Clinical Presentation of Type 2 Diabetes 1 Risk
Clinical Presentation of Type 2 Diabetes 1
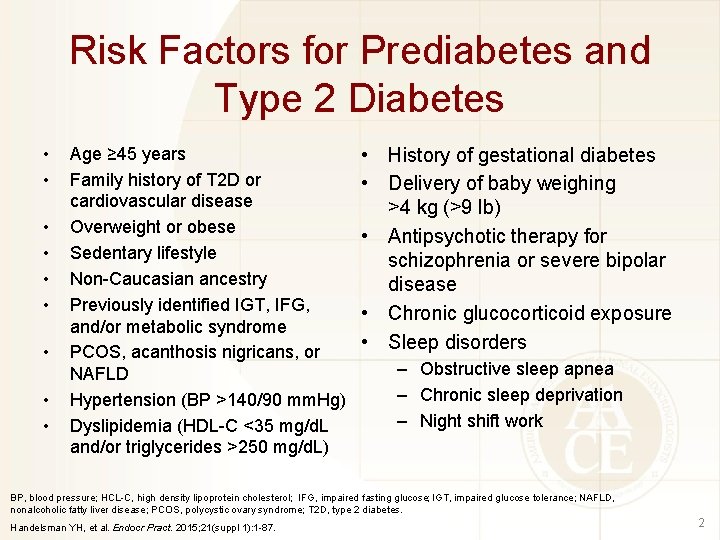
Risk Factors for Prediabetes and Type 2 Diabetes • • • Age ≥ 45 years Family history of T 2 D or cardiovascular disease Overweight or obese Sedentary lifestyle Non-Caucasian ancestry Previously identified IGT, IFG, and/or metabolic syndrome PCOS, acanthosis nigricans, or NAFLD Hypertension (BP >140/90 mm. Hg) Dyslipidemia (HDL-C <35 mg/d. L and/or triglycerides >250 mg/d. L) • History of gestational diabetes • Delivery of baby weighing >4 kg (>9 lb) • Antipsychotic therapy for schizophrenia or severe bipolar disease • Chronic glucocorticoid exposure • Sleep disorders – Obstructive sleep apnea – Chronic sleep deprivation – Night shift work BP, blood pressure; HCL-C, high density lipoprotein cholesterol; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; NAFLD, nonalcoholic fatty liver disease; PCOS, polycystic ovary syndrome; T 2 D, type 2 diabetes. Handelsman YH, et al. Endocr Pract. 2015; 21(suppl 1): 1 -87. 2
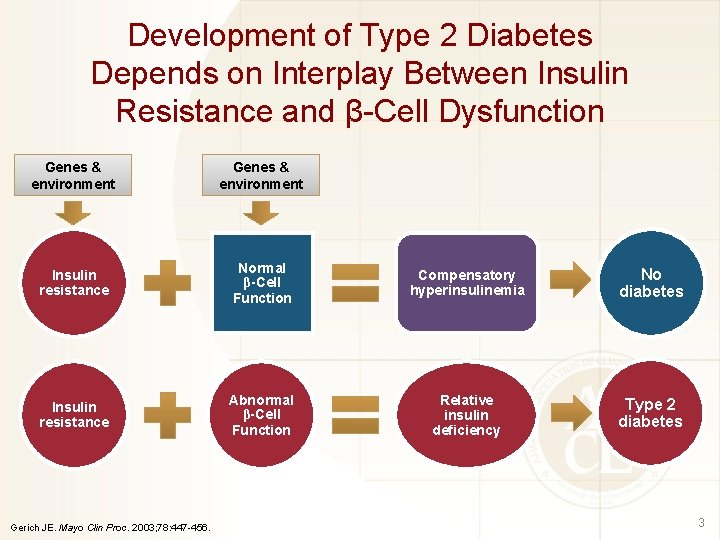
Development of Type 2 Diabetes Depends on Interplay Between Insulin Resistance and β-Cell Dysfunction Genes & environment Insulin resistance Normal β-Cell Function Compensatory hyperinsulinemia No diabetes Insulin resistance Abnormal β-Cell Function Relative insulin deficiency Type 2 diabetes Gerich JE. Mayo Clin Proc. 2003; 78: 447 -456. 3
