CNS Infections Sarah Mc Pherson Aug 15 2002

- Slides: 28
CNS Infections Sarah Mc. Pherson Aug. 15, 2002
14 yo male presents with headache ane fever X 24 hrs. Previously well. Seen in doctor’s office and sent to ED after a witnessed focal seizure involving the right arm. Other history unremarkable O/E: Hr 100, BP 110/70, Temp 39. 5 normal mental status, no nuchal rigidity normal neuro exam What would you do? ?
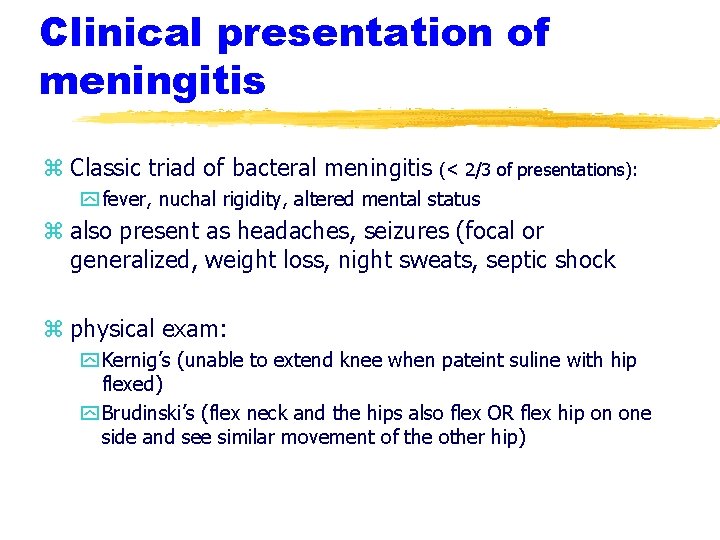
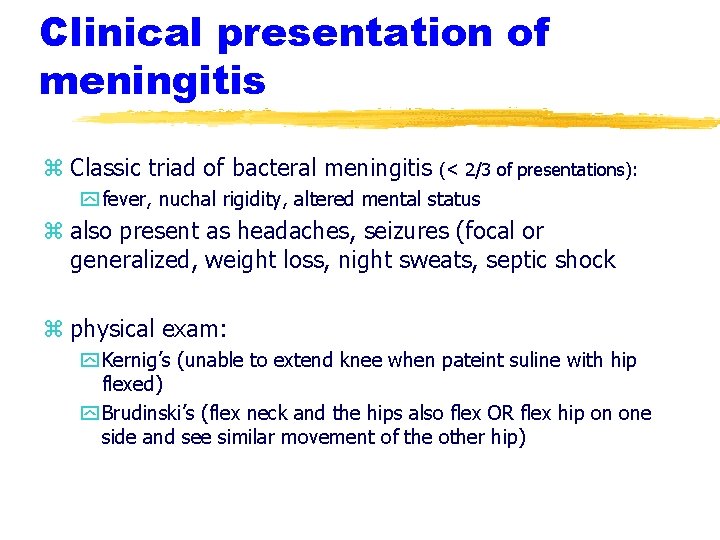
Clinical presentation of meningitis z Classic triad of bacteral meningitis (< 2/3 of presentations): y fever, nuchal rigidity, altered mental status z also present as headaches, seizures (focal or