Clinical Reasoning Lumbosacral Dysfunction Assessment Treatment Alex Wong
Clinical Reasoning Lumbosacral Dysfunction Assessment & Treatment Alex Wong Senior Physiotherapist Queen Elizabeth Hospital 3 January 2009 1
Contents v Classification of Lumbo-sacral v v Dysfunctions Clinical Reasoning Practice Case Illustration Examination /Treatment Skills Take Home Message 2
Vague Diagnosis of LBP v v v 80% no structural diagnosis Limited evidence to support classification Vague complaints to relate pathology Poor understanding biomechanics Complicated treatment outcomes impairment, disability, capability psychosocial………. 3
Classification of Lumbo-sacral Dysfunctions Purpose Direct Specific and Effective Treatments to Homogenous Sub-group Ford et al, 2007 4
Classification of Lumbo-sacral Dysfunctions Treatment Based Specific exercise – extension / flexion / lateral shift syndrome Mobilization – lumbar / sacroiliac mobilization Immobilization – immobilization syndrome Traction – traction / lateral shift syndrome George & Delitto, 2005 5
Classification of Lumbo-sacral Dysfunctions Mc. Kenzie Approach Postural – symptoms after static position Dysfunctional – symptoms at end range Derangement – symptoms through range Me. Kenzie 6
Classification of Lumbo-sacral Dysfunctions Physical Therapy Reviews 2007 632 papers retrieved from data base v 77 papers reviewed full document v 55% uni-dimensional v 6% multi-dimensional v Ford et al, 2007 7
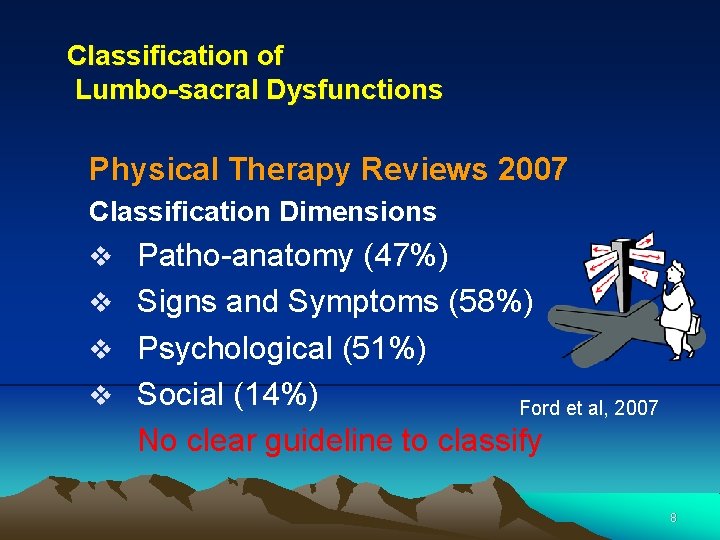
Classification of Lumbo-sacral Dysfunctions Physical Therapy Reviews 2007 Classification Dimensions v Patho-anatomy (47%) v Signs and Symptoms (58%) v Psychological (51%) v Social (14%) Ford et al, 2007 No clear guideline to classify 8
Clinical Reasoning Practice 9
Hypothesis-Oriented Algorithm for Clinicians II (HOAC II) Physical Therapy, Vol 83, No. 5, 2003 A Guide for Patient Management v A framework for science-based clinical practice v Focus on remediation of functional deficits v How changes in impairments related to these deficits Rothstein, 2003 10
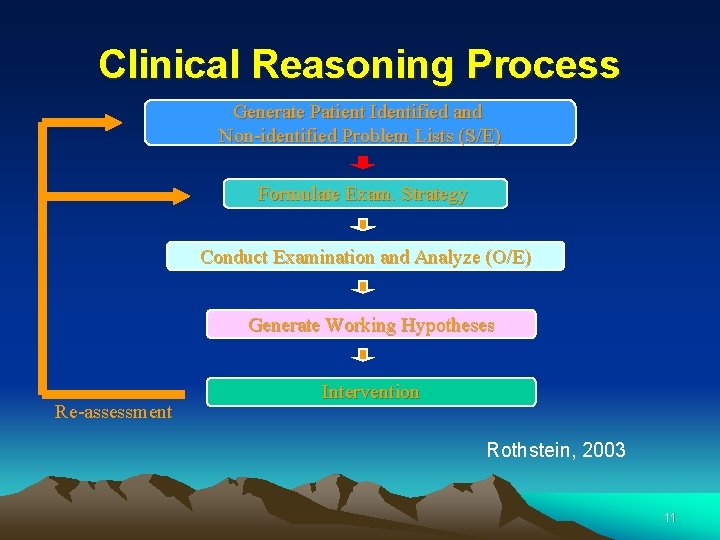
Clinical Reasoning Process Generate Patient Identified and Non-identified Problem Lists (S/E) Formulate Exam. Strategy Conduct Examination and Analyze (O/E) Generate Working Hypotheses Re-assessment Intervention Rothstein, 2003 11
Clinical Reasoning Process Subjective Complaint (generate the clinical hypothesis) Examination, O/E (confirm the clinical hypothesis) Intervention (base on the O/E, findings) 12
Case Illustration 13
Formulate Problem Lists (base on clinical presentations) Case 1 (Housewife, aged 48) C/O • right dull LBP down to right lateral calf • aggravated after prolonged walking • relieved by short duration of sitting • standing much worse • morning pain 14
