CNS LUPUS H Michael Belmont M D Director
CNS LUPUS H. Michael Belmont, M. D. Director, Lupus Clinic Bellevue Hospital Chief Medical Officer Hospital for Joint Diseases Associate Professor of Medicine New York University School of Medicine
OUTLINE PATHOLOGY ETIOLOGY IMAGING and DIAGNOSTIC TESTING CLINICAL SYNDROMES TREATMENT
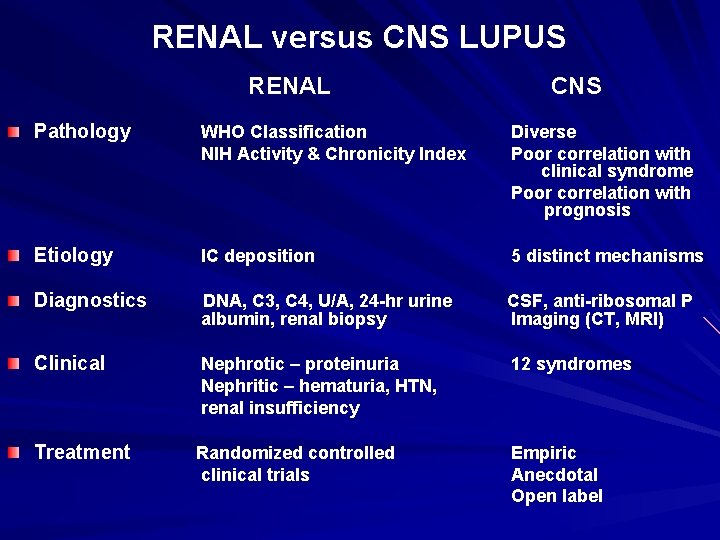
RENAL versus CNS LUPUS RENAL CNS Pathology WHO Classification NIH Activity & Chronicity Index Diverse Poor correlation with clinical syndrome Poor correlation with prognosis Etiology IC deposition 5 distinct mechanisms Diagnostics DNA, C 3, C 4, U/A, 24 -hr urine albumin, renal biopsy CSF, anti-ribosomal P Imaging (CT, MRI) Clinical Nephrotic – proteinuria Nephritic – hematuria, HTN, renal insufficiency 12 syndromes Treatment Randomized controlled clinical trials Empiric Anecdotal Open label
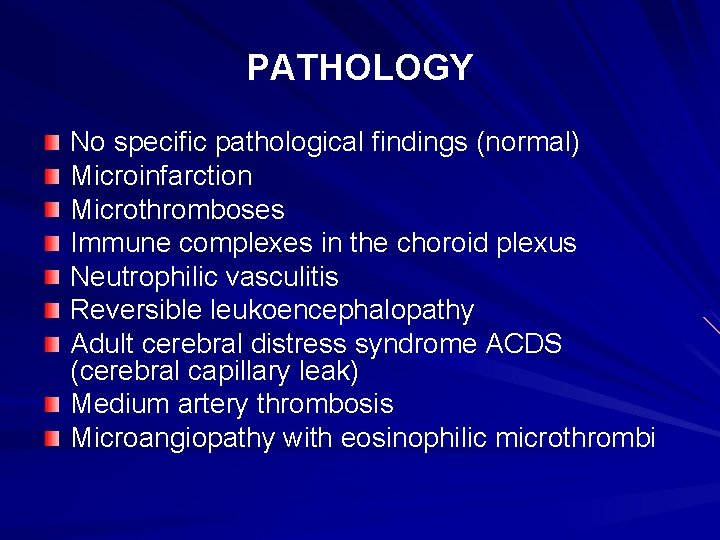
PATHOLOGY No specific pathological findings (normal) Microinfarction Microthromboses Immune complexes in the choroid plexus Neutrophilic vasculitis Reversible leukoencephalopathy Adult cerebral distress syndrome ACDS (cerebral capillary leak) Medium artery thrombosis Microangiopathy with eosinophilic microthrombi
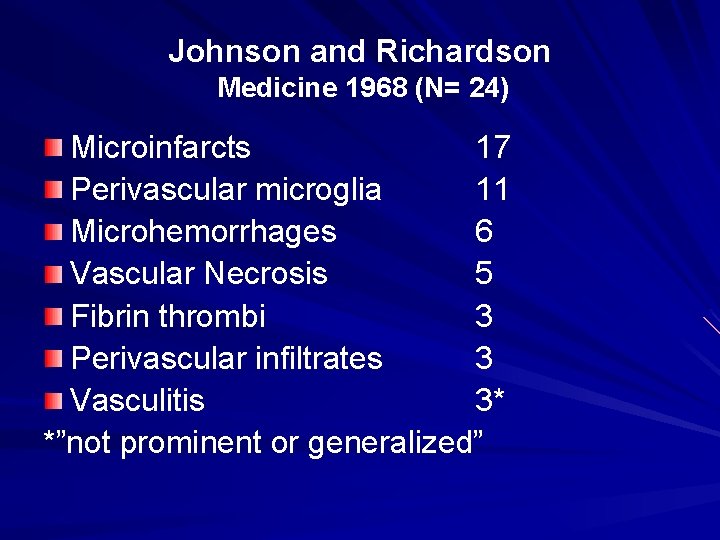
