CNS INFECTIONS Reat ZARAS MD Ass Prof Infection









- Slides: 44
CNS INFECTIONS Reşat ÖZARAS, MD, Ass. Prof. Infection Dept. rozaras@yahoo. com
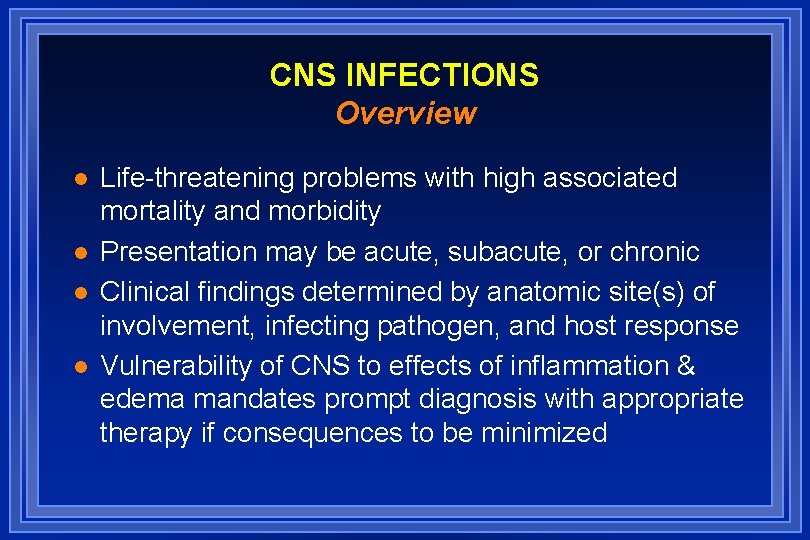
CNS INFECTIONS Overview l l Life-threatening problems with high associated mortality and morbidity Presentation may be acute, subacute, or chronic Clinical findings determined by anatomic site(s) of involvement, infecting pathogen, and host response Vulnerability of CNS to effects of inflammation & edema mandates prompt diagnosis with appropriate therapy if consequences to be minimized
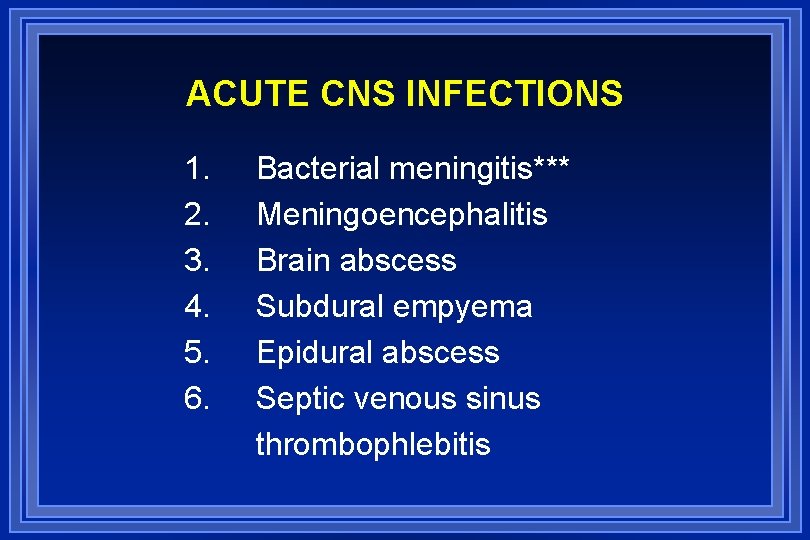
ACUTE CNS INFECTIONS 1. 2. 3. 4. 5. 6. Bacterial meningitis*** Meningoencephalitis Brain abscess Subdural empyema Epidural abscess Septic venous sinus thrombophlebitis
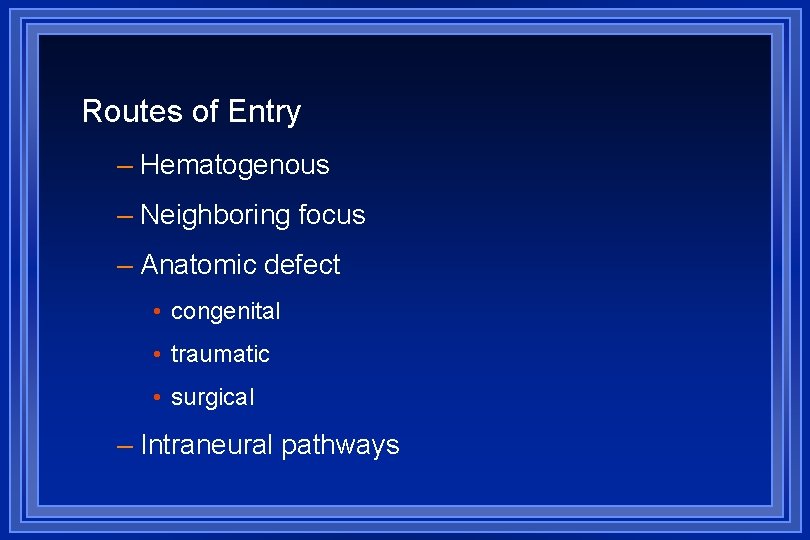
Routes of Entry – Hematogenous – Neighboring focus – Anatomic defect • congenital • traumatic • surgical – Intraneural pathways
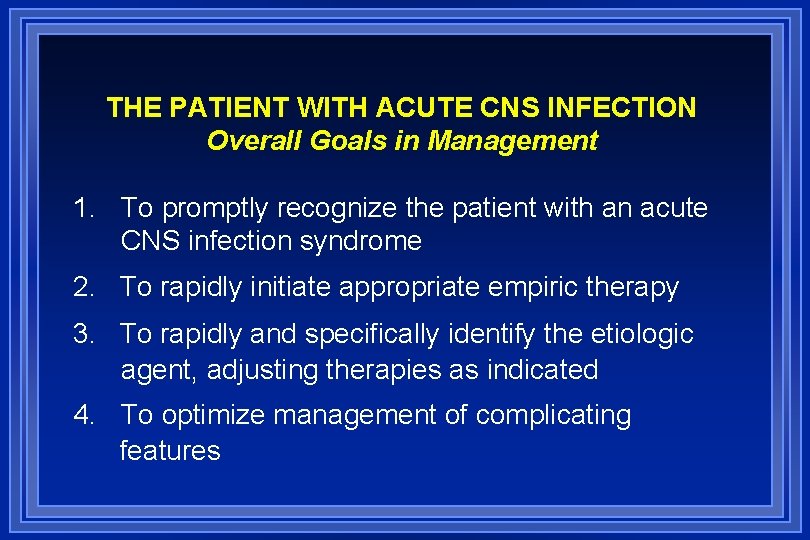
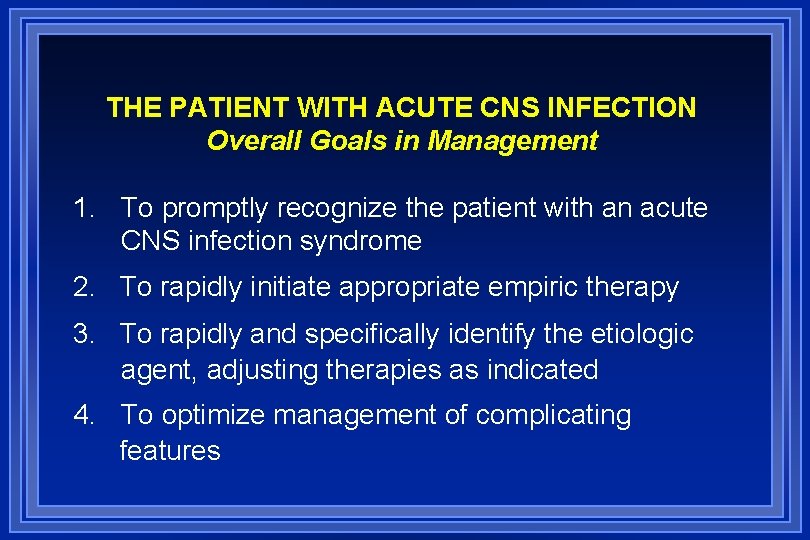
THE PATIENT WITH ACUTE CNS INFECTION Overall Goals in Management 1. To promptly recognize the patient with an acute CNS infection syndrome 2. To rapidly initiate appropriate empiric therapy 3. To rapidly and specifically identify the etiologic agent, adjusting therapies as indicated 4. To optimize management of complicating features
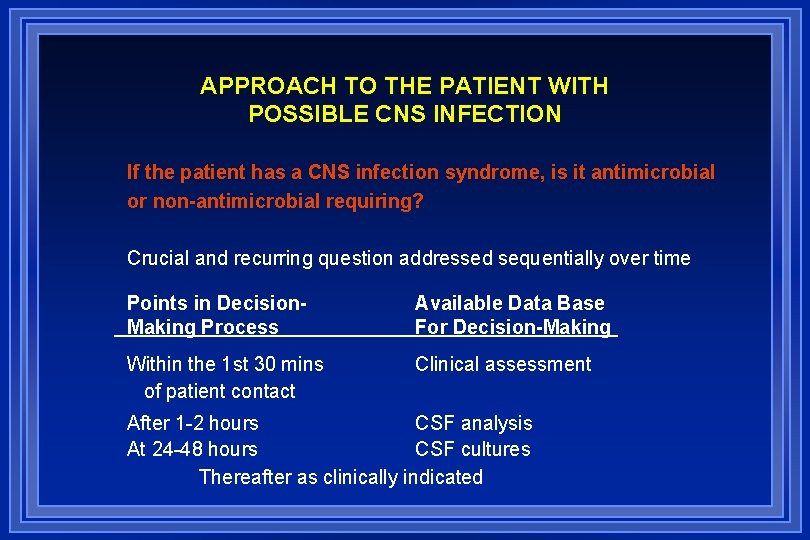
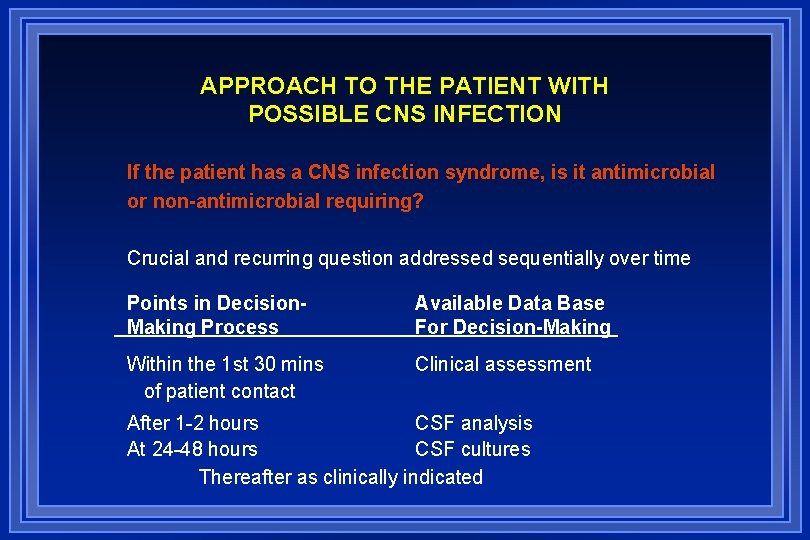
