CNS Pathology Inflammatory and Infectious Disorders Infection Leptomeningitis
































- Slides: 103
CNS Pathology Inflammatory and Infectious Disorders
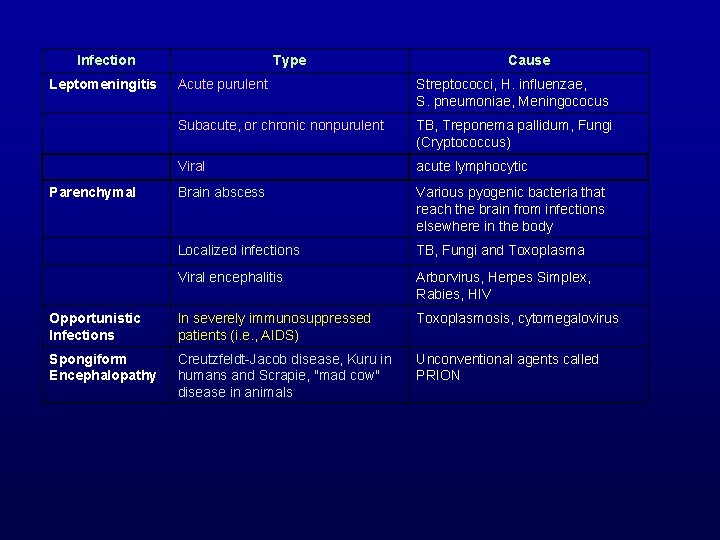
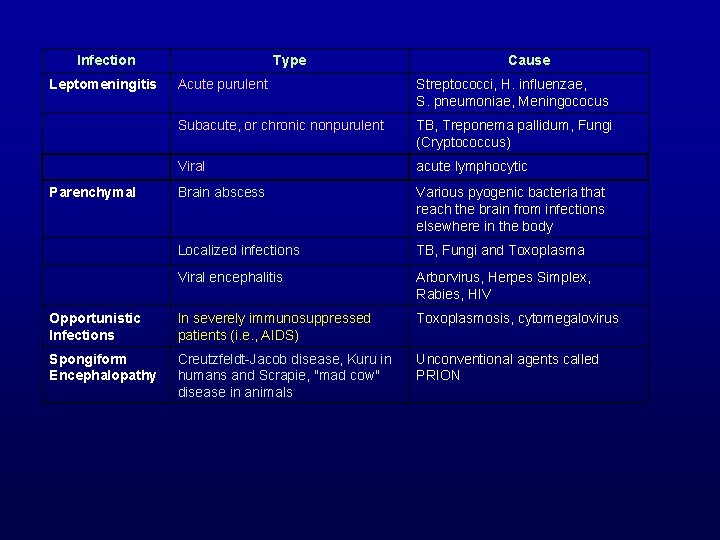
Infection Leptomeningitis Type Cause Acute purulent Streptococci, H. influenzae, S. pneumoniae, Meningococus Subacute, or chronic nonpurulent TB, Treponema pallidum, Fungi (Cryptococcus) Viral acute lymphocytic Brain abscess Various pyogenic bacteria that reach the brain from infections elsewhere in the body Localized infections TB, Fungi and Toxoplasma Viral encephalitis Arborvirus, Herpes Simplex, Rabies, HIV Opportunistic Infections In severely immunosuppressed patients (i. e. , AIDS) Toxoplasmosis, cytomegalovirus Spongiform Encephalopathy Creutzfeldt-Jacob disease, Kuru in humans and Scrapie, "mad cow" disease in animals Unconventional agents called PRION Parenchymal

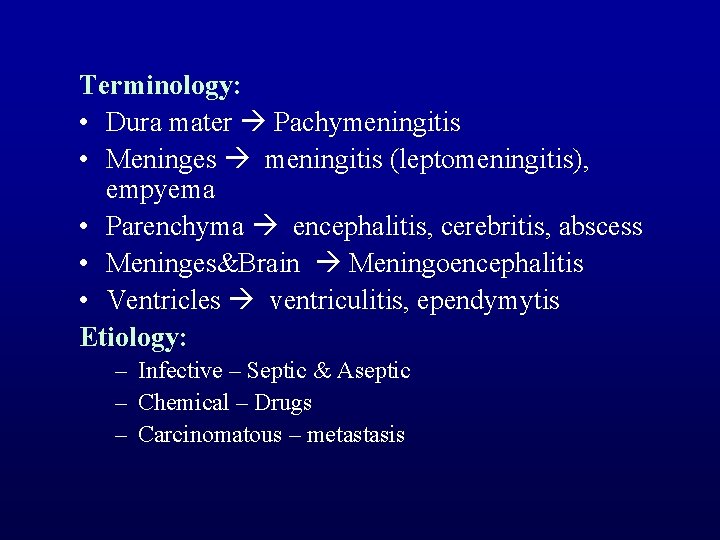
Classification of CNS INFECTIONS ETIOLOGY ANATOMY 1. MENINGES 2. PARENCHYMA 3. VENTRICLES 1. BACTERIAL meningitis, empyema 2. VIRAL encephalitis, cerebritis, abscess 3. FUNGAL ventriculitis, ependymytis 4. Others - PROTOZOAL - METAZOAL
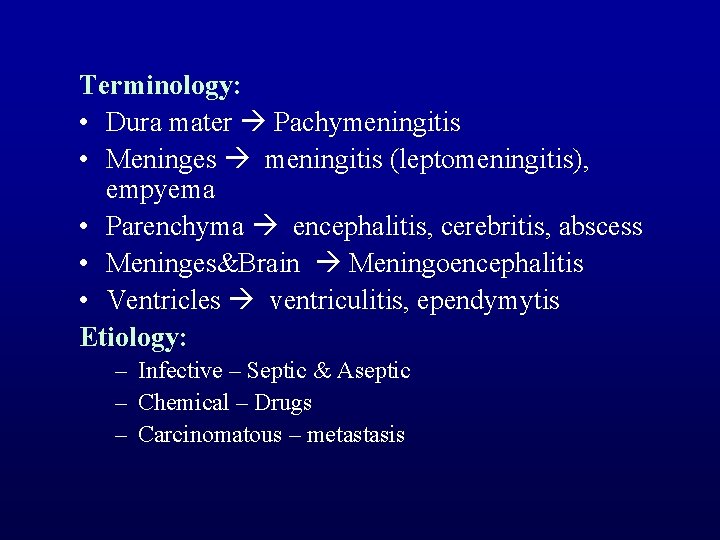
Terminology: • Dura mater Pachymeningitis • Meninges meningitis (leptomeningitis), empyema • Parenchyma encephalitis, cerebritis, abscess • Meninges&Brain Meningoencephalitis • Ventricles ventriculitis, ependymytis Etiology: – Infective – Septic & Aseptic – Chemical – Drugs – Carcinomatous – metastasis
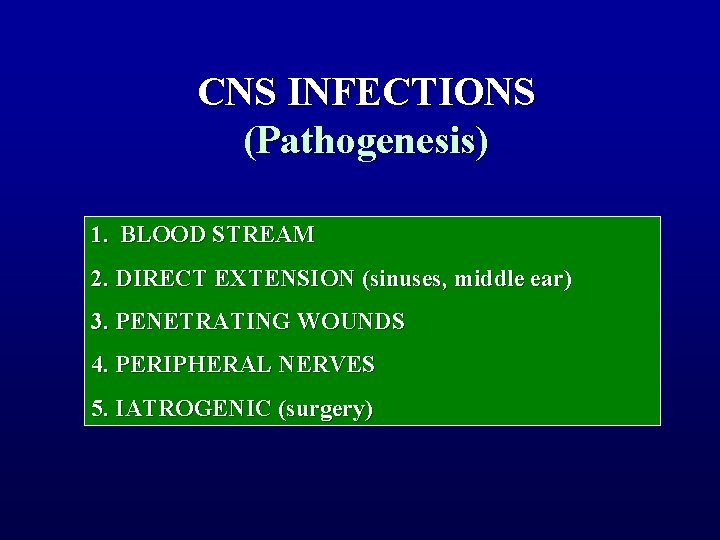
CNS INFECTIONS (Pathogenesis) 1. BLOOD STREAM 2. DIRECT EXTENSION (sinuses, middle ear) 3. PENETRATING WOUNDS 4. PERIPHERAL NERVES 5. IATROGENIC (surgery)

• Complications: – Encephalitis – Infarction – Abscess – Empyema – Raised ICP (Herniation & Hydrocephalus)
MAJOR CATEGORIES of CNS INFECTIONS • • • Bacterial: meningitis and abscess Fungal: meningitis and abscess Tuberculosis: tuberculoma and meningitis Neurosyphilis Parasitic Viral – acute – chronic • Unconventional transmissible agents
Risk groups • • The very young and the very old Alcoholics Patients with neural tube defects Patients with CNS trauma, or after neurosurgical intervention • Patients who are immunocompromised for any reason • Patients with sickle cell anemia • Patients with cardiac and pulmonary anomalies
BACTERIAL INFECTIONS • • • Meningitis Intracranial thrombophlebitis Brain abscess Epidural abscess Subdural empyema
Variables: Systemic Manifestations • Meningococcus: Massive derangement (bacteriemia, shock, DIC, etc. ) • Other organisms: CNS problems predominate (next slide) • Epidemic outbreaks: Meningococcus is the predominant organism (dorms, military barracks, etc. )
Variables: Age of onset • Neonatal: Coliforms, Group B Streptococci • Toddlers: Hemophilus influenzae B (decreasing in incidence, due to HIB vaccine) • Children, young adults: Meningococcus (vaccine available, routinely given to military recruits) • Young and adults: Pneumococcus (vaccine available for both age groups)
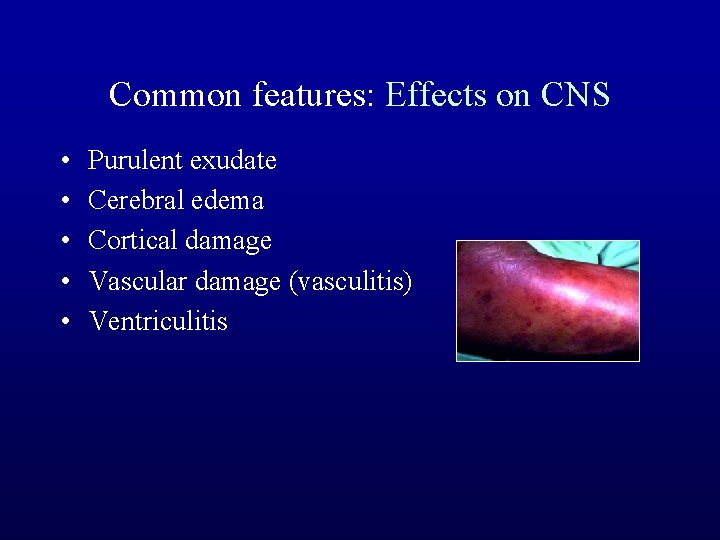
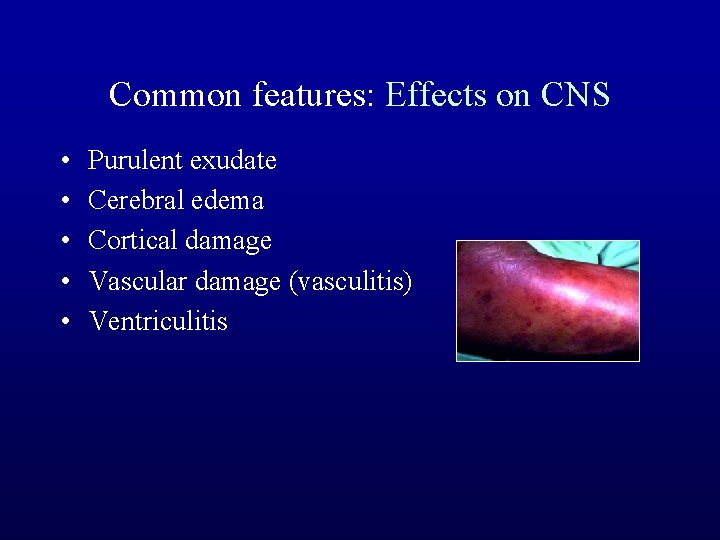
Common features: Effects on CNS • • • Purulent exudate Cerebral edema Cortical damage Vascular damage (vasculitis) Ventriculitis
Acute Pyogenic Leptomeningitis Purulent meningitis • An acute inflammation of the leptomeninges and subarachnoid space • Usually the infection is diffuse, since the CSF is a good culture medium & rapidly disseminates bacteria throughout the subarachnoid space
Origin • Hematogenous (bacteremia, infected emboli, septic thrombophlebitis) • Direct extension (otitis, sinusitis, mastoiditis, brain abscess) • Penetrating wounds • Developmental anomalies (neural tube defects)
Common organisms vary depending on the age of the patient • Infancy – – E. coli Group B Strep Staphylococcus L. monocytogenes • Childhood – H. influenzae – Pneumococcus – Meningococcus • Adulthood – Meningococcus – Pneumococcus