generalized, weight loss, night sweats, septic shock z physical exam: y Kernig’s (unable to extend knee when pateint suline with hip flexed) y Brudinski’s (flex neck and the hips also flex OR flex hip on one side and see similar movement of the other hip)
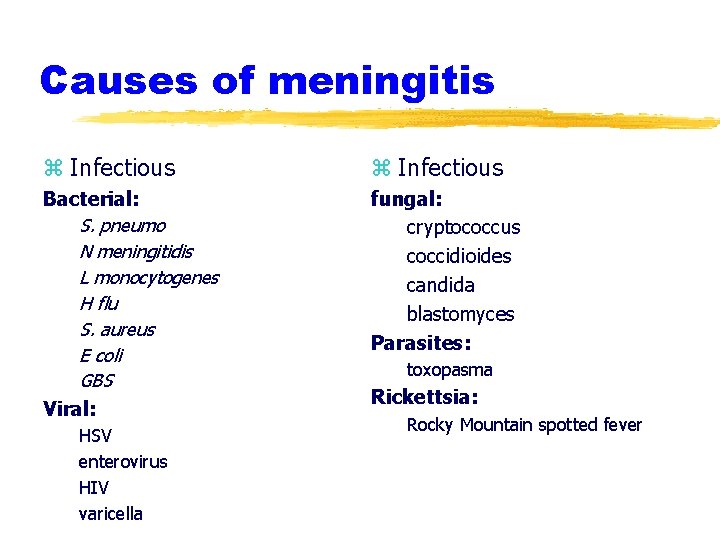
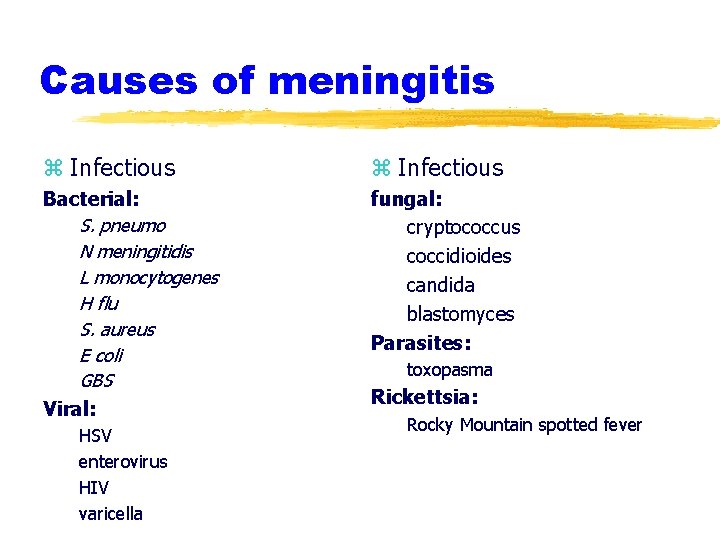
Causes of meningitis z Infectious Bacterial: S. pneumo N meningitidis L monocytogenes H flu S. aureus E coli GBS Viral: fungal: cryptococcus coccidioides candida blastomyces Parasites: HSV enterovirus HIV varicella toxopasma Rickettsia: Rocky Mountain spotted fever
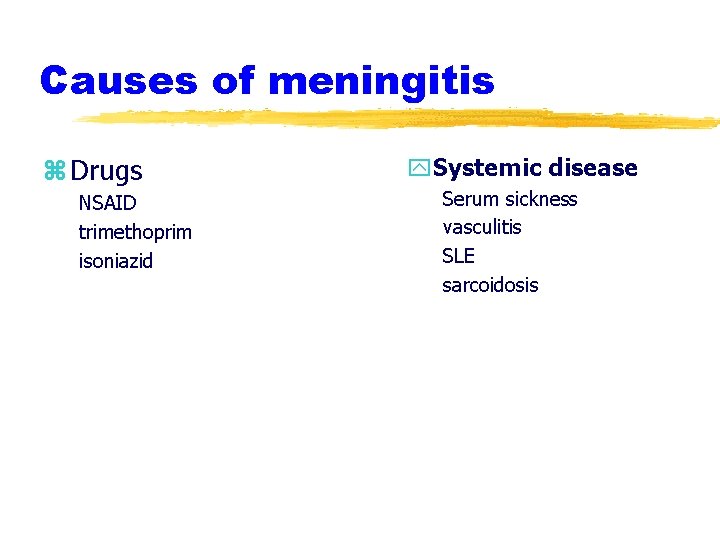