Johnson and Richardson Medicine 1968 (N= 24) Microinfarcts 17 Perivascular microglia 11 Microhemorrhages 6 Vascular Necrosis 5 Fibrin thrombi 3 Perivascular infiltrates 3 Vasculitis 3* *”not prominent or generalized”
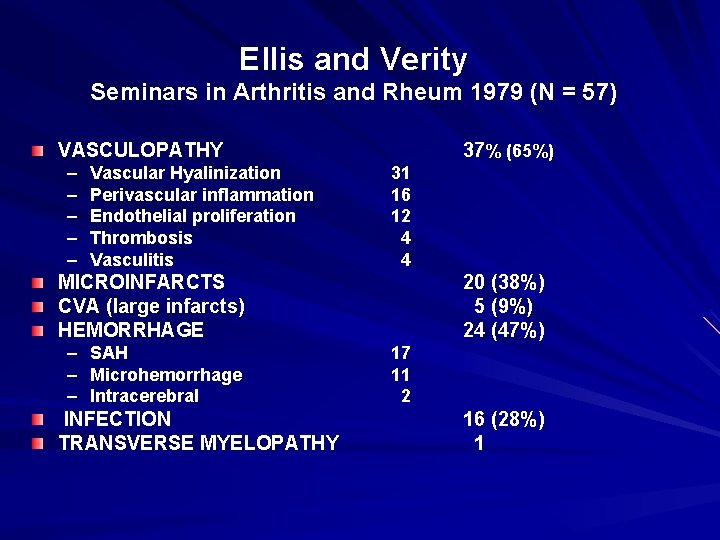
Ellis and Verity Seminars in Arthritis and Rheum 1979 (N = 57) VASCULOPATHY – – – Vascular Hyalinization Perivascular inflammation Endothelial proliferation Thrombosis Vasculitis 37% (65%) 31 16 12 4 4 MICROINFARCTS CVA (large infarcts) HEMORRHAGE – SAH – Microhemorrhage – Intracerebral INFECTION TRANSVERSE MYELOPATHY 20 (38%) 5 (9%) 24 (47%) 17 11 2 16 (28%) 1
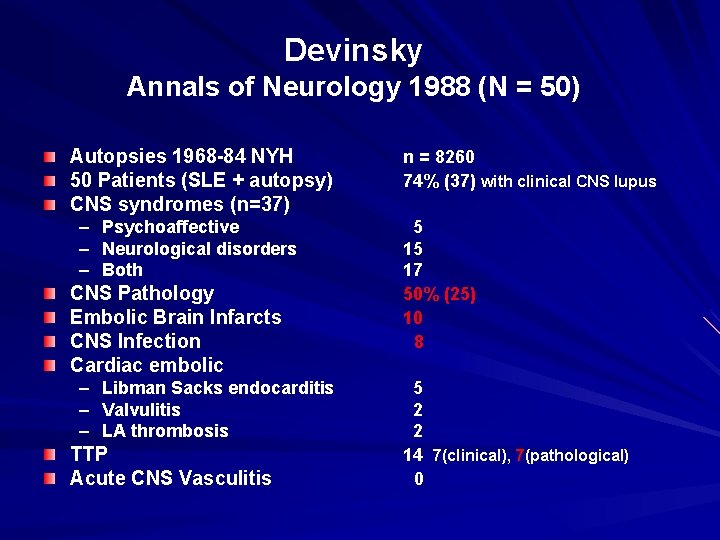
Devinsky Annals of Neurology 1988 (N = 50) Autopsies 1968 -84 NYH 50 Patients (SLE + autopsy) CNS syndromes (n=37) – Psychoaffective – Neurological disorders – Both CNS Pathology Embolic Brain Infarcts CNS Infection Cardiac embolic – – – Libman Sacks endocarditis Valvulitis LA thrombosis TTP Acute CNS Vasculitis n = 8260 74% (37) with clinical CNS lupus 5 15 17 50% (25) 10 8 5 2 2 14 7(clinical), 7(pathological) 0
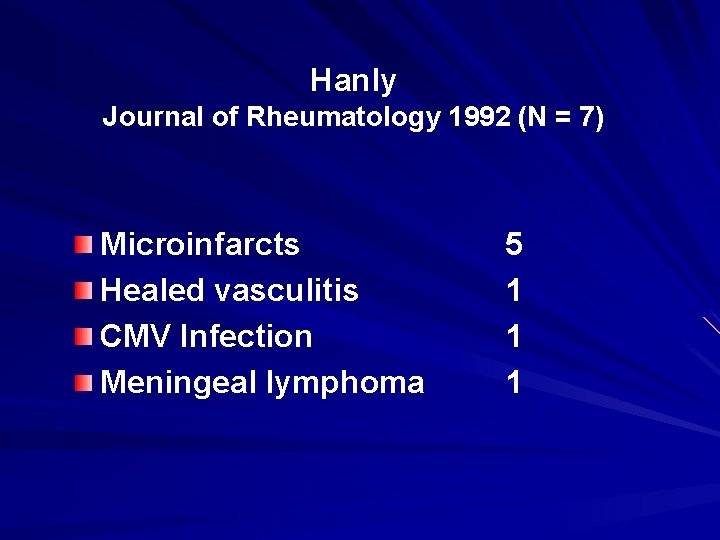
Hanly Journal of Rheumatology 1992 (N = 7) Microinfarcts Healed vasculitis CMV Infection Meningeal lymphoma 5 1 1 1
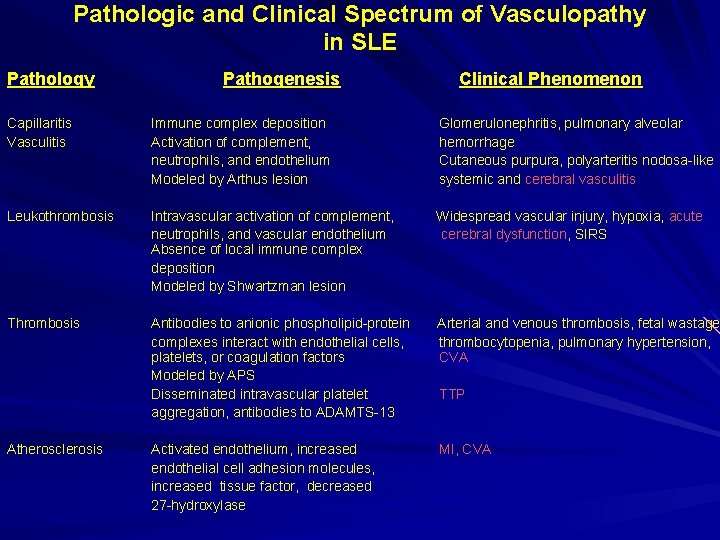