APPROACH TO THE PATIENT WITH POSSIBLE CNS INFECTION If the patient has a CNS infection syndrome, is it antimicrobial or non-antimicrobial requiring? Crucial and recurring question addressed sequentially over time Points in Decision. Making Process Available Data Base For Decision-Making Within the 1 st 30 mins of patient contact Clinical assessment After 1 -2 hours CSF analysis At 24 -48 hours CSF cultures Thereafter as clinically indicated
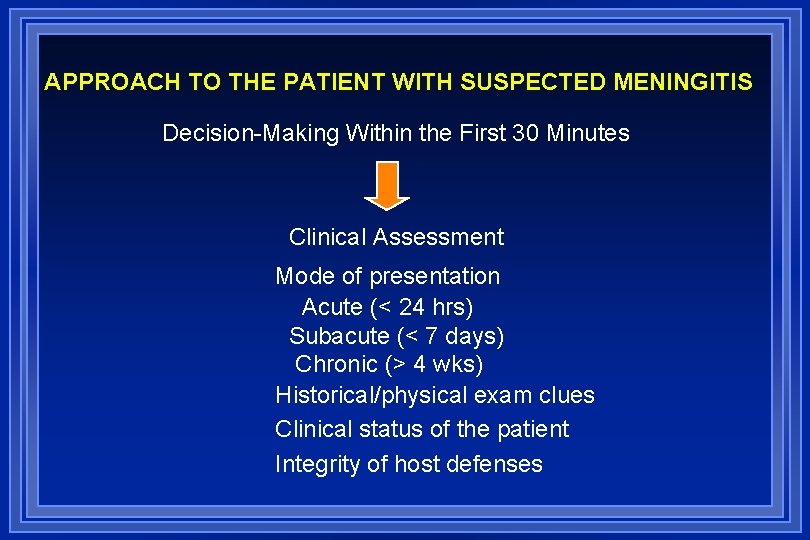
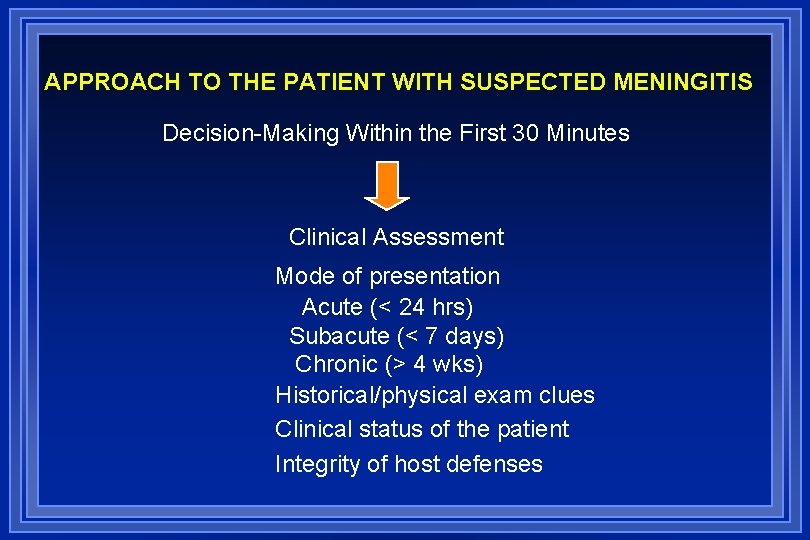
APPROACH TO THE PATIENT WITH SUSPECTED MENINGITIS Decision-Making Within the First 30 Minutes Clinical Assessment Mode of presentation Acute (< 24 hrs) Subacute (< 7 days) Chronic (> 4 wks) Historical/physical exam clues Clinical status of the patient Integrity of host defenses

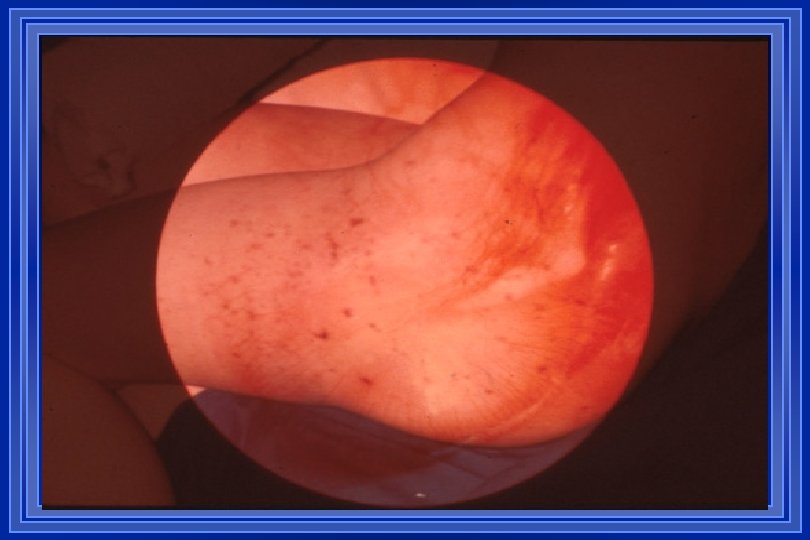
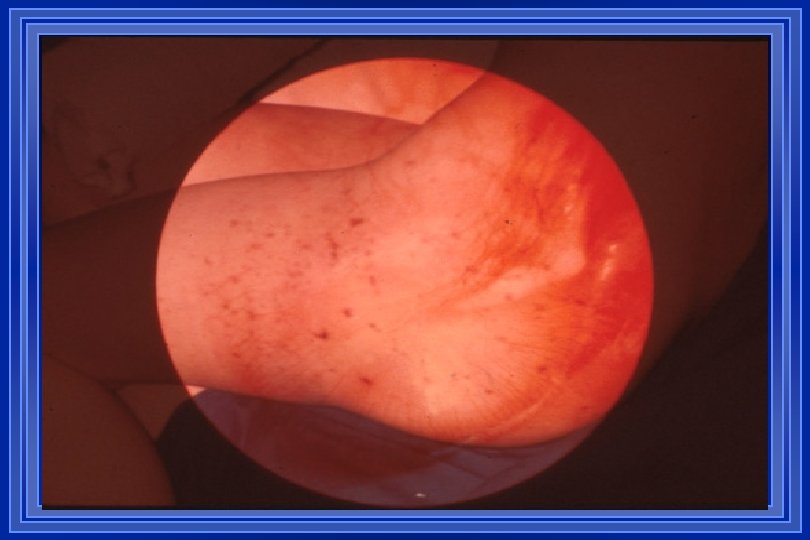
Clinical Features l l l l l Fever Headache Nuchal rigidity Altered mental status Photophobia Non-specific symptoms/signs Focal neurological signs Seizures Specific clinical stigmata according to etiological agent Children / elderly
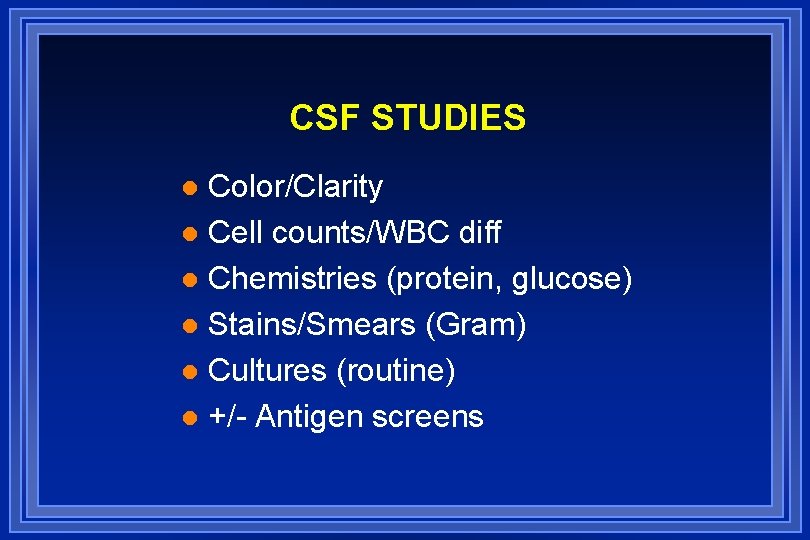
CSF STUDIES Color/Clarity l Cell counts/WBC diff l Chemistries (protein, glucose) l Stains/Smears (Gram) l Cultures (routine) l +/- Antigen screens l
APPROACH TO THE PATIENT WITH SUSPECTED MENINGITIS Decision-Making at 1 -2 Hours CSF Analysis CSF smears/stains CSF antigen screens CSF “profile”
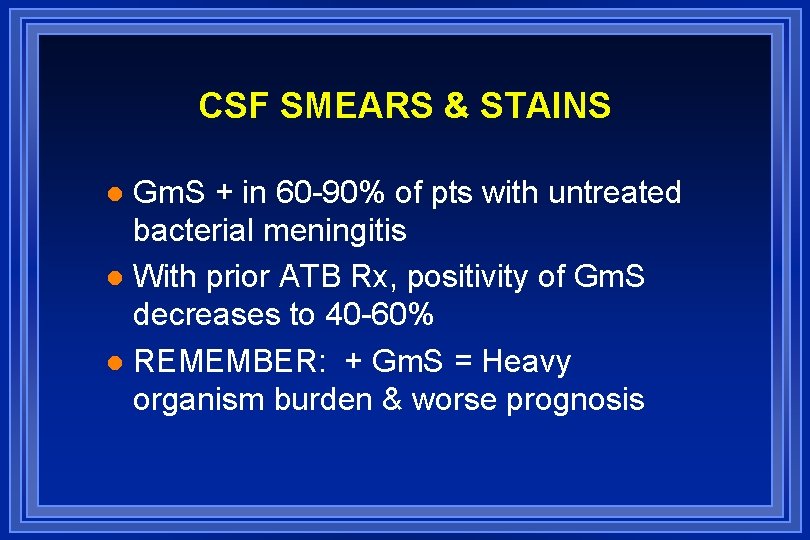
CSF SMEARS & STAINS Gm. S + in 60 -90% of pts with untreated bacterial meningitis l With prior ATB Rx, positivity of Gm. S decreases to 40 -60% l REMEMBER: + Gm. S = Heavy organism burden & worse prognosis l


