Cold Agglutinin Disease Patient History 62 year old

- Slides: 14

Cold Agglutinin Disease
Patient History 62 year old female who presented to clinic with a one month history of worsening fatigue and subjective fevers.
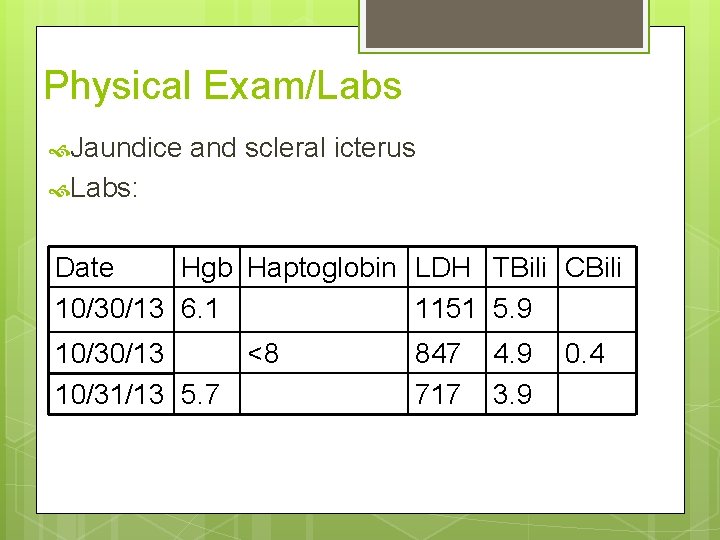
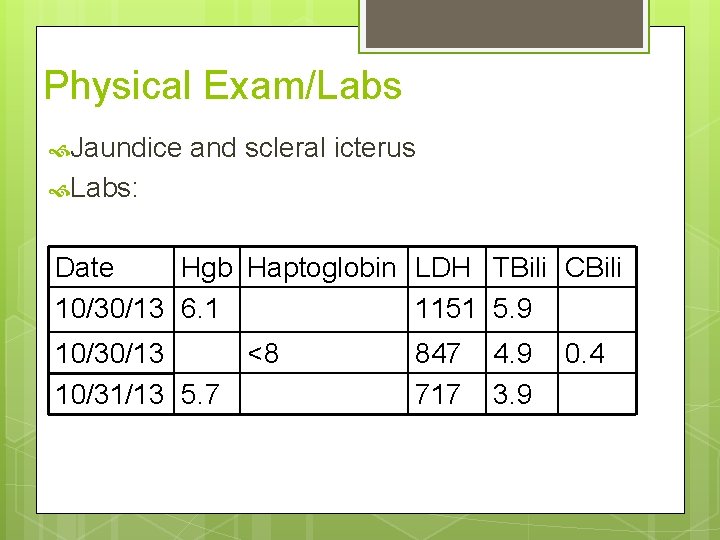
Physical Exam/Labs Jaundice and scleral icterus Labs: Date Hgb Haptoglobin LDH TBili CBili 10/30/13 6. 1 1151 5. 9 10/30/13 <8 10/31/13 5. 7 847 717 4. 9 3. 9 0. 4
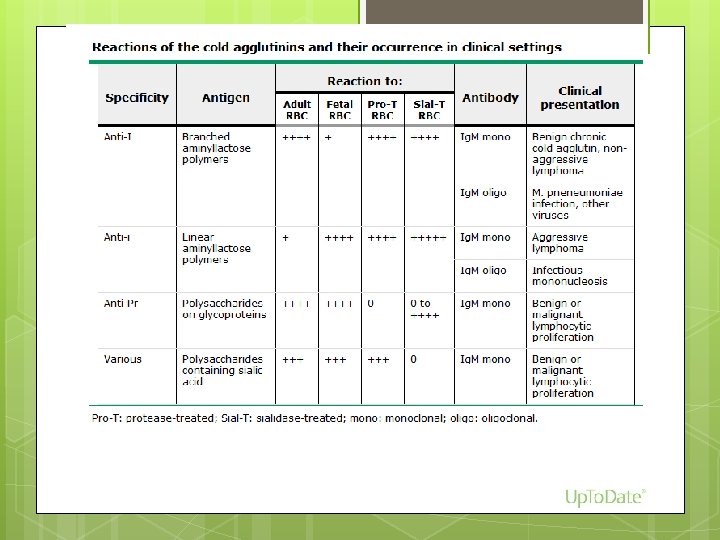
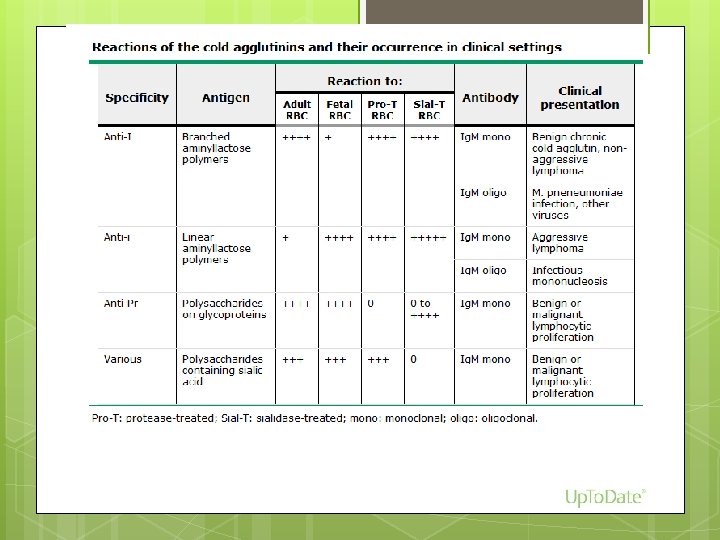
Labs - Previous 4/2012 Presented with exertional fatigue, jaundice, and dark urine and laboratory evidence of hemolysis Antibody screen (pre-warmed): negative Antibody screen (room temperature): positive Direct antiglobulin test (Coomb’s) was positive (+4) for complement fixation and negative for Ig. G The cold agglutinin titer at 4 C is 1: 512. The thermal amplitude is 30 C The specificity of the cold agglutinin is anti I.
