CNS Pathology RT 91 Fall 2010 Final INFLAMMATORY




- Slides: 103
CNS Pathology RT 91 Fall 2010 Final
INFLAMMATORY DISEASE OF CNS
Meningitis Ø Inflammation fo the meningeal coverings of the brain and spinal cord Ø Can be caused by l l Bacteria, virus and other organisms via blood or lymph Trauma, pentrating wounds or adjacent structures infected Bacterial is most common (can cause hydrocephalus) Ø Three types pus forming bacteria: Ø l l l Ø Meningococci - infants Streptococci - children Pneumococci- adults Tubercle bacillus
Different Pathogens causing Meningitis Ø Fungi l l Ø Virus l Ø Chronic meningitis Often associated with AIDS and immunodepressant drug therapy Viral meningitis can be caused by mumps, poliovirus and herpes simplex Bacteria l l Most common Bacteria release toxins that destroy meningeal cells stimulating immune & inflammatory reactions
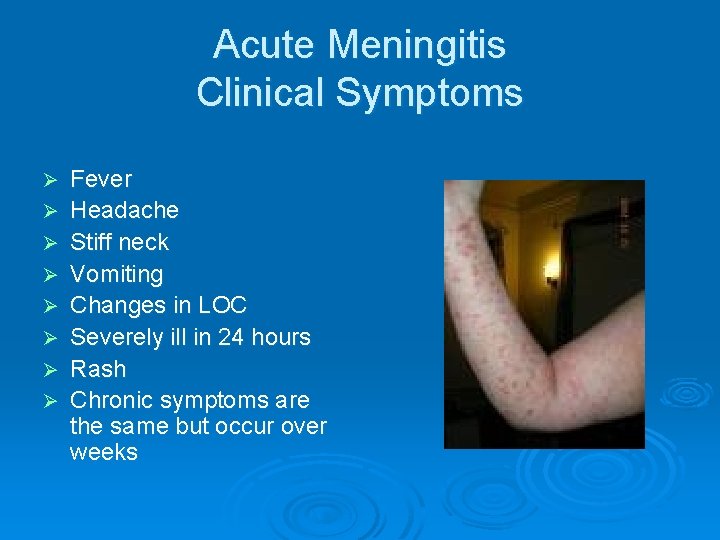
Acute Meningitis Clinical Symptoms Ø Ø Ø Ø Fever Headache Stiff neck Vomiting Changes in LOC Severely ill in 24 hours Rash Chronic symptoms are the same but occur over weeks
Diagnosis of Meningitis Ø Brain CT l Ø Spinal tap l Ø LP to remove CSF to send to lab Sometimes MRI is used l Ø Rule out contraindications to do a spinal tap Is most sensitive modality for demonstrating pia and arachnoid Treatment includes antibiotics and if secondary to encephalitis: antiviral drugs
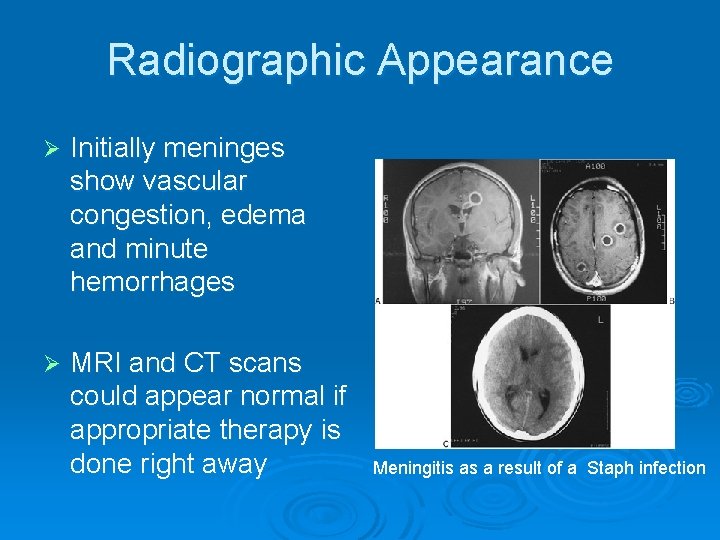
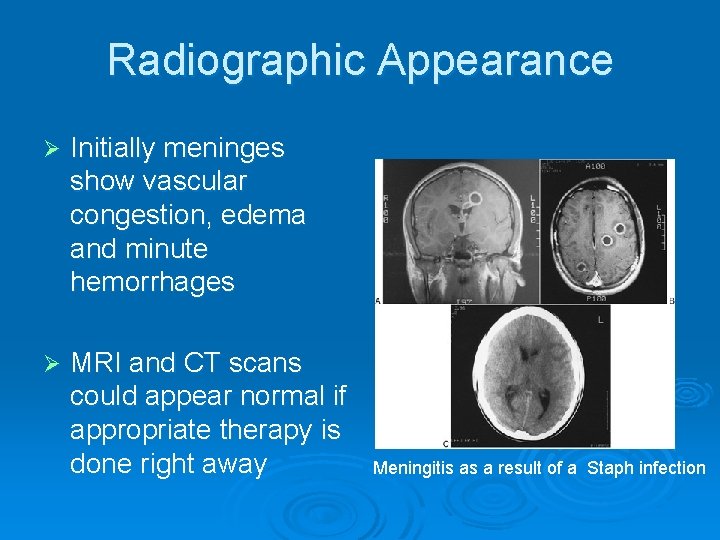
Radiographic Appearance Ø Initially meninges show vascular congestion, edema and minute hemorrhages Ø MRI and CT scans could appear normal if appropriate therapy is done right away Meningitis as a result of a Staph infection
Encephalitis Ø Infection of the brain tissue that is viral l l May occur subsequent to chickenpox, small pox, influenza and measles May be caused by mosquitoes and herpes Ø Survival rates depend of cause of the disease (can be fatal) l l 30% of cases in children When caused by herpes it is often fatal
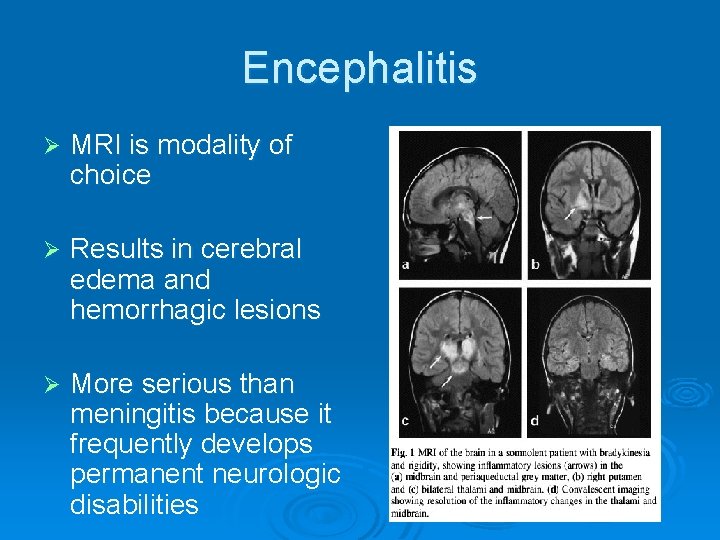
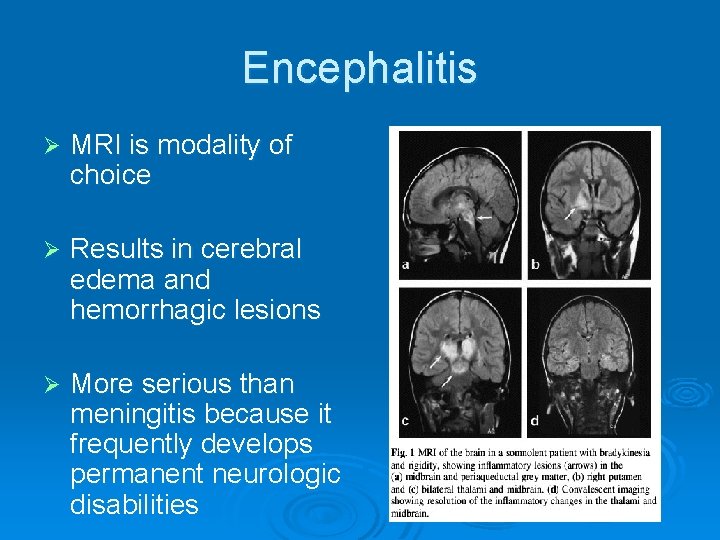
Encephalitis Ø MRI is modality of choice Ø Results in cerebral edema and hemorrhagic lesions Ø More serious than meningitis because it frequently develops permanent neurologic disabilities
Encephalitis: Symptoms and Treatment Ø Symptoms: l Headache l Malaise Ø Treatment: l l l Coma l Fever l Seizures Treated with antiviral medications Herpes induced is treated with Acyclovir • Interferes with DNA synthesis and inhibits viral replication
CONGENITAL DISEASES OF CNS
Spinal Bifida Ø Is a congenital disease Ø Bony neural arch that not completely closed Ø Most common in lumbar region l May or may not herniate through opening Ø Can range in risk from treatable to life threatening Ø Can be diagnosed in utero l l l With amniocentesis Ultrasound Elevated beta fetoprotein in mother’s blood
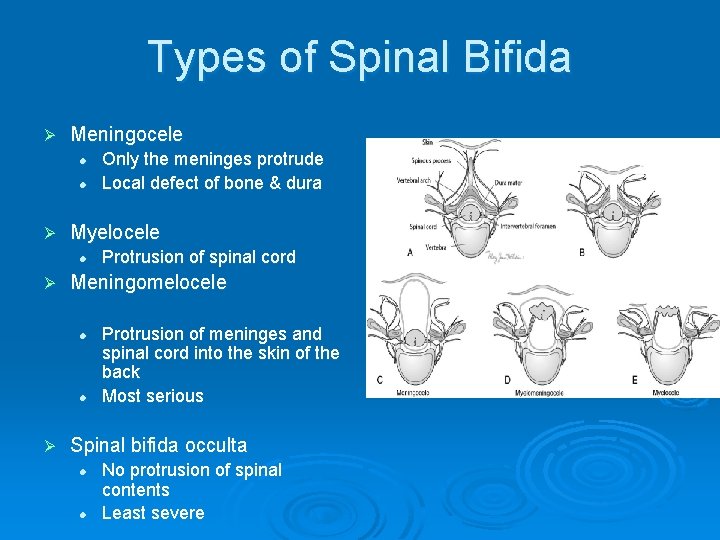
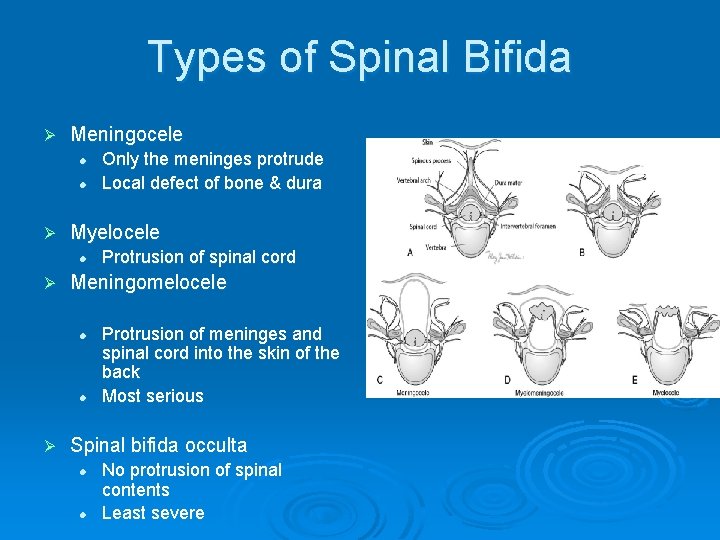
Types of Spinal Bifida Ø Meningocele l l Ø Myelocele l Ø Protrusion of spinal cord Meningomelocele l l Ø Only the meninges protrude Local defect of bone & dura Protrusion of meninges and spinal cord into the skin of the back Most serious Spinal bifida occulta l l No protrusion of spinal contents Least severe