Pathologic and Clinical Spectrum of Vasculopathy in SLE Pathology Pathogenesis Clinical Phenomenon Capillaritis Vasculitis Immune complex deposition Activation of complement, neutrophils, and endothelium Modeled by Arthus lesion Glomerulonephritis, pulmonary alveolar hemorrhage Cutaneous purpura, polyarteritis nodosa-like systemic and cerebral vasculitis Leukothrombosis Intravascular activation of complement, neutrophils, and vascular endothelium Absence of local immune complex deposition Modeled by Shwartzman lesion Widespread vascular injury, hypoxia, acute cerebral dysfunction, SIRS Thrombosis Antibodies to anionic phospholipid-protein complexes interact with endothelial cells, platelets, or coagulation factors Modeled by APS Disseminated intravascular platelet aggregation, antibodies to ADAMTS-13 Arterial and venous thrombosis, fetal wastage thrombocytopenia, pulmonary hypertension, CVA Activated endothelium, increased endothelial cell adhesion molecules, increased tissue factor, decreased 27 -hydroxylase MI, CVA Atherosclerosis TTP

IMMUNE MEDIATED MECHANISMS OF CNS LUPUS Inflammatory Focal or Diffuse Vasculitis Diffuse neutrophil mediated injury with leukoaggregation/leukothromboses Antibody mediated APS - Ab mediated thromboses TTP - Ab to v. WF cleaving protease/ADAMTS Anti-neuronal antibody Cytokine neurotoxicity

