CLOSTRIDIAL DISEASES Introduction Clostridial diseases are caused by

CLOSTRIDIAL DISEASES

Introduction Ø Clostridial diseases are caused by bacteria of the genus Clostridium. (ANAEROBES) Ø Clostridia are widespread in the environment and are normally found in soil and faeces. Ø They are also present in the gastrointestinal tract and as spores in tissues of healthy animals.

CLASSIFIACTION The clostridia can be divided into four major groups according to the kind of disease they produce.

The Histotoxic clostridia causes a variety of tissue (often muscle) infections frequently following wounds or other trauma (eg). Cl. chauvoei Cl. septicum Cattle, sheep (pigs) Many Spescies Cattle Sheep Chicken Black quarter (Black leg) Malignant oedema Equne. Braxy Necrotic dermatitis Cl. novyi Type A Sheep Cattle and Sheep Big head of rams Gas gangrene Type B Sheep (Cattle) Black disease (necrotic hepatitis) Type C Water buffaloe Osteomyelitis

Hepatotoxic clostridia produces their toxins in the liver, thus resulting in the disease Bacillary haemoglobinuria and Black disease (Eg. ) C. haemolyticum Cattle, (sheep) Bovine Bacillary haemoglobinuria C. sordellii Cattle, Sheep, Horses Gas gangrene C. colinum Birds Quail disease, Ulcerative enteritis C. piliforme foals, laboratory animals Calves, dogs and cats
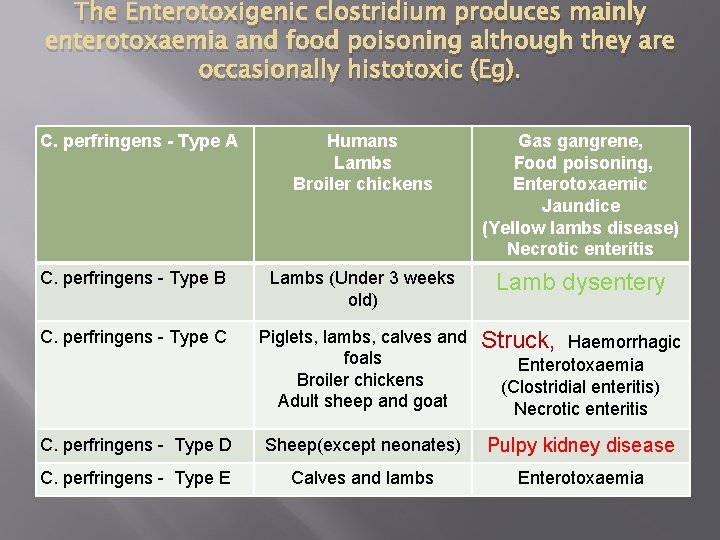
The Enterotoxigenic clostridium produces mainly enterotoxaemia and food poisoning although they are occasionally histotoxic (Eg). C. perfringens - Type A Humans Lambs Broiler chickens Gas gangrene, Food poisoning, Enterotoxaemic Jaundice (Yellow lambs disease) Necrotic enteritis C. perfringens - Type B Lambs (Under 3 weeks old) Lamb dysentery C. perfringens - Type C Piglets, lambs, calves and foals Broiler chickens Adult sheep and goat Struck, Haemorrhagic C. perfringens - Type D Sheep(except neonates) Pulpy kidney disease C. perfringens - Type E Calves and lambs Enterotoxaemia (Clostridial enteritis) Necrotic enteritis