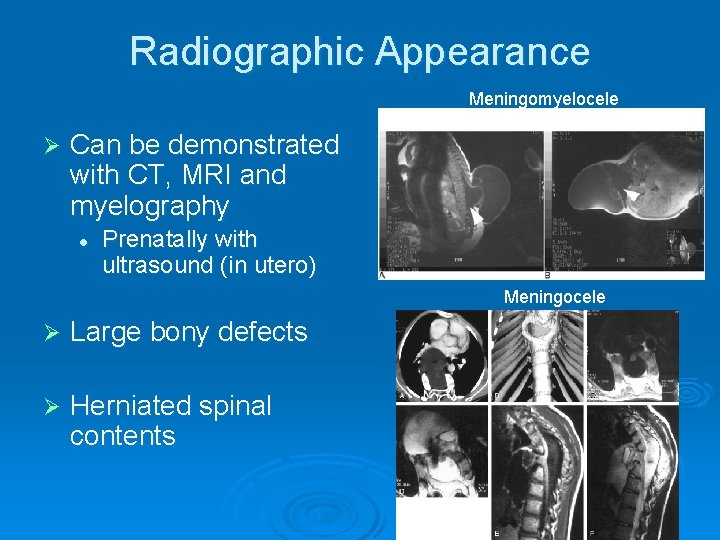
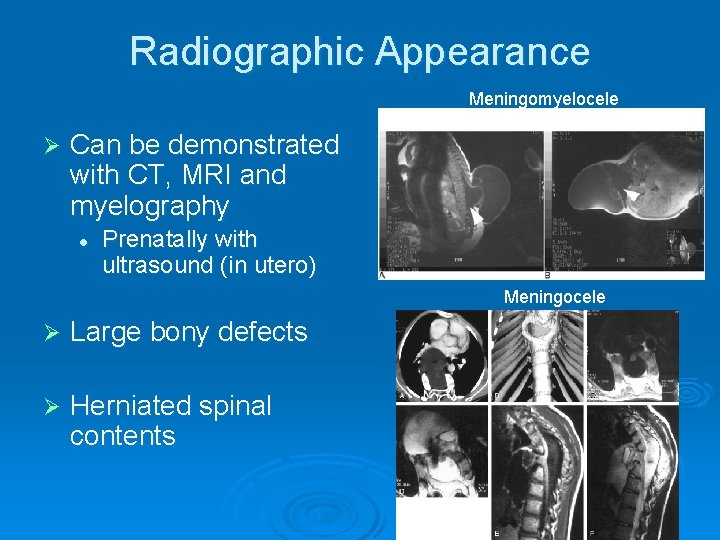
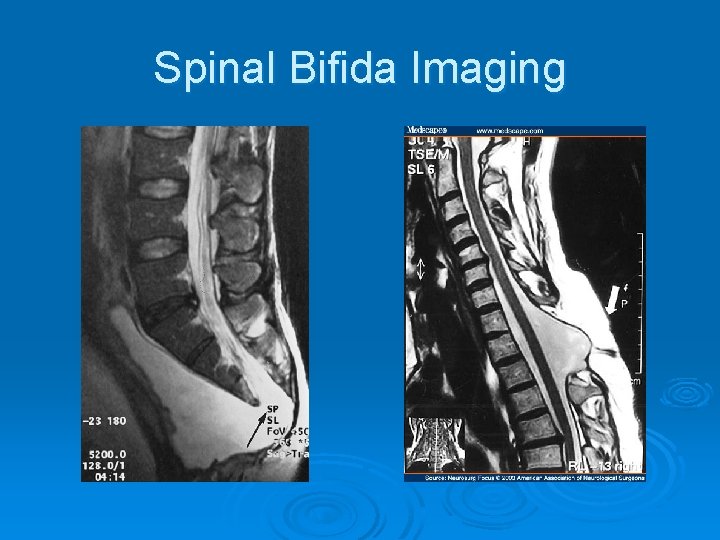
Radiographic Appearance Meningomyelocele Ø Can be demonstrated with CT, MRI and myelography l Prenatally with ultrasound (in utero) Meningocele Ø Large bony defects Ø Herniated spinal contents
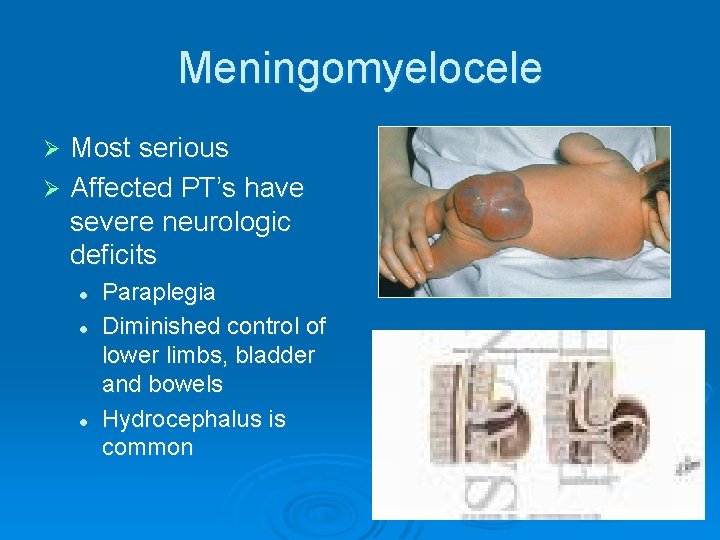
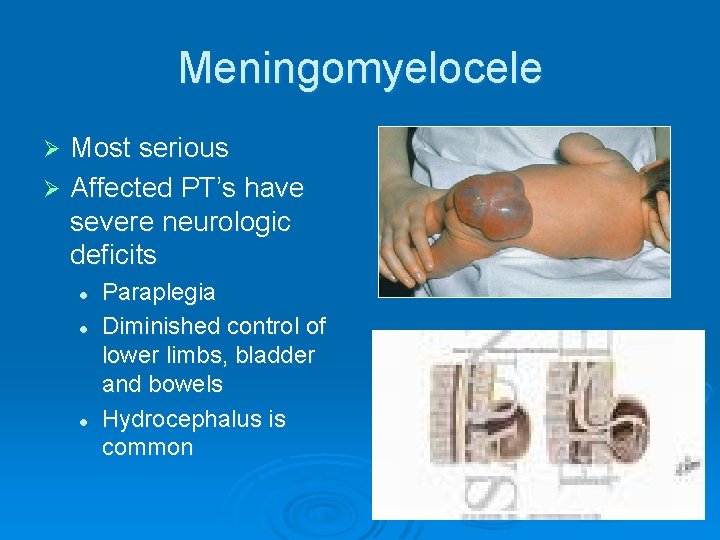
Meningomyelocele Most serious Ø Affected PT’s have severe neurologic deficits Ø l l l Paraplegia Diminished control of lower limbs, bladder and bowels Hydrocephalus is common
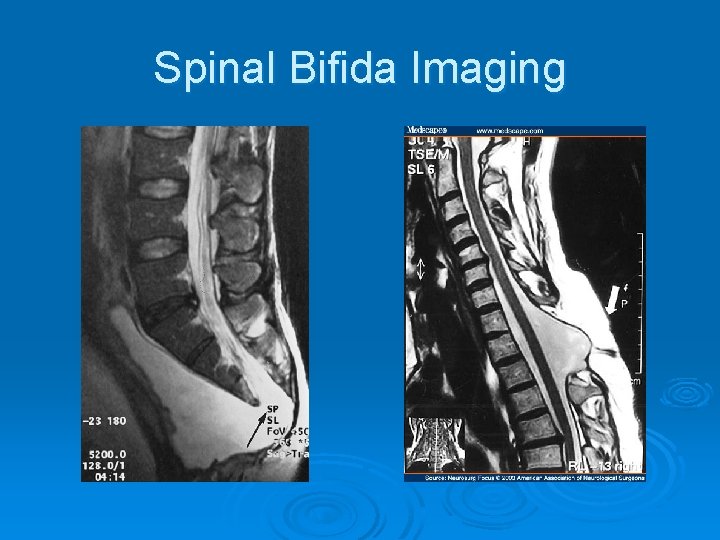
Spinal Bifida Imaging
Spinal Bifida Treatment Ø Can be surgically repaired l Ø Neurological damage is permanent still and cannot be reversed Most measures are supportive rather than corrective l l Physical therapy Physical supports Braces Splints
CRANIAL AND SPINAL FRACTURES
Cranial Fractures Ø Cerebral fractures usually occurs to fractures of the calvaria of the skull Ø 3 types of cranial fractures l Linear- straight and sharply defined • Is 80% of all cranial fractures l Depressed- curvilinear density l Basilar- Air fluid levels are indicative • Hard to diagnosis radiographically

Cranial Fractures Ø Location of FX is more important that the extent of the FX l l If FX crosses artery a bleed can occur causing a hematoma Fx that enters mastoid air cells or sinus can cause an infection that can result in • Meningitis • Encephalitis
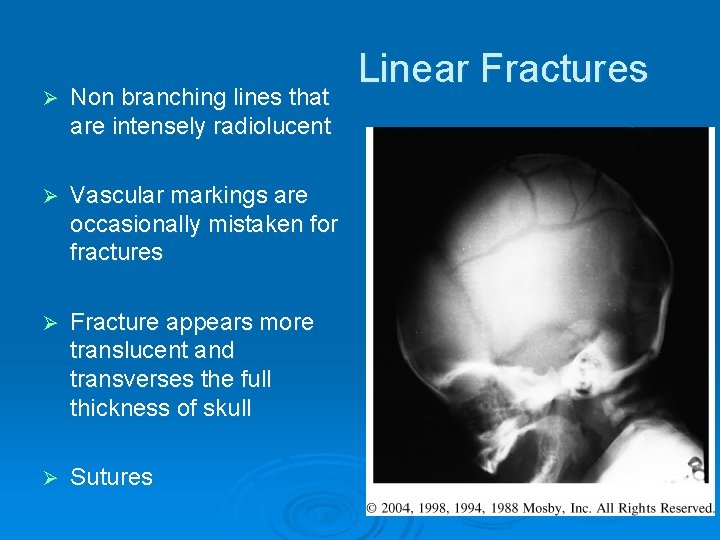
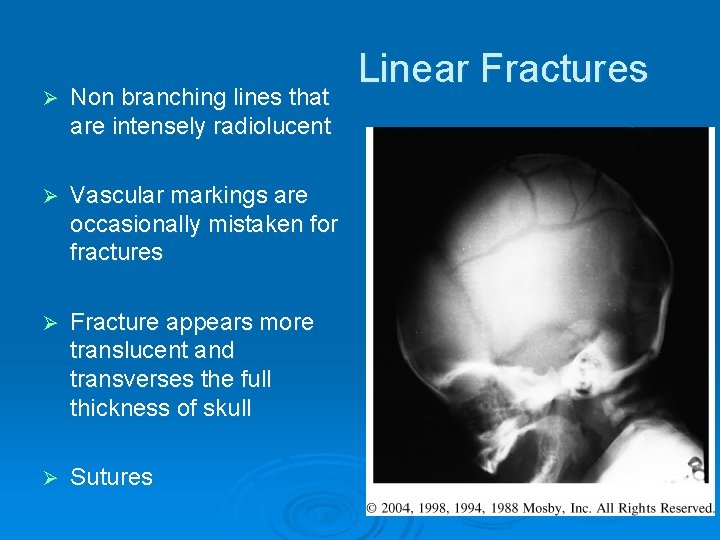
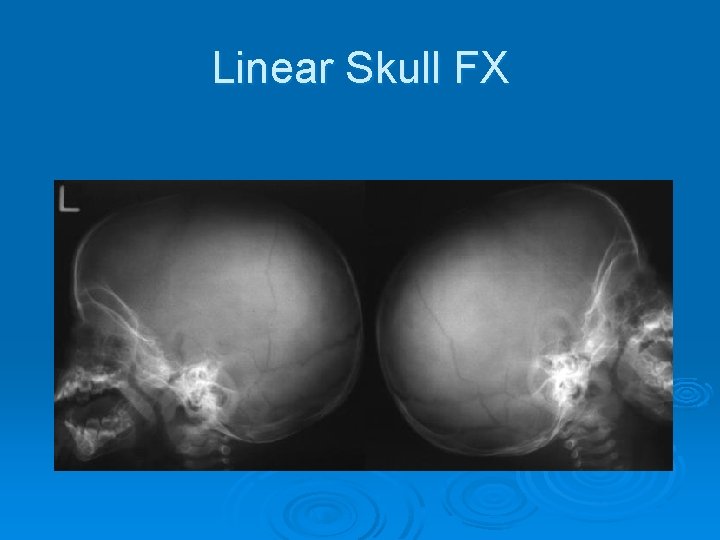
Ø Non branching lines that are intensely radiolucent Ø Vascular markings are occasionally mistaken for fractures Ø Fracture appears more translucent and transverses the full thickness of skull Ø Sutures Linear Fractures
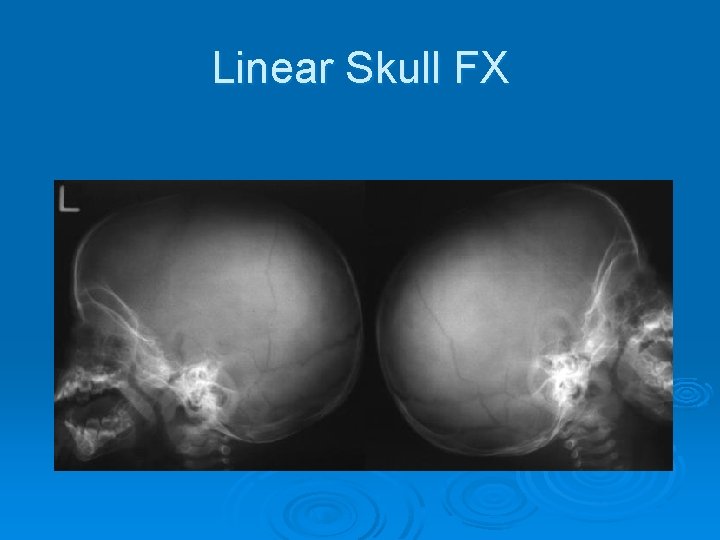
Linear Skull FX
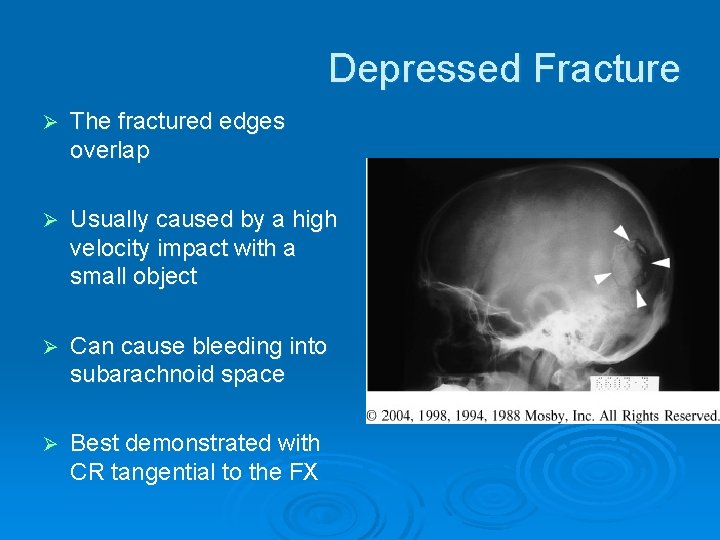
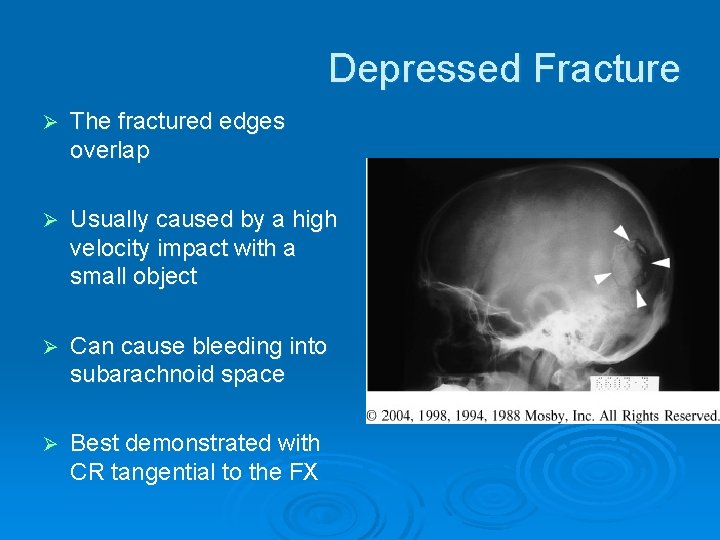
Depressed Fracture Ø The fractured edges overlap Ø Usually caused by a high velocity impact with a small object Ø Can cause bleeding into subarachnoid space Ø Best demonstrated with CR tangential to the FX
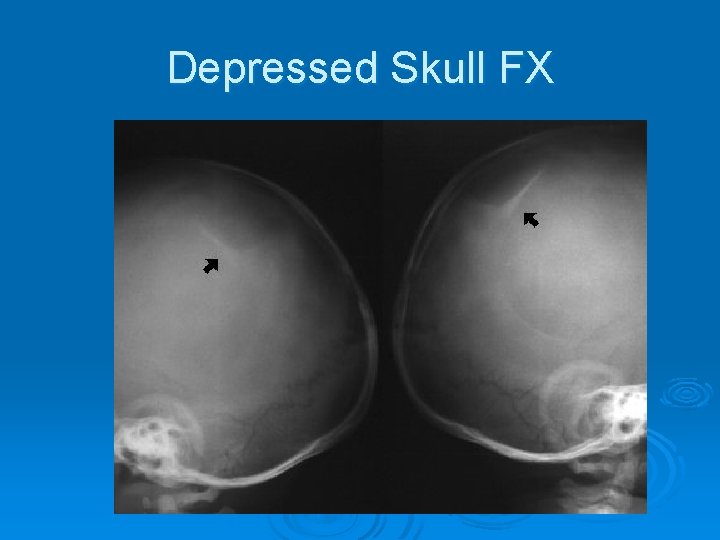
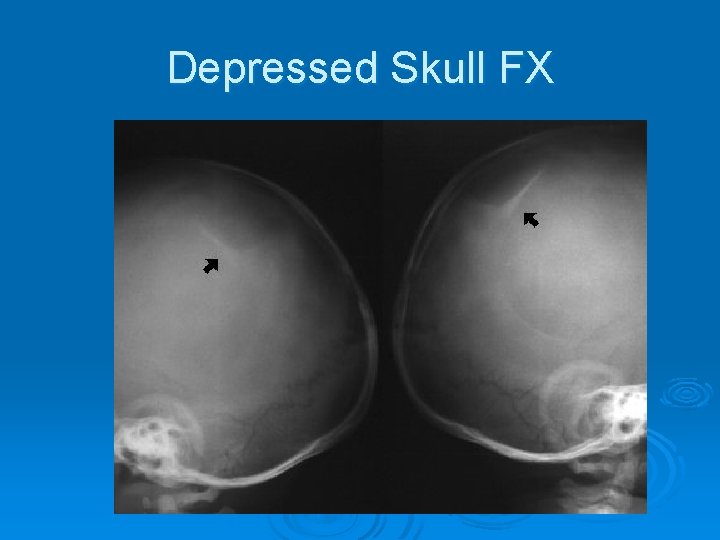
Depressed Skull FX
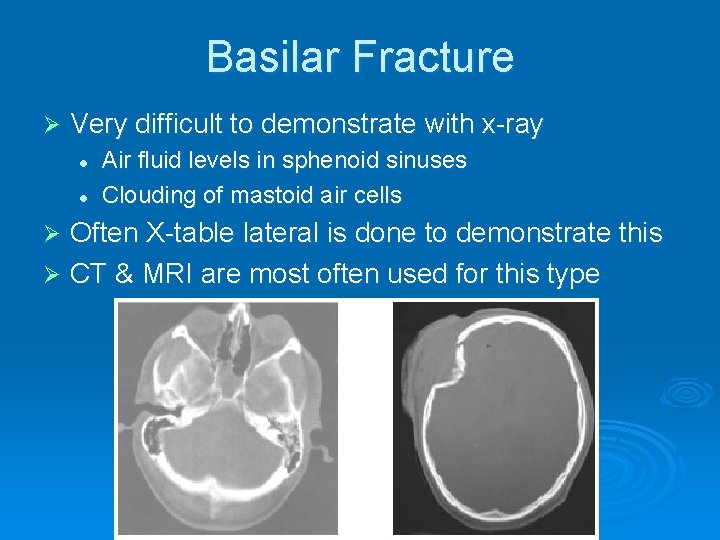
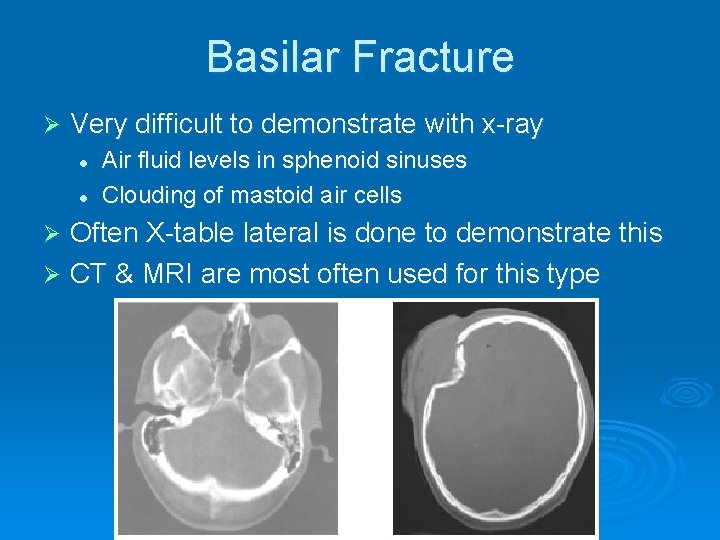
Basilar Fracture Ø Very difficult to demonstrate with x-ray l l Air fluid levels in sphenoid sinuses Clouding of mastoid air cells Often X-table lateral is done to demonstrate this Ø CT & MRI are most often used for this type Ø
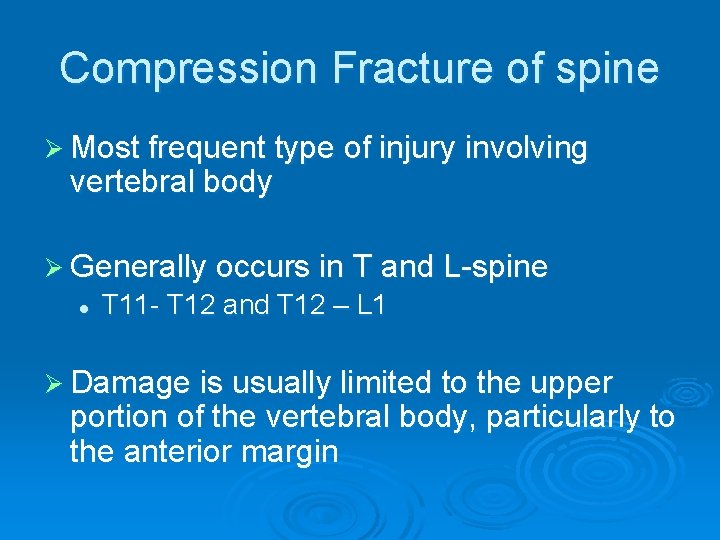
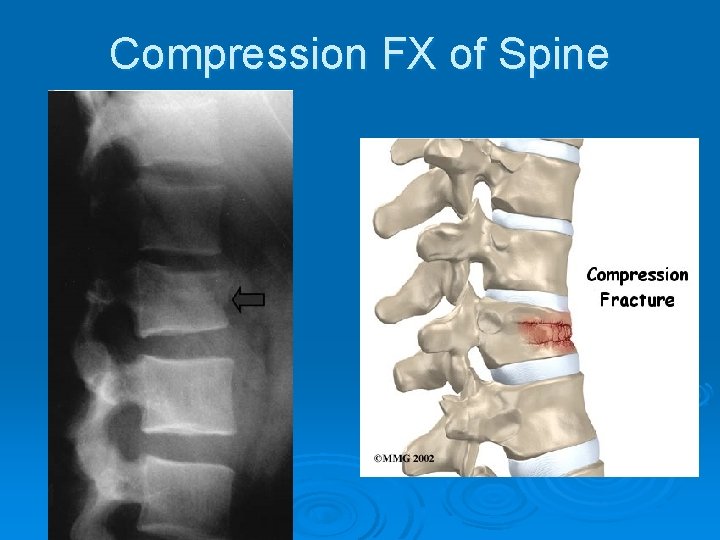
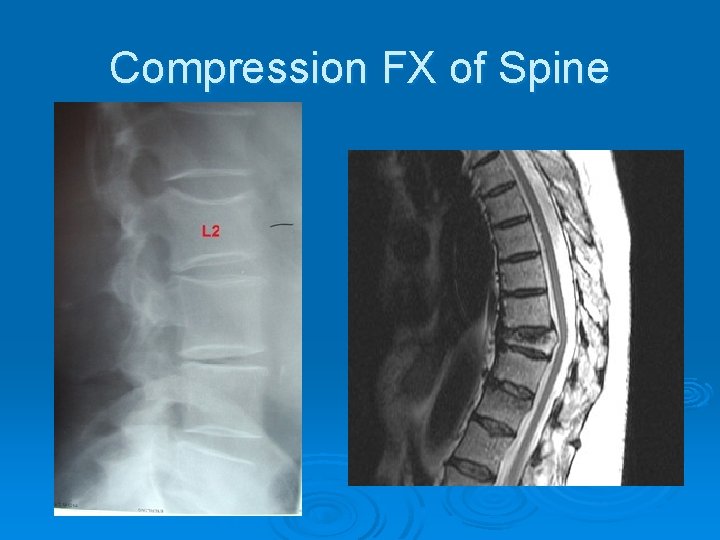
Compression Fracture of spine Ø Most frequent type of injury involving vertebral body Ø Generally occurs in T and L-spine l T 11 - T 12 and T 12 – L 1 Ø Damage is usually limited to the upper portion of the vertebral body, particularly to the anterior margin
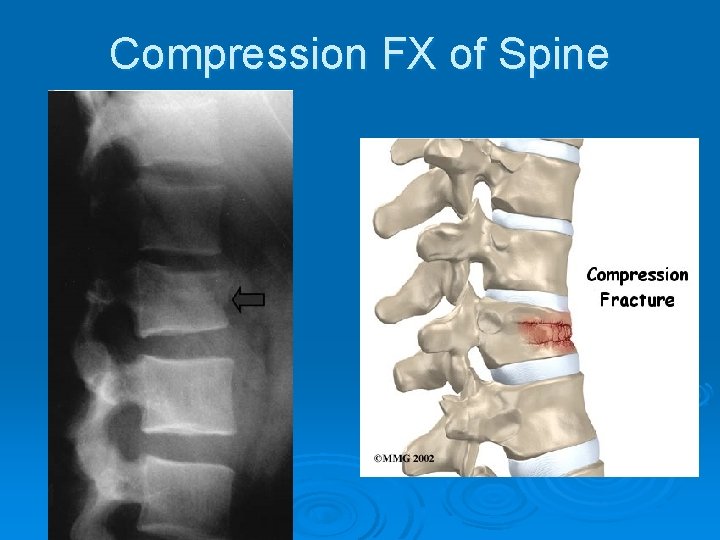
Compression FX of Spine
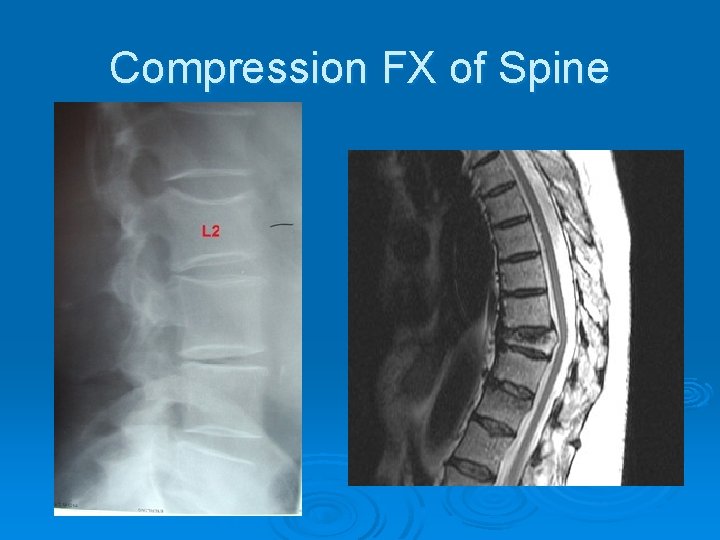
Compression FX of Spine
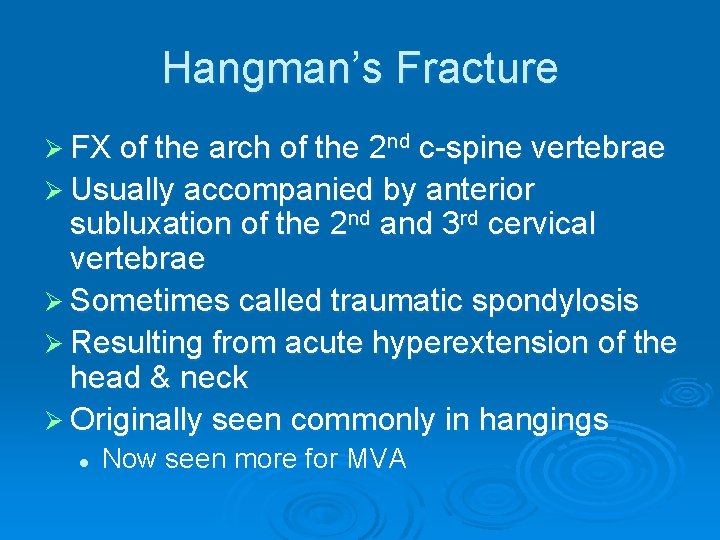
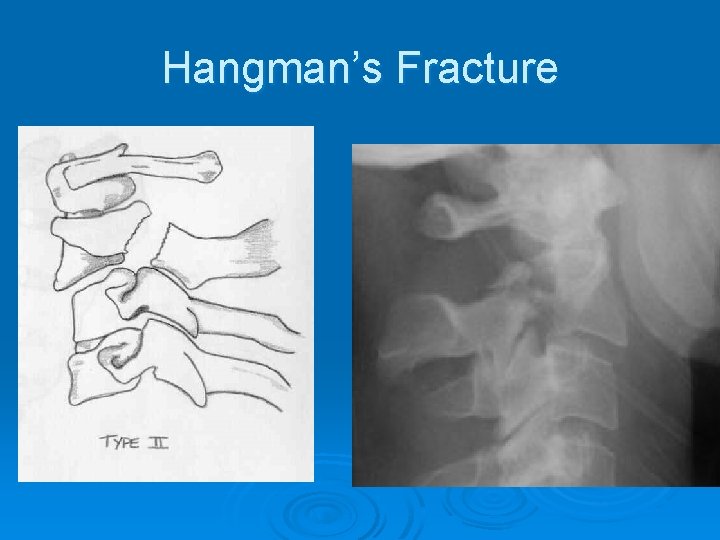