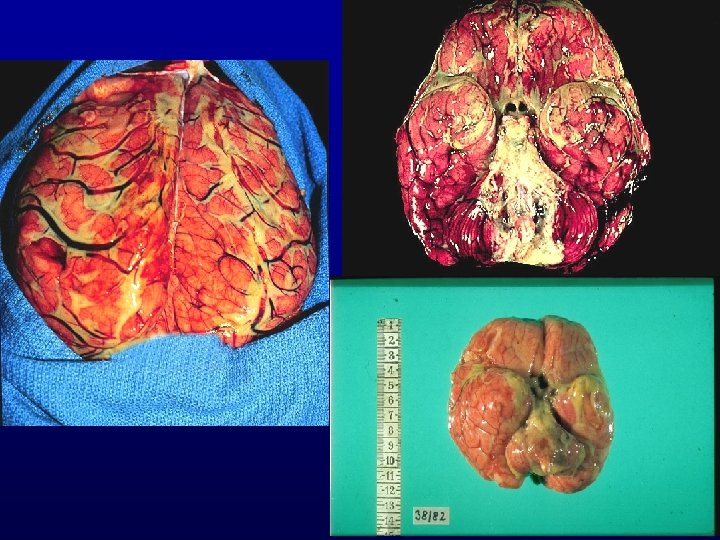
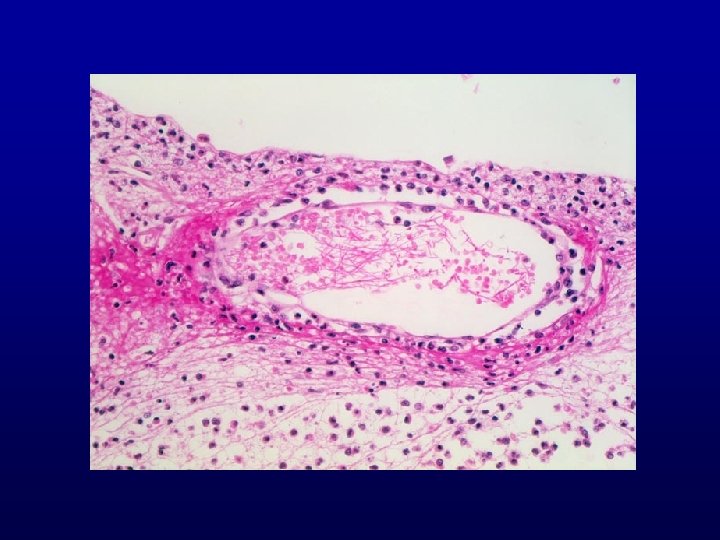
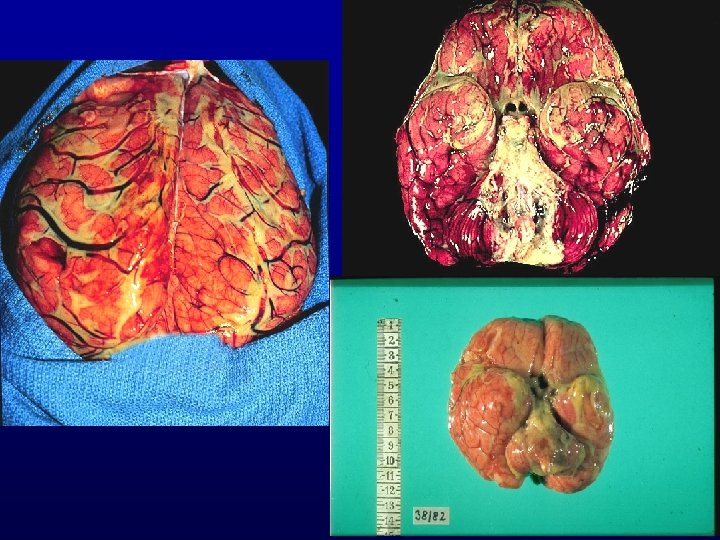
Pathology • The CSF is cloudy and contains many neutrophils • Protein is increased and glucose is reduced • Gram stain may demonstrate the causative organism (Gram negative diplococci = meningococci) • The meninges are opaque due to a covering of exudate, which often extends along the arachnoidal vessels – exudate tends to concentrate over the cerebral hemispheres in S. Pneumoniae meningitis – tends to be basal in location in H. Influenzae infection

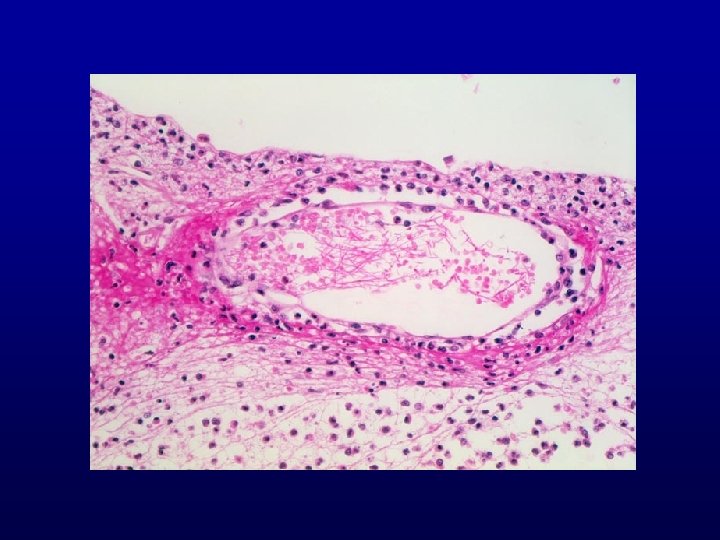
Pathology • Hyperemia of meningeal vessels • Exudation of polymorphonuclear (PMN) leukocytes • Location of the subarachnoid exudate- pus tends to accumulate along the course of cortical veins – Neutrophils are present in the subarachnoid/Virchow - Robin spaces and sometimes fill these spaces – Secondary invasion of the brain produces a meningoencephalitis – In fulminant cases, there may be involvement of the leptomeningeal veins - which may develop a septic thrombophlebitis with secondary venous infarction of the brain • Cerebral edema (slight to moderate)

• CSF mostly PMN, high protein, low sugar, high pressure, and positive cultures • Healing – complete resolution – fibrosis hydrocephalus • Meningococcal meningitis frequently accompanied by – meningococcemia – myocarditis – adrenal hemorrhage (W-F) – sudden death

Complications • 1. Brain swelling: An important early step in meningeal inflammation is the local release of cytokines by host cells. This release is induced by bacterial cell wall material. These cytokines initiate meningeal inflammation and brain swelling, which may be rapid and fatal (especially in meningococcal and pneumococcal infections). • 2. Hypoxic brain damage: In Gram negative infections, endotoxic shock may lead to severe hypotension and hypoxic brain damage.
• 3. Septicemia • 4. Waterhouse-Friderichsen syndrome: In meningococcal infection, organisms and/or toxins initiate the vascular damage and DIC, resulting in widespread petechial hemorrhages, which may affect many organs, including the brain. – An important complication of this process is hemorrhagic necrosis of the adrenal glands. • 5. Hydrocephalus: Organization of the subarachnoid exudate can produce adhesions (adhesive arachnoiditis) - obstructing the flow of CSF and producing a communicating hydrocephalus. – Early: Empyema acute hydrocephalus; – Late: Blockage of CSF pathways obstructive hydrocephalus.

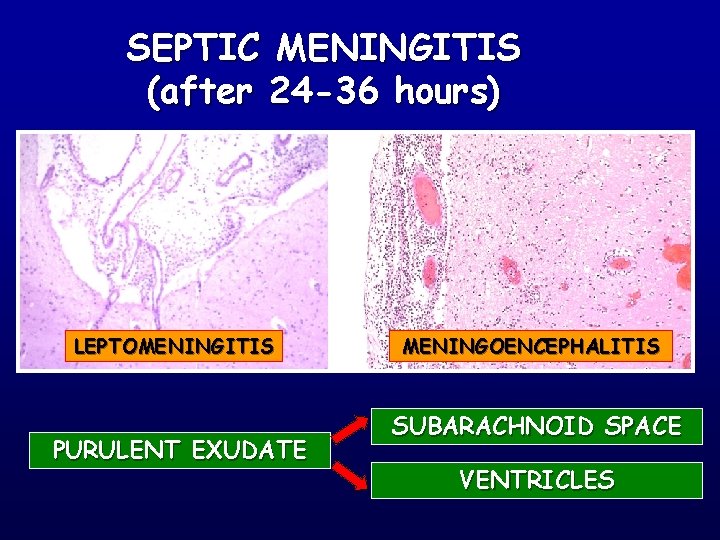
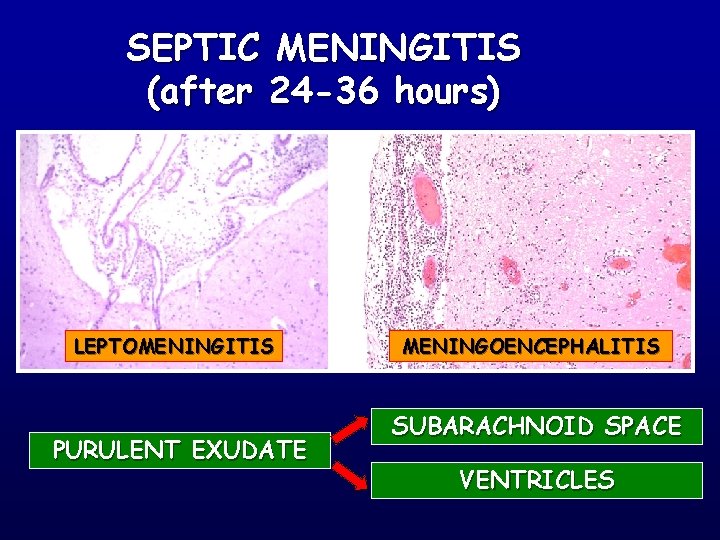
SEPTIC MENINGITIS (after 24 -36 hours) LEPTOMENINGITIS PURULENT EXUDATE MENINGOENCEPHALITIS SUBARACHNOID SPACE VENTRICLES


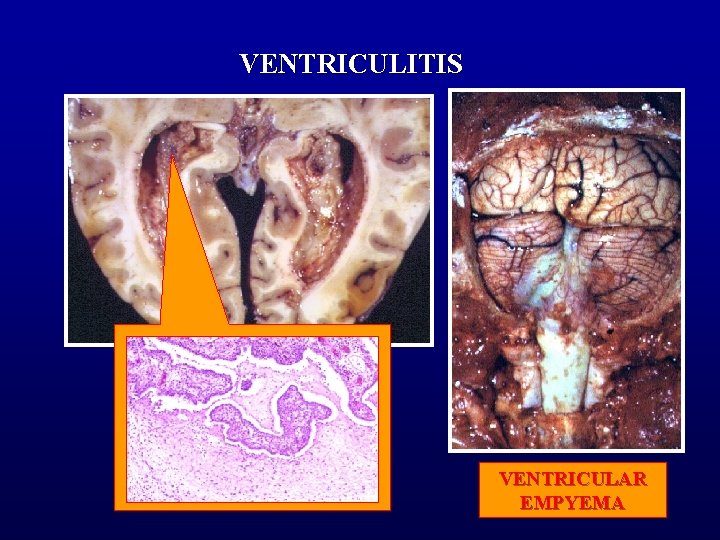
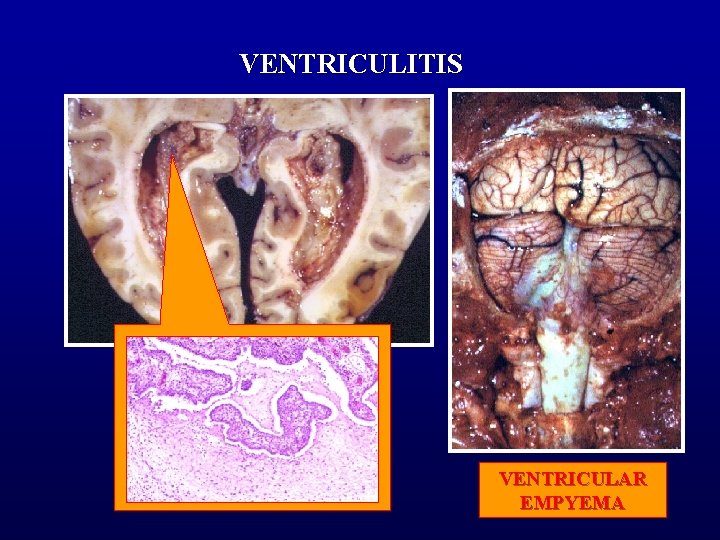
VENTRICULITIS VENTRICULAR EMPYEMA


