Coagulation Factor Deficiencies hemophilia A factor VIII Hemophilia






- Slides: 15

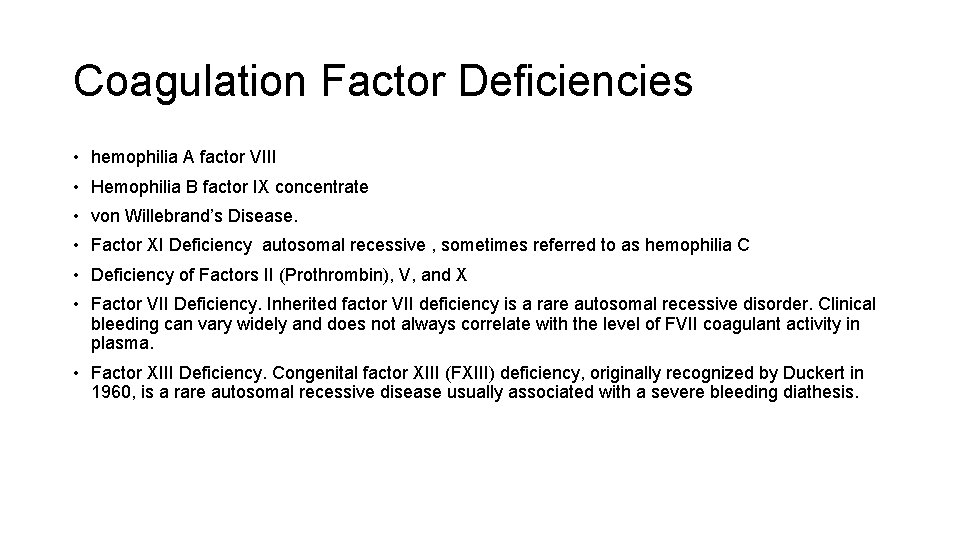
Coagulation Factor Deficiencies • hemophilia A factor VIII • Hemophilia B factor IX concentrate • von Willebrand’s Disease. • Factor XI Deficiency autosomal recessive , sometimes referred to as hemophilia C • Deficiency of Factors II (Prothrombin), V, and X • Factor VII Deficiency. Inherited factor VII deficiency is a rare autosomal recessive disorder. Clinical bleeding can vary widely and does not always correlate with the level of FVII coagulant activity in plasma. • Factor XIII Deficiency. Congenital factor XIII (FXIII) deficiency, originally recognized by Duckert in 1960, is a rare autosomal recessive disease usually associated with a severe bleeding diathesis.
Platelet Functional Defects
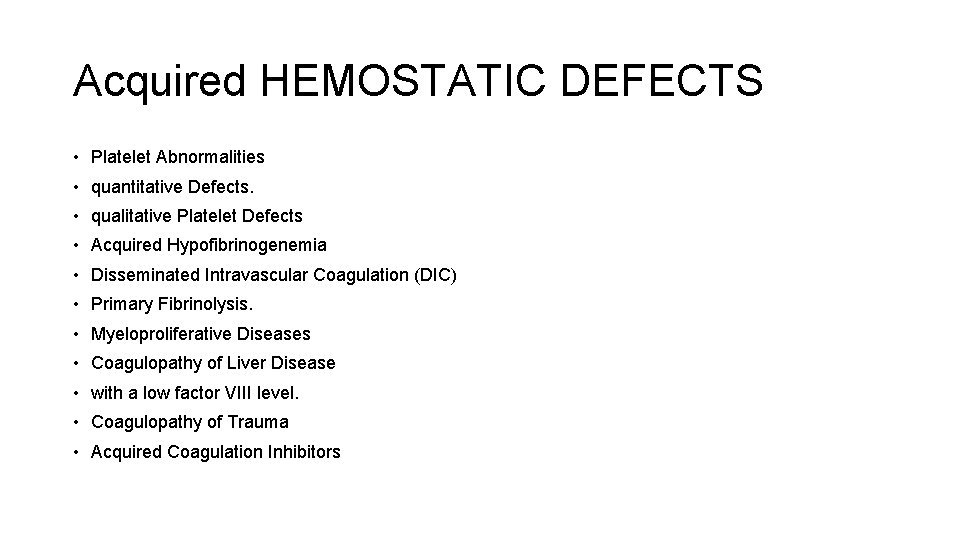
Acquired HEMOSTATIC DEFECTS • Platelet Abnormalities • quantitative Defects. • qualitative Platelet Defects • Acquired Hypofibrinogenemia • Disseminated Intravascular Coagulation (DIC) • Primary Fibrinolysis. • Myeloproliferative Diseases • Coagulopathy of Liver Disease • with a low factor VIII level. • Coagulopathy of Trauma • Acquired Coagulation Inhibitors

Transfusion Replacement Therapy
Typing and Cross-Matching • The use of autologous transfusion is growing. Up to 5 units can be collected for subsequent use during elective procedures. Patients can donate and store their own blood if their hemoglobin concentration exceeds 11 g/d. L or if the hematocrit is greater than 34%. The first procurement is performed 40 days before the planned operation, and the last one is performed 3 days before the operation. Donations can be scheduled at intervals of 3 to 4 days. Recombinant human erythropoietin (r. Hu. EPO) accelerates generation of red blood cells and allows for more frequent harvesting of blood.