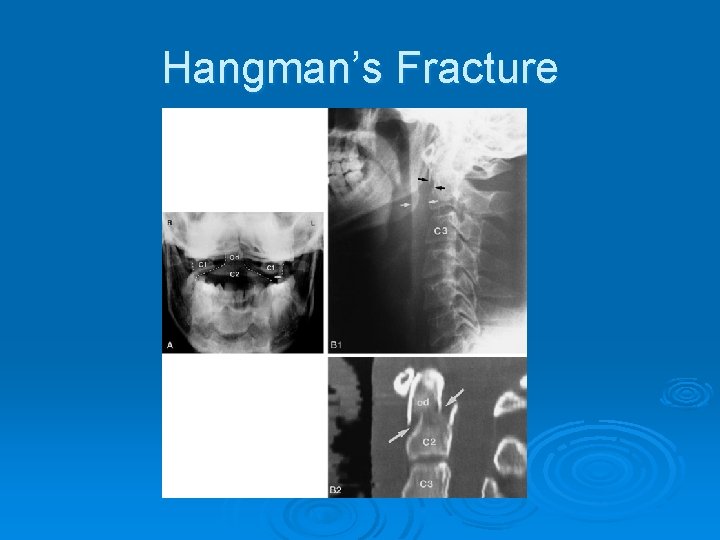
Hangman’s Fracture Ø FX of the arch of the 2 nd c-spine vertebrae Ø Usually accompanied by anterior subluxation of the 2 nd and 3 rd cervical vertebrae Ø Sometimes called traumatic spondylosis Ø Resulting from acute hyperextension of the head & neck Ø Originally seen commonly in hangings l Now seen more for MVA
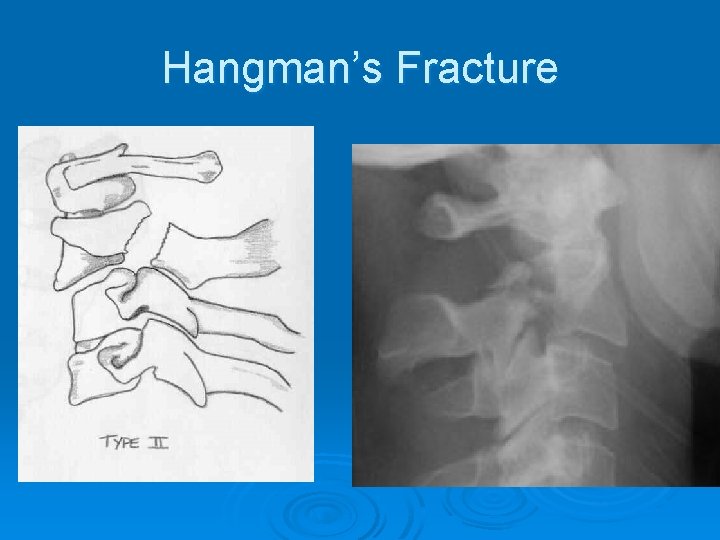
Hangman’s Fracture
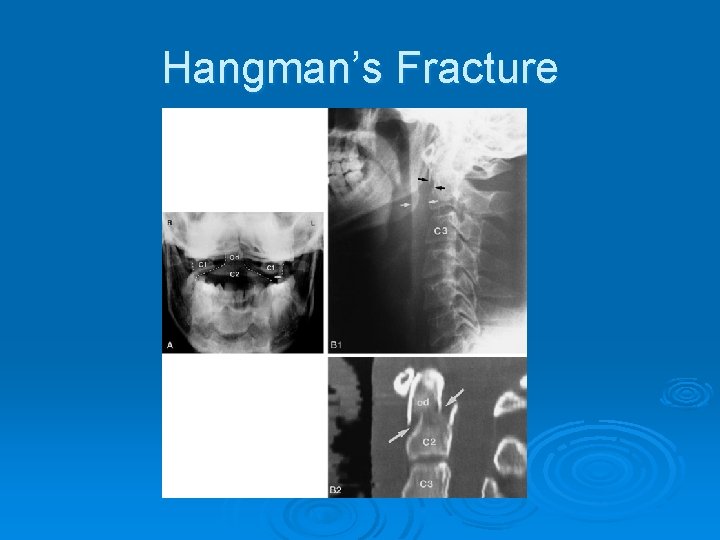
Hangman’s Fracture
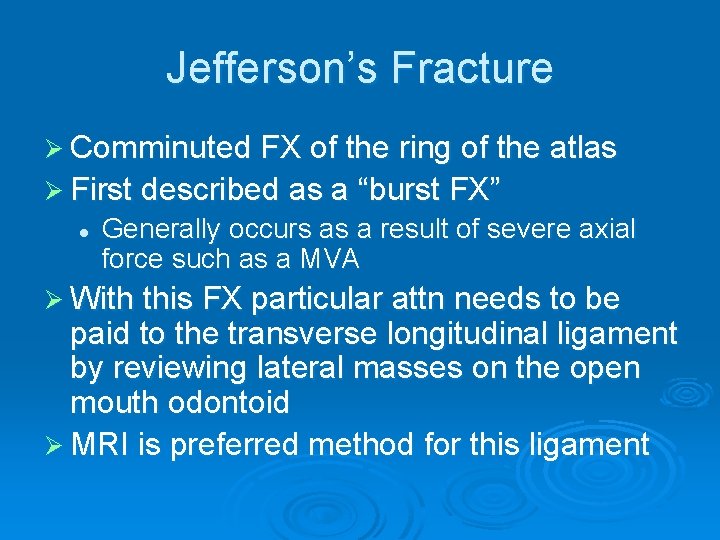
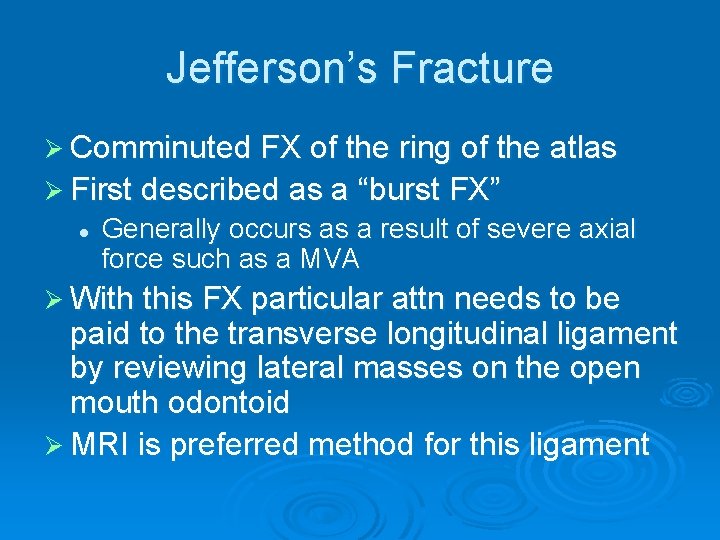
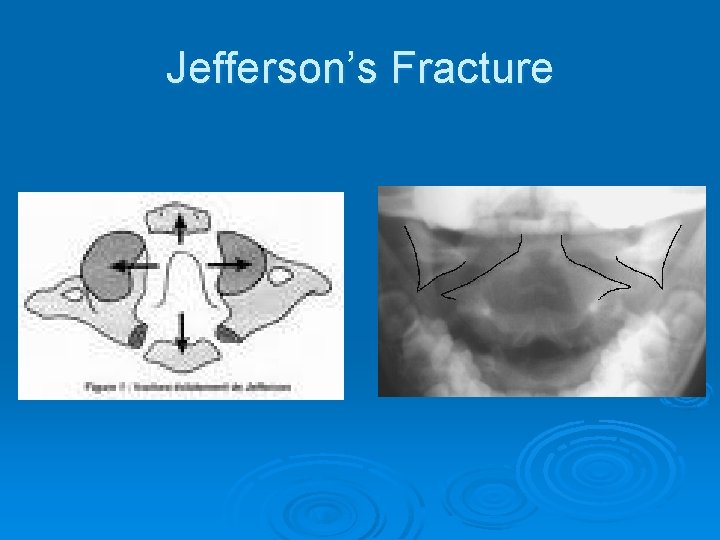
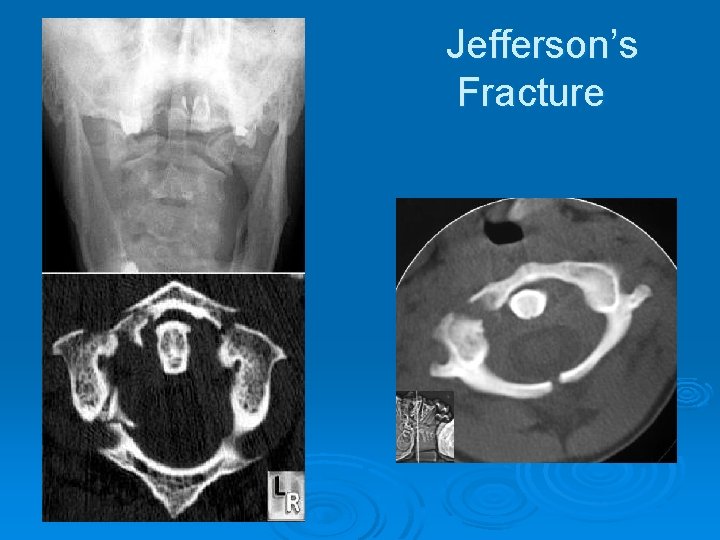
Jefferson’s Fracture Ø Comminuted FX of the ring of the atlas Ø First described as a “burst FX” l Generally occurs as a result of severe axial force such as a MVA Ø With this FX particular attn needs to be paid to the transverse longitudinal ligament by reviewing lateral masses on the open mouth odontoid Ø MRI is preferred method for this ligament
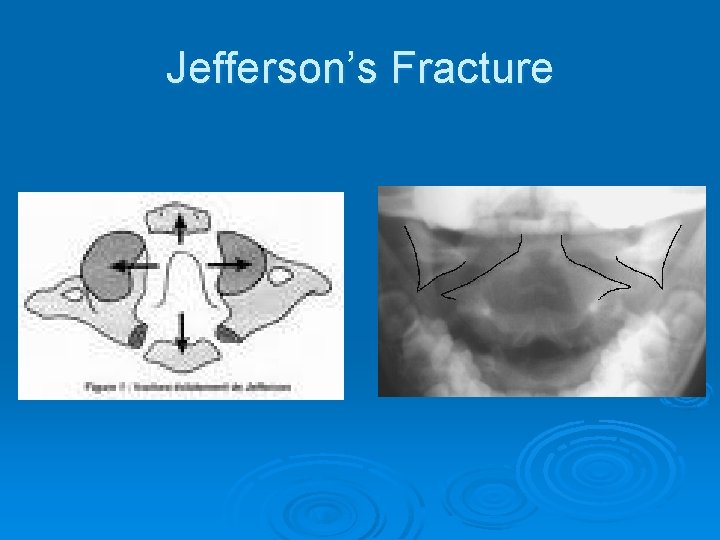
Jefferson’s Fracture
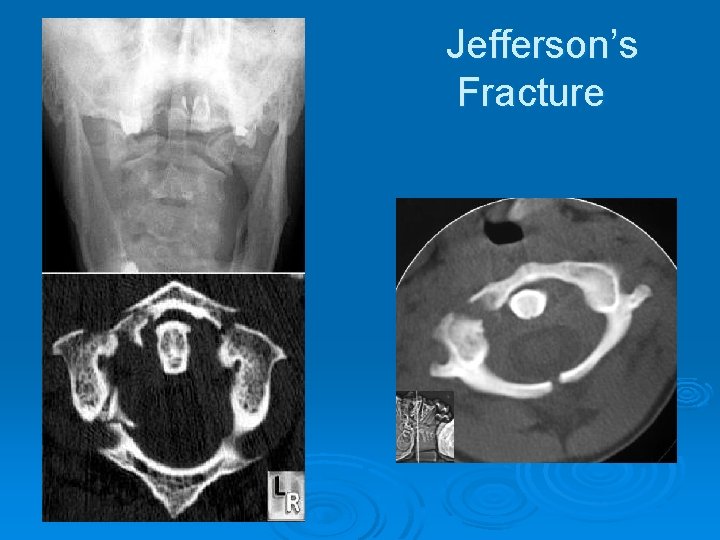
Jefferson’s Fracture

TRAUMATIC DISEASE
Cerebral Contusion Ø Is an injury to the brain tissue caused by a movement of the brain within the calvaria after blunt trauma Ø Occurs when brain contacts rough skull surfaces such as orbital floor and petrous ridges l l PT usually loses consciousness and cannot remember traumatic event Persitent LOC over 24 hrs is a coma and can be fatal
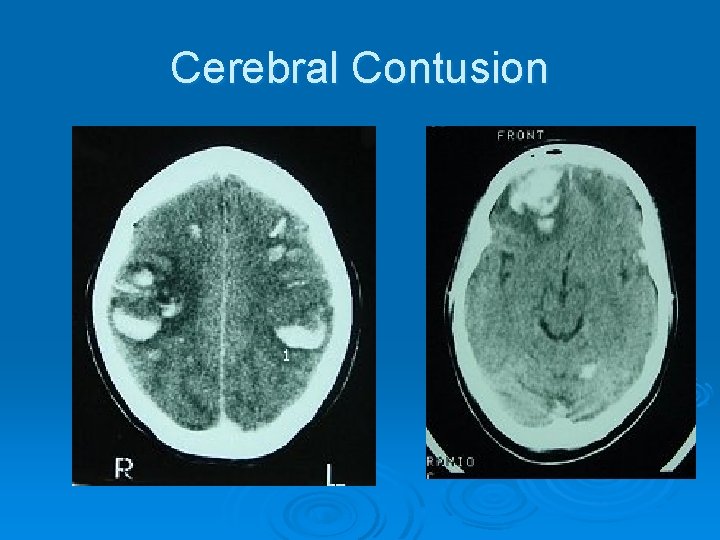
CT appearance of Cerebral Contusion Ø CT scans appear as low density areas of edema and tissue necrosis l l With or without homogenous density zones reflecting areas of hemorraghe Most common sites of injury are frontal and anterior temporal regions. When IV contrast is used it will enhance several weeks after injury Ø Plays an important role in diagnosis Ø
MR of Cerebral Contusion Ø Cerebral edema causes high signal intensity on T 2 scans Ø T 1 scans may produce high signal regions Ø Diagnosis can also include CT, MRI and PET
Cerebral Contusion Ø Treatment: l PT is hospitalized • Prevent shock l Ø Clinical symptoms: l l l Drowsiness Confusion Agitiation Hemiparesis Unequal pupil size If there is swelling meidcation is given to decrease cranial pressure • Control edema • Draniage of hematoma l Surgery is usually not necessary
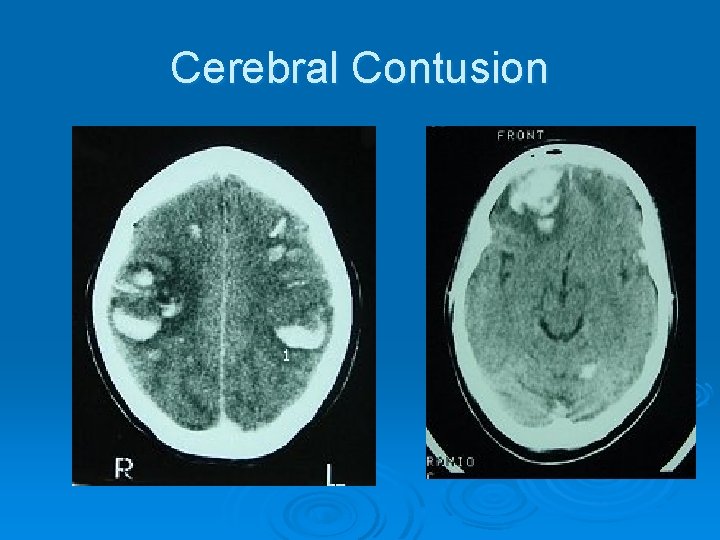
Cerebral Contusion
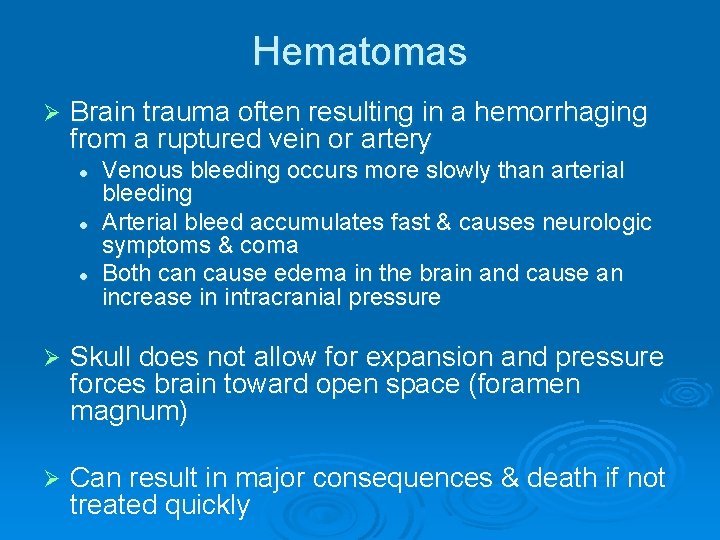
Hematomas Ø Brain trauma often resulting in a hemorrhaging from a ruptured vein or artery l l l Venous bleeding occurs more slowly than arterial bleeding Arterial bleed accumulates fast & causes neurologic symptoms & coma Both can cause edema in the brain and cause an increase in intracranial pressure Ø Skull does not allow for expansion and pressure forces brain toward open space (foramen magnum) Ø Can result in major consequences & death if not treated quickly
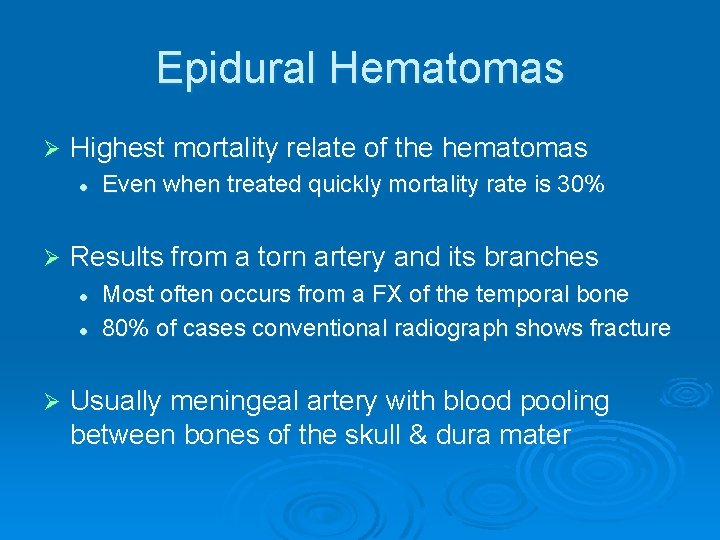
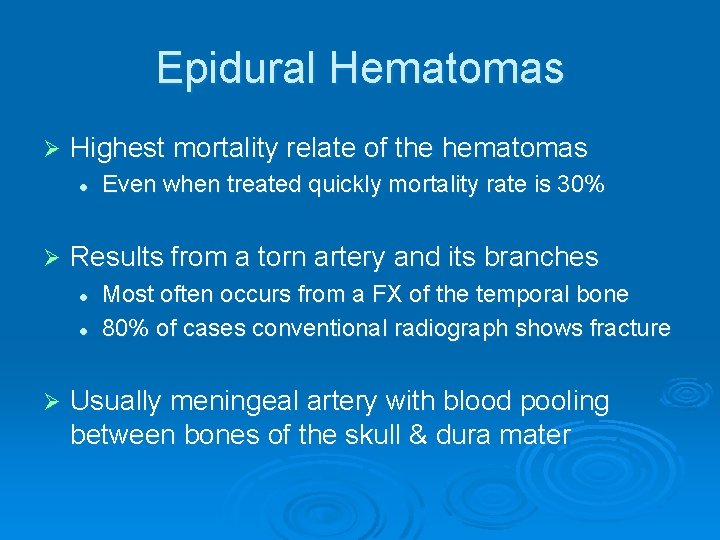
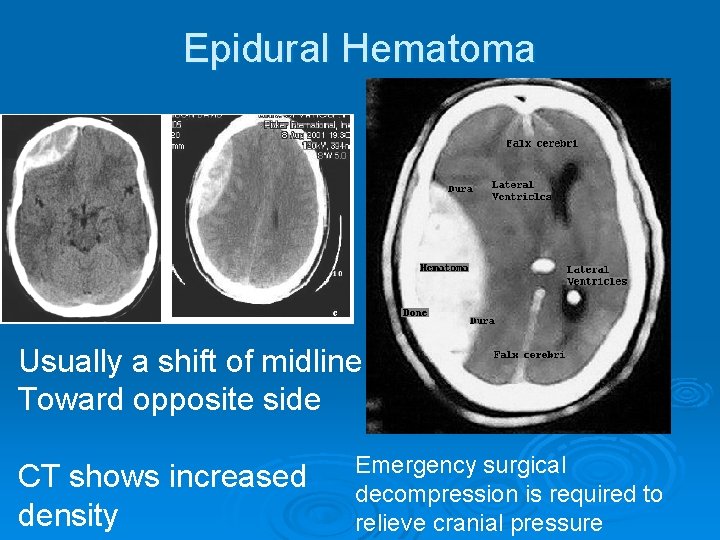
