COLLECTING SOCIAL DETERMINANTS OF HEALTH DATA USING PRAPARE





















- Slides: 57
COLLECTING SOCIAL DETERMINANTS OF HEALTH DATA USING PRAPARE TO REDUCE DISPARITIES, IMPROVE OUTCOMES AND TRANSFORM CARE PROTOCOL FOR RESPONDING TO AND ASSESSING PATIENTS’ ASSETS, RISKS, AND EXPERIENCES This project was made possible with funding from: Presented by: Tuyen Tran Association of Asian Pacific Community Health Organizations April 24, 2017 © 2016. National Association of Community Health Centers, Inc. , Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association. PRAPARE and its resources are proprietary information of NACHC and its partners, intended for use by NACHC, its partners, and authorized recipients. Do not publish, copy, or distribute this information in part of whole without written consent from NACHC. 1
PRESENTATION OBJECTIVES 1. Present AAPCHO’s collaboration in PRAPARE 1. Discuss the importance of documenting and addressing social determinants of health for improving patient and population health 2. Describe the PRAPARE protocol and how it was developed and implemented in four different Electronic Health Records at health centers nationally 3. Learn about free resources and information about how to get started in data collection on the social determinants of health 2
Association of Asian Pacific Community Health Organizations (AAPCHO) Non-profit, national association established in 1987 with a mission to improve health status and access of Asian Americans, Native Hawaiians and other Pacific Islanders. Represents 35 community health organizations, mostly health centers serving primarily underserved Asian Americans, Native Hawaiians and other Pacific Islanders (AA&NHPI). BPHC funded National Cooperative Agreement holder providing T/TA to health centers serving AA&NHPI.

STORYTELLING WITH OUR DATA SELECTED SDOH DATA