• Banked Whole Blood. Once the gold standard, whole blood is rarely available in Western countries. With sequential changes in storage solutions, the shelf life of red blood cells is now 42 days. Recent evidence has demonstrated that the age of red cells may play a significant role in the inflammatory response and incidence of multiple organ failure. 54 The changes in the red blood cells that occur during storage include reduction of intracellular ADP and 2, 3 -diphosphoglycerate (2, 3 DPG), which alters the oxygen dissociation curve of hemoglobin, resulting in a decrease in oxygen transport. Stored RBCs progressively becomes acidodic with elevated levels of lactate, potassium, and ammonia.
• Red Blood Cells and Frozen Red Blood Cells. Red blood cells are the product of choice for most clinical situations requiring resuscitation. Concentrated suspensions of red blood cells can be prepared by removing most of the supernatant plasma after centrifugation. The preparation reduces but does not eliminate reactions caused by plasma components. Frozen red blood cells are not currently available for use in emergencies, as the thawing and preparation time is measured in hours. They are used for patients who are known to have been previously sensitized. The red blood cell viability is improved, and the ATP and 2, 3 -DPG concentrations are maintained
• Leukocyte-Reduced and Leukocyte-Reduced/Washed Red Blood Cells. These products are prepared by filtration that removes about 99. 9% of the white blood cells and most of the platelets (leukocyte-reduced red blood cells) and, if necessary, by additional saline washing (leukocytereduced/washed red blood cells). Leukocyte reduction prevents almost all febrile, nonhemolytic transfusion reactions (fever and/or rigors), alloimmunization to HLA class I antigens, and platelet transfusion refractoriness and cytomegalovirus transmission. In most Western nations, it is the standard red blood cell transfusion product. Supporters of universal leukocyte reduction argue that allogenic transfusion of white cells predisposes to postoperative bacterial infection and multiorgan failure. Reviews of randomized trials and meta-analyses have not provided convincing evidence either way, 55, 56 although a large Canadian retrospective study suggests a decrease in mortality and infections

• Platelet Concentrates. The indications for platelet transfusion include thrombocytopenia caused by massive blood loss and replacement with platelet-poor products, thrombocytopenia caused by inadequate production, and qualitative platelet disorders. The shelf life of platelets is 120 hours from time of donation. One unit of platelet concentrate has a volume of approximately 50 m. L. Platelet preparations are capable of transmitting infectious diseases and can account for allergic reactions similar to those caused by red blood cell transfusion. A therapeutic level of platelets is in the range of 50, 000 to 100, 000/μL but is very dependent on the clinical situation. Recent evidence suggests that earlier use of platelets may improve outcomes in bleeding patients
• TFresh Frozen Plasma. Fresh frozen plasma (FFP) prepared from freshly donated blood is the usual source of the vitamin K-dependent factors and is the only source of factor V. FFP carries similar infectious risks as other component therapies. Use of plasma as a primary resuscitation modality in patients who are rapidly bleeding has received attention over the last few years, and ongoing studies are under way to evaluate this concept. FFP can be thawed and stored for up to 5 days, greatly increasing its immediate availability. In an effort to increase the shelf life and avoid the need for refrigeration, lyophilized plasma is being tested. Preliminary animal studies suggest that it preserves the beneficial effects of FFP.
Indications for Replacement of Blood and Its Elements
Improvement in Oxygen-Carrying Capacity.

Treatment of Anemia: Transfusion Triggers • unresolved issue related to transfusion triggers is the safety of maintaining a hemoglobin of 7 g/d. L in a patient with ischemic heart disease. Data on this subject are mixed, and many studies have significant design flaws, including their retrospective nature. However, the majority of the published data favors a restrictive transfusion trigger for patients with non-ST elevation acute coronary syndrome, with many reporting worse outcomes in those patients receiving transfusions.

Volume Replacement • The most common indication for blood transfusion in surgical patients is the replenishment of the blood volume; however, a deficit is difficult to evaluate. Measurements of hemoglobin or hematocrit levels are frequently used to assess blood loss. These measurements can be occasionally misleading in the face of acute loss. Both the amount and the rate of bleeding are factors in the development of signs and symptoms of blood loss. • • Loss of blood in the operating room can be roughly evaluated by estimating the amount of blood in the wound and on the drapes, weighing the sponges, and quantifying blood suctioned from the operative field. In patients with normal preoperative values, blood loss up to 20% of total blood volume can be replaced with crystalloid or colloid solutions. Blood loss above this value may require the addition of a balanced resuscitation including red blood cells, FFP, and platelet
 Pampered style of life
Pampered style of life Unity of personality adler
Unity of personality adler Slide method of clotting time principle
Slide method of clotting time principle Antifibrinolytic drugs
Antifibrinolytic drugs Ecchumosis
Ecchumosis Dicoumoral
Dicoumoral Coagulation profile test
Coagulation profile test Coagulation pathway made easy
Coagulation pathway made easy Coagulation disorders
Coagulation disorders Coagulation factors list
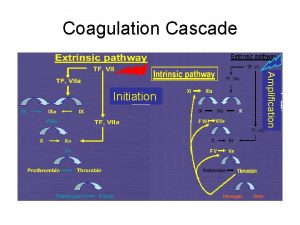
Coagulation factors list Blood clotting mechanism
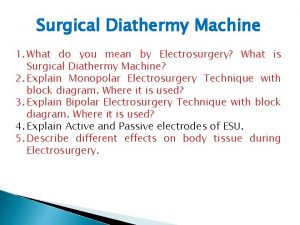
Blood clotting mechanism Diathermy machine used in surgery
Diathermy machine used in surgery Plasma and serum
Plasma and serum Coagulation profile test
Coagulation profile test Denaturation simple definition
Denaturation simple definition Dextrinisation examples
Dextrinisation examples