Clostridium Infections and Laboratory Diagnosis family Clostridiaceae genus
Clostridium Infections and Laboratory Diagnosis

(family): Clostridiaceae (genus): Clostridium (species): C. perfringens More than 200 species C. botulinum C. tetani C. novyi C. septicum C. haemolyticum

• Clostridium species are anaerobic or microaerophilic, spore-bearing microorganisms commonly found in environment and especially in the soil • These microorganisms, which are found as flora bacteria in the digestive system of humans and animals, cause diseases with toxins and vegetative forms affecting nerves, digestion, muscles and internal organs in many animal species
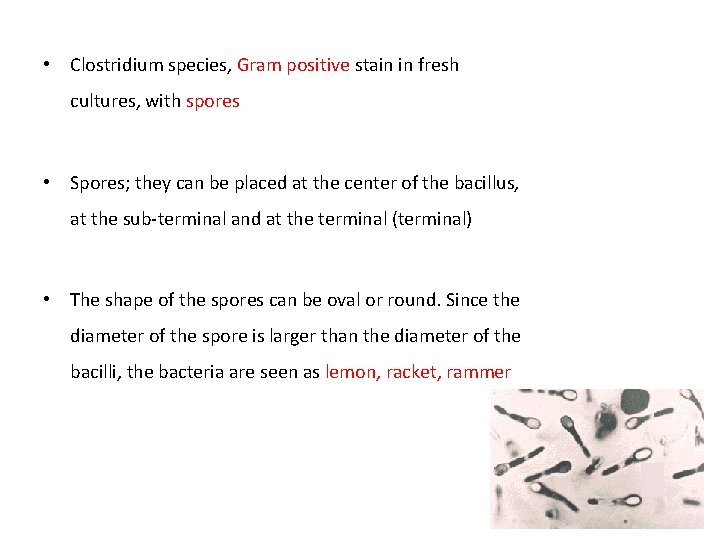
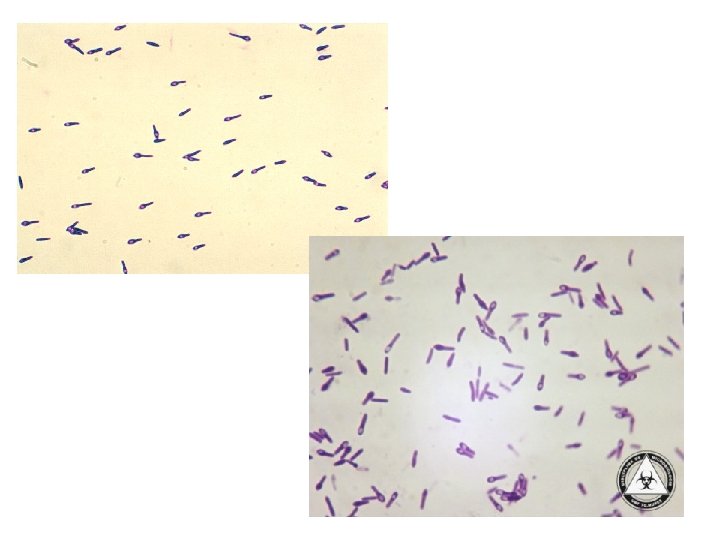
• Clostridium species, Gram positive stain in fresh cultures, with spores • Spores; they can be placed at the center of the bacillus, at the sub-terminal and at the terminal (terminal) • The shape of the spores can be oval or round. Since the diameter of the spore is larger than the diameter of the bacilli, the bacteria are seen as lemon, racket, rammer

• All species are catalase negative, oxidase negative • Moving species have peritric flagella • Motile and encapsulating • C. perfringens is immotile!!
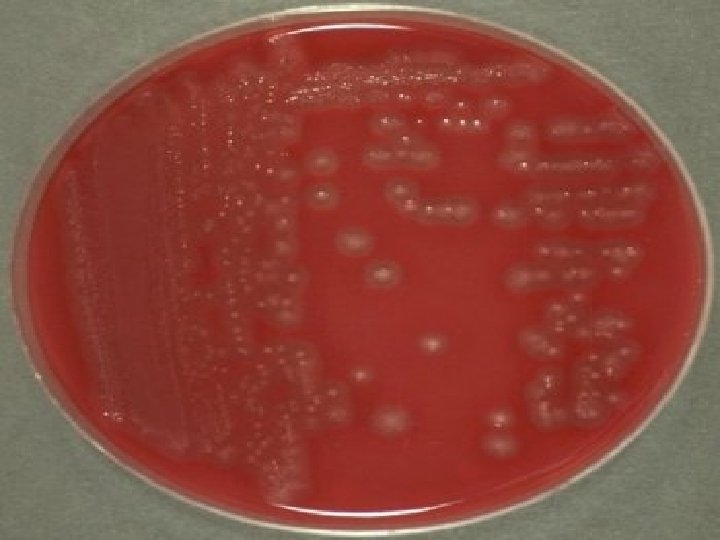
• Most are obligatory anaerobes and oxygen has a toxic effect at various degrees • 5% CO₂ environments are suitable for the production of the bacteria and this environment can be provided with commercial catalysts in the jar • The addition of blood and serum to the medium facilitates reproduction. They grow at 37°C • In 1 -2 days round, transparent, with filamentous colonies; hemolytic colony on blood agar
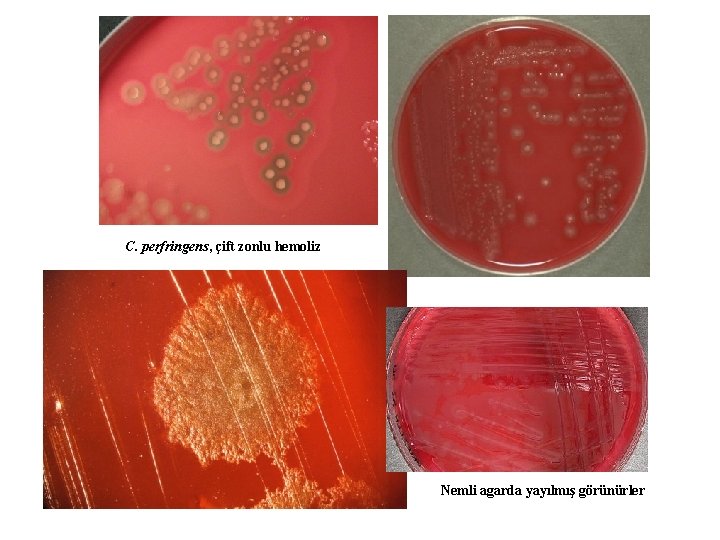
C. perfringens, çift zonlu hemoliz Nemli agarda yayılmış görünürler
• They have very strong toxins • Some are toxic to the intestine with enterotoxemi • Some toxins cause tissue necrosis • Clostridial infections occur in two ways: Ø From the outside by digestion or wound infection (exogenous) – Digestion; burns, botulism, enterotoxemia, basil hemoglobinuria – Wound; C. tetani, C. chauvoei, C. septicum Ø The agent found in the normal intestinal flora (endogenous) – Necrotic enteritis (C. perfringens)
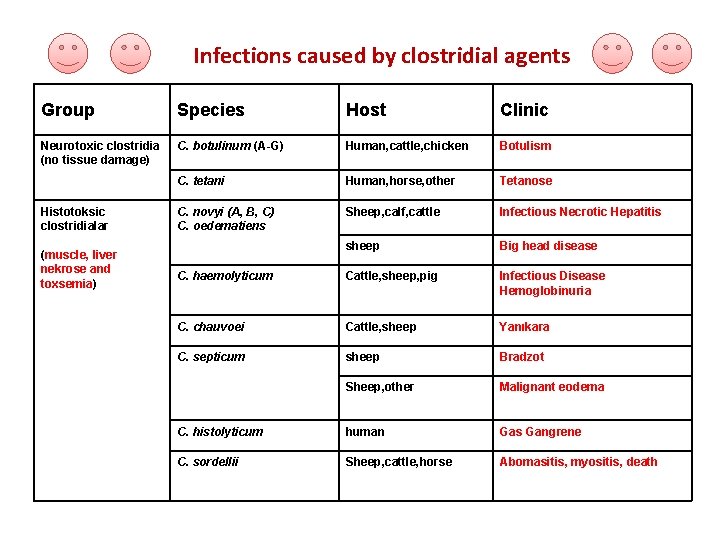
Infections caused by clostridial agents Group Species Host Clinic Neurotoxic clostridia (no tissue damage) C. botulinum (A-G) Human, cattle, chicken Botulism C. tetani Human, horse, other Tetanose C. novyi (A, B, C) C. oedematiens Sheep, calf, cattle Infectious Necrotic Hepatitis sheep Big head disease C. haemolyticum Cattle, sheep, pig Infectious Disease Hemoglobinuria C. chauvoei Cattle, sheep Yanıkara C. septicum sheep Bradzot Sheep, other Malignant eodema C. histolyticum human Gas Gangrene C. sordellii Sheep, cattle, horse Abomasitis, myositis, death Histotoksic clostridialar (muscle, liver nekrose and toxsemia)

