CML and Imatinib Resistance Which TKI and When
CML and Imatinib Resistance: Which TKI and When? Elias Jabbour, MD University of Texas – M. D. Anderson Cancer Center
CML and Imatinib Resistance: Which TKI and When? Marcos de Lima, MD Stem Cell Transplantation Program Case Western Reserve University Hospitals Seidman Cancer Center Cleveland - OH
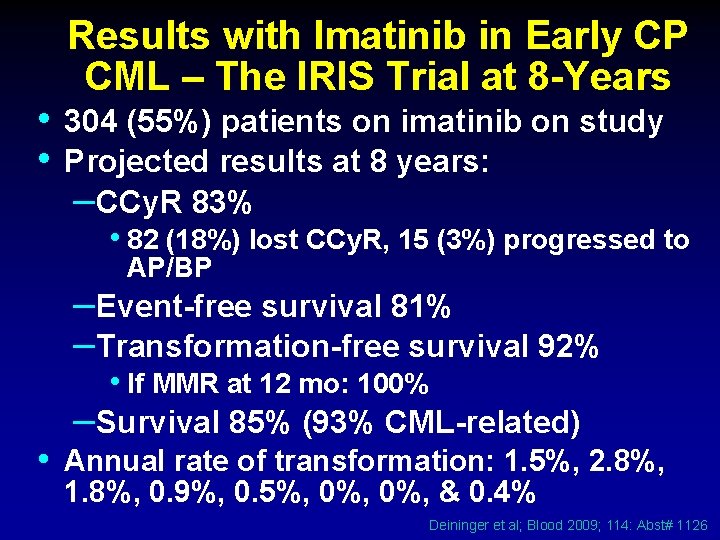
Results with Imatinib in Early CP CML – The IRIS Trial at 8 -Years • 304 (55%) patients on imatinib on study • Projected results at 8 years: –CCy. R 83% • 82 (18%) lost CCy. R, 15 (3%) progressed to AP/BP –Event-free survival 81% –Transformation-free survival 92% • If MMR at 12 mo: 100% –Survival 85% (93% CML-related) • Annual rate of transformation: 1. 5%, 2. 8%, 1. 8%, 0. 9%, 0. 5%, 0%, & 0. 4% Deininger et al; Blood 2009; 114: Abst# 1126
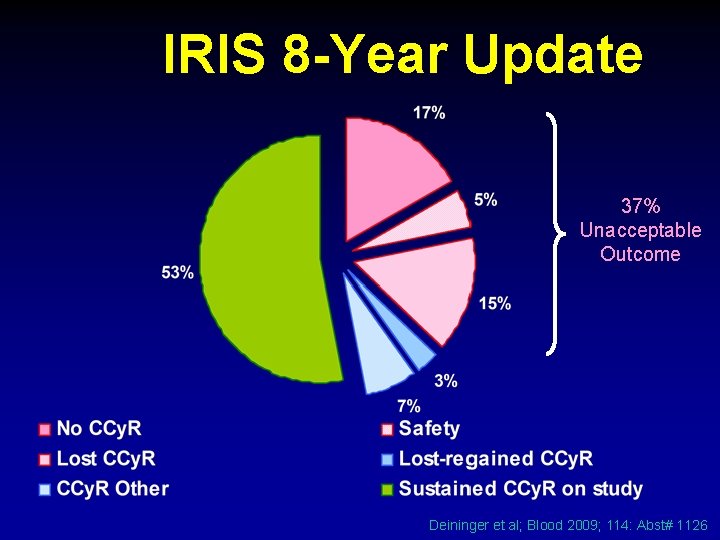
IRIS 8 -Year Update 37% Unacceptable Outcome Deininger et al; Blood 2009; 114: Abst# 1126
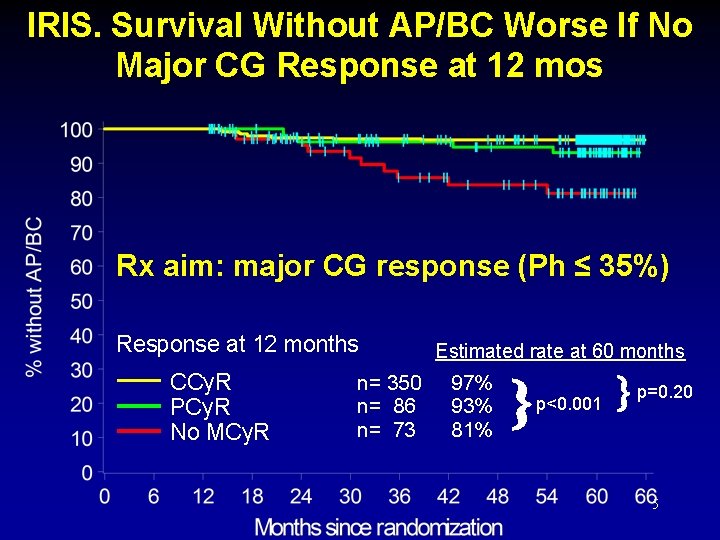
IRIS. Survival Without AP/BC Worse If No Major CG Response at 12 mos Rx aim: major CG response (Ph ≤ 35%) Response at 12 months CCy. R PCy. R No MCy. R n= 350 n= 86 n= 73 Estimated rate at 60 months 97% 93% 81% p<0. 001 p=0. 20 5

Criteria for Failure and Suboptimal Response to Imatinib Time (mo) Response Failure Suboptimal Optimal 3 No CHR No CG Response < 65% Ph+ 6 No CHR >95% Ph+ ≥ 35% Ph+ ≤ 35% Ph+ 12 ≥ 35% Ph+ 1 -35% Ph+ 0% Ph+ 18 ≥ 5% Ph+ No MMR Any Loss of CHR Loss of CCg. R Mutation CE Loss of MMR Mutation Stable or improving MMR Baccarani. JCO 2009; 27: 6041 -51
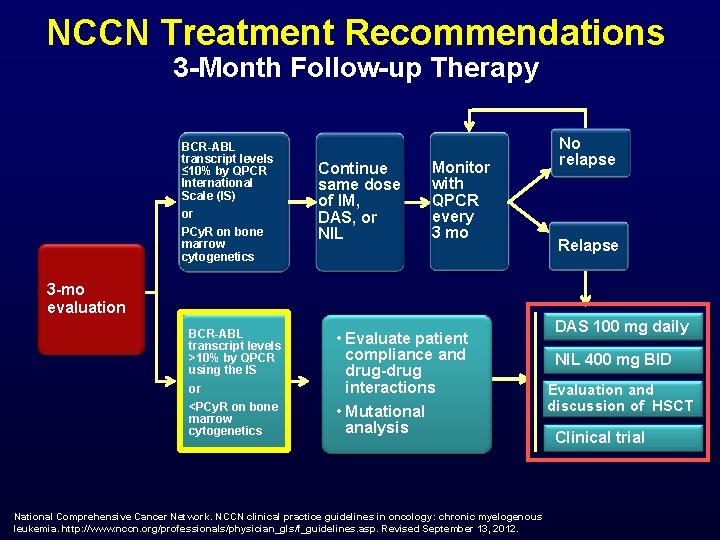
NCCN Treatment Recommendations 3 -Month Follow-up Therapy BCR-ABL transcript levels ≤ 10% by QPCR International Scale (IS) or PCy. R on bone marrow cytogenetics Continue same dose of IM, DAS, or NIL Monitor with QPCR every 3 mo No relapse Relapse 3 -mo evaluation BCR-ABL transcript levels >10% by QPCR using the IS or <PCy. R on bone marrow cytogenetics • Evaluate patient compliance and drug-drug interactions • Mutational analysis National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: chronic myelogenous leukemia. http: //www. nccn. org/professionals/physician_gls/f_guidelines. asp. Revised September 13, 2012. DAS 100 mg daily NIL 400 mg BID Evaluation and discussion of HSCT Clinical trial
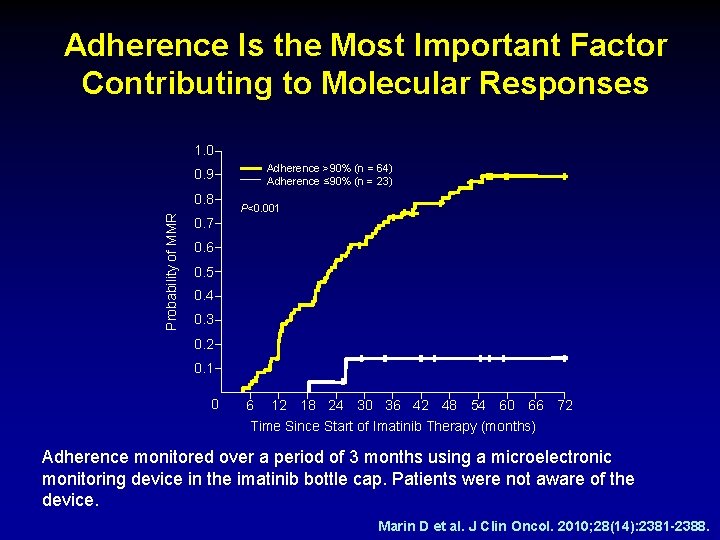
Adherence Is the Most Important Factor Contributing to Molecular Responses 1. 0 0. 9 Probability of MMR 0. 8 Adherence >90% (n = 64) Adherence ≤ 90% (n = 23) P<0. 001 0. 7 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 6 12 18 24 30 36 42 48 54 60 66 72 Time Since Start of Imatinib Therapy (months) Adherence monitored over a period of 3 months using a microelectronic monitoring device in the imatinib bottle cap. Patients were not aware of the device. Marin D et al. J Clin Oncol. 2010; 28(14): 2381 -2388.