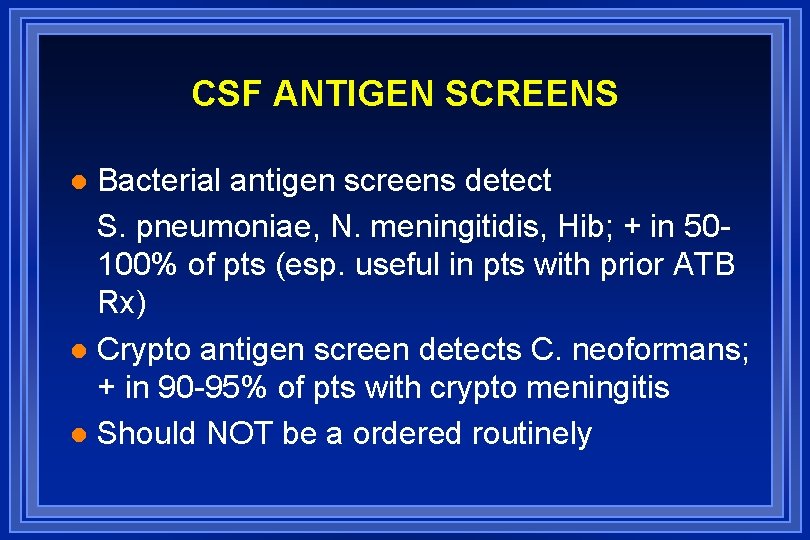
CSF ANTIGEN SCREENS Bacterial antigen screens detect S. pneumoniae, N. meningitidis, Hib; + in 50100% of pts (esp. useful in pts with prior ATB Rx) l Crypto antigen screen detects C. neoformans; + in 90 -95% of pts with crypto meningitis l Should NOT be a ordered routinely l

CEREBROSPINAL FLUID PROFILES Neutrophilic/Low glucose (purulent) Lymphocytic/Normal glucose Lymphocytic/Low glucose
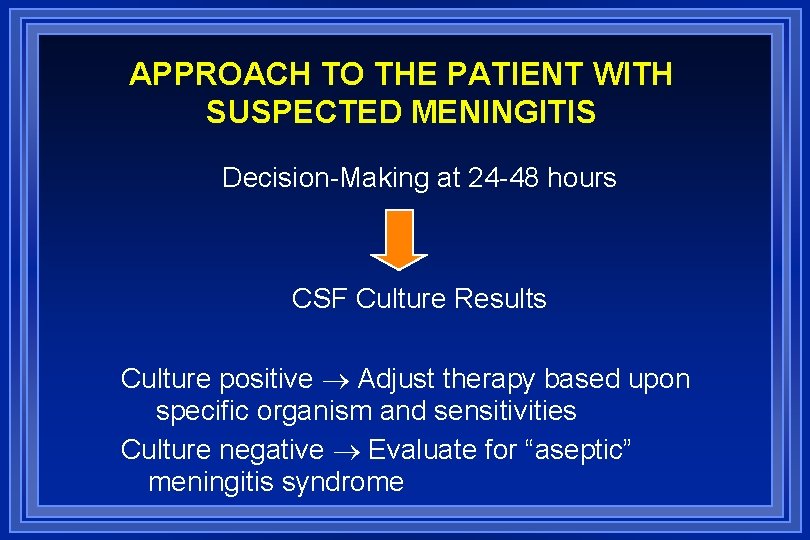
APPROACH TO THE PATIENT WITH SUSPECTED MENINGITIS Decision-Making at 24 -48 hours CSF Culture Results Culture positive Adjust therapy based upon specific organism and sensitivities Culture negative Evaluate for “aseptic” meningitis syndrome
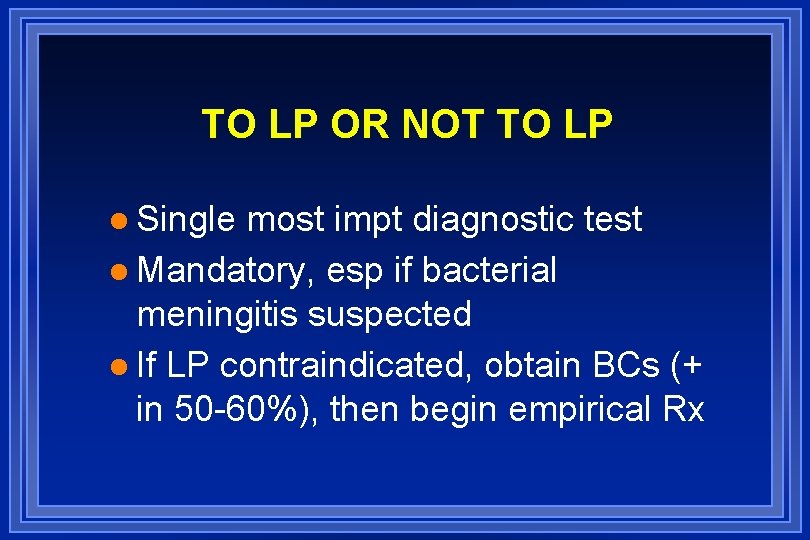
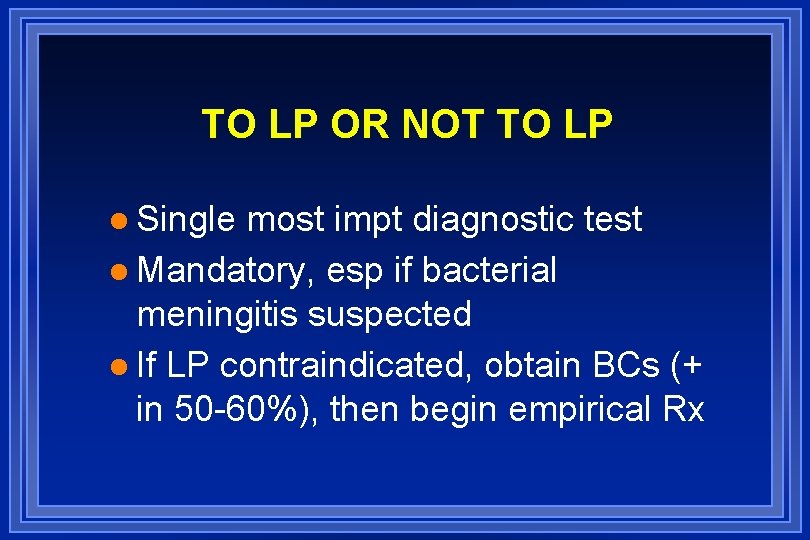
TO LP OR NOT TO LP l Single most impt diagnostic test l Mandatory, esp if bacterial meningitis suspected l If LP contraindicated, obtain BCs (+ in 50 -60%), then begin empirical Rx
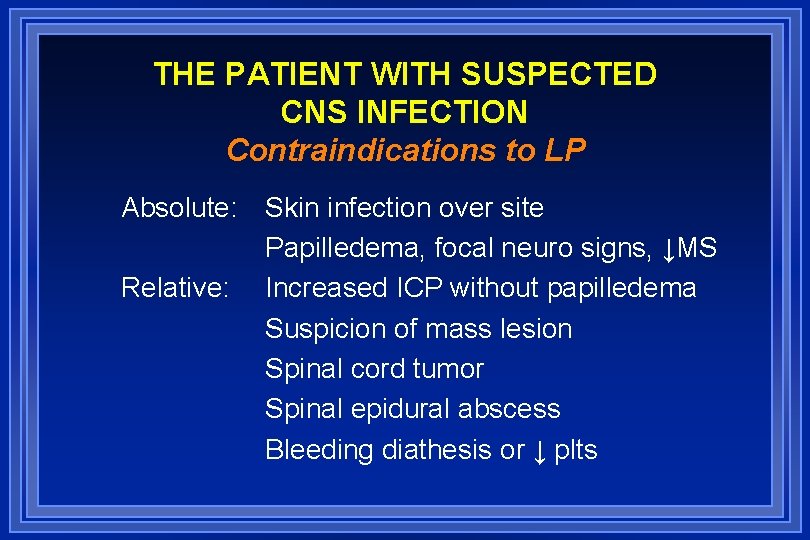
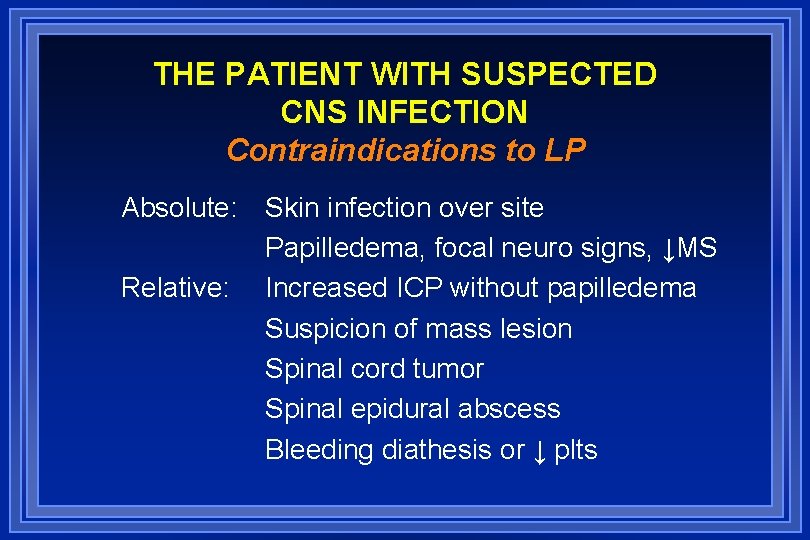
THE PATIENT WITH SUSPECTED CNS INFECTION Contraindications to LP Absolute: Skin infection over site Papilledema, focal neuro signs, ↓MS Relative: Increased ICP without papilledema Suspicion of mass lesion Spinal cord tumor Spinal epidural abscess Bleeding diathesis or ↓ plts
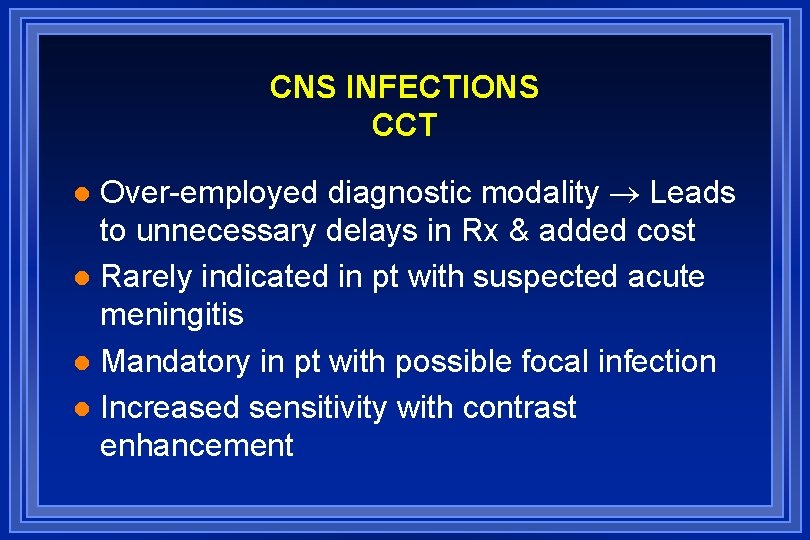
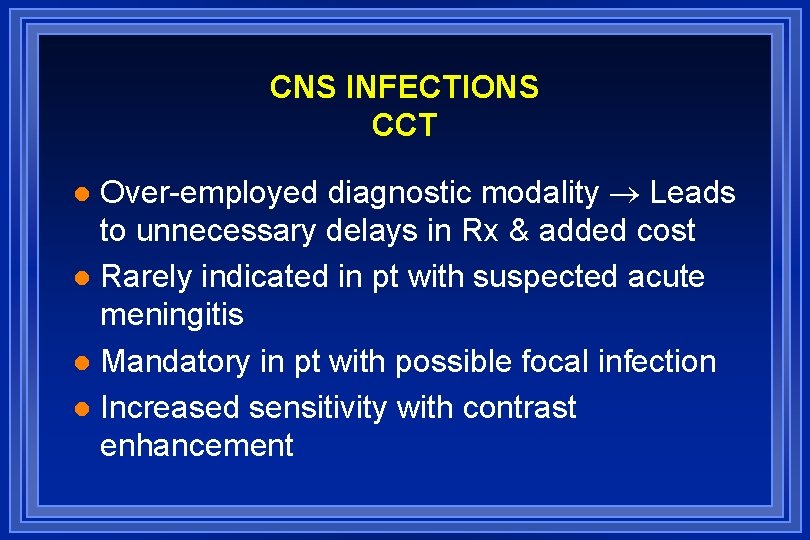