Epidural Hematomas Ø Highest mortality relate of the hematomas l Ø Results from a torn artery and its branches l l Ø Even when treated quickly mortality rate is 30% Most often occurs from a FX of the temporal bone 80% of cases conventional radiograph shows fracture Usually meningeal artery with blood pooling between bones of the skull & dura mater
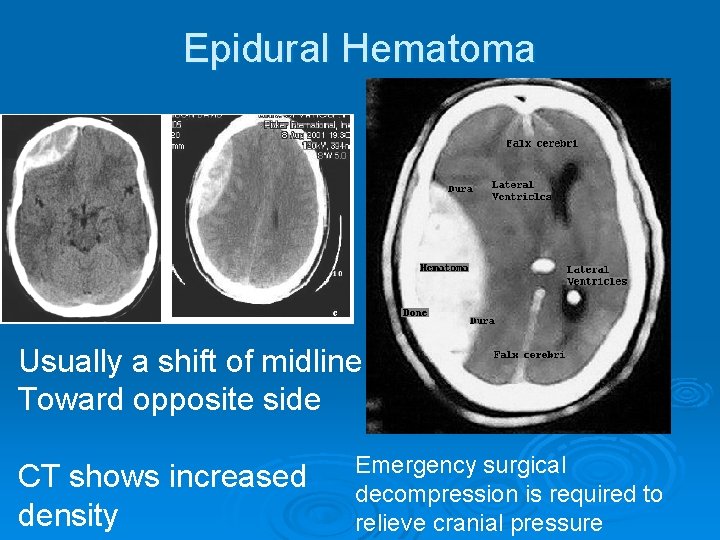
Epidural Hematoma Usually a shift of midline Toward opposite side CT shows increased density Emergency surgical decompression is required to relieve cranial pressure
Subdural Hematomas Ø Between the dura mater & arachnoid meningeal layers l Caused by blunt trauma to frontal or occipital lobes and can tear subdural veins Ø Pushes brain away from skull across midline (including ventricles)
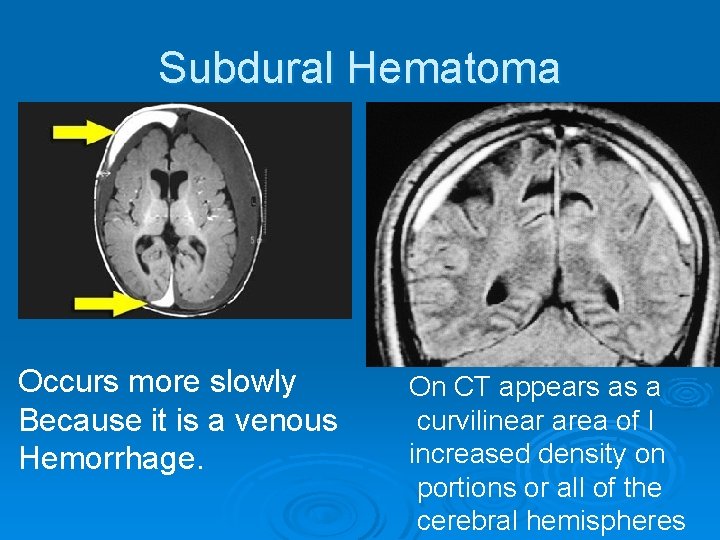
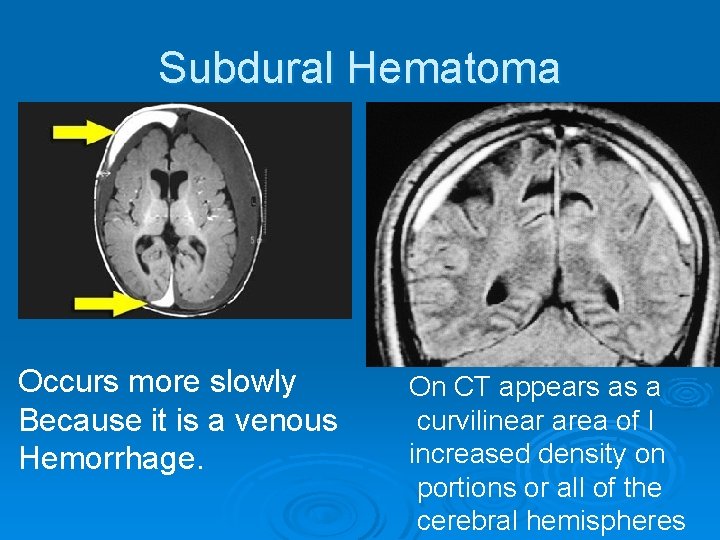
Subdural Hematoma Occurs more slowly Because it is a venous Hemorrhage. On CT appears as a curvilinear area of I increased density on portions or all of the cerebral hemispheres
Subdural Hematomas Ø Subacute stage (up to several days) l Appears on CT as a decreased density or isodense fluid collection Ø In chronic state (2 -3 weeks) l l The surface of the hematoma becomes concave Delayed coma con occur
Symptoms of Hematomas Ø Headaches Ø Agitation Ø Drowsiness Ø Gradual radiograph deficits
Treatment of Hematomas Ø In small hematomas without inclination to rebleed l l Ø Severe cases l l Ø the hemorrhage is reabsorbed naturally no treatment is necessary Require surgical ligation Evacuation of hematoma to prevent herniation Less invasive treatment may include l l Drug therapy Intraventricular catheter to remove CSF, which may cause herniation

Degenerative Diseases
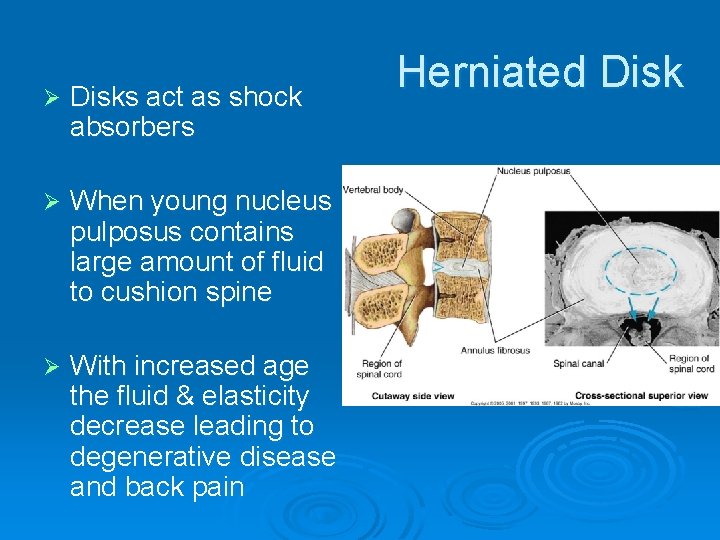
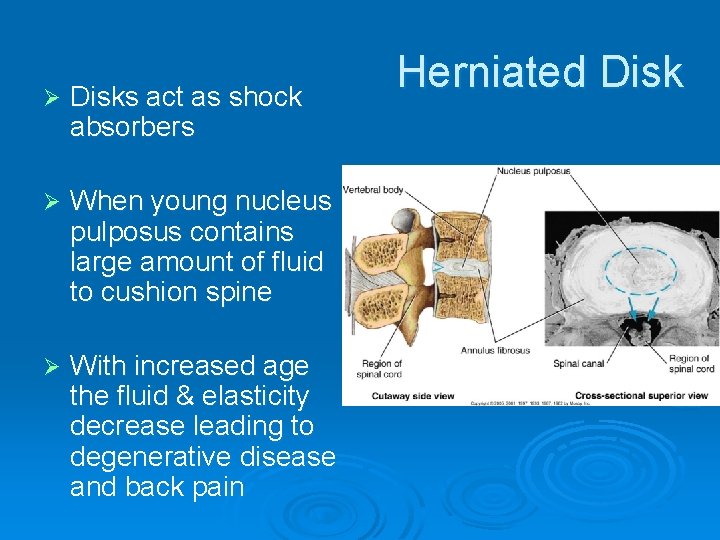
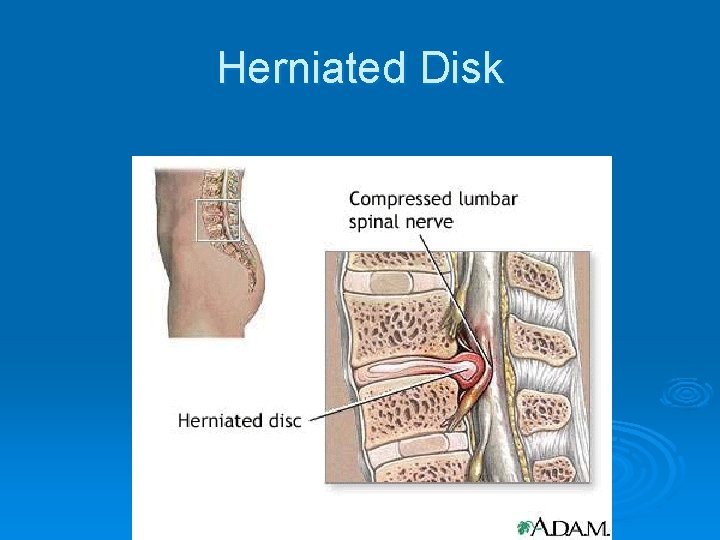
Ø Disks act as shock absorbers Ø When young nucleus pulposus contains large amount of fluid to cushion spine Ø With increased age the fluid & elasticity decrease leading to degenerative disease and back pain Herniated Disk
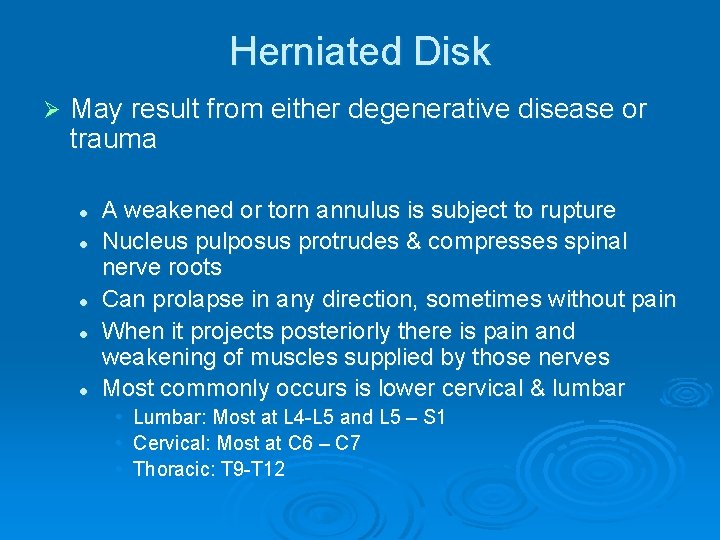
Herniated Disk Ø May result from either degenerative disease or trauma l l l A weakened or torn annulus is subject to rupture Nucleus pulposus protrudes & compresses spinal nerve roots Can prolapse in any direction, sometimes without pain When it projects posteriorly there is pain and weakening of muscles supplied by those nerves Most commonly occurs is lower cervical & lumbar • • • Lumbar: Most at L 4 -L 5 and L 5 – S 1 Cervical: Most at C 6 – C 7 Thoracic: T 9 -T 12
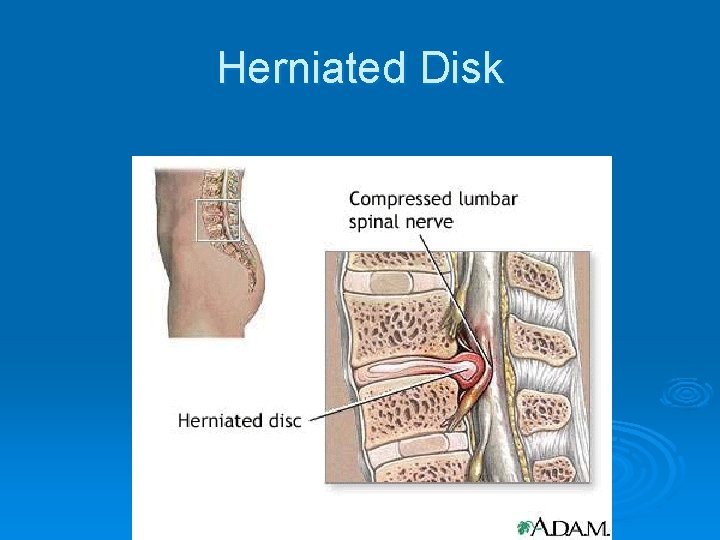
Herniated Disk
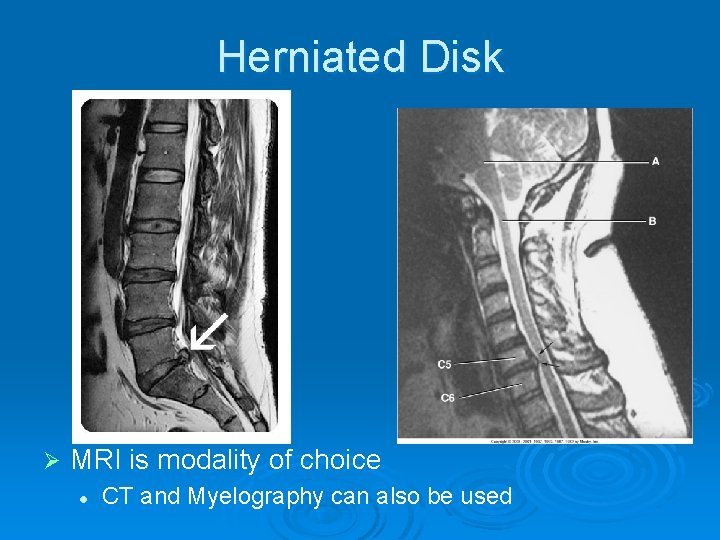
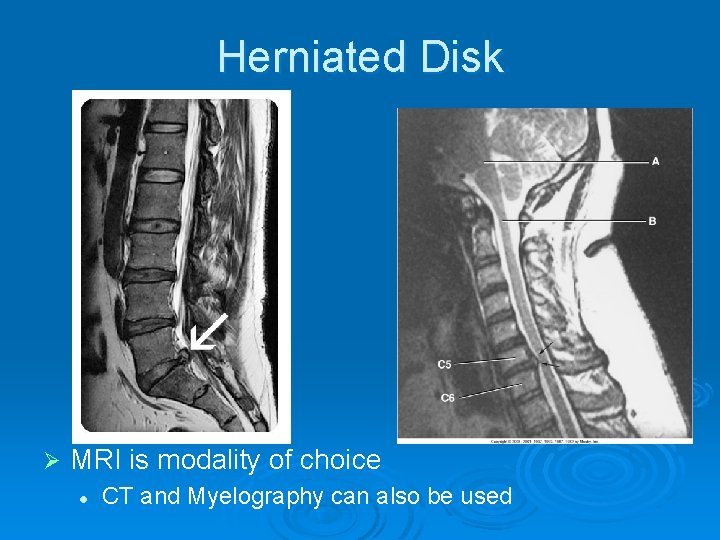
Herniated Disk Ø MRI is modality of choice l CT and Myelography can also be used
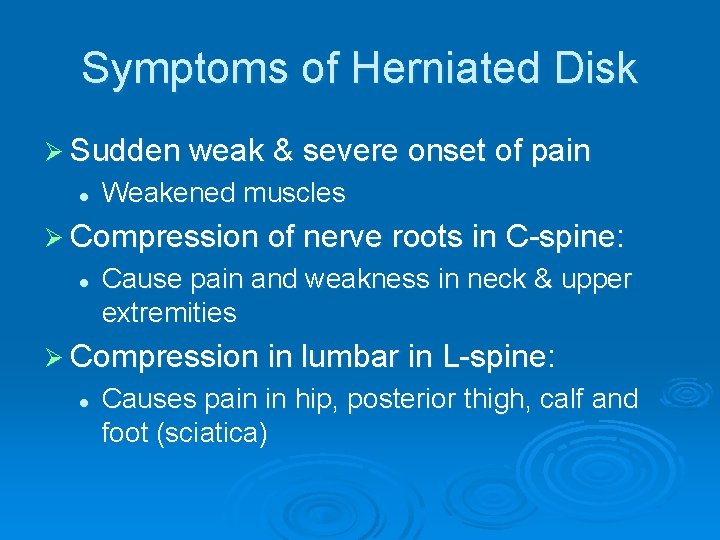
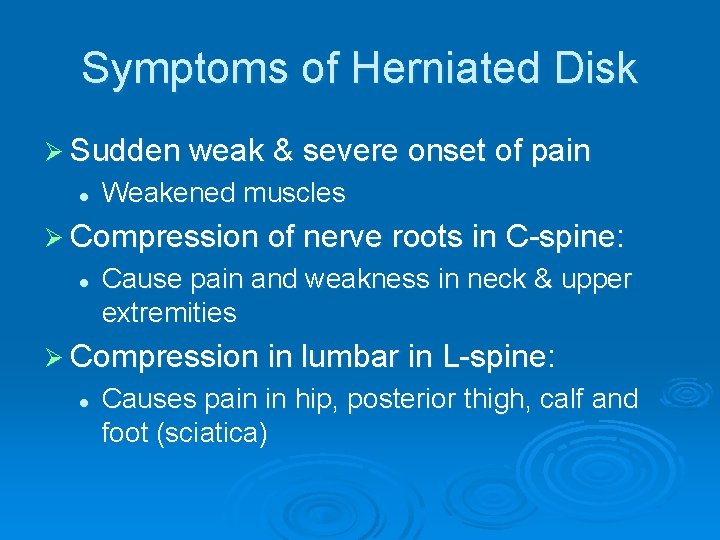
Symptoms of Herniated Disk Ø Sudden weak & severe onset of pain l Weakened muscles Ø Compression of nerve roots in C-spine: l Cause pain and weakness in neck & upper extremities Ø Compression in lumbar in L-spine: l Causes pain in hip, posterior thigh, calf and foot (sciatica)
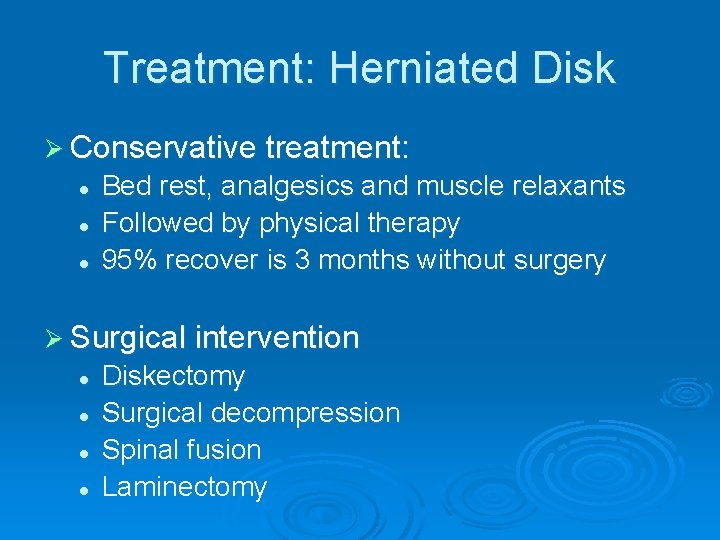
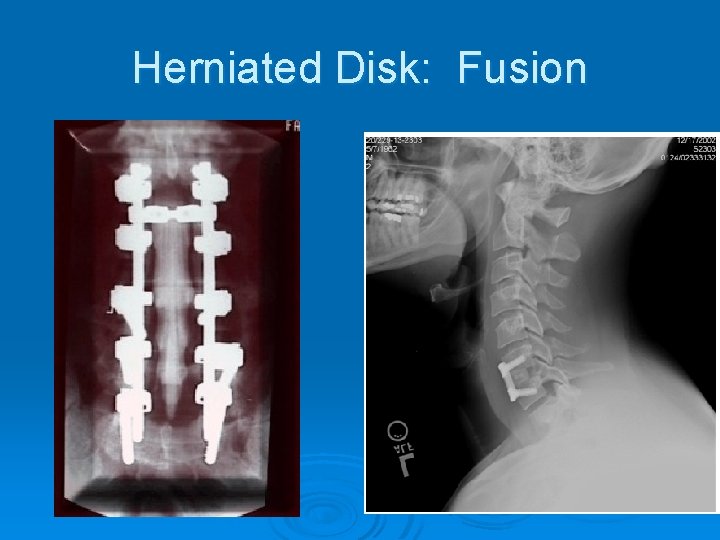