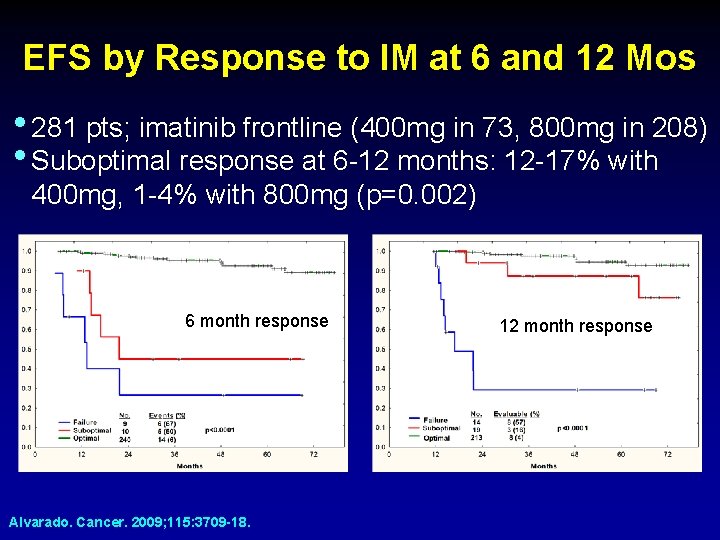
EFS by Response to IM at 6 and 12 Mos • 281 pts; imatinib frontline (400 mg in 73, 800 mg in 208) • Suboptimal response at 6 -12 months: 12 -17% with 400 mg, 1 -4% with 800 mg (p=0. 002) 6 month response Alvarado. Cancer. 2009; 115: 3709 -18. 12 month response
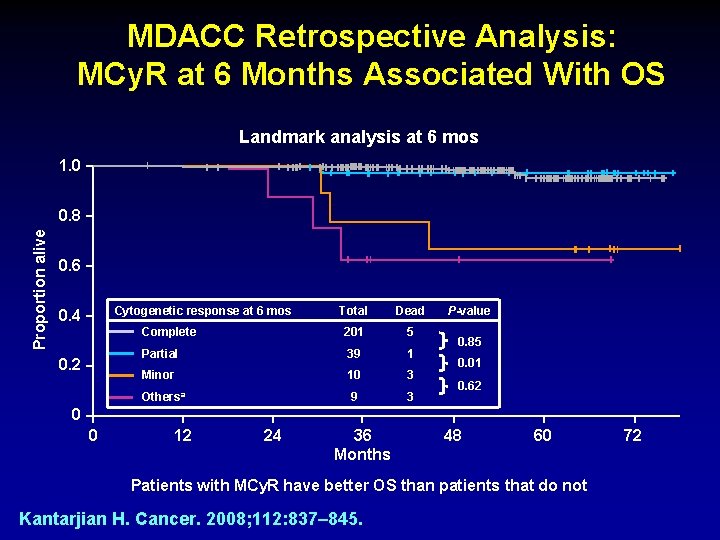
MDACC Retrospective Analysis: MCy. R at 6 Months Associated With OS Landmark analysis at 6 mos 1. 0 Proportion alive 0. 8 0. 6 Cytogenetic response at 6 mos 0. 4 0. 2 Total Dead Complete 201 5 Partial 39 1 Minor 10 3 Othersa 9 3 P-value 0. 85 0. 01 0. 62 0 0 12 24 36 Months 48 60 Patients with MCy. R have better OS than patients that do not Kantarjian H. Cancer. 2008; 112: 837– 845. 72
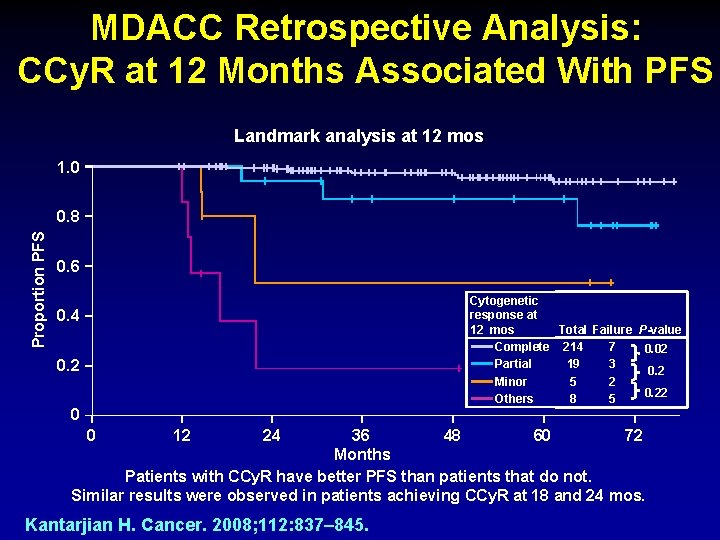
MDACC Retrospective Analysis: CCy. R at 12 Months Associated With PFS Landmark analysis at 12 mos 1. 0 Proportion PFS 0. 8 0. 6 Cytogenetic response at 12 mos Total Failure P-value Complete 214 7 0. 02 Partial 19 3 0. 2 Minor 5 2 0. 22 Others 8 5 0. 4 0. 2 0 0 12 24 36 48 60 72 Months Patients with CCy. R have better PFS than patients that do not. Similar results were observed in patients achieving CCy. R at 18 and 24 mos. Kantarjian H. Cancer. 2008; 112: 837– 845.