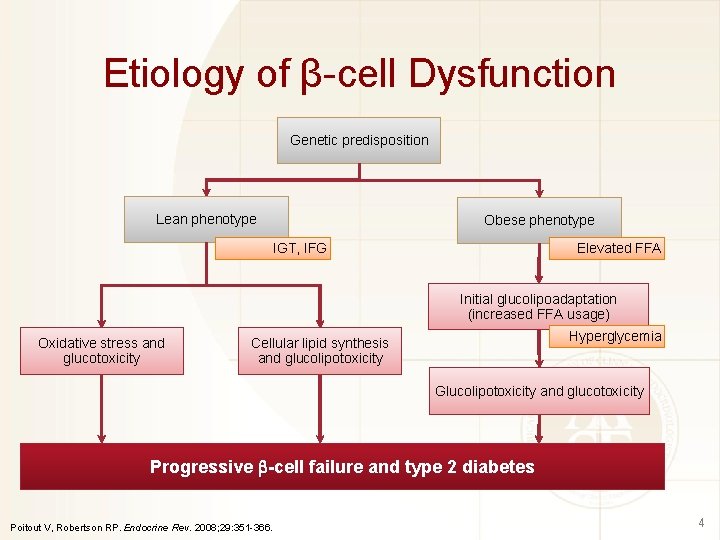
Etiology of β-cell Dysfunction Genetic predisposition Lean phenotype Obese phenotype Elevated FFA IGT, IFG Initial glucolipoadaptation (increased FFA usage) Oxidative stress and glucotoxicity Hyperglycemia Cellular lipid synthesis and glucolipotoxicity Glucolipotoxicity and glucotoxicity Progressive -cell failure and type 2 diabetes Poitout V, Robertson RP. Endocrine Rev. 2008; 29: 351 -366. 4
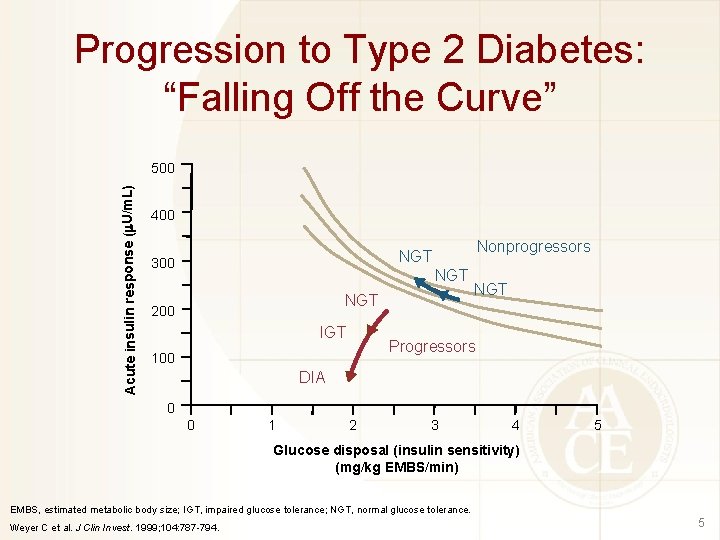
Progression to Type 2 Diabetes: “Falling Off the Curve” Acute insulin response ( U/m. L) 500 400 Nonprogressors NGT 300 NGT 200 IGT NGT Progressors 100 DIA 0 0 1 2 3 4 5 Glucose disposal (insulin sensitivity) (mg/kg EMBS/min) EMBS, estimated metabolic body size; IGT, impaired glucose tolerance; NGT, normal glucose tolerance. Weyer C et al. J Clin Invest. 1999; 104: 787 -794. 5
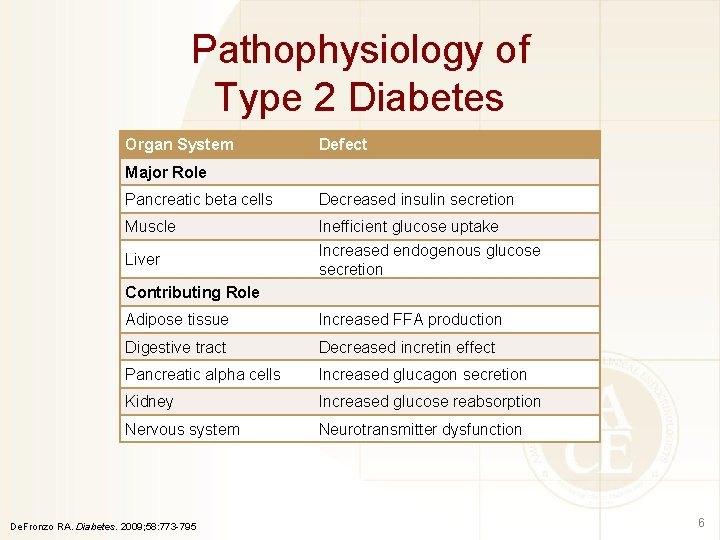
Pathophysiology of Type 2 Diabetes Organ System Defect Major Role Pancreatic beta cells Decreased insulin secretion Muscle Inefficient glucose uptake Increased endogenous glucose secretion Liver Contributing