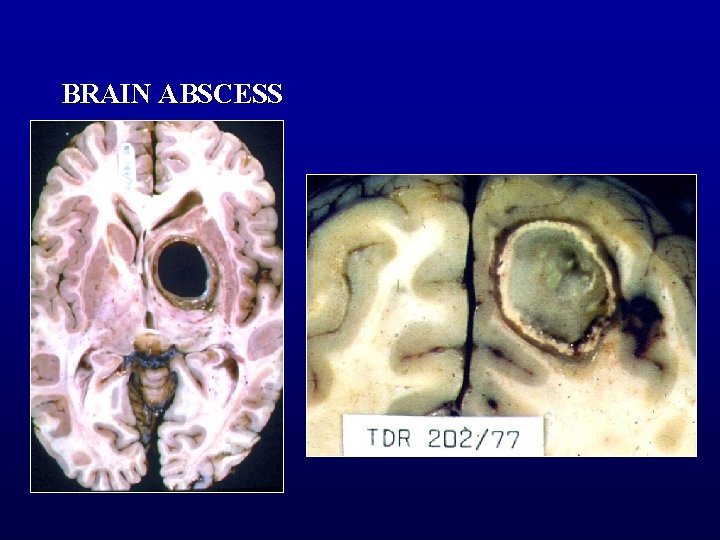
Brain Abscess • Bacterial and fungal organisms • Sources of brain abscesses – Otogenous (temporal lobe or cerebellar) – Rhinogenic (paranasal sinuses) – Traumatic (e. g. , stab wound) – Metastatic, hematogenously spread from • Bacterial endocarditis, septicemia • Lung abscess or bronchiectasis • Intestinal flora in congenital heart disease with a right to left shunt • Osteomyelitis
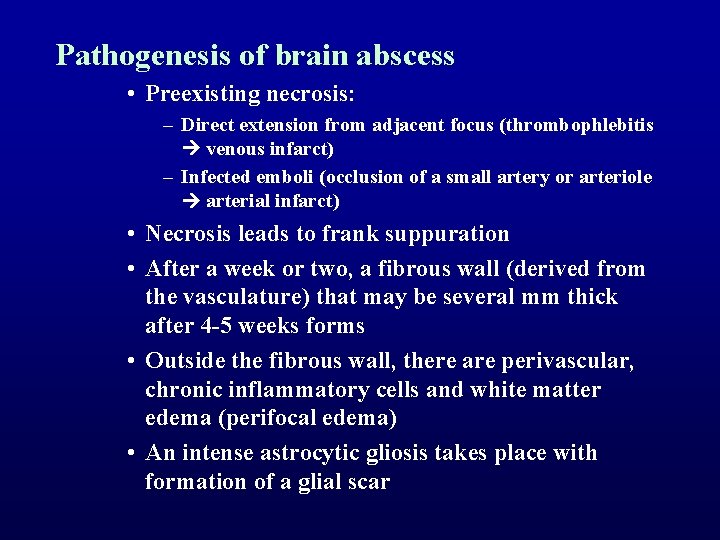
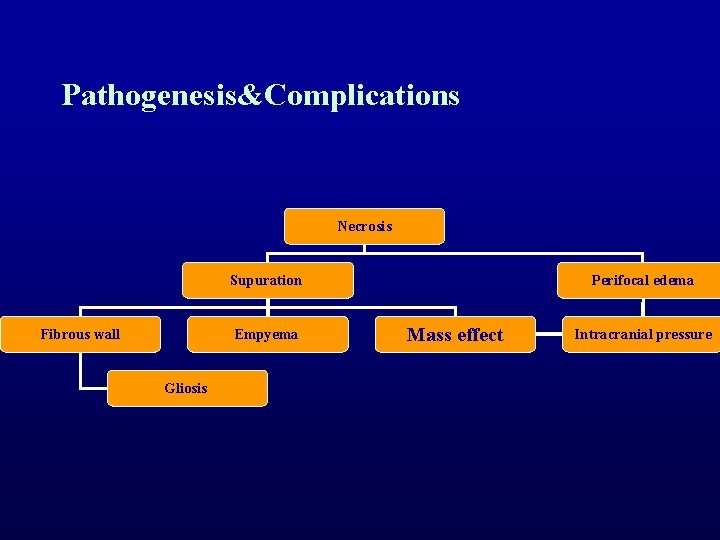
Pathogenesis of brain abscess • Preexisting necrosis: – Direct extension from adjacent focus (thrombophlebitis venous infarct) – Infected emboli (occlusion of a small artery or arteriole arterial infarct) • Necrosis leads to frank suppuration • After a week or two, a fibrous wall (derived from the vasculature) that may be several mm thick after 4 -5 weeks forms • Outside the fibrous wall, there are perivascular, chronic inflammatory cells and white matter edema (perifocal edema) • An intense astrocytic gliosis takes place with formation of a glial scar
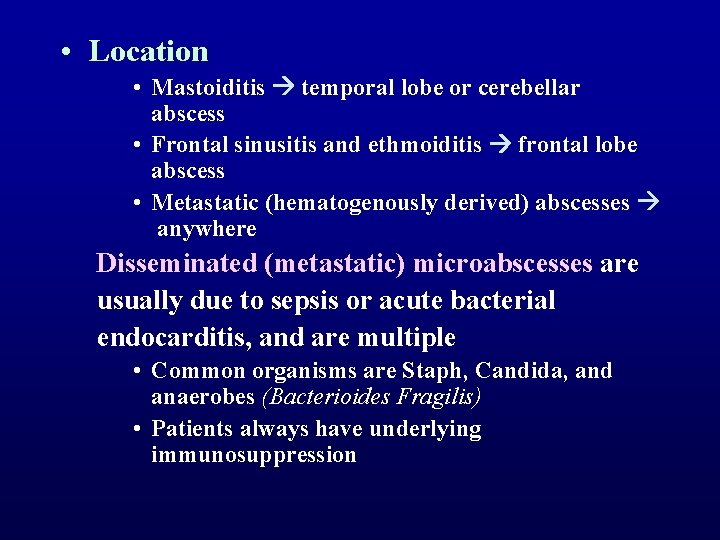
• Location • Mastoiditis temporal lobe or cerebellar abscess • Frontal sinusitis and ethmoiditis frontal lobe abscess • Metastatic (hematogenously derived) abscesses anywhere Disseminated (metastatic) microabscesses are usually due to sepsis or acute bacterial endocarditis, and are multiple • Common organisms are Staph, Candida, and anaerobes (Bacterioides Fragilis) • Patients always have underlying immunosuppression
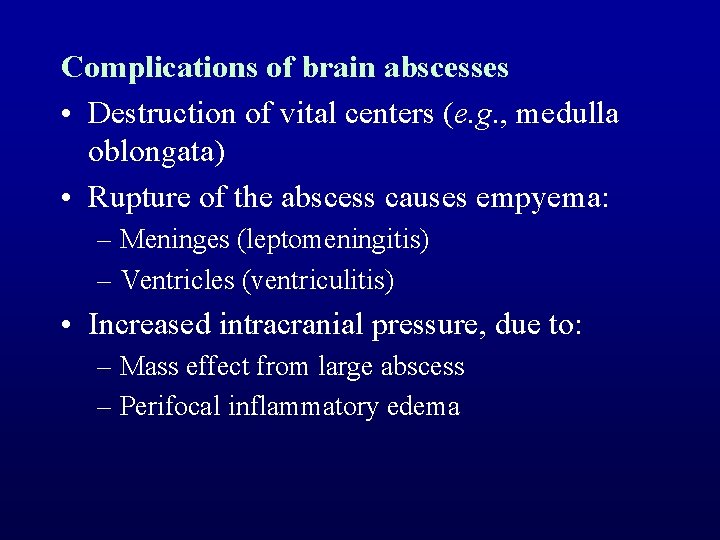
Complications of brain abscesses • Destruction of vital centers (e. g. , medulla oblongata) • Rupture of the abscess causes empyema: – Meninges (leptomeningitis) – Ventricles (ventriculitis) • Increased intracranial pressure, due to: – Mass effect from large abscess – Perifocal inflammatory edema
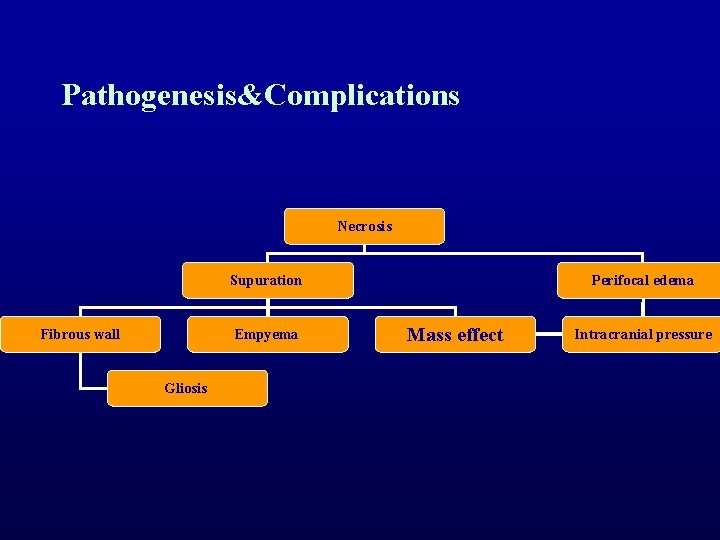
Pathogenesis&Complications Necrosis Supuration Fibrous wall Empyema Gliosis Perifocal edema Mass effect Intracranial pressure
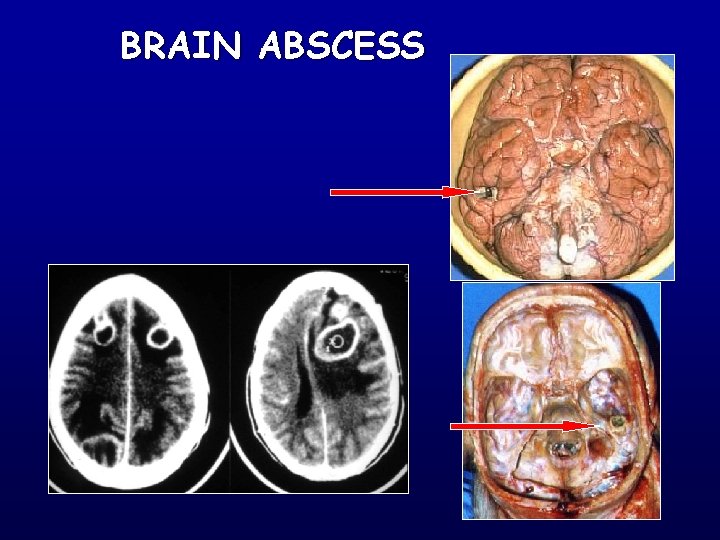
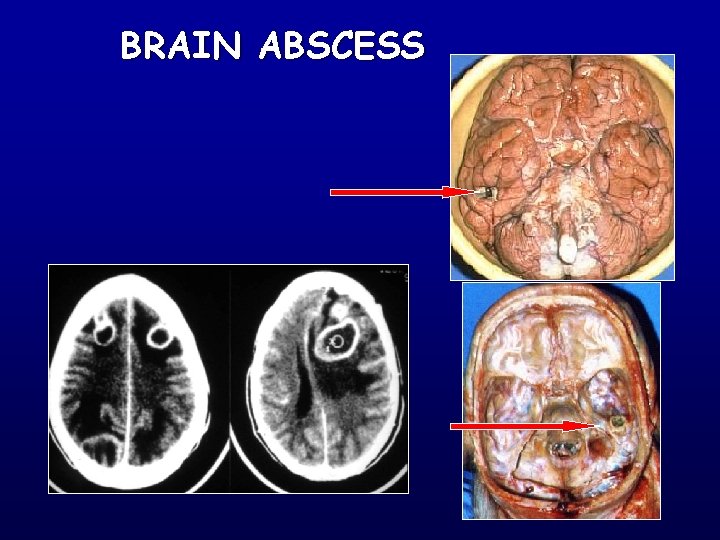
BRAIN ABSCESS
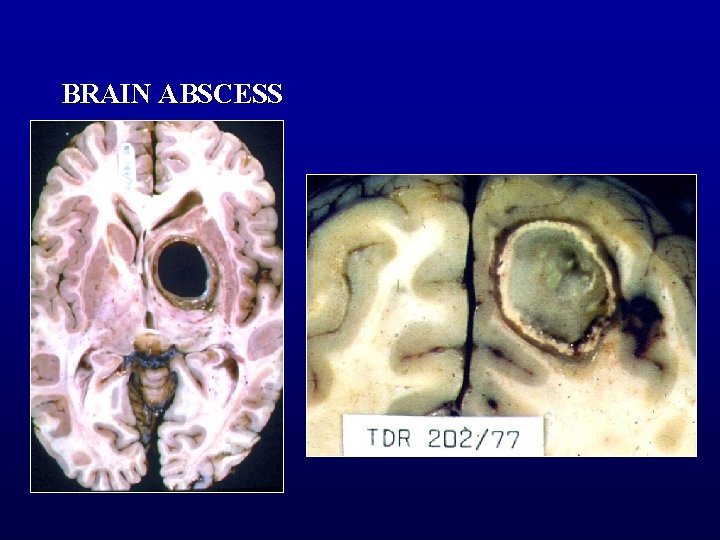
BRAIN ABSCESS




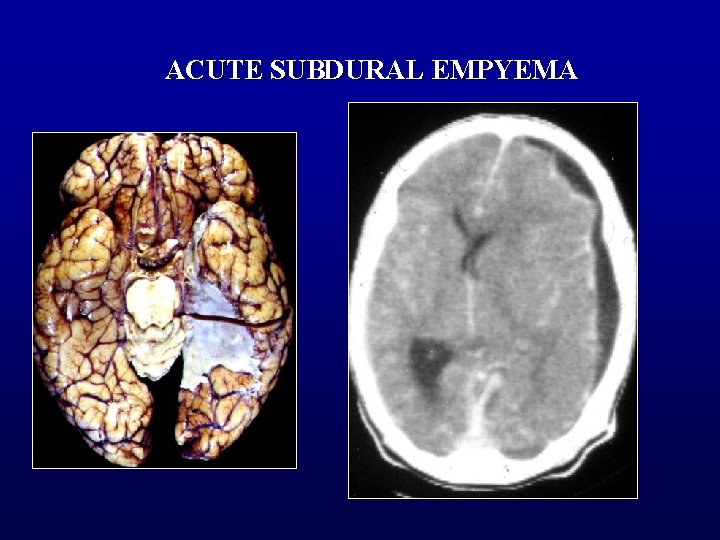
EPIDURAL & SUBDURAL EMPYEMA • A subdural empyema is usually secondary to sinus or middle ear infection • It is a neurosurgical emergency since antibiotics do not penetrate the subdural space, and surgical drainage of the pus is necessary • The CT scan is diagnostic • The adjacent cerebral hemisphere is usually swollen (perifocal edema)

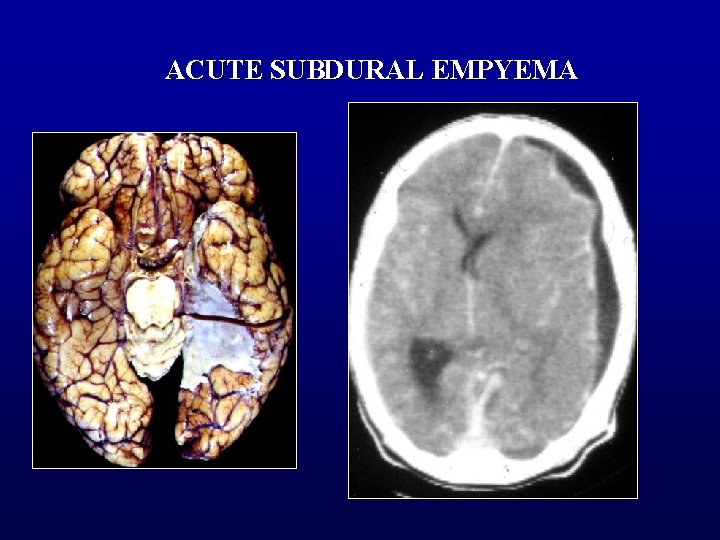
ACUTE SUBDURAL EMPYEMA
FUNGAL MENINGITIS • Cause a chronic meningitis, in some instances, granulomatous • Brain and cord may be involved • Most fungi produce infection of the CNS in either immunosuppressed or debilitated hosts

