Clinical Radiographic and Esthetic Evaluation of Immediately Loaded







- Slides: 42

Clinical, Radiographic, and Esthetic Evaluation of Immediately Loaded Laser Microtextured Implants Placed into Fresh Extraction Sockets in the Anterior Maxilla: A 2 -Year Retrospective Multicentric Study
STATEMENT OF PROBLEM : REDUCTION OF MARGINAL BONE LOSS USING LASER MICROTEXTURING

INTRODUCTION Causes of marginal bone loss : • • • Implant design the density of bone surgical trauma at implant insertion occlusal overload apical migration of the crevicular epithelium due to bacterial-induced infection blood supply interruption
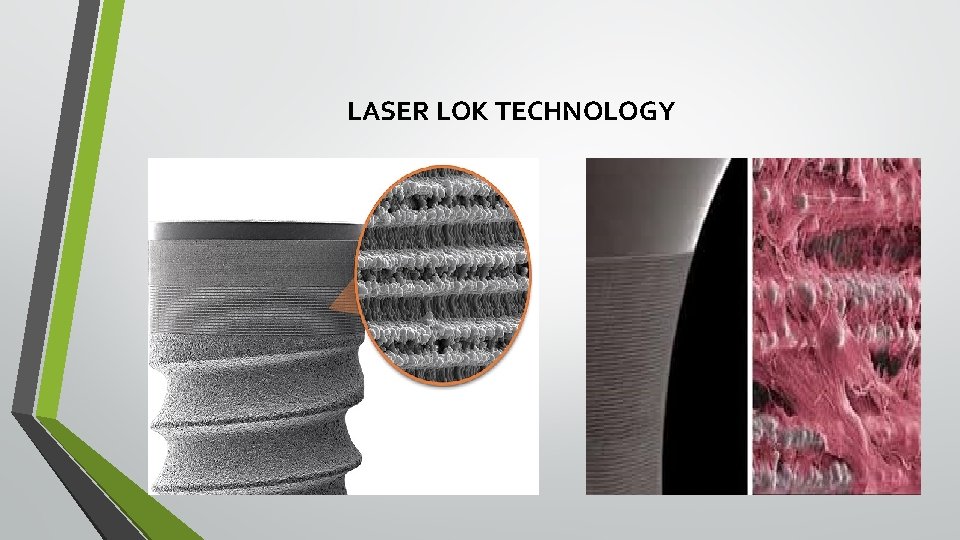
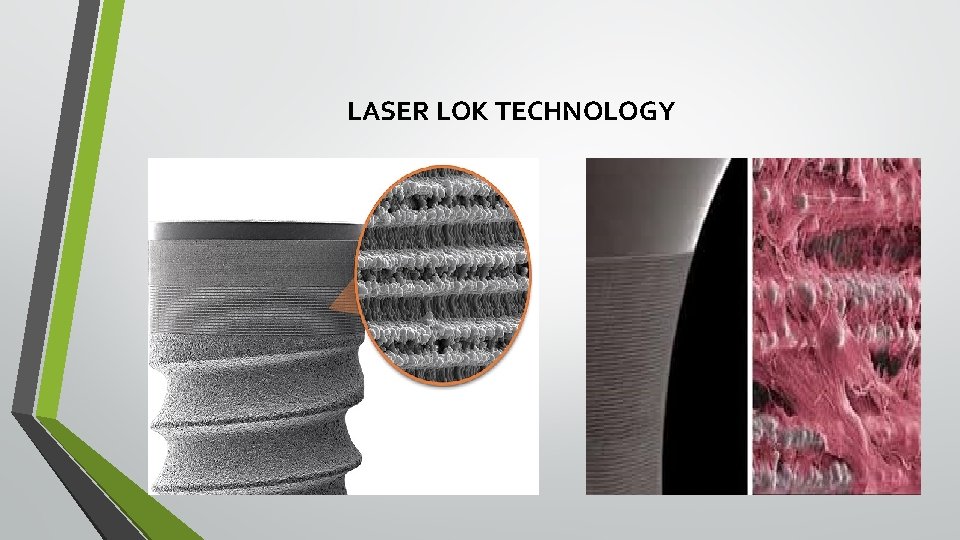
LASER LOK TECHNOLOGY

CLINICAL, RADIOGRAPHIC, AND ESTHETIC EVALUATION OF IMMEDIATELY LOADED LASER MICROTEXTURED IMPLANTS PLACED INTO FRESH EXTRACTION SOCKETS IN THE ANTERIOR MAXILLA: A 2 -YEAR RETROSPECTIVE MULTICENTRIC STUDY • Renzo Guarnieri, Roberto Placella, Luca Testarelli, Vincenzo Iorio-Siciliano and Maurizio Grande • Implant dentistry 2014; 23(2): 144– 154.