Treatment: Herniated Disk Ø Conservative treatment: l l l Bed rest, analgesics and muscle relaxants Followed by physical therapy 95% recover is 3 months without surgery Ø Surgical intervention l l Diskectomy Surgical decompression Spinal fusion Laminectomy
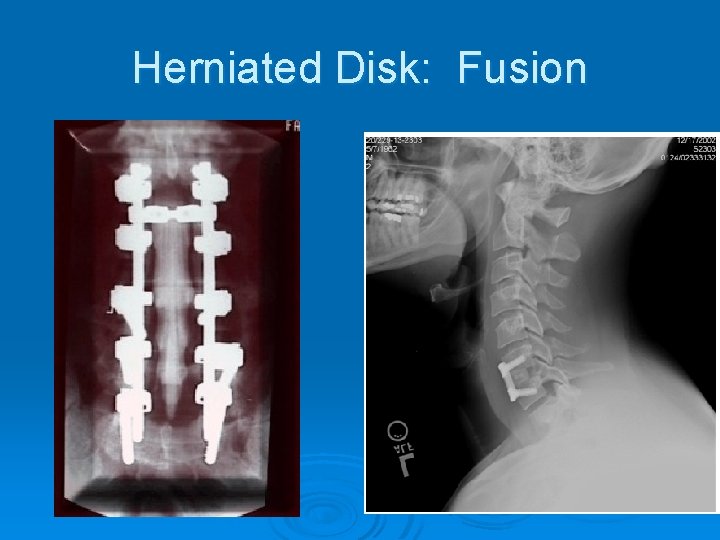
Herniated Disk: Fusion
Brain & Spinal Tumors
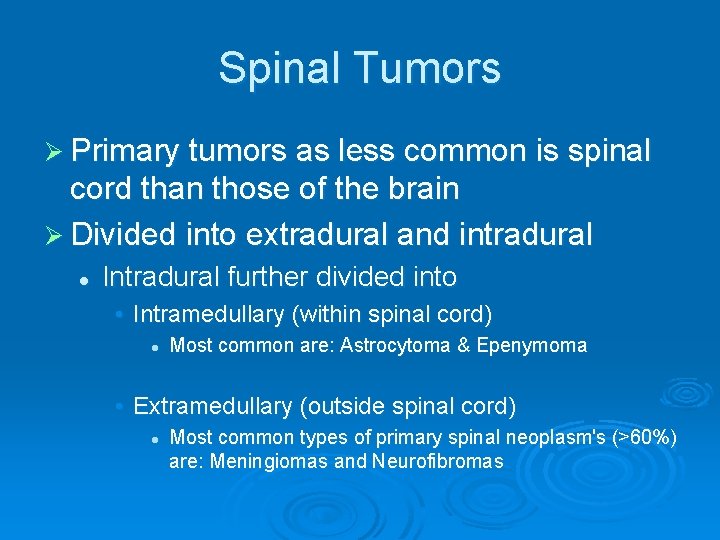
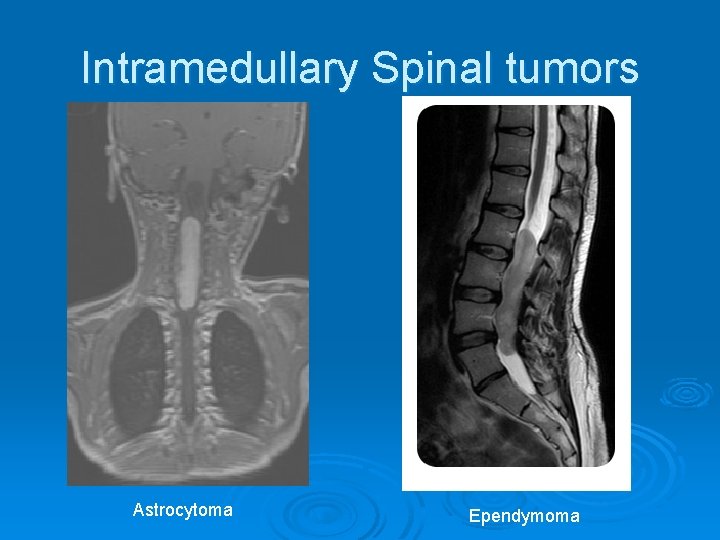
Spinal Tumors Ø Primary tumors as less common is spinal cord than those of the brain Ø Divided into extradural and intradural l Intradural further divided into • Intramedullary (within spinal cord) l Most common are: Astrocytoma & Epenymoma • Extramedullary (outside spinal cord) l Most common types of primary spinal neoplasm's (>60%) are: Meningiomas and Neurofibromas
Symptoms of Spinal Tumors Ø Extramedullary l l Similar symptoms as a herniated nucleus pulposus Compress nerve roots leading to pain and muscle weakness Ø Intramedullary l l Can cause progressive paraparesis Sensory loss

Extramedullary Spinal Tumors Neurofibroma Meningioma
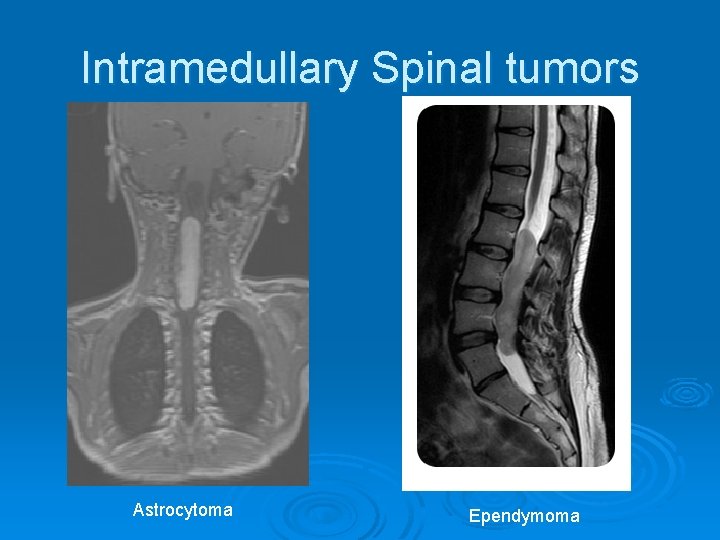
Intramedullary Spinal tumors Astrocytoma Ependymoma
Imaging of Spinal Tumors Ø MRI is the modality of choice Ø Conventional radiography l l l Can demonstrate bony destruction Widening of the vertebral pedicles CT myelo may be necessary to identify extradural tumors
Treatment of Spinal Tumors Ø Both intramedullary and extramedullary can be removed surgically l 50% of patients who have surgery experience a reverse of clinical anomalies Ø In cases where surgery is contraindicated l Radiation therapy is the primary means of treating a tumor
Brain Tumors Ø Gliomas acct for 50% of all brain tumors l l Ø Types of gliomas include: Astrocytoma & ependymoma Ependymomas predominate in 3 -4 yr olds Meningiomas are the most frequently occurring nonglial tumors l l Primarily affecting adults around 50 yrs old They are non-aggressive Ø All tumors have greater incidence in males Ø Interfere with circulation of the CSF causing a hydrocephalus
Brain Tumors Ø In children 20% of all tumors are brain tumors l l 60 – 70% are located in the cerebellum & posterior fossa Most common are astrocytomas, medulloblastomas, glioblastomas and craniopharyngliomas • 30% of primary ped. Tumors are medulloblastoma Ø In adults most prevalent are: l Astrocytomas, glioblastomas, metastatic tumors and menigiomas
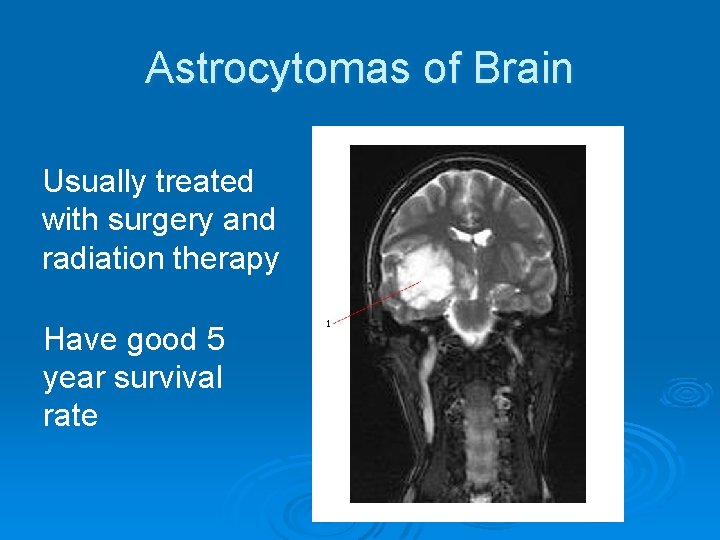
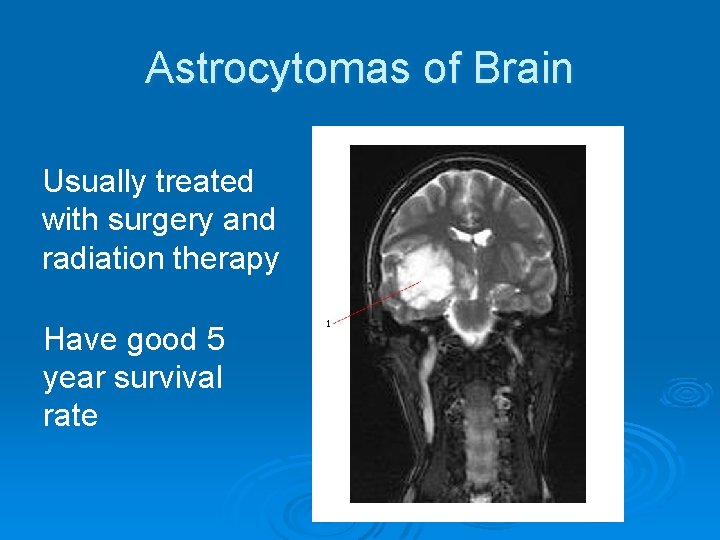
Astrocytomas of Brain Usually treated with surgery and radiation therapy Have good 5 year survival rate
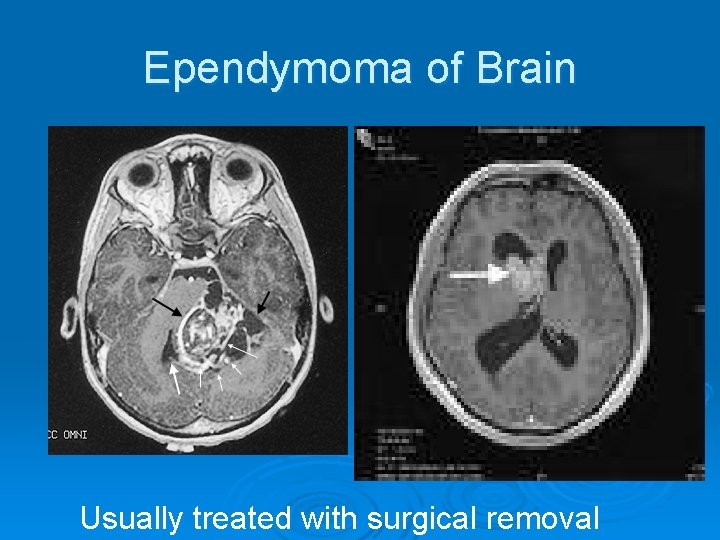
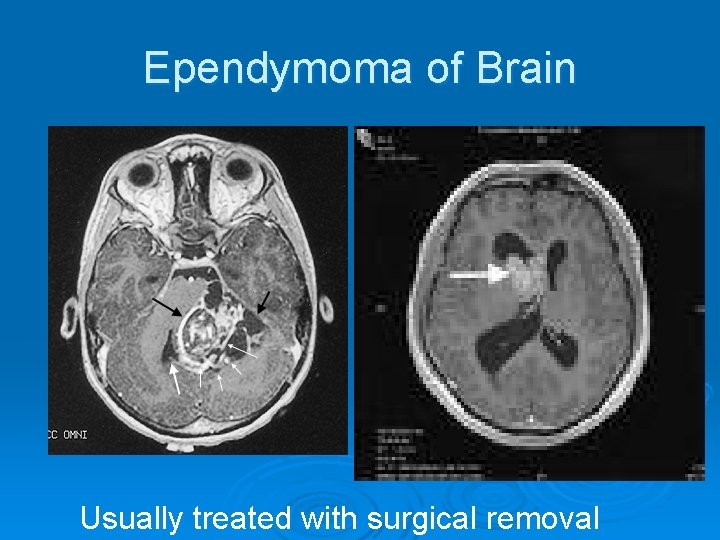
Ependymoma of Brain Usually treated with surgical removal
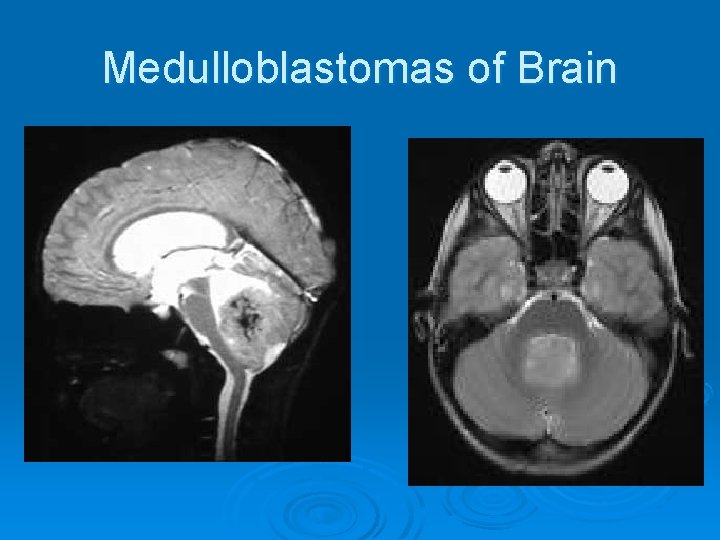
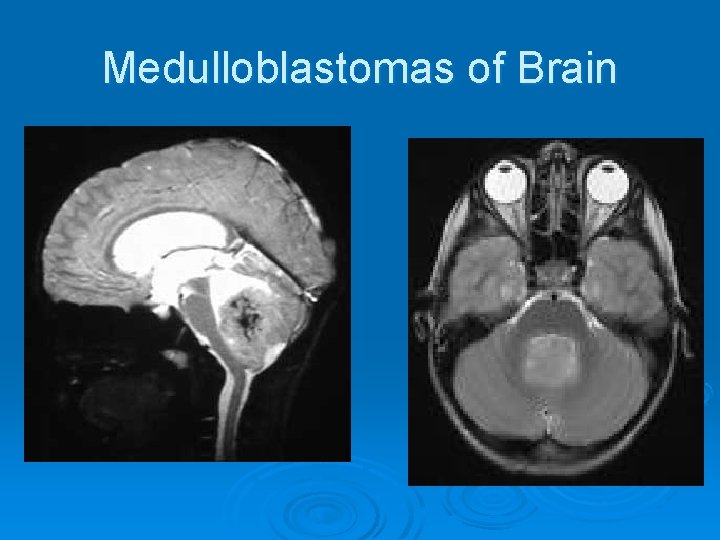
Medulloblastomas of Brain
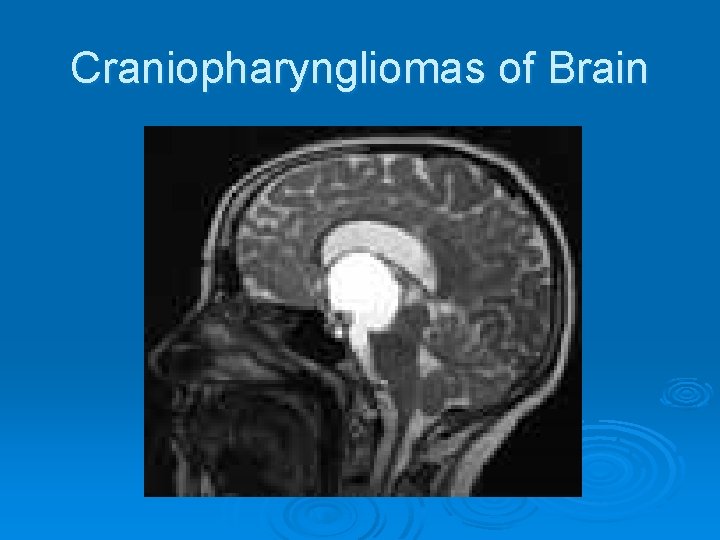
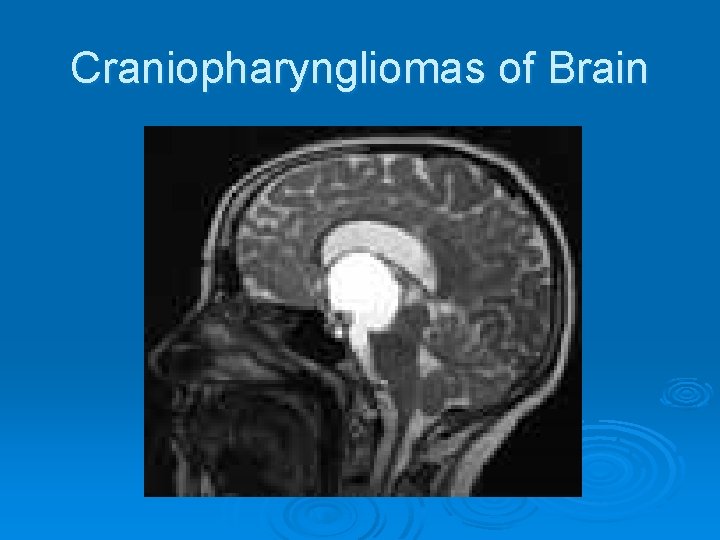
Craniopharyngliomas of Brain
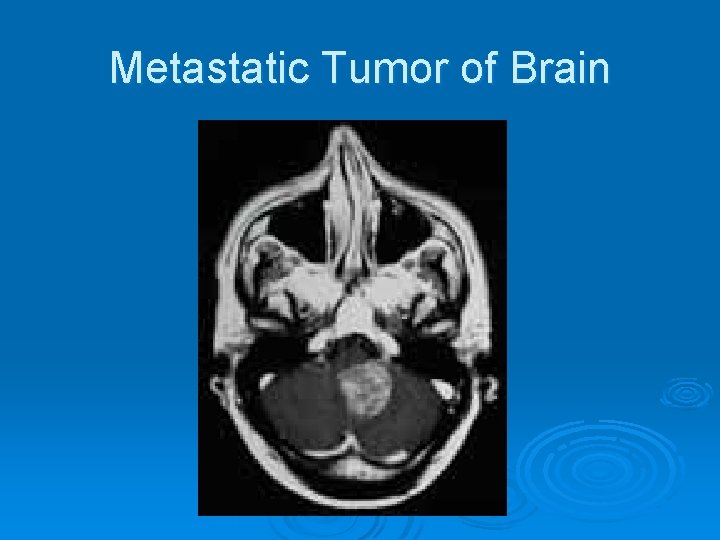
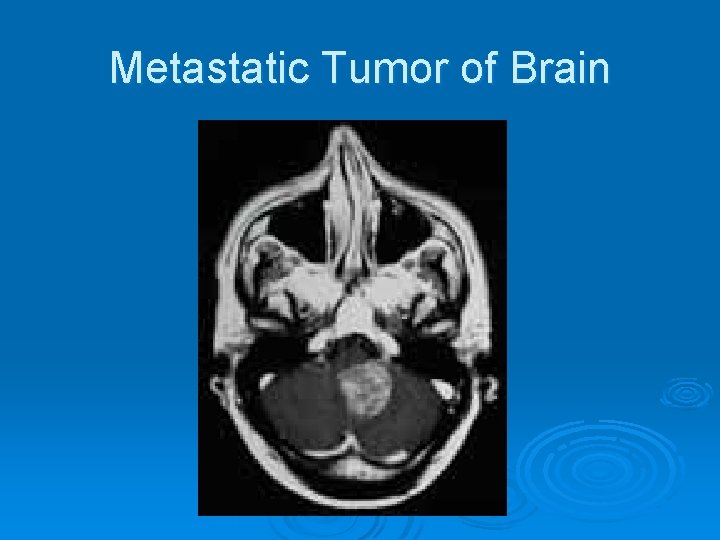
Metastatic Tumor of Brain
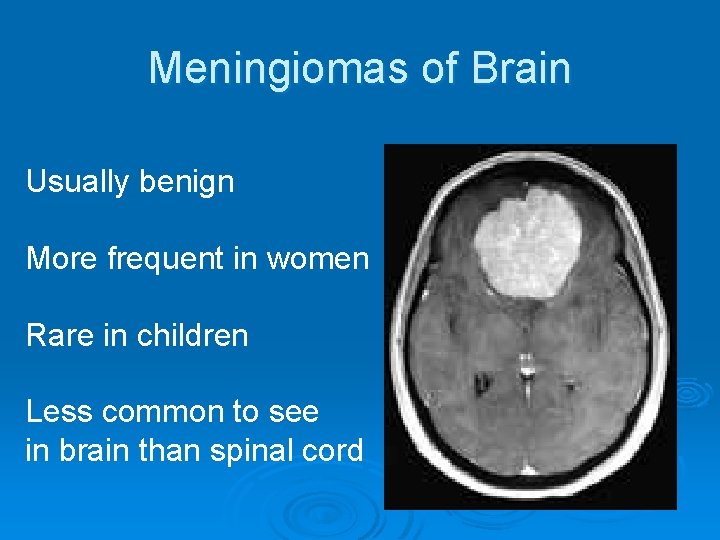
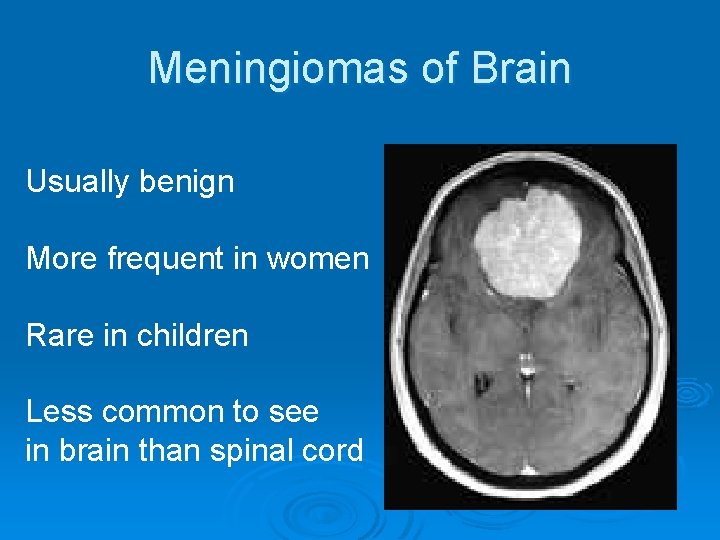
Meningiomas of Brain Usually benign More frequent in women Rare in children Less common to see in brain than spinal cord