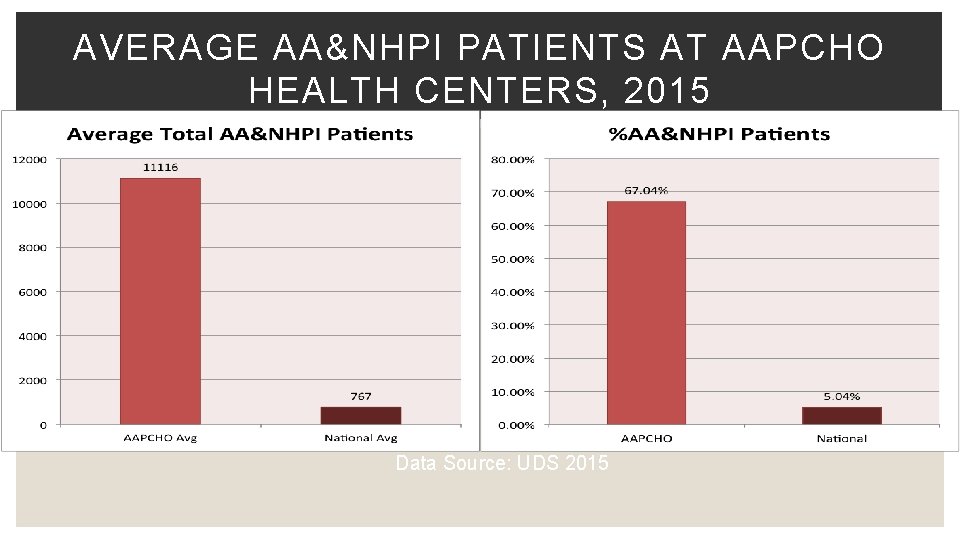
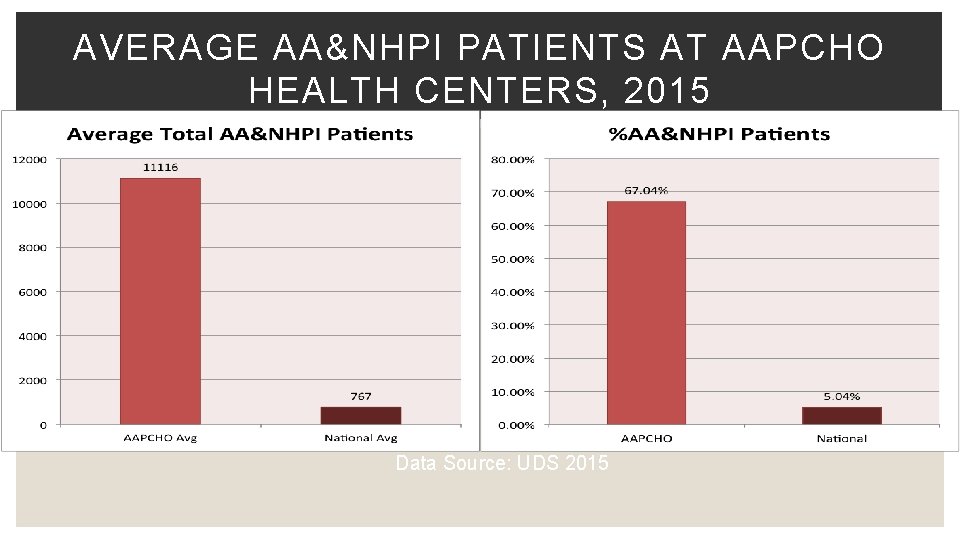
AVERAGE AA&NHPI PATIENTS AT AAPCHO HEALTH CENTERS, 2015 Data Source: UDS 2015
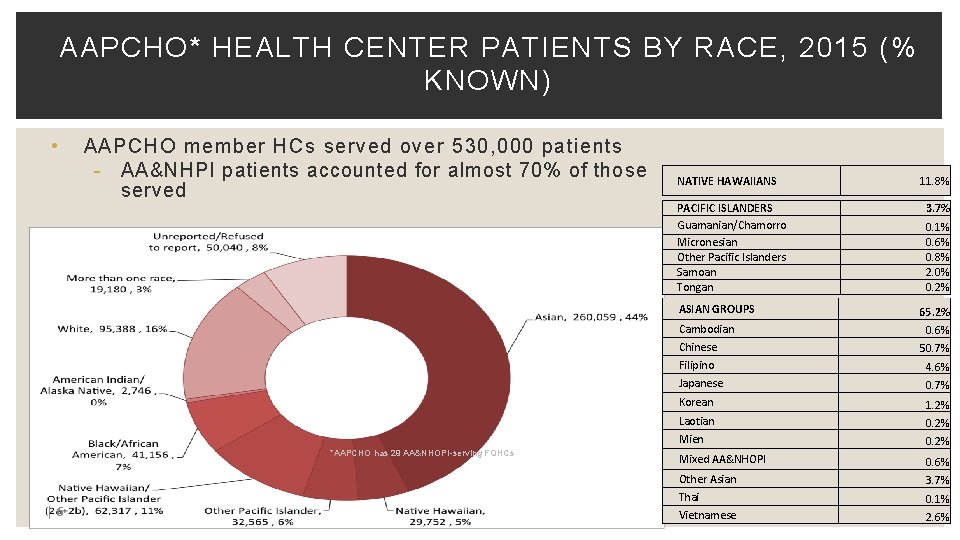
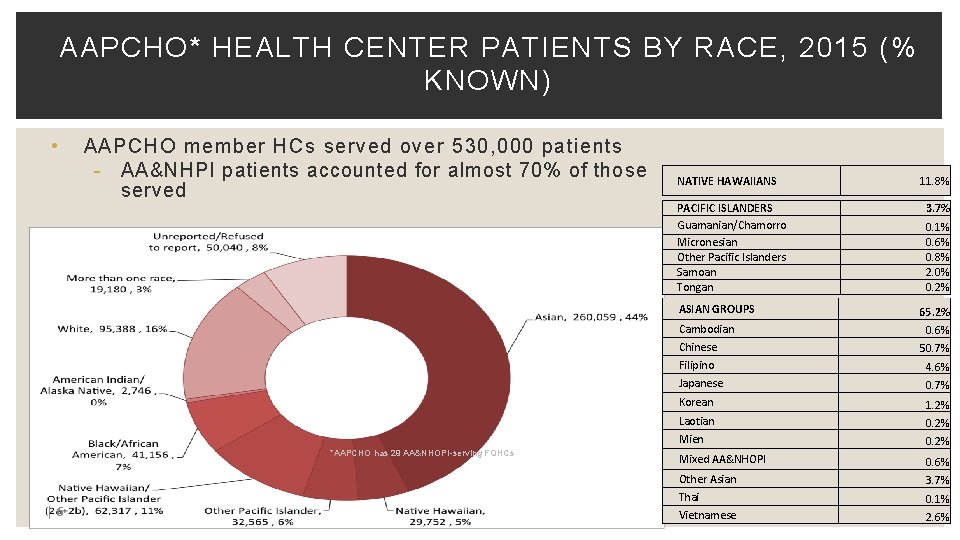
AAPCHO* HEALTH CENTER PATIENTS BY RACE, 2015 (% KNOWN) • AAPCHO member HCs served over 530, 000 patients - AA&NHPI patients accounted for almost 70% of those served NATIVE HAWAIIANS PACIFIC ISLANDERS Guamanian/Chamorro Micronesian Other Pacific Islanders Samoan Tongan ASIAN GROUPS Cambodian *AAPCHO has 29 AA&NHOPI-serving FQHCs |6 11. 8% 3. 7% 0. 1% 0. 6% 0. 8% 2. 0% 0. 2% 65. 2% 0. 6% Chinese 50. 7% Filipino 4. 6% Japanese 0. 7% Korean 1. 2% Laotian 0. 2% Mien 0. 2% Mixed AA&NHOPI 0. 6% Other Asian 3. 7% Thai 0. 1% Vietnamese 2. 6%
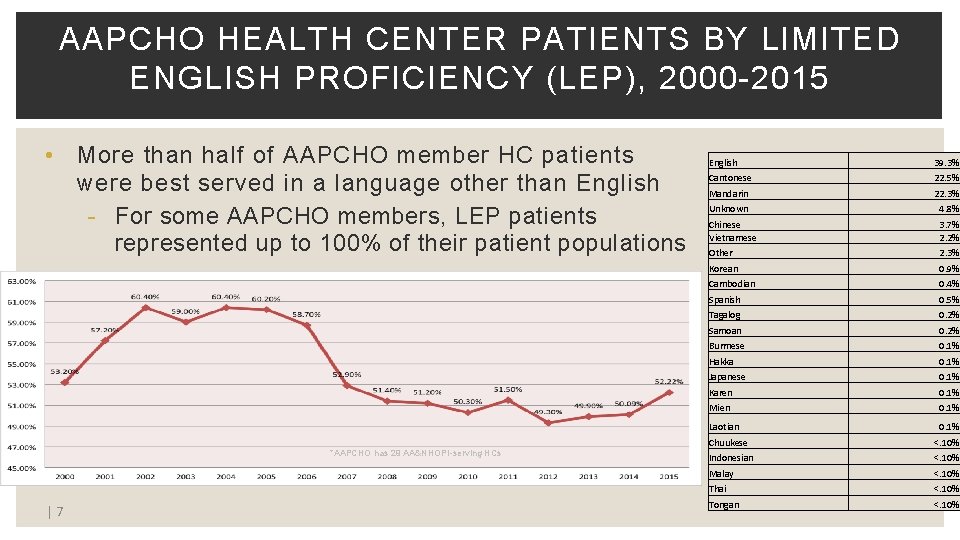
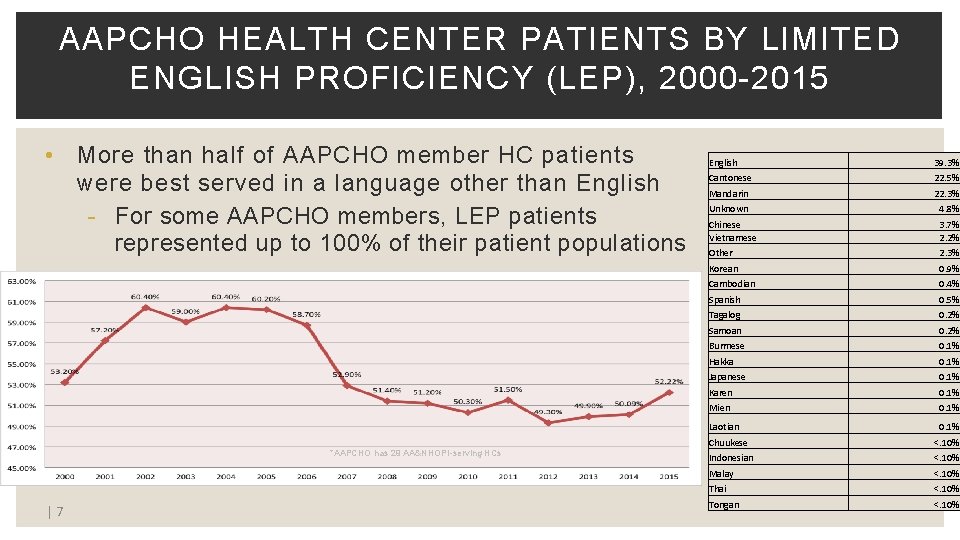
AAPCHO HEALTH CENTER PATIENTS BY LIMITED ENGLISH PROFICIENCY (LEP), 2000 -2015 • More than half of AAPCHO member HC patients were best served in a language other than English - For some AAPCHO members, LEP patients represented up to 100% of their patient populations *AAPCHO has 29 AA&NHOPI-serving HCs |7 English 39. 3% Cantonese 22. 5% Mandarin 22. 3% Unknown 4. 8% Chinese Vietnamese 3. 7% 2. 2% Other 2. 3% Korean 0. 9% Cambodian 0. 4% Spanish 0. 5% Tagalog 0. 2% Samoan 0. 2% Burmese 0. 1% Hakka 0. 1% Japanese 0. 1% Karen 0. 1% Mien 0. 1% Laotian 0. 1% Chuukese <. 10% Indonesian <. 10% Malay <. 10% Thai <. 10% Tongan <. 10%
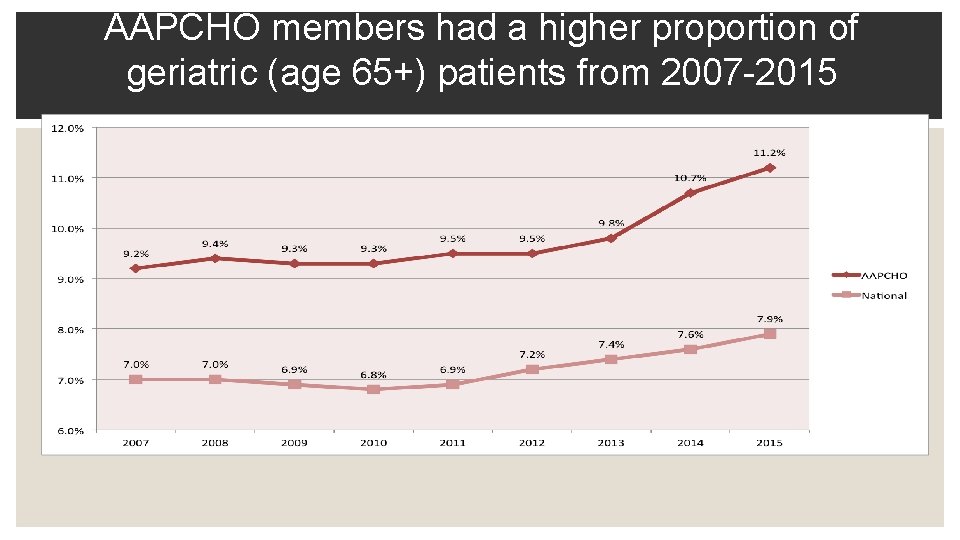
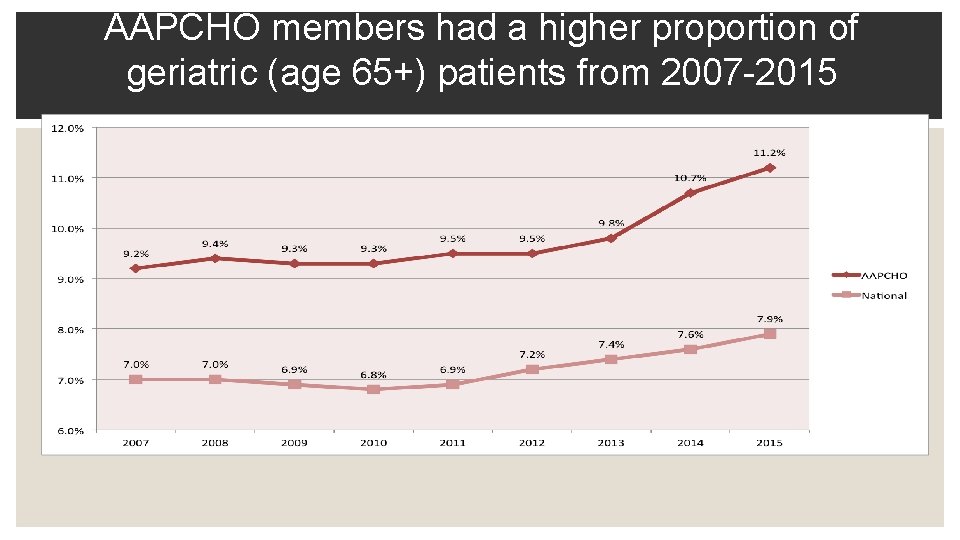
AAPCHO members had a higher proportion of geriatric (age 65+) patients from 2007 -2015
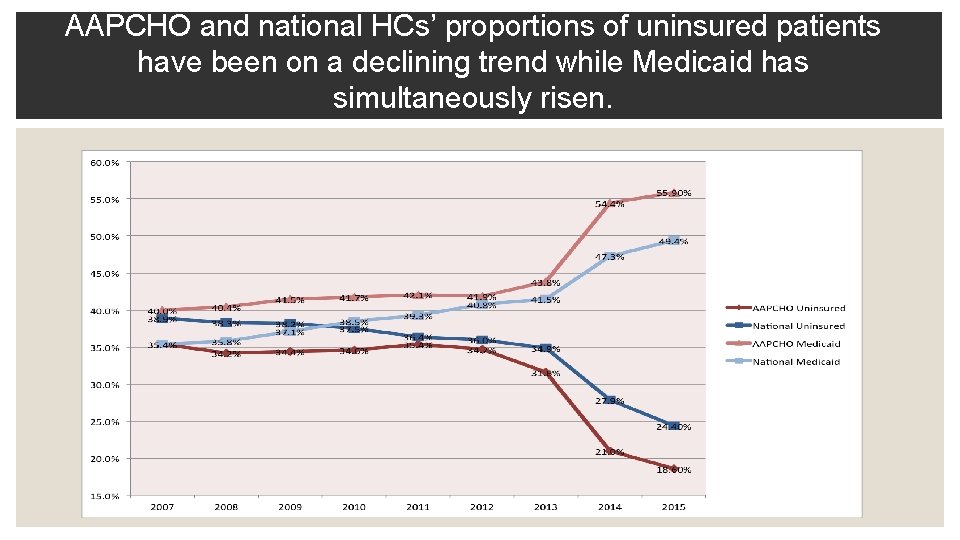
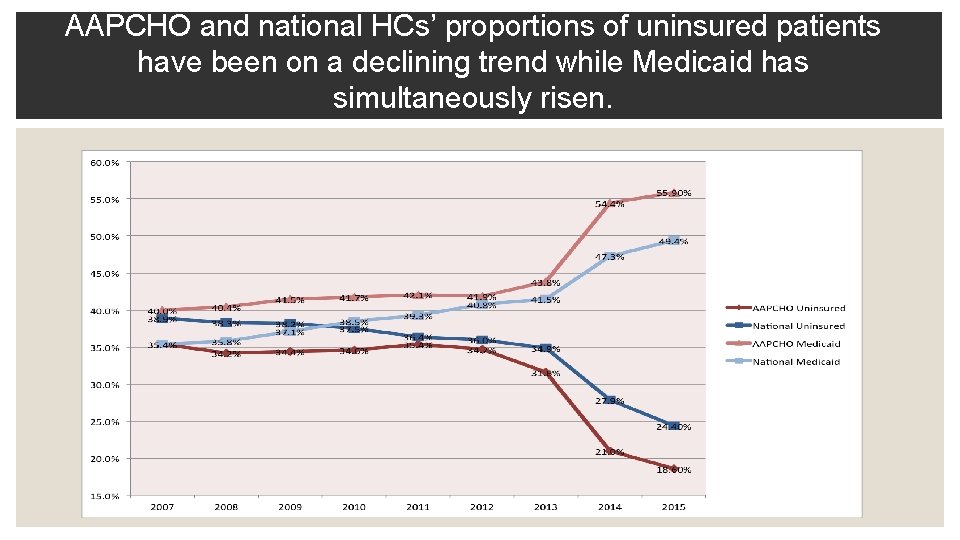
AAPCHO and national HCs’ proportions of uninsured patients have been on a declining trend while Medicaid has simultaneously risen.
SELECTED CLINICAL DATA