REFERENCES CITED • Influence of Laser-Lok Surface on Immediate Functional Loading of Implants in Single-Tooth Replacement: A 2 -Year Prospective Clinical Study - Davide Farronato, Francesco Mangano, Francesco Briguglio, Vincenzo Iorio-Siciliano, Francesco Riccitiello, Renzo Guarnieri. - Int J Periodontics Restorative Dent 2014; 34: 79– 89. • Soft tissue conditions and marginal bone levels of implants with a lasermicrotextured collar: A 5 -year, retrospective, controlled study - V. Iorio-Siciliano, R. Matarasso, R. Guarnieri, M. Nicolo, D. Farronato, S. Matarasso. -Clin. Oral Impl. Res 2015; 26: 257– 262
INTRODUCTION • Numerous clinical studies have proved that good success and high implant survival rate can be obtained with immediate implants and immediate provisionalization procedures • However this therapy is associated with certain esthetic risks like development of gingival recession which in turn is due to the loss of crestal bone • Hence based on the principles of tissue engineering certain new strategies like laser microtexturing of surfaces have been developed to improve hard and soft tissue integration and to prevent crestal bone loss
OBJECTIVES • To assess clinical survival and success rates of Laser-Lok implants placed in the anterior zone of maxilla • To assess the periimplant bone loss, soft tissue dynamics, and esthetic aspects over a period of 2 years
MATERIALS AND METHODS • 46 implants were placed in 46 patients in anterior maxilla immediately after extraction of teeth and immediate non functional loading was carried out. • Of the 46 patients 24 were men and 22 were women. • Age range of patients : 26 – 60(mean of 45. 5)
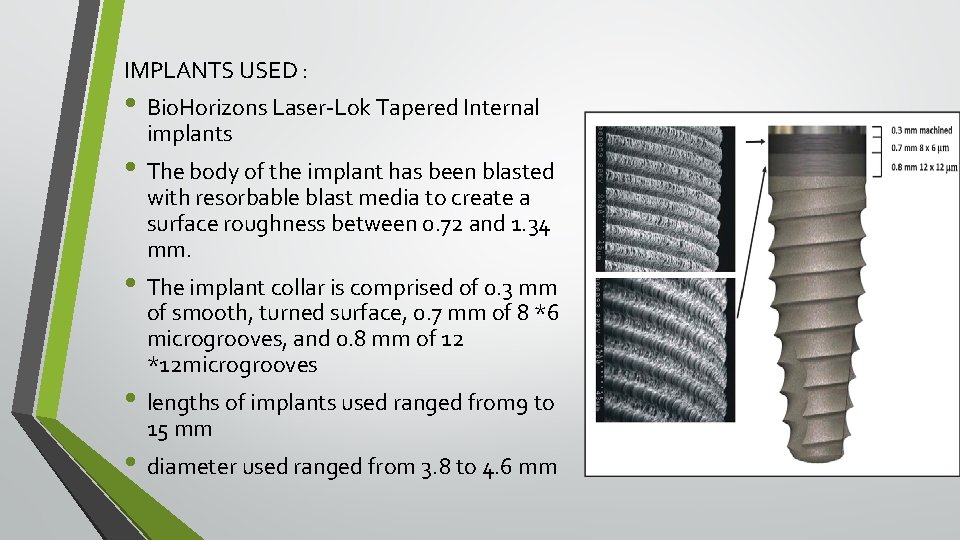
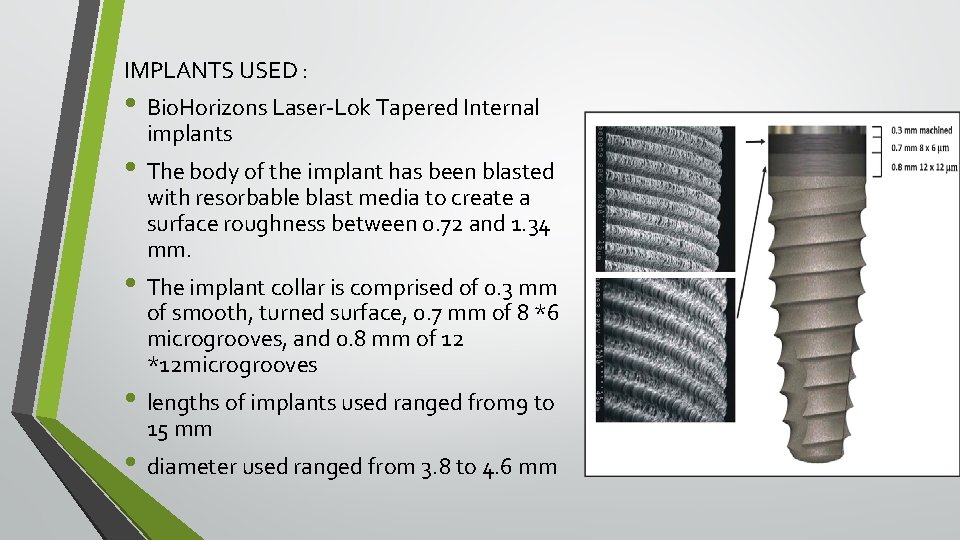
IMPLANTS USED : • Bio. Horizons Laser-Lok Tapered Internal implants • The body of the implant has been blasted with resorbable blast media to create a surface roughness between 0. 72 and 1. 34 mm. • The implant collar is comprised of 0. 3 mm of smooth, turned surface, 0. 7 mm of 8 *6 microgrooves, and 0. 8 mm of 12 *12 microgrooves • lengths of implants used ranged from 9 to 15 mm • diameter used ranged from 3. 8 to 4. 6 mm
INCLUSION CRITERIA • Patients in good general health condition with no chronic systemic disease or smoking habits • Teeth indicated for removal must have at least 4 mm of bone beyond the root apex and at least 10 mm height and 4. 5 mm width of available bone. • Indications : - trauma - root fractures - endodontic failures - non restorable crowns
EXCLUSION CRITERIA • Patients with -bruxism -unstable posterior occlusion - uncontrolled periodontal disease -adjacent teeth that exceeded Class 1 mobility • Teeth with - Unmanageable recession -loss of labial or lingual plate -active periapical or periodontal lesions
PROCEDURE
RADIOGRAPHIC EXAMINATION • Intraoral radiographs were taken after insertion of the implant and at 6, 12 and 24 months using a paralleling technique • crestal bone level: top of the implants to the crestal bone.