Enterotocsemic / Enteropathogenic clostridia (inflammation, enterotoxemia, food poisoning) Other clostridia C. perfiringens Type A human Gas gangrene, food poisoning C. perfiringens Type B lamb Disanteria Calf, lamb Nekrotic enteritis Lamb, calf, piglet Hemorrhagic enterotoxemia sheep Enterotoxemia C. perfiringens Type D sheep Enterotoxemia (Soft kidney disease) C. perfiringens Type E Calf, lamb Enterotoxemia C. perfiringens Type F human Nekrotic enteritis C. difficile Human, rabbit Colitis due to antibiotic use C. perfiringens Type C C. argentinense C. spiroforme Botulism (experimental) rabbit Diarrhea C. butyricum Botulism, typ E C. baratii Botulism, type F

Important Clostridial species, toxins and clinical manifestations they form species Toxins Clinical picture C. botulinum Neurotoxin Botulism C. argentinense* Neurotoxin Botulism C. tetani Neurotoxin, tetanolysin Tetanus C. perfringens Alpha, beta, epsilon, Iota, enterotoxin, delta, theta, kapa, lambda, mu, neuraminidase Enteroto. Xemia, death, myonecrosis, diarrhea (food borne) C. difficile Toxin A ve B, CDT Colitis C. sordelii Alpha, beta, hemolizin Death C. novyi/C. haemolyticum Alpha, beta, gamma, delta, epsilon Death C. chauvoei/C. septicum Alpha, beta, gamma, delta Death C. histolyticum Alpha, beta, gamma, delta, epsilon Necrosis C. spiroforme Iota Diarrhea in rabbits C. butyricum Neurotoxin Botulism, type E C. baratii Neurotoxin Botulism, type F * C. botulinum tip G
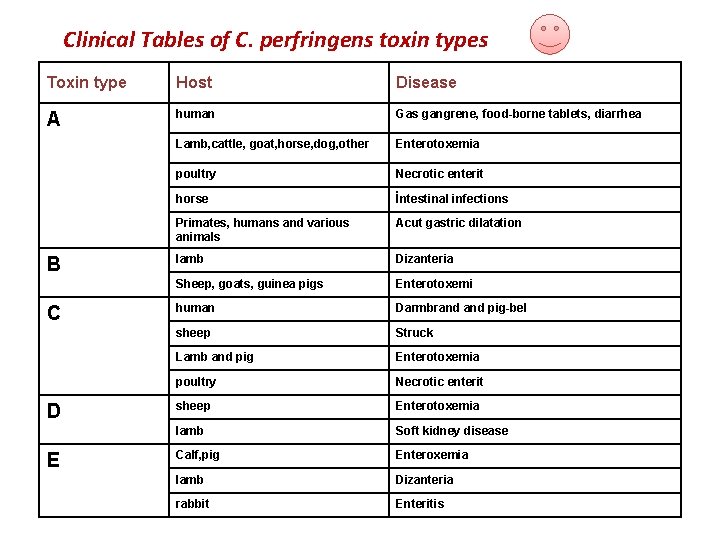
Clinical Tables of C. perfringens toxin types Toxin type Host Disease A human Gas gangrene, food-borne tablets, diarrhea Lamb, cattle, goat, horse, dog, other Enterotoxemia poultry Necrotic enterit horse İntestinal infections Primates, humans and various animals Acut gastric dilatation lamb Dizanteria Sheep, goats, guinea pigs Enterotoxemi human Darmbrand pig-bel sheep Struck Lamb and pig Enterotoxemia poultry Necrotic enterit sheep Enterotoxemia lamb Soft kidney disease Calf, pig Enteroxemia lamb Dizanteria rabbit Enteritis B C D E
NEUROTOXIC CLOSTRIDIA
Tetanus • Tetanus acute and fatal intoxication • Agent C. tetani • Gram positive rod • Compulsory anaerobic (85% nitrogen, 10% hydrogen, 5% CO 2) • The endospores are at the tip and 2 -3 times larger than the diameter of the bacillus (drumstick) • Motile, non-encapsulated, beta hemolytic, gray colony at 37ºC • Butanol, acetic and butyric acid which are the latest products of metabolism, produces burnt nail odor • Neurotoxin: tetanospasmin • Tetanospasmin is a very potent toxin that is split into two after it is released from the cell, which is caused by the bacterin protease (A-B toxin). Heat resistant. • Cytotoxin: tetanolin • Oxygen sensitive hemolysis. Lyse erythrocytes, macrophages and PMNLs. It is heat resistant and forms necrosis.