Causes of meningitis z Drugs NSAID trimethoprim isoniazid y. Systemic disease Serum sickness vasculitis SLE sarcoidosis
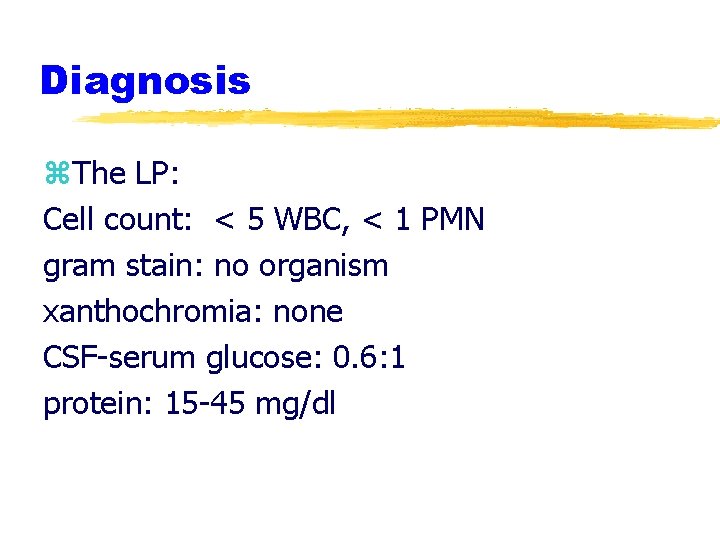
Diagnosis z. The LP: Cell count: < 5 WBC, < 1 PMN gram stain: no organism xanthochromia: none CSF-serum glucose: 0. 6: 1 protein: 15 -45 mg/dl
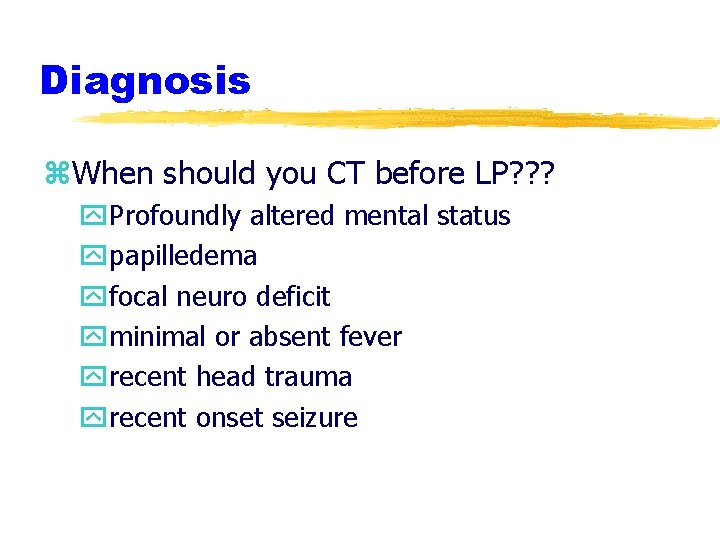
Diagnosis z. When should you CT before LP? ? ? y. Profoundly altered mental status ypapilledema yfocal neuro deficit yminimal or absent fever yrecent head trauma yrecent onset seizure
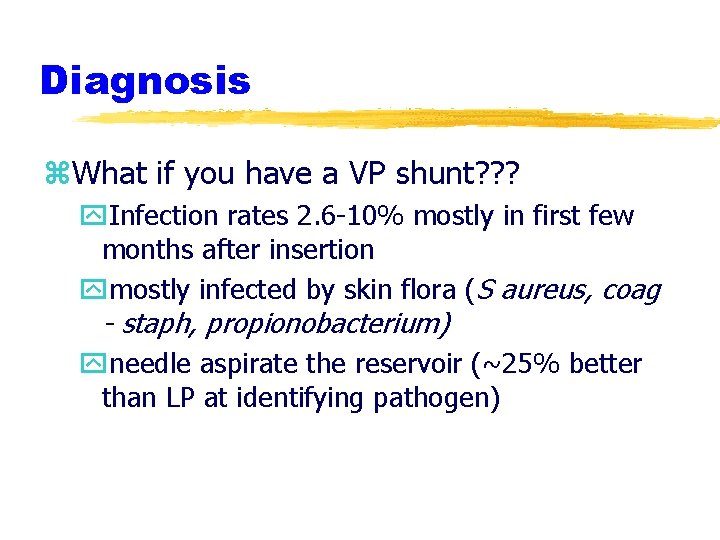
Diagnosis z. What if you have a VP shunt? ? ? y. Infection rates 2. 6 -10% mostly in first few months after insertion ymostly infected by skin flora (S aureus, coag - staph, propionobacterium) yneedle aspirate the reservoir (~25% better than LP at identifying pathogen)