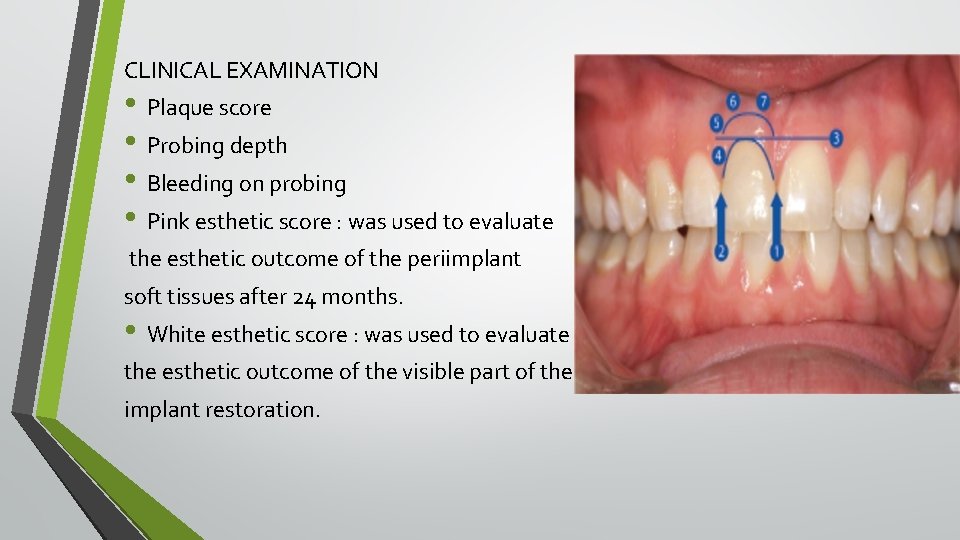
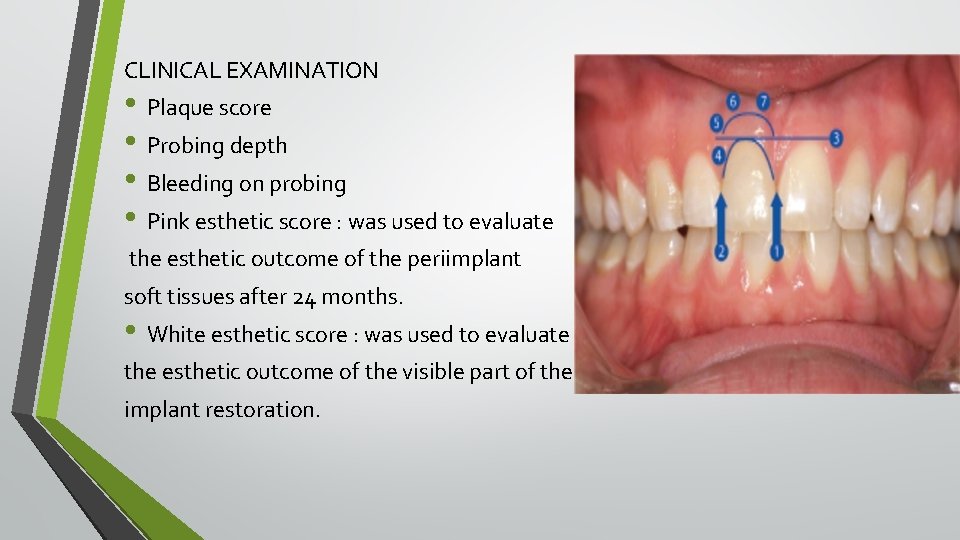
CLINICAL EXAMINATION • Plaque score • Probing depth • Bleeding on probing • Pink esthetic score : was used to evaluate the esthetic outcome of the periimplant soft tissues after 24 months. • White esthetic score : was used to evaluate the esthetic outcome of the visible part of the implant restoration.
Implant Survival Criteria • An implant was considered surviving if it is clinically stable, complies with the function of supporting the prosthesis, and was causing no discomfort to the patient. Failure was defined as removal of an implant for any reason
RESULTS Implant Survival and Complications • Two implants were lost during the 6 -month follow-up observation period (tooth location 22, 13) and not included in the final study group. • implant survival rate after 2 years : 95. 6 % • 1 permanent crown lost retention at 24 months of follow-up and was recemented.

• Hard tissue parameters Soft tissue parameters : • Probing depth : reduced from 2. 42 to 1. 52 • Bleeding on probing : reduced from 36% to 22%
• Esthetic outcome :
Overall esthetic outcome : • Successful results (PES ≥ 12 and WES ≥ 9) : 30/44 (68%) cases • Acceptable results (PES, 8– 11 and WES, 6– 8) : 14/44 (32%) cases • Unfavourable results : 0%

DISCUSSION • invitro studies : - surfaces with 12µm grooves – inhibits fibroblast cell growth relative to osteoblast cell growth - Surfaces with 8µm grooves – inhibits cell migration across grooves Mechanical attachment of connective tissue fibres perpendicular to laser microtextured surface – prevents apical migration of gingival epithelial cells – therby preserves coronal level of bone • the timing of implant placement and loading relative to tooth extraction in the esthetic zone does not seem to result in a different implant survival rate than conventionally installed single implants after a comparable observation period
• Success of single implant therapy – long term quality of survival which is dictated by - esthetics - level of peri implant marginal bone loss - condition of peri implant soft tissues • Effect of immediate implantation and provisionalisation on soft tissues is dependent on - gingival biotype - buccal bone crest - implant type - implant positioning - grafting
CONCLUSION The results showed that immediate implants with laser microtextured surface restored at the day of surgery may be considered as a predictable procedure in terms of implant survival and hard and soft tissue remodeling.