SELECTED CLINICAL DIFFERENCES AAPCHO( %) National ( %) % Hepatitis B 2. 6% 0. 2% % TB 0. 09% 0. 04% % Abnormal breast findings 0. 83% 0. 6% % Abnormal cervical findings 0. 94% 0. 8%

SELECTED QUALITY OF CARE MEASURES | 12 AAPCHO ( %) National (%) Cervical cancer screening 58. 3% 56. 0% Hypertensive patients with controlled BP 67. 6% 68. 7% Diabetic patients with Hb. A 1 c > 9 26. 1% 29. 8%

SELECTED ENCOUNTER & CO$T DATA

AAPCHO HAD A HIGHER AVERAGE NUMBER OF ENABLING SERVICE (ES) ENCOUNTERS COMPARED TO THE NATIONAL AVERAGE
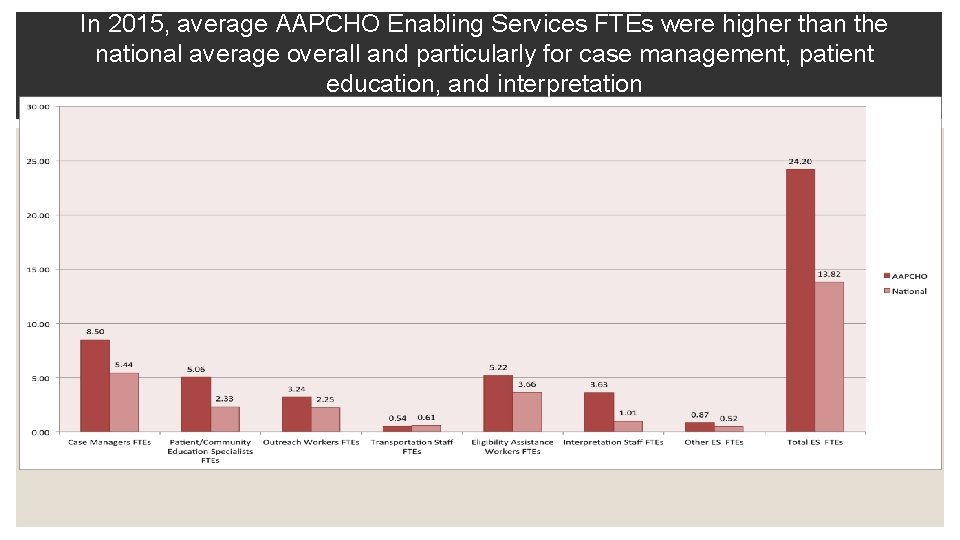
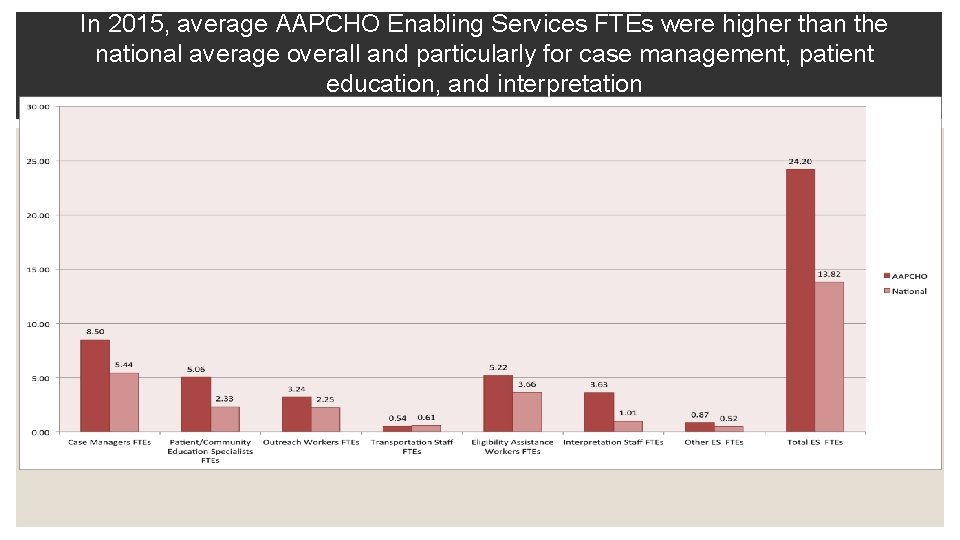
In 2015, average AAPCHO Enabling Services FTEs were higher than the national average overall and particularly for case management, patient education, and interpretation

AAPCHO total costs for enabling services per HC were higher than national average
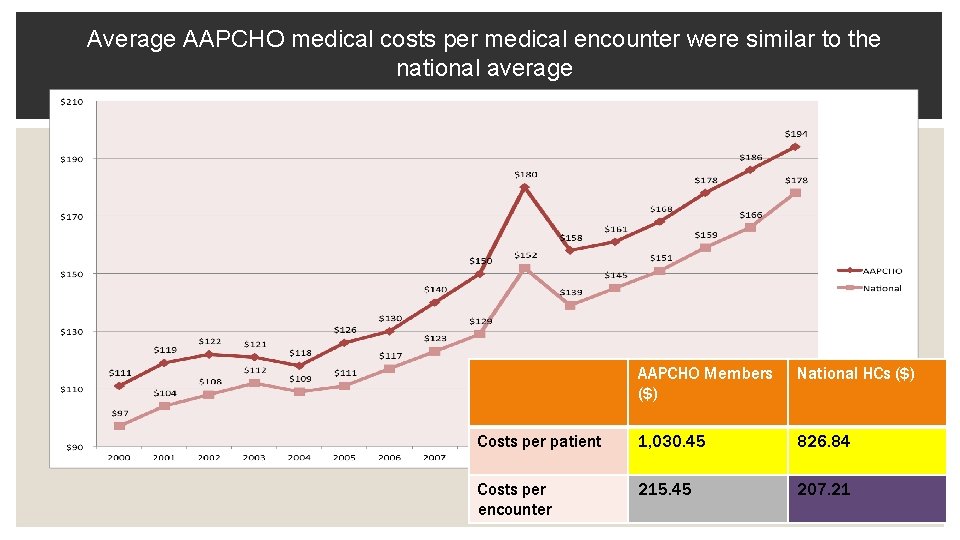
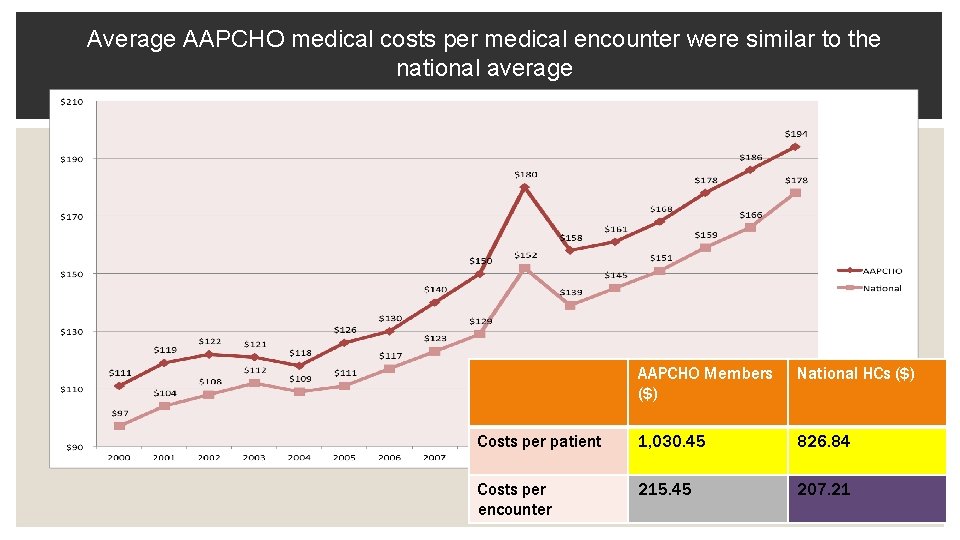
Average AAPCHO medical costs per medical encounter were similar to the national average AAPCHO Members ($) National HCs ($) Costs per patient 1, 030. 45 826. 84 Costs per encounter 215. 45 207. 21
CONTRIBUTION OF NON-CLINICAL SERVICES • AAPCHO centers have better health outcomes compared to national averages for pap test, hypertension, and diabetes. This may be due to the higher number of enabling services and resulting quality outcomes provided by AAPCHO centers compared to national health centers.
ENABLING SERVICES (ES) • non-clinical services that are provided to health center patients that promote, support and assist in the delivery of health care and facilitate access to quality patient care. -NACHC/MGMA 2000

AAPCHO’S ENABLING SERVICES ACCOUNTABILITY PROJECT (ESAP) PARTICIPATING CENTERS: Charles B. Wang Community Health Center NY, NY International Community Health Services Seattle, WA Kalihi-Palama Health Center Honolulu, HI Waianae Coast Comprehensive Health Center Waianae, HI
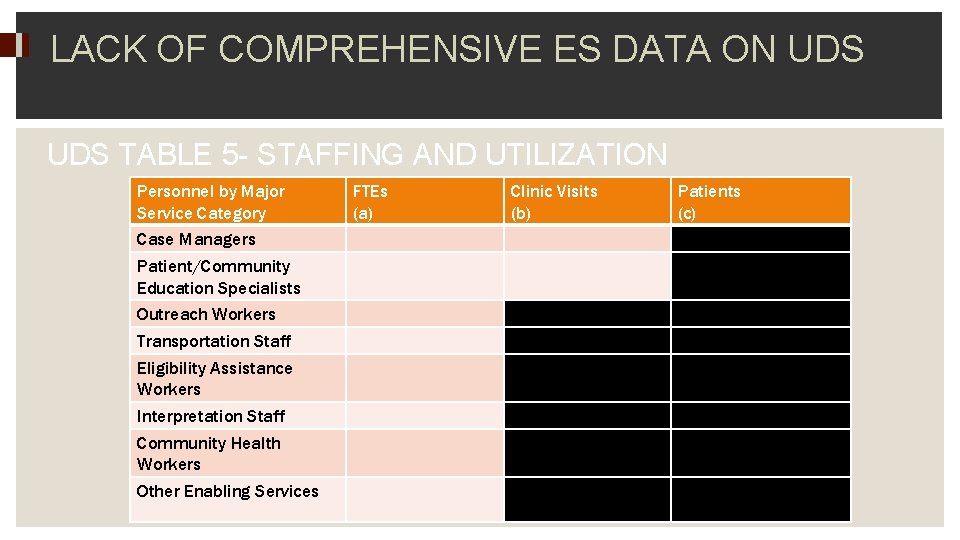
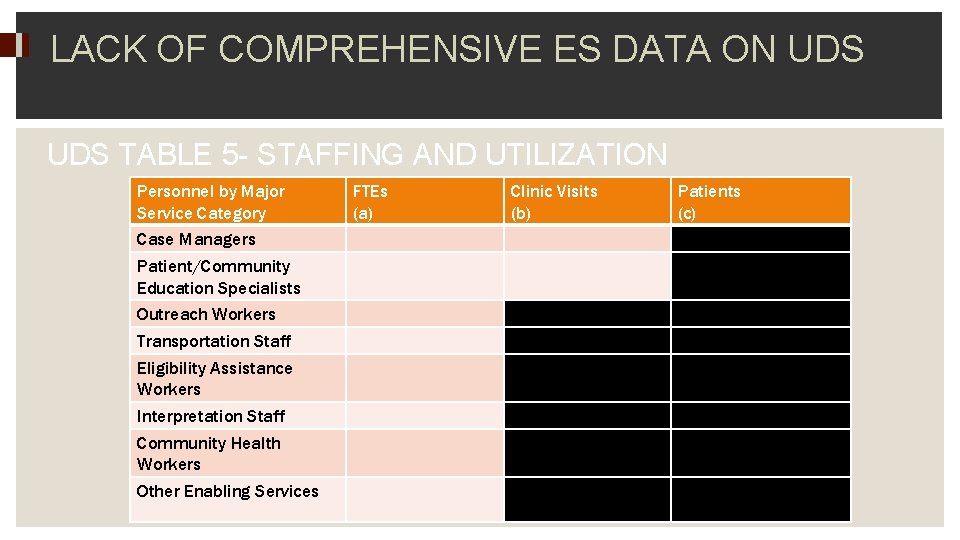
LACK OF COMPREHENSIVE ES DATA ON UDS TABLE 5 - STAFFING AND UTILIZATION Personnel by Major Service Category Case Managers Patient/Community Education Specialists Outreach Workers Transportation Staff Eligibility Assistance Workers Interpretation Staff Community Health Workers Other Enabling Services FTEs (a) Clinic Visits (b) Patients (c)