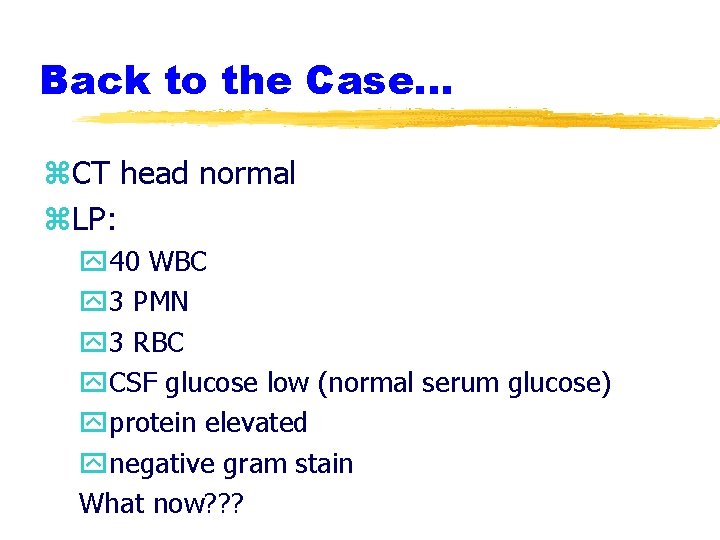
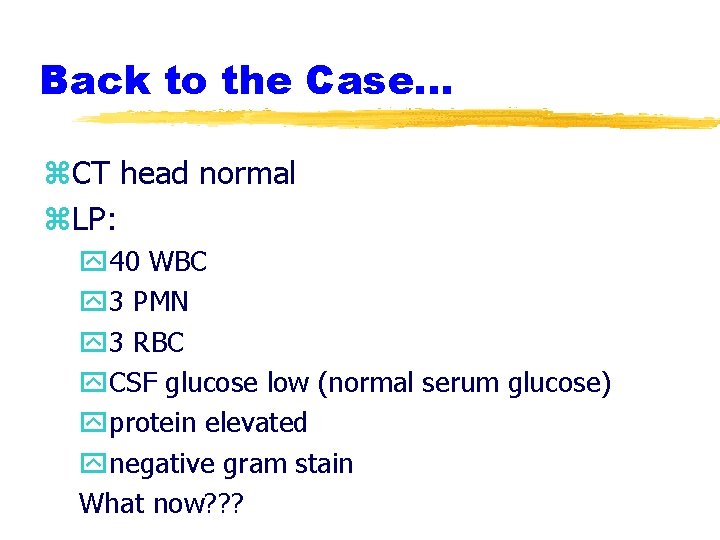
Back to the Case. . . z. CT head normal z. LP: y 40 WBC y 3 PMN y 3 RBC y. CSF glucose low (normal serum glucose) yprotein elevated ynegative gram stain What now? ? ?

Definitive therapy z. Bacterial Meningitis: y 3 rd generation cephalosporin yadd Vanco if in area where drug resistant S. pneumo is prevelant yadd ampicillin to cover Listeria (< 3 months, > 50 years)
Definitive therapy z. What if your gram stain shows gramnegative coccobacilli? ? ? z. The controversy of pre-treatment with steroids. . .