The Neurotoxic clostridia cause the disease by the production of the potent exotoxins (Neurotoxins) (eg. ) C. tetani Tetanus C. botulinum Botulism
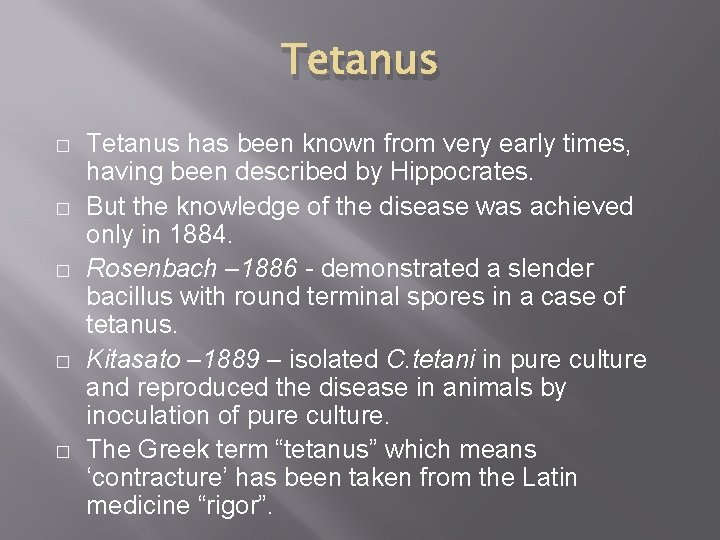
Tetanus � � � Tetanus has been known from very early times, having been described by Hippocrates. But the knowledge of the disease was achieved only in 1884. Rosenbach – 1886 - demonstrated a slender bacillus with round terminal spores in a case of tetanus. Kitasato – 1889 – isolated C. tetani in pure culture and reproduced the disease in animals by inoculation of pure culture. The Greek term “tetanus” which means ‘contracture’ has been taken from the Latin medicine “rigor”.
HABITAT � � � Soil, especially that contaminated by animal faeces, is the natural habitat as C. tetani is often transient in the intestines of horses and other animals. It is ubiquitous and has been recovered from a wide variety of other sources, including street and hospital dust, cotton wool, bandages, catgut, plaster of paris, clothing etc. It may occur as an apparently harmless contaminant in wounds.

tetnus � � Synonym : Lock jaw Definition Acute fatal infectious disease of man and animals characterized by involuntary contraction of voluntary muscles caused by toxins of Clostridium tetani Horse is more susceptible and birds is resistant.

Tetanus � � � Aetiology Clostridium tetani Exotoxin - CI. Tetani - Gram positive sporulating, anaerobic, rod shaped anaerobe, Spores – “Drum Stick” Incidence Tetanus occurs in all parts of the world

Tetnaus Susceptibility � Hores and mules are susceptible Transmission � Wound infection
Pathogenesis The organisms enter the body through the nail prick, castration, docking, shearing, umbilical wound (tetanus neonatorum) or during parturition � Anaerobic condition allows germination of spores and release exotoxin � Reaches brain ether blood circulation or through nerve �
Pathogenesis � The tetanus toxin gets fixed to a substance called protagon ( made of cerebroside + oligosaccharides) in the nervous tissue. � It acts on the inhibitoty synapses interfering with the action of the inhibitory transmitter thus producing spastic action � The toxin causes hyperirritability responsible for the tetanic spasms.

Tetnaus Three types of toxins � Haemolysin – Tetanolysin – Not important � tetanospasmin- Neurotoxin - responsible for the nervous symptoms � Fibrinolysin- not very potent
Tetnaus � The toxin causing spasmodic contraction of muscles, stiffness and immobilization.
symptoms � � � Contraction of muscles Arched back Twisting neck Dropping of third eyelid Convulsions Sensitive to loud sound.
Tetanus � � � Clinical signs Involuntary, persistent, intense painful contraction of one or more group of muscles. Horse- Stiffness and moves like 'wooden horse'. Raised Tail, third eyelid Protrusion, and Stiffness of Jaw muscle -‘ Lock Jaw’ Ruminants – Symptoms are less severe
Tetanus � � � Gross lesion No characteristic lesion Death due to Toxaemia Microscopic lesions No specific microscopic lesions. Degeneration of the neurones in the brain and spinal cord (due to anoxaemia)
Tetanus � � � Diagnosis Characteristic clinical signs. Organisms are local but not septicaemic Demonstration of toxin in the serum