Labs- Previous 12/2012 Antibody screen was performed on prewarmed plamsa was negative A cold agglutinin titer showed: anti-I titer at 37 degrees C is 0 anti-I titer at 30 degrees C is 1: 256 the anti-I titer at 4 degrees C is 1: 32768 A DAT was perfomed and was positive for complement (4+) and negative for Ig. G.
Labs - Current Cold (Ig. M) antibody at a titer of 1: 4096 The patient's blood type is B positive. The reverse type is discrepant, likely due to high cold agglutinin titer. Antibody screen was negative A direct antiglobulin test (DAT) was negative for Ig. G and positive for complement (4+).
Cold Agglutinin Disease 15% of AIHAs Usually presents in 7 th decade of life, F>M 90% of cases - Ig. M antibodies react with RBC antigens at temperatures below core body temperature Ig. M can span the distance between RBCs, thus producing in vitro agglutination
Diagnosis Signs/symptoms of hemolysis DAT: +C 3 d, - Ig. G (classically) Both C 3 d and Ig. G in ~20% Titer and thermal activity >512 is clinically significant, but hemolysis can occur in lower titers
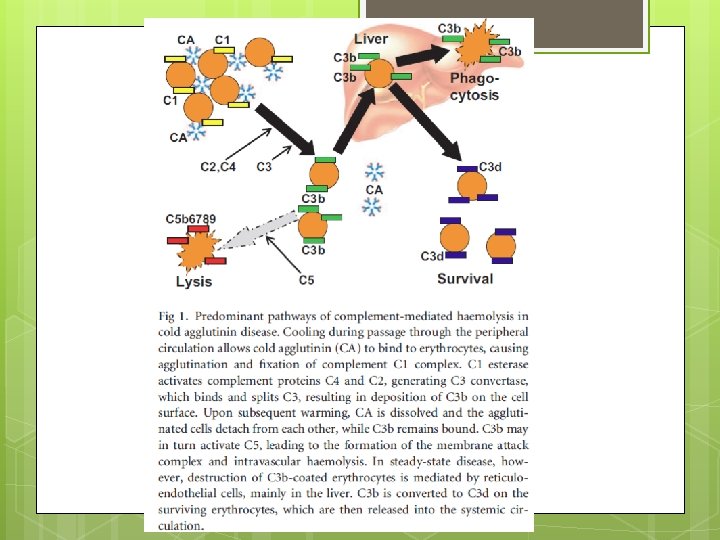
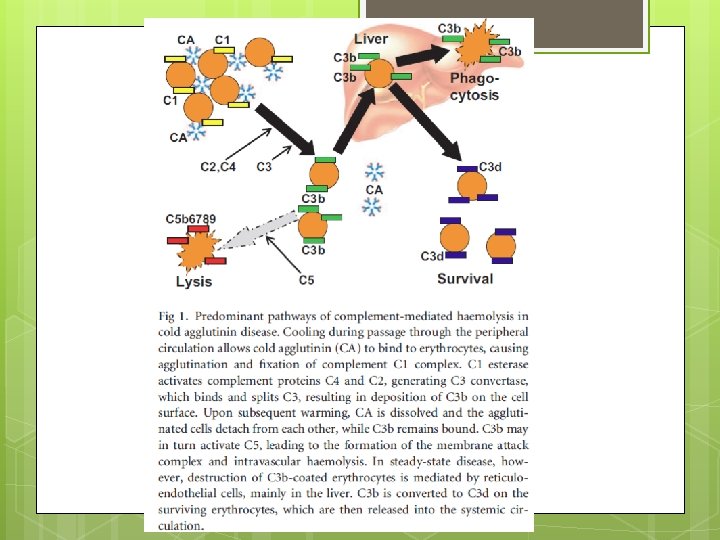
CAD, hemolysis Once Ig. M binds to RBC, complement activation occurs C 3 b binds to cell surface in periphery RBC travels to body core Ig. M dissociates Can lead to extravascular or intravascular hemolysis Can be polyclonal or monoclonal Polyclonal – postinfectious (Mycoplasma, EBV, legionella) Monoclonal – underlying lymphoproliferative d/o (clonal light chain predominance in 90%, trisomies 3, 12 and t(8: 22); )
Monoclonal Those that bind to the I/i antigens have heavy chains encoded by V 4. 34 gene segment 10% of all mature B cells use this gene segment why normal subjects can have lowtiters
Treatment Supportive Corticosteroids, analogs Rituximab Plasmapheresis cytotoxic agents, purine
References Swiecicki PL, Hegerova LT, and Gertz MA. Cold Agglutinin Disease. BLOOD, 15 AUGUST 2013 x VOLUME 122, NUMBER 7 Gertz MA. Cold Hemolytic Syndrome. Hematology 2006