ETIOPATHOGENESIS of CNS LUPUS I. Vasculopathy Inflammatory Vasculitis (1) – immune complex deposition Shwartzman Phenomenon (2) -- neutrophil mediated injury Noninflammatory Thrombotic (3) – APS, TTP Arteriosclerosis II. Anti-neuronal antibody (4) anti-lymphocyte abs cross reacting with anti-neuronal anti-ribosomal P antibody anti-50 kd neuronal filament antibody anti-DNA cross reacting with NMDA glutamate receptor III. Cytokine (5)
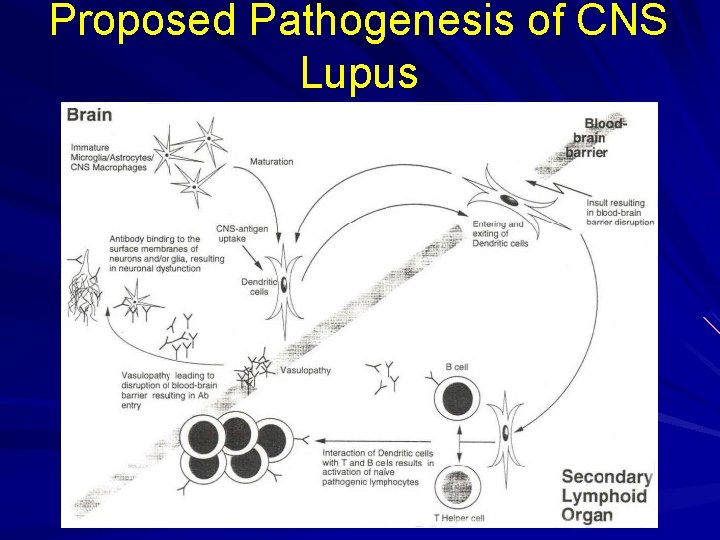
Proposed Pathogenesis of CNS Lupus
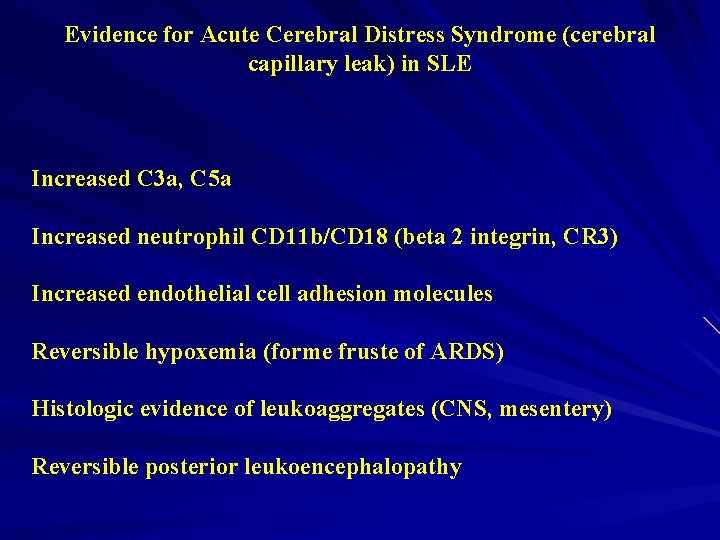
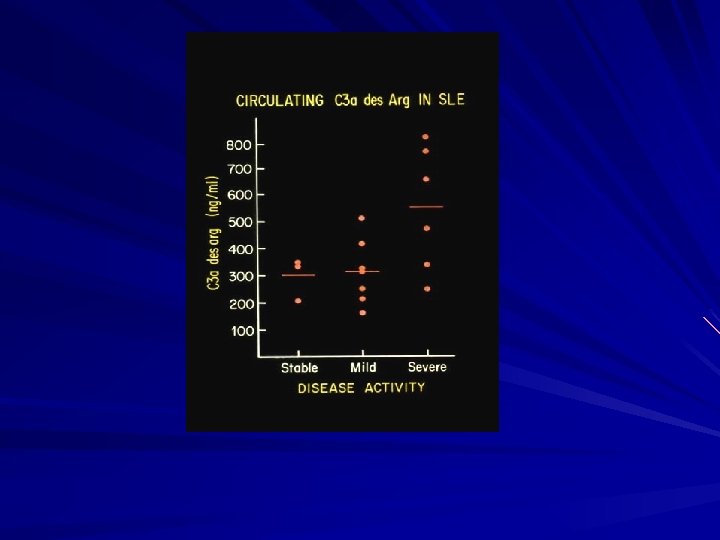
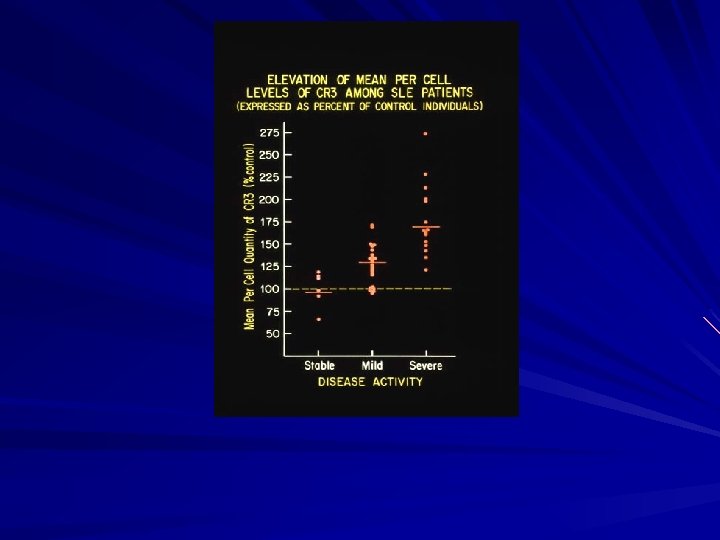
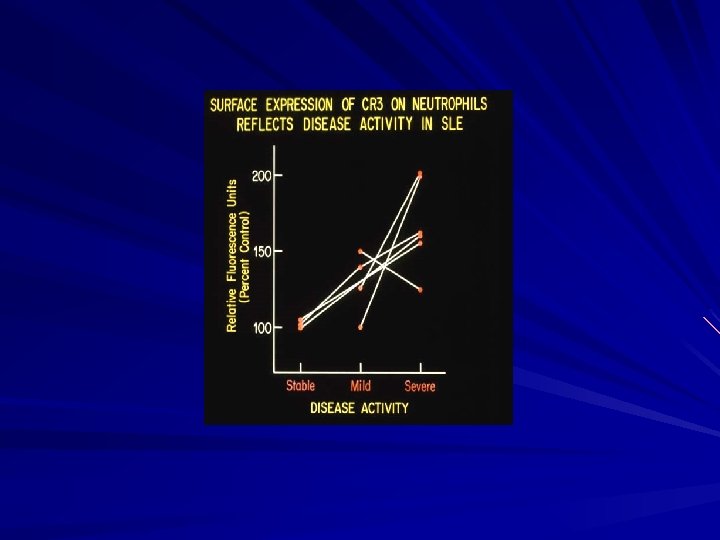
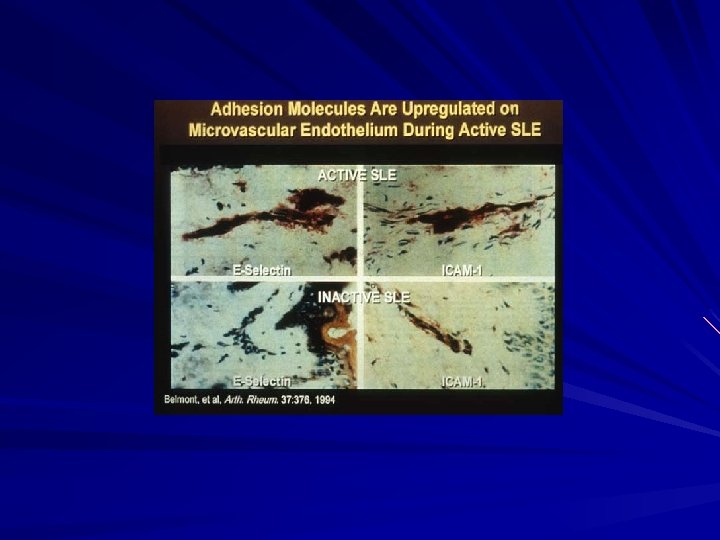
Evidence for Acute Cerebral Distress Syndrome (cerebral capillary leak) in SLE Increased C 3 a, C 5 a Increased neutrophil CD 11 b/CD 18 (beta 2 integrin, CR 3) Increased endothelial cell adhesion molecules Reversible hypoxemia (forme fruste of ARDS) Histologic evidence of leukoaggregates (CNS, mesentery) Reversible posterior leukoencephalopathy
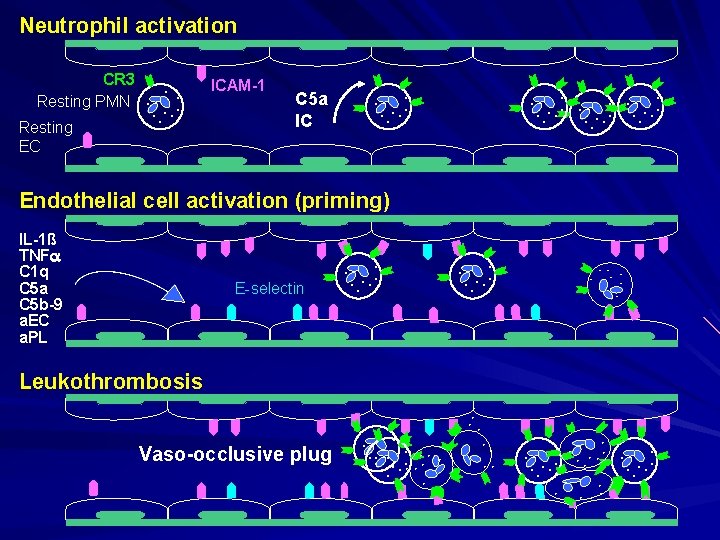
Neutrophil activation CR 3 Resting PMN Resting EC . . . . ICAM-1 C 5 a IC . . . . Endothelial cell activation (priming) E-selectin . . IL-1ß TNF C 1 q C 5 a C 5 b-9 a. EC a. PL . . . . Vaso-occlusive plug . . Leukothrombosis . . . .