• INFLUENCE OF LASER-LOK SURFACE ON IMMEDIATE FUNCTIONAL LOADING OF IMPLANTS IN SINGLE-TOOTH REPLACEMENT: A 2 -YEAR PROSPECTIVE CLINICAL STUDY -Davide Farronato, Francesco Mangano, Francesco Briguglio, Vincenzo Iorio-Siciliano, Francesco Riccitiello, Renzo Guarnieri. - Int J Periodontics Restorative Dent 2014; 34: 79– 89.
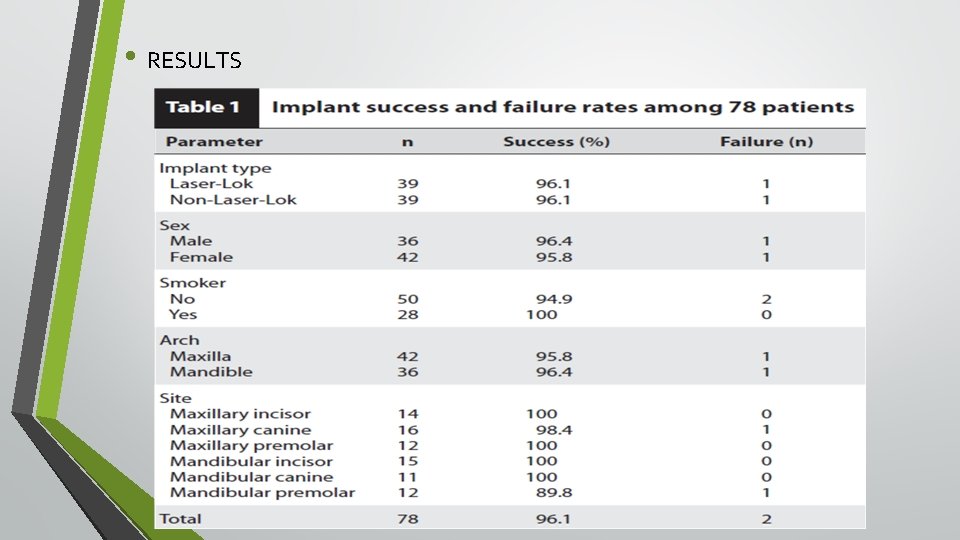
OBJECTIVES • To evaluate the influence of a Laser-Lok microtexturing surface on clinical attachment level and crestal bone remodelling around immediately loaded implants in single-tooth replacement MATERIALS AND METHOD • Number of patients : 78 (36 men and 42 women) • Age range : 45 – 65 (mean of 49. 3) • Site of implant placement : Maxillary and mandibular anterior and premolar region • Control group (group 1) : Bio. Horizons. Tapered Internal non-Laser-Lok type • Test group (group 2): , Bio. Horizons Tapered Internal Laser-Lok type
INCLUSION CRITERIA • Absence of systemic diseases • Single tooth loss with neighbouring teeth in normal occlusion • Recipient site must have healed for ≥ 3 months following tooth extraction • Available bone for atleast 9 -mm-long and 3. 8 -mm-wide implants • An insertion torque of 35 Ncm. EXCLUSION CRITERIA • Poor oral hygiene • patients smoking> 10 cigarettes a day.
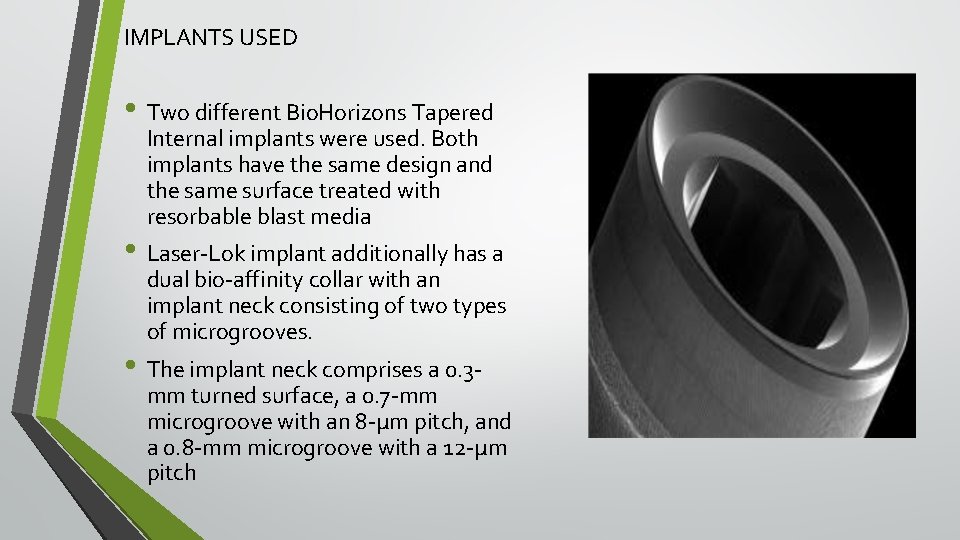
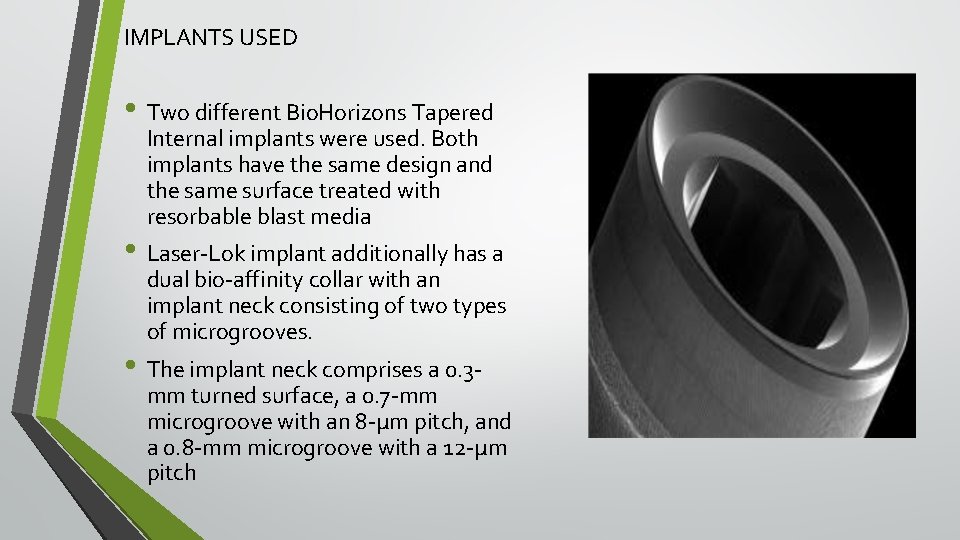
IMPLANTS USED • Two different Bio. Horizons Tapered Internal implants were used. Both implants have the same design and the same surface treated with resorbable blast media • Laser-Lok implant additionally has a dual bio-affinity collar with an implant neck consisting of two types of microgrooves. • The implant neck comprises a 0. 3 - mm turned surface, a 0. 7 -mm microgroove with an 8 -μm pitch, and a 0. 8 -mm microgroove with a 12 -μm pitch
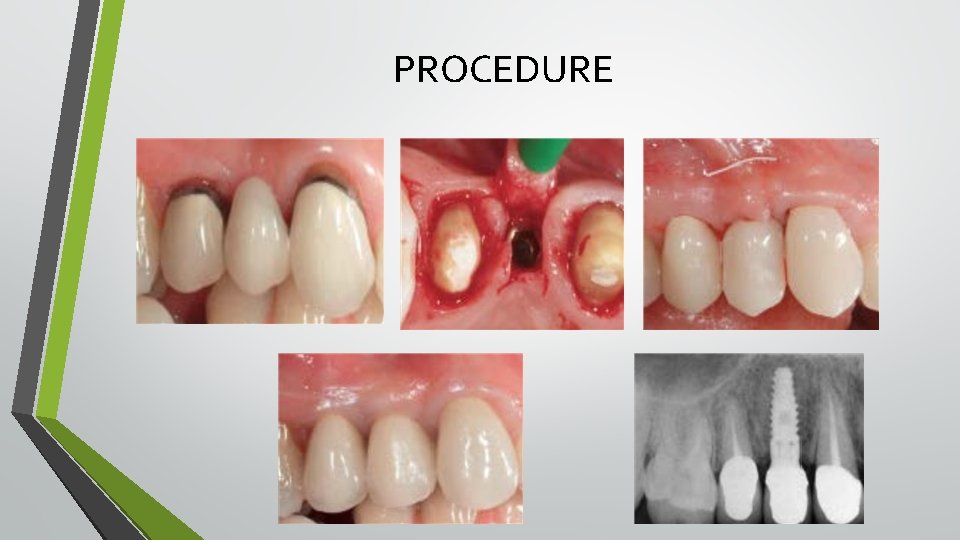
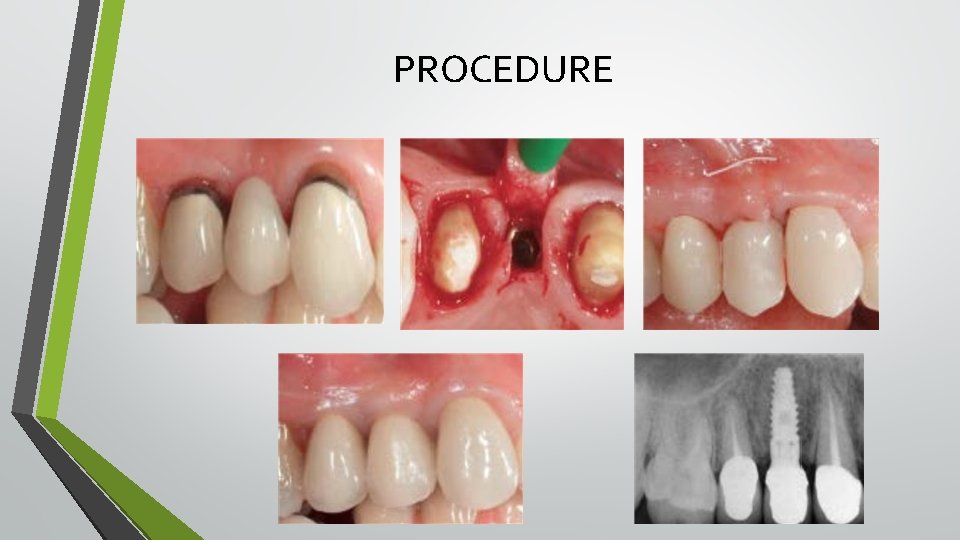
PROCEDURE