Generate Clinical Hypothesis (base on clinical presentations) Case 1 (Housewife, aged 48) Clinical Concerns • somatic referred symptoms (L 4, 5) • regular compression pattern • decrease lordosis • worst in static extension • favourable to movement 15
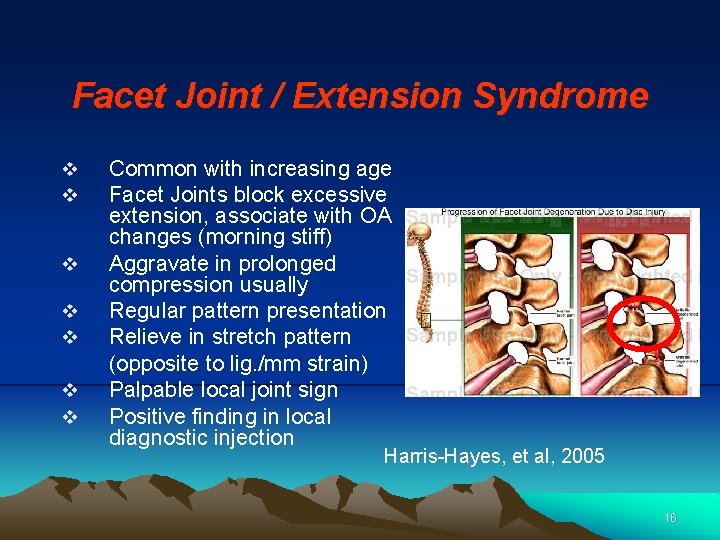
Facet Joint / Extension Syndrome v v v v Common with increasing age Facet Joints block excessive extension, associate with OA changes (morning stiff) Aggravate in prolonged compression usually Regular pattern presentation Relieve in stretch pattern (opposite to lig. /mm strain) Palpable local joint sign Positive finding in local diagnostic injection Harris-Hayes, et al, 2005 16
Conduct Examination, O/E (base on clinical hypothesis) Case 1 O/E • postural defect • movement quality (L 4, 5) • regular movement pattern • quadrant • palpation (extension) 17

Treatment Choice (base on examination findings) Case 1 Treatment • facet joint passive mobilization • mobilize in extended position (L 4, 5) • extension exercises 18
Formulate Problem Lists (base on clinical presentations) Case 2 (Construction site worker, aged 38) C/O • minor sprained 2 days ago • left stabbing LBP down to left lateral ankle gradually afterwards • aggravated after prolonged sitting, walking • relieved by lying only • moderate morning pain – difficult to bend for brushing teeth and wearing shoes • listing pain • can’t tolerate public transport (bus, mini-bus) 19
Generate Clinical Hypothesis (base on clinical presentations) Case 2 (Construction site worker, aged 38) Clinical Concerns • associated with injury • delayed onset of neurogenic symptoms • relieved by decreasing disc pressure • morning symptoms • restricted neurodynamic movement • sensitive to vibration irritation • listing postural defect 20
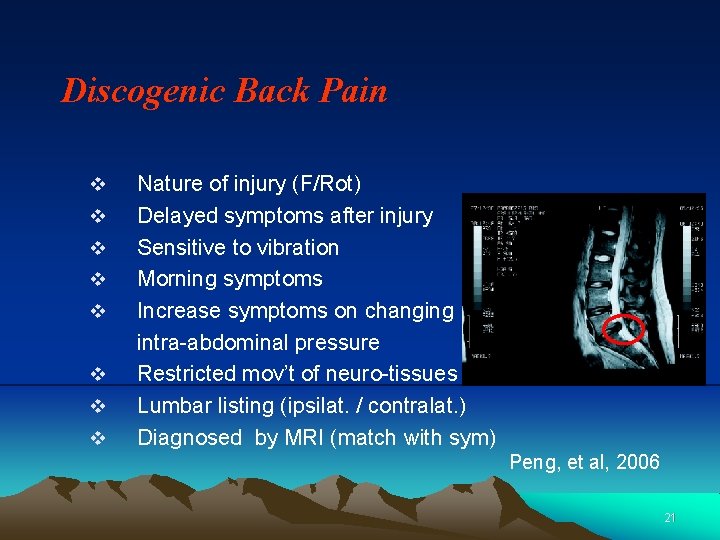
Discogenic Back Pain v v v v Nature of injury (F/Rot) Delayed symptoms after injury Sensitive to vibration Morning symptoms Increase symptoms on changing intra-abdominal pressure Restricted mov’t of neuro-tissues Lumbar listing (ipsilat. / contralat. ) Diagnosed by MRI (match with sym) Peng, et al, 2006 21
Conduct Examination, O/E (base on examination strategy) Case 2 (relieving approach) O/E • postural defect (listing) • movement quality (L 4, 5), extension • neurodynamic movement • neuro assessment • vibration • manual traction • MRI confirmed 22
Treatment Choice (base on examination findings) Case 2 Treatment • listing correction • rotation mobilization • Mckenzie exercises • extension with listing correction 23
Formulate Problem Lists (base on clinical presentations) Case 3 (3 children housewife, aged 33) C/O • minor ankle sprained 7 days ago • dull pain from right buttock down to thigh • aggravated after prolonged sitting, stairs • relieved by walking around • moderate night pain – difficult to roll in bed • can’t tolerate cross leg sitting & pulling activities 24