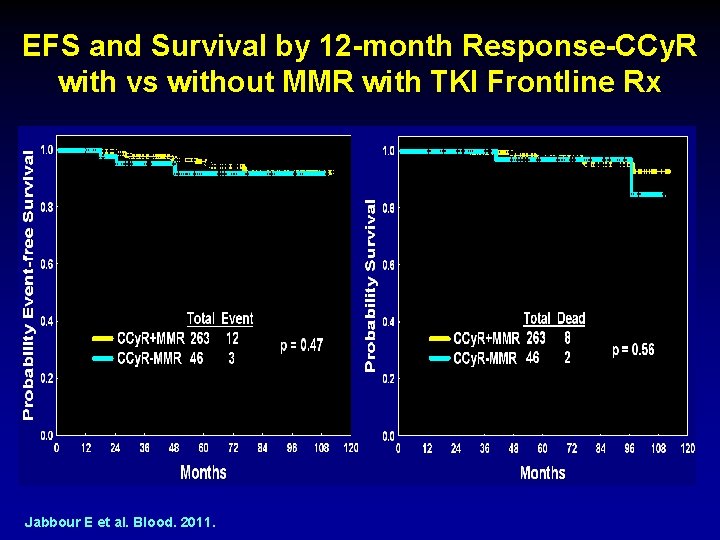
EFS and Survival by 12 -month Response-CCy. R with vs without MMR with TKI Frontline Rx Jabbour E et al. Blood. 2011.
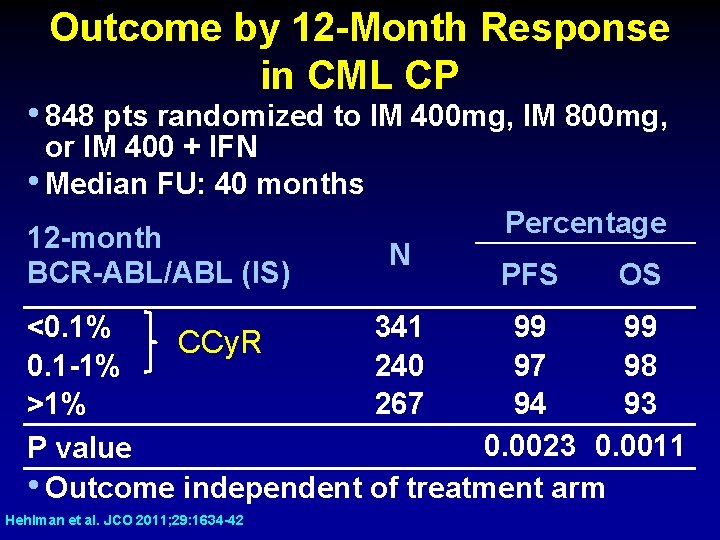
Outcome by 12 -Month Response in CML CP • 848 pts randomized to IM 400 mg, IM 800 mg, or IM 400 + IFN • Median FU: 40 months 12 -month BCR-ABL/ABL (IS) N Percentage PFS OS <0. 1% 341 99 99 CCy. R 0. 1 -1% 240 97 98 >1% 267 94 93 0. 0023 0. 0011 P value • Outcome independent of treatment arm Hehlman et al. JCO 2011; 29: 1634 -42
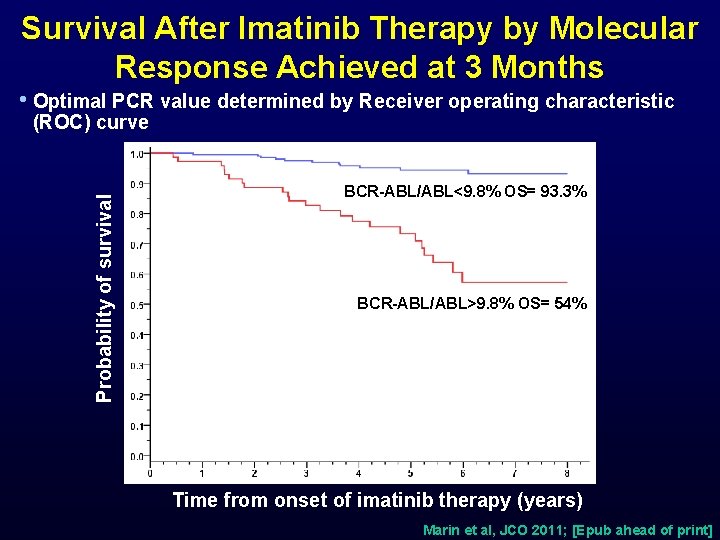
Survival After Imatinib Therapy by Molecular Response Achieved at 3 Months • Optimal PCR value determined by Receiver operating characteristic (ROC) curve Probability of survival BCR-ABL/ABL<9. 8% OS= 93. 3% BCR-ABL/ABL>9. 8% OS= 54% p<0. 0001 Time from onset of imatinib therapy (years) Marin et al, JCO 2011; [Epub ahead of print]

CML IV: Long-Term Impact of Response at 3 Months • 1223 pts randomized to imatinib 400, imatinib + IFN, imatinib + ara-C, imatinib 800 • 3 month analysis: PCR in 692 pts, cytogenetics in 460 • 3 mo transcript levels predictive of achievement of CCy. R and MMR Cytogenetics Molecular % 5 -year (% Ph+) [BCR-ABL/ABL (IS)] outcome ≤ 35% >35% ≤ 10% >10% PFS 94 87 93 87 OS 95 87 Hanfstein et al. ASH 2011; Abstract #783
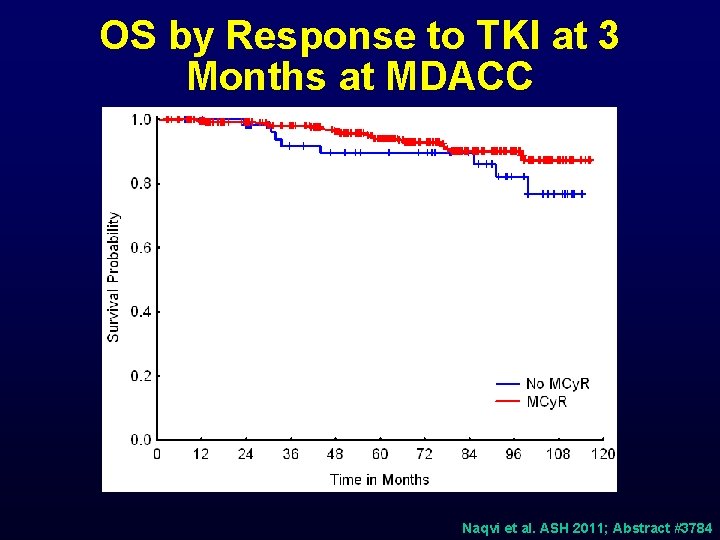
OS by Response to TKI at 3 Months at MDACC Naqvi et al. ASH 2011; Abstract #3784
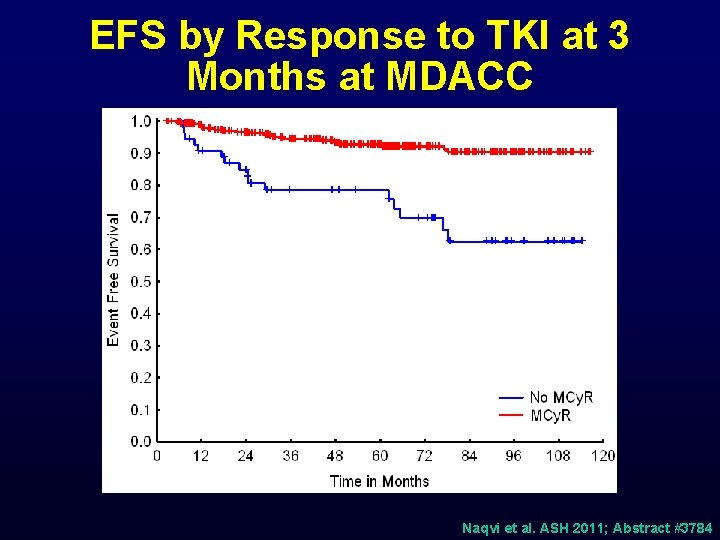
EFS by Response to TKI at 3 Months at MDACC Naqvi et al. ASH 2011; Abstract #3784