• CLINICAL EXAMINATION • Bleeding on probing, plaque index and clinical attachment level were recorded on four surfaces of each implant. • Measurements were recorded at the time of definitive crown placement and at 6, 12, and 24 month examinations. • RADIOGRAPHIC EXAMINATION • Intraoral radiographs were taken after insertion of the implant and at 6, 12 and 24 months
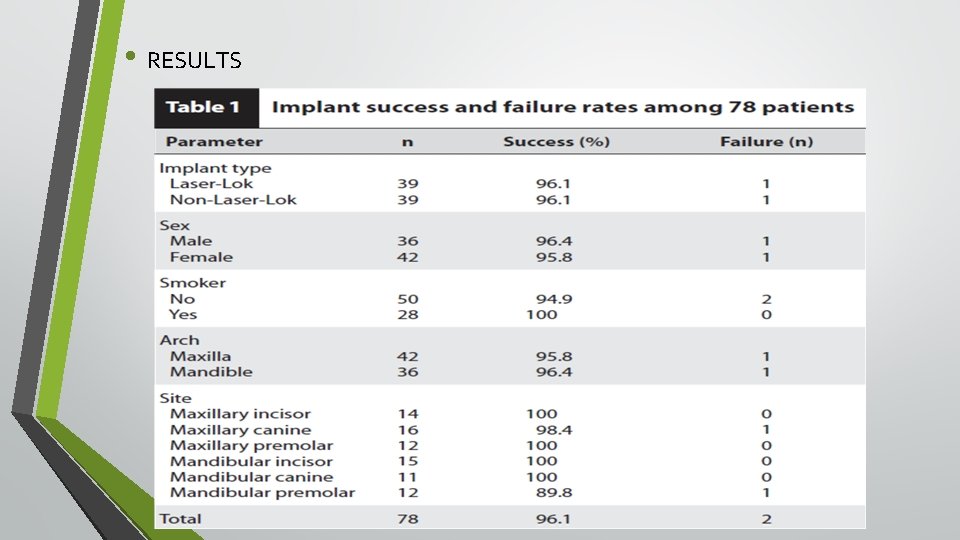
• RESULTS

DISCUSSION • • • 2 factors that have a major influence on immediate loading protocols - Bone density , Implant stability – primary, secondary. Primary stability depends on bone density, the technique and accuracy of the osteotomy preparation, implant design Secondary stability depends on bone formation and remodeling at the implant bone interface and is influenced by the implant surface. To facilitate adequate primary stability, a screw implant design has been shown to have a higher mechanical retention as well as greater ability to transfer compressive forces Surface coating of implant influences secondary stability by accelerating the osseointegration process.
• In this study it was shown that CAL loss and CBL loss was much lesser for test group compared to control group • Hence it can be concluded that in an immediate loading protocol, a Laser- Lok microtextured surface on an implant collar may eliminate the negative sequelae connected with peri-implant bone loss.
• Soft tissue conditions and marginal bone levels of implants with a lasermicrotextured collar: A 5 -year, retrospective, controlled study - V. Iorio-Siciliano, R. Matarasso, R. Guarnieri, M. Nicolo, D. Farronato, S. Matarasso. -Clin. Oral Impl. Res 2015; 26: 257– 262 AIM: • To compare clinical and radiographic outcomes of implants with a Laser-Lok -microtextured collar to implants with a resorbable blast textured (RBT) collar after a 5 -year follow-up period. MATERIALS AND METHODS : • 45 patients of age more than 18 yrs were included in the study and were divided into 2 groups : • Control group : Bio. Horizons Tapered Internal implants with a rbt collar • Test group : Bio. Horizons Tapered Internal Laser-Lok type implants