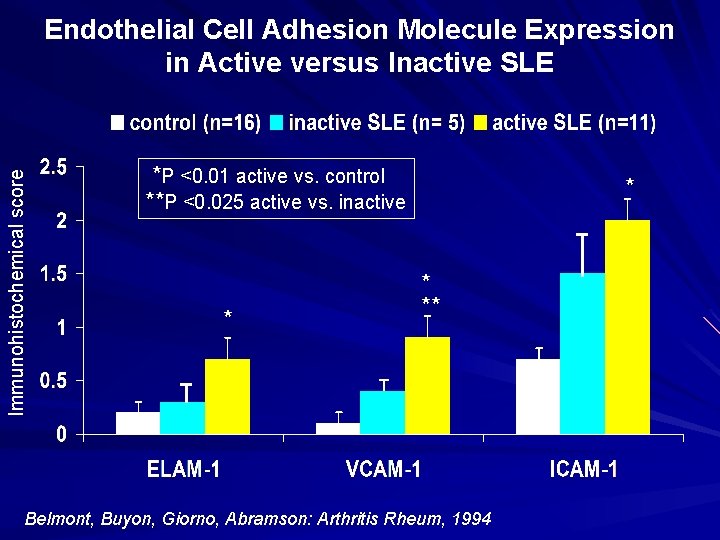
Immunohistochemical score Endothelial Cell Adhesion Molecule Expression in Active versus Inactive SLE *P <0. 01 active vs. control **P <0. 025 active vs. inactive * * ** * T Belmont, Buyon, Giorno, Abramson: Arthritis Rheum, 1994
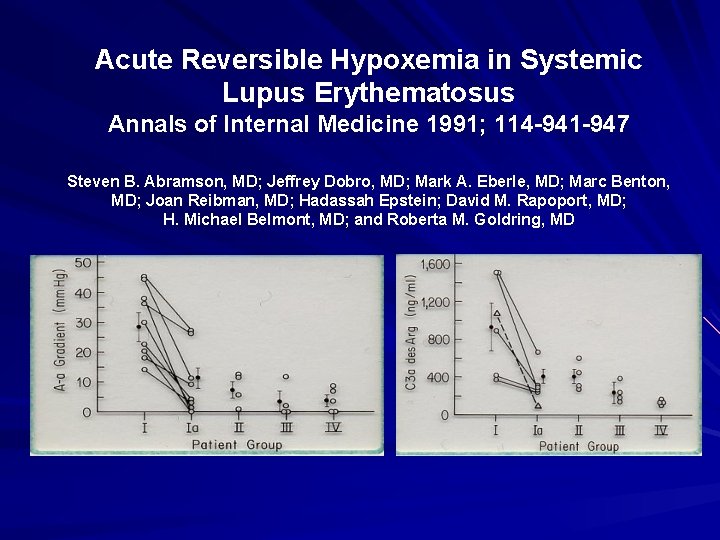
Acute Reversible Hypoxemia in Systemic Lupus Erythematosus Annals of Internal Medicine 1991; 114 -941 -947 Steven B. Abramson, MD; Jeffrey Dobro, MD; Mark A. Eberle, MD; Marc Benton, MD; Joan Reibman, MD; Hadassah Epstein; David M. Rapoport, MD; H. Michael Belmont, MD; and Roberta M. Goldring, MD
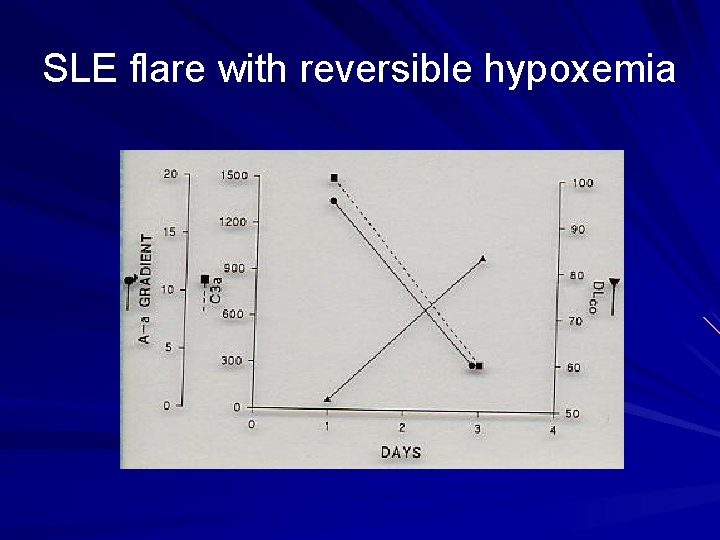
SLE flare with reversible hypoxemia

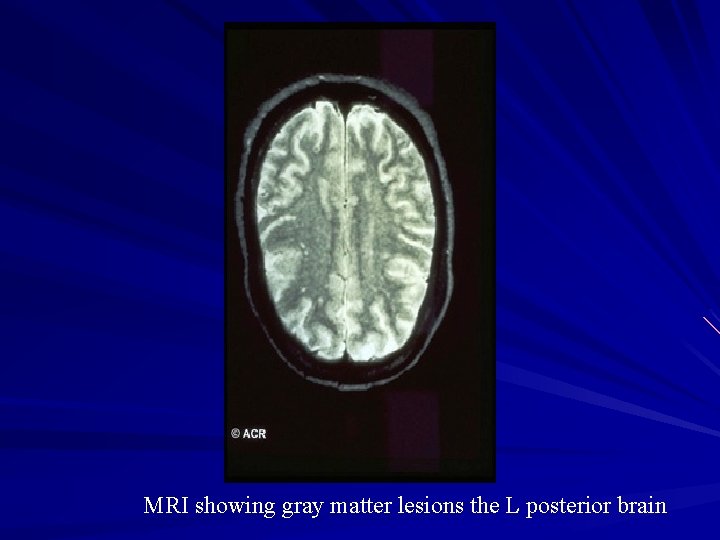
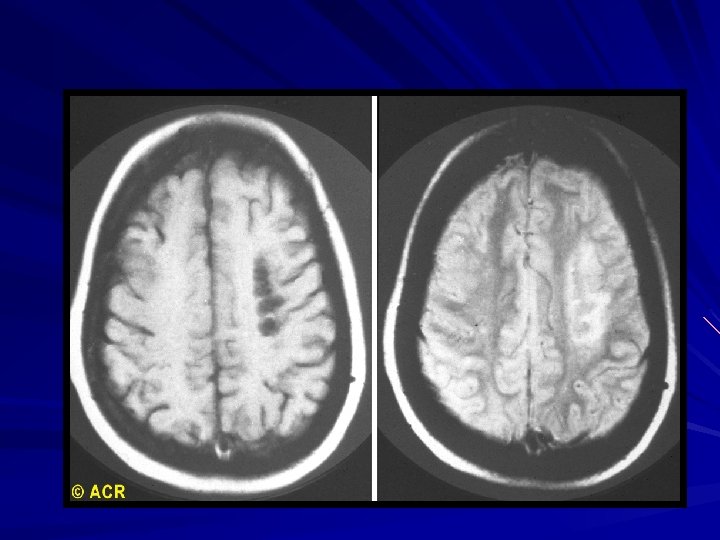
MRI showing gray matter lesions the L posterior brain
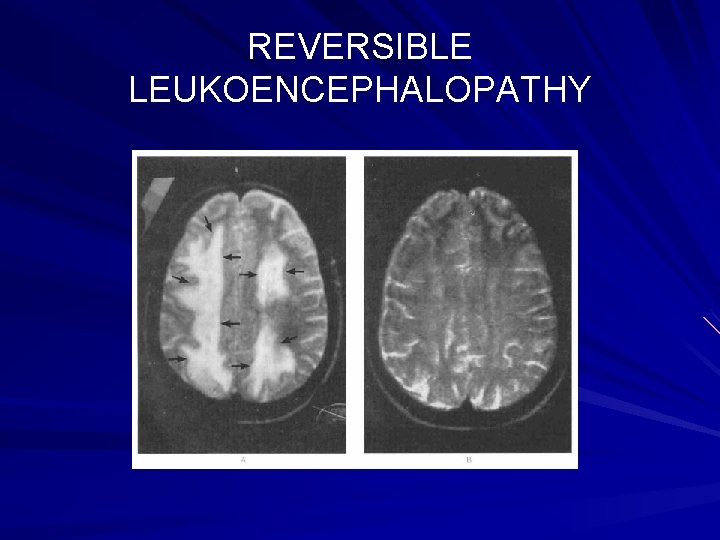
REVERSIBLE LEUKOENCEPHALOPATHY

IMAGING AND DIAGNOSTIC STUDIES CT MRI SPECT PET ANGIOGRAPHY CSF studies EEG Neuropsychological testing Serological (autoantibodies)
IMAGING CT MRI SPECT PET MRA CT angiogram Conventional angiograms CSF analyses – Cells – Protein – Oligoclonal bands – Ig. G/albumin index – Cytokines EEG Neuropsychological testing Anti-neuronal antibodies (e. g. ribosomal-P, neurofilimant, NR 2 NMDA glutamate receptor)