ESAP GOALS • Develop standard data collection protocol and database for ES at health centers nationally • Describe utilization of ES at health centers and the patients who use them • Evaluate the impact of enabling services on health access, outcomes and utilization of primary care • Disseminate findings to health centers and policy makers to guide effective resource allocation • Facilitate research and expansion opportunities to other health centers and networks
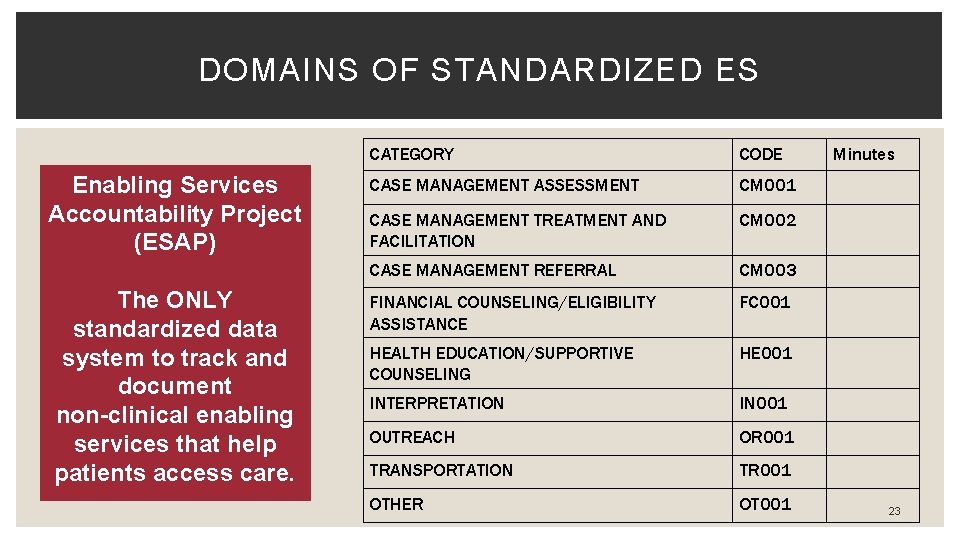
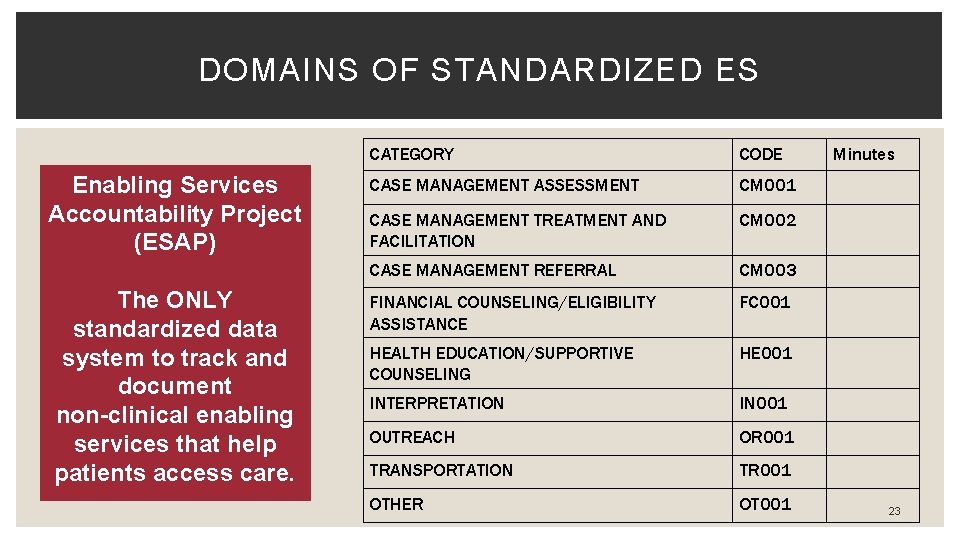
DOMAINS OF STANDARDIZED ES Enabling Services Accountability Project (ESAP) The ONLY standardized data system to track and document non-clinical enabling services that help patients access care. CATEGORY CODE CASE MANAGEMENT ASSESSMENT CM 001 CASE MANAGEMENT TREATMENT AND FACILITATION CM 002 CASE MANAGEMENT REFERRAL CM 003 FINANCIAL COUNSELING/ELIGIBILITY ASSISTANCE FC 001 HEALTH EDUCATION/SUPPORTIVE COUNSELING HE 001 INTERPRETATION IN 001 OUTREACH OR 001 TRANSPORTATION TR 001 OTHER OT 001 Minutes 23

SAMPLE ENABLING SERVICES EMR TEMPLATE

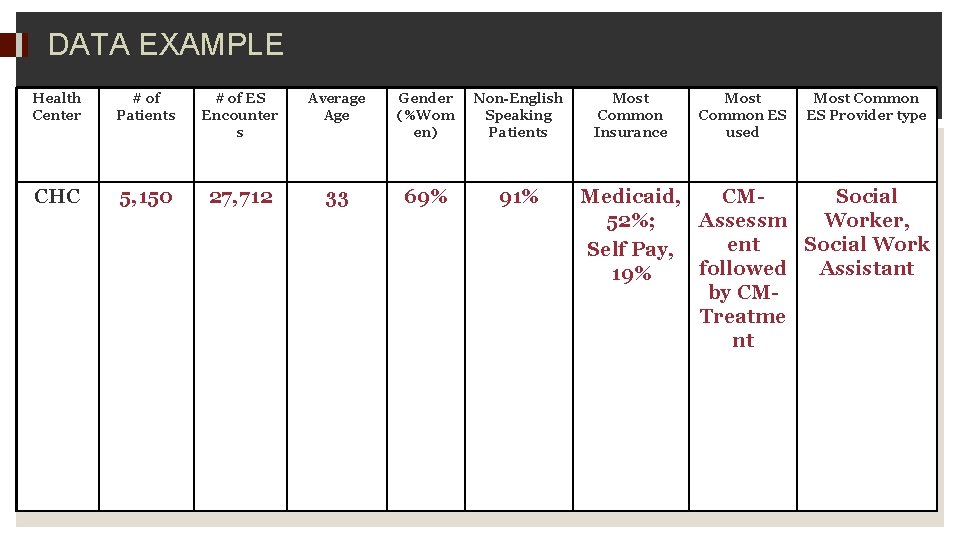
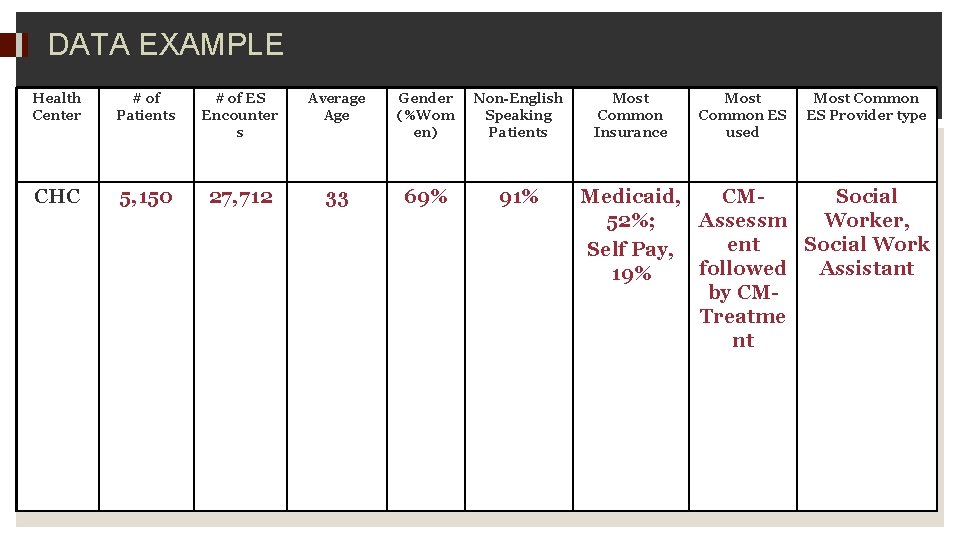
DATA EXAMPLE Health Center # of Patients # of ES Encounter s Average Age Gender (%Wom en) Non-English Speaking Patients CHC 5, 150 27, 712 33 69% 91% Most Common Insurance Most Common ES used Most Common ES Provider type Medicaid, CMSocial 52%; Assessm Worker, ent Social Work Self Pay, followed Assistant 19% by CMTreatme nt
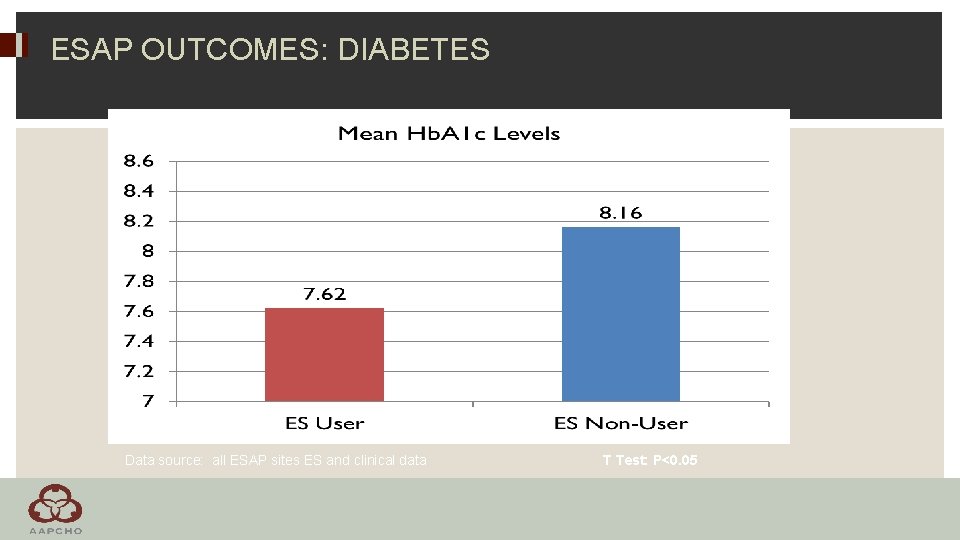
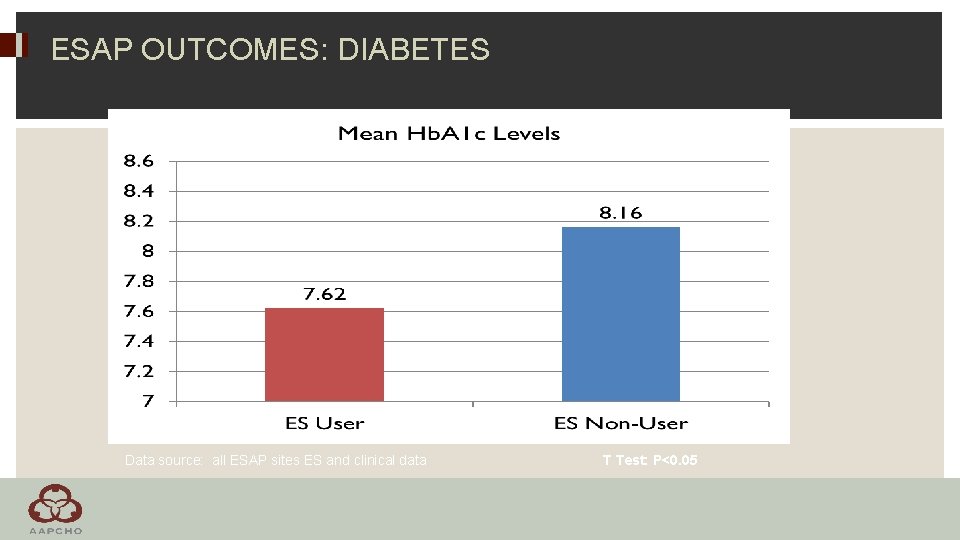
ESAP OUTCOMES: DIABETES Data source: all ESAP sites ES and clinical data T Test: P<0. 05

