CNS Drug Delivery Beyond the Spinal Cord Mission
CNS Drug Delivery: Beyond the Spinal Cord Mission: Improve outcomes for epileptic patients who don’t respond to conventional treatments by administering reformulated, microdoses of anti-epileptic drugs directly to the brain. Daniel J. Abrams, MD December 2012
Disclaimer on Product Use • This presentation includes the description of drugs, devices and their therapeutic uses that are in early stages of development, are not commercially available and have not been approved by regulatory institutions. • Before commercialization is possible the drugs, devices and their therapeutic uses need to undergo additional preclinical and clinical evaluation and obtain regulatory approval.
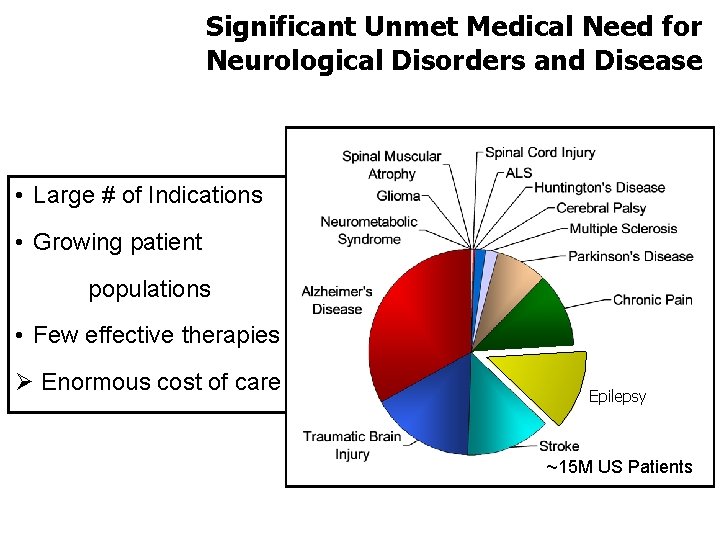
Significant Unmet Medical Need for Neurological Disorders and Disease • Large # of Indications • Growing patient populations • Few effective therapies Ø Enormous cost of care Epilepsy ~15 M US Patients
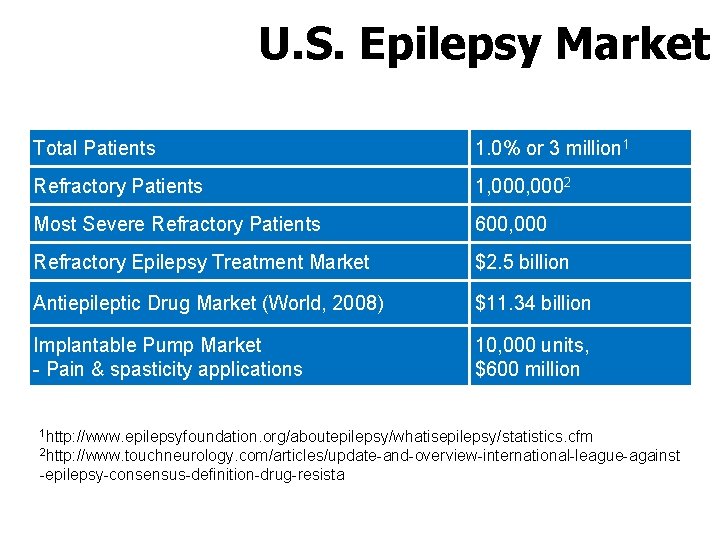
U. S. Epilepsy Market Total Patients 1. 0% or 3 million 1 Refractory Patients 1, 0002 Most Severe Refractory Patients 600, 000 Refractory Epilepsy Treatment Market $2. 5 billion Antiepileptic Drug Market (World, 2008) $11. 34 billion Implantable Pump Market - Pain & spasticity applications 10, 000 units, $600 million 1 http: //www. epilepsyfoundation. org/aboutepilepsy/whatisepilepsy/statistics. cfm 2 http: //www. touchneurology. com/articles/update-and-overview-international-league-against -epilepsy-consensus-definition-drug-resista
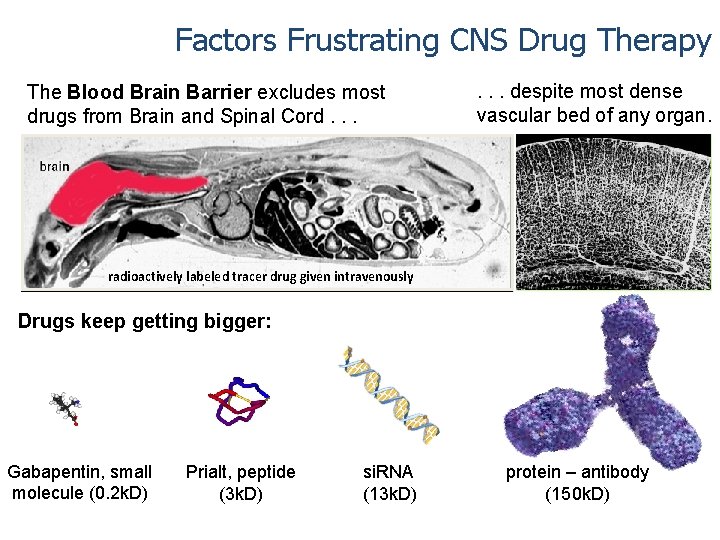