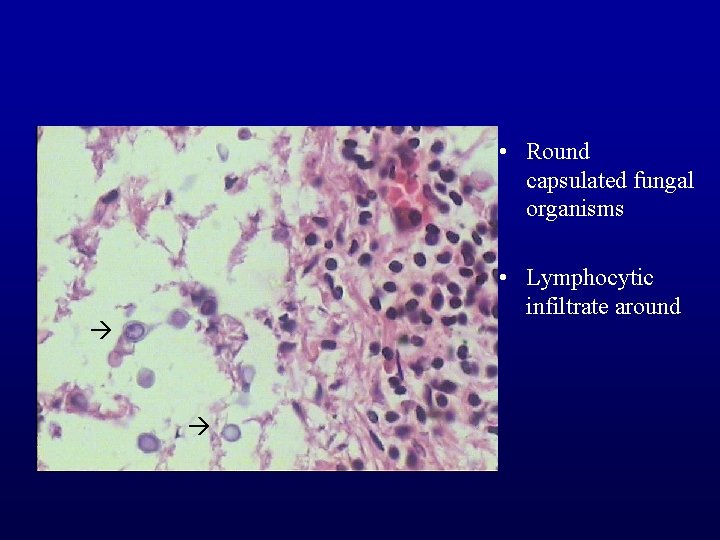
CRYPTOCOCCUS NEOFORMANS • • • Most common fungal infection Produces a chronic basilar meningitis Mononuclear inflammatory cells, foreign body giant cells, and the characteristic yeasts (mucicarmine- positive) are present within the subarachnoid and Virchow - Robin spaces – • Produce the characteristic "soap bubble" appearance India Ink stains of the CSF often demonstrate the encapsulated yeasts
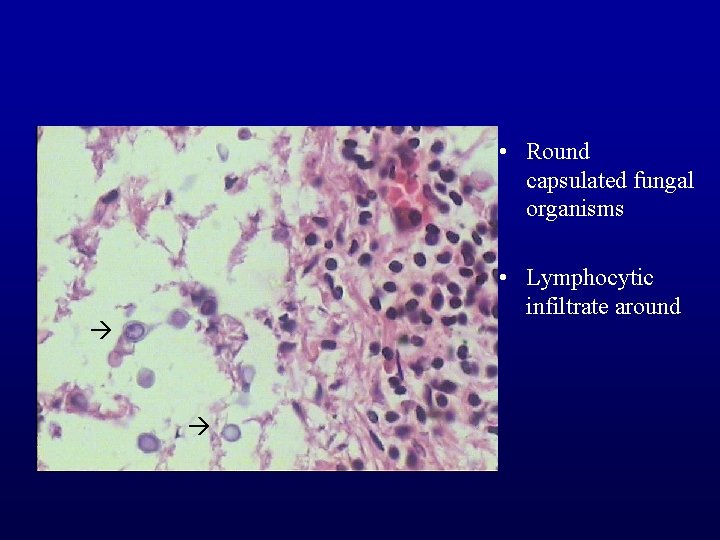
• Round capsulated fungal organisms • Lymphocytic infiltrate around

Aspergillus infection
MUCOR • Infects the sinuses of diabetic patients with ketoacidosis – • with direct invasion of the orbits and CNS (rhinocerebral mucormycosis) Mucor has a propensity for – – vascular invasion with secondary thrombosis hemorrhagic cerebral infarction

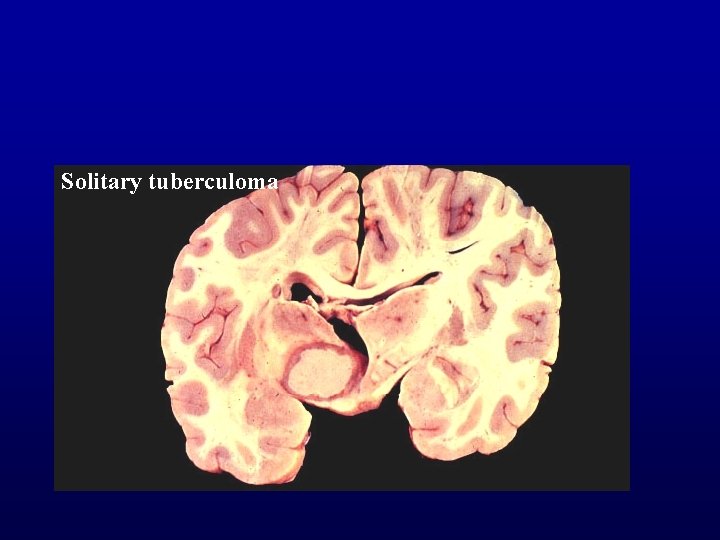
TUBERCULOSIS • Pathologic response is a typical granulomatous inflammatory response of tuberculosis • Four main CNS lesions: – Solitary tuberculoma: caseous encapsulated large mass – Multiple tuberculomas of brain and meninges • Miliary tuberculosis (children) • Microscopic or a few mm in size – Tuberculous meningitis: produces a chronic basilar meningitis – Spinal : extension from vertebrae (Pott’s disease)
TUBERCULOMA • • • A focal tuberculous infection Forming an expanding mass lesion Occur in brain, cord or meninges Simulates a neoplasm May require surgical removal
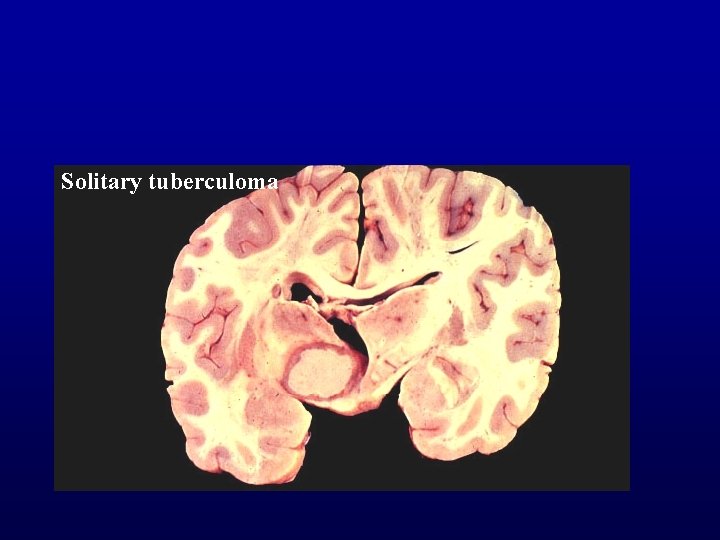
Solitary tuberculoma

TUBERCULOMA
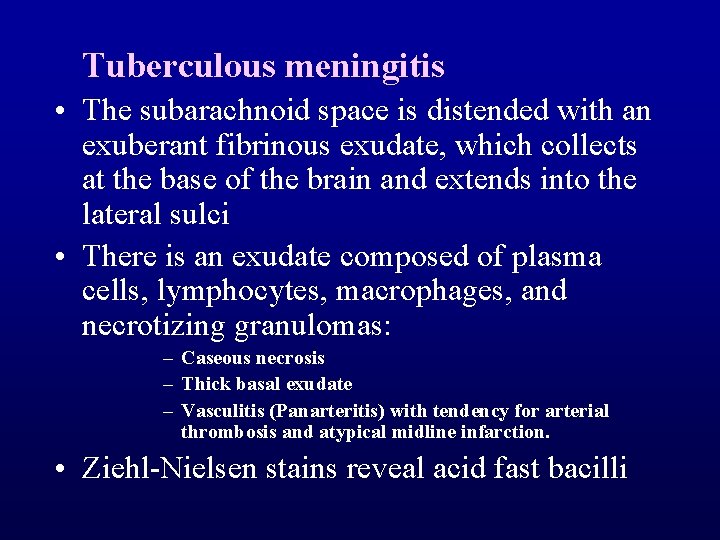
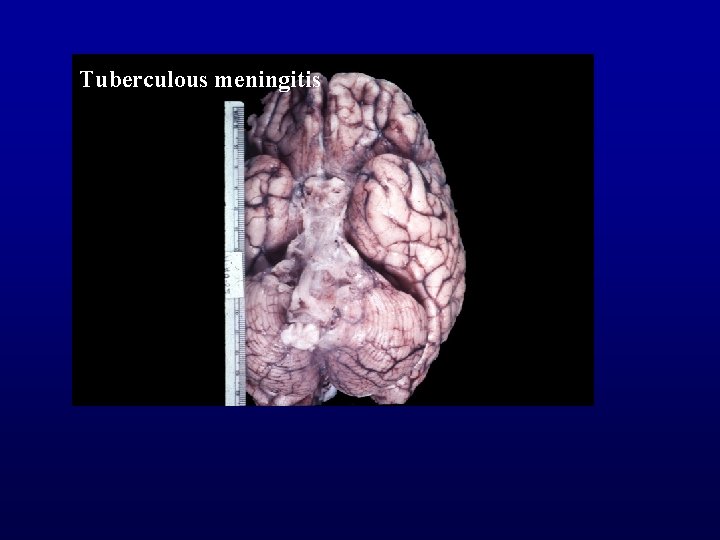
Tuberculous meningitis • The subarachnoid space is distended with an exuberant fibrinous exudate, which collects at the base of the brain and extends into the lateral sulci • There is an exudate composed of plasma cells, lymphocytes, macrophages, and necrotizing granulomas: – Caseous necrosis – Thick basal exudate – Vasculitis (Panarteritis) with tendency for arterial thrombosis and atypical midline infarction. • Ziehl-Nielsen stains reveal acid fast bacilli
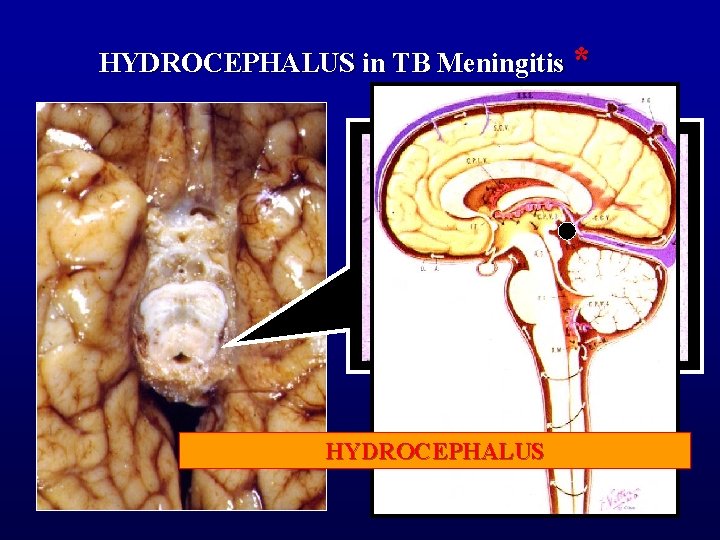
Complications • Organization (very common) – a resultant adhesive arachnoiditis often produces a communicating hydrocephalus • Obliterative arteritis in Subarachnoidal vessels – with secondary cerebral/spinal infarction • Entrapment of cranial nerves passing through the affected subarachnoid space – cranial nerve palsies • Tuberculoma (uncommon) – produces symptoms of a space-occupying lesion similiar to a brain tumor

TUBERCULOUS MENINGITIS CHRONIC COURSE THICK BASAL EXUDATE GRANULOMATOUS INFLAMMATION VASCULITIS CSF: -predominance of lymphocytes -high protein, -low sugar, -positive culture.
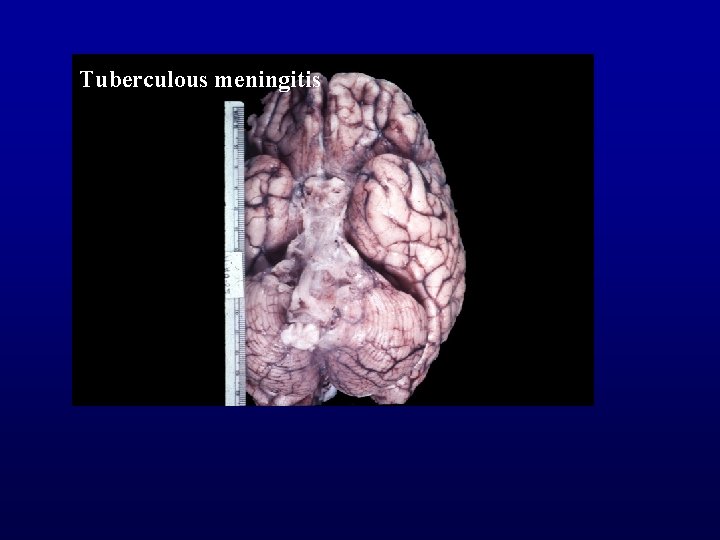
Tuberculous meningitis
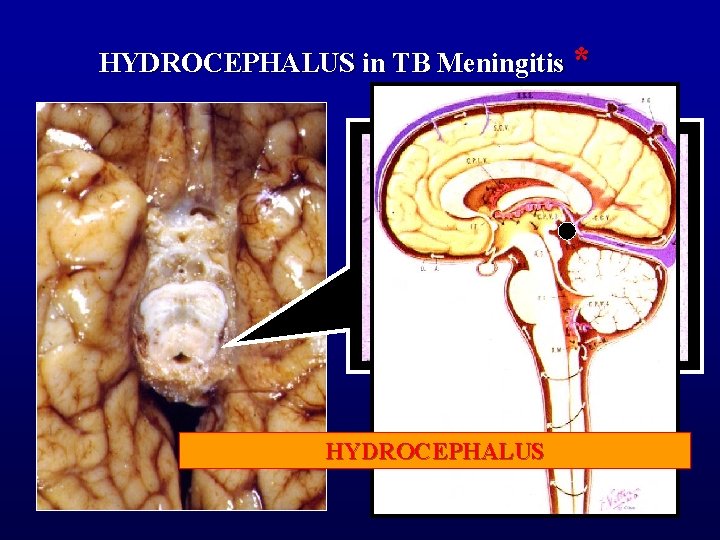
HYDROCEPHALUS in TB Meningitis * EXUDATE FILLING (BLOCKING) AMBIENT HYDROCEPHALUS CISTERN
*****NEUROSYPHILIS • The various forms of this entity are making a comeback in the age of AIDS • The initial infection is probably always meningeal • This may lead to: – – – Meningeal neurosyphilis Meningovascular neurosyphilis Tabetic neurosyphilis (tabes dorsalis) Neurosyphilitic optic atrophy Gummatous neurosyphilis Paretic neurosyphilis (general paresis)
• Meningeal neurosyphilis – A lymphocytic meningitis – May remain asymptomatic – May lead to arteritis or meningeal fibrosis with obstruction to flow of CSF
• Meningovascular neurosyphilis – Syphilitic endarteritis with thrombosis – Ischemic effects in brain and spinal cord
• Tabetic neurosyphilis (tabes dorsalis) – Infection extends around and probably into posterior roots of the spinal cord (reason for this selective involvement is not clear) with root inflammation and degeneration – Posterior column degeneration is secondary to the root involvement
• Neurosyphilitic optic atrophy – Extension of infection into optic nerve with secondary inflammation and degeneration • Gummatous neurosyphilis – Gumma
• Paretic neurosyphilis (general paresis) – Lymphocytic meningeal and perivascular inflammation – cortical nerve cell degeneration – small infarcts – astrocyte proliferation – microglial activation with production of elongated rod forms