Symptoms of Brain Tumors Headache Ø Nausea and Vomiting Ø Lethargy Ø Seizures Ø Paralysis Ø Aphasia Ø Blindness Ø Deafness Ø Abnormal changes in personality & behavior Ø
Treatment of Brain Tumors Ø Surgical resection Ø Radiation therapy l l Survival rate for surgery & Radiation therapy combined is 80% over a 5 year period Rate of survival decrease to 3% over a 10 year period
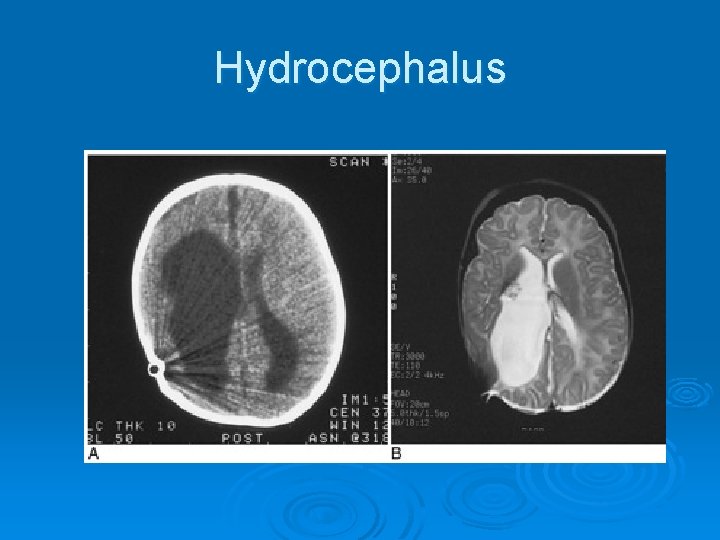
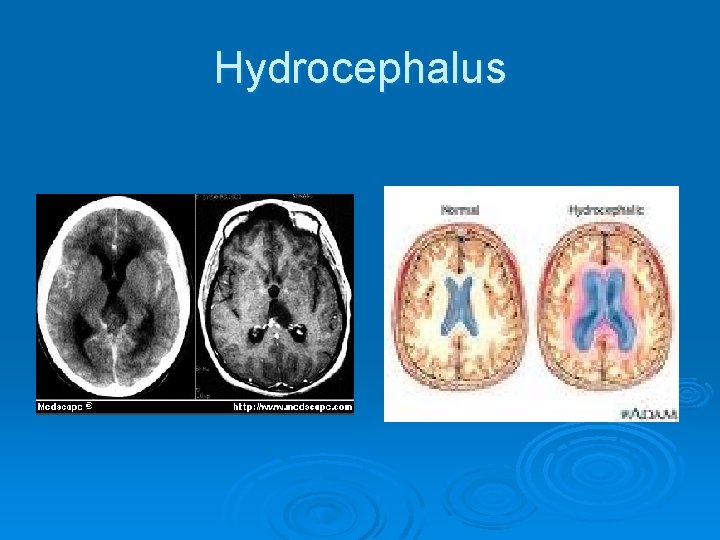
Hydrocephalus Can be congenital or acquired Ø Refers to an excessive amount of fluid in the ventricles Ø Two types Ø l Non- communicating • Interferes or blocks normal CSF circulation from the ventricles to the subarachnoid space l Communicating • Poor absorption of the CSF by the arachnoid Villi l Least common cause is from overproduction of CSF
Hydrocephalus Ø Non-communicating l l Can be congenital Can be from tumor growth Trauma (hemorrhage) Inflammation Ø Communicating l l Can come with increased cranial pressure Raised intrathoracic pressure impairing venous flow Inflammation from meningitis Subarachnoid hemorrhage
Radiographic Appearance Ø Generalized enlargement of the ventricular system Ø PA radiograph can reveal separation of the sutures Ø CT clearly demonstrates ventricular dilatation Ø MRI is more specific in demonstrating the underlying cause of obstruction or in excluding obstruction Ø Ultrasound is useful in utero and in infants l Sound waves transverse open fontanels
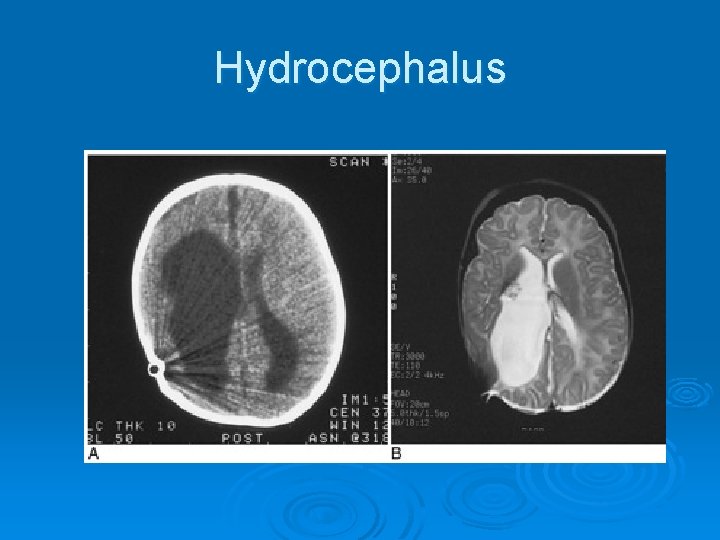
Hydrocephalus
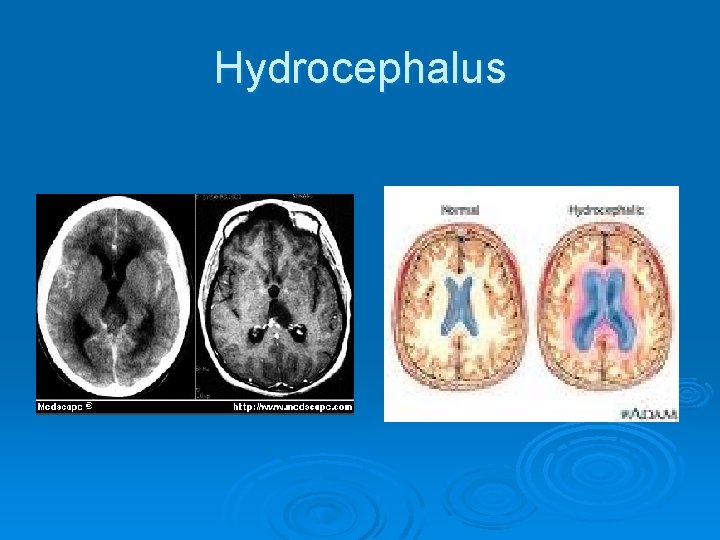
Hydrocephalus
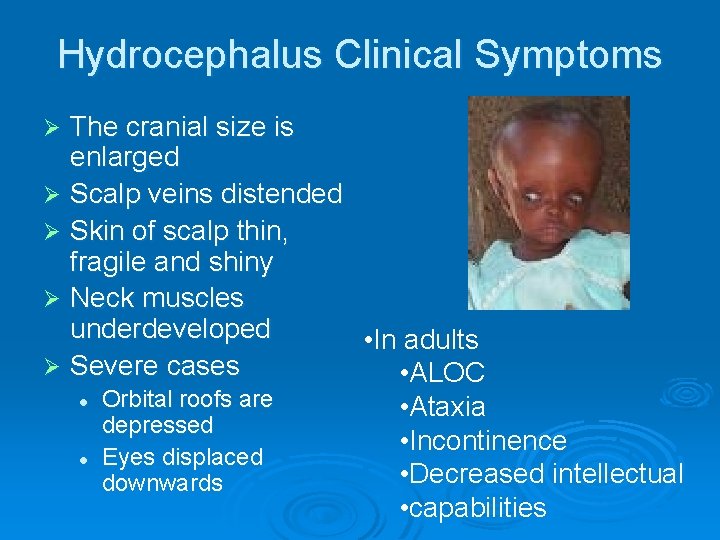
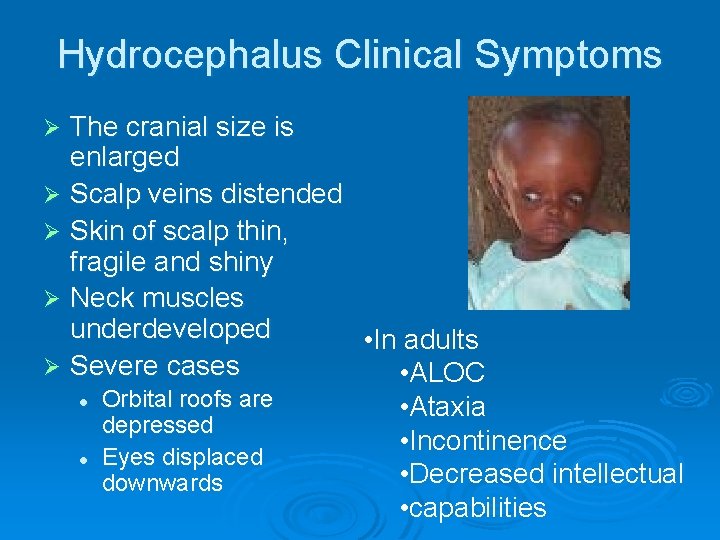
Hydrocephalus Clinical Symptoms The cranial size is enlarged Ø Scalp veins distended Ø Skin of scalp thin, fragile and shiny Ø Neck muscles underdeveloped • In adults Ø Severe cases • ALOC l Orbital roofs are • Ataxia depressed • Incontinence l Eyes displaced • Decreased intellectual downwards • capabilities Ø
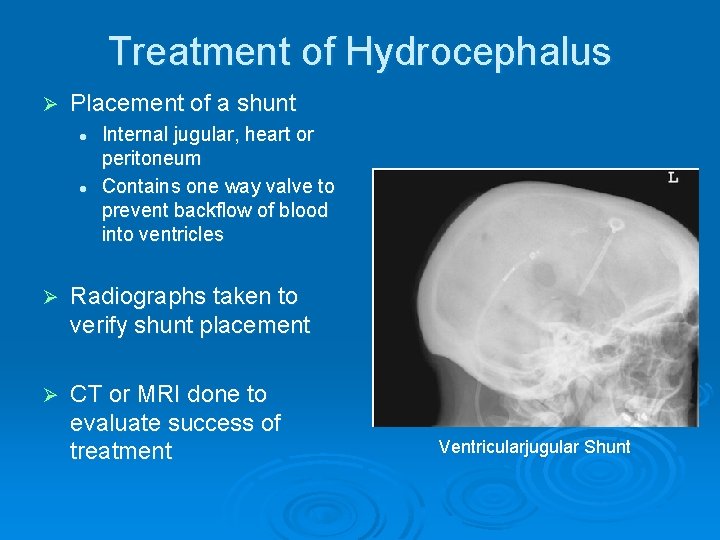
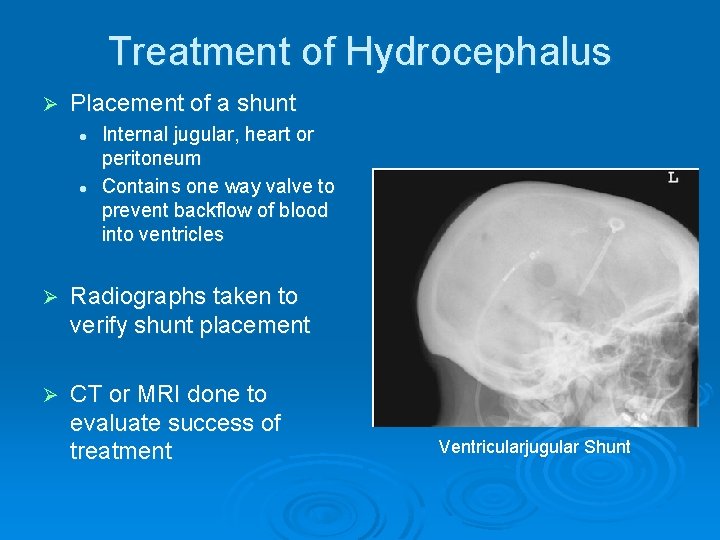
Treatment of Hydrocephalus Ø Placement of a shunt l l Internal jugular, heart or peritoneum Contains one way valve to prevent backflow of blood into ventricles Ø Radiographs taken to verify shunt placement Ø CT or MRI done to evaluate success of treatment Ventricularjugular Shunt
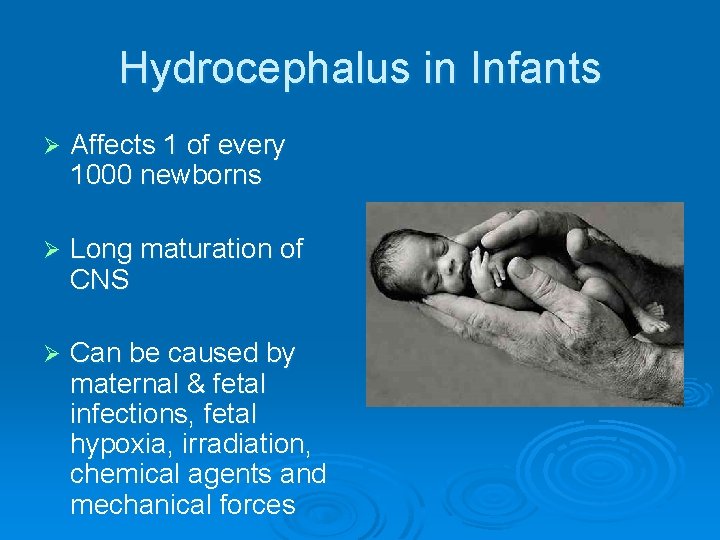
Hydrocephalus in Infants Ø Affects 1 of every 1000 newborns Ø Long maturation of CNS Ø Can be caused by maternal & fetal infections, fetal hypoxia, irradiation, chemical agents and mechanical forces
Hydrocephalus In Utero Ø X-ray used to be taken for fetal age and position Ø With hydrocephalic fetus- hard to deliver vaginally Ø Pelvimetry was ordered to determine measurements of inlet and outlet l l Very uncomfortable Three exposures
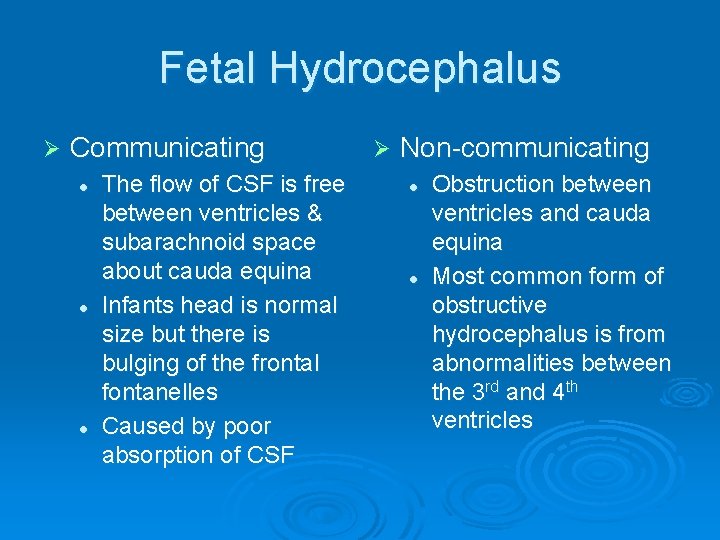
Fetal Hydrocephalus Ø Communicating l l l The flow of CSF is free between ventricles & subarachnoid space about cauda equina Infants head is normal size but there is bulging of the frontal fontanelles Caused by poor absorption of CSF Ø Non-communicating l l Obstruction between ventricles and cauda equina Most common form of obstructive hydrocephalus is from abnormalities between the 3 rd and 4 th ventricles