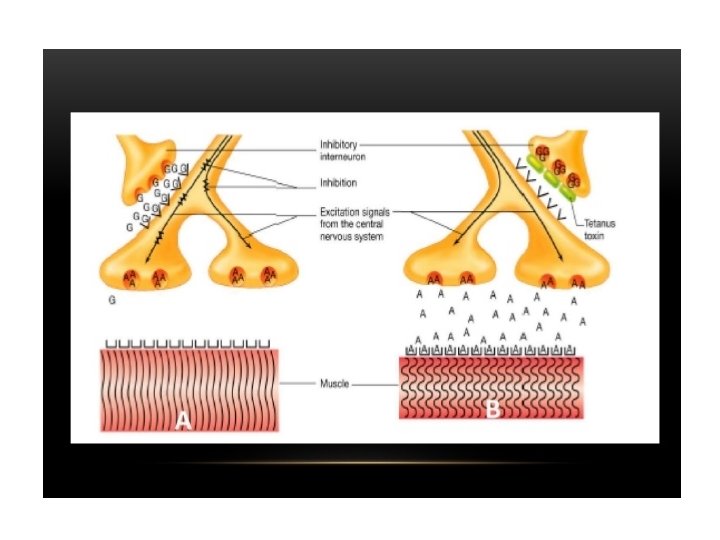
Epidemiology and Pathogenesis • The most sensitive saw-horse and human; medium, ruminant and pork; resistant, chicken • Infection occurs when the spores enters from impaired tissue • Other bacteria present in the wound and necrosis formation provide anaerobic environment • This causes C. tetani spores to turn into vegetative form • It does not spread in tissues, it first reproduces where it enters • After a few weeks, the tetanospasmin spreading to the muscles passes into the lymphatic system and into the blood • Tetanospasmin binds irreversibly to gangliosides in synaptic connections (nerve endings, spinal cord, brain) and inhibits the release of inhibitor-neurotransmitter (glycine) by providing hydrolysis of synaptobrevin. Therefore, acetylcholine (neurotransmitter) is continuously released and spastic paralysis (convulsive paralysis) develops • The toxin does not neutralize with antitoxin after binding to the receptor
Symptoms • General and local findings • Spasms spread throughout the body through the area of injury. • Dysphagia (difficulty swallowing), different facial expressions, muscle stiffness, respiratory insufficiency and death • The neonatal course is usually very severe and quite lethal
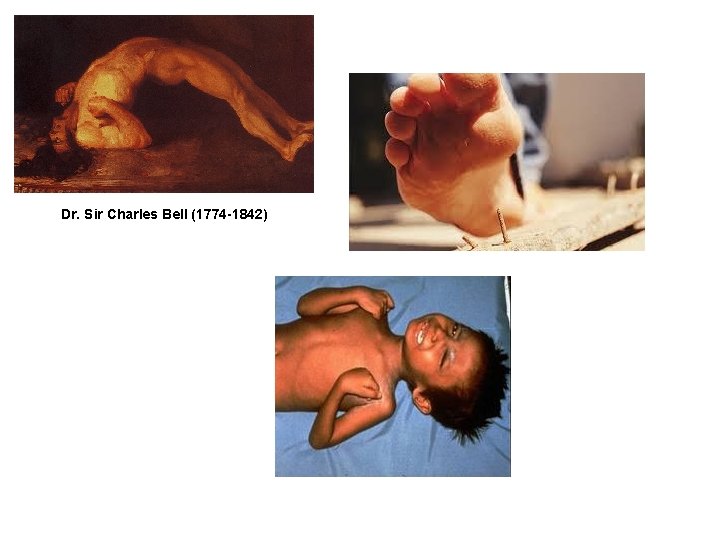
Dr. Sir Charles Bell (1774 -1842)
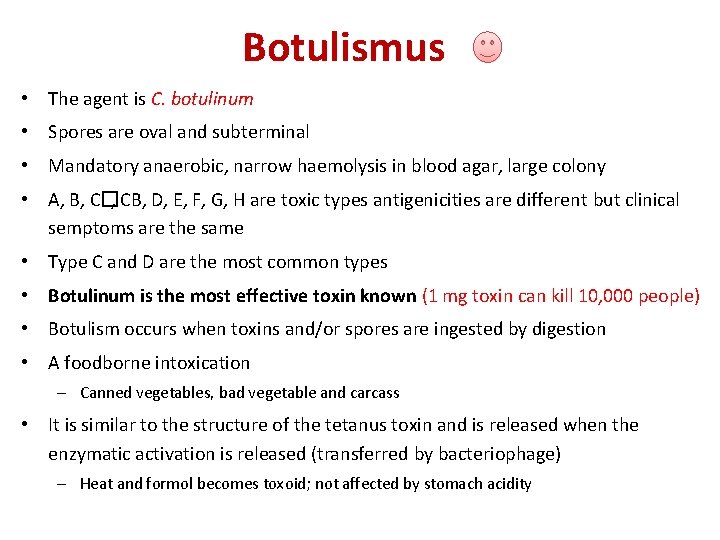
Botulismus • The agent is C. botulinum • Spores are oval and subterminal • Mandatory anaerobic, narrow haemolysis in blood agar, large colony • A, B, C�, CB, D, E, F, G, H are toxic types antigenicities are different but clinical semptoms are the same • Type C and D are the most common types • Botulinum is the most effective toxin known (1 mg toxin can kill 10, 000 people) • Botulism occurs when toxins and/or spores are ingested by digestion • A foodborne intoxication – Canned vegetables, bad vegetable and carcass • It is similar to the structure of the tetanus toxin and is released when the enzymatic activation is released (transferred by bacteriophage) – Heat and formol becomes toxoid; not affected by stomach acidity
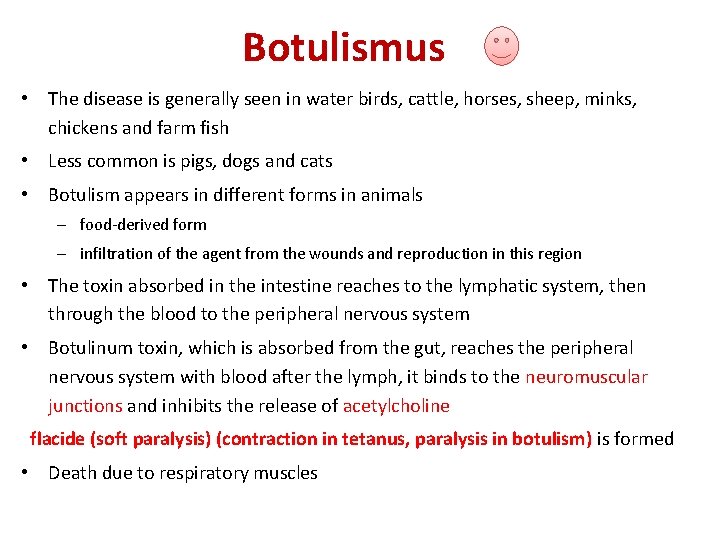
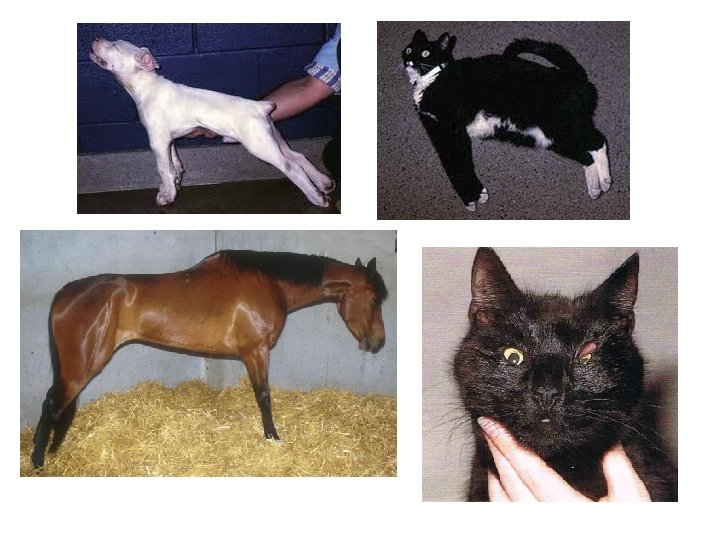
Botulismus • The disease is generally seen in water birds, cattle, horses, sheep, minks, chickens and farm fish • Less common is pigs, dogs and cats • Botulism appears in different forms in animals – food-derived form – infiltration of the agent from the wounds and reproduction in this region • The toxin absorbed in the intestine reaches to the lymphatic system, then through the blood to the peripheral nervous system • Botulinum toxin, which is absorbed from the gut, reaches the peripheral nervous system with blood after the lymph, it binds to the neuromuscular junctions and inhibits the release of acetylcholine flacide (soft paralysis) (contraction in tetanus, paralysis in botulism) is formed • Death due to respiratory muscles