PARASITE INFECTIONS • Protozoal eg. malaria, toxoplasmosis, trypanosomiasis, amoebic • Metazoal eg. cysticercosis, hydatid cyst • Transmissible agent (prion) diseases (not infection)
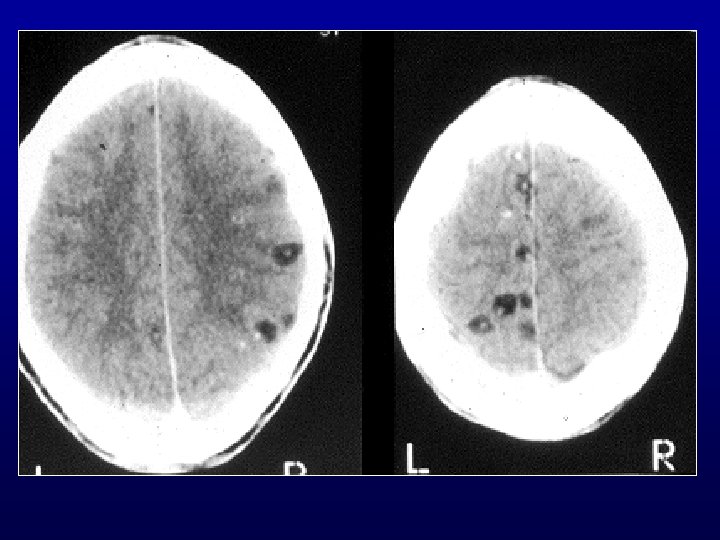
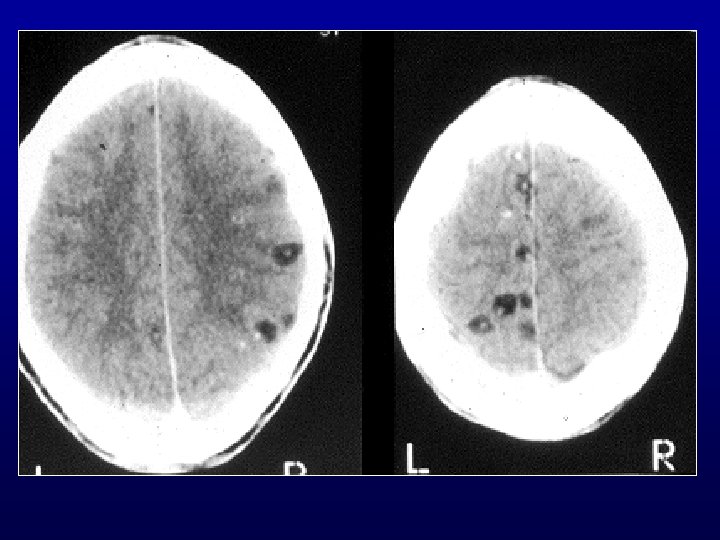
• NEUROCYSTICERCOSIS – Basal granulomatous meningitis – Meningeal, parenchymal, ventricular cysts – Parenchymal granulomas/abscesses – Mineralised (calcium) nodules Taenia solium - pork tape worm
• Cysticercosis important in some parts of the world – Subarachnoid space (producing meningitis) – Ventricular system (producing hydrocephalus) – Brain parenchyme (producing focal lesions)
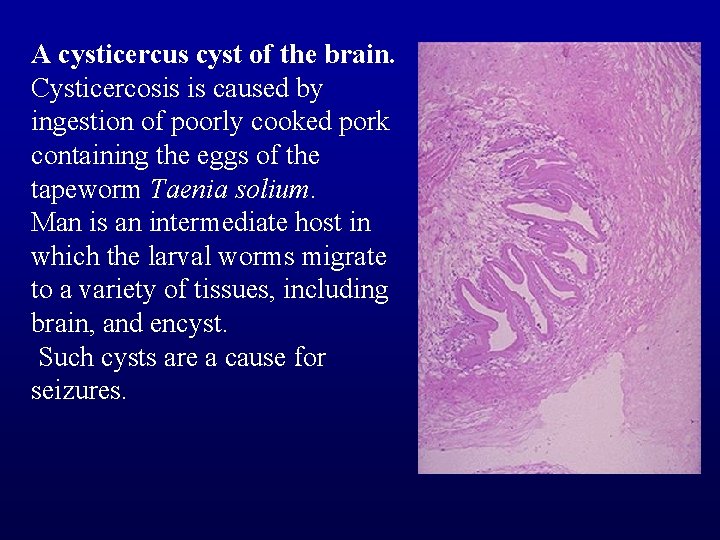
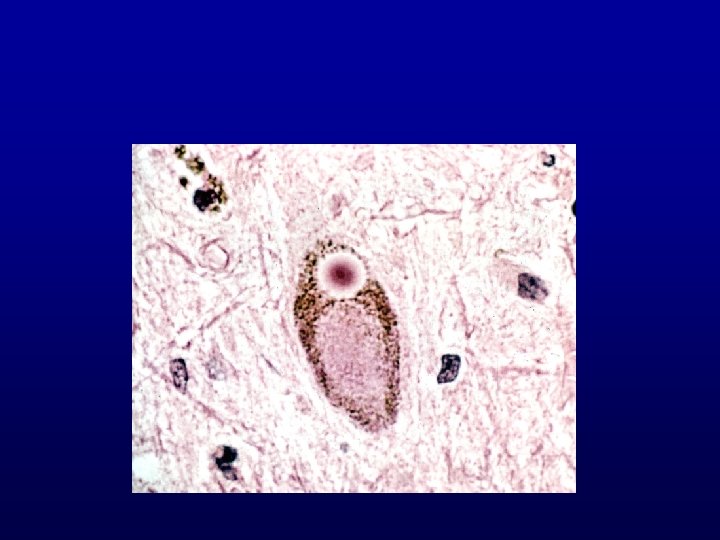
Encysted metacestode
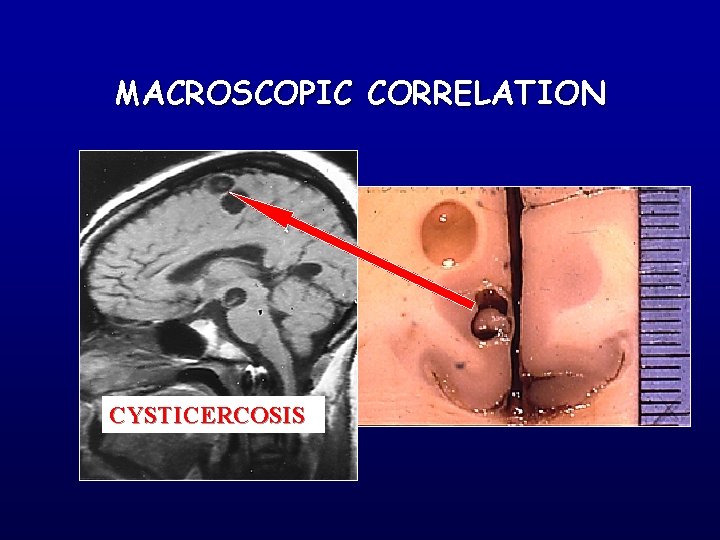
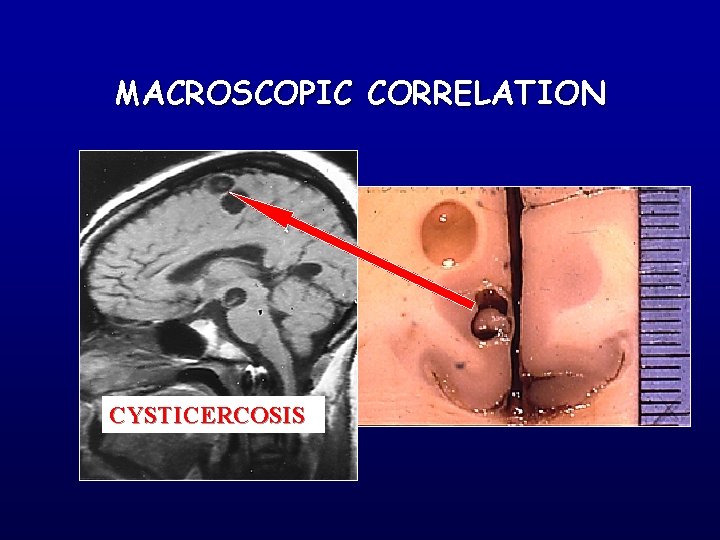
MACROSCOPIC CORRELATION CYSTICERCOSIS
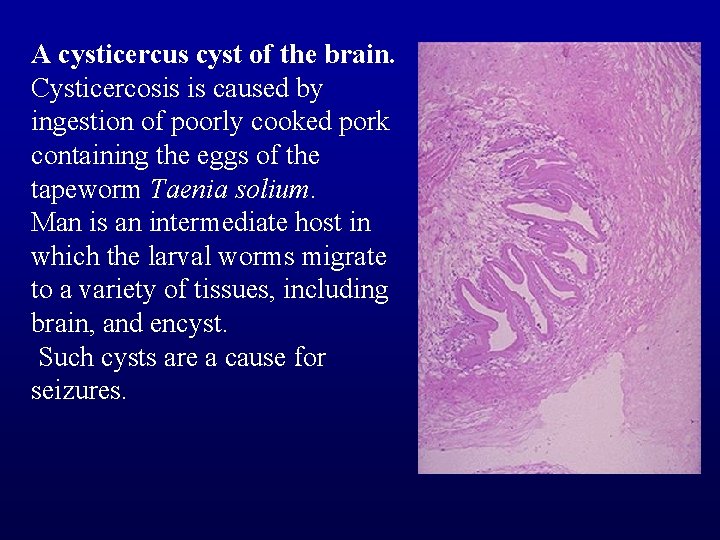
A cysticercus cyst of the brain. Cysticercosis is caused by ingestion of poorly cooked pork containing the eggs of the tapeworm Taenia solium. Man is an intermediate host in which the larval worms migrate to a variety of tissues, including brain, and encyst. Such cysts are a cause for seizures.