Factors Frustrating CNS Drug Therapy The Blood Brain Barrier excludes most drugs from Brain and Spinal Cord. . . despite most dense vascular bed of any organ. * radioactively labeled tracer drug given intravenously Drugs keep getting bigger: Gabapentin, small molecule (0. 2 k. D) Prialt, peptide (3 k. D) si. RNA (13 k. D) protein – antibody (150 k. D)
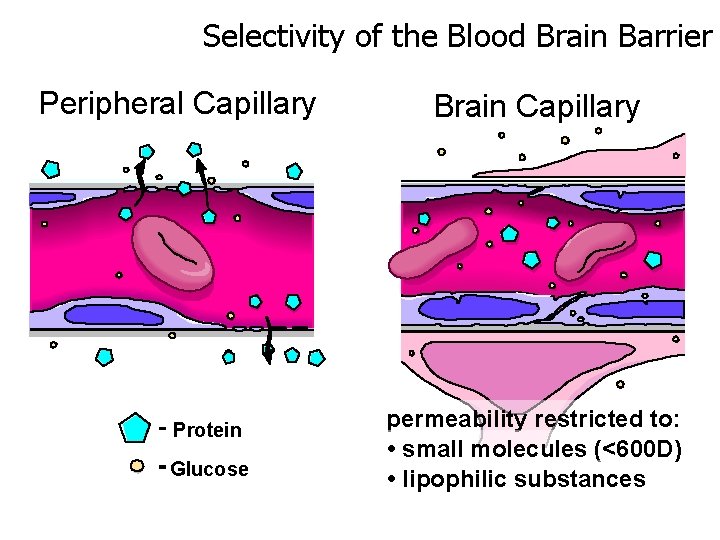
Selectivity of the Blood Brain Barrier Peripheral Capillary Protein Glucose Brain Capillary permeability restricted to: • small molecules (<600 D) • lipophilic substances
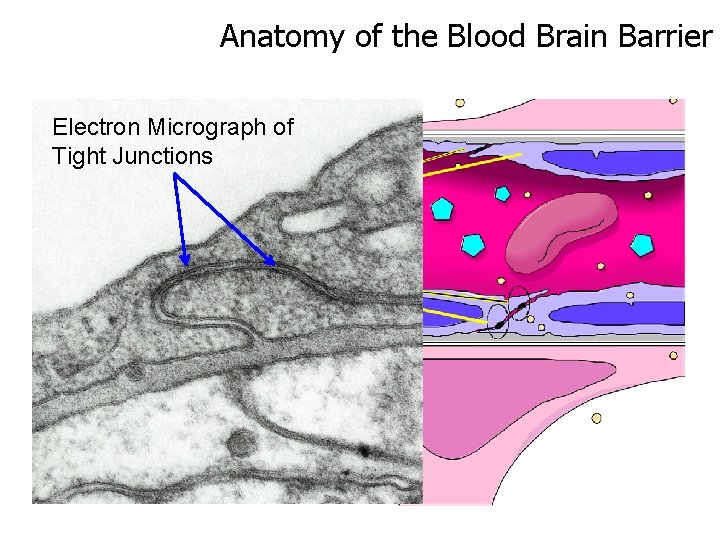
Anatomy of the Blood Brain Barrier Electron Micrograph of Tight Junctions
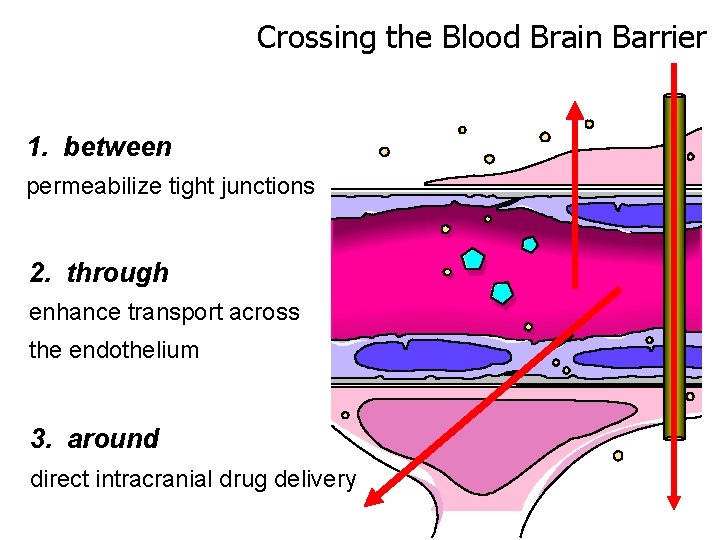
Crossing the Blood Brain Barrier 1. between permeabilize tight junctions 2. through enhance transport across the endothelium 3. around direct intracranial drug delivery
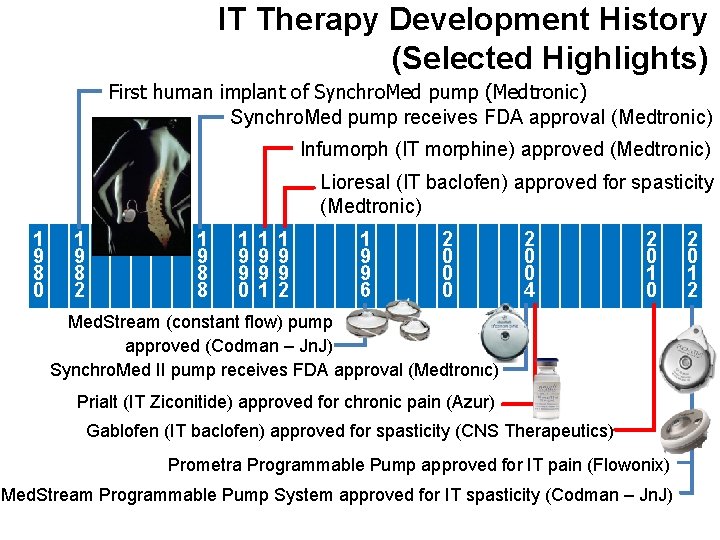
IT Therapy Development History (Selected Highlights) First human implant of Synchro. Med pump (Medtronic) Synchro. Med pump receives FDA approval (Medtronic) Infumorph (IT morphine) approved (Medtronic) Lioresal (IT baclofen) approved for spasticity (Medtronic) 1 9 8 0 1 9 8 2 1 9 8 8 1 9 9 0 1 9 9 1 1 9 9 2 1 9 9 6 2 0 0 0 2 0 0 4 2 0 1 0 Med. Stream (constant flow) pump approved (Codman – Jn. J) Synchro. Med II pump receives FDA approval (Medtronic) Prialt (IT Ziconitide) approved for chronic pain (Azur) Gablofen (IT baclofen) approved for spasticity (CNS Therapeutics) Prometra Programmable Pump approved for IT pain (Flowonix) Med. Stream Programmable Pump System approved for IT spasticity (Codman – Jn. J) 2 0 1 2