CNS INFECTIONS CCT Over-employed diagnostic modality Leads to unnecessary delays in Rx & added cost l Rarely indicated in pt with suspected acute meningitis l Mandatory in pt with possible focal infection l Increased sensitivity with contrast enhancement l

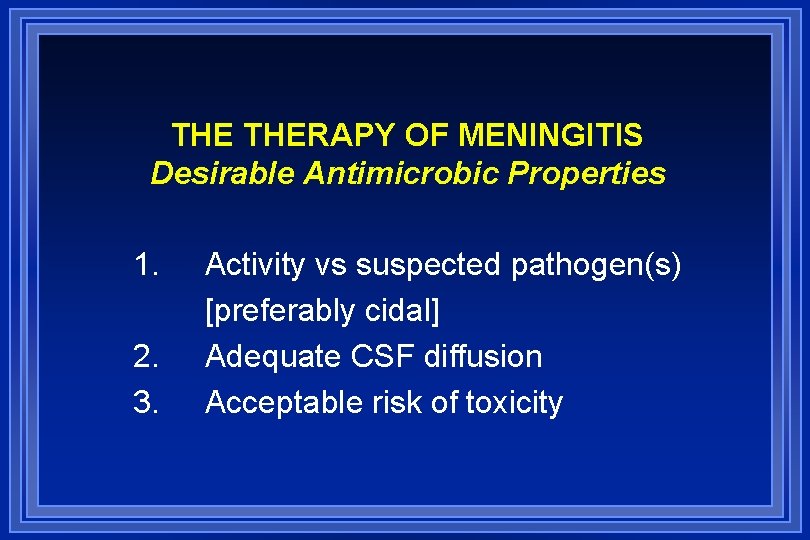
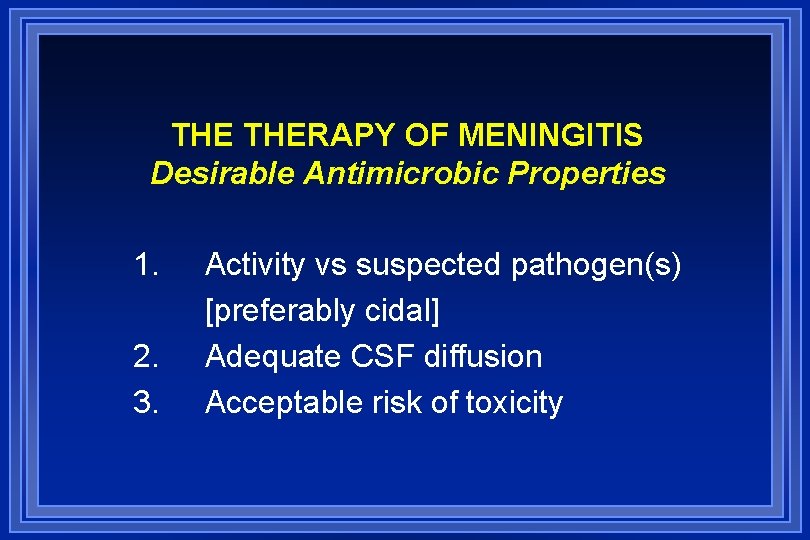
THE THERAPY OF MENINGITIS Desirable Antimicrobic Properties 1. 2. 3. Activity vs suspected pathogen(s) [preferably cidal] Adequate CSF diffusion Acceptable risk of toxicity
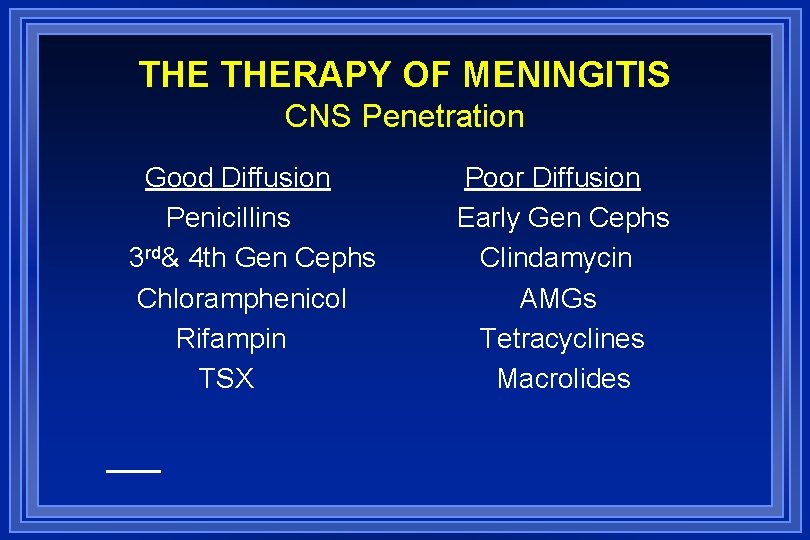
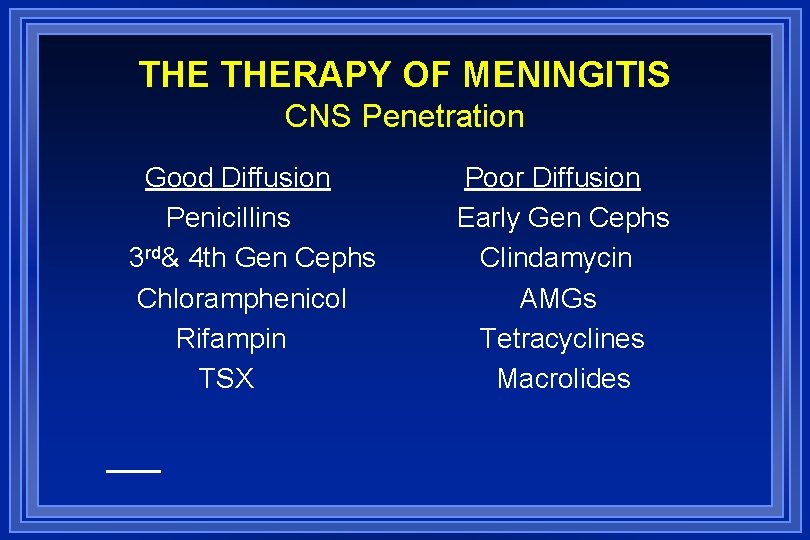
THE THERAPY OF MENINGITIS CNS Penetration Good Diffusion Penicillins 3 rd& 4 th Gen Cephs Chloramphenicol Rifampin TSX Poor Diffusion Early Gen Cephs Clindamycin AMGs Tetracyclines Macrolides
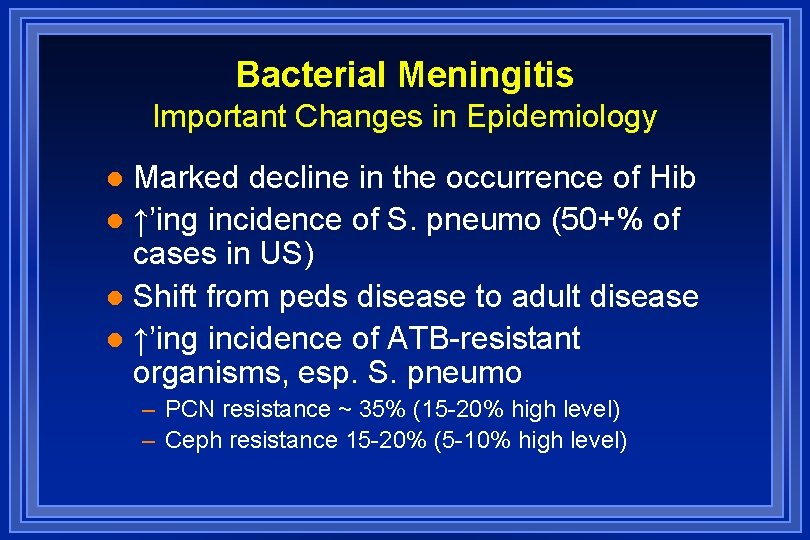
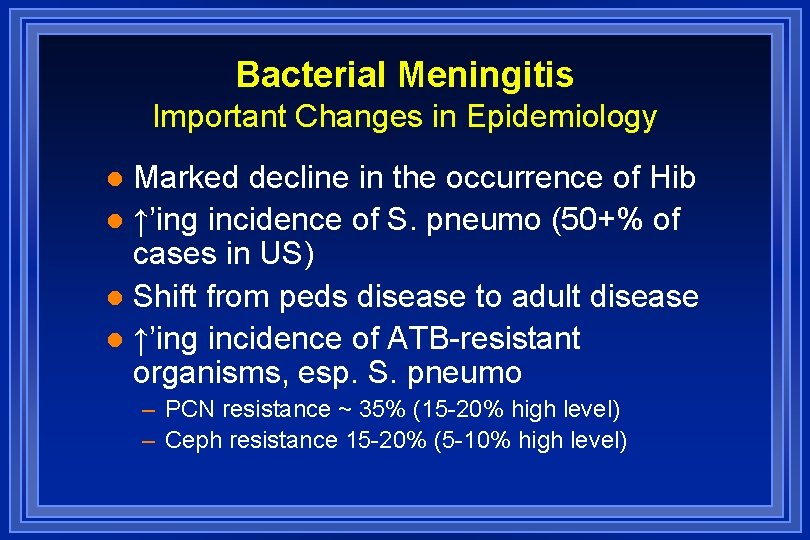
Bacterial Meningitis Important Changes in Epidemiology Marked decline in the occurrence of Hib l ↑’ing incidence of S. pneumo (50+% of cases in US) l Shift from peds disease to adult disease l ↑’ing incidence of ATB-resistant organisms, esp. S. pneumo l – PCN resistance ~ 35% (15 -20% high level) – Ceph resistance 15 -20% (5 -10% high level)
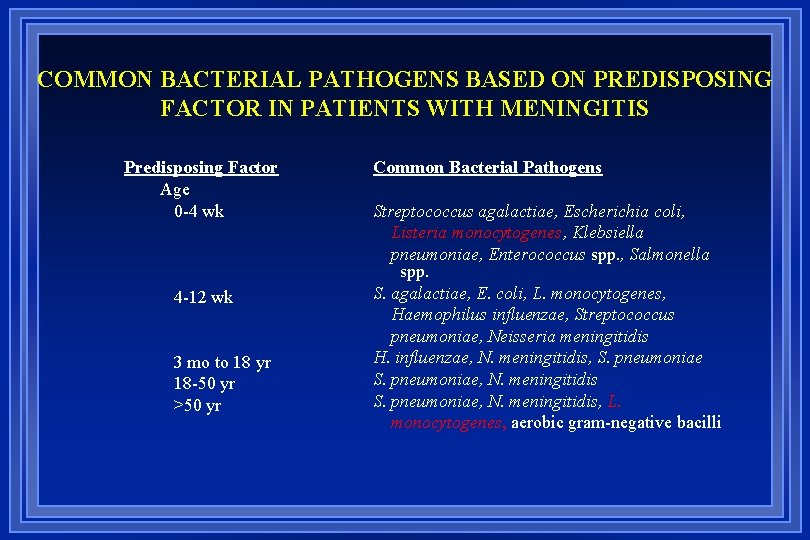
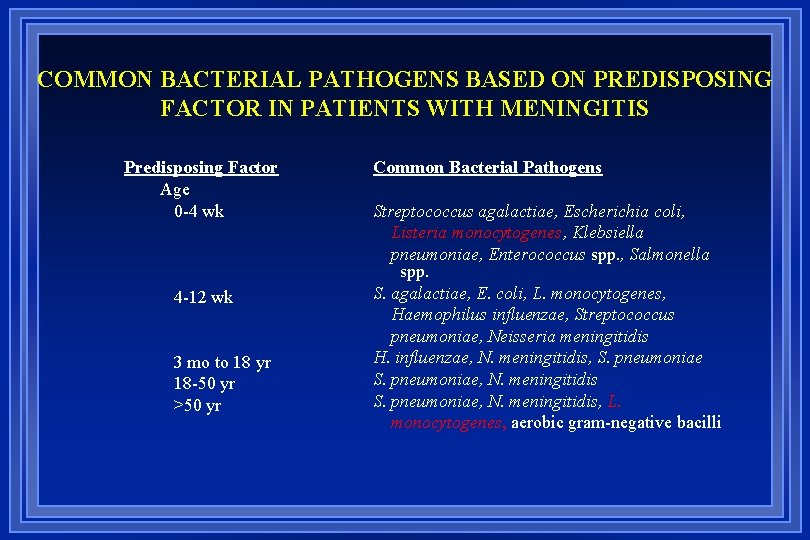
COMMON BACTERIAL PATHOGENS BASED ON PREDISPOSING FACTOR IN PATIENTS WITH MENINGITIS Predisposing Factor Age 0 -4 wk 4 -12 wk 3 mo to 18 yr 18 -50 yr >50 yr Common Bacterial Pathogens Streptococcus agalactiae, Escherichia coli, Listeria