Generate Clinical Hypothesis (base on clinical presentations) Case 3 (3 children housewife, aged 33) Clinical Concerns • associated with injury / child-birth • symptoms usually not below knee • aggravated if asymmetrical stress to SI Joint & pulling activities • rolling pain in bed at night 25
Sacral Iliac Joint Syndrome v v v v Age / Sex History of Trauma / child-birth Buttock pain / tender over PSIS Symptoms likely not below knee Symptoms when rolling at night Occ cross SLR / Step forward pain Muscle imbalance Priformis, Hamstring, iliopsoas, Gluteus maximus Cluster of tests to confirm Don. Tigny, 1990 De. Mann, 1997 26
Conduct Examination, O/E (base on examination strategy) Case 3 (aggravating approach) O/E • PSIS tender • anterior / posterior stress tests • cross SLR • Long sitting length difference • cluster tests to confirm • hip rotation tests 27
Treatment Choice (base on examination findings) Case 3 Treatment • leg traction • posterior pelvic tilting • hamstring strengthening (muscle energy) 28
Formulate Problem Lists (base on clinical presentations) Case 4 (retired policeman, aged 65) C/O • gradually onset LBP within one year • stretching pain down to left lateral calf • aggravated after prolonged walking • relieved by sitting • moderate mid-range pain when bending forward • difficult to resume hiking and carry back-pack 29
Generate Clinical Hypothesis (base on clinical presentations) Case 4 (retired policeman, aged 65) Clinical Concerns • clinical / functional instability • observable kink of spinal curvature • aggravating with dynamic flexion stress • variable catching pain during mid-range • flexion / extension x-ray to confirm (usually inferior disc problem 67% at L 5 level) Luk, 2003 30
Lumbar Dynamic Stability v Decrease the cross section area of multifidus over the injured / defect segment v Clinically ‘catching pain’ in different range of motion esp. forward flexion v Intrinsic muscles minimize unnecessary rotational stress over the disc Hides, 1994; Lee et Al, 2006 31
Conduct Examination, O/E (base on examination strategy) Case 4 (aggravating approach) O/E • postural defect (hyperlordosis) • movement quality (L 4, 5) • catching pain during movement • shearing test • abdominus weakness & hamstring tightness 32
Treatment Choice (base on examination findings) Case 4 Treatment • supine traction prone traction • abdominal exercises • stabilization exercises 33
Formulate Problem Lists (base on clinical presentations) Case 5 (Student, aged 22) C/O • back sprain injury half year ago • stretching pain down to lateral calf gradually • recent P&Ns over lateral calf • difficult to wear shock in the morning • unfavorable to sit sofa • relieved by walking around 34