Several Infusion Systems Available for Targeted Drug Delivery MEDSTREAM™ Programmable Infusion Pump and Control Unit Prometra Pump and Programmer Synchro. Med II Infusion Pump & N’vision Clinical Programmer

Common Features of Implantable Drug Infusion Systems Catheter Access Port – bypasses drug reservoir, used to check for catheter patency Reservoir Refill Port – septum through which drug enters the pump upon refill Titanium Housing – typically rigid outer housing that protects pump from mechanical damage Programmer – used Drug Catheter – flexible tubing that runs from the pump with special tip for drug delivery with ‘smart’ pumps, controls drug infusion rate, records drug history Medtronic Synchro. Med® II pump and N’Vision® Programmer shown above
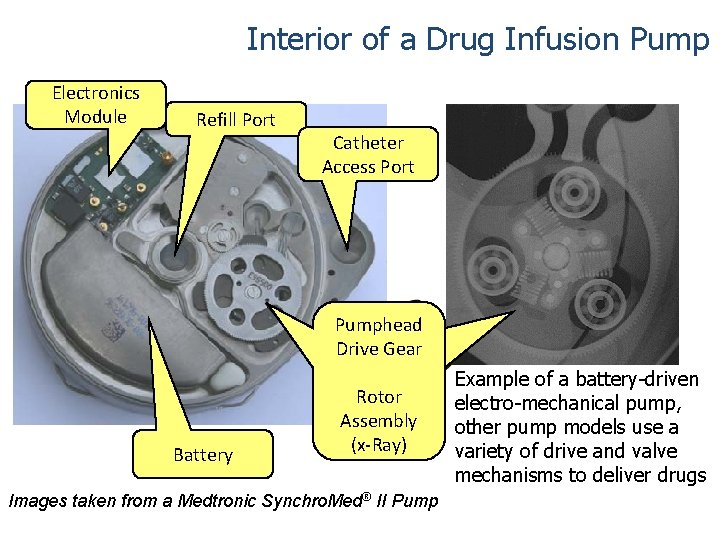
Interior of a Drug Infusion Pump Electronics Module Refill Port Battery Catheter Access Port Pumphead d a Drive Gear e ar h p Ge m u e Rotor P riv D Assembly (x-Ray) Images taken from a Medtronic Synchro. Med® II Pump Example of a battery-driven electro-mechanical pump, other pump models use a variety of drive and valve mechanisms to deliver drugs

Flowonix Prometra - Pain Infusion System Features: • Dose Accuracy – 98% • Longevity – >10 years • Weight – 10% lighter • Easy refill • Designed to deliver any compound • Can deliver micro-doses • Can be programmed off
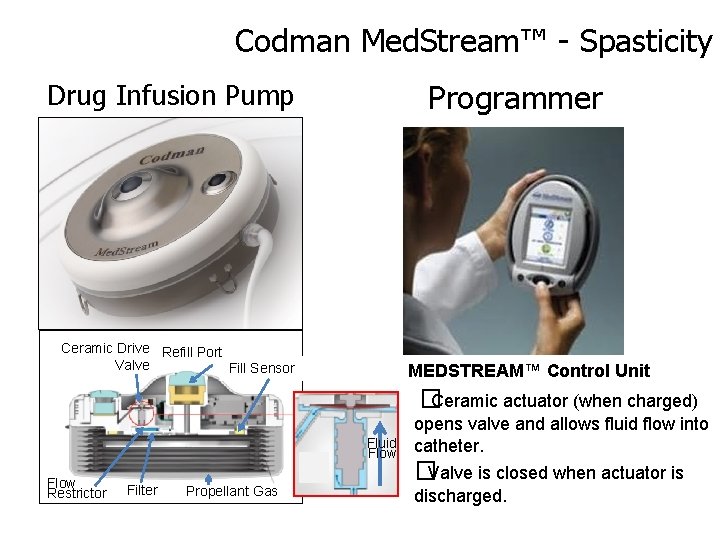
Codman Med. Stream™ - Spasticity Drug Infusion Pump Programmer Ceramic Drive Refill Port Valve Fill Sensor MEDSTREAM™ Control Unit Fluid Flow Restrictor Filter Propellant Gas � Ceramic actuator (when charged) opens valve and allows fluid flow into catheter. � Valve is closed when actuator is discharged.