INCLUSION CRITERIA • Implants placed in healed bone • Loading was performed 3– 6 months after implant placement • Availability of a periodontal chart and periapical radiograph obtained using the parallel long cone technique at the time of crown insertion and at the 5 -year followup period. • The implant supported a single crown or fixed partial dentures EXCLUSION CRITERIA • Tobacco smoking • Periodontally compromised patients • Full-mouth plaque score (FMPS) ≥ 25% • Full-mouth bleeding score (FMBS)≥ 25% • Unloaded implants • Implant-supported overdentures

PROCEDURE • All implants included in the study had been placed following the classic, twostage protocol • The implants of both groups were placed with the collar portion at the level of the bone crest and then covered with the mucosal flap • The second-stage surgery and the installation of the healing cap were performed 3– 6 months thereafter. Definitive crowns were cemented 4– 6 months after second-stage surgery.
EXAMINATIONS • The full-mouth plaque score, full-mouth bleeding score, number of sites with plaque, and the number of sites with bleeding on probing (BOP) were recorded atbaseline, and at 1 -, 2 -, 3 -, 4 -, and 5 -year follow-up. • Probing depth (PD) and mucosal recession were assessed at baseline and after the 5 -year follow-up period. • The radiographic marginal bone loss (MBL) was calculated by subtracting the bone level at the time of crown insertion from the bone level at the 5 year follow-up
RESULTS • An implant survival rate of 94% and of 90% was reported for the TG and the CG, respectively. • No statistical differences were found between the study groups for presence of plaque (10. 1% vs. 25%) or for number of sites with BOP (10. 3% vs. 23%). • The differences between both study groups were statistically significant for mean MBL (0. 81 ± 0. 24 vs. 2. 02 ± 0. 32 mm), mean PD (2. 32 ± 0. 44 vs. 4. 25 ± 0. 87 mm), and mean mucosal recession (0. 16 ± 0. 3 vs. 0. 22 ± 0. 3 mm).