ESAP OUTCOMES: APPROPRIATE CHILD IMMUNIZATION Data source: all ESAP sites ES and clinical data
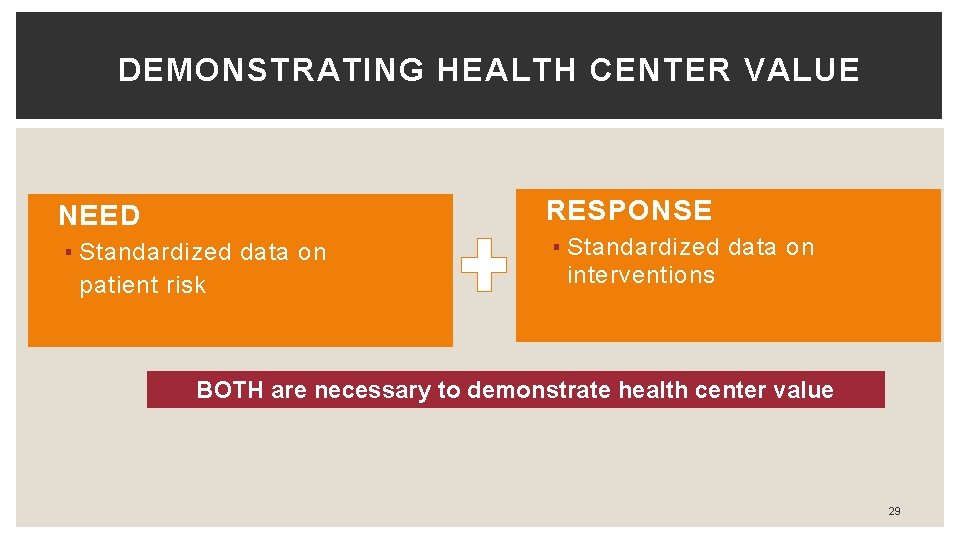
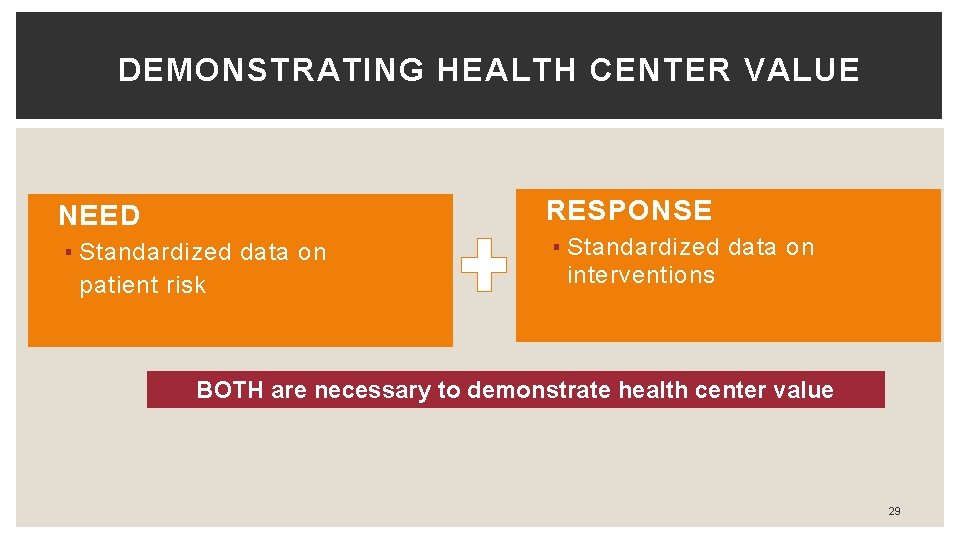
DEMONSTRATING HEALTH CENTER VALUE �RESPONSE �NEED ▪ Standardized data on patient risk ▪ Standardized data on interventions BOTH are necessary to demonstrate health center value 29

WHY IS IT IMPORTANT TO COLLECT STANDARDIZED DATA ON THE SOCIAL DETERMINANTS OF HEALTH? 30
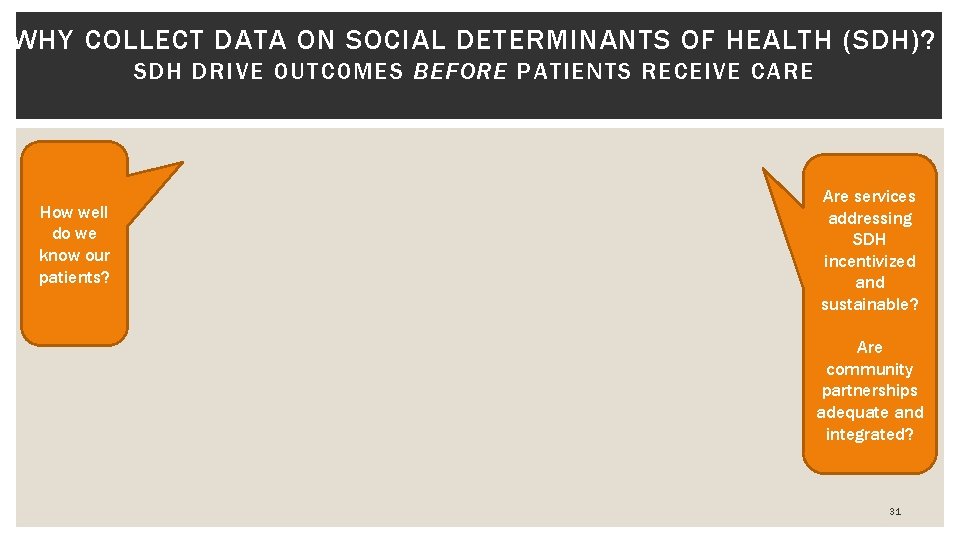
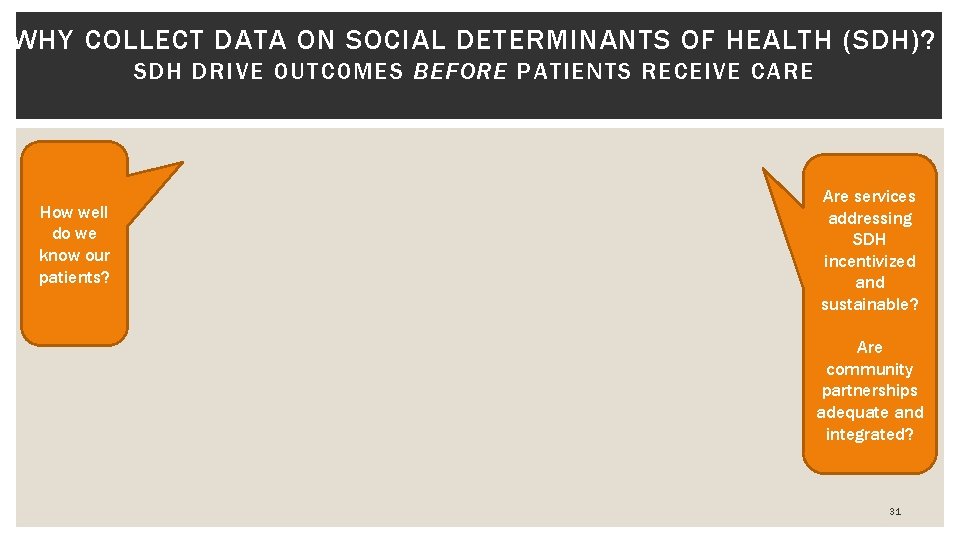
WHY COLLECT DATA ON SOCIAL DETERMINANTS OF HEALTH (SDH)? SDH DRIVE OUTCOMES BEFORE PATIENTS RECEIVE CARE How well do we know our patients? Are services addressing SDH incentivized and sustainable? Are community partnerships adequate and integrated? 31

WHY IS ADDRESSING SOCIAL DETERMINANTS OF HEALTH (SDH) IMPORTANT TO COMMUNITY HEALTH CENTERS? 1. Provide Better Care 2. Reduced Costs 3. Community Connection 4. Standardized data to see the big picture
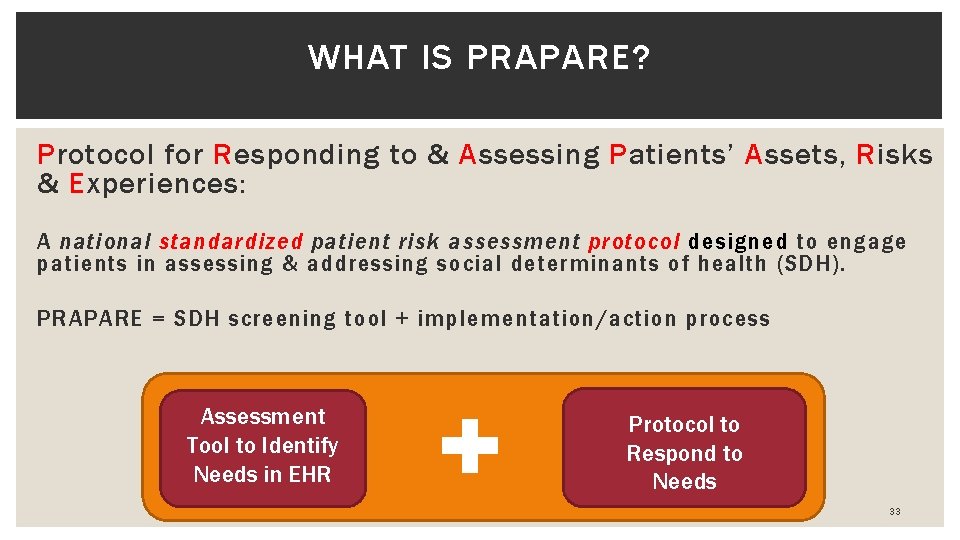
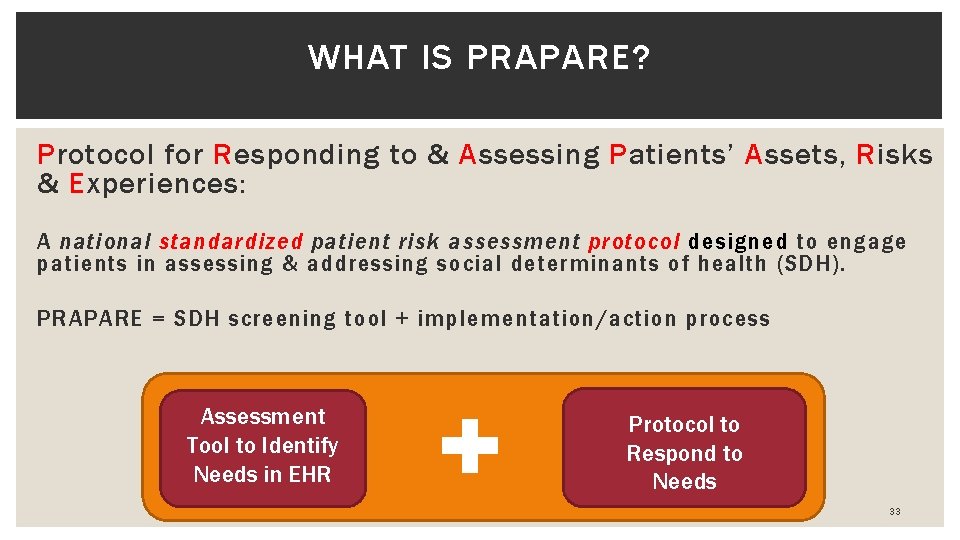
WHAT IS PRAPARE? Protocol for Responding to & Assessing Patients’ Assets, Risks & Experiences: A national standardized patient risk assessment protocol designed to engage patients in assessing & addressing social determinants of health (SDH). PRAPARE = SDH screening tool + implementation/action process Assessment Tool to Identify Needs in EHR + Protocol to Respond to Needs 33