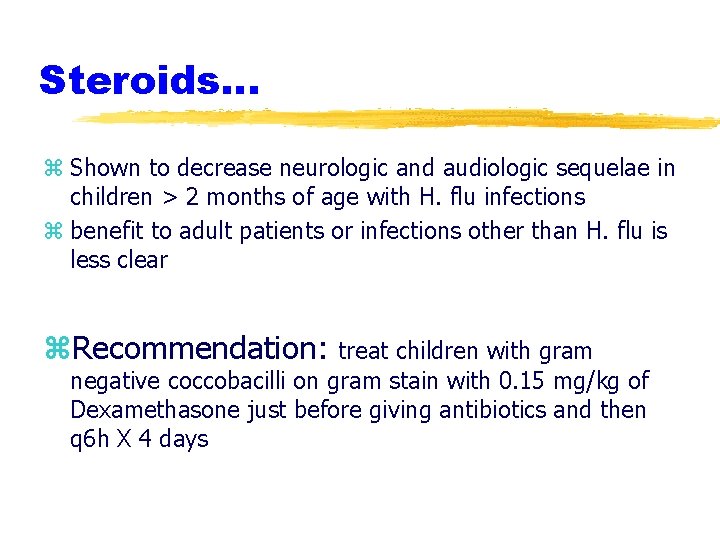
Steroids. . . z Shown to decrease neurologic and audiologic sequelae in children > 2 months of age with H. flu infections z benefit to adult patients or infections other than H. flu is less clear z. Recommendation: treat children with gram negative coccobacilli on gram stain with 0. 15 mg/kg of Dexamethasone just before giving antibiotics and then q 6 h X 4 days
Another Case 22 yo girl presents with purpuric rash, nuchal rigidity, temp 39. 1, HR 110, BP 95/60, with altered mental status How would this presentation alter your approach? ABC’s first, blood cultures, Antibiotics then LP
Aseptic meningitis z. Typically present as fever and nuchal rigidity, may have headache, N&V z. CSF may show increased WBC with increased lymphocytes; normal to slightly elevated protein; normal gram stain
Aseptic meningitis z. Management: ysupportive xrelief of headache, fever, and dehydration ymedical xif WBC on gram stain most clinicans will start on empiric antibiotics pending C&S xif evidence of primary HSV infection, acyclovir (oral 200 5 X/day for 10 days)
z 70 yo man presents with fever 38. 5 X 6 hr, headache, altered LOC and aphasia, HR 85, BP 105/80 z. CT shows edema of the right temporal lobe z. LP 30 WBC, increased protein, normal gram stain
Viral encephalitits z Rare z typically present with fever, headache, altered LOC, behavioral or speech disturbnce, focal neuro deficits, seizures z CSF: mononuclear cell pleocytosis; elevated protein; normal gram stain; PCR for HSV, CMV, HHV-6, enterovirus (99% sens and 94% spec for HSV) z CT, MRI, EEG may be helpful