Multiple Sclerosis Ø Chronic progressive disease of the nervous system l Affects women more than men at approx 2040 years of age Ø There is no cure and it s origin is unknown l l l Treatment only slows the process Some research indicates it may come from herpes or retrovirus Appears more in temperate climants than tropical climates
Multiple Sclerosis Ø Demyelination of the myelin sheath covering nervous tissue of spinal cord & white matter within the brain Ø It has episodes of relapses and remission Ø Eventually leads to neurological damage l Ø Impairment of nerve conduction Patients life is not shortened l Quality of life is diminished
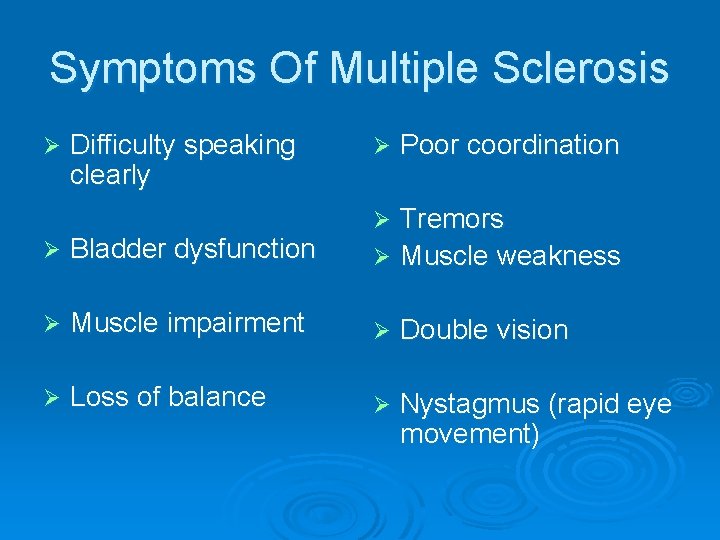
Symptoms Of Multiple Sclerosis Ø Difficulty speaking clearly Ø Poor coordination Tremors Ø Muscle weakness Ø Ø Bladder dysfunction Ø Muscle impairment Ø Double vision Ø Loss of balance Ø Nystagmus (rapid eye movement)
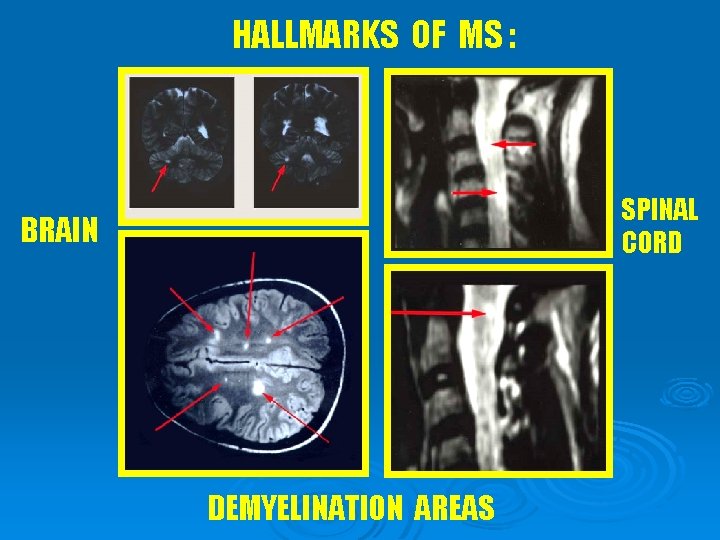
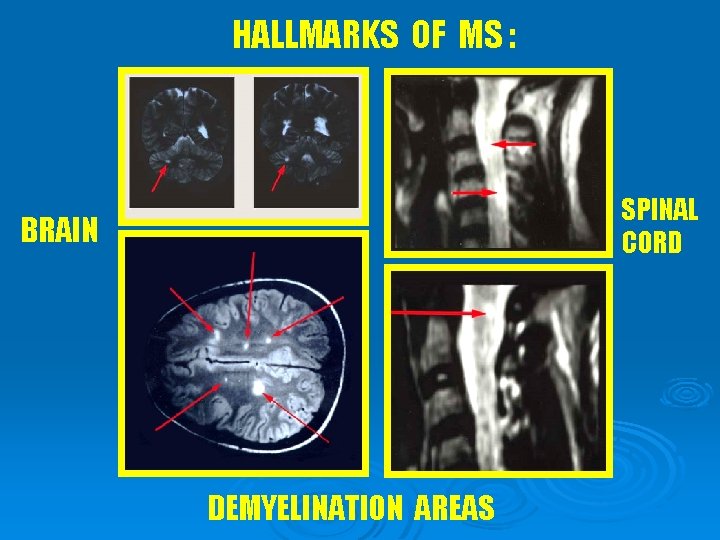
HALLMARKS OF MS : SPINAL CORD BRAIN DEMYELINATION AREAS
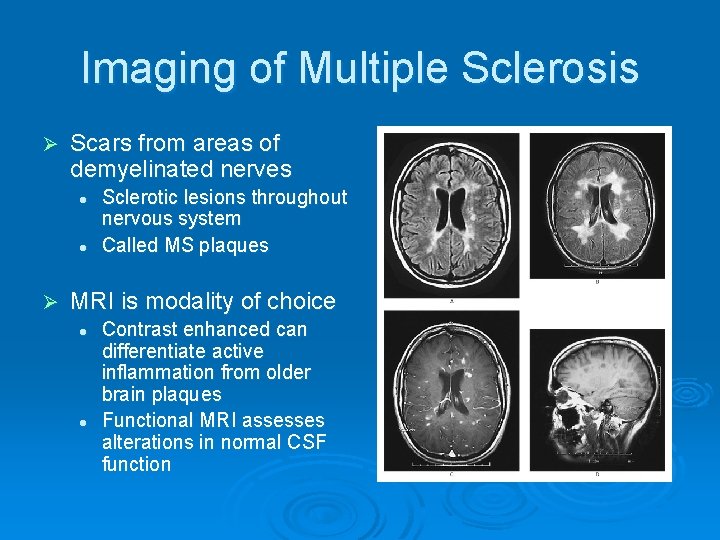
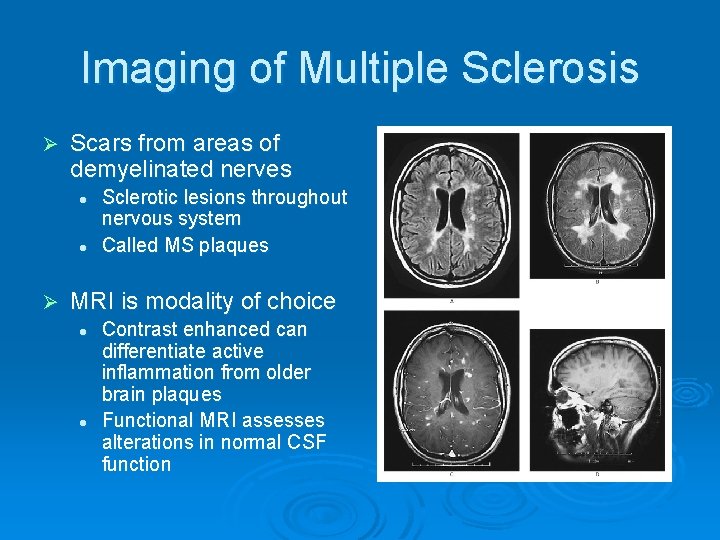
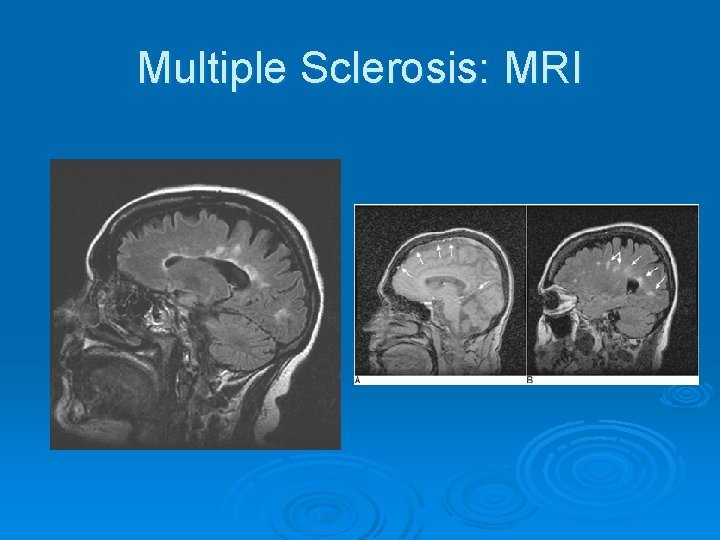
Imaging of Multiple Sclerosis Ø Scars from areas of demyelinated nerves l l Ø Sclerotic lesions throughout nervous system Called MS plaques MRI is modality of choice l l Contrast enhanced can differentiate active inflammation from older brain plaques Functional MRI assesses alterations in normal CSF function
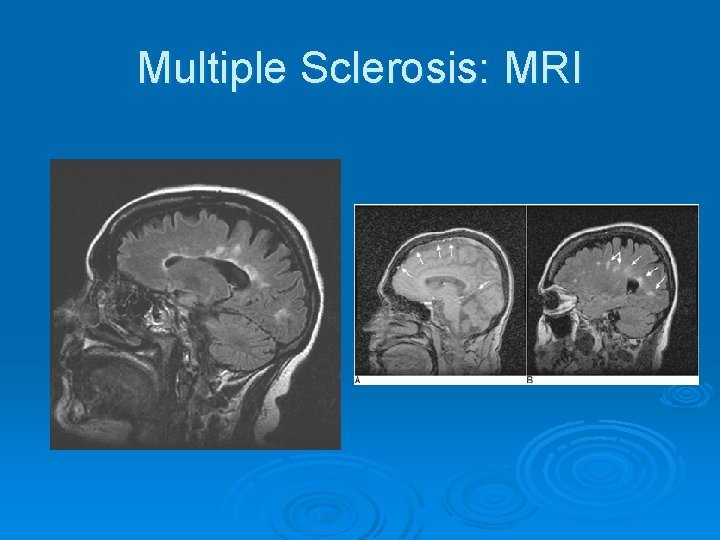
Multiple Sclerosis: MRI
CT imaging of Multiple Sclerosis Ø CT shows old inactive disease l Well defined areas of decreased attenuation Ø With contrast, in an acute phase l l Shows a mixture of decreased density (old) Enhancing regions (active)
Treatment for MS Ø Immunosuppressive agents l Ø Limit the autoimmune attack Corticosteroids (short term) l l Ø Antiviral l Ø Slows the progress of the disease Beta interferon l l l Immunomodulatory agents that reduce the severity of the attacks Given subcutaneously Ø Shortens the symptomatic periods Delays progression of disease Reduces frequency of attacks Regular exercise l Reduces spasms and increases ROM
Cerebrovascular Accident (CVA) Is an atherosclerotic disease affecting blood supply to the brain Ø 3 rd leading cause of death in U. S. Ø 2 types of stroke: Ø l Ø Both CT and MRI distinguish between the two types l l Ø Ischemic and Hemorrhagic MRI is especially sensitive to infarction within hours of onset CT, at times appears negative for a day or so Carotid duplex and MRA are also useful in the diagnosis of a stroke
Ischemic Stroke Blood clot blocks a blood vessel in the brain Ø Is the majority of strokes Ø Ø Two types: l Thrombosis of cerebral artery • Blood clot that blocks a blood vessel l Embolism of the brain • Is a mass of undissolved matter (solid, liquid or gas) present in a blood vessel brought there by blood current Ø Diagnosed with CT and MRI l Angiography can be used if other modalites are questionable
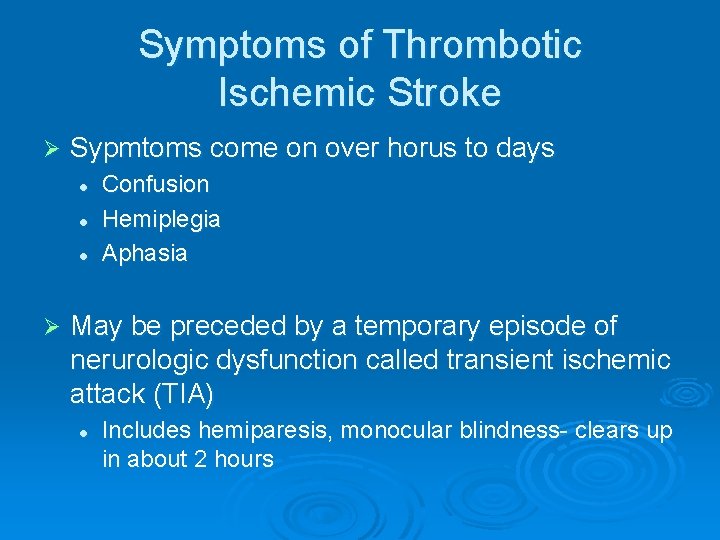
Symptoms of Thrombotic Ischemic Stroke Ø Sypmtoms come on over horus to days l l l Ø Confusion Hemiplegia Aphasia May be preceded by a temporary episode of nerurologic dysfunction called transient ischemic attack (TIA) l Includes hemiparesis, monocular blindness- clears up in about 2 hours