monocytogenes, Klebsiella pneumoniae, Enterococcus spp. , Salmonella spp. S. agalactiae, E. coli, L. monocytogenes, Haemophilus influenzae, Streptococcus pneumoniae, Neisseria meningitidis H. influenzae, N. meningitidis, S. pneumoniae, N. meningitidis, L. monocytogenes, aerobic gram-negative bacilli
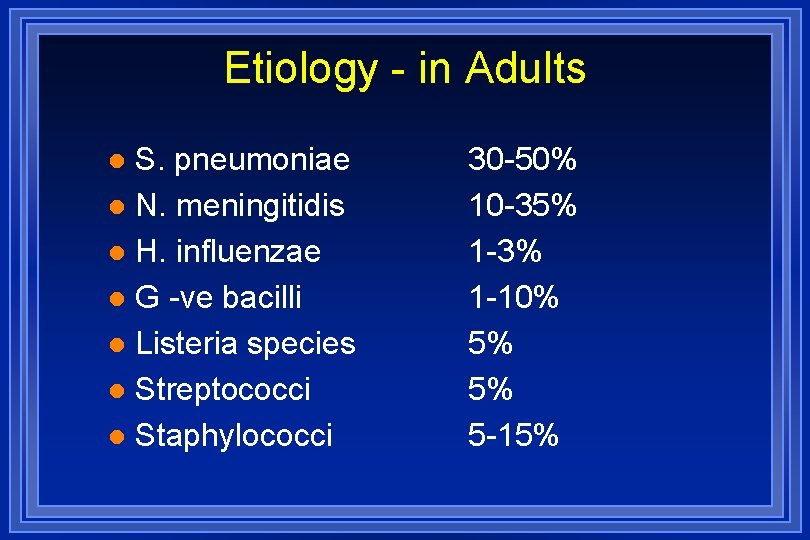
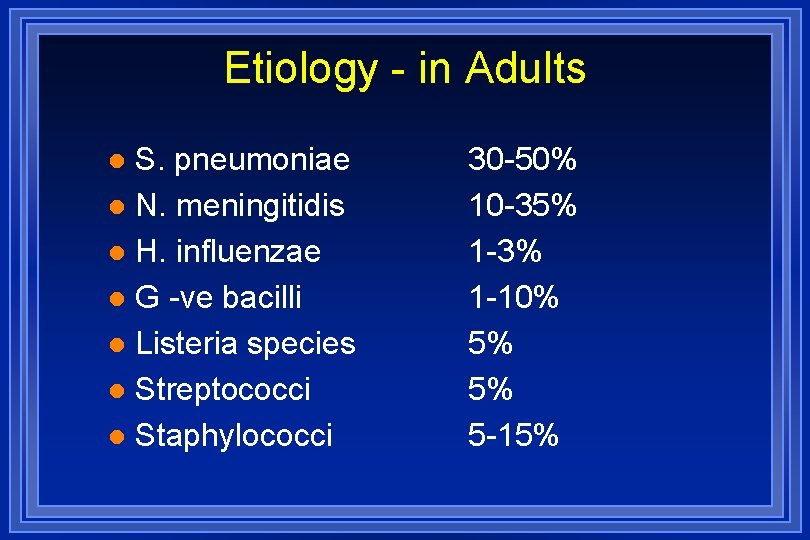
Etiology - in Adults S. pneumoniae l N. meningitidis l H. influenzae l G -ve bacilli l Listeria species l Streptococci l Staphylococci l 30 -50% 10 -35% 1 -3% 1 -10% 5% 5% 5 -15%
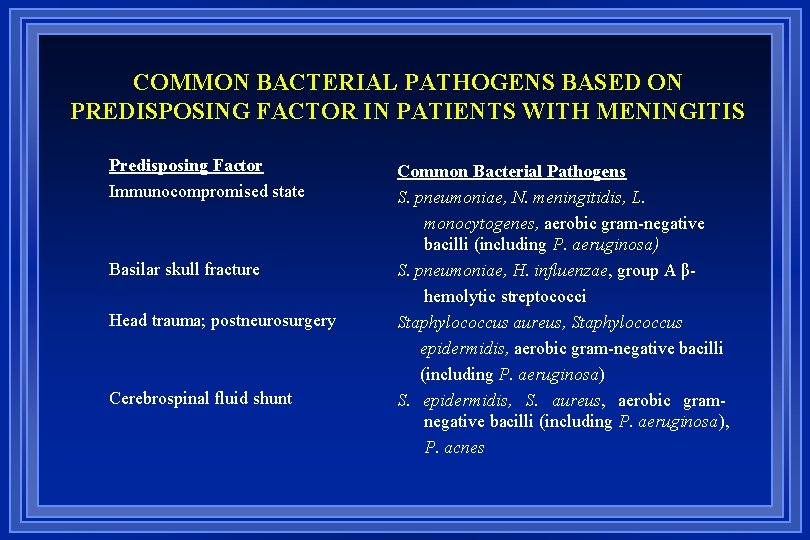
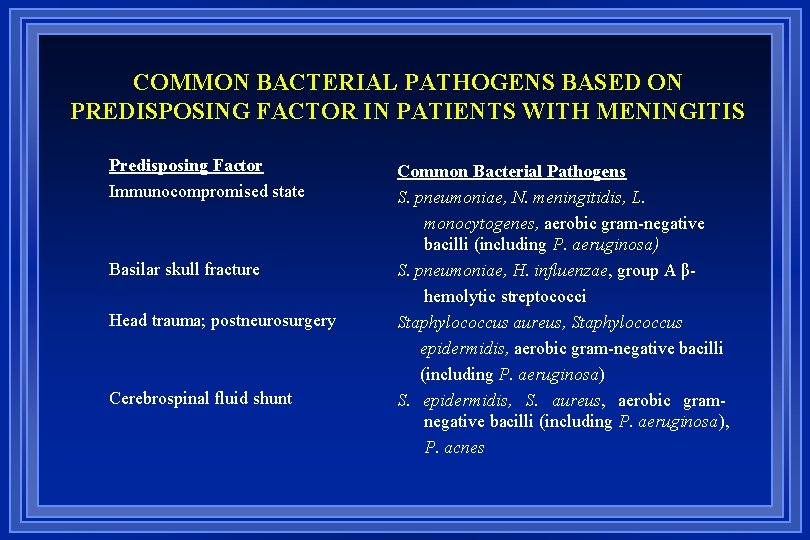
COMMON BACTERIAL PATHOGENS BASED ON PREDISPOSING FACTOR IN PATIENTS WITH MENINGITIS Predisposing Factor Immunocompromised state Basilar skull fracture Head trauma; postneurosurgery Cerebrospinal fluid shunt Common Bacterial Pathogens S. pneumoniae, N. meningitidis, L. monocytogenes, aerobic gram-negative bacilli (including P. aeruginosa) S. pneumoniae, H. influenzae, group A βhemolytic streptococci Staphylococcus aureus, Staphylococcus epidermidis, aerobic gram-negative bacilli (including P. aeruginosa) S. epidermidis, S. aureus, aerobic gramnegative bacilli (including P. aeruginosa), P. acnes
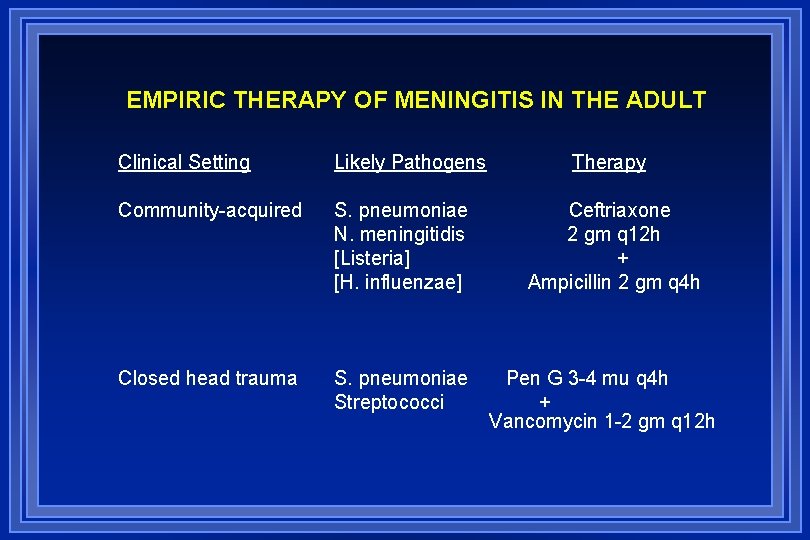
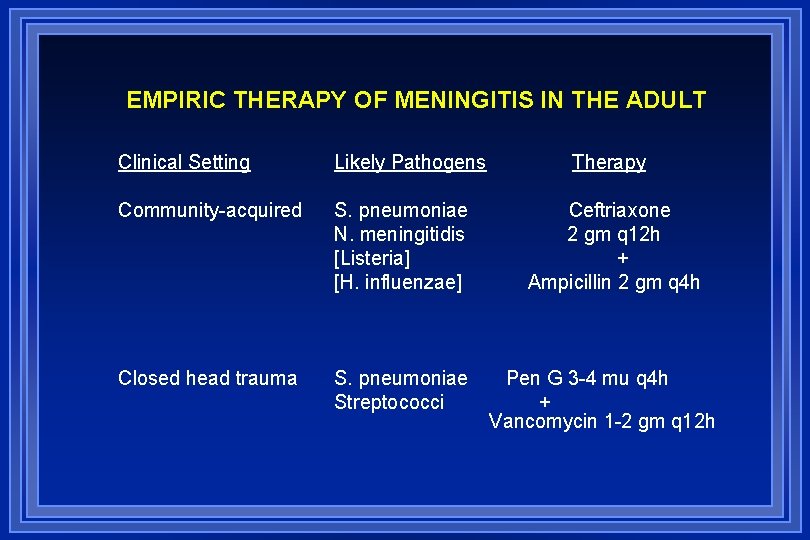
EMPIRIC THERAPY OF MENINGITIS IN THE ADULT Clinical Setting Likely Pathogens Community-acquired S. pneumoniae N. meningitidis [Listeria] [H. influenzae] Closed head trauma S. pneumoniae Streptococci Therapy Ceftriaxone 2 gm q 12 h + Ampicillin 2 gm q 4 h Pen G 3 -4 mu q 4 h + Vancomycin 1 -2 gm q 12 h