Role Adipose tissue Increased FFA production Digestive tract Decreased incretin effect Pancreatic alpha cells Increased glucagon secretion Kidney Increased glucose reabsorption Nervous system Neurotransmitter dysfunction De. Fronzo RA. Diabetes. 2009; 58: 773 -795 6

Tissues Involved in T 2 D Pathophysiology Organ System Normal Metabolic Function Defect in T 2 D Pancreatic beta cells Secrete insulin Decreased insulin secretion Muscle Metabolizes glucose for energy Inefficient glucose uptake Liver Secretes glucose during fasting periods to maintain brain function; main site of gluconeogenesis (glucose production in the body) Increased endogenous glucose secretion Adipose tissue (fat) Stores small amounts of glucose for its own use. When fat is broken down, glycerol is released, which is used by the liver to produce glucose Increased FFA production Digestive tract Digests and absorbs carbohydrates and secretes incretin hormones Decreased incretin effect Pancreatic alpha cells Secrete glucagon, which stimulates hepatic glucose production between meals and also helps suppress insulin secretion during fasting periods Increased glucagon secretion Kidney Reabsorbs glucose from renal filtrate to maintain glucose at steady-state levels; also an important site for gluconeogenesis (glucose production) Increased glucose reabsorption Brain Utilizes glucose for brain and nerve function Regulates appetite Neurotransmitter dysfunction Major Role Contributing Role T 2 D, type 2 diabetes. De. Fronzo RA. Diabetes. 2009; 58: 773 -795 7
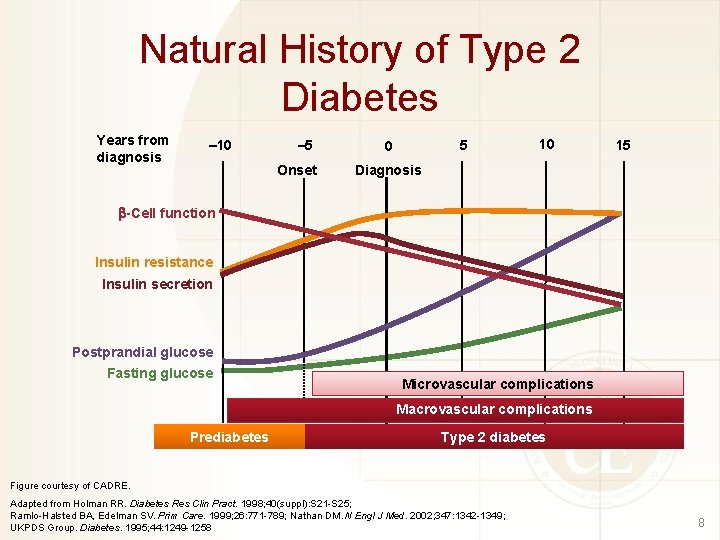
Natural History of Type 2 Diabetes Years from diagnosis – 10 – 5 Onset 5 0 10 15 Diagnosis -Cell function Insulin resistance Insulin secretion Postprandial glucose Fasting glucose Microvascular complications Macrovascular complications Prediabetes Type 2 diabetes Figure courtesy of CADRE. Adapted from Holman RR. Diabetes Res Clin Pract. 1998; 40(suppl): S 21 -S 25; Ramlo-Halsted BA, Edelman SV. Prim Care. 1999; 26: 771 -789; Nathan DM. N Engl J Med. 2002; 347: 1342 -1349; UKPDS Group. Diabetes. 1995; 44: 1249 -1258 8
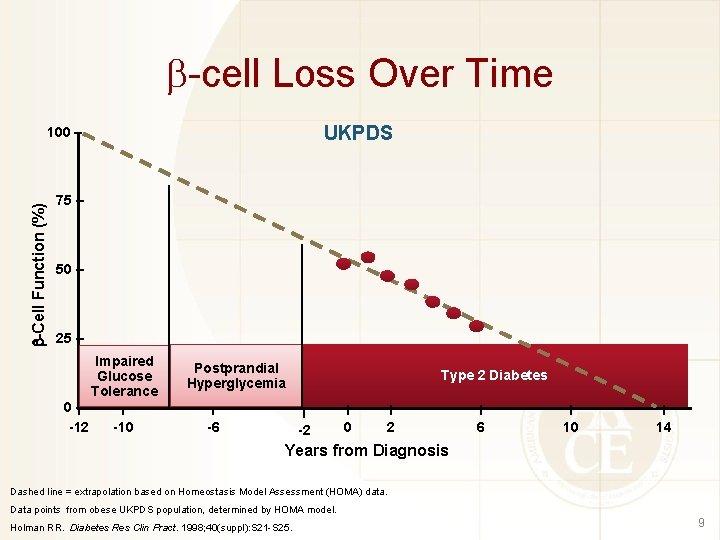
-cell Loss Over Time UKPDS -Cell Function (%) 100 – 75 – 50 – 25 – Impaired Glucose Tolerance 0 –l l -12 -10 Postprandial Hyperglycemia l -6 Type 2 Diabetes l -2 l 0 l 2 l 6 l 10 l 14 Years from Diagnosis Dashed line = extrapolation based on Homeostasis Model Assessment (HOMA) data. Data points from obese UKPDS population, determined by HOMA model. Holman RR. Diabetes Res Clin Pract. 1998; 40(suppl): S 21 -S 25. 9