PRAPARE WAS DESIGNED TO ACCELERATE SYSTEMIC CHANGE for insured and uninsured patients 34
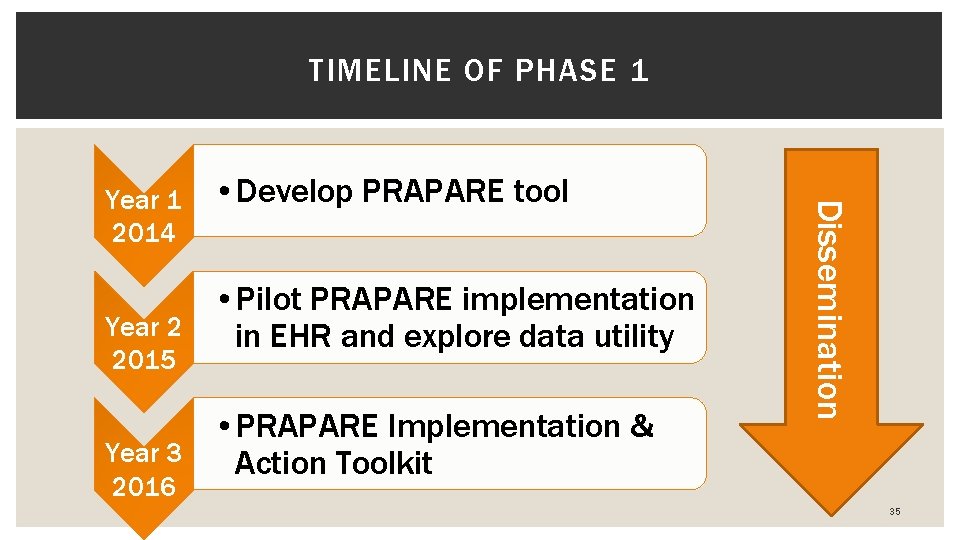
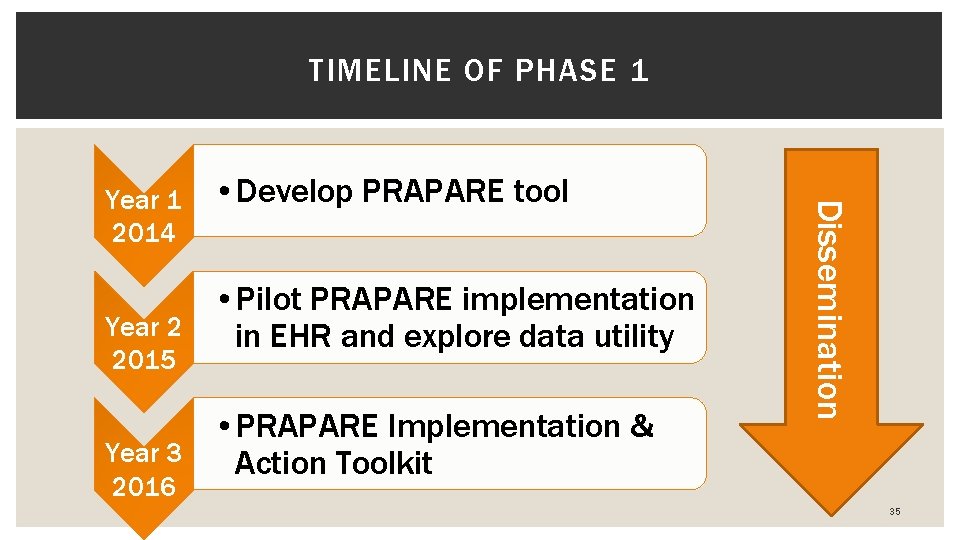
TIMELINE OF PHASE 1 • Develop PRAPARE tool • Pilot PRAPARE implementation Year 2 in EHR and explore data utility 2015 • PRAPARE Implementation & Year 3 Action Toolkit Dissemination Year 1 2014 2016 35

DEVELOPING PRAPARE Experience of Existing Protocols Stakeholder Feedback Literature Review Aligned with National Initiatives: * Healthy People 2020 * ICD-10 * Meaningful Use Stage 3 * NQF on Risk Adjustment Burden of Data Collection Actionability Criteria Sensitivity Identified 15 Core Social Determinants of Health 36
37
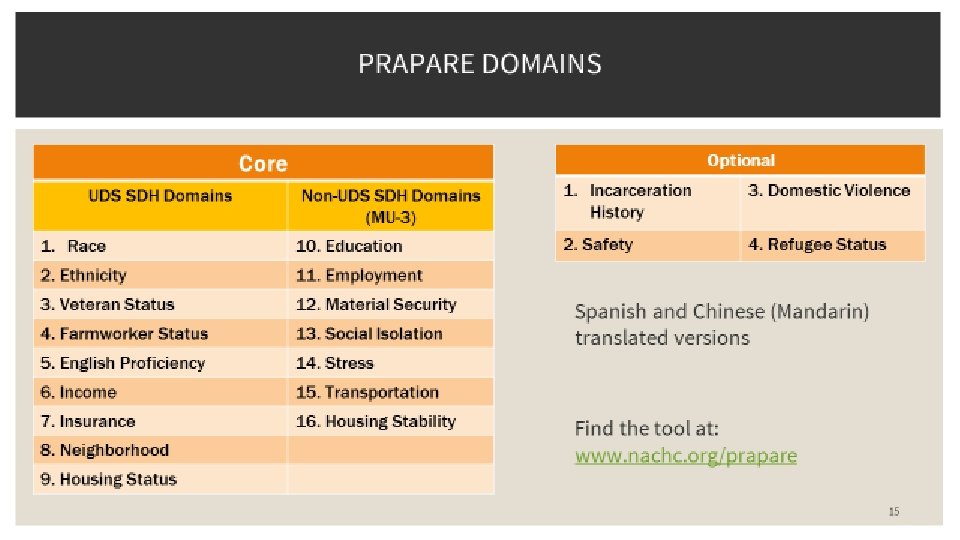
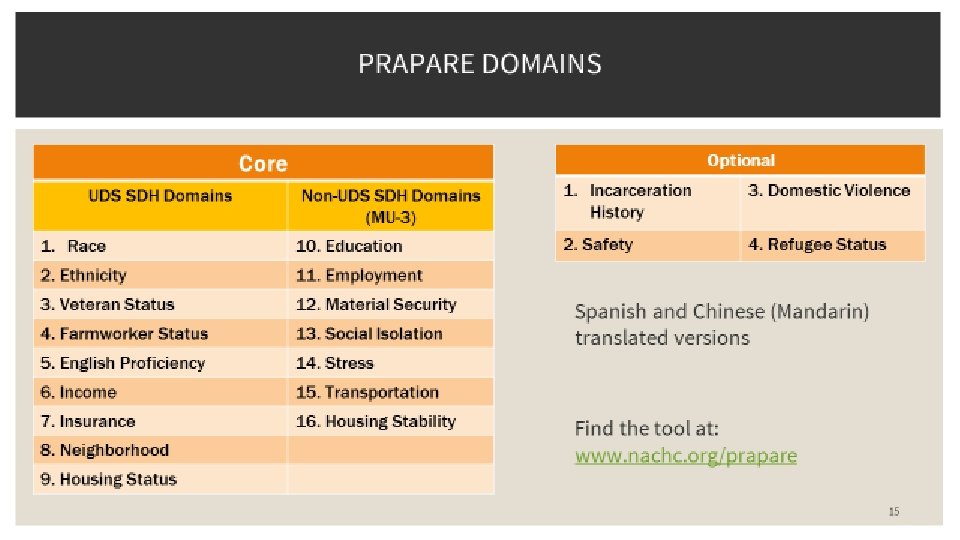
WHAT MAKES PRAPARE UNIQUE AND FEASIBLE 17 core questions § 9 of which already collected by health centers through federal reporting (UDS) § All align with national initiatives Design § Vetted and stakeholder engaged development process § In the EHR to facilitate assessment & interventions (free templates) § Conversation starter and patient-centered § Common core yet flexible: § Able to make more granular and/or add questions § Focus on standardizing the need, not question § Can be used in combination with other tools/data 38

PRAPARE ALIGNS WITH OTHER NATIONAL INITIATIVES PRAPARE Domain UDS Race/Ethnicity X Farmworker Status X Veteran Status X English Proficiency X Income X Insurance Status X Housing X ICD-10 IOM Meaningful Use (2 and 3) HP 2020 RWJF County Health X X Seeking comments X X X Education X X X Employment X X X Material Security X X X Social Integration X X X Stress X X Transportation Also includes neighborhood and optional questions (incarceration history, refugee status, safety, domestic violence) X