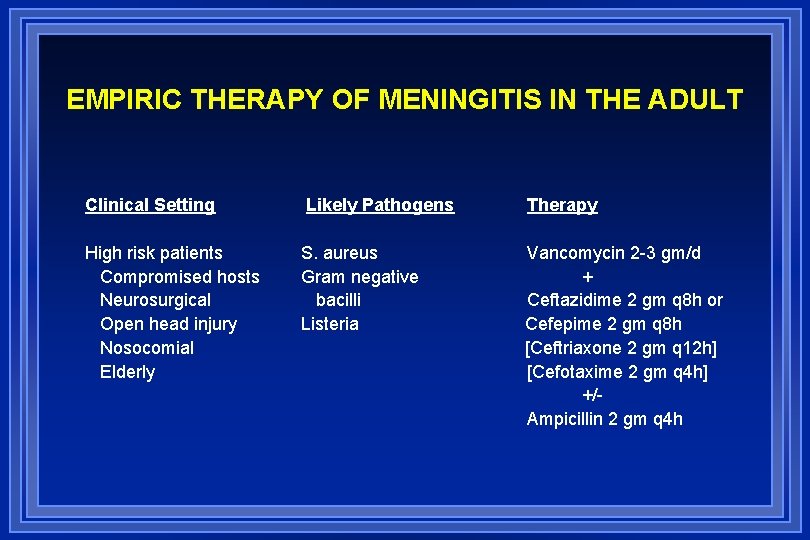
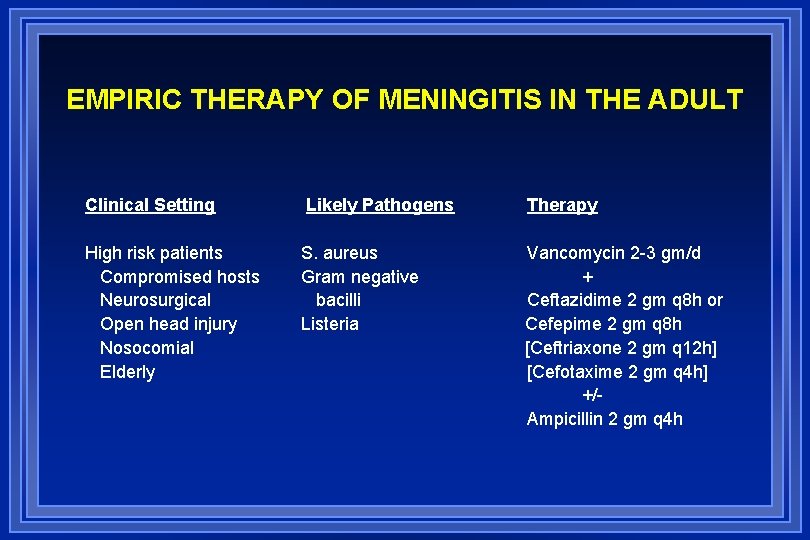
EMPIRIC THERAPY OF MENINGITIS IN THE ADULT Clinical Setting Likely Pathogens Therapy High risk patients Compromised hosts Neurosurgical Open head injury Nosocomial Elderly S. aureus Gram negative bacilli Listeria Vancomycin 2 -3 gm/d + Ceftazidime 2 gm q 8 h or Cefepime 2 gm q 8 h [Ceftriaxone 2 gm q 12 h] [Cefotaxime 2 gm q 4 h] +/Ampicillin 2 gm q 4 h
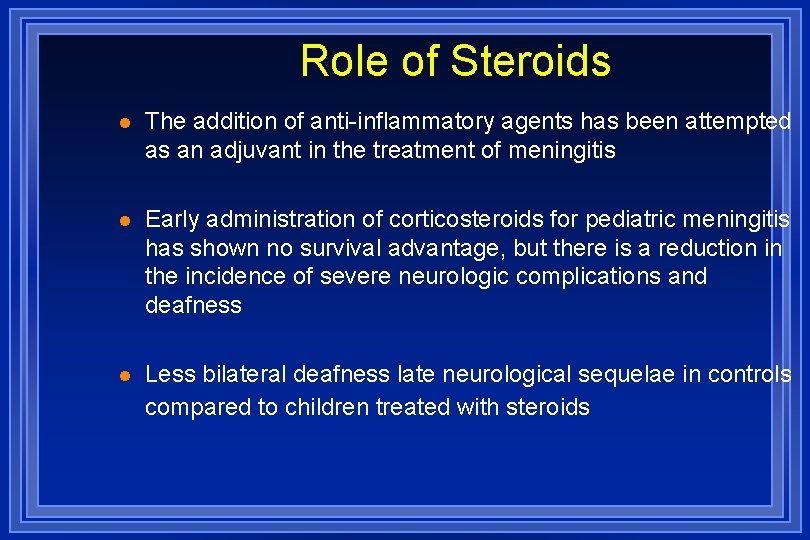
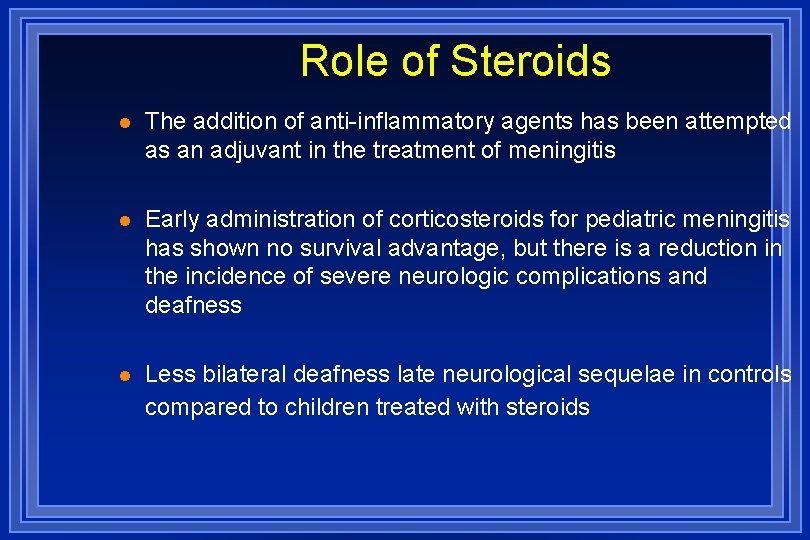
Role of Steroids l The addition of anti-inflammatory agents has been attempted as an adjuvant in the treatment of meningitis l Early administration of corticosteroids for pediatric meningitis has shown no survival advantage, but there is a reduction in the incidence of severe neurologic complications and deafness l Less bilateral deafness late neurological sequelae in controls compared to children treated with steroids

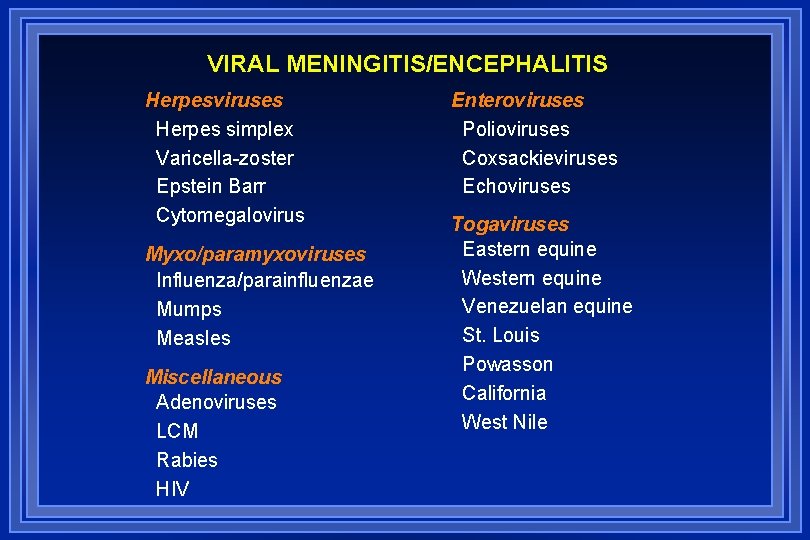
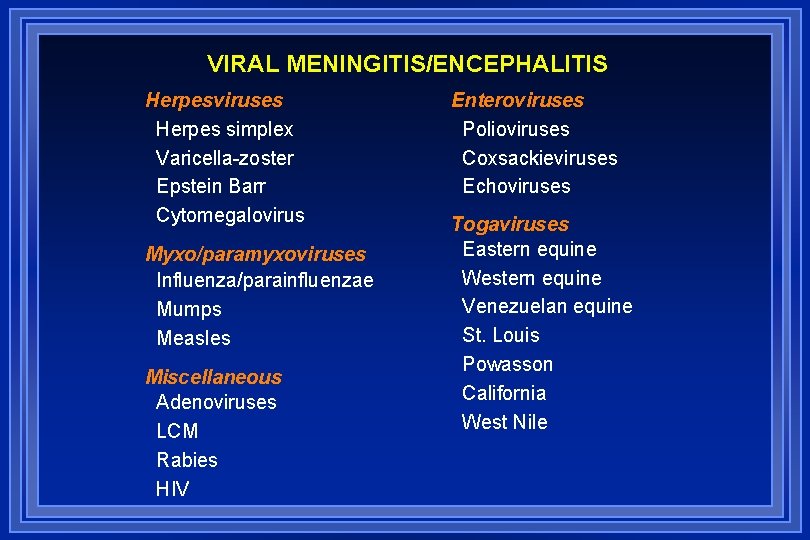
VIRAL MENINGITIS/ENCEPHALITIS Herpesviruses Herpes simplex Varicella-zoster Epstein Barr Cytomegalovirus Myxo/paramyxoviruses Influenza/parainfluenzae Mumps Measles Miscellaneous Adenoviruses LCM Rabies HIV Enteroviruses Polioviruses Coxsackieviruses Echoviruses Togaviruses Eastern equine Western equine Venezuelan equine St. Louis Powasson California West Nile

37 y/male Headache, spontaneous tendency to sleep, Mental changes: unrecognising time and location, Dx?