Imaging No pathognomonic finding MRI and CT can both exclude brain absecess, intracerebral hemorrhage, gross cerebral edema and CVA MRI superior to CT in detecting acute CNS injury including transverse myelitis, new infarct or disruption of the blood brain barrier Normal MRI doesn’t exclude CNS lupus and punctate lesions, especially on T 2 weighted images, not specific MRA, angiography and CT angiogram typically incapably of resolution to demonstrate small vessel vasculopathy SPECT and PET lack specificity and not reliable EEG useful for identifying seizure, encephalopathy or brain death
Diagnostic Testing LP most useful to exclude infection, hemorrhage or confirm organic rather than functional process NP testing most useful to distinguish functional from organic etiology of psychiatric syndromes Anti-ribosomal P antibodies useful in patients with psychosis Antiphospholipid antibodies useful in CVA, seizures and focal neurological defects
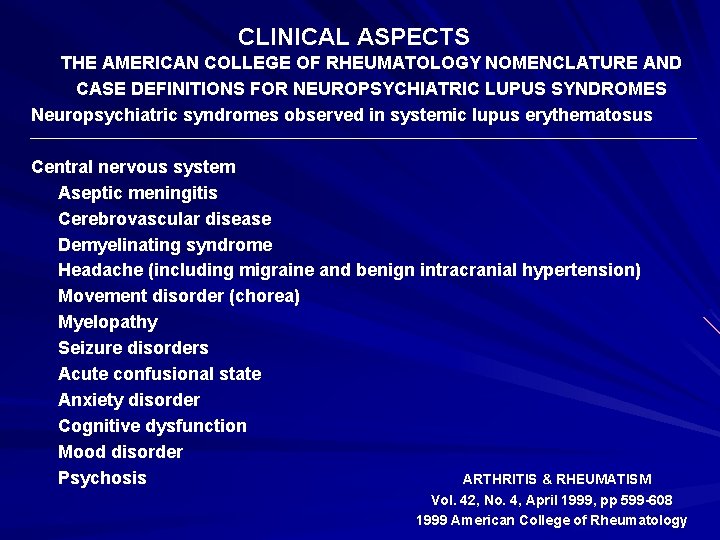
CLINICAL ASPECTS THE AMERICAN COLLEGE OF RHEUMATOLOGY NOMENCLATURE AND CASE DEFINITIONS FOR NEUROPSYCHIATRIC LUPUS SYNDROMES Neuropsychiatric syndromes observed in systemic lupus erythematosus Central nervous system Aseptic meningitis Cerebrovascular disease Demyelinating syndrome Headache (including migraine and benign intracranial hypertension) Movement disorder (chorea) Myelopathy Seizure disorders Acute confusional state Anxiety disorder Cognitive dysfunction Mood disorder Psychosis ARTHRITIS & RHEUMATISM Vol. 42, No. 4, April 1999, pp 599 -608 1999 American College of Rheumatology
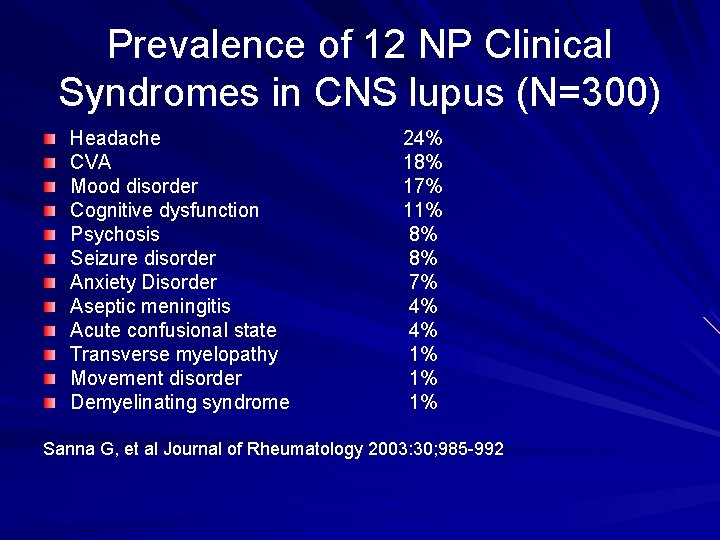