Herpes Encephalitis z Neonatal y CNS involvement in majority infants with herpetic disease in the newborn period y CSF PCR is the gold standard y treatment : Acyclovir 30 mh/kg/d divided q 8 h y with antiviral decreased mortality from 50% to 15% (pts with CNS involvement) y 2/3 will have long term neurologic sequelae despite treatment
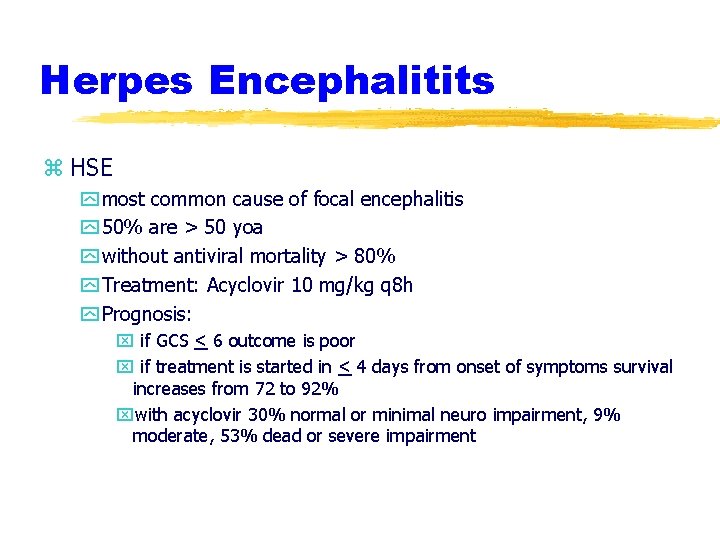
Herpes Encephalitits z HSE y most common cause of focal encephalitis y 50% are > 50 yoa y without antiviral mortality > 80% y Treatment: Acyclovir 10 mg/kg q 8 h y Prognosis: x if GCS < 6 outcome is poor x if treatment is started in < 4 days from onset of symptoms survival increases from 72 to 92% xwith acyclovir 30% normal or minimal neuro impairment, 9% moderate, 53% dead or severe impairment
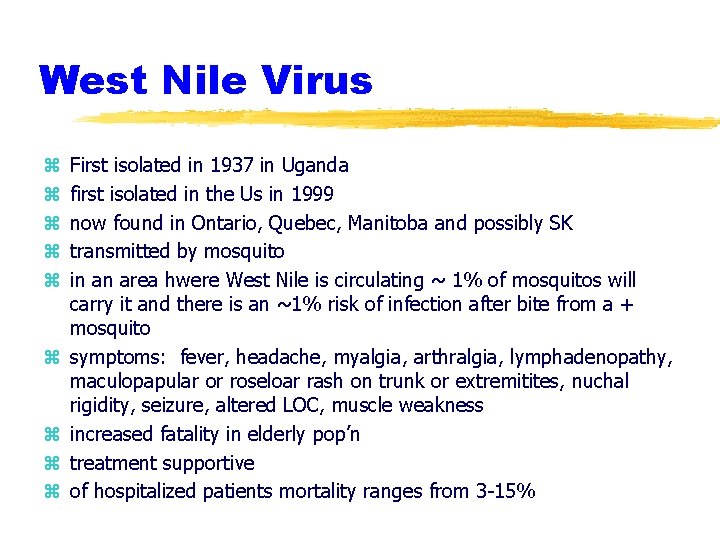
West Nile Virus z z z z z First isolated in 1937 in Uganda first isolated in the Us in 1999 now found in Ontario, Quebec, Manitoba and possibly SK transmitted by mosquito in an area hwere West Nile is circulating ~ 1% of mosquitos will carry it and there is an ~1% risk of infection after bite from a + mosquito symptoms: fever, headache, myalgia, arthralgia, lymphadenopathy, maculopapular or roseloar rash on trunk or extremitites, nuchal rigidity, seizure, altered LOC, muscle weakness increased fatality in elderly pop’n treatment supportive of hospitalized patients mortality ranges from 3 -15%
z 45 yo man with HIV presents with headache and fever neuro exam normal, temp 38. 2, normal vitals What next? ?
z. Normal CT head but when infused shows ring enhancing lesion z. DX? Toxoplasmosis z. Rx? Admission, pyrimethamine 200 mg po then 50 -100 mg qd plus clindamycin 900 iv q 6 h