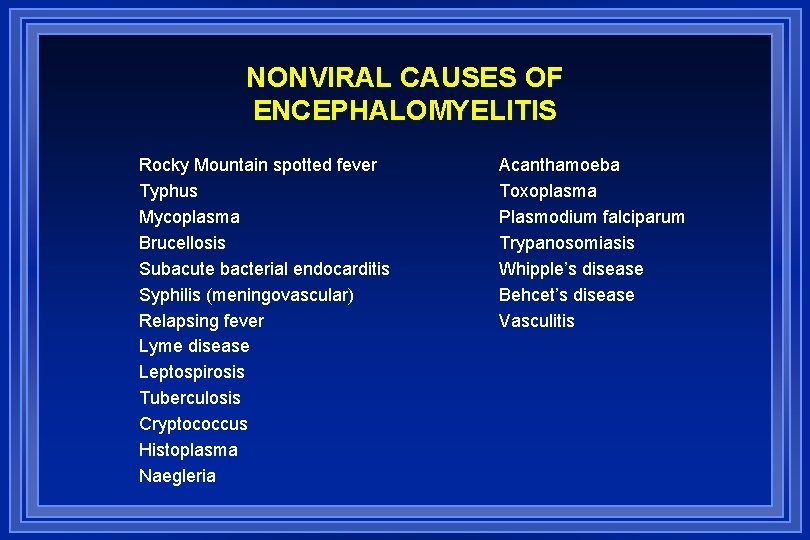
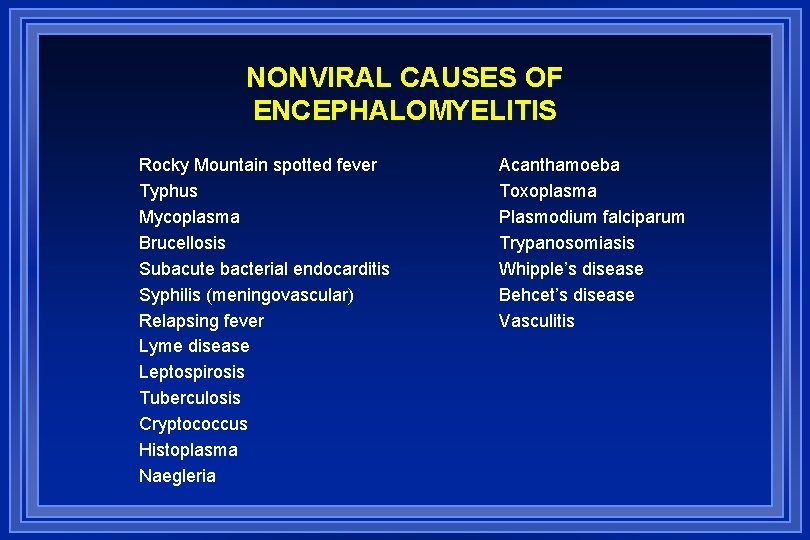
NONVIRAL CAUSES OF ENCEPHALOMYELITIS Rocky Mountain spotted fever Typhus Mycoplasma Brucellosis Subacute bacterial endocarditis Syphilis (meningovascular) Relapsing fever Lyme disease Leptospirosis Tuberculosis Cryptococcus Histoplasma Naegleria Acanthamoeba Toxoplasma Plasmodium falciparum Trypanosomiasis Whipple’s disease Behcet’s disease Vasculitis
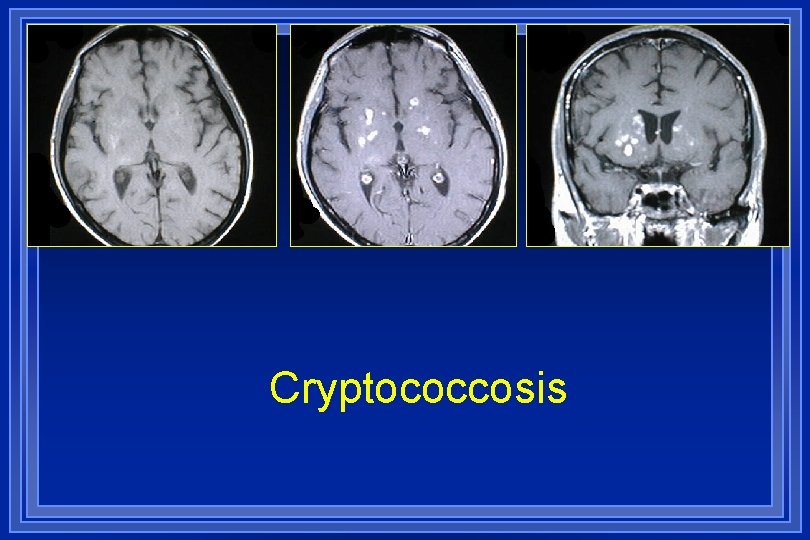
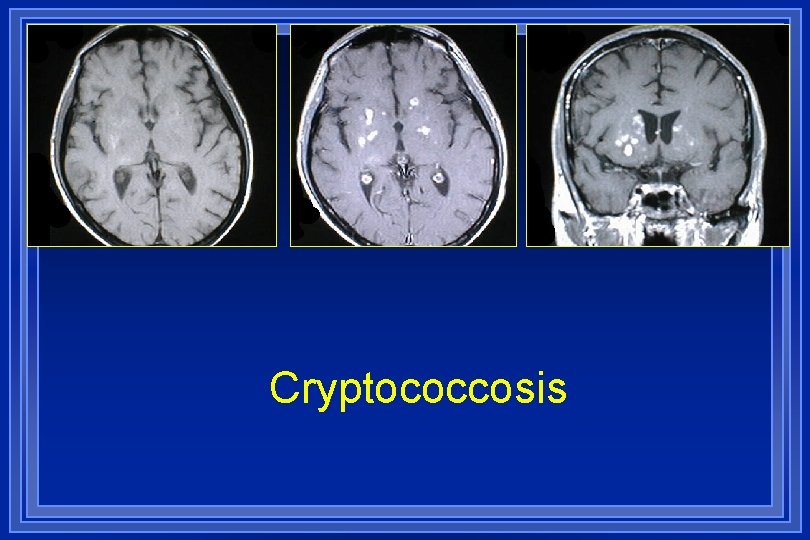
Cryptococcosis
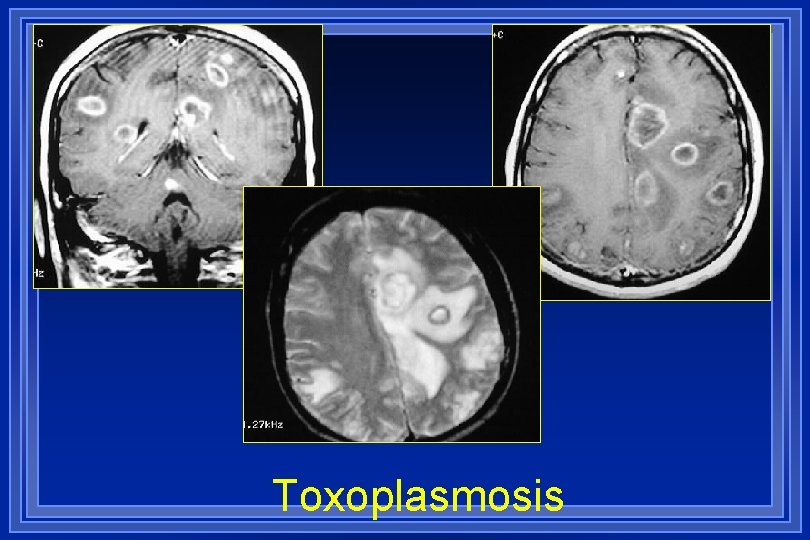
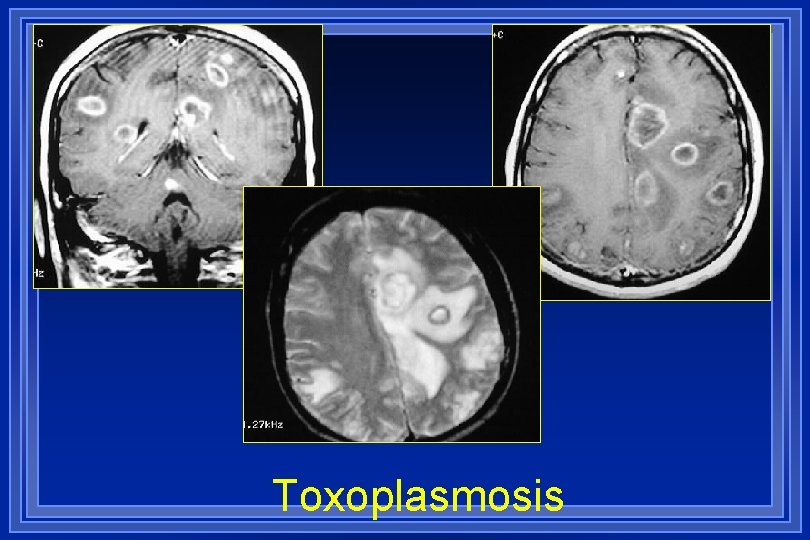
Toxoplasmosis

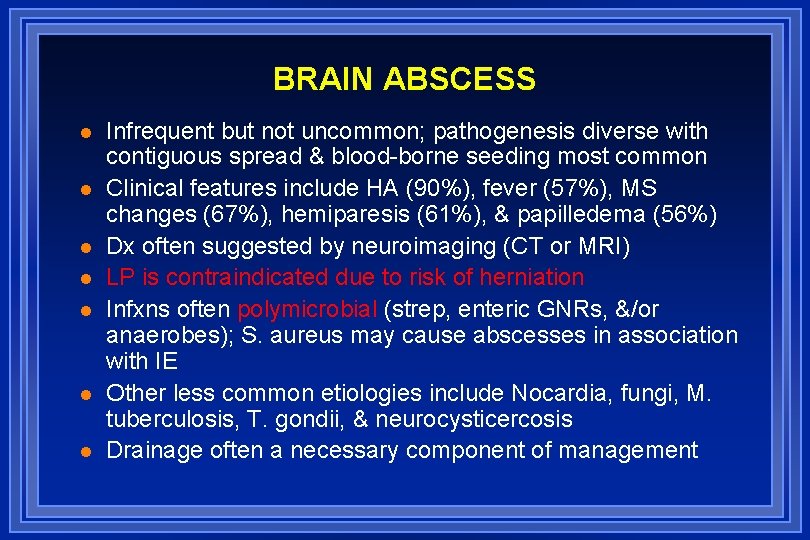
BRAIN ABSCESS l l l l Infrequent but not uncommon; pathogenesis diverse with contiguous spread & blood-borne seeding most common Clinical features include HA (90%), fever (57%), MS changes (67%), hemiparesis (61%), & papilledema (56%) Dx often suggested by neuroimaging (CT or MRI) LP is contraindicated due to risk of herniation Infxns often polymicrobial (strep, enteric GNRs, &/or anaerobes); S. aureus may cause abscesses in association with IE Other less common etiologies include Nocardia, fungi, M. tuberculosis, T. gondii, & neurocysticercosis Drainage often a necessary component of management

Multiple abscesses in a 6 -yearold child
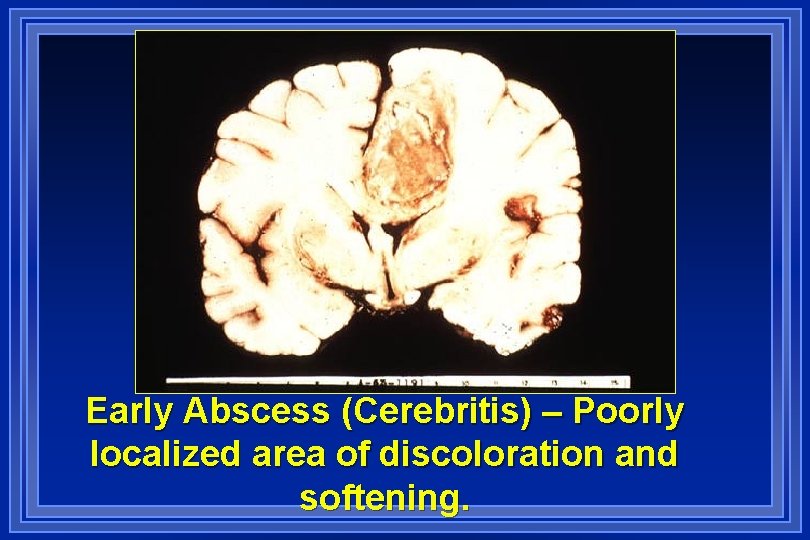
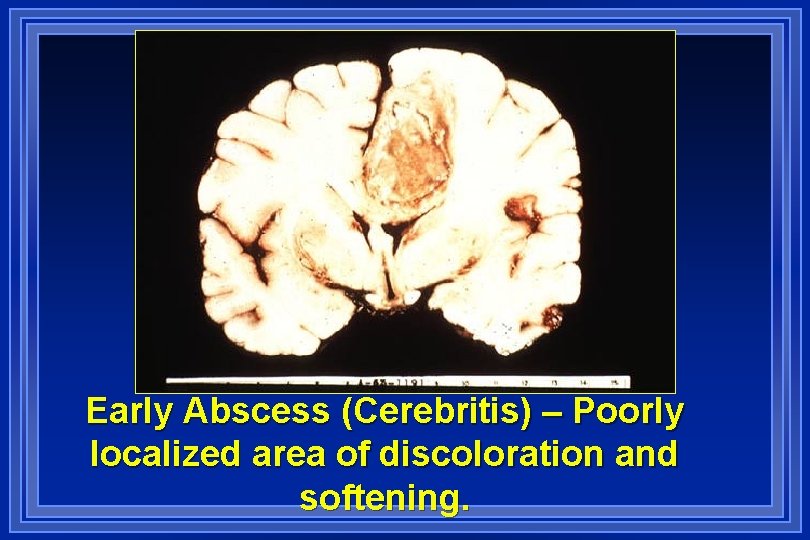
Early Abscess (Cerebritis) – Poorly localized area of discoloration and softening.