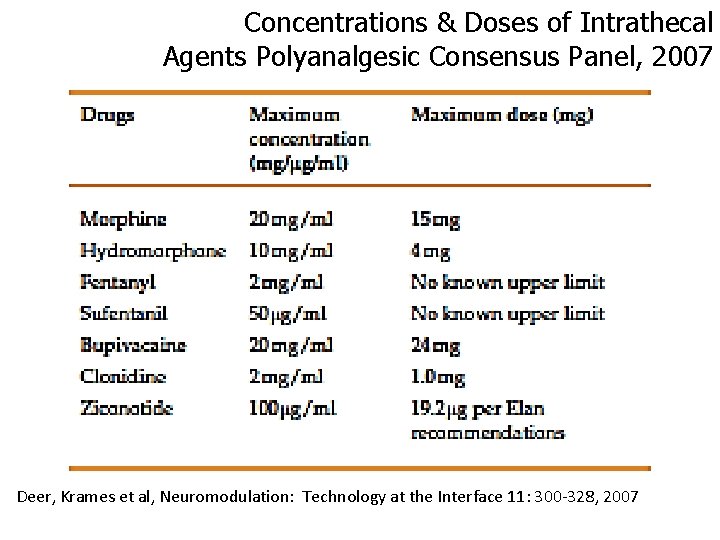
Concentrations & Doses of Intrathecal Agents Polyanalgesic Consensus Panel, 2007 Deer, Krames et al, Neuromodulation: Technology at the Interface 11: 300 -328, 2007
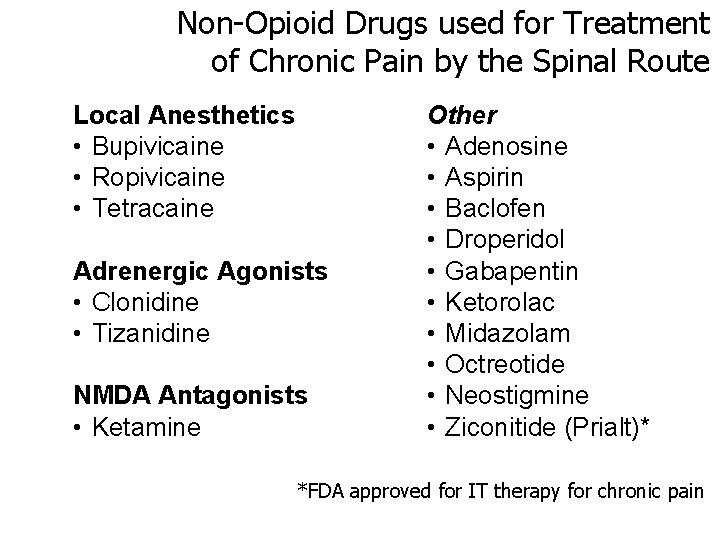
Non-Opioid Drugs used for Treatment of Chronic Pain by the Spinal Route Local Anesthetics • Bupivicaine • Ropivicaine • Tetracaine Adrenergic Agonists • Clonidine • Tizanidine NMDA Antagonists • Ketamine Other • Adenosine • Aspirin • Baclofen • Droperidol • Gabapentin • Ketorolac • Midazolam • Octreotide • Neostigmine • Ziconitide (Prialt)* *FDA approved for IT therapy for chronic pain
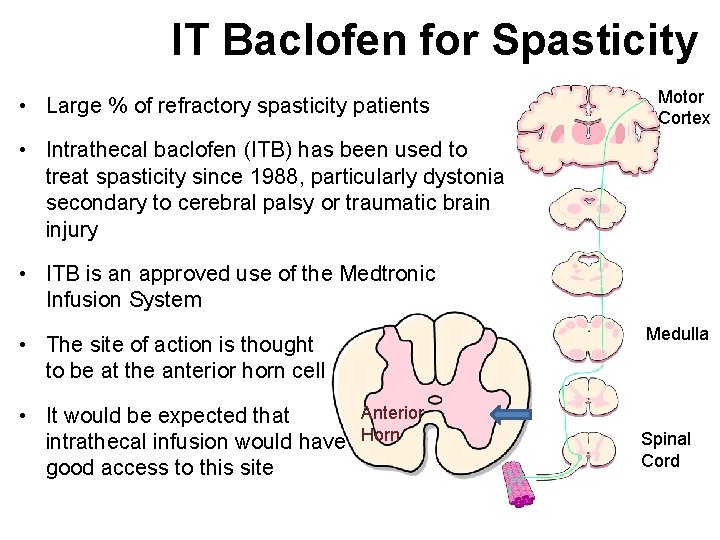
IT Baclofen for Spasticity • Large % of refractory spasticity patients Motor Cortex • Intrathecal baclofen (ITB) has been used to treat spasticity since 1988, particularly dystonia secondary to cerebral palsy or traumatic brain injury • ITB is an approved use of the Medtronic Infusion System Medulla • The site of action is thought to be at the anterior horn cell • It would be expected that intrathecal infusion would have good access to this site Anterior Horn Spinal Cord