• Botulism, – Transmitted by the defeat of the silo-winged poultry litter used as scattering or litter. – Consuming bad quality bale stalk, silage or rodent carcass containing feed – Canned meat, spoiled vegetables in humans • Symptoms develop within 1 -17 days • Intense pupil, dry mucous membranes, soft tongue, incoordination, lying on the back, paralysis progressing, paralysis and complete paralysis, death resulting in respiratory muscles affected, severe paralysis after limb wing and neck fall (limberneck)

HISTOTOXIC CLOSTRIDIA
• It enters from the wound or digestive system and is influenced both in the region where it enters and generalize • The dormant spores in the tissues turn into vegetative form and the toxins cause necrosis to death. • C. chauvoei, C. septicum, C. novyi, C. haemolyticum, C. sordellii
Black Disease • C. chauvoei (alpha toxin, hyaluronidase, beta, gamma, delta) • Mandatory anaerobic, spore terminal and subterminal, motile, hemolytic colony • It is an acute and fatal disease characterized by myositis of muscles in the gluteal region of sheep and cattle. • The disease is mostly seen in summer and autumn • Disease; ü from digestive tract by feed and water ü wounds in the mouth and during birth ü castration, coach injury in sheep ü The agent should reach the muscles by the way in which it is taken. • Bowel-lymph-blood-frame
• In both cattle and sheep, exotoxins produced by bacteria that grow in the muscles cause gangrenous, cellulitis and myositis and death usually occurs in a short time • Muscles of the legs, back and neck are affected. Lumpiness, bloating and gas accumulation (creeping sound) occur • Myocardial and diaphramatic lesions may cause sudden deaths without an initial finding
Malignant Edema and Gas Gangrene • C. septicum Malignant edema • C. perfringens type A • In addition C. novyi type A, C. chauvoei and C. sordellii • C. septicum (alpha, beta, gamma and delta toxin and neurominidase important) • It is a characteristic infection with soft tissue necrosis • Limited necrosis and gas in malignant edema; The gas gangrene develops in the Gaseous gangrene larger area • Malignant edema is an acute, toxic and lethal disease characterized by inflammation of the abomasum mucosa in young sheep
• The disease occurs more frequently in the autumn months, when the frozen grass is fed and it is more common in those who are fed with high ration, especially in terms of carbonhydrates. • The bradzot formed after the ingestion of the agent by the digestive system, It is seen that the agent causes the inflammation of abomasum and causes sudden death after toxemia • Malignant edema occurs when the agent enters the body from wounds • Gas gangrene is characterized by diffuse edema (crepitation), extensive bacterial invasion in damaged muscle