41
42

WHAT WE’VE LEARNED FROM IMPLEMENTATION 43
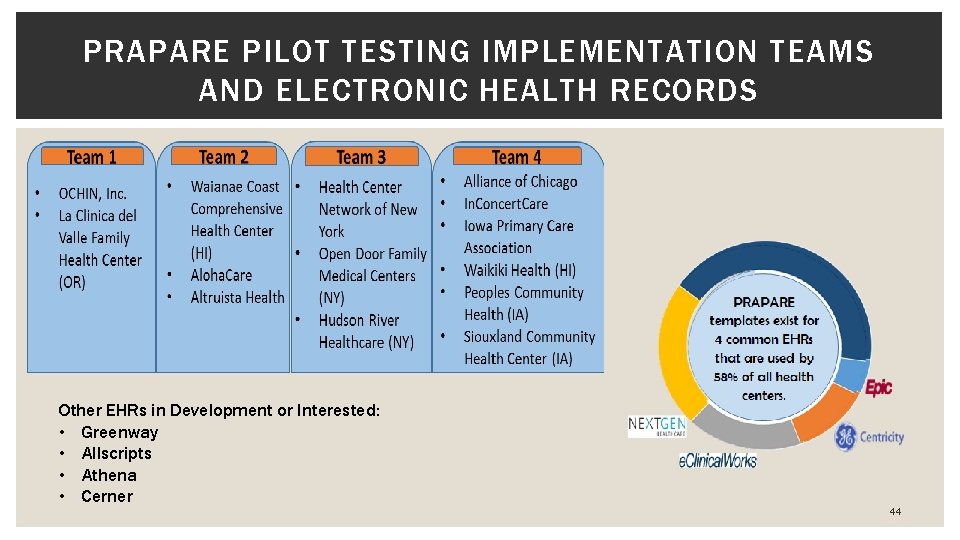
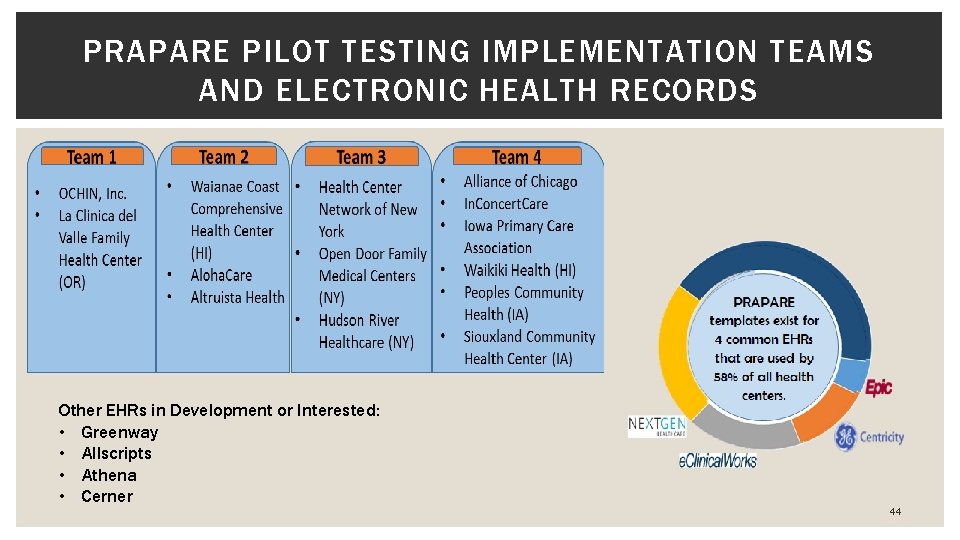
PRAPARE PILOT TESTING IMPLEMENTATION TEAMS AND ELECTRONIC HEALTH RECORDS Other EHRs in Development or Interested: • Greenway • Allscripts • Athena • Cerner 44
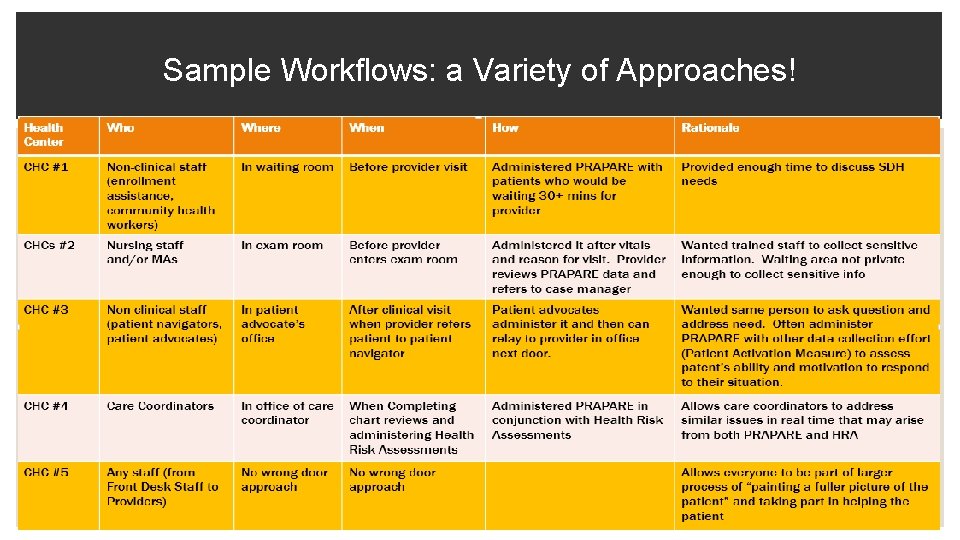
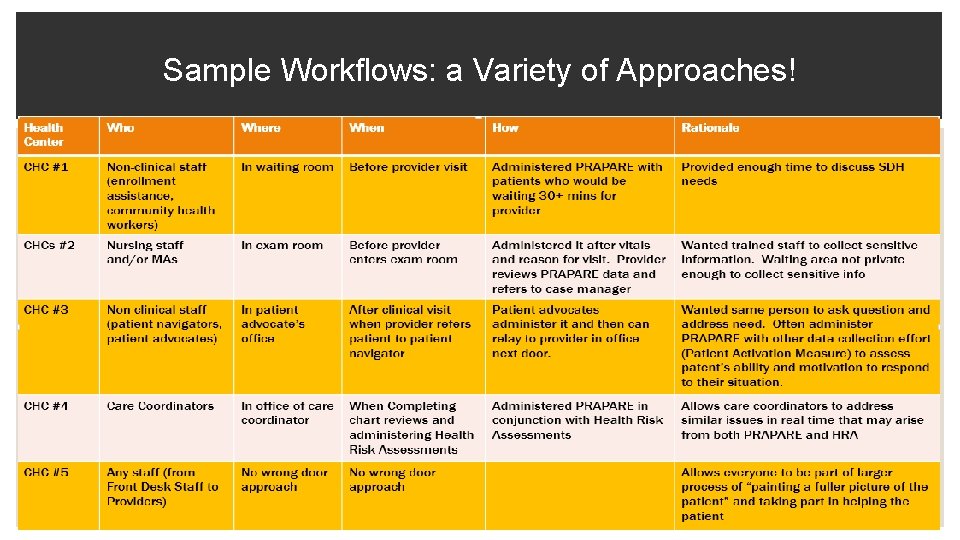
Sample Workflows: a Variety of Approaches! 45
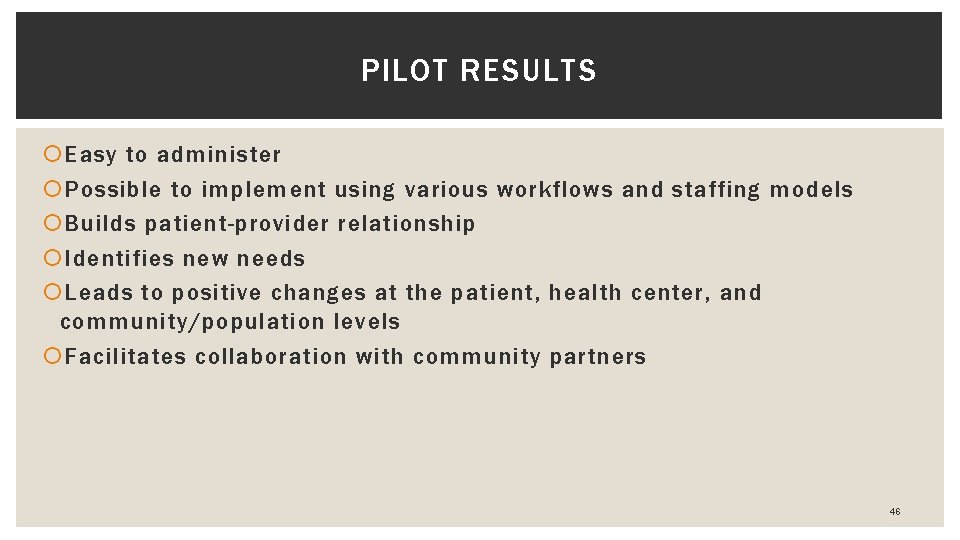
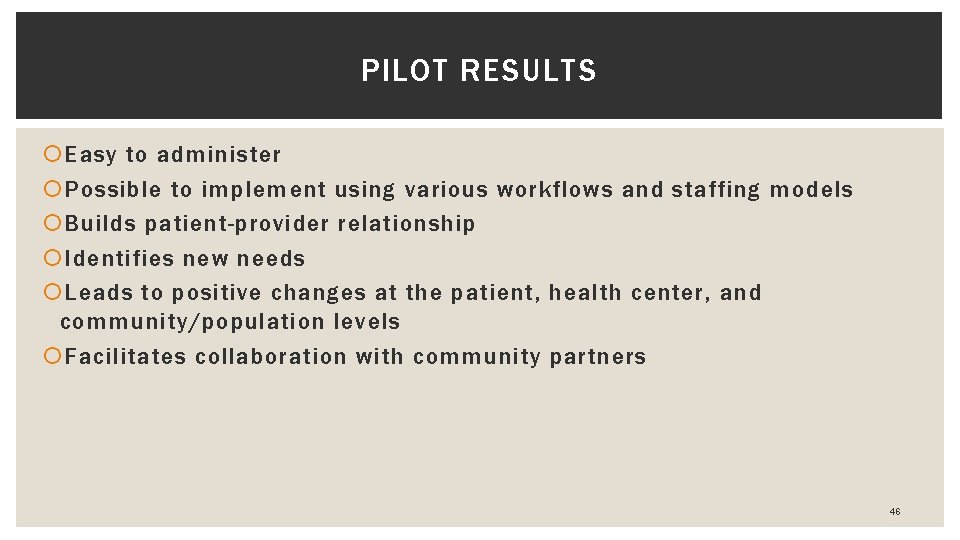
PILOT RESULTS Easy to administer Possible to implement using various workflows and staffing models Builds patient-provider relationship Identifies new needs Leads to positive changes at the patient, health center, and community/population levels Facilitates collaboration with community partners 46

PILOT DATA RESULTS SDH risks vary by community Most common risks*: § High stress § Having less than a high school education § Uninsured § Unemployed § Preference for language other than English But, patients are very socially integrated, § Half of patients see people they care about 5+ times a week * Excludes low income
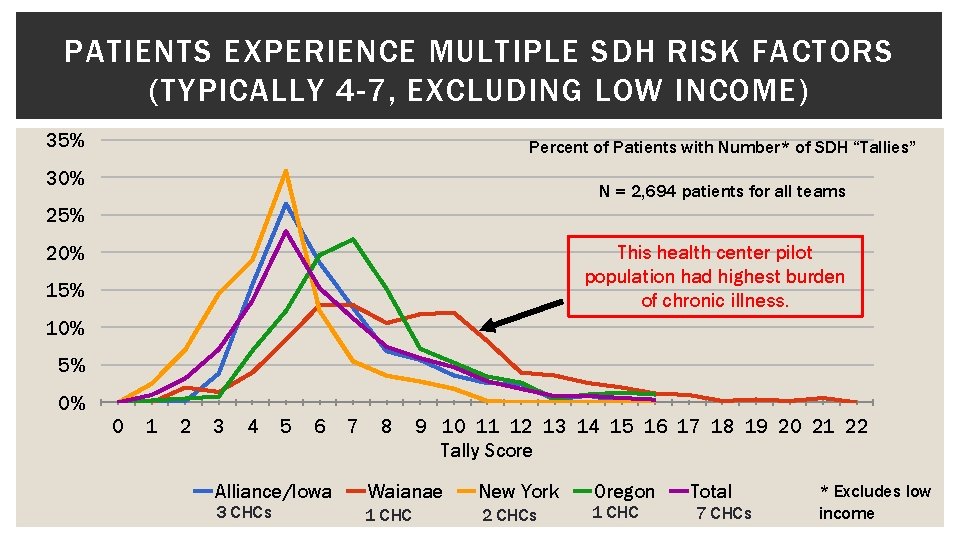
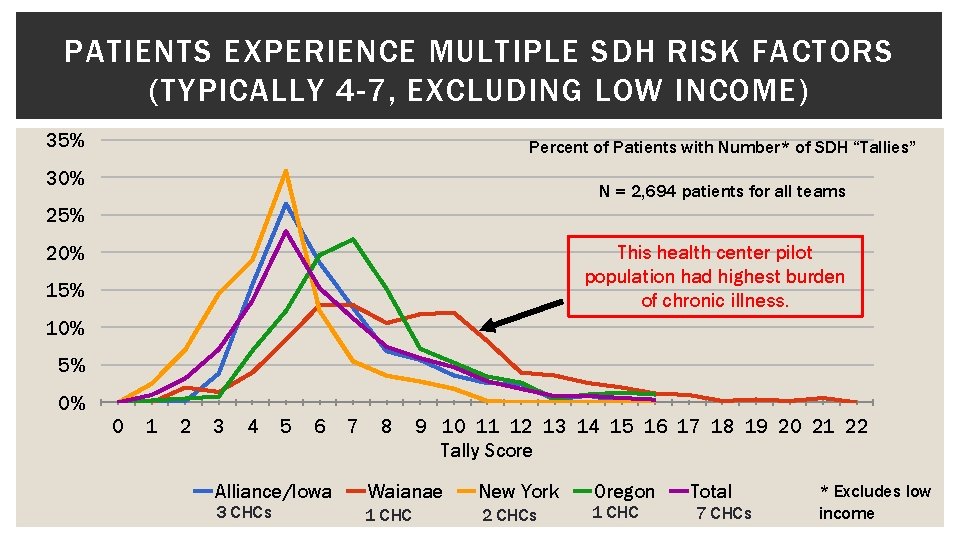
PATIENTS EXPERIENCE MULTIPLE SDH RISK FACTORS (TYPICALLY 4 -7, EXCLUDING LOW INCOME) 35% Percent of Patients with Number* of SDH “Tallies” 30% N = 2, 694 patients for all teams 25% This health center pilot population had highest burden of chronic illness. 20% 15% 10% 5% 0% 0 1 2 3 4 5 6 Alliance/Iowa 3 CHCs 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Tally Score Waianae New York 1 CHC 2 CHCs Oregon 1 CHC Total 7 CHCs * Excludes low income
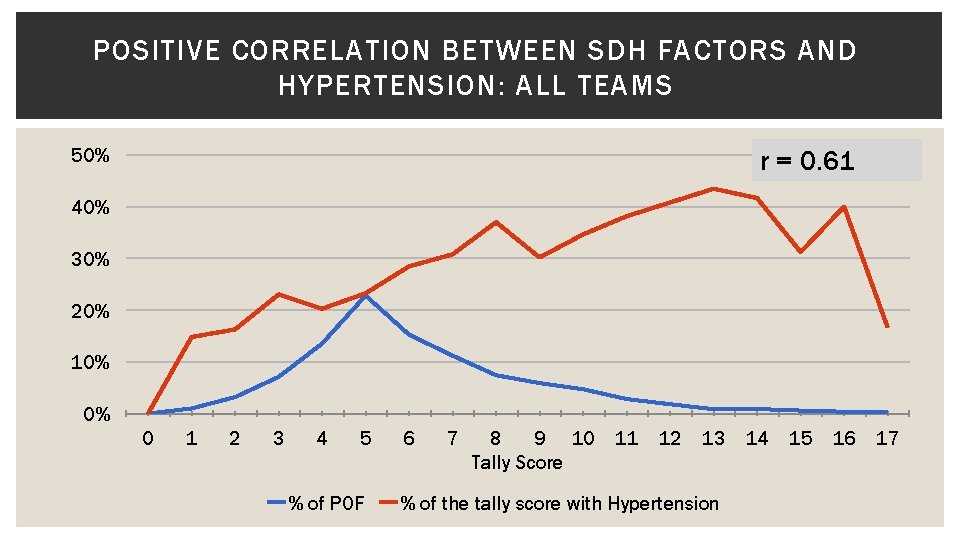
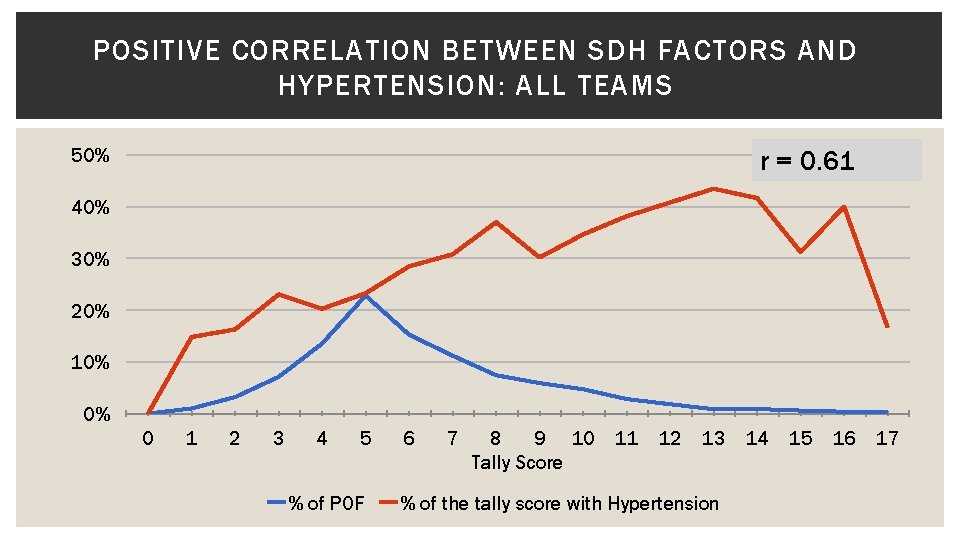
POSITIVE CORRELATION BETWEEN SDH FACTORS AND HYPERTENSION: ALL TEAMS 50% r = 0. 61 40% 30% 20% 10% 0% 0 1 2 3 4 5 % of POF 6 7 8 9 10 Tally Score 11 12 13 % of the tally score with Hypertension 14 15 16 17