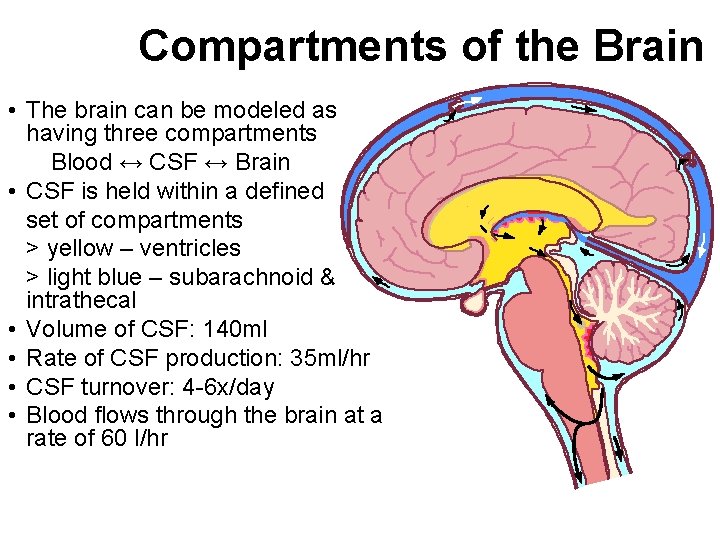
Compartments of the Brain • The brain can be modeled as having three compartments Blood ↔ CSF ↔ Brain • CSF is held within a defined set of compartments > yellow – ventricles > light blue – subarachnoid & intrathecal • Volume of CSF: 140 ml • Rate of CSF production: 35 ml/hr • CSF turnover: 4 -6 x/day • Blood flows through the brain at a rate of 60 l/hr
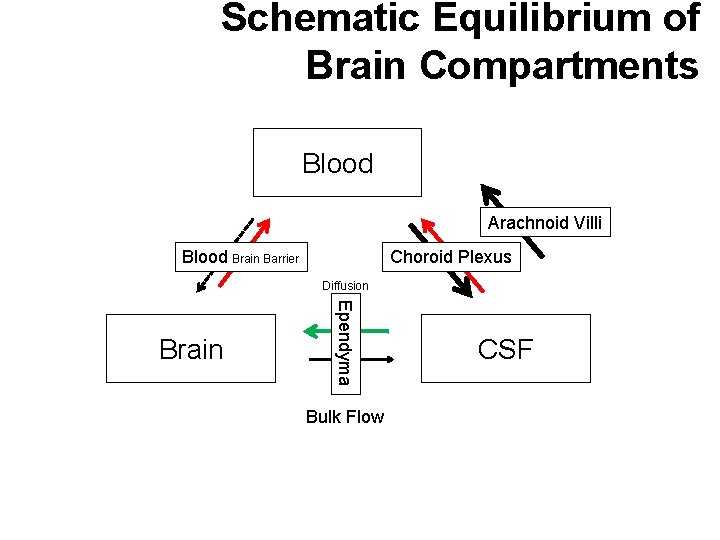
Schematic Equilibrium of Brain Compartments Blood Arachnoid Villi Blood Brain Barrier Choroid Plexus Diffusion Ependyma Brain Bulk Flow CSF
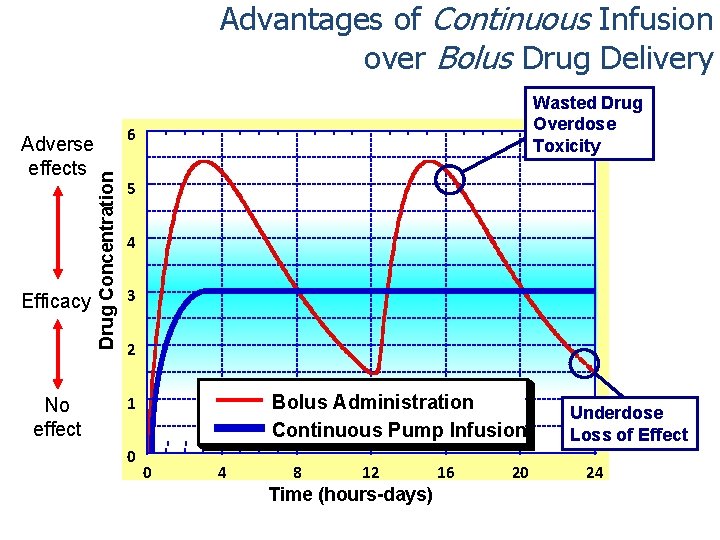
Advantages of Continuous Infusion over Bolus Drug Delivery Efficacy No effect 6 Drug Concentration Adverse effects Wasted Drug Overdose Toxicity 5 4 3 2 Bolus Administration Continuous Pump Infusion 1 0 0 4 8 12 Time (hours-days) 16 20 Underdose Loss of Effect 24
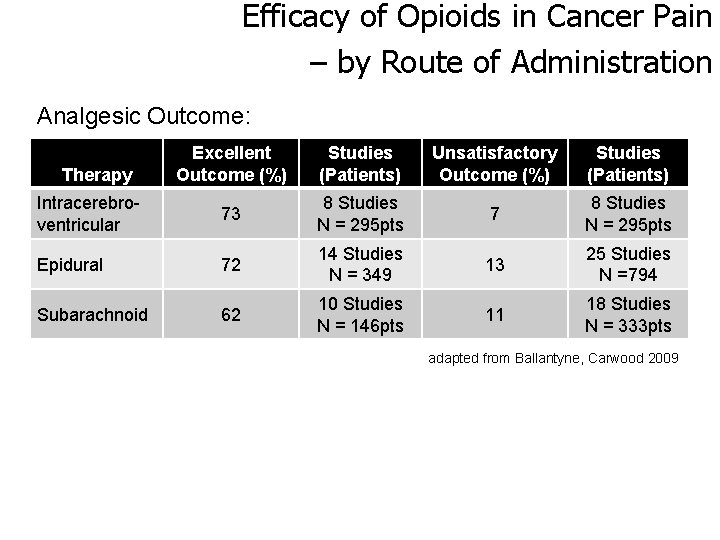