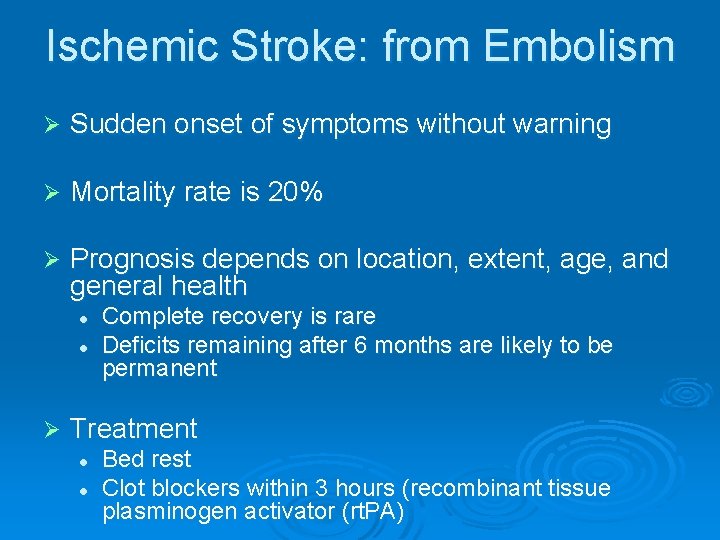
Ischemic Stroke: from Embolism Ø Sudden onset of symptoms without warning Ø Mortality rate is 20% Ø Prognosis depends on location, extent, age, and general health l l Ø Complete recovery is rare Deficits remaining after 6 months are likely to be permanent Treatment l l Bed rest Clot blockers within 3 hours (recombinant tissue plasminogen activator (rt. PA)
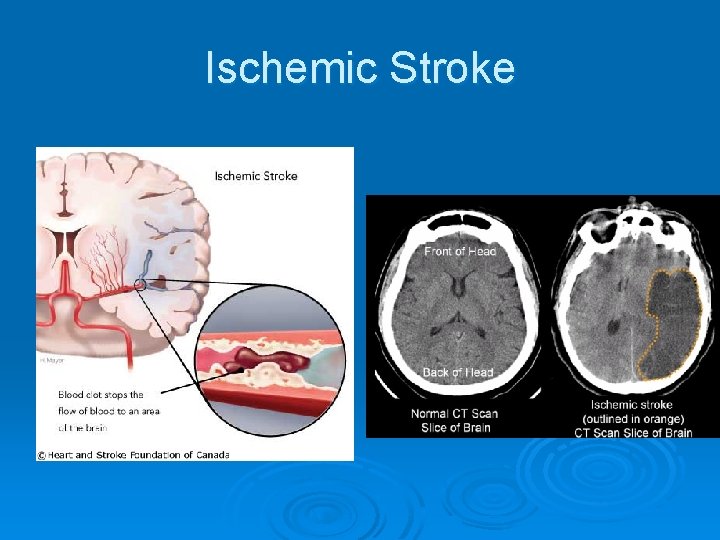
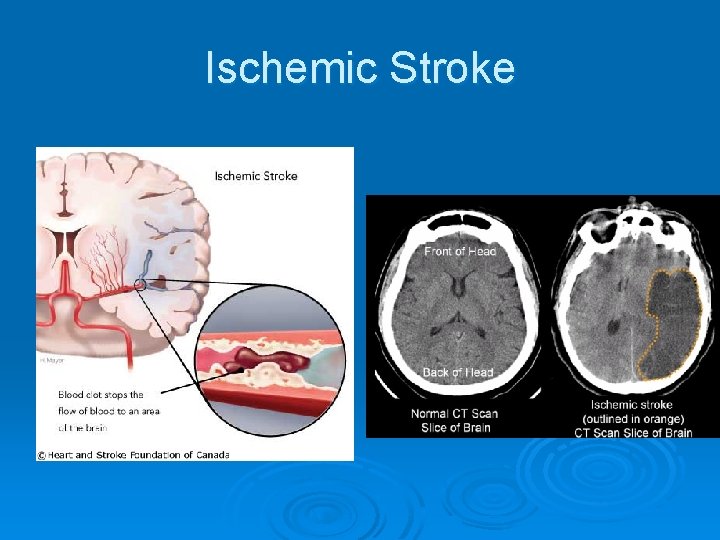
Ischemic Stroke
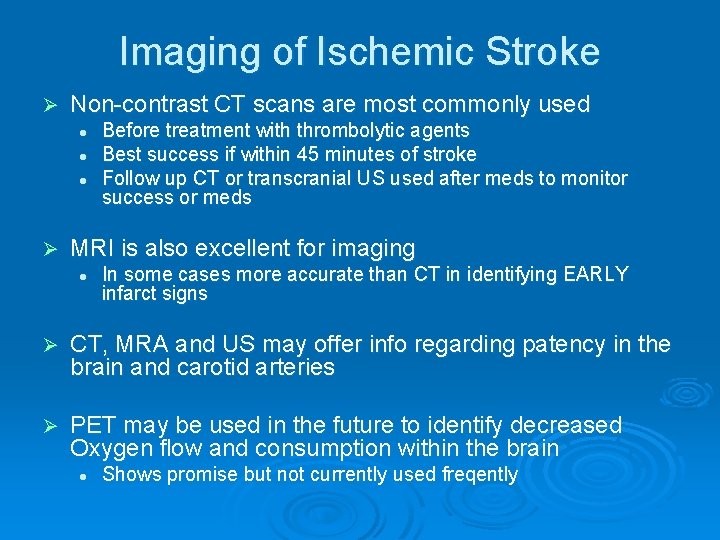
Imaging of Ischemic Stroke Ø Non-contrast CT scans are most commonly used l l l Ø Before treatment with thrombolytic agents Best success if within 45 minutes of stroke Follow up CT or transcranial US used after meds to monitor success or meds MRI is also excellent for imaging l In some cases more accurate than CT in identifying EARLY infarct signs Ø CT, MRA and US may offer info regarding patency in the brain and carotid arteries Ø PET may be used in the future to identify decreased Oxygen flow and consumption within the brain l Shows promise but not currently used freqently
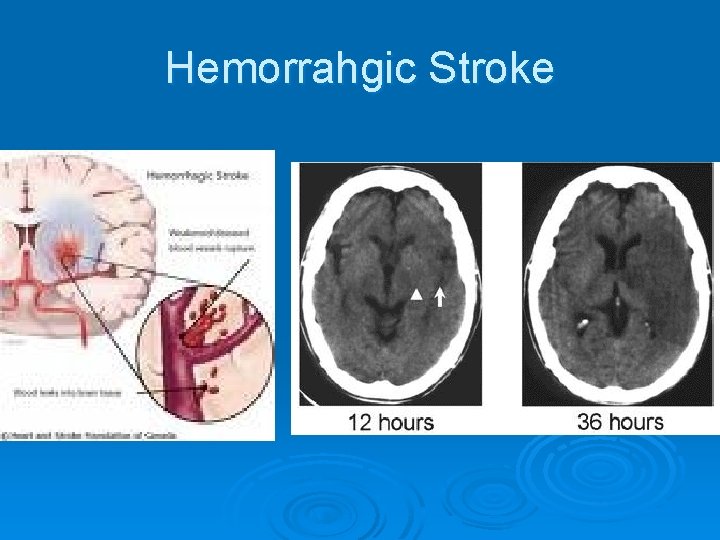
Hemorrahgic Stroke Ø Occurs from a weaknening in the diseased blood vessel l Typically weakened from atheroscleosis from hypertension Ø Sudden and often lethal because it comes on so suddenly Ø Accoutns for 10 -15% of all CVA’s Ø Two types: l Subarachnoid and Intracerebral
Hemorrahgic Stroke Ø Most occur in the cerebrum and bleed into lateral ventricle Ø Most often preceded by an intense headache and vomiting Ø LOC follows in minutes and leads to contralateral hemiplegia or death Ø Prognosis is poor l l 35% die day after stroke 15% die within a few weeks, usually from another vessel rupture
Imaging of Hemorrahgic Strokes Ø CT is modality of choice l l l Can demonstrate high density blood in the subarachnoid space in more than 95% of cases Can demonstrate aneurysms greaeter than 3 mm With contrast is contraindicated because surgeon will not operate without an angiogram Ø MRI is relatively insensitive for subarachoid bleeds
Treatment of Hemorrahgic Strokes Ø Surgery l Preceded by a surgical angiogram Ø If surgical intervention is postponed the angiogram so will
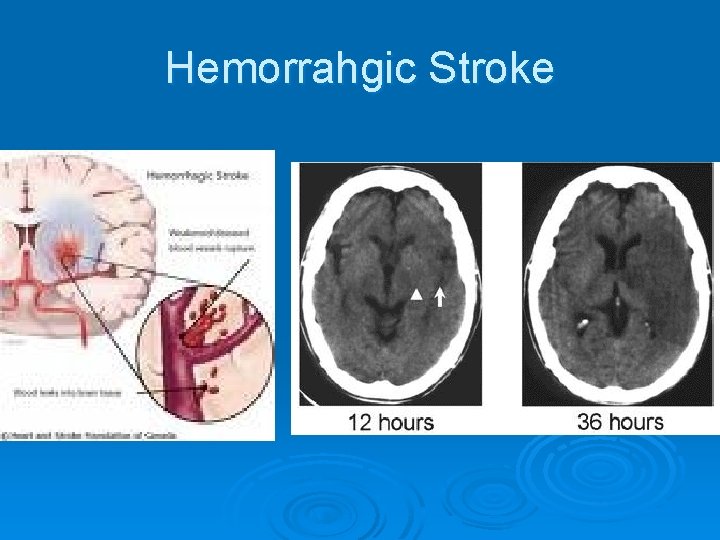
Hemorrahgic Stroke
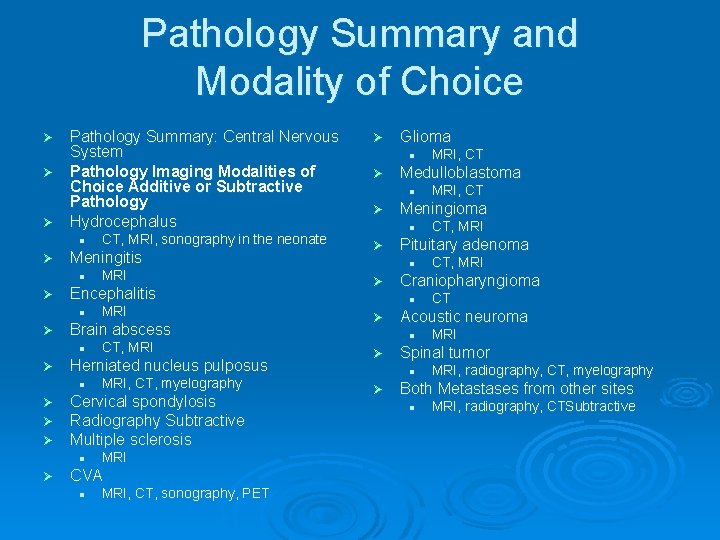
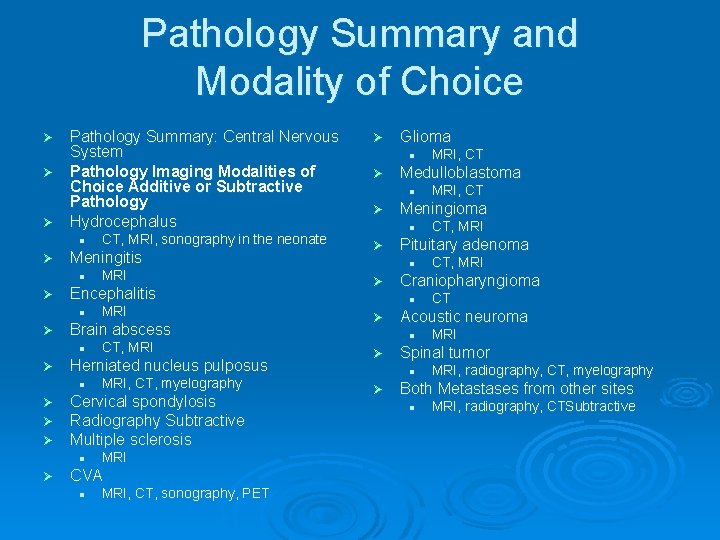
Pathology Summary and Modality of Choice Pathology Summary: Central Nervous System Ø Pathology Imaging Modalities of Choice Additive or Subtractive Pathology Ø Hydrocephalus Ø l Ø Meningitis l Ø MRI, CT, myelography Cervical spondylosis Radiography Subtractive Multiple sclerosis l Ø CT, MRI Herniated nucleus pulposus l Ø Ø Ø MRI Brain abscess l Ø MRI Encephalitis l Ø CT, MRI, sonography in the neonate MRI CVA l MRI, CT, sonography, PET Ø Glioma l Ø Medulloblastoma l Ø MRI Spinal tumor l Ø CT Acoustic neuroma l Ø CT, MRI Craniopharyngioma l Ø CT, MRI Pituitary adenoma l Ø MRI, CT Meningioma l Ø MRI, CT MRI, radiography, CT, myelography Both Metastases from other sites l MRI, radiography, CTSubtractive