HOW PRAPARE DATA HAS BEEN USED TO IMPROVE CARE DELIVERY AND HEALTH OUTCOMES Better Understand INDIVIDUAL Patient’s Socioeconomic Situation Better Understand Needs of Patient POPULATION Drive STATE and NATIONAL Care Transformation Build services in-house for same-day use as clinic visit (children’s book corner, food banks, clothing closets, wellness center, transportation shuttle, etc) Build partnerships with local community based organizations to offer bi-directional referrals and discounts on services (ex: Iowa transportation) Inform both Medicaid and Medicare ACO discussions (ex: Iowa, New York) Create risk score to inform risk adjustment (ex: Hawaii) Ensure prescriptions and treatment plan match patient’s socioeconomic situation Guide work of local foundations (ex: New York housing) Streamline care management plans for better resource allocation (ex: Hawaii) Inform payment reform and APM discussions with state agencies (e. g. , Medicaid) on caring for complex patients (ex: Oregon, Hawaii) 50
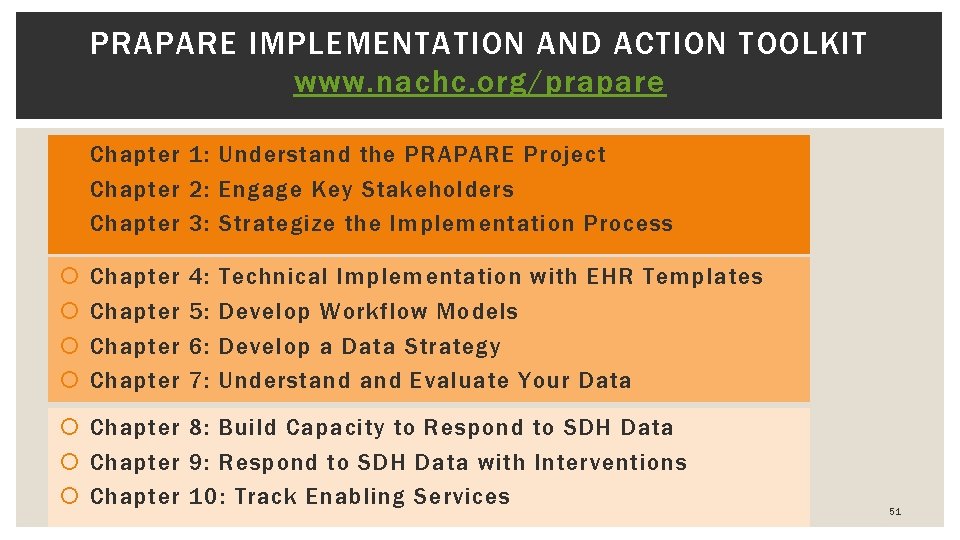
PRAPARE IMPLEMENTATION AND ACTION TOOLKIT www. nachc. org/prapare Chapter 1: Understand the PRAPARE Project Chapter 2: Engage Key Stakeholders Chapter 3: Strategize the Implementation Process Chapter 4: 5: 6: 7: Technical Implementation with EHR Templates Develop Workflow Models Develop a Data Strategy Understand Evaluate Your Data Chapter 8: Build Capacity to Respond to SDH Data Chapter 9: Respond to SDH Data with Interventions Chapter 10: Track Enabling Services 51
PRAPARE READINESS ASSESSMENT Culture of Organization Leadership and Management Workflow Process Improvement Technology Paper form: www. nachc. org/prapare Online form: https: //www. surveymonkey. com/r/PR APARE_Readiness_Assessment 52

PHASE 2: PRAPARE LEARNING AND ACTION NETWORK (PLAN) Build health center capacity to deploy a common, standardized patient-centered SDH assessment protocol Create a PRAPARE community of users with shared learning Accelerate spread of PRAPARE Document impact With support from the Kresge Foundation: Audience Health Centers PCAs/HCCNs Breadth Online PRAPARE Engagement Platform (promote shared learning, track use, provide resources and access to experts) PRAPARE Readiness resources for supporting members Depth PRAPARE Engagement Grants PRAPARE Train the Trainer Academy 53
PRAPARE IS A NATIONAL MOVEMENT • Health centers and/or PCAs in every state including AK have expressed interest in PRAPARE • Health centers in over 30 states including AK downloaded PRAPARE EHR Templates • 7000+ hits on PRAPARE website • Health and hospital systems are interested in PRAPARE 54
RESOURCES AVAILABLE NOW � Visit www. nachc. org/prapare ▪ PRAPARE Tool ▪ PRAPARE Implementation and Action Toolkit ▪ Electronic Health Record PRAPARE Templates ▪ Readiness Assessment ▪ Webinars ▪ PRAPARE Overview ▪ EHR and Workflow-specific � Visit http: //enablingservices. aapcho. org ▪ AAPCHO’s Enabling Services Accountability Project ▪ protocol for data collection of nonclinical enabling services ▪ Enabling Services Data Collection Implementation Guide ▪ White Papers, Best Practices, Studies Contact Tuyen Tran at ttran@aapcho. org ▪ Frequently Asked Questions ▪ Contact: Michelle Jester at mjester@nachc. org 55
HOW QUESTIONS ARE ASKED JUST AS CRITICAL RESOURCES ON EMPATHIC INQUIRY Waianae Demo: https: //youtu. be/i. Qj. J_Qs. Dvm. I OPCA Demo: https: //www. youtube. com/watch? v=9 rfmfs. MMe. EU 56
FOR MORE INFORMATION ON PRAPARE, VISIT www. nachc. org/prapare This project was made possible with funding from: 57
 Prapare score interpretation
Prapare score interpretation What are the 6 main social determinants of health?
What are the 6 main social determinants of health? Matrices and determinants cengage
Matrices and determinants cengage Collecting highly parallel data for paraphrase evaluation
Collecting highly parallel data for paraphrase evaluation Collecting and displaying data
Collecting and displaying data Samples of collecting engineering data
Samples of collecting engineering data Physical environment determinants of health
Physical environment determinants of health Social determinants of personality
Social determinants of personality Social determinants of aggression
Social determinants of aggression Health and social care component 3
Health and social care component 3 Using big data to solve economic and social problems
Using big data to solve economic and social problems Social thinking and social influence in psychology
Social thinking and social influence in psychology Social thinking social influence social relations
Social thinking social influence social relations Tubular lumen
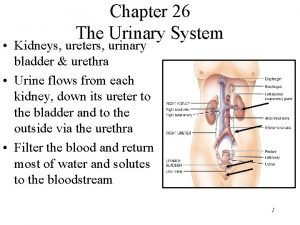
Tubular lumen Thin ascending limb
Thin ascending limb Internal naris
Internal naris Mathsbot starter generator
Mathsbot starter generator Coupon collecting problem
Coupon collecting problem Collecting gas over water
Collecting gas over water Chapter 34 collecting and testing specimens
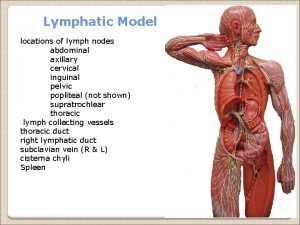
Chapter 34 collecting and testing specimens The lymphatic system consists of
The lymphatic system consists of Collecting gas over water
Collecting gas over water Physics or stamp collecting
Physics or stamp collecting Coin collecting merit badge
Coin collecting merit badge Collect gas over water
Collect gas over water Dr frost maths
Dr frost maths Prize collecting steiner tree
Prize collecting steiner tree Collecting banker
Collecting banker Collecting information and forecasting demand
Collecting information and forecasting demand Questionstag
Questionstag Visceral layer
Visceral layer Collecting ducts
Collecting ducts Collecting duct meaning
Collecting duct meaning Where does most reabsorption occur
Where does most reabsorption occur Collecting ducts
Collecting ducts Peritubular capillaries vs vasa recta
Peritubular capillaries vs vasa recta Collecting duct
Collecting duct Collecting duct meaning
Collecting duct meaning Marketing research and forecasting demand
Marketing research and forecasting demand Handling information in health and social care
Handling information in health and social care What are the determinants of market structure
What are the determinants of market structure Acdc copyright
Acdc copyright Non price determinants of supply
Non price determinants of supply Non price determinants of supply
Non price determinants of supply Non price determinants of supply
Non price determinants of supply Non price determinants of supply
Non price determinants of supply What are the determinants of market structure
What are the determinants of market structure Color 23112006
Color 23112006 Pes curves
Pes curves Define organizational behavior
Define organizational behavior Multiplication of determinants
Multiplication of determinants Types of international assignment in ihrm
Types of international assignment in ihrm What are the 5 determinants of price elasticity of demand
What are the 5 determinants of price elasticity of demand What are the 5 determinants of price elasticity of demand
What are the 5 determinants of price elasticity of demand Midpoint formula economics
Midpoint formula economics Cytoplasmic determinants
Cytoplasmic determinants Determinant of gait
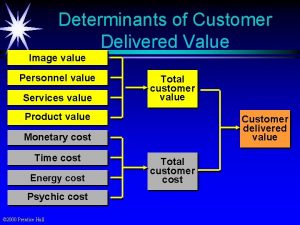
Determinant of gait Determinants of customer delivered value
Determinants of customer delivered value