Efficacy of Opioids in Cancer Pain – by Route of Administration Analgesic Outcome: Excellent Outcome (%) Studies (Patients) Unsatisfactory Outcome (%) Studies (Patients) Intracerebroventricular 73 8 Studies N = 295 pts 7 8 Studies N = 295 pts Epidural 72 14 Studies N = 349 13 25 Studies N =794 Subarachnoid 62 10 Studies N = 146 pts 11 18 Studies N = 333 pts Therapy adapted from Ballantyne, Carwood 2009
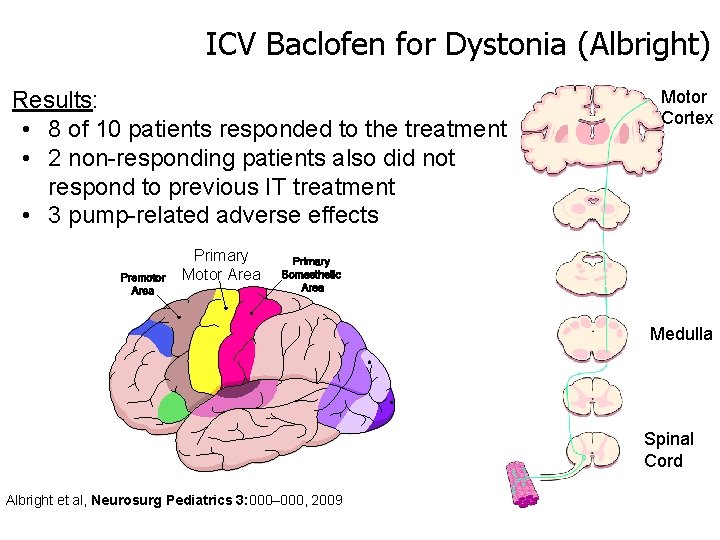
ICV Baclofen for Dystonia (Albright) Results: • 8 of 10 patients responded to the treatment • 2 non-responding patients also did not respond to previous IT treatment • 3 pump-related adverse effects Motor Cortex Primary Motor Area Medulla Spinal Cord Albright et al, Neurosurg Pediatrics 3: 000– 000, 2009
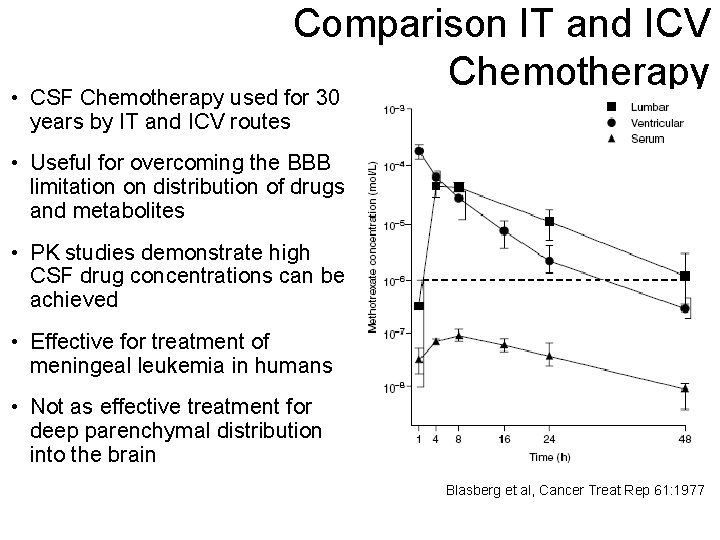
Comparison IT and ICV Chemotherapy • CSF Chemotherapy used for 30 years by IT and ICV routes • Useful for overcoming the BBB limitation on distribution of drugs and metabolites • PK studies demonstrate high CSF drug concentrations can be achieved • Effective for treatment of meningeal leukemia in humans • Not as effective treatment for deep parenchymal distribution into the brain Blasberg et al, Cancer Treat Rep 61: 1977
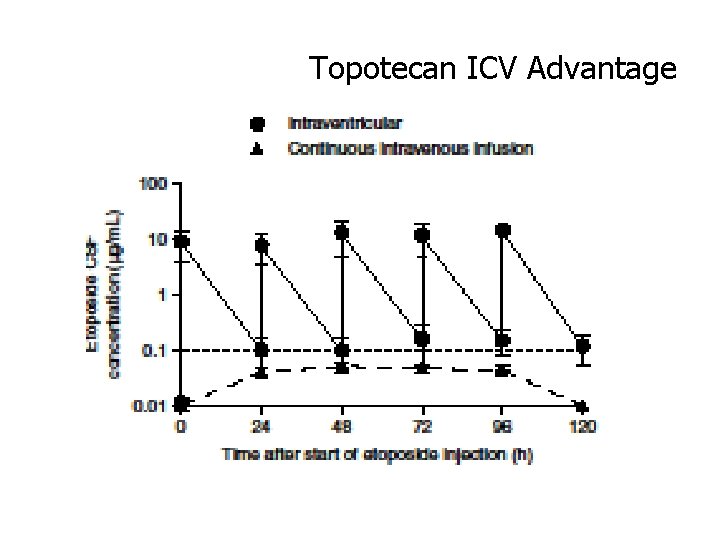