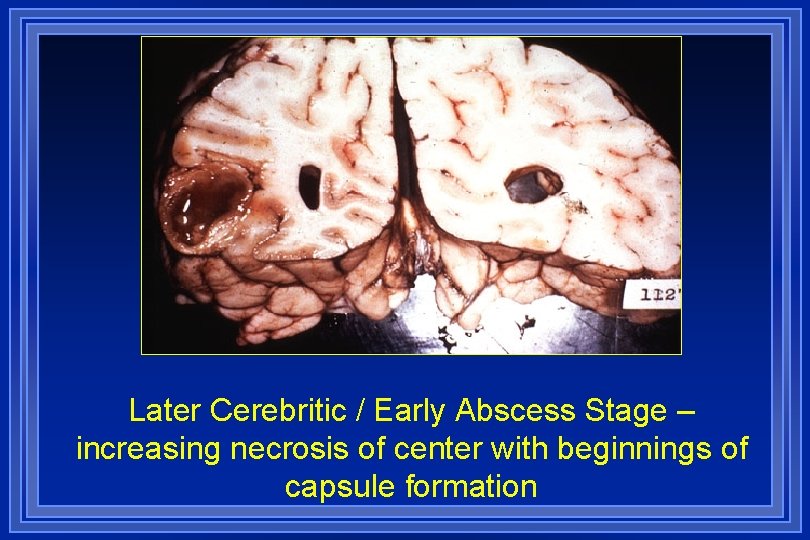
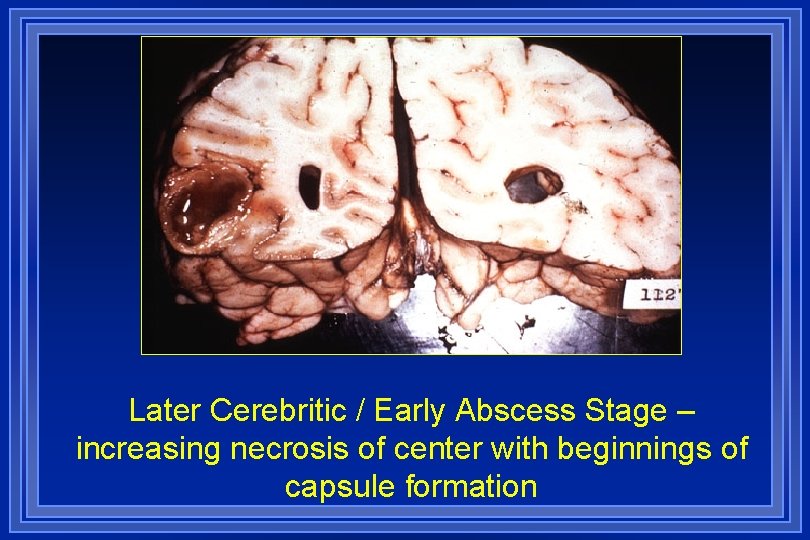
Later Cerebritic / Early Abscess Stage – increasing necrosis of center with beginnings of capsule formation
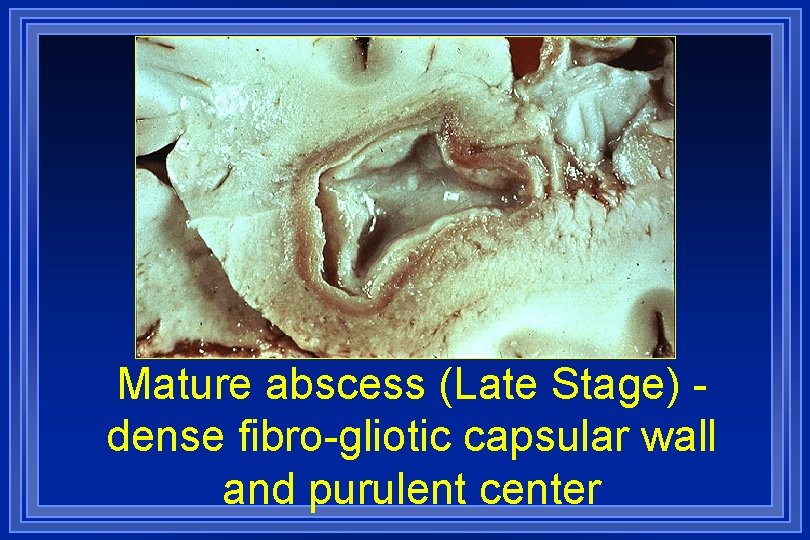
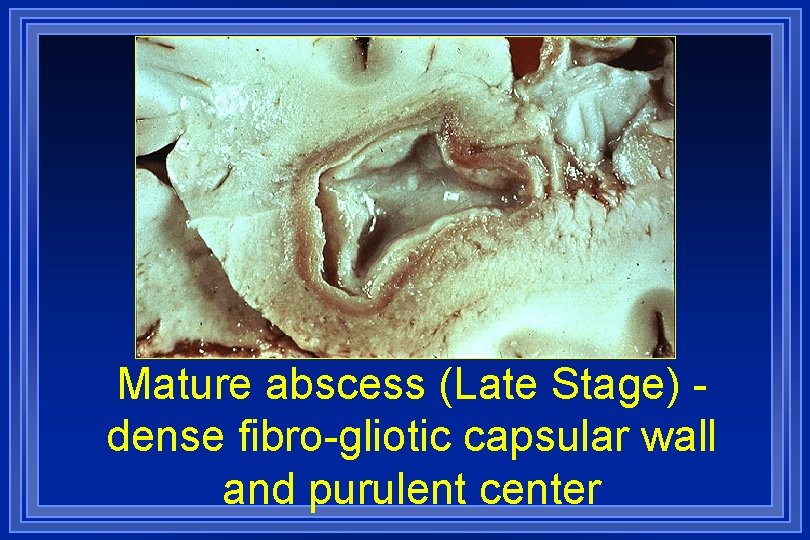
Mature abscess (Late Stage) dense fibro-gliotic capsular wall and purulent center
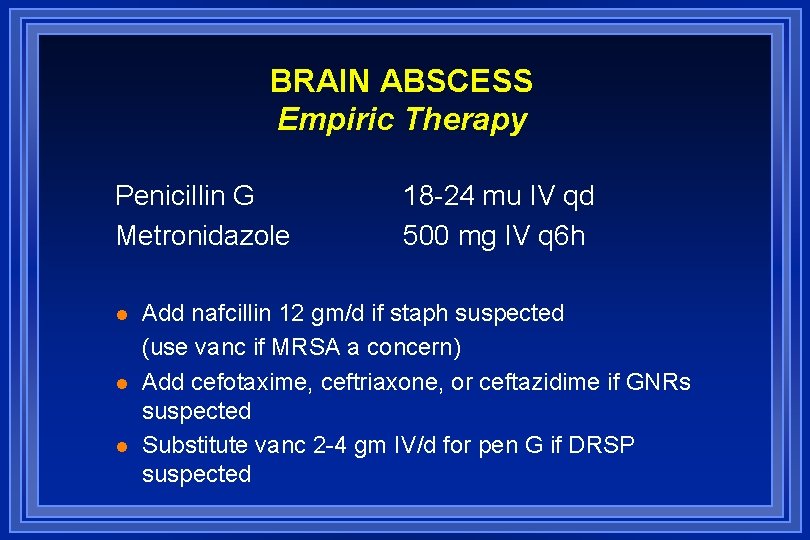
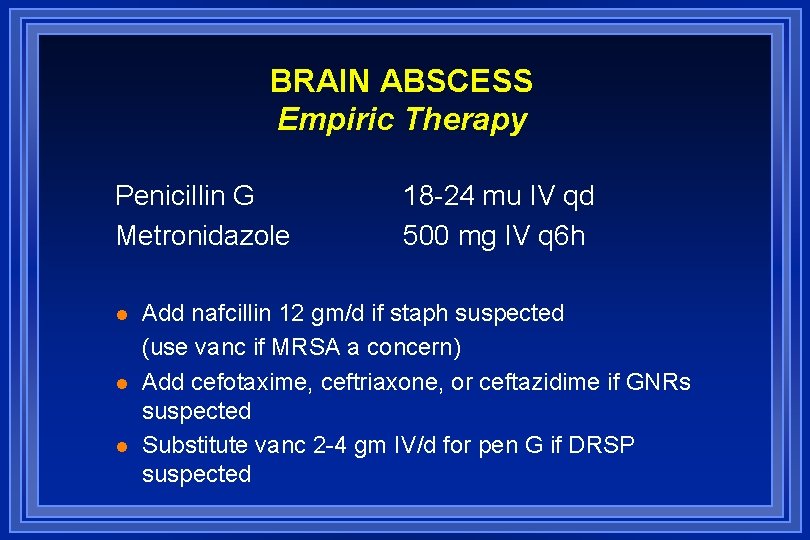
BRAIN ABSCESS Empiric Therapy Penicillin G Metronidazole l l l 18 -24 mu IV qd 500 mg IV q 6 h Add nafcillin 12 gm/d if staph suspected (use vanc if MRSA a concern) Add cefotaxime, ceftriaxone, or ceftazidime if GNRs suspected Substitute vanc 2 -4 gm IV/d for pen G if DRSP suspected
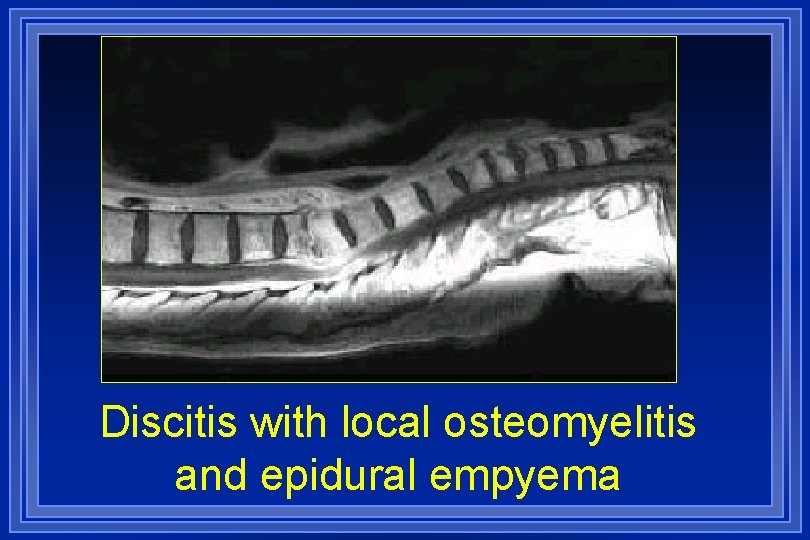
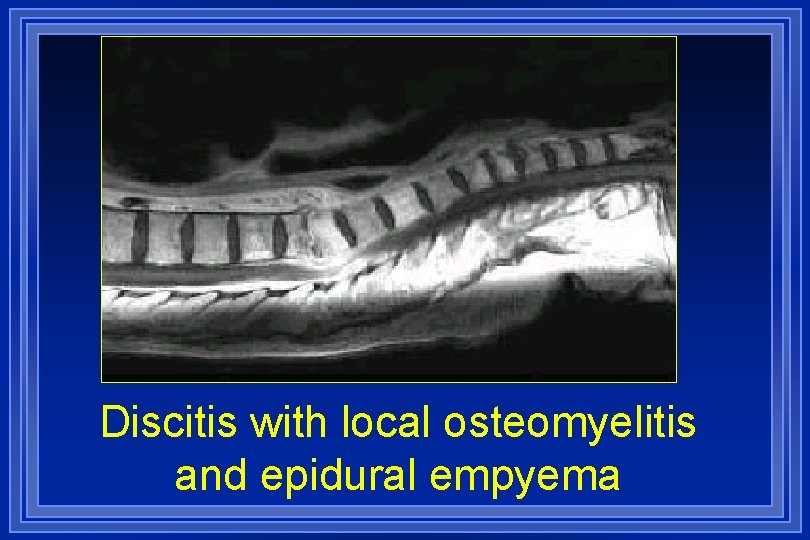
Discitis with local osteomyelitis and epidural empyema
 Big asd fans
Big asd fans Eye infections
Eye infections Opportunistic infections
Opportunistic infections Opsonization
Opsonization Genital infections
Genital infections Storch infections
Storch infections Postpartum infections
Postpartum infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Acute gingival infections
Acute gingival infections Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Johnson and johnson botnet infections
Johnson and johnson botnet infections Neurosiphyllis
Neurosiphyllis Methotrexate yeast infection
Methotrexate yeast infection Genital infections
Genital infections Storch infections
Storch infections Depresori cns
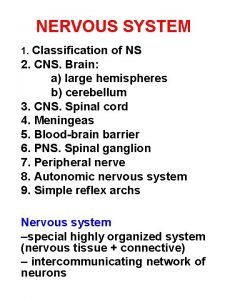
Depresori cns Structure of the reflex arc
Structure of the reflex arc Grading of reflexes
Grading of reflexes Depresori cns
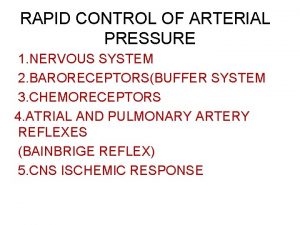
Depresori cns Cns ischemic response
Cns ischemic response Pagitane
Pagitane Cns
Cns Cns ward
Cns ward Ans and cns difference
Ans and cns difference Cns ischemic response
Cns ischemic response Cns15506
Cns15506 Classification of cns
Classification of cns Cns and sns
Cns and sns Cns ischemic response
Cns ischemic response Cns-cp
Cns-cp Cns educar
Cns educar Cns
Cns Cns depressants ppt
Cns depressants ppt Cns international school
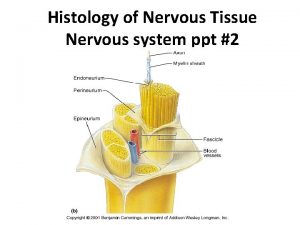
Cns international school Nervous tissue ppt
Nervous tissue ppt Soma cns
Soma cns Cns summer school
Cns summer school Bainbridge reflex
Bainbridge reflex Cns 2779-1
Cns 2779-1 Reeling gait
Reeling gait Central nervous
Central nervous Cns poruchy
Cns poruchy Cns
Cns