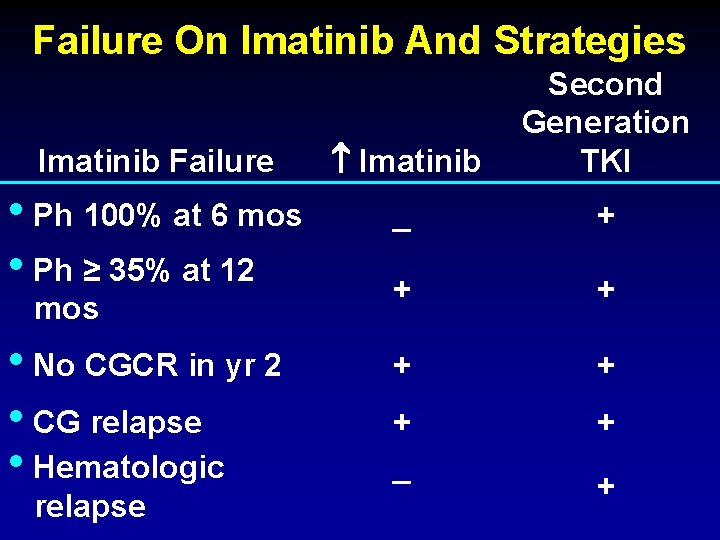
Failure On Imatinib And Strategies Imatinib Failure Imatinib Second Generation TKI • Ph 100% at 6 mos • Ph ≥ 35% at 12 _ + + + _ + mos • No CGCR in yr 2 • CG relapse • Hematologic relapse +
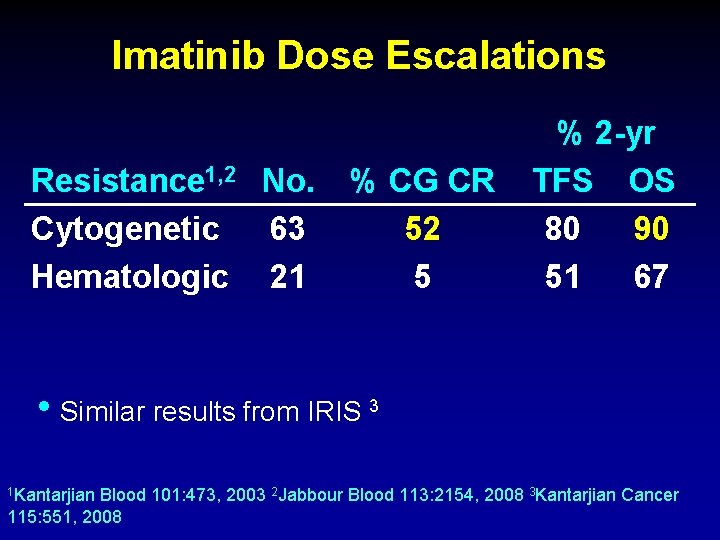
Imatinib Dose Escalations Resistance 1, 2 No. Cytogenetic 63 Hematologic 21 % CG CR 52 5 % 2 -yr TFS OS 80 90 51 67 • Similar results from IRIS 3 1 Kantarjian Blood 101: 473, 2003 2 Jabbour Blood 113: 2154, 2008 3 Kantarjian Cancer 115: 551, 2008

2 nd Generation TKI in CML Parameter Potency (fold vs IM) Target BCR-ABL binding Resistant mutations Mutations with intermediate sensitivity Dasatinib Nilotinib Bosutinib 325 30 20 -50 Src & Abl Src & ABL Active + Inactive Intermediate T 315 I E 255 K/V, V 299 L, E 255 K/V, Y 253 F/H, E 255 V/K, F 317 L Q 252 H, F 359 V V 299 L, F 317 L Standard dose (CP) 100 mg QD 400 mg BID 500 mg QD Grade 3 -4 neutropenia & thrombocytopenia 33% / 22% 31% / 33% 12% / 21% Other notable toxicities Pleural effusion, bleeding Bilirubin, lipase elevation Diarrhea, rash C-kit inhibition (vs imatinib) Increased Similar None PDGFR inhibition (vs imatinib) Increased Similar None Highly active Clinical activity
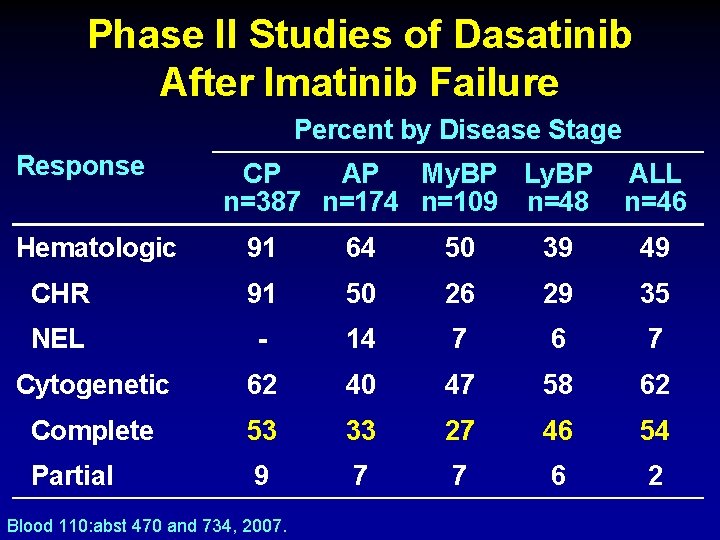
Phase II Studies of Dasatinib After Imatinib Failure Percent by Disease Stage Response Hematologic CP AP My. BP Ly. BP n=387 n=174 n=109 n=48 ALL n=46 91 64 50 39 49 CHR 91 50 26 29 35 NEL - 14 7 6 7 Cytogenetic 62 40 47 58 62 Complete 53 33 27 46 54 Partial 9 7 7 6 2 Blood 110: abst 470 and 734, 2007.