BOTULISM Definition � Botulism is a rapidly and fatal motor paralytic condition caused by ingestion of CIostridium botulinum exotoxin. � Botulism is a food poisoning, the toxin being elaborated as an exotoxin by CIostridium botulinum.
� � � For the poisoning to occur, the toxin should be present in the food before ingestion, since the organism cannot generate the toxin in the alimentary tract A, B, C, D, E, types A – Limber neck – Poultry D – Lamsiekte C – Forage poisoning in horses E – Fish and fish products
Botolisum � � � By clostridum botulinum Disease which occur by ingestion of pre-formed toxin. The toxin donot enter CNS but affect PNS. The toxin block release of acetylcholine The toxin through blood or nerves reach PNS and inhibit release of inhibtory neurotransmitters like GABA, glycine etc. Due to this muscle remain in relaxed state.
Botolisum � � � The disease is also known as Bulbar paralysis or loin disease. The animal died of respiratory paralysis. In birds disease is known as Limber neck and in hourse also known as Shakers foal syndrome.
� � � Clinical signs Cattle -Pica-Chew bones (due to deficiency of phosphorus) which may contain toxin in the decaying meat and get poisoning. Cattle and Horse: Forage Poisoning (Ingestion of hay contaminated with dead animals or poultry litter) Wound botulism – Horses Salivation, paralysis with difficulty of movement and impaired vision. Tongue paralysed leads to swallowing is impossible.
� � � Swine are resistant since the toxin is poorly absorbed. Botulism in birds is exhibited by torticollis – ‘Limber neck’ caused by eating infected blow fly maggots and vegetable matter Head and neck droop Death – Respiratory failure and asphyxia No characteristic lesions
Entertoxaemia � � � There are 5 strains and there production of toxins A – alpha – Gas gangrene, food poisoning in human. B – alpha, beta, epsilon & iota - Lamb dysentery, Hemorrhagic enteritis in sheep & goat. C – alpha, beta - Struck in sheep & enteritis in lambs, calves & piglet. Enteritis necroticans ( Human) D – alpha& iota- Enterotoxaemia in sheep & Pulpy Kidney E –alpha& iota- Enterotoxaemia in Calves and Lambs.
� � � � � Cl. Perringens ( H, Co 2 Gas formation in tissue) Exotoxin Alpha – Toxin Phospholipase Phosophlipids Phospholipid lecithin Which is in cell wall of RBC, WBC & Muscle cells Produce characteristic hemolysis & myconecrosis Myconecrosis with accompanying gas formation known as Gas gangrene.

� � � Cl. Per produce multiple other pathogenic toxin heat- labile entrotoxin which causes Cl. Food poisoning manifested abdominal pain & Diarrhea The typical synerio involves meat i. e kept warm for long period of time alowing spore to germinate & produce bacteria in vegiate state that produce exotoxin. Cl. Food poisoning rerarly fatal but gas gangrene can be rapidly lethal & lead to shock unless to death.
� CI. perfringens type ‘A’ Enterotoxaemia occurs in lamb and calves Haemolytic anaemia, Haemoglobinuria and Icterus - acute syndrome
Lamb dysentery � � � � � CI. perfringens type ‘B’ Lamb – Less than 3 weeks Also occurs in calves and foals Haemorrhagic enteritis with ulceration Beta toxin Acute – Abdominal pain, depression and reluctance to suckle Peracute -death without symptoms Microscopic lesions : Haemorrhagic enteritis and ulceration.
‘Struck’ CI. Perfringens type 'C' Adult Sheep – Haemorrhagic enteritis and ulceration of Jejunum and duodenum Peritionitis with large volume of clear yellow fluid accumulation Another form -CI. Perfringens type 'C' – Haemorrhagic enterotoxaemia Affects lambs, calves and piglets within a few days of birth and fatal �

“Puply Kidney disease”, Synonym - “Over eating disease” Definition Acute toxaemia of fattening lambs and sheep which receive sample milk and high concentration of diet characterized by nervous symptoms and sudden death with development of pulpy kidney �
“Puply Kidney disease”, Incidence � It is occurs throughout the world including India � Susceptibility It is an important disease of goats, sheep (fattening lambs) and less commonly in adult sheep Enterotoxaemia has also been reported in calves �
Pathogenesis � Organism is a normal inhabitant of alimentary tract and the toxin produced are removed by normal movement of ingesta � When excessive starch food is fed, the bacteria proliferate and liberate toxin. Hence the name “Over eating disease” Atony of intestine & Stasis of ingests also favours growth of organisms The epsilon toxin produced will be abosrbed immediately by intestinal mucosa resulting in toxaemia � �
� Smaller quantities of alpha and beta fractions � Toxins reaches the brain causing opisthotonus, convulsion and coma. � Toxaemia (Few hours - chronic convulsions) � Hyperglycaemia and glycos uria are also observed
Gross lesions � � Petechial or ecchymotic haemorrhages of epicardium, endocardium, serous surface of intestine, abdominal muscles, diaphragm and hydropericardium Catarrhal or haemorrhagic gastroenteritis Kidneys – swollen and pulpy – “Puply Kidney disease” Reaching the brain causing symmetrical encephalomalacia
Microscopic lesions � � Kidney: Cloudy swelling and necrosis of epithelium of proximal convuluted tubules Liver and spleen- Congested Brain: Lysis and liquefaction of the white matter, while the grey matter is oedematous. Hyperglycaemia due to increased glycogenolysis of liver glycogen

BLACK QUARTER � � � Synonym: Black leg, quarter ill, Symptomatic anthrax Definition Acute febrile disease of cattle (6 month to 2 years), less often of sheep, goat and swine characterized by emphysematous, sero haemorrhagic swelling in the heavy muscles, especially of the hind limbs.