Topotecan ICV Advantage
Key Elements for Drug : Device Therapy Development Device Drug/Biologic Therapy Success Delivery Principles
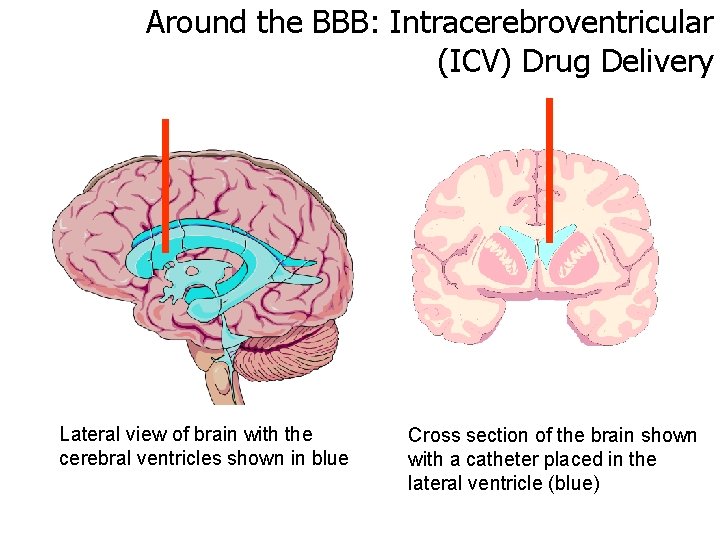
Around the BBB: Intracerebroventricular (ICV) Drug Delivery Lateral view of brain with the cerebral ventricles shown in blue Cross section of the brain shown with a catheter placed in the lateral ventricle (blue)
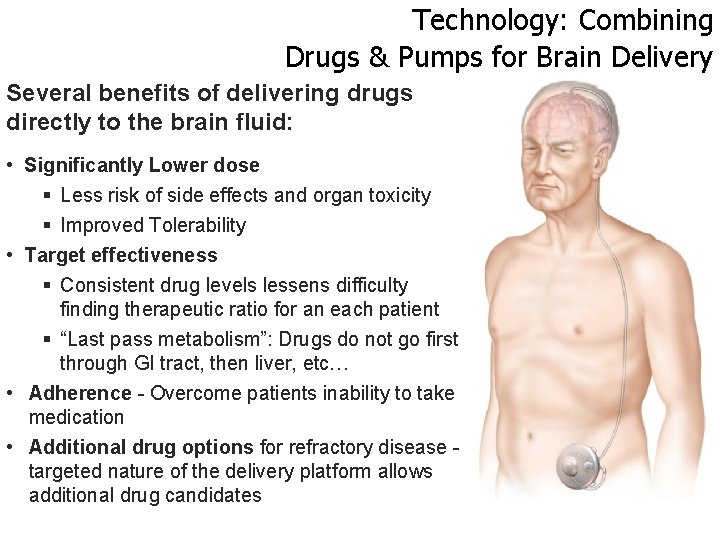
Technology: Combining Drugs & Pumps for Brain Delivery Several benefits of delivering drugs directly to the brain fluid: • Significantly Lower dose § Less risk of side effects and organ toxicity § Improved Tolerability • Target effectiveness § Consistent drug levels lessens difficulty finding therapeutic ratio for an each patient § “Last pass metabolism”: Drugs do not go first through GI tract, then liver, etc… • Adherence - Overcome patients inability to take medication • Additional drug options for refractory disease - targeted nature of the delivery platform allows additional drug candidates
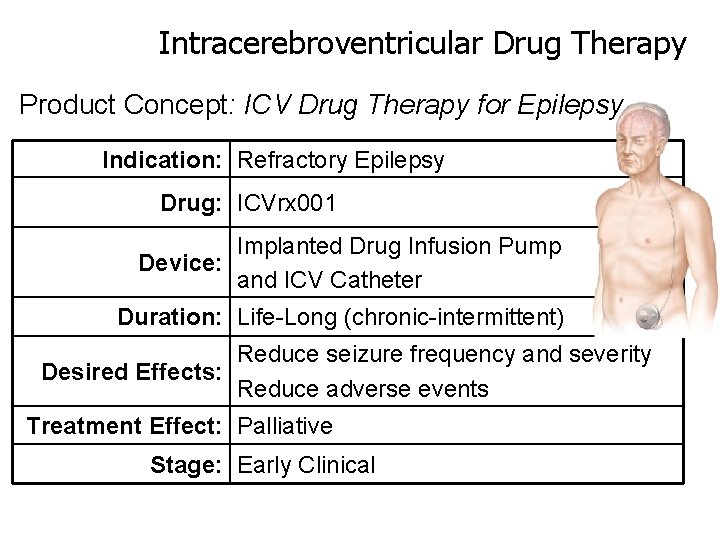
Intracerebroventricular Drug Therapy Product Concept: ICV Drug Therapy for Epilepsy Indication: Refractory Epilepsy Drug: ICVrx 001 Implanted Drug Infusion Pump Device: and ICV Catheter Duration: Life-Long (chronic-intermittent) Reduce seizure frequency and severity Desired Effects: Reduce adverse events Treatment Effect: Palliative Stage: Early Clinical
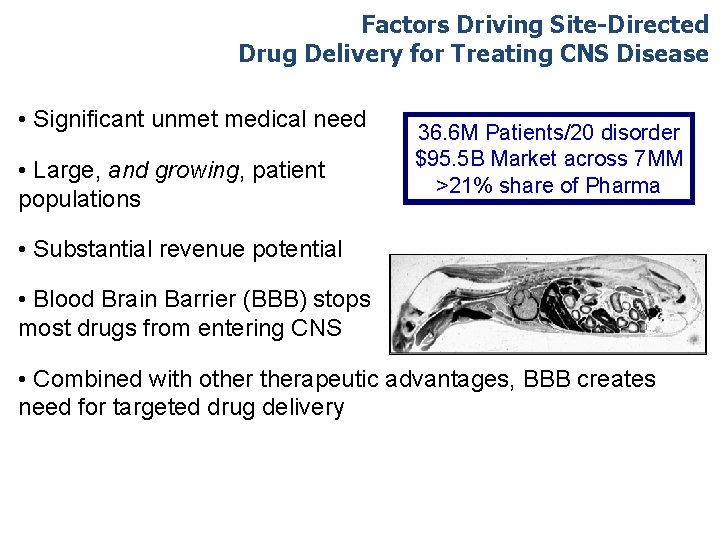
Factors Driving Site-Directed Drug Delivery for Treating CNS Disease • Significant unmet medical need • Large, and growing, patient populations 36. 6 M Patients/20 disorder $95. 5 B Market across 7 MM >21% share of Pharma • Substantial revenue potential • Blood Brain Barrier (BBB) stops most drugs from entering CNS • Combined with otherapeutic advantages, BBB creates need for targeted drug delivery
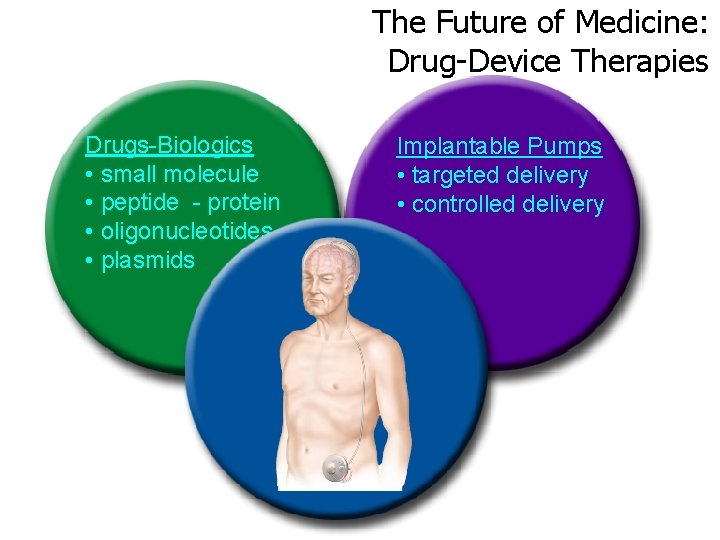
The Future of Medicine: Drug-Device Therapies Drugs-Biologics • small molecule • peptide - protein • oligonucleotides • plasmids Implantable Pumps • targeted delivery • controlled delivery
Thank You …. .
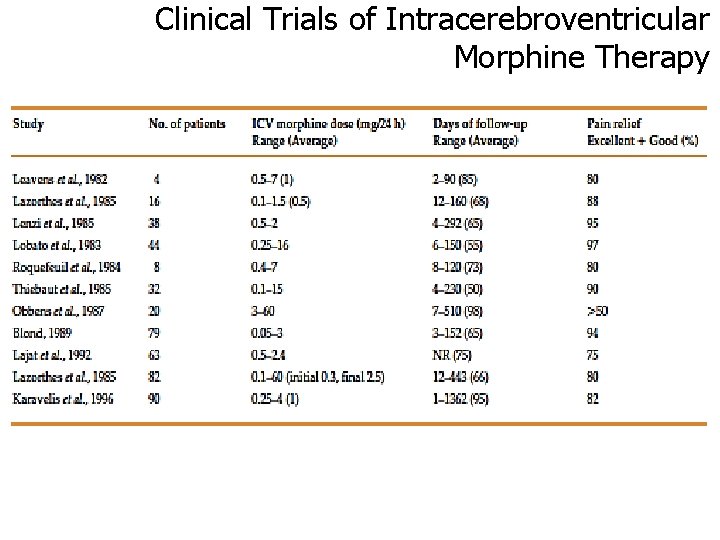
Clinical Trials of Intracerebroventricular Morphine Therapy
- Slides: 32