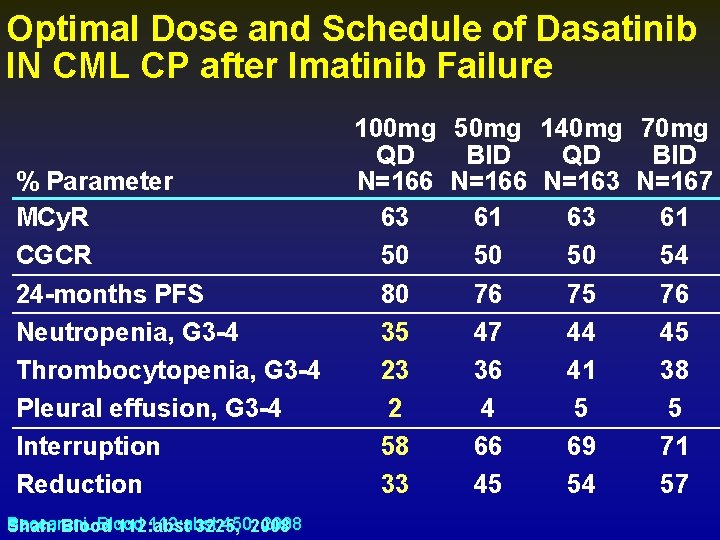
Optimal Dose and Schedule of Dasatinib IN CML CP after Imatinib Failure % Parameter MCy. R CGCR 24 -months PFS Neutropenia, G 3 -4 Thrombocytopenia, G 3 -4 Pleural effusion, G 3 -4 Interruption Reduction Baccarani. Blood 112: abst 450, 2008 Shah. Blood 112: abst 3225, 100 mg 50 mg 140 mg 70 mg QD BID N=166 N=163 N=167 63 61 50 50 50 54 80 76 75 76 35 47 44 45 23 36 41 38 2 4 5 5 58 66 69 71 33 45 54 57
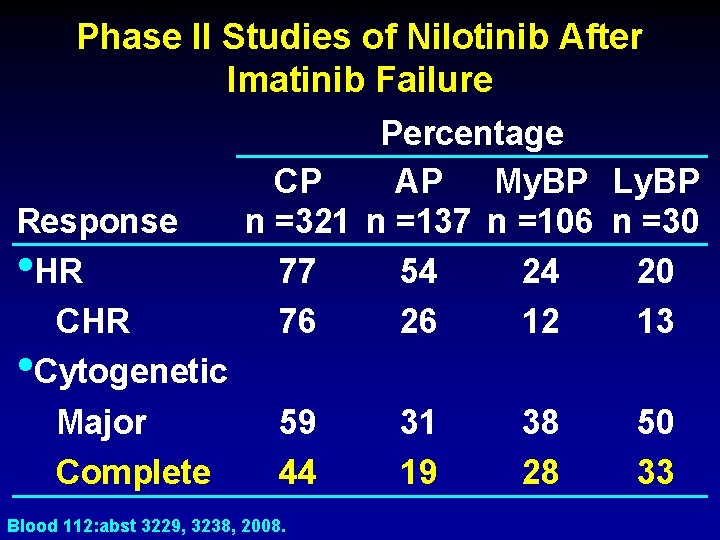
Phase II Studies of Nilotinib After Imatinib Failure Response • HR CHR • Cytogenetic Major Complete Percentage CP AP My. BP Ly. BP n =321 n =137 n =106 n =30 77 54 24 20 76 26 12 13 59 44 Blood 112: abst 3229, 3238, 2008. 31 19 38 28 50 33
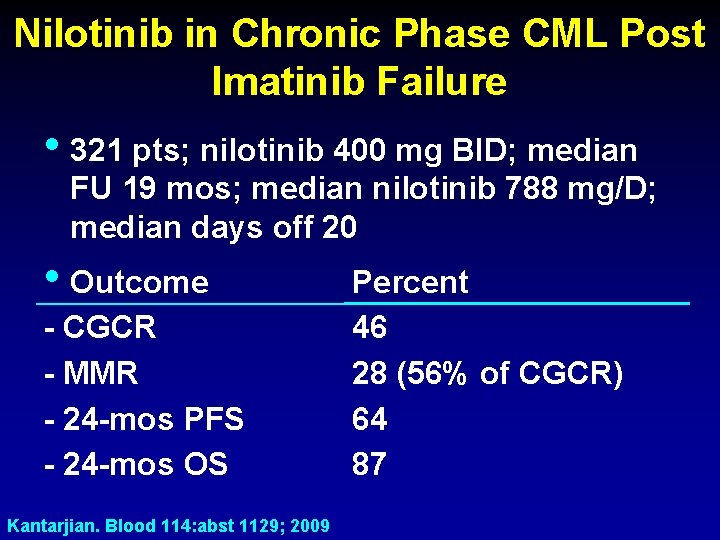
Nilotinib in Chronic Phase CML Post Imatinib Failure • 321 pts; nilotinib 400 mg BID; median FU 19 mos; median nilotinib 788 mg/D; median days off 20 • Outcome - CGCR - MMR - 24 -mos PFS - 24 -mos OS Kantarjian. Blood 114: abst 1129; 2009 Percent 46 28 (56% of CGCR) 64 87
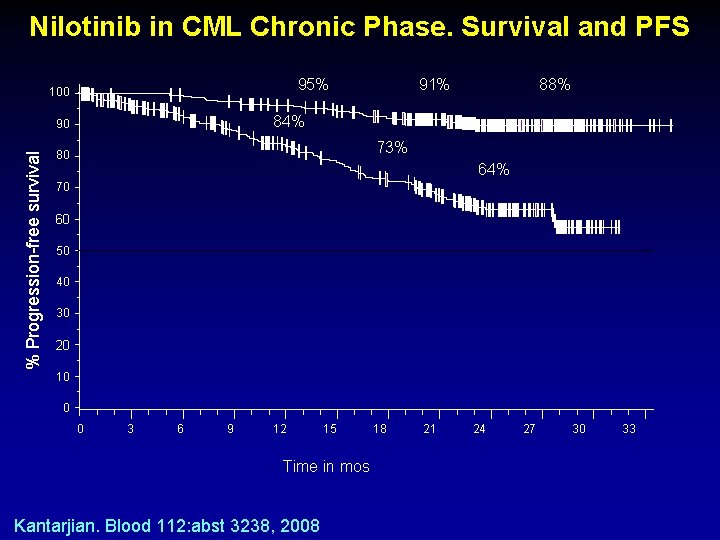
Nilotinib in CML Chronic Phase. Survival and PFS 95% 100 88% 84% 90 % Progression-free survival 91% 73% 80 64% 70 60 50 40 30 20 10 0 0 3 6 9 12 15 Time in mos Kantarjian. Blood 112: abst 3238, 2008 18 21 24 27 30 33
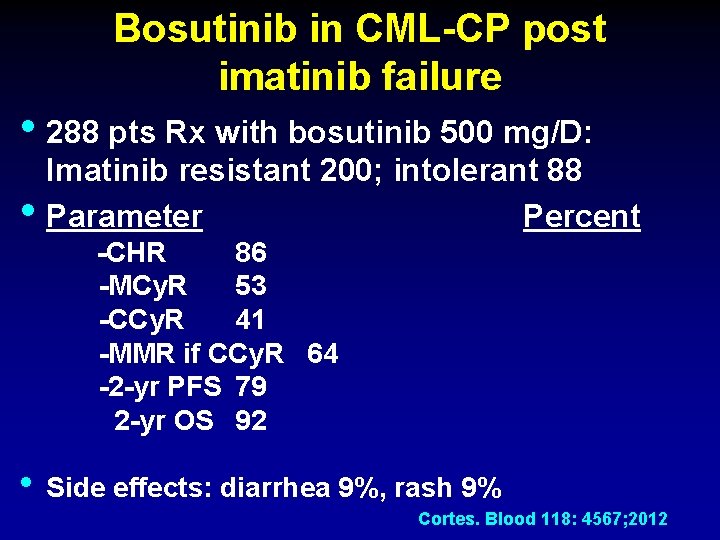
Bosutinib in CML-CP post imatinib failure • 288 pts Rx with bosutinib 500 mg/D: • Imatinib resistant 200; intolerant 88 Parameter Percent -CHR 86 -MCy. R 53 -CCy. R 41 -MMR if CCy. R 64 -2 -yr PFS 79 2 -yr OS 92 • Side effects: diarrhea 9%, rash 9% Cortes. Blood 118: 4567; 2012
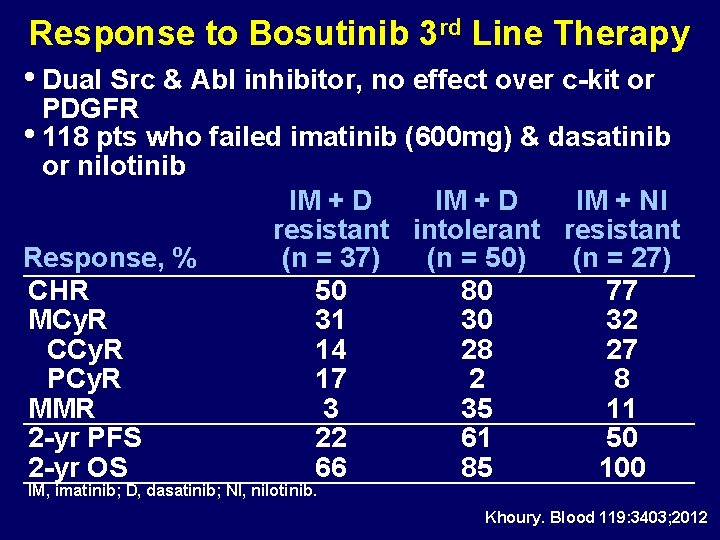