Generate Clinical Hypothesis (base on clinical presentations) Case 5 (student, aged 22) Clinical Concerns • associated history • stable neurogenic symptoms • distal symptoms dominated • regular stretching pattern • morning symptoms • not related to loading stress • favorable to movement 35
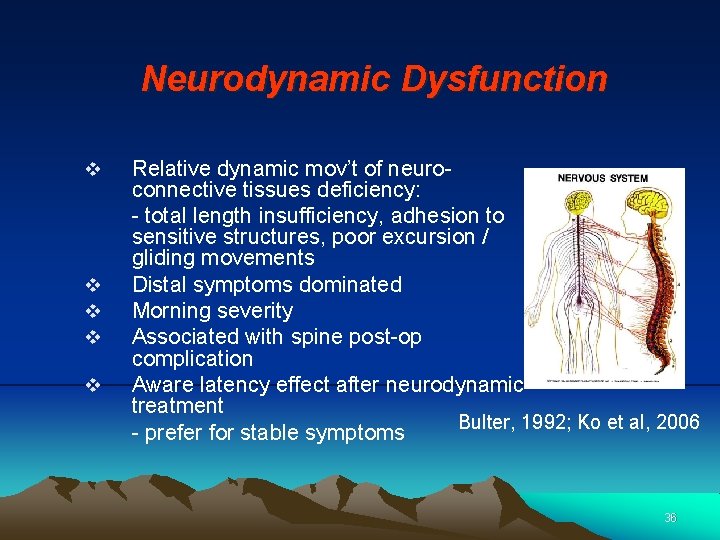
Neurodynamic Dysfunction v v v Relative dynamic mov’t of neuroconnective tissues deficiency: - total length insufficiency, adhesion to sensitive structures, poor excursion / gliding movements Distal symptoms dominated Morning severity Associated with spine post-op complication Aware latency effect after neurodynamic treatment Bulter, 1992; Ko et al, 2006 - prefer for stable symptoms 36
Conduct Examination, O/E (base on examination strategy) Case 5 (aggravating approach) O/E • stable symptoms • relative dynamic mov’t of neuroconnective tissues deficiency: - total length insufficiency, adhesion to sensitive structures, poor excursion / gliding movements • ULTT, Slump 37
Treatment Choice (base on examination findings) Case 5 Treatment • hamstring stretching (cadual / cephelic direction) • slump 38
Formulate Problem Lists (base on clinical presentations) Case 6 (Teacher, aged 56) C/O • no history of injury • stretching & squeezing pain over left calf muscle • symptoms aggravated after walking ~ 15 min. • relieved by sitting or squatting ~ 15 min. • tolerate standing ~ half hr. • much worse when up & down slop 39
Generate Clinical Hypothesis (base on clinical presentations) Case 6 (Teacher, aged 56) Clinical Concerns • dynamic flex / ext problem • relieved by (static) flexion • distal symptoms dominated • not significantly related to loading • not immediately relieved by standing • variable in walking distance • worse in slope walking 40
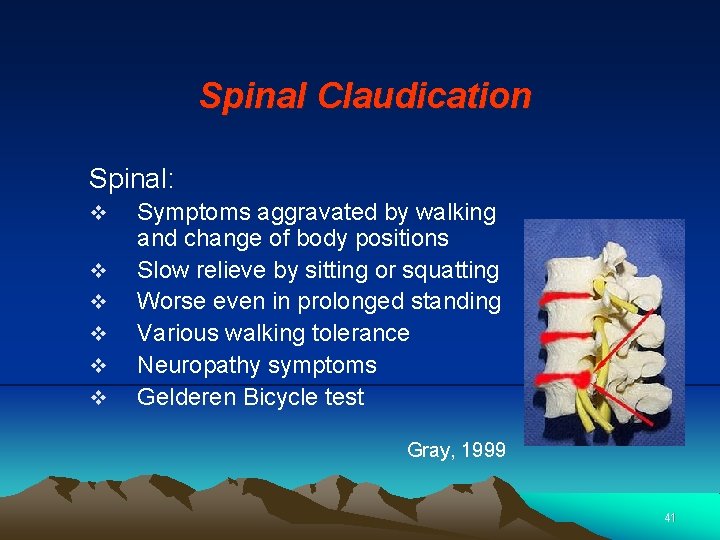
Spinal Claudication Spinal: v v v Symptoms aggravated by walking and change of body positions Slow relieve by sitting or squatting Worse even in prolonged standing Various walking tolerance Neuropathy symptoms Gelderen Bicycle test Gray, 1999 41
Conduct Examination, O/E (base on examination strategy) Case 6 (relieving approach) O/E • distal symptoms dominated • fluctuated symptoms • repeated flex & ext • step standing extension • flex with rotation test • Gelderen Test • x-ray oblique view 42
Treatment Choice (base on examination findings) Case 6 Treatment • crook lying traction • rotation mobilization • rotation with SLR • abdominal strengthening 43