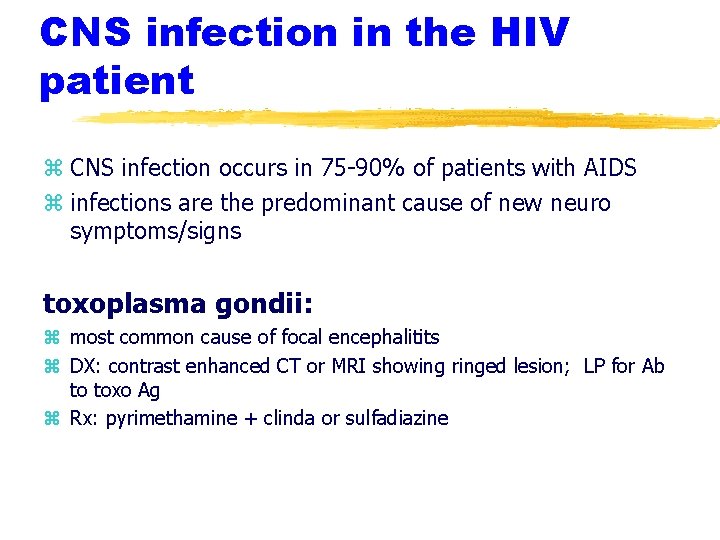
CNS infection in the HIV patient z CNS infection occurs in 75 -90% of patients with AIDS z infections are the predominant cause of new neuro symptoms/signs toxoplasma gondii: z most common cause of focal encephalitits z DX: contrast enhanced CT or MRI showing ringed lesion; LP for Ab to toxo Ag z Rx: pyrimethamine + clinda or sulfadiazine
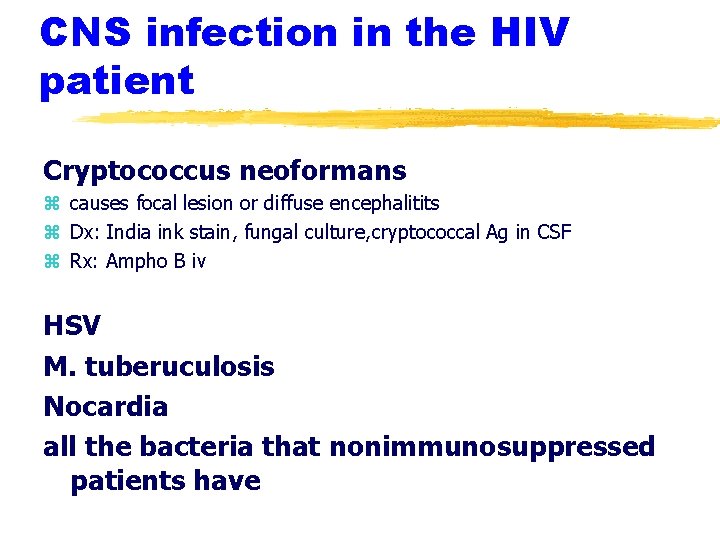
CNS infection in the HIV patient Cryptococcus neoformans z causes focal lesion or diffuse encephalitits z Dx: India ink stain, fungal culture, cryptococcal Ag in CSF z Rx: Ampho B iv HSV M. tuberuculosis Nocardia all the bacteria that nonimmunosuppressed patients have
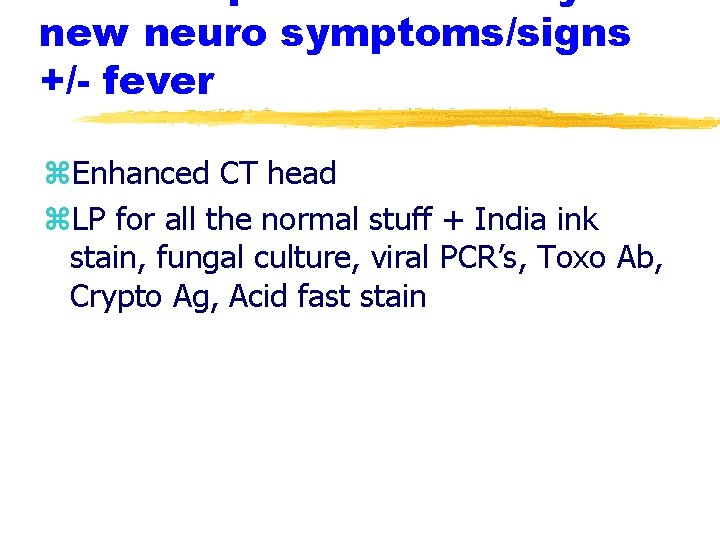
new neuro symptoms/signs +/- fever z. Enhanced CT head z. LP for all the normal stuff + India ink stain, fungal culture, viral PCR’s, Toxo Ab, Crypto Ag, Acid fast stain
25 yo women presents with back pain X 2 days. She has no other concerns. O/E afebrile, hemodynamically stable, normal neuro exam, you notice track marks on her arms. She admits to ongoing IVDU. What would you do next? What are your concerns?
Epidural Abscess z Risk factors: y IVDU y recent spinal or epidural anaesthesia y systemic infection z Clinical features: y back pain y focal neuro deficits y fever (83% of the time) z all IVDUers with back pain should be considered infectious until proven otherwise (osteo vs epidural abscess)
Epidural Abscess z. Dx: CT, if negative and clinical suspicion is high then need an MRI z. Rx: yemergent surgical debridement y 3 rd generation cephalosporin + Flagyl