Prevalence of 12 NP Clinical Syndromes in CNS lupus (N=300) Headache CVA Mood disorder Cognitive dysfunction Psychosis Seizure disorder Anxiety Disorder Aseptic meningitis Acute confusional state Transverse myelopathy Movement disorder Demyelinating syndrome 24% 18% 17% 11% 8% 8% 7% 4% 4% 1% 1% 1% Sanna G, et al Journal of Rheumatology 2003: 30; 985 -992
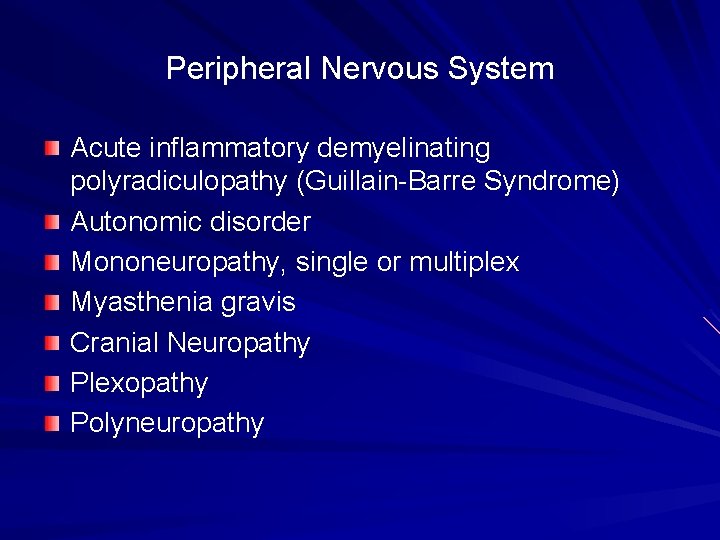
Peripheral Nervous System Acute inflammatory demyelinating polyradiculopathy (Guillain-Barre Syndrome) Autonomic disorder Mononeuropathy, single or multiplex Myasthenia gravis Cranial Neuropathy Plexopathy Polyneuropathy
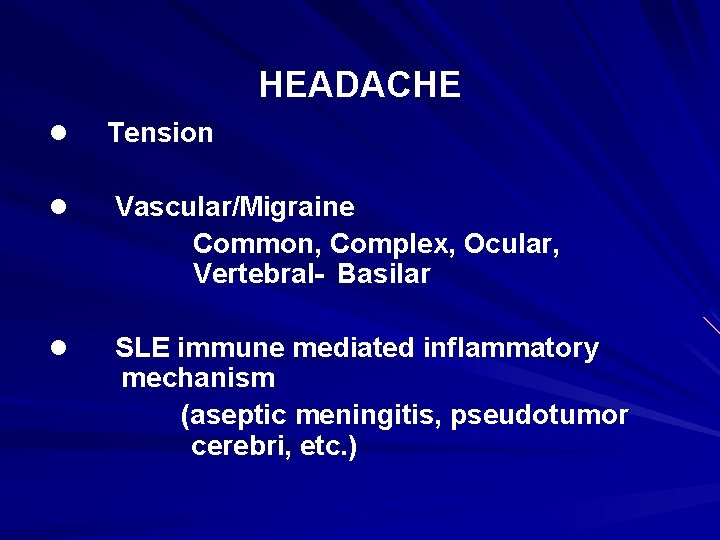
HEADACHE l Tension l Vascular/Migraine Common, Complex, Ocular, Vertebral- Basilar l SLE immune mediated inflammatory mechanism (aseptic meningitis, pseudotumor cerebri, etc. )
SEIZURE Diffuse cerebral injury Diffuse APS Diffuse vasculitis Diffuse leukoaggregation/ACDS/PMN mediated Anti-neuronal antibody Cytokines l l Focal APS
ACUTE CONFUSIONAL SYNDROME (DELIRIUM, OMS) l Diffuse cerebral injury Diffuse APS Diffuse vasculitis Diffuse leukoaggregation/ACDS/PMN mediated Anti-neuronal antibody Cytokines
CEREBRAL VASCULAR ACCIDENT l Atherogenesis and thrombogenesis HTN, DM, cigarettes, cholesterol, sedentary, LDL, homocysteine Steroids Immune complex injury l APS l Larger vessel vasculitis (RARE)
ASEPTIC MENINGITIS l Viral l NSAIDS - Ibuprofen l SLE - Immune mediated inflammatory disorder (IMID) (e. g. meningeal vasculopathy)
PSYCHIATRIC DISORDERS l. PSYCHOSES l. ORGANIC AFFECTIVE (MOOD) DISORDER l. ANXIETY DISORDER l SLE Immune mediated inflammatory disorder (IMID)