Reference Butler DS (1992) Mobilization of Nervous System. Churchill Livingstones Cibulka MT, Koldehoff R. (1999) Clinical usefulness of a cluster of sacroiliac joint test in patietns with and without low back pain. Journal of orthopaedic and sports Physical Therapy 29(2): 83 -92 De. Mann LE (1997) Sacroiliac Dysfunction in Dancers with Low Back Pain, Manual Therapy 2(1), 2 -10. Don. Tigny RY (1990) Anterior Dysfunction of the Sacroiliac Joint as a Major Factor in the Etiology of the Idiopathic Low Back Pain Syndrome. Physical Therapy 70: 250 -256 Ford J, Story I, O’Sullivan P and Mc. Meeken J (2007) Classification Systems for Low Back Pain: A Review of the Methodology for Development and Validation Physical Therapy Reviews 12: 33 -42. Gay R E, Ilharrebode B, Zhao K, Zhao C and An K N (2006) Sagittal Plane Motion in the Human Lumbar Spine: Comparsion of the in Vitro Quasistatic Neutral Zone and Dynamic Motion Parameters, Clinical Biomechanics 21, p. 914 -919. George SZ, Delitto A (2005) Clinical Examination Variables Discriminate Among Treatment-based Classification Groups: A Study of Construct Validity in Patients with Acute Low Back Pain, Physical Therapy vol 85 (4) 306 -314. Harris-Hayes M, Linda R, Van Dillen, Sahrmann S A (2005) Classification, Treatment and Outcomes of a patient with Lumbar Extension Syndrome Physiotherapy Theory and Practice, 21: 3, 181 -196. 44
Reference Hides JA, Stokes MJ, Saide M, Jull GA, Copper DH (1994) Evidence of Lumbar Multifidus Wasting Isilateral to Symptoms in Patients with Acute/Subacute Low Back Pain. Spine. 19: 165 -172. Ko HY, Park PK, Park JH, Shin YB, Shon HJ and Lee HC (2006) Intrathecal Movement and Tension of the Lumbosacral Roots Induced by Straight Leg Raising. American Physical Medical Rehabilitation. March , 85(3), 222 -227. Kuncewicz E, Gajewska E, Sobiska M and Samborski W (2006) Piriformis Muscle Syndrome, Ann Acad Med Stetin, 52(3) 99 -101. Lee S W, Chan CKM, Lam TS, Lam C, Lau NC, Lau RWL and Chan ST (2006) Relationship Between Low Back Pain and Lumbar Multifidus Size at Different Postures. Spine, vol 31, 19, p. 2258 -2262. Oldreive WL. (1995) A critical review of the literature on tests of the sacroiliac joint. J. Manual Manipulative Therapy 3(4): 156 -161. Peng P, Hao J, Hou S, Wu W, Jiang D, Fu X and Yang Y Possible Pathogenesis of Painful Intervertebral Disc Degeneration Spine vol 31 (5) p. 560 -566 Rothestein J M, Echternack J L and Riddle D (2003) The Hypothesis. Oriented Algorithm for Clinicians II (HOACII): A guide for Patient Management, Physical Therapy Vol 83, Number 5, 455 -470 Sanders RJ, Hammond SL and Rao NM (2007) Journal of Vascular Surgery. Sept. 46(3): 601 -604. Sebastian D (2006) Thoracolumbar Junction Syndrome: A case Report. Physiotherapy Theory and Practice 22: 1 53 -60. Wilk V (2004) Acute low back pain: assessment and management, Aust Fam Physician, June; 33(6): 403 -7. 45
- Slides: 45