CONCLUSION Laser-microtextured implant collar surface may provide more favorable conditions for the attachment of hard and soft tissues, and reduce the level of MBL.
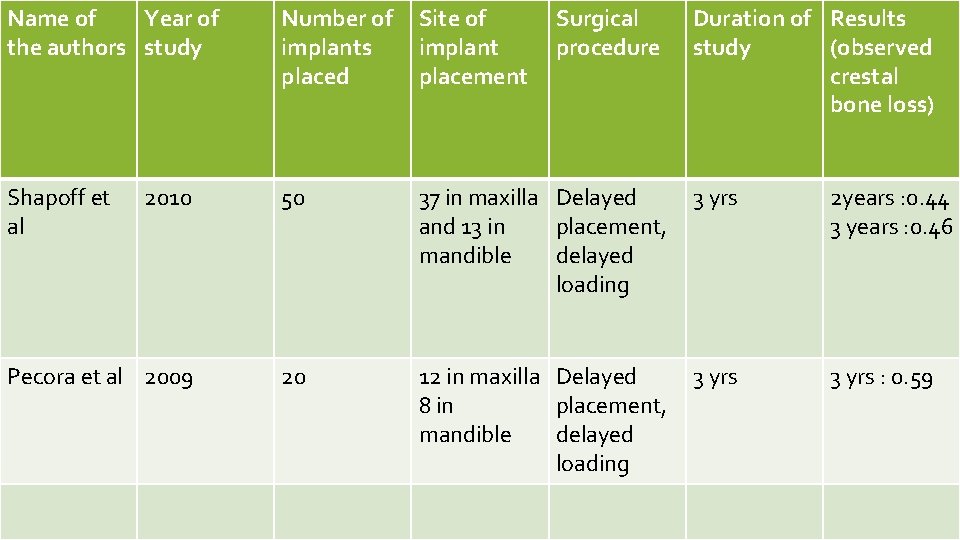
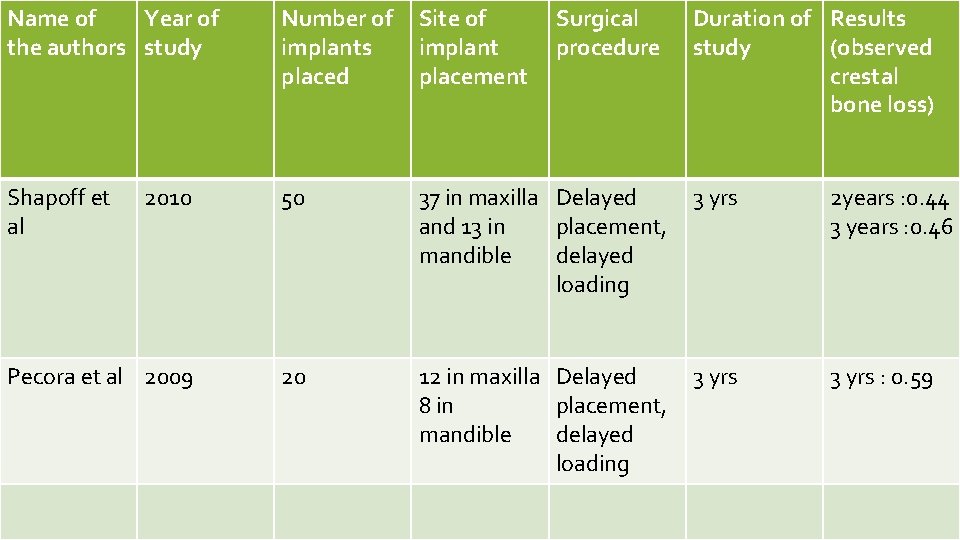
Name of Year of the authors study Number of implants placed Site of implant placement Surgical procedure Duration of Results study (observed crestal bone loss) Shapoff et al 2010 50 37 in maxilla Delayed and 13 in placement, mandible delayed loading 3 yrs 2 years : 0. 44 3 years : 0. 46 Pecora et al 2009 20 12 in maxilla Delayed 8 in placement, mandible delayed loading 3 yrs : 0. 59
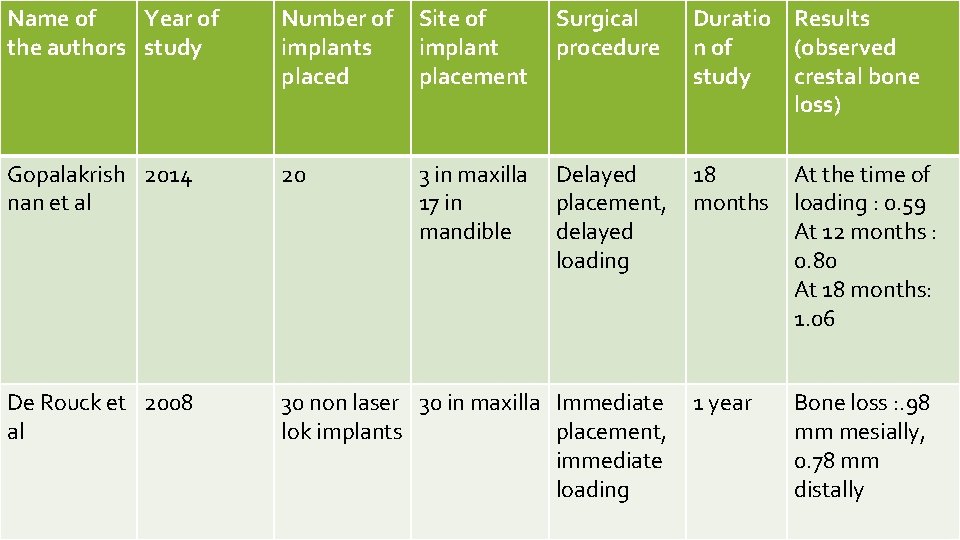
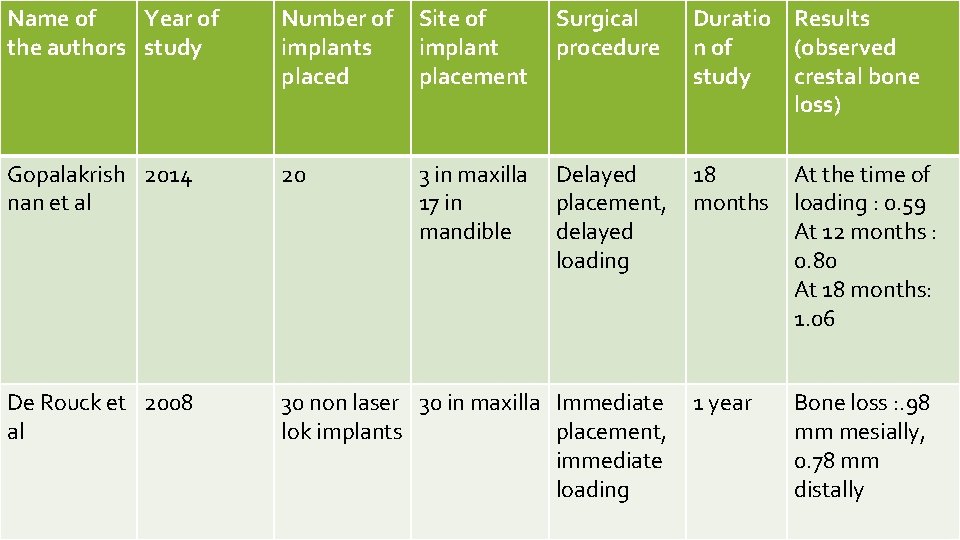
Name of Year of the authors study Number of implants placed Site of implant placement Surgical procedure Duratio Results n of (observed study crestal bone loss) Gopalakrish 2014 nan et al 20 3 in maxilla 17 in mandible Delayed placement, delayed loading 18 months At the time of loading : 0. 59 At 12 months : 0. 80 At 18 months: 1. 06 De Rouck et 2008 al 30 non laser 30 in maxilla Immediate lok implants placement, immediate loading 1 year Bone loss : . 98 mm mesially, 0. 78 mm distally
 What are somesthetic senses
What are somesthetic senses Radiographic baseline skull
Radiographic baseline skull Ventral decubitus position
Ventral decubitus position Grid ratio conversion factors
Grid ratio conversion factors Xray dark room layout
Xray dark room layout Dental radiographic interpretation ppt
Dental radiographic interpretation ppt Occipitomental view
Occipitomental view Warped cassette
Warped cassette Trabecular pattern of maxilla and mandible
Trabecular pattern of maxilla and mandible Radiographic film
Radiographic film Kink marks artifact
Kink marks artifact Reverse townes view positioning
Reverse townes view positioning Radiographic films
Radiographic films Geometric unsharpness of margins in radiographic image
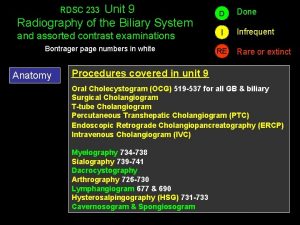
Geometric unsharpness of margins in radiographic image Ercp images
Ercp images Clinical evaluation of language fundamentals