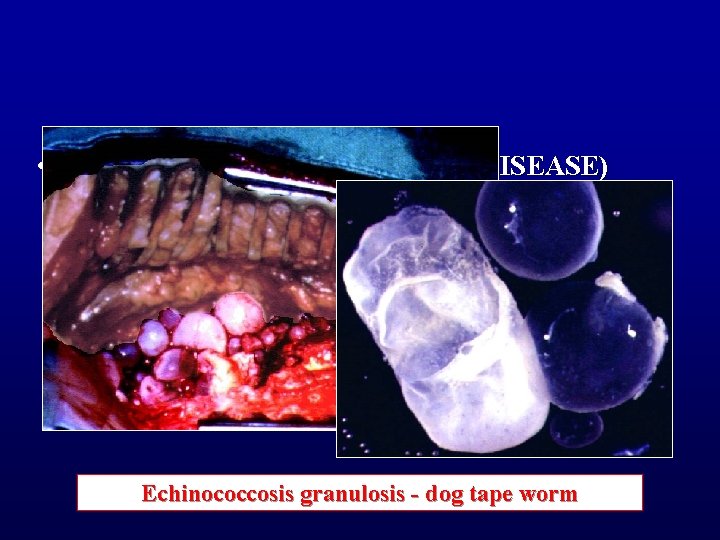
• ECHINOCOCCOSIS (HYDATID DISEASE) Echinococcosis granulosis - dog tape worm
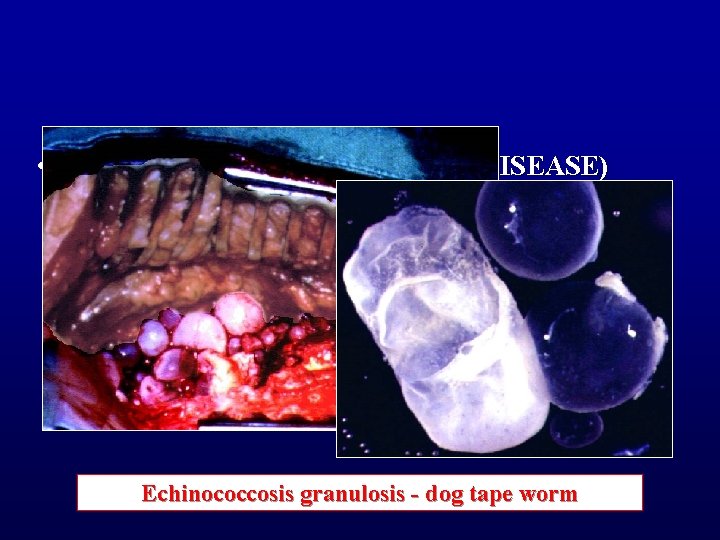
• ECHINOCOCCOSIS (HYDATID DISEASE) Echinococcosis granulosis - dog tape worm
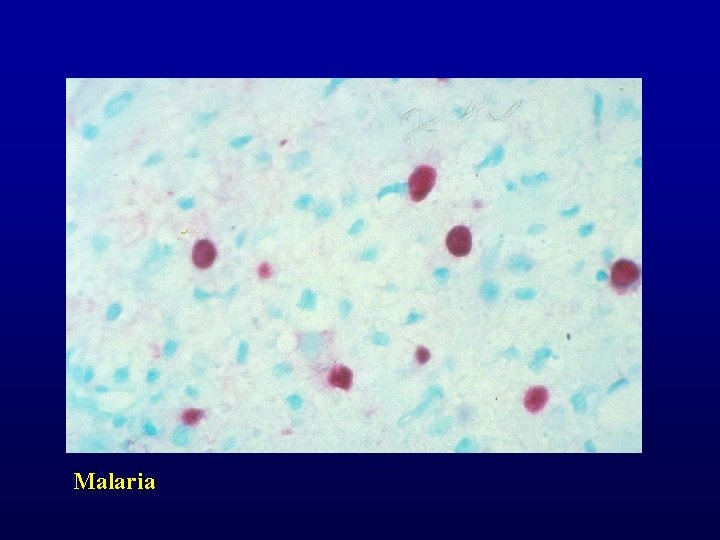
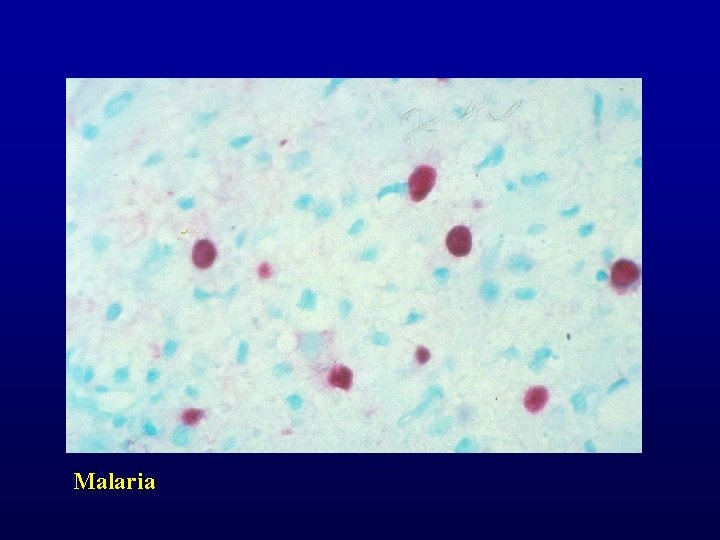
Malaria
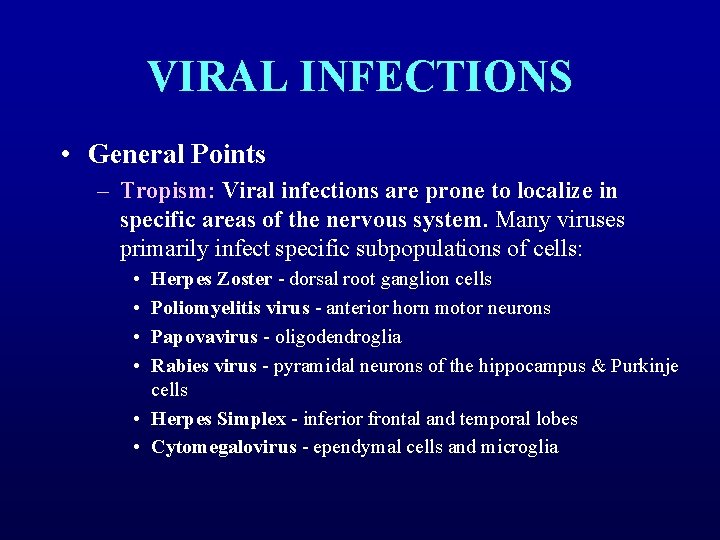
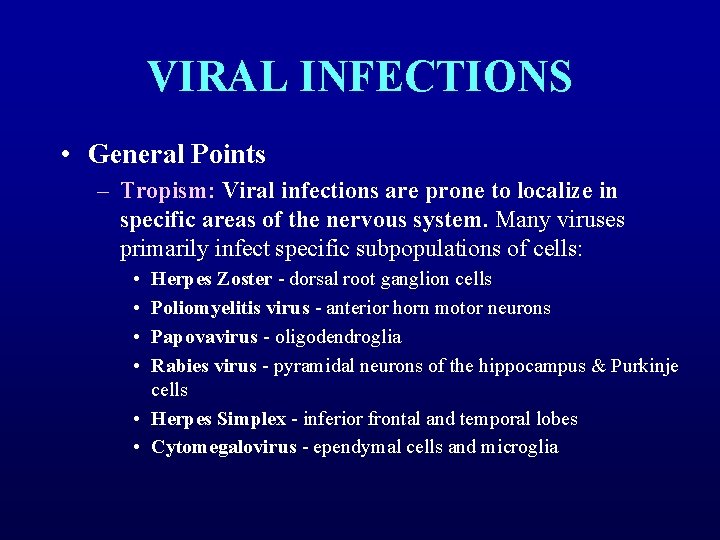
VIRAL INFECTIONS • General Points – Tropism: Viral infections are prone to localize in specific areas of the nervous system. Many viruses primarily infect specific subpopulations of cells: • • Herpes Zoster - dorsal root ganglion cells Poliomyelitis virus - anterior horn motor neurons Papovavirus - oligodendroglia Rabies virus - pyramidal neurons of the hippocampus & Purkinje cells • Herpes Simplex - inferior frontal and temporal lobes • Cytomegalovirus - ependymal cells and microglia

– Virus must be inoculated into host – Latency • Herpes Simplex and Varicella-Zoster remain latent in host neurons, only to be reactivated months or years after the initial infection – Routes of spread to the CNS: • • • Neural Olfactory Hematogenous (most viruses)

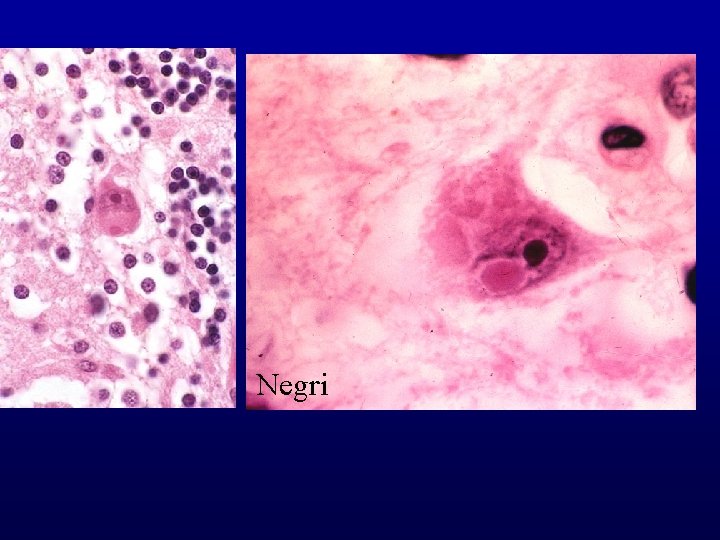
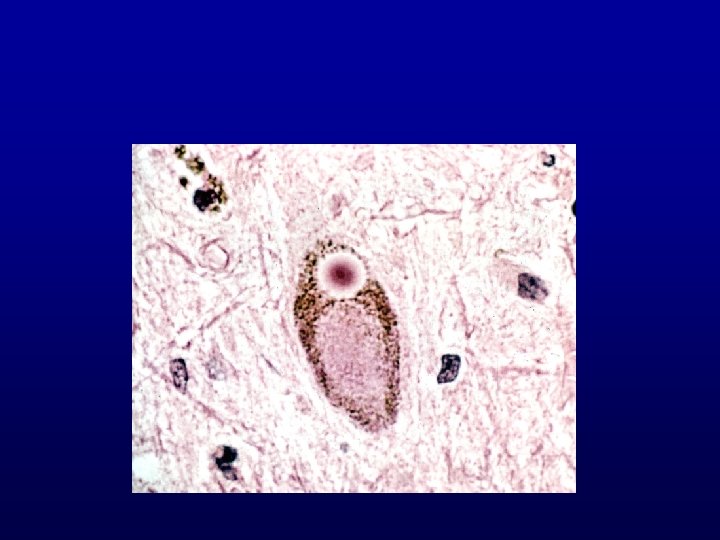
Pathologic Characteristics of Viral Encephalitis – Parenchymal and perivascular mononuclear cell infiltrates • • lymphocytes, plasma cells, and macrophages mononuclear cells in the CSF – Microglial nodules which form around degenerate/necrotic neurons (neuronophagia) • many microglia have elongated nuclei (rod cells) – Inclusion Bodies: • • Nuclear Inclusions: H. simplex, Varicella-Zoster, Cytomegalovirus, Subacute Sclerosing Panencephalitis Cytoplasmic Inclusions: Negri body (rabies)
• Viral infections of the CNS: Sites of predilection –Arbovirus: Pan-encephalitis –Rabies: Hypothalamus, cranial nerves –Polio: Motor system –von Economo’s disease (postencephalitic parkinsonism): Midbrain –Herpes simplex: Medial temporal lobe
Nomenclature – (a) only in the meninges - viral meningitis – (b) largely in the brain - viral encephalitis – (c) largely in the spinal cord - myelitis
Common lesions 1. Immunoallergic reactions perivenous demyelination 2. Actual invasion by virus meningitis, encephalitis, myelitis 3. Persistent (slow viral) infections “degeneration” of neurons/myelin
Acute Viral Infections • The best known of these is that caused by the poliovirus. • This virus selectively attacks neurones (ie. neurotropic) of the – anterior horns (especially) – brain stem motor nuclei – motor cortex The loss of the nerve cells Wallerian degeneration of axons neurogenic atrophy of muscles

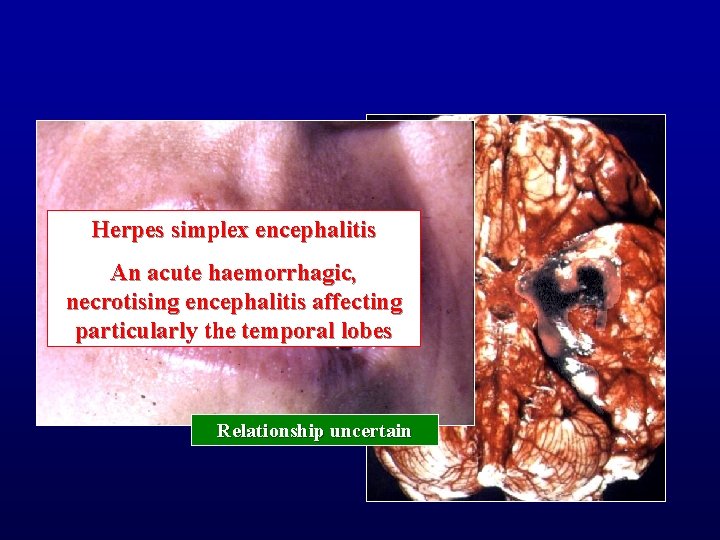
Other acute viral encephalitides include: – 1. Rabies - the virus enters via peripheral nerves; identified by presence of diagnostic intracytoplasmic inclusions in pyramidal neurones (Negri bodies) – 2. Herpes simplex (type I) encephalitis - this virus has a propensity to attack several organs and is unselective in its effect on nervous tissue (pantropic reaction) • acute necrotising encephalitis (affecting particularly the temporal lobes) • severe cerebral edema and swelling • death is caused by brain shift
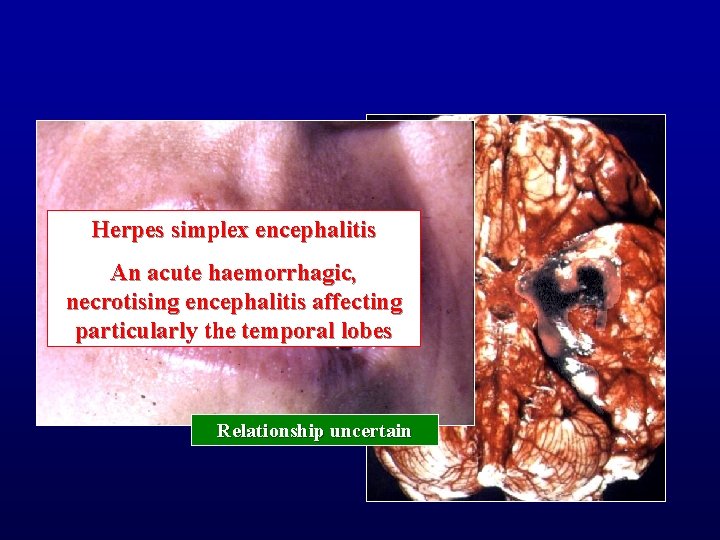
Herpes simplex encephalitis An acute haemorrhagic, necrotising encephalitis affecting particularly the temporal lobes Relationship uncertain
• The pathology of acute viral infections: – Acute degeneration of nerve cell – Microglial activation forming microglial nodules at sites of degenerating neurons – Perivascular lymphocytic infiltrates – Astrocytic proliferation – Intracytoplasmic or intranuclear inclusions may be characteristic • Cowdry type A inclusion in herpes simplex type I • the Negri body of rabies