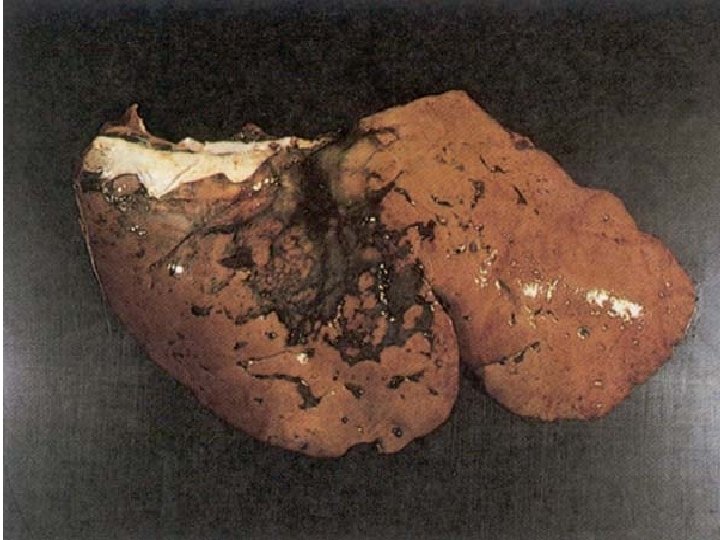
Infectious Necrotic Hepatitis • C. novyi Type B (C. oedematiens) • Infectious necrotic hepatitis is an acute, toxic infectious disease characterized by liver necrosis in sheep • These microorganisms are examined in three groups as A, B and C according to their toxin types – Type A (alpha, gamma, delta, epsilon); Type B (alpha, beta, zeta); Type C (gamma) • Strains identified as Type D in previous years have been named C. haemoliticum • C. novyi creates two different disease setting. The first is infectious necrotic hepatitis in sheep and cattle, and the second is large head disease in sheep
• In Infectious necrotic hepatitis, the agents taken by the digestive tract reach the liver (dormant spore) and after the reproduction lesions formed by toxins are seen • Liver damage caused by liver parasites (Fasciola hepatica) provides an environemnt for reproduction of C. novyi. In this form, sudden death occurs in animals before any clinical symptoms occur • In the clinical form defined as large head disease in the sheep, the edema that occurs after the reproduction of the agent which enters the body from head wound and their toxins • Subcutaneous bleeding skin gets black color and is called black disease
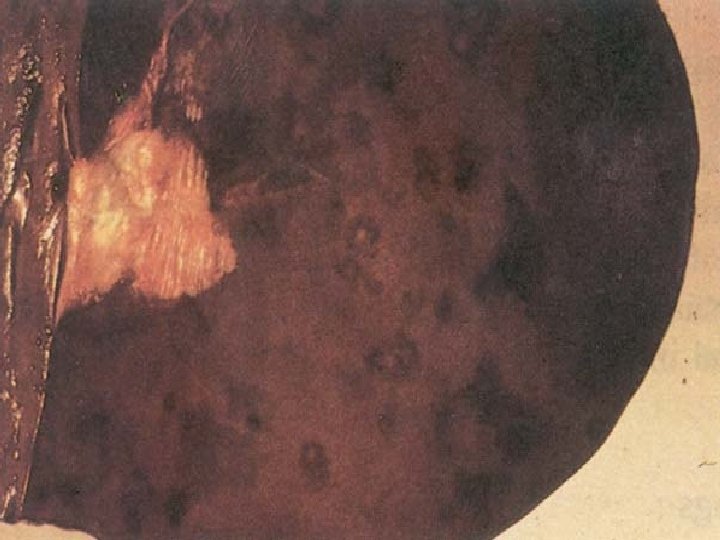
Infectious Iterohemoglobinuria • C. haemolyticum • This disease is characterized by high fever, hemoglobinuria and icterus, also seen in sheep, cattle, goats and pigs • Beta toxin (lecithinase) of the agent is very important in pathogenesis and is formed by vegetative bacteria • This toxin causes both necrosis in the liver and haemolysis of blood cells in the veins
• The disease is mostly seen in summer and autumn, and the agent taken by gi-tract reaches the liver by blood path • There is a relationship between the parasites that settled in the liver and the outbreak of the disease • In affected animals, high fever, stagnation, red color, blood in stool and in urine • Jaundice is seen in mucous membranes and there is abort in pregnant animals • Mortality is high and up to 90 -95%
C. sordellii infection • It has smiliar disease setting with malignant oedema • It is isolated from the cases characterized by gas and ulcers in the cattle and in young sheep and in cases of sudden death
ENTEROTOXEMIC / ENTEROPATHOGENIC CLOSTRIDIA
Enterotoxemi • C. perfringens • Clostridial entorotoxemics are acute and highly fatal intoxications affecting sheep, lamb, cattle, piglets and rats rarely • In animals, C. perfringens types B, C and D are rarely caused by these types of exotoxins of type A and E. • There are five types (A-E) according to the type of toxin formation
Clostridium perfringens • immotile • encapsulated • aerotolerant • Short rod • Spores oval and subterminal • Double-zone hemolysis – First zone caused by theta, the second zone caused by alpha toxin • Fast growing on mixed culture and at 45 ° C are the distinguishable characters