BQ � Etiology Clostridium chauvoei - Gram + (positive), spore forming, rod shaped bacterium

BQ � This disease is spread generally in Rainey Season.
BQ � Incubation period: 1 - 5 days
Pathogenesis � Infection is by ingestion of spore of Cl. Chauvoi The organisms multiply in the intestinal mucosa. Goes into the intestinal macrophase Inters the lymph & blood Precipitates' in the heavy muscle of thigh& limb & shoulder.
BQ During devitilization , when some injury to the muscles anaerobic condition sets up. ( due to wound or heave exercise anaerobic condition developed) The bacteria vegetates in bacilli form. start causing necrosis by release of toxins. Causing emphysematous necrotizing myositis of the muscles. Black gas gangrenous muscles with crepitating sound. �
BQ Filled with serosaguinous fluid ( foul smelling) � Fe. S deposition Toxemia Death within 24 hrs to 60 hrs. Death may be due to toxaemia
� Different types of toxins are releases by Cl. Chauvoea α – toxin is most imp toxin. β γ δ These toxins causes necrosis of muscles ( Gluteal) Here breakdown of RBC lysis ---- Iron is release & due to necrosis of muscle H 2 S is release.
BQ � H 2 S + Fe = Fe 2 S - which is black in colour of affected muscles. � Release of gas is due to fermentation of sugar in anaerobic medium.
BQ � � � Clinical signs Fever lameness, visible swelling of muscles- Tongue, diaphragm, myocardium and gluteal muscles In early stages, the swelling is hot and painful to the touch but soon cold and painless and oedema and emphysema can be felt
Gross lesions � � � � Crepitating swelling of the muscle(extremities) Rubber sponge and dark brown or black sero sanguineous fluid exudes with gas bubbles -Gas gangrene Affected muscles appears black Muscle – Centre area is dry and have odour of rancid butter Regional lymph nodes – Swollen and oedematous Large muscles – Diaphragm and tongue Internal organs – Heart, lung, kidneys, liver, spleen and intestine showed acute congestion

Microscopic lesions � Muscle fibres separated and showed waxy degeneration and coagulation necrosis � Streaks of haemorrhages - Collection of neutrophils, lymphocytes and Gram positive organisms demonstrated in tissue sections
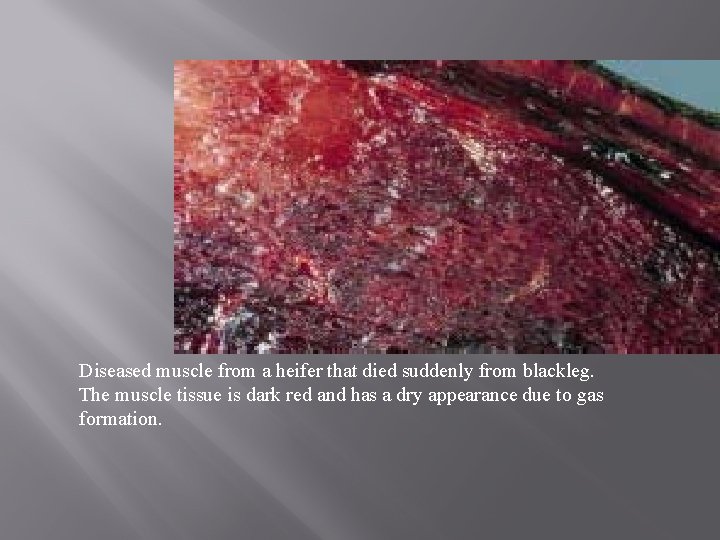
Diseased muscle from a heifer that died suddenly from blackleg. The muscle tissue is dark red and has a dry appearance due to gas formation.

Blackleg - generalised discoloration/gaseous degeneration of carcass in Blackleg case.

Blackleg – accurately located typically ‘dry’ lesion (area to right of label) from PM.
Diagnosis May be confirmed by gross lesions Demonstration of organism – from the fluid incised swelling Biological tests using guinea pigs Fluorescent Antibody Technique (FAT) Fatal course and found dead before signs of illness are seen
- Slides: 55