TRANSVERSE MYELITIS l Spinal artery - APS - Vasculitis - Leukoaggregation/neutrophil mediated
MOVEMENT DISORDER DEMYELINATING SYNDROME COGNITIVE DYSFUNCTION
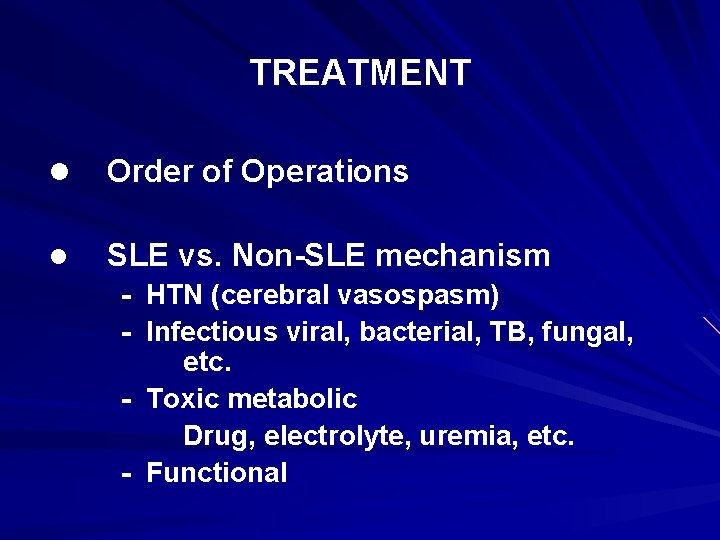
TREATMENT l Order of Operations l SLE vs. Non-SLE mechanism - HTN (cerebral vasospasm) - Infectious viral, bacterial, TB, fungal, etc. - Toxic metabolic Drug, electrolyte, uremia, etc. - Functional
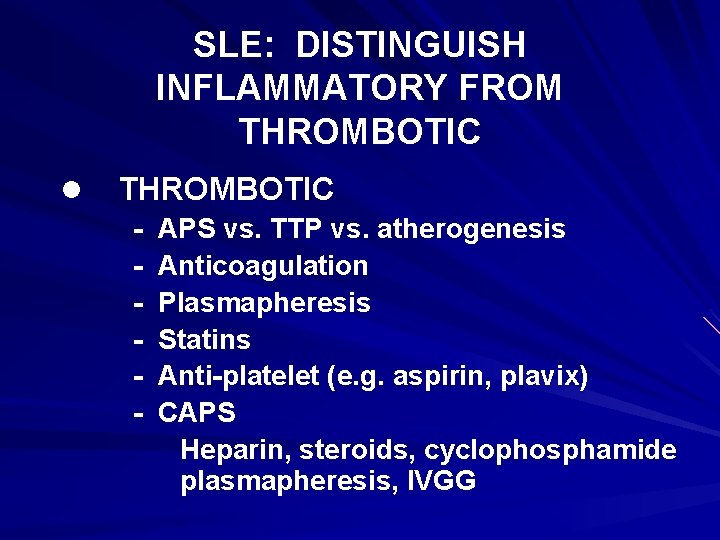
SLE: DISTINGUISH INFLAMMATORY FROM THROMBOTIC l THROMBOTIC - APS vs. TTP vs. atherogenesis Anticoagulation Plasmapheresis Statins Anti-platelet (e. g. aspirin, plavix) CAPS Heparin, steroids, cyclophosphamide plasmapheresis, IVGG
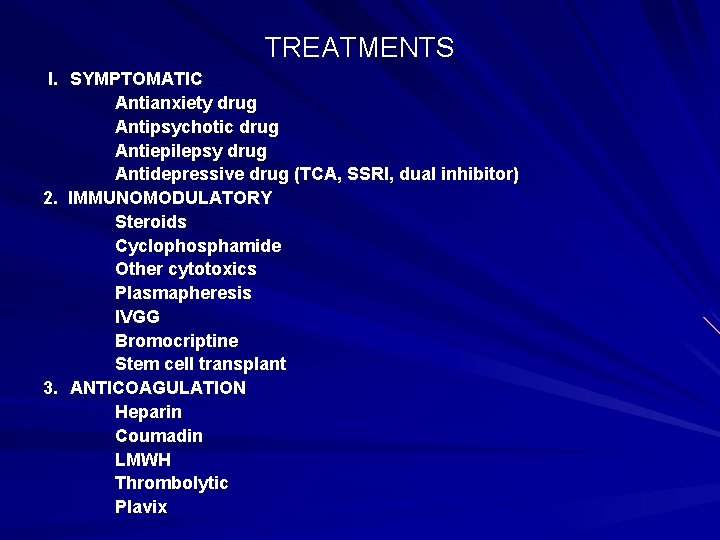
TREATMENTS I. SYMPTOMATIC Antianxiety drug Antipsychotic drug Antiepilepsy drug Antidepressive drug (TCA, SSRI, dual inhibitor) 2. IMMUNOMODULATORY Steroids Cyclophosphamide Other cytotoxics Plasmapheresis IVGG Bromocriptine Stem cell transplant 3. ANTICOAGULATION Heparin Coumadin LMWH Thrombolytic Plavix
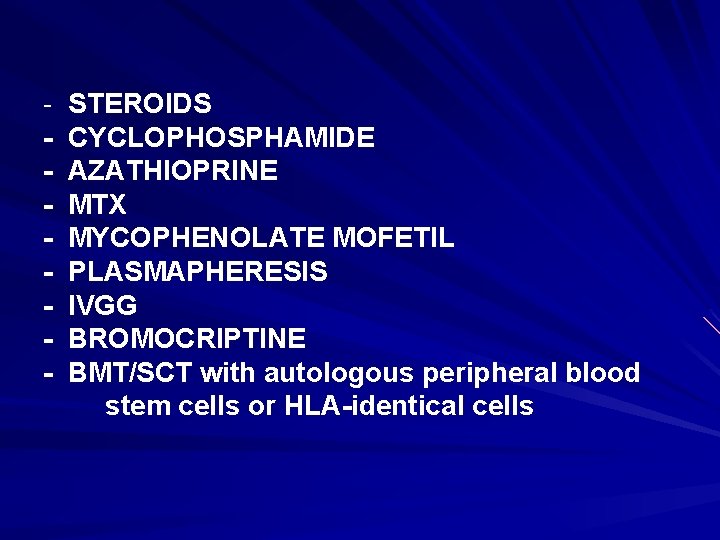
- STEROIDS CYCLOPHOSPHAMIDE AZATHIOPRINE MTX MYCOPHENOLATE MOFETIL PLASMAPHERESIS IVGG BROMOCRIPTINE BMT/SCT with autologous peripheral blood stem cells or HLA-identical cells
SUMMARY DIVERSE ETIOLOGY and PATHOLOGY DIVERSE CLINICAL SYNDROMES EXCLUDE NON-SLE, NONIMMUNE MEDIATED PROCESS DISTINGUISH INFLAMMATORY versus THROMBOTIC MECHANISMS ANTICOAGULATION versus INFLAMMATORY/IMMUNOMODULATORY THERAPY
- Slides: 45