C. perfringens toxins • Lethal toxins – alpha toxin, lecithinase, C. perfringens types A, B, C, D and E – iota is only type E, activated by trypsin – beta toxin types B and C, are inactivated with trypsin – epsilon is synthesized by types B and D, activated by trypsin • Other (minor) toxins related to pathogenicity – tetra (hemolysin), kapa (collagenase), mu (hyalurinidase) and nu (DNAse) tissue damage. • Enterotoxin – Type A, C and D
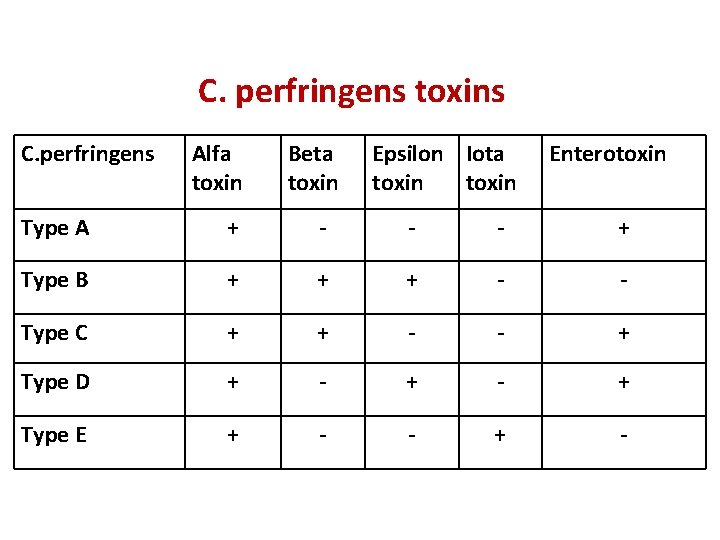
C. perfringens toxins C. perfringens Alfa toxin Beta toxin Epsilon Iota toxin Enterotoxin Type A + - - - + Type B + + + - - Type C + + - - + Type D + - + Type E + - - + -
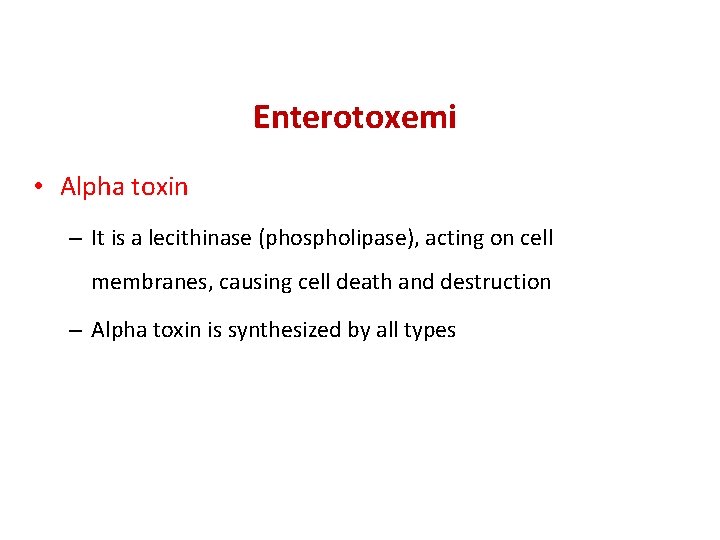
Enterotoxemi • Alpha toxin – It is a lecithinase (phospholipase), acting on cell membranes, causing cell death and destruction – Alpha toxin is synthesized by all types
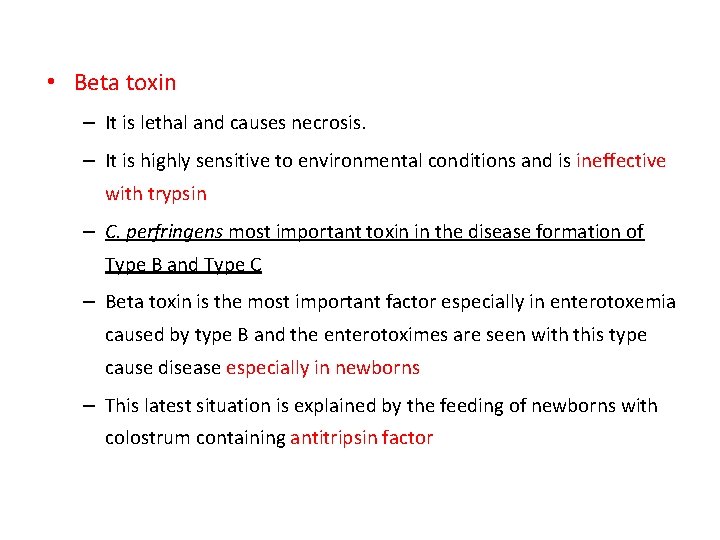
• Beta toxin – It is lethal and causes necrosis. – It is highly sensitive to environmental conditions and is ineffective with trypsin – C. perfringens most important toxin in the disease formation of Type B and Type C – Beta toxin is the most important factor especially in enterotoxemia caused by type B and the enterotoximes are seen with this type cause disease especially in newborns – This latest situation is explained by the feeding of newborns with colostrum containing antitripsin factor
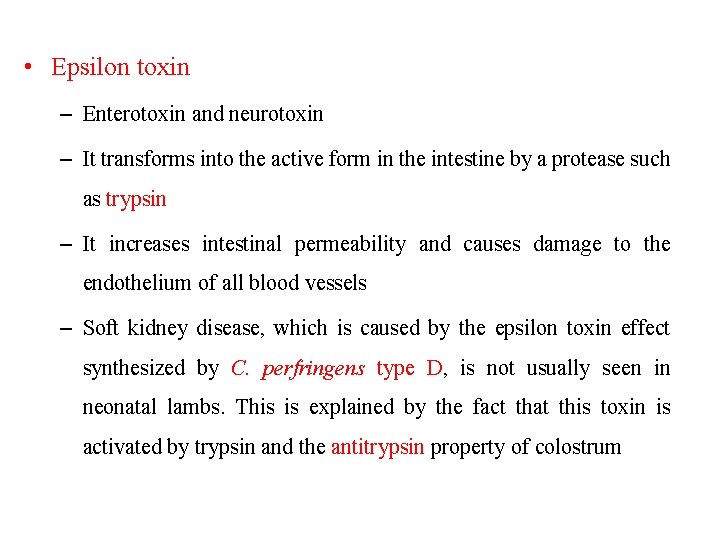
• Epsilon toxin – Enterotoxin and neurotoxin – It transforms into the active form in the intestine by a protease such as trypsin – It increases intestinal permeability and causes damage to the endothelium of all blood vessels – Soft kidney disease, which is caused by the epsilon toxin effect synthesized by C. perfringens type D, is not usually seen in neonatal lambs. This is explained by the fact that this toxin is activated by trypsin and the antitrypsin property of colostrum
• Iota toxin – This toxin is released as protoxin and is released by C. perfringens type E and C. spiroforme and C. difficile – The effect of this toxin is not clearly understood
• C. perfringens is a pathogenic strain that is very common in an environment • It is also found in the intestines of humans and animals • While the vegetative forms of the bacteria are sensitive to environmental conditions, their spores continue to live for several months
• Poor breeding conditions and environmental factors lead to increased enterotoxemia cases in animals • These factors include sudden changes in feeding (often in transition to rich diets), feeding with overfat, obesity, high protein and energy rich diets • The above factors provide a suitable environment for reproduction of C. perfringens as a result of peristaltic reduction in the intestines and inadequate digestion of carbohydrates • after the overgrowth of C. perfringens found in the flora normally, the large amount of toxins reaches to small intestine and absorbed from this region, the enterotoxemia is formed