Clinical evaluation of language fundamentals Narration rules
Narration rules If a laboratory fire erupts immediately
If a laboratory fire erupts immediately If a laboratory fire erupts, immediately
If a laboratory fire erupts, immediately Reflective studs between motorway and slip road
Reflective studs between motorway and slip road Msha immediately reportable
Msha immediately reportable The gorgeous model slinked down the runway
The gorgeous model slinked down the runway A boat full of scrap iron floats
A boat full of scrap iron floats Progress and performance measurement and evaluation
Progress and performance measurement and evaluation Pregnancy and infant cohort monitoring and evaluation
Pregnancy and infant cohort monitoring and evaluation Evaluation in progress
Evaluation in progress Understanding and managing clinical risk
Understanding and managing clinical risk Clinical observation of motor and postural skills pdf
Clinical observation of motor and postural skills pdf What is administrative information systems in healthcare
What is administrative information systems in healthcare Clinical systems transformation
Clinical systems transformation Nature of clinical psychology
Nature of clinical psychology Scope of clinical pharmacist
Scope of clinical pharmacist Phs human subjects and clinical trials information
Phs human subjects and clinical trials information Brunnstrom's clinical kinesiology 7th edition
Brunnstrom's clinical kinesiology 7th edition Difference between inspection and audit
Difference between inspection and audit Clinical kinesiology and anatomy 6th edition
Clinical kinesiology and anatomy 6th edition 1. the gorgeous model slinked down the runway.
1. the gorgeous model slinked down the runway. Beam loaded as shown in fig. p-428
Beam loaded as shown in fig. p-428 “pro-death” is a loaded phrase.
“pro-death” is a loaded phrase. A child is on a playground swing motionless
A child is on a playground swing motionless Advertisement using propaganda techniques
Advertisement using propaganda techniques Loaded words propaganda definition
Loaded words propaganda definition Loaded words advertising
Loaded words advertising