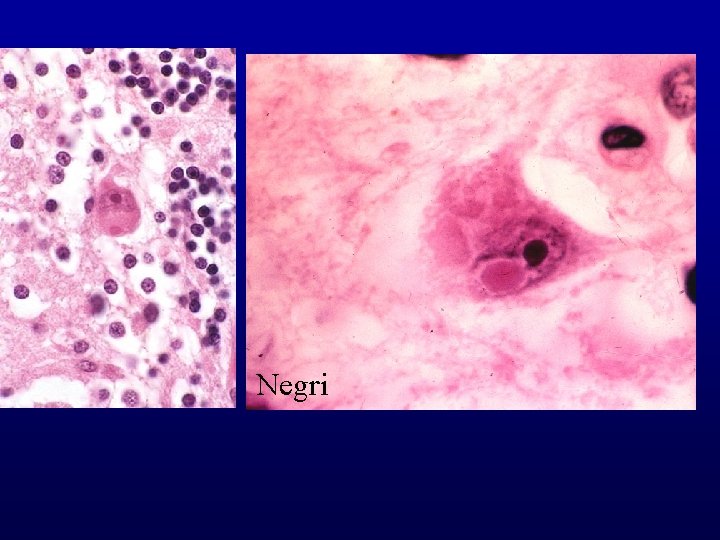
Negri
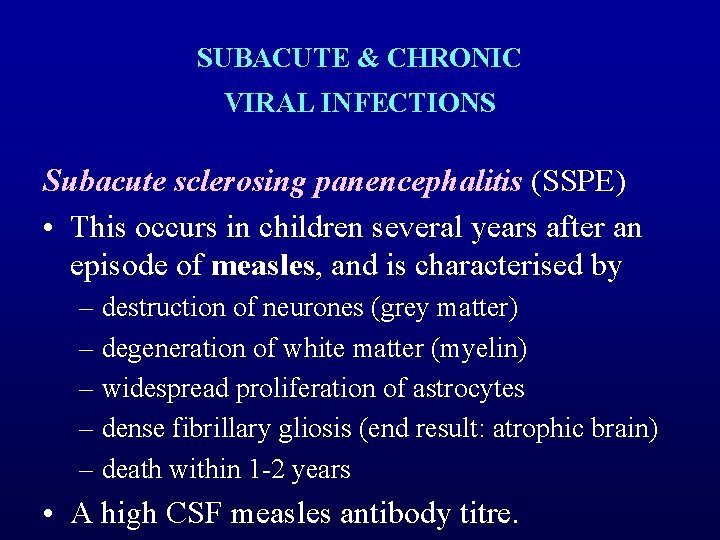
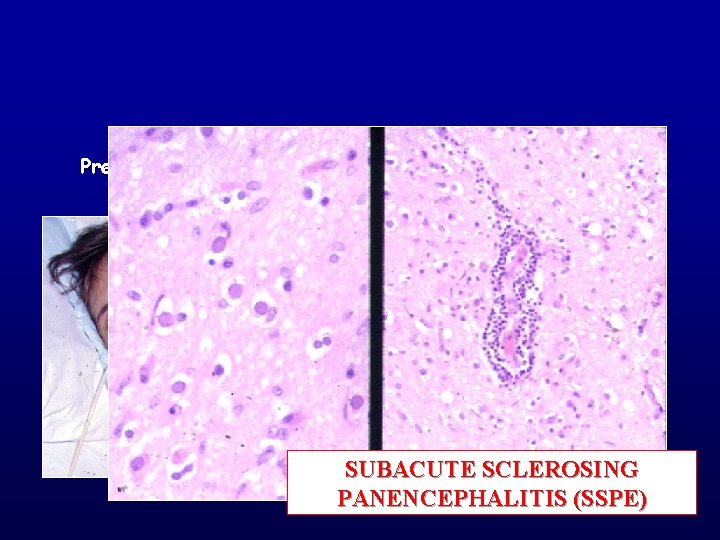
SUBACUTE & CHRONIC VIRAL INFECTIONS Subacute sclerosing panencephalitis (SSPE) • This occurs in children several years after an episode of measles, and is characterised by – destruction of neurones (grey matter) – degeneration of white matter (myelin) – widespread proliferation of astrocytes – dense fibrillary gliosis (end result: atrophic brain) – death within 1 -2 years • A high CSF measles antibody titre.
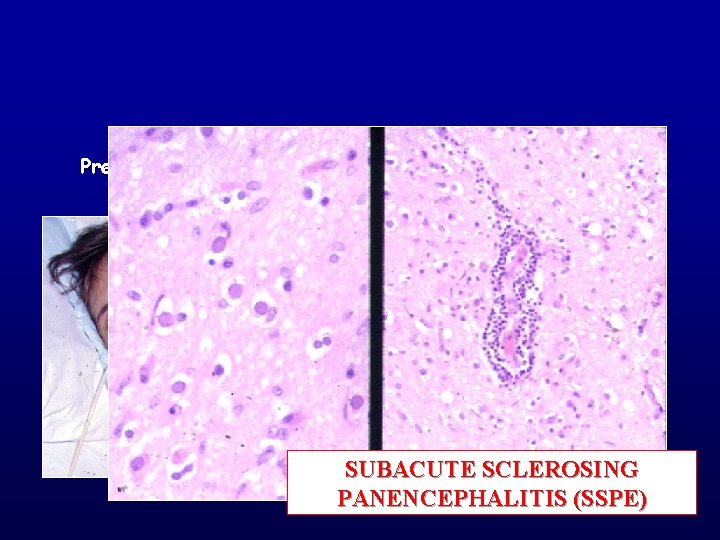
Previous measles infection SUBACUTE SCLEROSING PANENCEPHALITIS (SSPE)

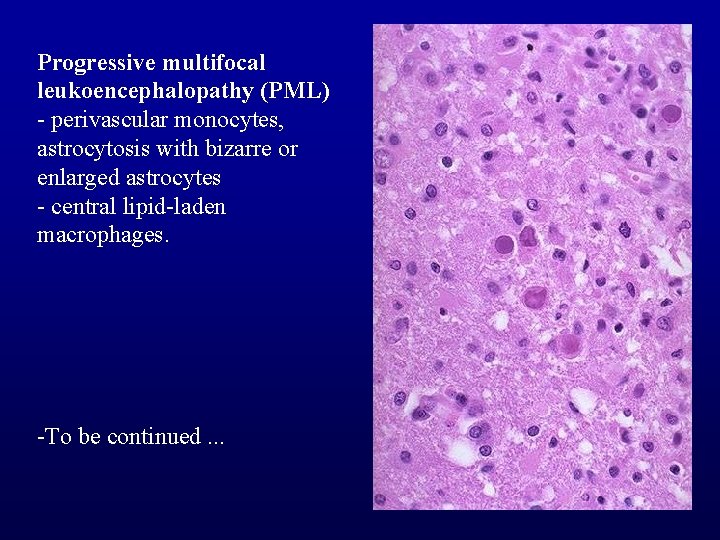
Progressive multifocal leukoencephalopathy • A Papovavirus infection of oligodendroglial cells. – The virus destroys oligodendroglial cells with focal demyelination • It is associated with immunosuppressed hosts – Hodgkin's disease – AIDS • There are multiple poorly demarcated areas of demyelination present within the cerebral, cerebellar, and spinal white matter.

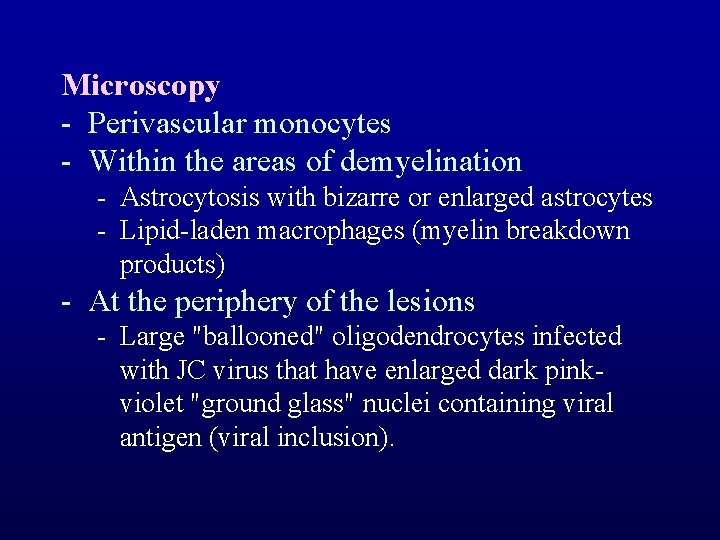
Microscopy - Perivascular monocytes - Within the areas of demyelination - Astrocytosis with bizarre or enlarged astrocytes - Lipid-laden macrophages (myelin breakdown products) - At the periphery of the lesions - Large "ballooned" oligodendrocytes infected with JC virus that have enlarged dark pinkviolet "ground glass" nuclei containing viral antigen (viral inclusion).
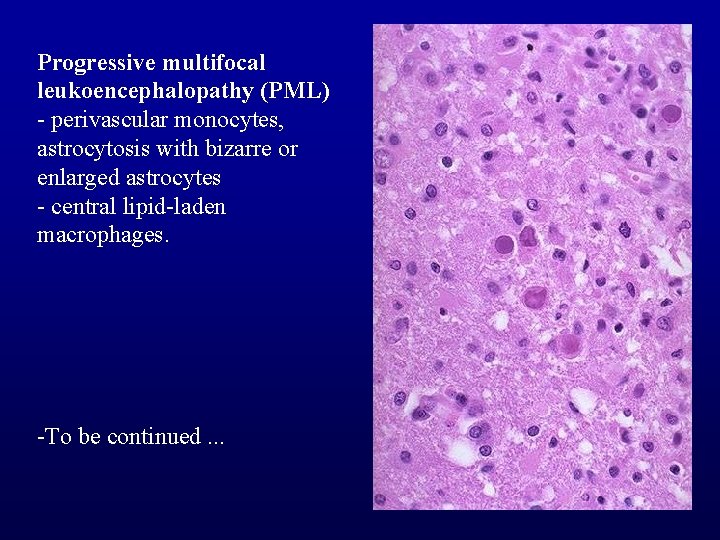
Progressive multifocal leukoencephalopathy (PML) - perivascular monocytes, astrocytosis with bizarre or enlarged astrocytes - central lipid-laden macrophages. -To be continued. . .
HUMAN IMMUNODEFICIENCY VIRUS
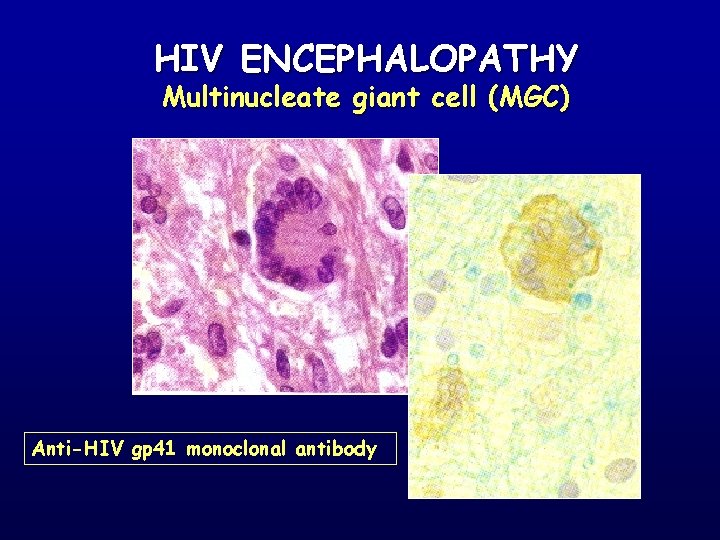
HUMAN IMMUNODEFICIENCY VIRUS • An acute encephalopathy is one of the commonest findings in AIDS patients. • This has been attributed to the affects of the virus, which is present mainly in macrophages, or multi-nucleated giant cells (MCG's) derived from them – MCG's are regarded as the hallmark of HIV productive infection of the brain.
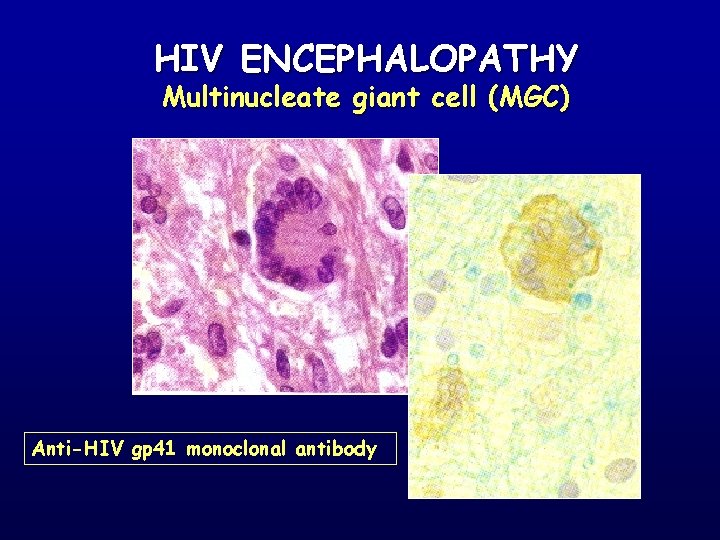
HIV ENCEPHALOPATHY Multinucleate giant cell (MGC) Anti-HIV gp 41 monoclonal antibody

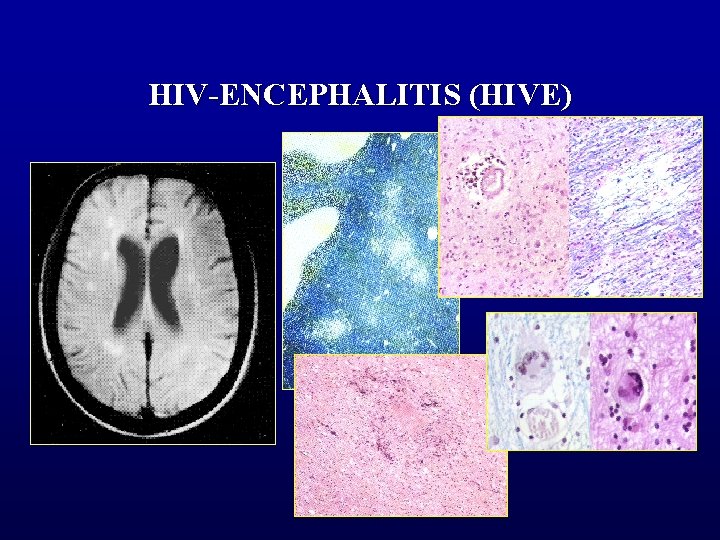
– Damage to CNS tissues: • • neuronotoxicity of HIV proteins various factors (cytokines) secreted from infected cells – Pathologically two major patterns of HIV-specific damage occur: 1. Multifocal & inflammatory: HIV encephalitis (HIVE) 2. Diffuse and degenerative: HIV leucoencephalopathy (HIVL)
• HIVE is characterised by multiple microgranulomatous foci, preferentially involving white matter, basal ganglia and brainstem.
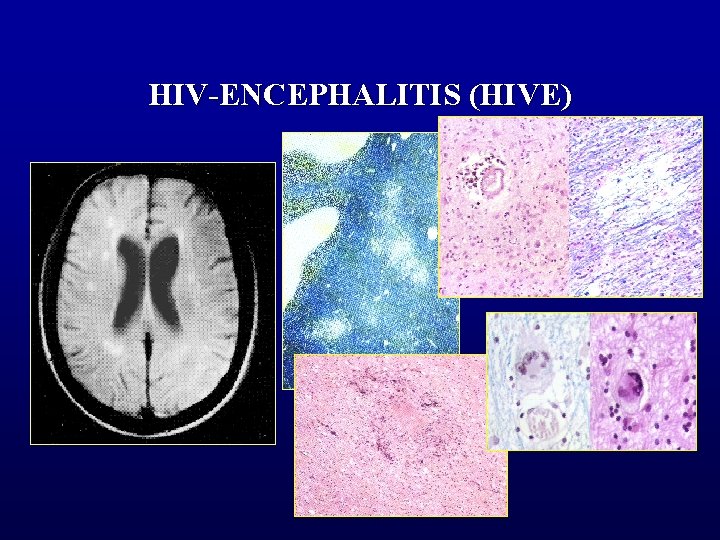
HIV-ENCEPHALITIS (HIVE)
• In HIVL – a diffuse or focal loss (breakdown) of myelin – reactive astrogliosis – macrophages – MCG's