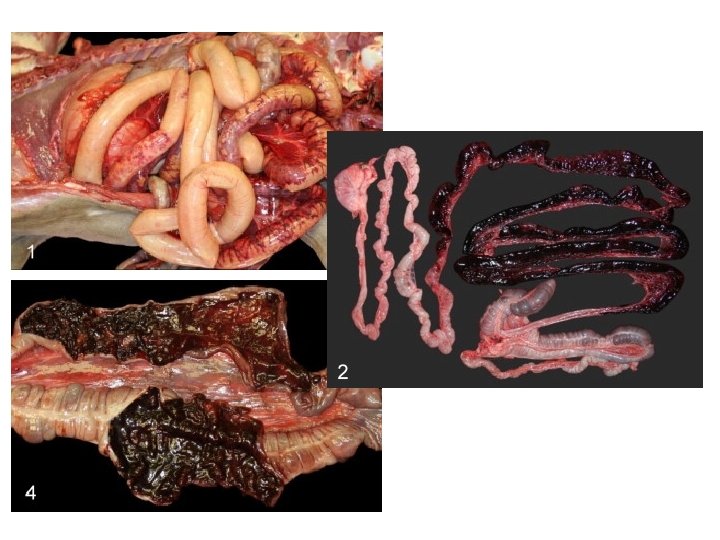
• The clinical symptoms caused by C. perfringens are mainly formed by Type B, Type C and Type D in animals. • The lamb dysentery formed by Type B is characterized by early deaths (2 -5 days), especially those that suddenly start in animals in the first weeks of colostrum. Mortality in the disease reaches up to 30% and is more common in certain regions of the world. • Infection with C. perfringens type C is defined as struck in sheep and is an acute enterotoxemia. It is seen in adult sheep and is dominant in certain geographical areas. In this table, sudden deaths are noticed without any additional findings
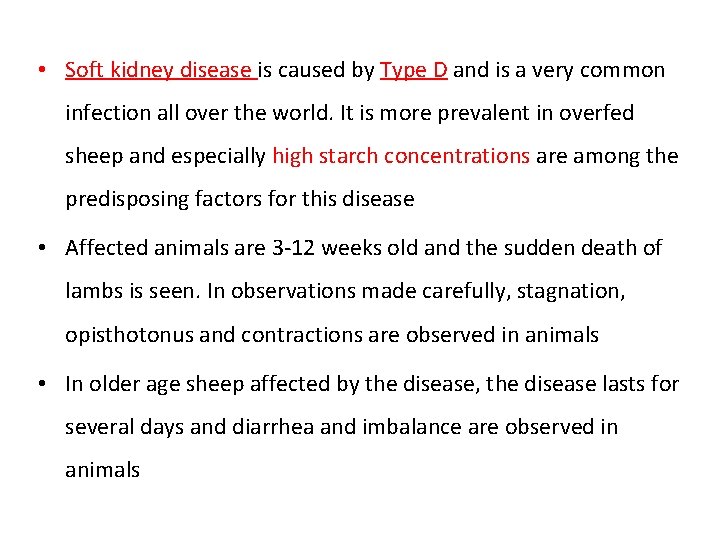
• Soft kidney disease is caused by Type D and is a very common infection all over the world. It is more prevalent in overfed sheep and especially high starch concentrations are among the predisposing factors for this disease • Affected animals are 3 -12 weeks old and the sudden death of lambs is seen. In observations made carefully, stagnation, opisthotonus and contractions are observed in animals • In older age sheep affected by the disease, the disease lasts for several days and diarrhea and imbalance are observed in animals
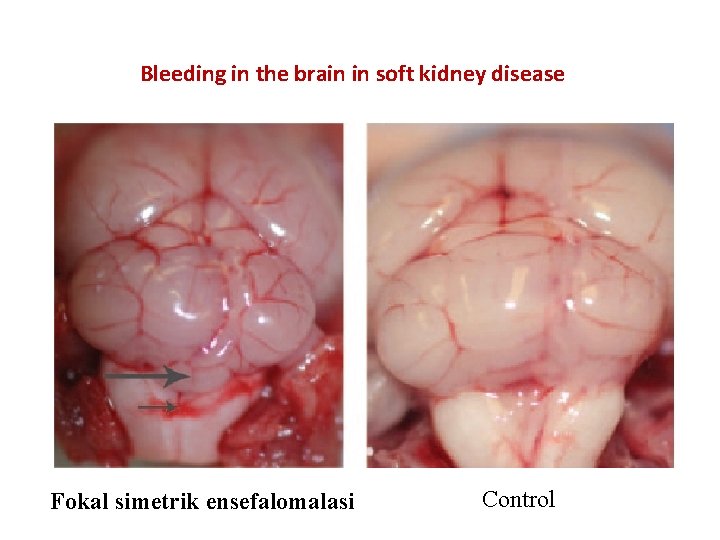
Bleeding in the brain in soft kidney disease Fokal simetrik ensefalomalasi Control
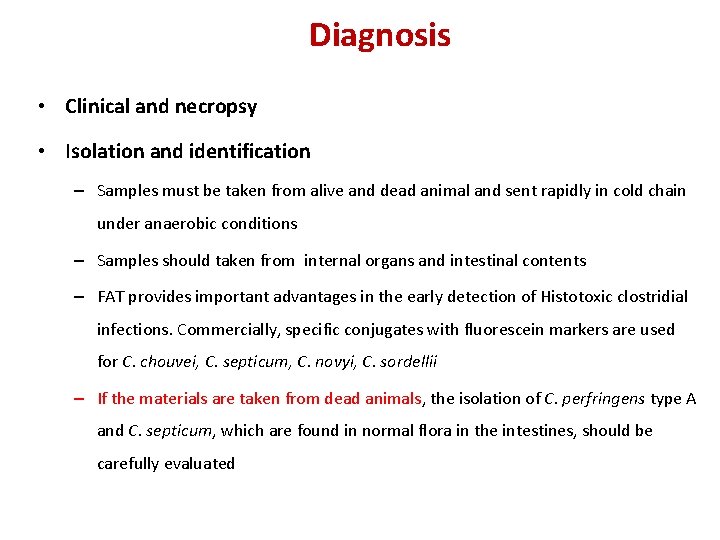
Diagnosis • Clinical and necropsy • Isolation and identification – Samples must be taken from alive and dead animal and sent rapidly in cold chain under anaerobic conditions – Samples should taken from internal organs and intestinal contents – FAT provides important advantages in the early detection of Histotoxic clostridial infections. Commercially, specific conjugates with fluorescein markers are used for C. chouvei, C. septicum, C. novyi, C. sordellii – If the materials are taken from dead animals, the isolation of C. perfringens type A and C. septicum, which are found in normal flora in the intestines, should be carefully evaluated
• Inoculation to laboratory animal – Isolation – Detection of toxin – Toxin neutralization tests • Serology • Molecular techniques




Laboratory Test • The agents are sensitive to the environment as they are anaerobes • So samples should be taken from live or newly dead animals • Otherwise, the results are wrong bacause of the agents which are found in flora (C. perfringens, C. septicum)
• Samples should be taken under the anaerobic conditions and immediately cultured in the laboratory • For example; affected tissues, internal organs and bowel contents should be taken
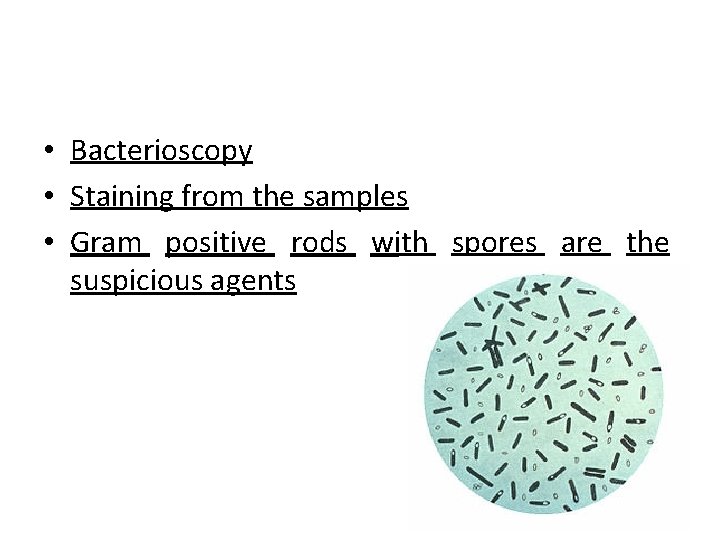
• Bacterioscopy • Staining from the samples • Gram positive rods with spores are the suspicious agents
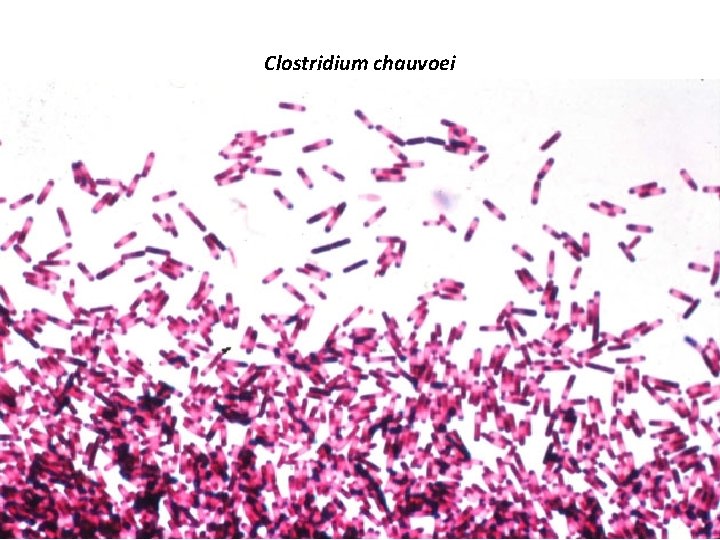
Clostridium chauvoei
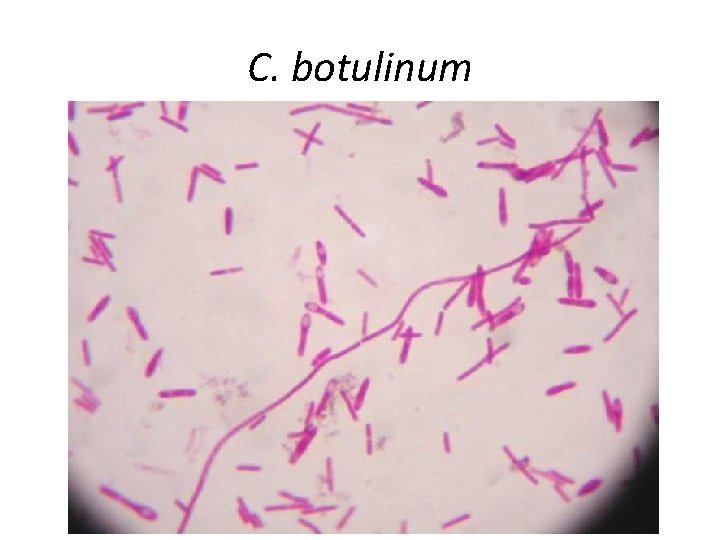
C. botulinum
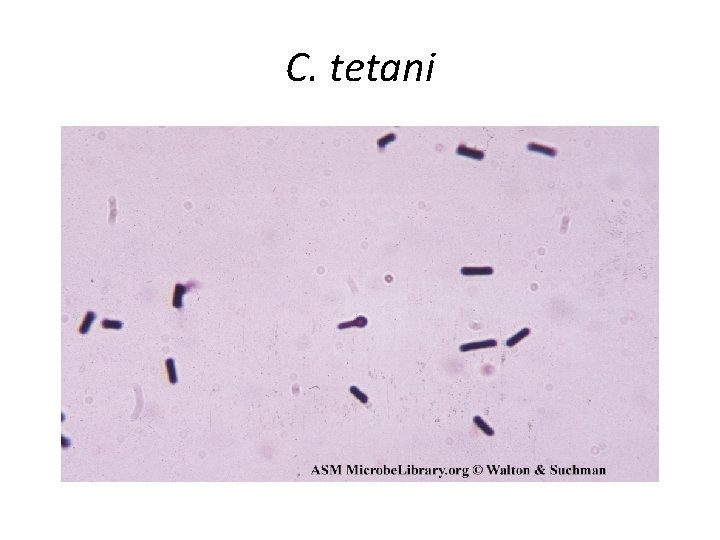
C. tetani
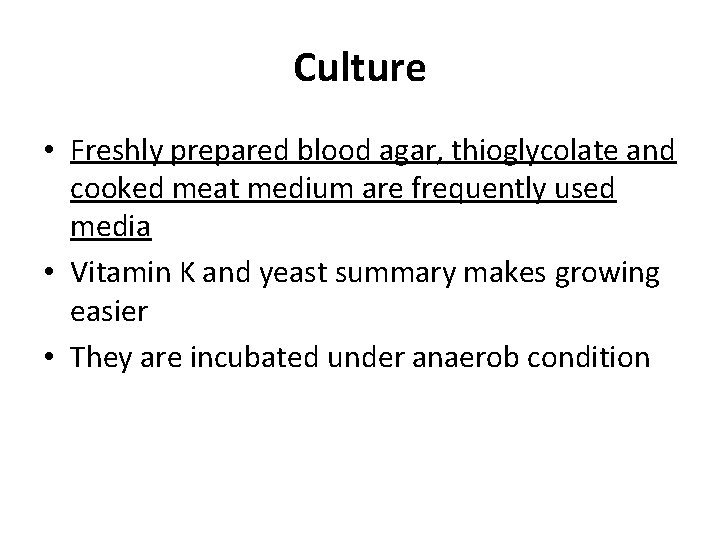
Culture • Freshly prepared blood agar, thioglycolate and cooked meat medium are frequently used media • Vitamin K and yeast summary makes growing easier • They are incubated under anaerob condition

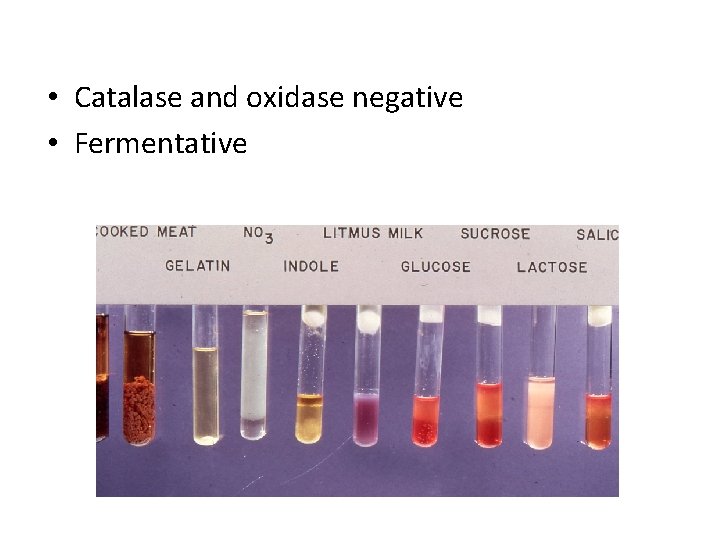
• Catalase and oxidase negative • Fermentative
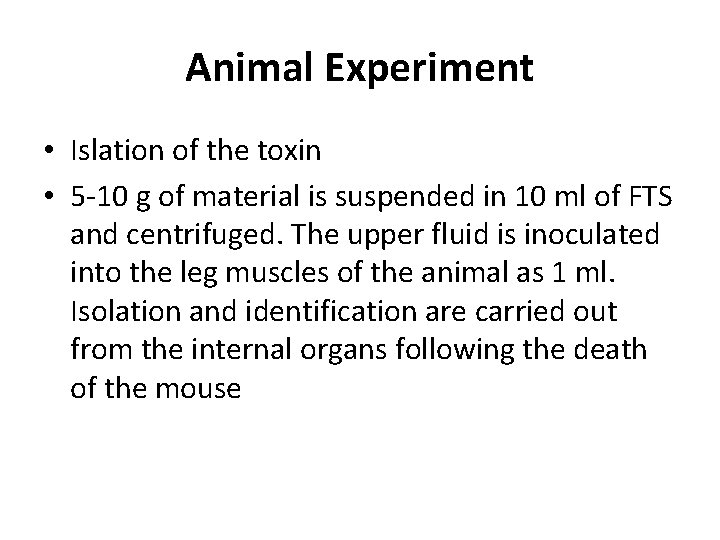
Animal Experiment • Islation of the toxin • 5 -10 g of material is suspended in 10 ml of FTS and centrifuged. The upper fluid is inoculated into the leg muscles of the animal as 1 ml. Isolation and identification are carried out from the internal organs following the death of the mouse
Toxin Neutralization Test • The toxin-containing suspension that is inoculated into the mice after the presence of toxin is detected, is given to the mice as either IV or ID by mixing with each commercial antitoxin (C. perfringens A-E antitoxins in the intrinsic enterotoxems). The immortal antitoxin group indicates the type of toxin present in the intestinal contents
Treatment • In Enterotoxemia, the chance of treatment is very low because the cases are acute. • In infections caused by histotoxic clostridials characterized by gas gangrene and basil hemoglobinuria, penicillin and broad spectrum antibiotics are used early, in the course of treatment • Treatment of all cattle with antibiotics in a herd that has black disease, provides useful results. • Symptomatic treatment with high doses of penicillin or broad spectrum antibiotics and antitoxin in tetanus; giving antitoxin is useful in botulism
Protection and Control • Maternal immunity – 2 to 12 weeks after birth • Vaccinations – Inactivated vaccines (toxoid, main culture)
• Toxoid vaccines are used in the control of tetanus in farm animals. It is administered in a single dose • It is useful to clean the wound and to wash it with antiseptic when injured. If the injured animal is vaccinated, antitoxin is administered. Protect for 3 weeks
• Vaccination for histotoxic and enterotoxic Clostridium is an indispensable procedure for protection and control. • Combined vaccines are used in area. The first dose is made on 3 -4 months old animals and is repeated after 3 -4 weeks. Repetition every year is sufficient for protection. • Vaccination to pregnant animals one month before birth is effective in protecting newborns with maternal immunity.
Vaccination schedule • • • Identification of diseases in operation Observation of Clostridial infections Maintenance-management conditions in operation Determination of the first vaccination time Second vaccination Repeat of vaccination
- Slides: 76