Response to Bosutinib 3 rd Line Therapy • Dual Src & Abl inhibitor, no effect over c-kit or PDGFR • 118 pts who failed imatinib (600 mg) & dasatinib or nilotinib IM + D IM + NI resistant intolerant resistant Response, % (n = 37) (n = 50) (n = 27) CHR 50 80 77 MCy. R 31 30 32 CCy. R 14 28 27 PCy. R 17 2 8 MMR 3 35 11 2 -yr PFS 22 61 50 2 -yr OS 66 85 100 IM, imatinib; D, dasatinib; NI, nilotinib. Khoury. Blood 119: 3403; 2012

2 nd Generation TKI in CML CP Post-Imatinib Resistance Response Percentage Dasatinib Nilotinib Bosutinib FU (mo) >24 24* CHR 89 77 86 MCy. R 59 56 54 CCy. R 44 41 41 24 mo PFS** 80% 64% 79% 24 mo OS** 91% 87% 92% * Median ** All patients Shah et al. Haematologica 2010; 95: 232 -40 Kantarjian et al. Blood 2011; 117: 1141 -45 Cortes et al. Blood 2011; 118; 4567 -76
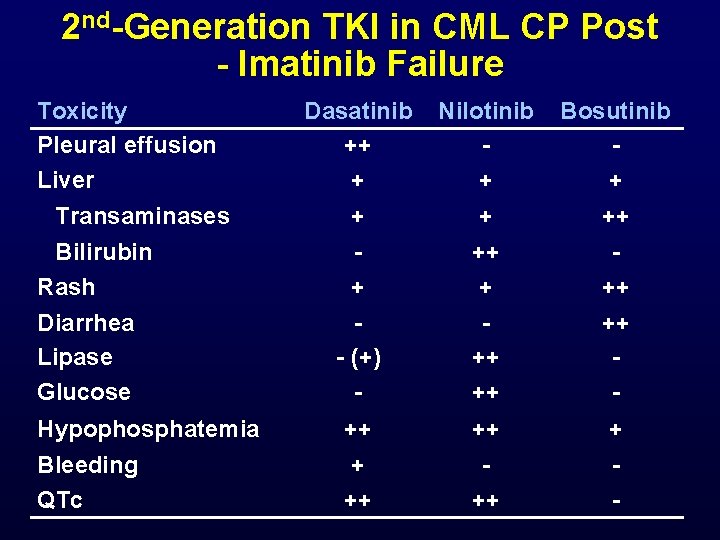
2 nd-Generation TKI in CML CP Post - Imatinib Failure Toxicity Pleural effusion Liver Dasatinib ++ + Nilotinib + Bosutinib + ++ - (+) - ++ ++ ++ - Hypophosphatemia ++ ++ + Bleeding QTc + ++ ++ - Transaminases Bilirubin Rash Diarrhea Lipase Glucose
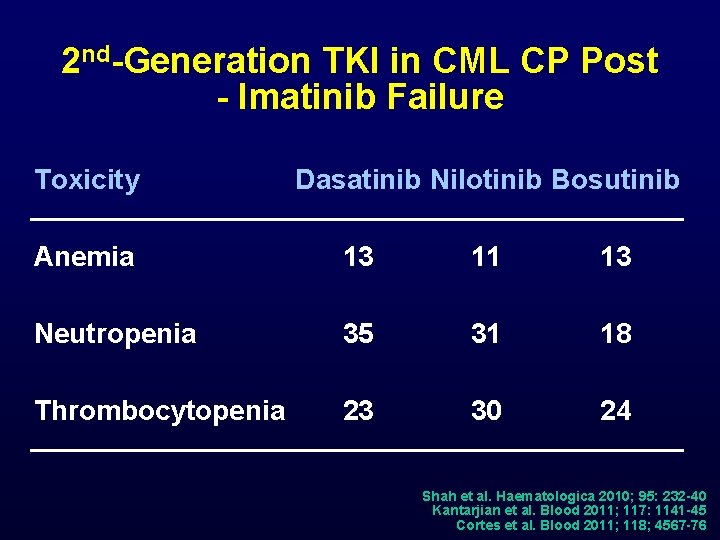
2 nd-Generation TKI in CML CP Post - Imatinib Failure Toxicity Dasatinib Nilotinib Bosutinib Anemia 13 11 13 Neutropenia 35 31 18 Thrombocytopenia 23 30 24 Shah et al. Haematologica 2010; 95: 232 -40 Kantarjian et al. Blood 2011; 117: 1141 -45 Cortes et al. Blood 2011; 118; 4567 -76
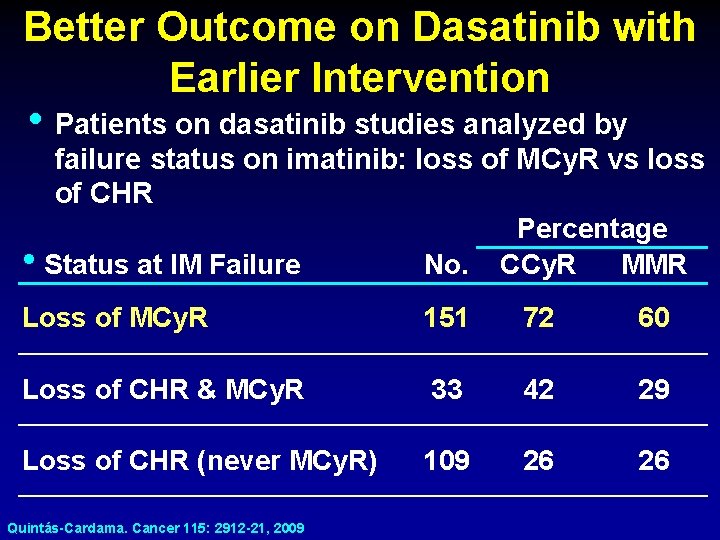
Better Outcome on Dasatinib with Earlier Intervention • Patients on dasatinib studies analyzed by failure status on imatinib: loss of MCy. R vs loss of CHR Percentage MMR • Status at IM Failure No. CCy. R Loss of MCy. R 151 72 60 Loss of CHR & MCy. R 33 42 29 Loss of CHR (never MCy. R) 109 26 26 Quintás-Cardama. Cancer 115: 2912 -21, 2009
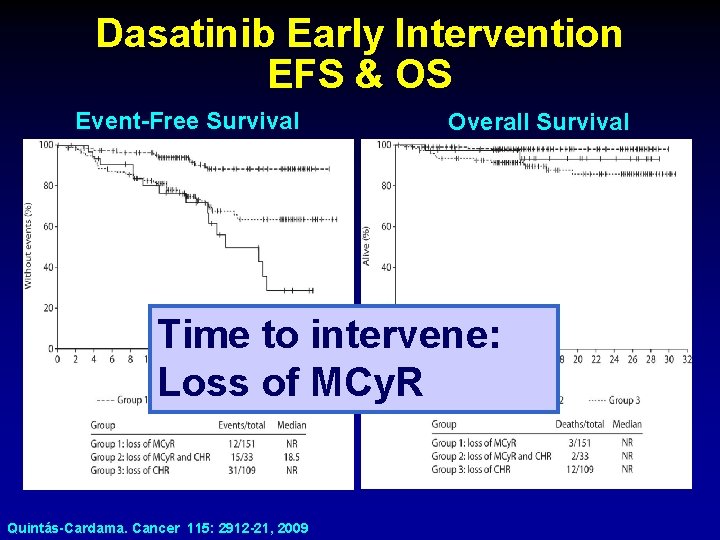
Dasatinib Early Intervention EFS & OS Event-Free Survival Overall Survival Time to intervene: Loss of MCy. R Quintás-Cardama. Cancer 115: 2912 -21, 2009