• HIVE and HIVL consistently harbour large amounts of HIV antigen, as detected immunocytochemically or by in situ hybridisation.
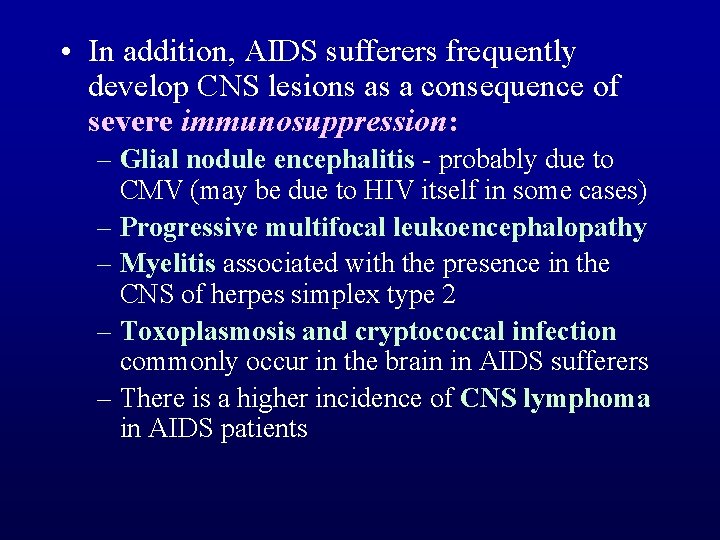
• In addition, AIDS sufferers frequently develop CNS lesions as a consequence of severe immunosuppression: – Glial nodule encephalitis - probably due to CMV (may be due to HIV itself in some cases) – Progressive multifocal leukoencephalopathy – Myelitis associated with the presence in the CNS of herpes simplex type 2 – Toxoplasmosis and cryptococcal infection commonly occur in the brain in AIDS sufferers – There is a higher incidence of CNS lymphoma in AIDS patients
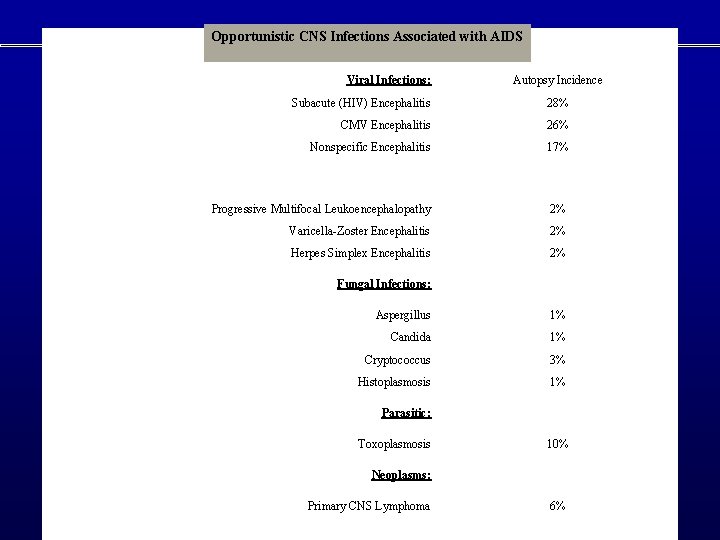
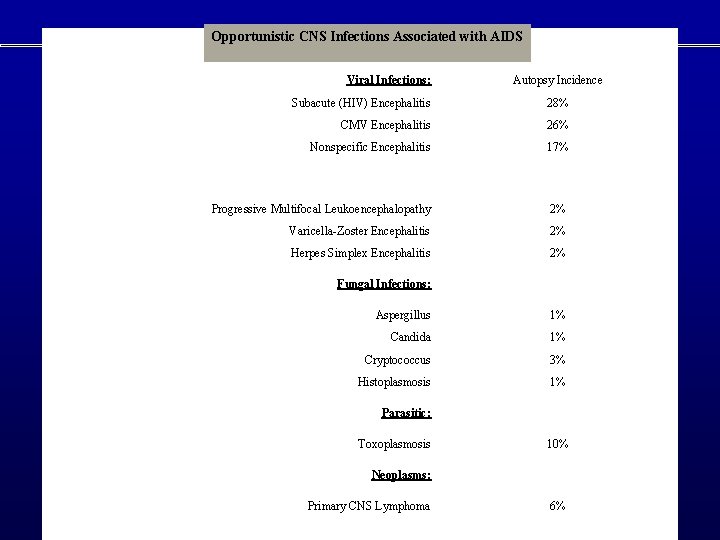
Opportunistic CNS Infections Associated with AIDS Viral Infections: Autopsy Incidence Subacute (HIV) Encephalitis 28% CMV Encephalitis 26% Nonspecific Encephalitis 17% Progressive Multifocal Leukoencephalopathy 2% Varicella-Zoster Encephalitis 2% Herpes Simplex Encephalitis 2% Fungal Infections: Aspergillus 1% Candida 1% Cryptococcus 3% Histoplasmosis 1% Parasitic: Toxoplasmosis 10% Neoplasms: Primary CNS Lymphoma 6%
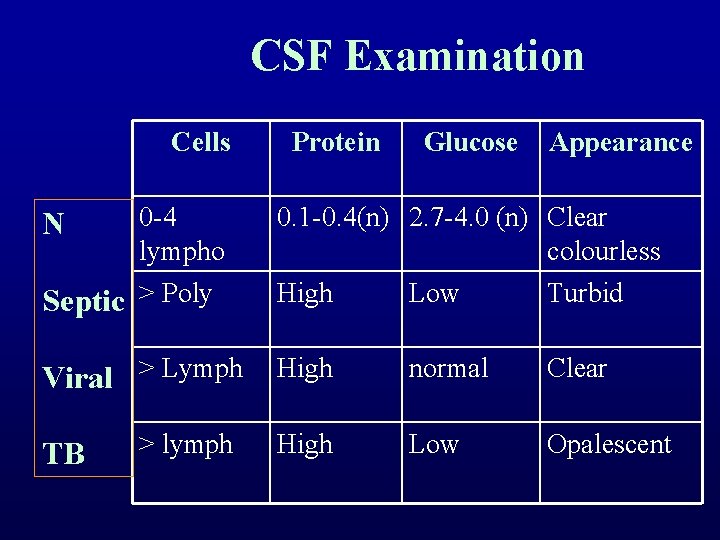
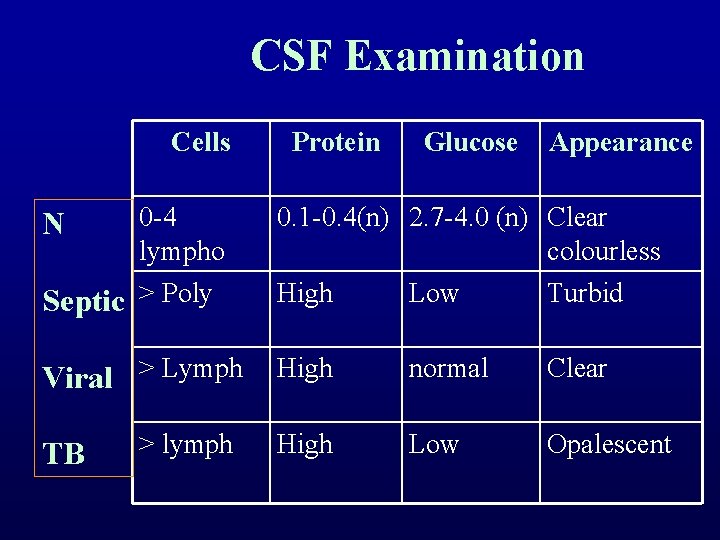
CSF Examination Cells N 0 -4 lympho Protein Glucose Appearance 0. 1 -0. 4(n) 2. 7 -4. 0 (n) Clear colourless Septic > Poly High Low Turbid Viral > Lymph High normal Clear High Low Opalescent TB > lymph
CNS Pathology Inflammatory and Infectious Disorders • Late effects on CNS – Organizing exudate hydrocephalus – Vascular occlusions infarcts
 Coagulation casecade
Coagulation casecade Pro and anti inflammatory
Pro and anti inflammatory Desquamative inflammatory vaginitis
Desquamative inflammatory vaginitis Humira vs remicade
Humira vs remicade Abcsses
Abcsses Inflammatory breast cancer
Inflammatory breast cancer Treatment of inflammatory breast cancer
Treatment of inflammatory breast cancer Post inflammatory erythema
Post inflammatory erythema Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Dr adria rusli
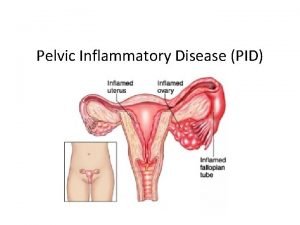
Dr adria rusli Pelvic inflammatory disease men
Pelvic inflammatory disease men Pelvic girdle pain
Pelvic girdle pain Inflammatory cells
Inflammatory cells Types of colitis
Types of colitis Bệnh gì
Bệnh gì Ans and cns difference
Ans and cns difference Cns and sns
Cns and sns Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Hpps symbol
Hpps symbol C=0 sampling plan
C=0 sampling plan Naas community national school
Naas community national school Haemorrhage
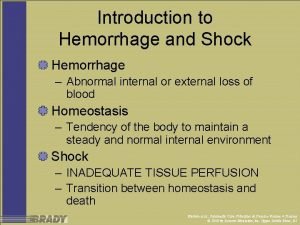
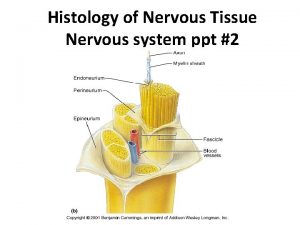
Haemorrhage Cns histology ppt
Cns histology ppt Composition of cns
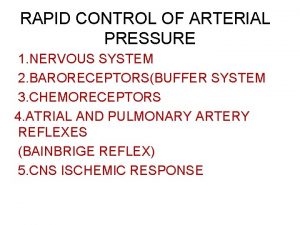
Composition of cns Cns ischemic response
Cns ischemic response Mean bp formula
Mean bp formula Bainbridge reflex
Bainbridge reflex Www.lispa.it cns
Www.lispa.it cns Cns depressants ppt
Cns depressants ppt Tuberculomas
Tuberculomas Depresori cns
Depresori cns Cns international school
Cns international school Cns poruchy
Cns poruchy Muscle power grading scale
Muscle power grading scale Fhbdf
Fhbdf Mesencephalon
Mesencephalon Cns ward
Cns ward Cns
Cns Label the parts of the central nervous system
Label the parts of the central nervous system Cns
Cns Cns classification
Cns classification Soma cns
Soma cns Perineurium
Perineurium Classification of cholinergic drugs
Classification of cholinergic drugs Cns educar
Cns educar Soma cns
Soma cns Cns
Cns Cns-cp
Cns-cp Reeling gait
Reeling gait Depresori cns
Depresori cns Cns15506
Cns15506 Mebosha
Mebosha Infectious disease quality controls
Infectious disease quality controls Stages of infection
Stages of infection Stages of infectious disease
Stages of infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Stridor
Stridor What is the smallest infectious agent
What is the smallest infectious agent Papillomitosis
Papillomitosis Infectious nucleic acid
Infectious nucleic acid Lead poisoning
Lead poisoning Infectious disease
Infectious disease Infectious mononucleosis
Infectious mononucleosis Hennepin county infectious disease manual
Hennepin county infectious disease manual Epidemiological triad
Epidemiological triad Quizlet
Quizlet Infectious stunting syndrome
Infectious stunting syndrome Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 16 infection prevention and control
Chapter 16 infection prevention and control Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Most quats solutions disinfect implements in
Most quats solutions disinfect implements in Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Cbic recertification
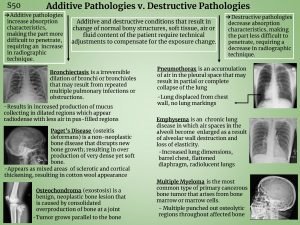
Cbic recertification Pneumothorax additive or destructive
Pneumothorax additive or destructive Introduction to cryptology
Introduction to cryptology Cryptology and pathology
Cryptology and pathology Cryptology and pathology
Cryptology and pathology Systemic pathology questions and answers pdf
Systemic pathology questions and answers pdf Introduction and importance of seed pathology
Introduction and importance of seed pathology Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Albugo eye
Albugo eye Pathology of blood and urine ppt
Pathology of blood and urine ppt Fish and shellfish pathology
Fish and shellfish pathology Leeds pathology tests and tubes
Leeds pathology tests and tubes Unit 14 physiological disorders examples
Unit 14 physiological disorders examples Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Assistive technology for emotional disturbance
Assistive technology for emotional disturbance Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Neurotic stress related and somatoform disorders
Neurotic stress related and somatoform disorders Retention hyperkeratosis dermnet
Retention hyperkeratosis dermnet Physical disorders and health psychology
Physical disorders and health psychology Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Types of somatic disorder
Types of somatic disorder Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Personality disorder vs mental illness
Personality disorder vs mental illness Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders