nearby tissues or organs (T 4). Stage IIIA: T 1 -T 2, N 1, M 0 83% Stage IIIB: T 3 -T 4, N 1, M 0 64% Stage IIIC: Any T, N 2, M 0 44% IIIA: Has grown into submucosa (T 1) or into muscularis propria (T 2) and has spread to 1 -3 nearby lymph nodes (N 1) IIIB: Has spread into subserosa (T 3) or into nearby tissues or organs (T 4), and has spread to 1 -3 nearby lymph nodes (N 1) IIIC: Any stage of T, but has spread to 4 or more nearby lymph nodes (N 2). Stage IV: Any T, Any N, M 1 8% The earliest stage. Has not grown beyond inner layer (mucosa) of colon or rectum. Any T or N, and has spread to distant sites such as liver, lung, peritoneum (membrane lining abdominal cavity), or ovaries (M 1).
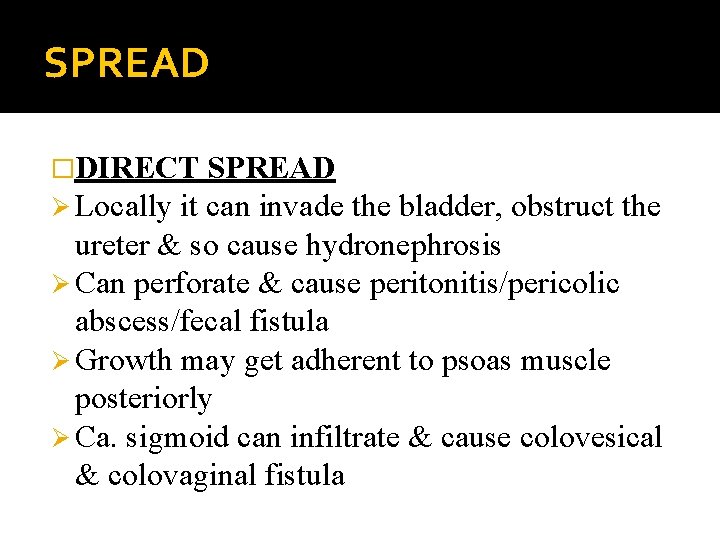
SPREAD �DIRECT SPREAD Ø Locally it can invade the bladder, obstruct the ureter & so cause hydronephrosis Ø Can perforate & cause peritonitis/pericolic abscess/fecal fistula Ø Growth may get adherent to psoas muscle posteriorly Ø Ca. sigmoid can infiltrate & cause colovesical & colovaginal fistula
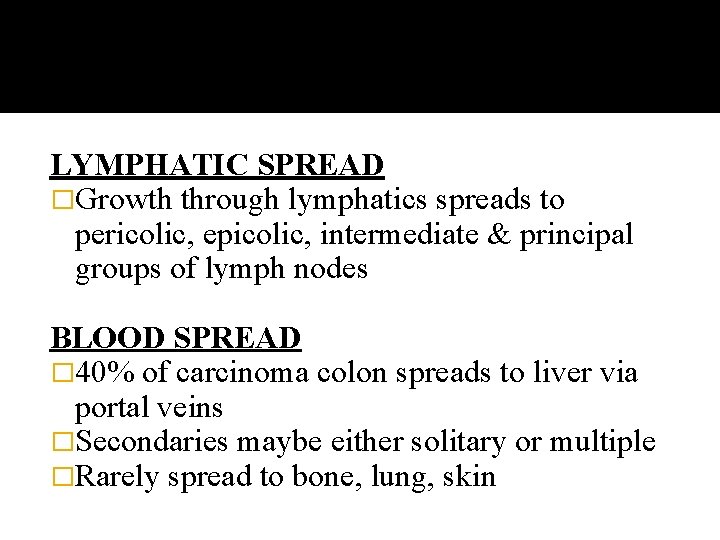
LYMPHATIC SPREAD �Growth through lymphatics spreads to pericolic, epicolic, intermediate & principal groups of lymph nodes BLOOD SPREAD � 40% of carcinoma colon spreads to liver via portal veins �Secondaries maybe either solitary or multiple �Rarely spread to bone, lung, skin
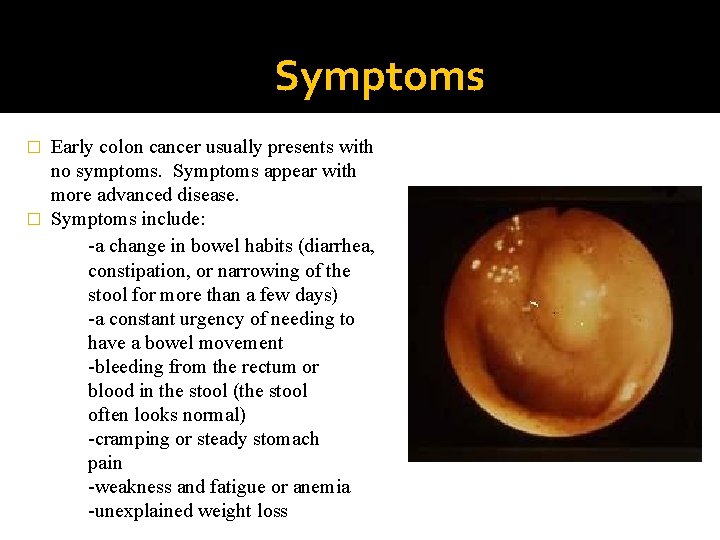
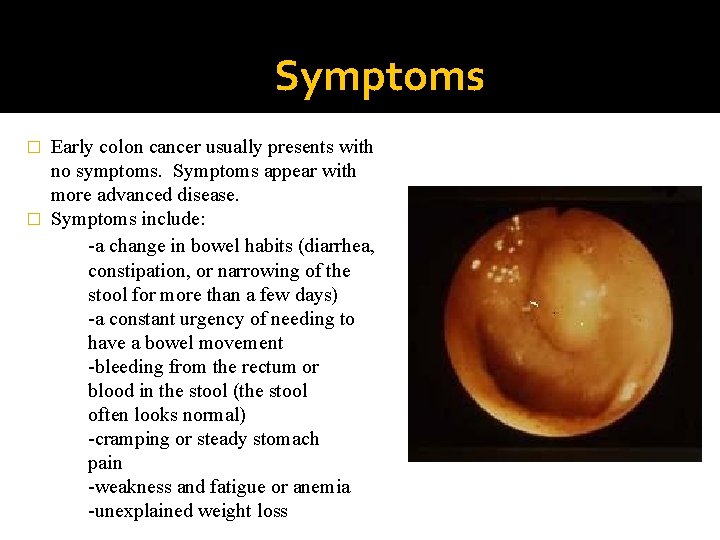
Symptoms Early colon cancer usually presents with no symptoms. Symptoms appear with more advanced disease. � Symptoms include: -a change in bowel habits (diarrhea, constipation, or narrowing of the stool for more than a few days) -a constant urgency of needing to have a bowel movement -bleeding from the rectum or blood in the stool (the stool often looks normal) -cramping or steady stomach pain -weakness and fatigue or anemia -unexplained weight loss �
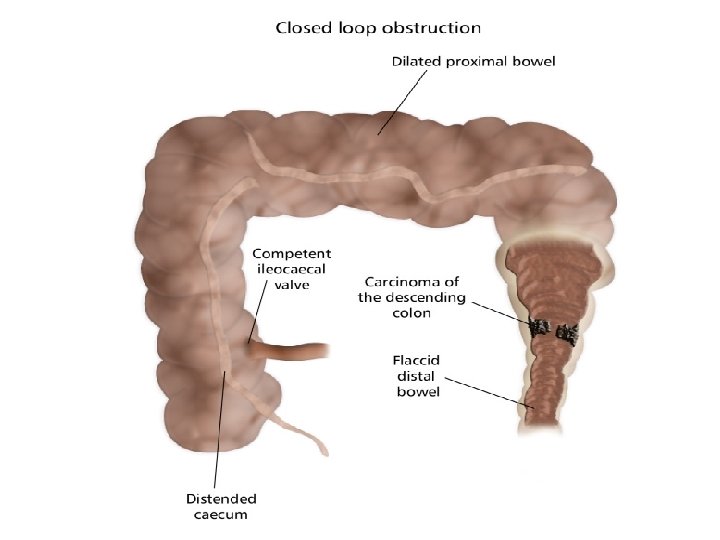
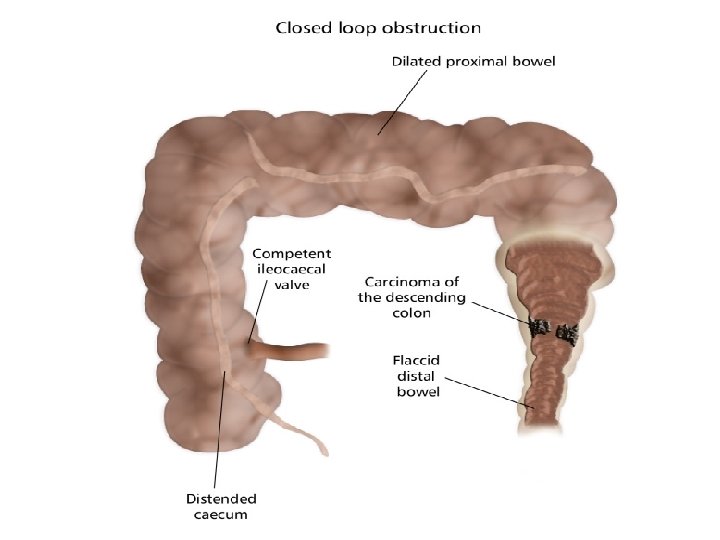
CLINICAL FEATURES - CONTD �Right sided growth commonly presents with anaemia, palpable mass in the right iliac fossa �Left sided growth presents with colicky pain, altered bowel habits (alternating constipation & diarrhea), palpable lump, distension of abdomen. �Perforation/peritonitis might be the 1 st presentation �Closed loop obstruction may occur in transverse colon growth �Enlarged liver with multiple secondaries, ascites
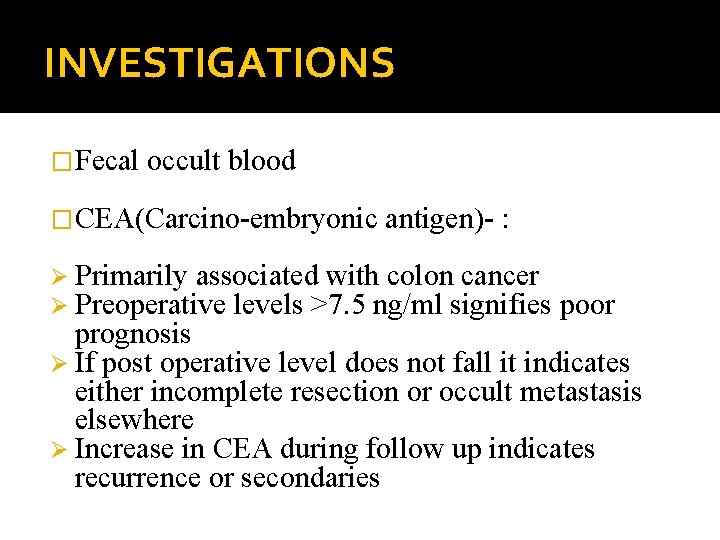
INVESTIGATIONS �Fecal occult blood �CEA(Carcino-embryonic antigen)- : Ø Primarily associated with colon cancer Ø Preoperative levels >7. 5 ng/ml signifies poor prognosis Ø If post operative level does not fall it indicates either incomplete resection or occult metastasis elsewhere Ø Increase in CEA during follow up indicates recurrence or secondaries
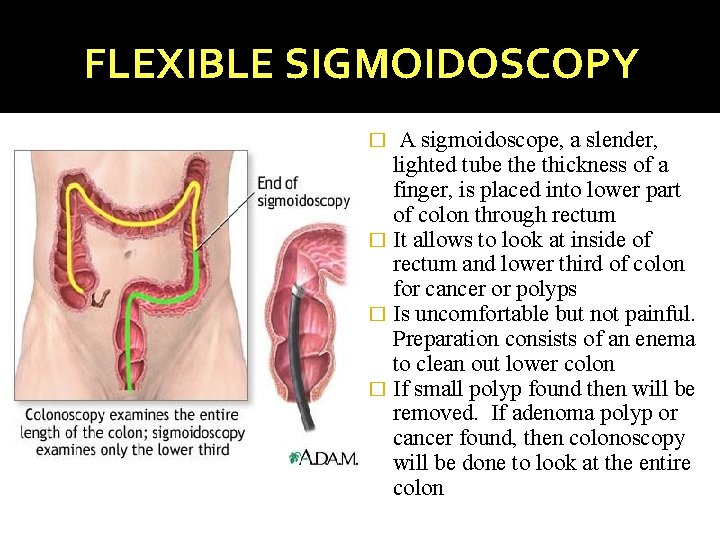
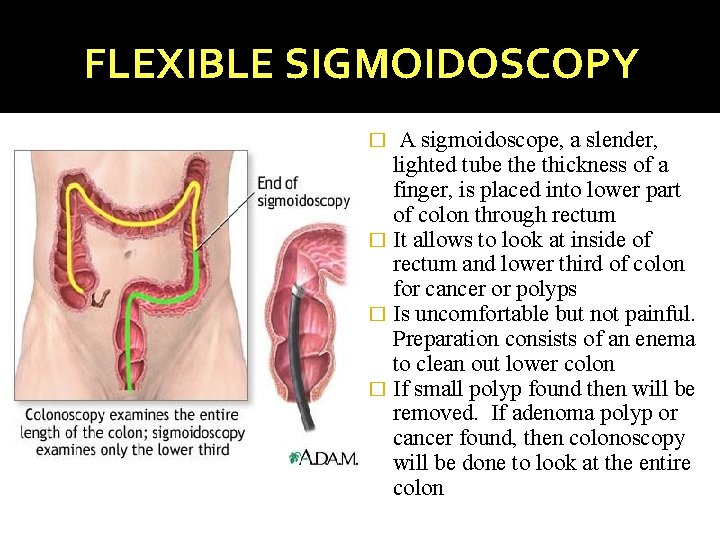
FLEXIBLE SIGMOIDOSCOPY A sigmoidoscope, a slender, lighted tube thickness of a finger, is placed into lower part of colon through rectum � It allows to look at inside of rectum and lower third of colon for cancer or polyps � Is uncomfortable but not painful. Preparation consists of an enema to clean out lower colon � If small polyp found then will be removed. If adenoma polyp or cancer found, then colonoscopy will be done to look at the entire colon �
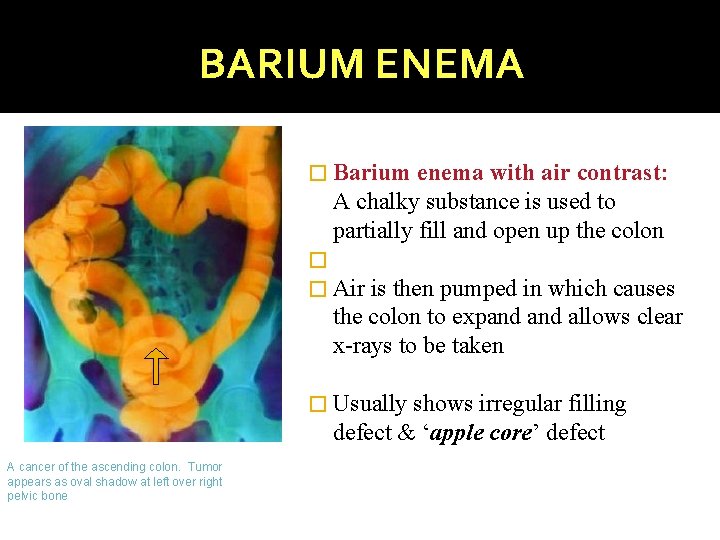
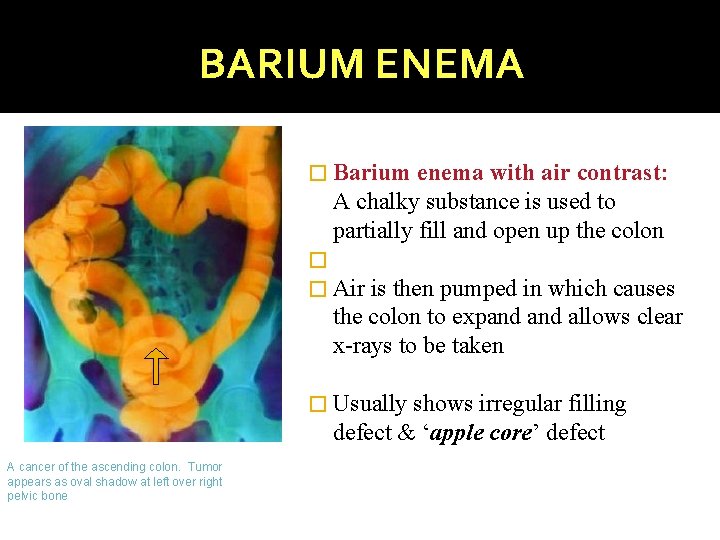
BARIUM ENEMA � Barium enema with air contrast: A chalky substance is used to partially fill and open up the colon � � Air is then pumped in which causes the colon to expand allows clear x-rays to be taken � Usually shows irregular filling defect & ‘apple core’ defect A cancer of the ascending colon. Tumor appears as oval shadow at left over right pelvic bone
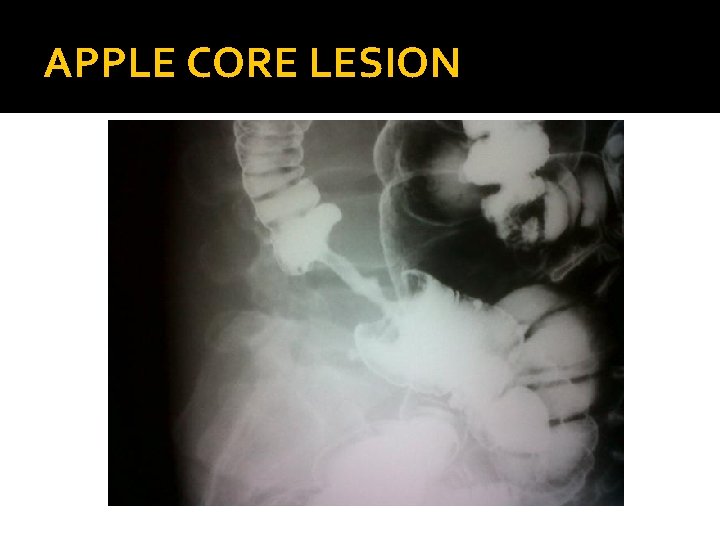
APPLE CORE LESION
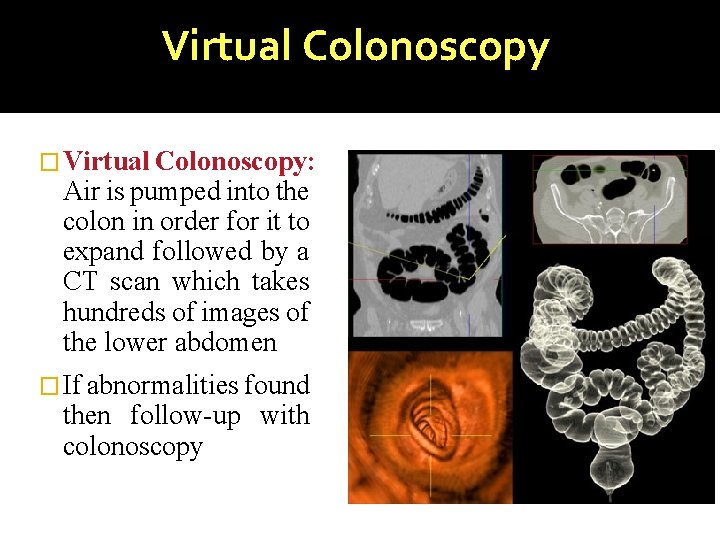
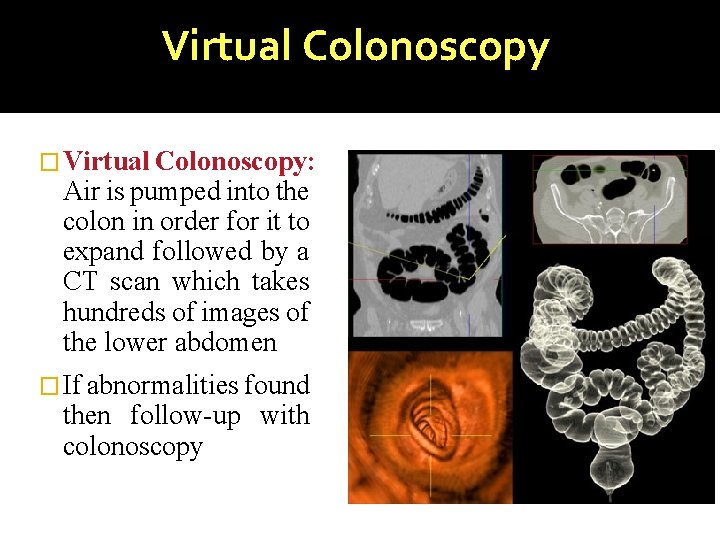
Virtual Colonoscopy � Virtual Colonoscopy: Air is pumped into the colon in order for it to expand followed by a CT scan which takes hundreds of images of the lower abdomen � If abnormalities found then follow-up with colonoscopy
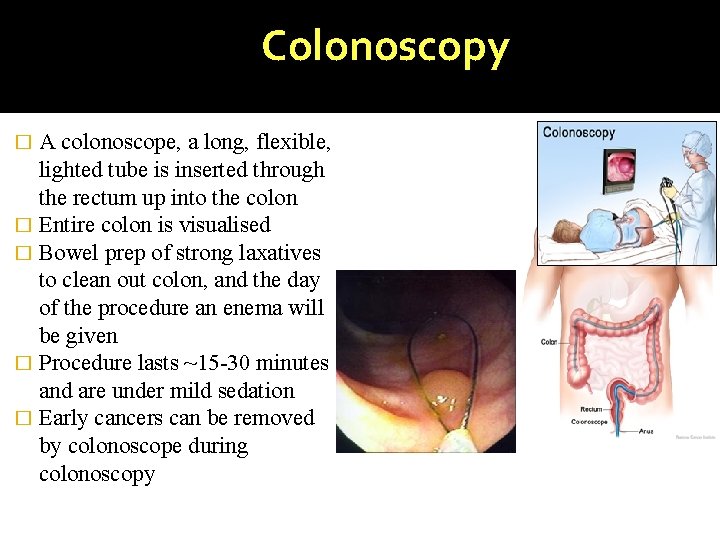
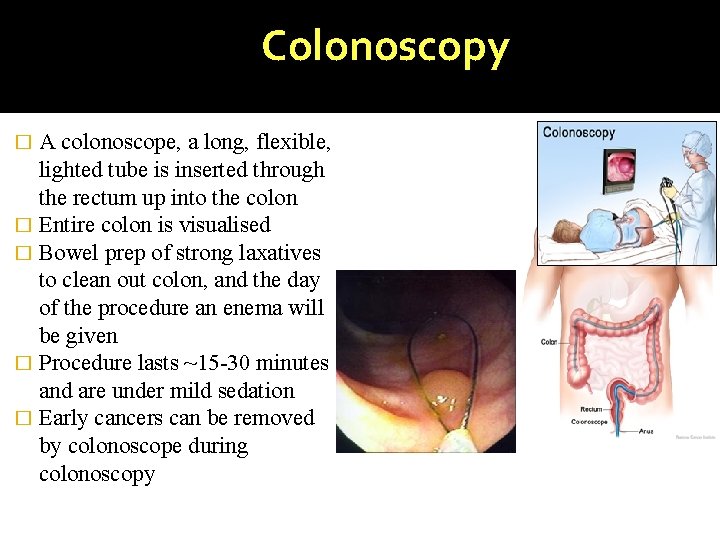
Colonoscopy A colonoscope, a long, flexible, lighted tube is inserted through the rectum up into the colon � Entire colon is visualised � Bowel prep of strong laxatives to clean out colon, and the day of the procedure an enema will be given � Procedure lasts ~15 -30 minutes and are under mild sedation � Early cancers can be removed by colonoscope during colonoscopy �
INVESTIGATIONS (CONTD) �If left supraclavicular lymph node is palpable, FNAC may aid in the diagnosis �CT scan abdomen & pelvis – to see local spread & invasion, size & extent, stage, nodal status & liver secondaries �Liver Function Tests
TREATMENT
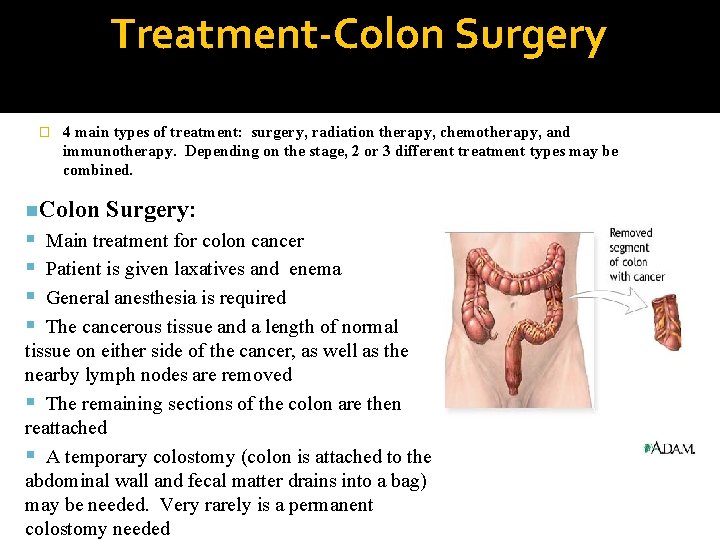
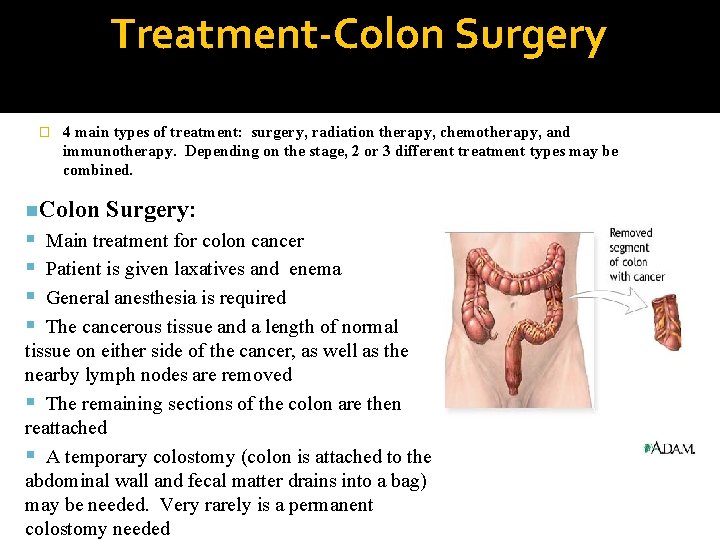
Treatment-Colon Surgery � 4 main types of treatment: surgery, radiation therapy, chemotherapy, and immunotherapy. Depending on the stage, 2 or 3 different treatment types may be combined. n. Colon Surgery: Main treatment for colon cancer Patient is given laxatives and enema General anesthesia is required The cancerous tissue and a length of normal tissue on either side of the cancer, as well as the nearby lymph nodes are removed The remaining sections of the colon are then reattached A temporary colostomy (colon is attached to the abdominal wall and fecal matter drains into a bag) may be needed. Very rarely is a permanent colostomy needed
RIGHT SIDED GROWTH �Right radical hemicolectomy with Ileo-transverse anastomosis �Structures removed – ü Terminal 6 cm of ileum ü Caecum & appendix ü Ascending colon ü 1/3 rd of transverse colon ü Lymph nodes(epicolic, paracolic, intermediate) �In inoperable right sided growth, ileotransverse anastomosis is done
TRANSVERSE COLON GROWTH �Extended right hemicolectomy �Includes division of right colic, middle colic arteries at their origin, removal of terminal 6 cm ileum, ascending & transverse colon, anastomosing terminal ileum & proximal part of descending colon �Alternatively transverse colon with both flexures can be removed followed by colocolic anastomosis
LEFT SIDED EARLY GROWTH �Left radical hemicolectomy is done �Here left ½ of transverse colon & descending colon is removed along with lymph nodes
LEFT SIDED STENOSING GROWTH �Presents with acute intestinal obstruction �Initially colostomy is done � 3 -6 weeks later formal procedure is done colostomy closure 8 weeks later with
MULTIPLE SYNCHRONOUS PRIMARIES IN THE COLON Total abdominal colectomy with ileorectal anastomosis SURGICAL TREATMENT OF LIVER SECONDARIES In solitary liver secondary segmental hepatic resection is done In case of multiple secondaries confined to one lobe of liver, hemihepatectomy
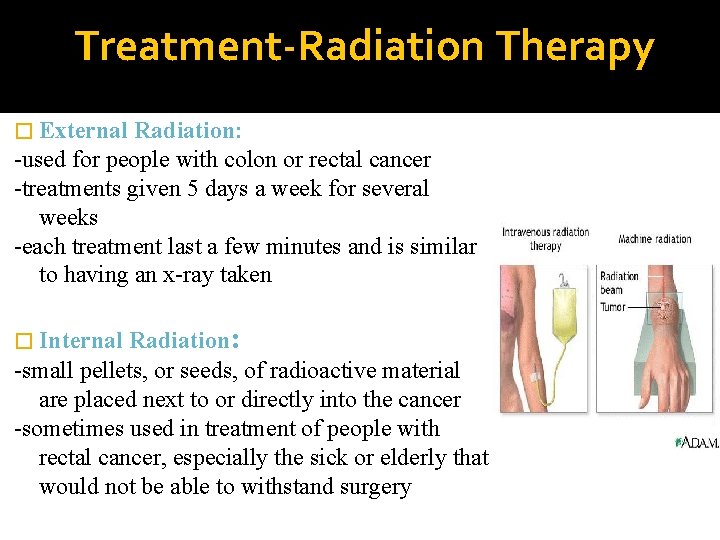
Treatment-Radiation Therapy -Treatment with high energy rays (such as xrays) to kill or shrink cancer cells -May be external radiation (from outside of the body) or radioactive materials placed directly in the tumor (internal or implant radiation) -Adjuvant treatment (after surgery)-radiation is given to kill small areas of the cancer that are hard to see -Neoadjuvant treatment (before surgery)radiation shrinks the tumor if the size or location of the tumor makes surgery difficult
-Radiation can be used to alleviate symptoms of advanced cancer including: intestinal blockage, bleeding, or pain. -Main use for colon cancer: when cancer has attached to an internal organ or the lining of the abdomen, radiation is used to insure that all cancer cells left behind from surgery are destroyed -Main use for rectal cancer: radiation is given to prevent cancer from coming back to the place of origin, and to treat local recurrences causing symptoms of pain -Radiation is seldom used for metastatic colon cancer
Treatment-Radiation Therapy � External Radiation: -used for people with colon or rectal cancer -treatments given 5 days a week for several weeks -each treatment last a few minutes and is similar to having an x-ray taken Radiation: -small pellets, or seeds, of radioactive material are placed next to or directly into the cancer -sometimes used in treatment of people with rectal cancer, especially the sick or elderly that would not be able to withstand surgery � Internal
CHEMOTHERAPY INDICATIONS Ø Positive nodes Ø T 4 lesions Ø Venous spread Ø Signet cell type Ø Poorly differentiated tumor Ø Changes in CEA level
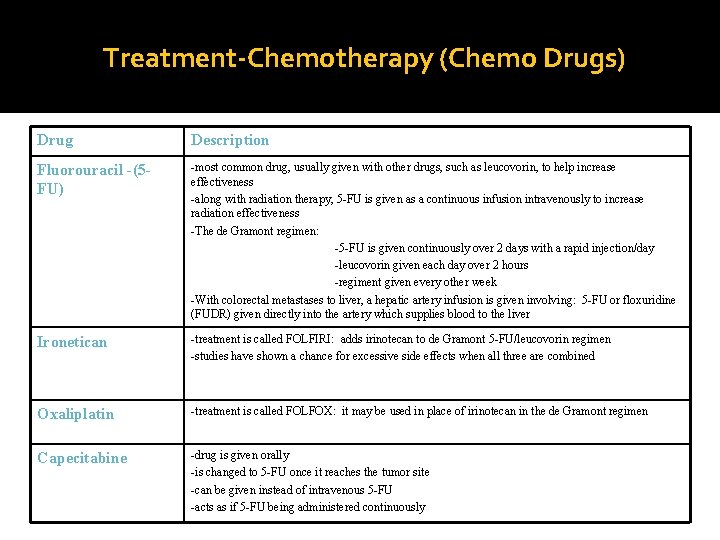
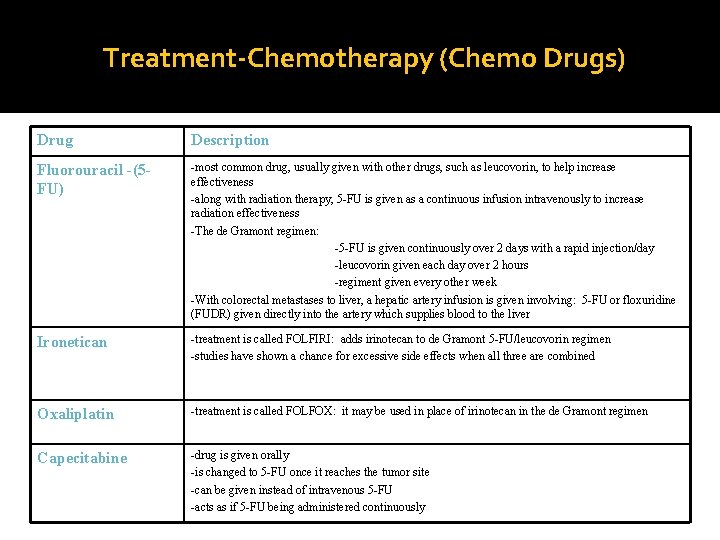
Treatment-Chemotherapy (Chemo Drugs) Drug Description Fluorouracil -(5 FU) -most common drug, usually given with other drugs, such as leucovorin, to help increase effectiveness -along with radiation therapy, 