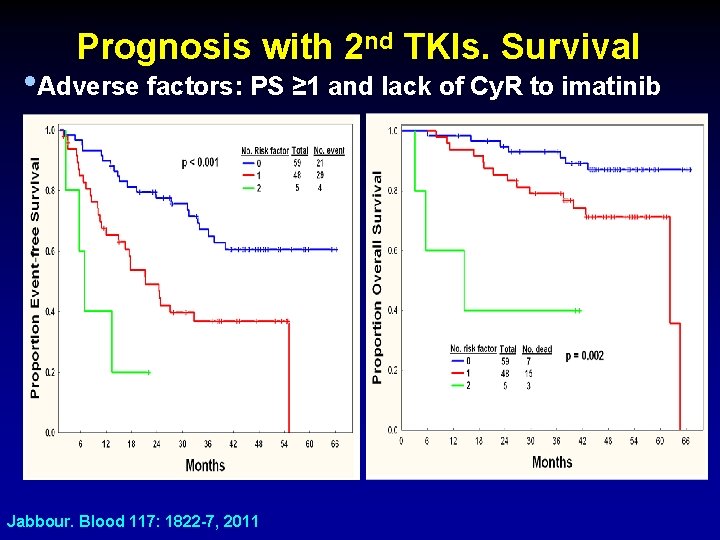
Prognosis with 2 nd TKIs. Survival • Adverse factors: PS ≥ 1 and lack of Cy. R to imatinib Jabbour. Blood 117: 1822 -7, 2011
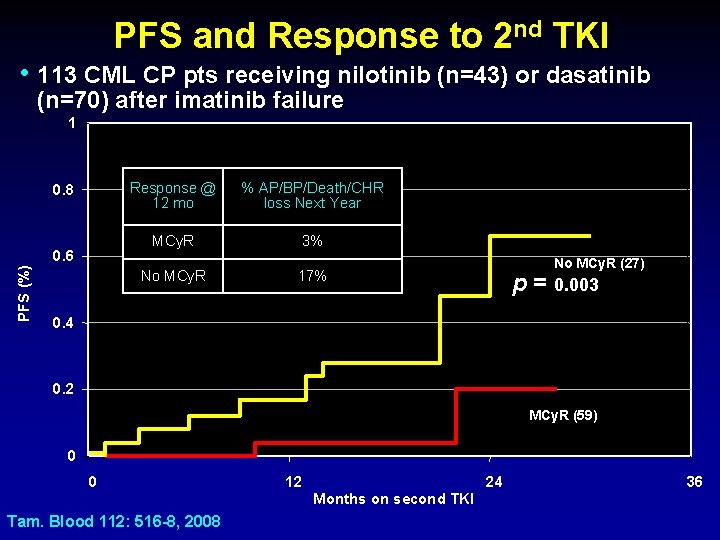
PFS and Response to 2 nd TKI • 113 CML CP pts receiving nilotinib (n=43) or dasatinib (n=70) after imatinib failure 1 0. 8 PFS (%) 0. 6 Response @ 12 mo % AP/BP/Death/CHR loss Next Year MCy. R 3% No MCy. R 17% No MCy. R (27) p = 0. 003 0. 4 0. 2 MCy. R (59) 0 0 Tam. Blood 112: 516 -8, 2008 12 Months on second TKI 24 36
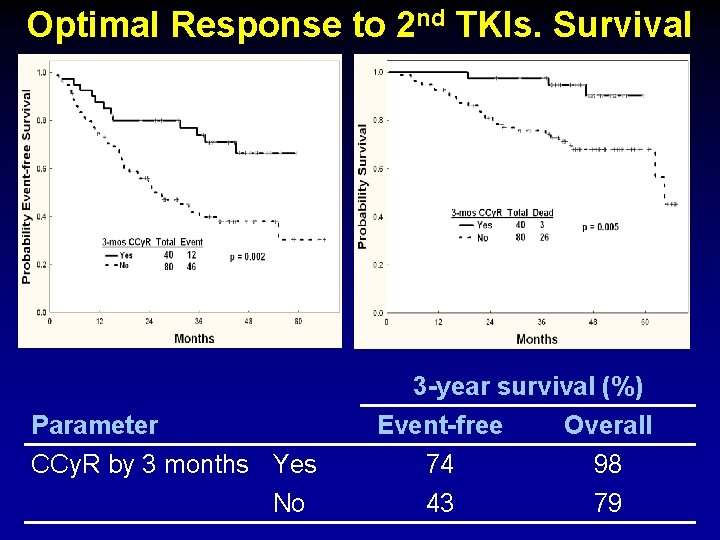
Optimal Response to 2 nd TKIs. Survival Parameter CCy. R by 3 months Yes No 3 -year survival (%) Event-free Overall 74 98 43 79
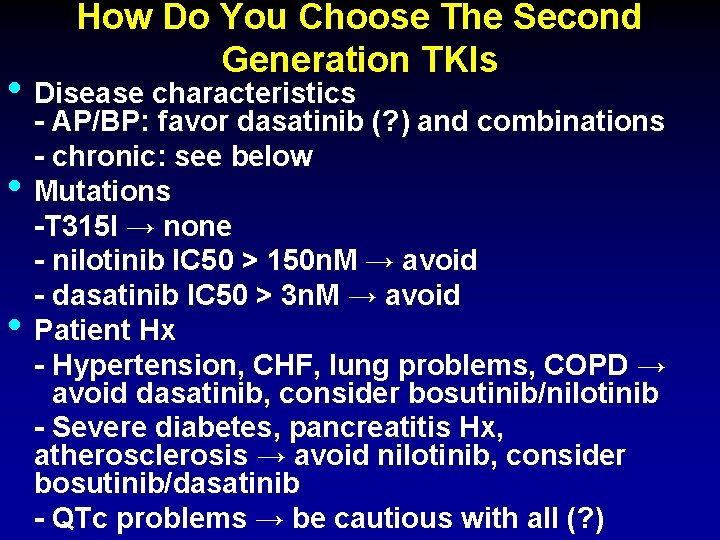
How Do You Choose The Second Generation TKIs • Disease characteristics • • - AP/BP: favor dasatinib (? ) and combinations - chronic: see below Mutations -T 315 I → none - nilotinib IC 50 > 150 n. M → avoid - dasatinib IC 50 > 3 n. M → avoid Patient Hx - Hypertension, CHF, lung problems, COPD → avoid dasatinib, consider bosutinib/nilotinib - Severe diabetes, pancreatitis Hx, atherosclerosis → avoid nilotinib, consider bosutinib/dasatinib - QTc problems → be cautious with all (? )
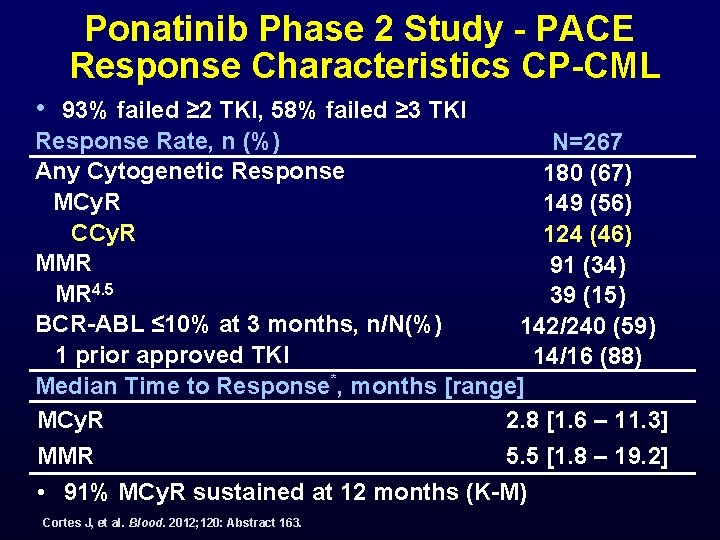
Ponatinib Phase 2 Study - PACE Response Characteristics CP-CML • 93% failed ≥ 2 TKI, 58% failed ≥ 3 TKI Response Rate, n (%) N=267 Any Cytogenetic Response 180 (67) MCy. R 149 (56) CCy. R 124 (46) MMR 91 (34) MR 4. 5 39 (15) BCR-ABL ≤ 10% at 3 months, n/N(%) 142/240 (59) 1 prior approved TKI 14/16 (88) Median Time to Response*, months [range] 2. 8 [1. 6 – 11. 3] MCy. R 5. 5 [1. 8 – 19. 2] MMR • 91% MCy. R sustained at 12 months (K-M) Cortes J, et al. Blood. 2012; 120: Abstract 163.
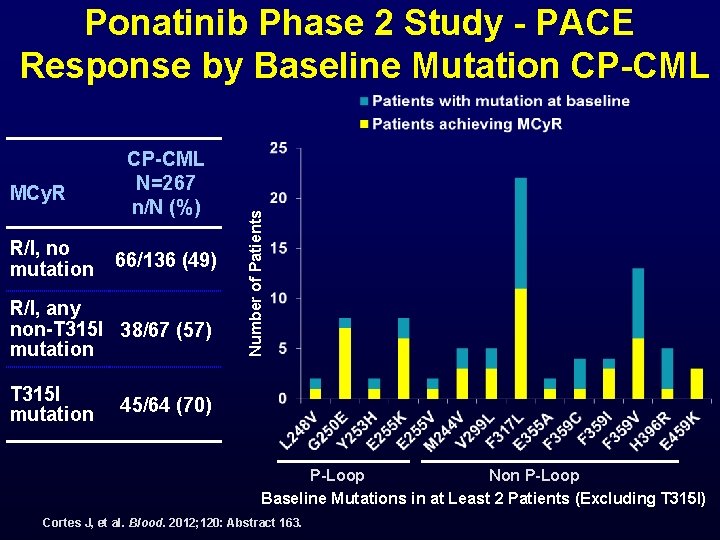
MCy. R R/I, no mutation CP-CML N=267 n/N (%) 66/136 (49) R/I, any non-T 315 I 38/67 (57) mutation T 315 I mutation Number of Patients Ponatinib Phase 2 Study - PACE Response by Baseline Mutation CP-CML 45/64 (70) P-Loop Non P-Loop Baseline Mutations in at Least 2 Patients (Excluding T 315 I) Cortes J, et al. Blood. 2012; 120: Abstract 163.

Ponatinib Phase 2 Study - PACE Response in Advanced Phase AP-CML N=83 n (%) BP-CML N=62 Ph+ ALL Myeloid Lymphoid N=32 N=52 N=10 Ma. HR* 47 (57) 15 (29) 4 (40) 13 (41) Any Cy. R** 46 (55) 19 (37) 5 (50) 15 (47) MCy. R 32 (39) 10 (19) 4 (40) 15 (47) 20 (24) 8 (15) 3 (30) 12 (38) 13 (16) N/A N/A CCy. R MMR# *Ma. HR = primary endpoint; 14 AP-CML patients with baseline Ma. HR and 1 AP-CML patient with no baseline Ma. HR assessment counted as non-responders **CCy. R + PCy. R + minor Cy. R + minimal Cy. R #MMR was assessed on the International Scale using peripheral blood; Patients missing a valid baseline MMR assessment , or who met the criteria for MMR at baseline, were counted as non-responders Kantarjian HM, et al. Blood. 2012; 120: Abstract 915.
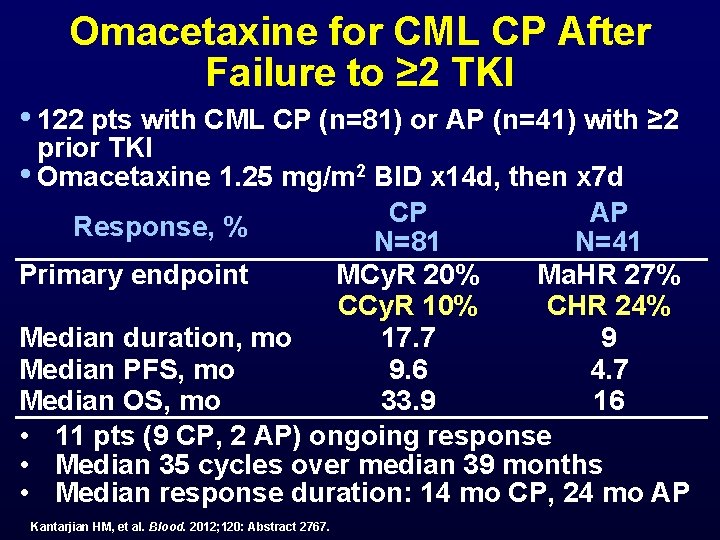
Omacetaxine for CML CP After Failure to ≥ 2 TKI • 122 pts with CML CP (n=81) or AP (n=41) with ≥ 2 prior TKI • Omacetaxine 1. 25 mg/m 2 BID x 14 d, then x 7 d CP AP Response, % N=81 N=41 Primary endpoint MCy. R 20% Ma. HR 27% CCy. R 10% CHR 24% Median duration, mo 17. 7 9 Median PFS, mo 9. 6 4. 7 Median OS, mo 33. 9 16 • 11 pts (9 CP, 2 AP) ongoing response • Median 35 cycles over median 39 months • Median response duration: 14 mo CP, 24 mo AP Kantarjian HM, et al. Blood. 2012; 120: Abstract 2767.
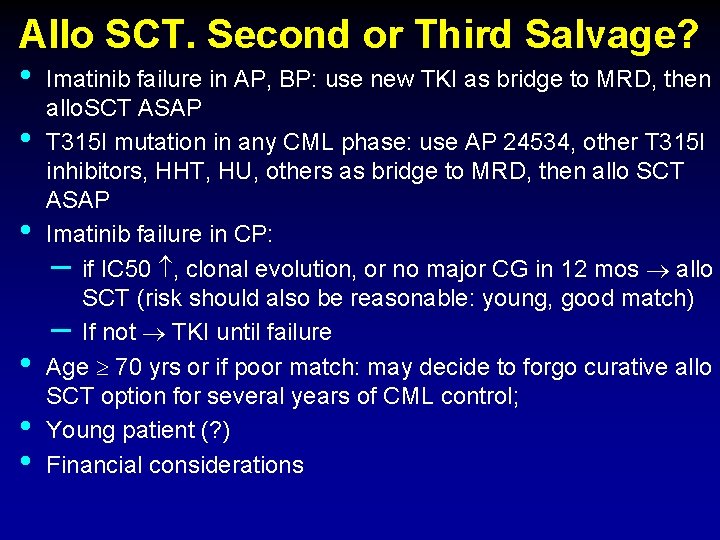
Allo SCT. Second or Third Salvage? • • • Imatinib failure in AP, BP: use new TKI as bridge to MRD, then allo. SCT ASAP T 315 I mutation in any CML phase: use AP 24534, other T 315 I inhibitors, HHT, HU, others as bridge to MRD, then allo SCT ASAP Imatinib failure in CP: – if IC 50 , clonal evolution, or no major CG in 12 mos allo SCT (risk should also be reasonable: young, good match) – If not TKI until failure Age 70 yrs or if poor match: may decide to forgo curative allo SCT option for several years of CML control; Young patient (? ) Financial considerations
Monitoring Patients with CML While on TKI Therapy • Adequate monitoring required to optimize outcome / Not too much, not too little • CCy. R is associated with survival benefit • MMR is associated with durable CCy. R and may therefore decrease probability of relapse • CMR offers hope for treatment discontinuation (clinical trials only) • Results should be interpreted in the context of alternative options • Not failure criterion / QPCR in CCy. R
CML in 2013 • Imatinib, nilotinib, dasatinib are standard frontline Rx (except p 190 CML) • Dose optimization and adequate monitoring • Sub-optimal response – dose imatinib (400 mg → 800 mg) – New TKI • Failure – Dasatinib, nilotinib, bosutinib – Allogeneic SCT • T 315 I: ponatinib, omacetaxine
Questions? ejabbour@mdanderson. org Marcos. delima@uhhospitals. org
- Slides: 44