5 -FU is given as a continuous infusion intravenously to increase radiation effectiveness -The de Gramont regimen: -5 -FU is given continuously over 2 days with a rapid injection/day -leucovorin given each day over 2 hours -regiment given every other week -With colorectal metastases to liver, a hepatic artery infusion is given involving: 5 -FU or floxuridine (FUDR) given directly into the artery which supplies blood to the liver Ironetican -treatment is called FOLFIRI: adds irinotecan to de Gramont 5 -FU/leucovorin regimen -studies have shown a chance for excessive side effects when all three are combined Oxaliplatin -treatment is called FOLFOX: it may be used in place of irinotecan in the de Gramont regimen Capecitabine -drug is given orally -is changed to 5 -FU once it reaches the tumor site -can be given instead of intravenous 5 -FU -acts as if 5 -FU being administered continuously
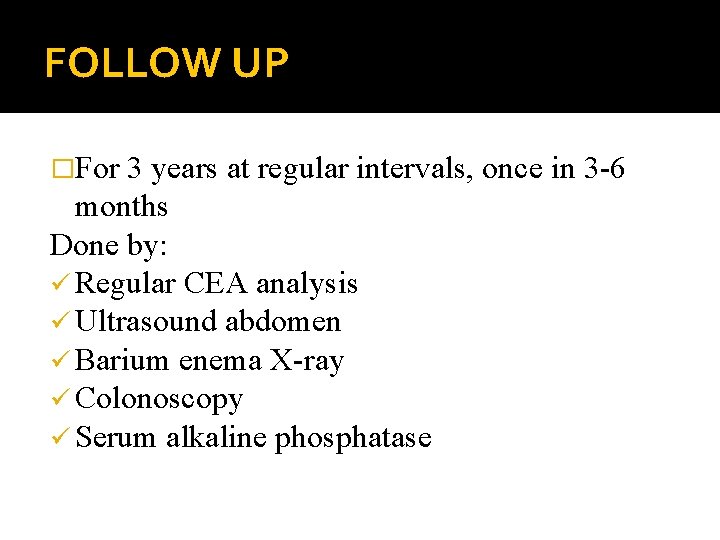
FOLLOW UP �For 3 years at regular intervals, once in 3 -6 months Done by: ü Regular CEA analysis ü Ultrasound abdomen ü Barium enema X-ray ü Colonoscopy ü Serum alkaline phosphatase
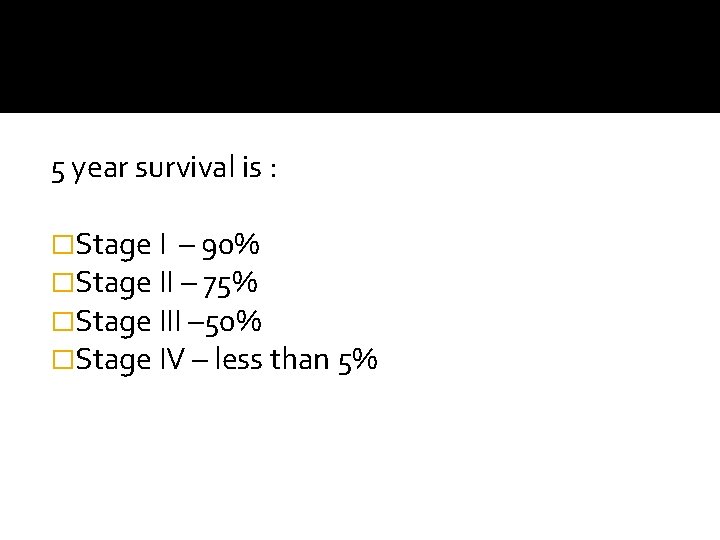
5 year survival is : �Stage I – 90% �Stage II – 75% �Stage III – 50% �Stage IV – less than 5%