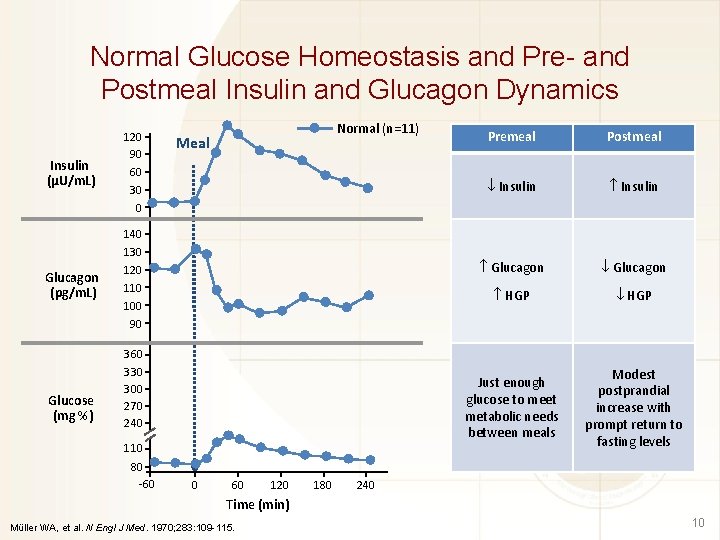
Normal Glucose Homeostasis and Pre- and Postmeal Insulin and Glucagon Dynamics Insulin (µU/m. L) 120 90 60 30 0 Glucagon (pg/m. L) 140 130 120 110 100 90 Glucose (mg %) Normal (n=11) Meal 360 330 300 270 240 110 80 -60 0 60 120 180 Premeal Postmeal Insulin Glucagon HGP Just enough glucose to meet metabolic needs between meals Modest postprandial increase with prompt return to fasting levels 240 Time (min) Müller WA, et al. N Engl J Med. 1970; 283: 109 -115. 10
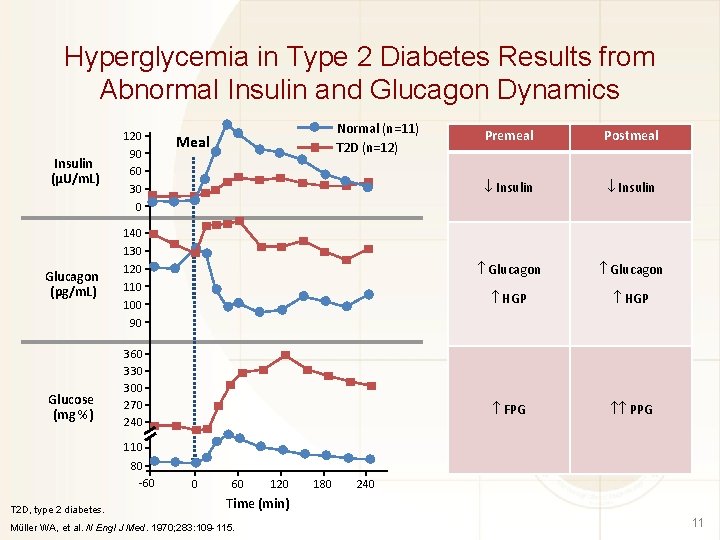
Hyperglycemia in Type 2 Diabetes Results from Abnormal Insulin and Glucagon Dynamics Insulin (µU/m. L) 120 90 60 30 0 Glucagon (pg/m. L) 140 130 120 110 100 90 Glucose (mg %) Normal (n=11) T 2 D (n=12) Meal 360 330 300 270 240 Premeal Postmeal Insulin Glucagon HGP FPG PPG 110 80 -60 T 2 D, type 2 diabetes. 0 60 120 180 240 Time (min) Müller WA, et al. N Engl J Med. 1970; 283: 109 -115. 11
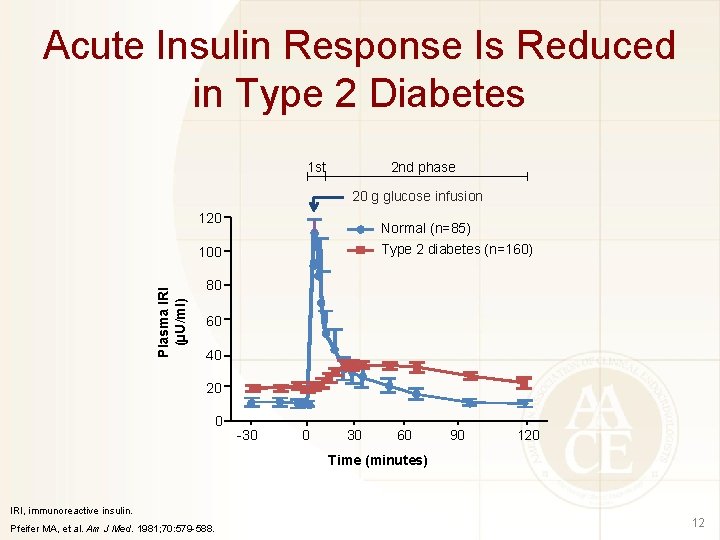
Acute Insulin Response Is Reduced in Type 2 Diabetes 1 st 2 nd phase 20 g glucose infusion 120 Normal (n=85) Type 2 diabetes (n=160) Plasma IRI (µU/ml) 100 80 60 40 20 0 -30 0 30 60 90 120 Time (minutes) IRI, immunoreactive insulin. Pfeifer MA, et al. Am J Med. 1981; 70: 579 -588. 12
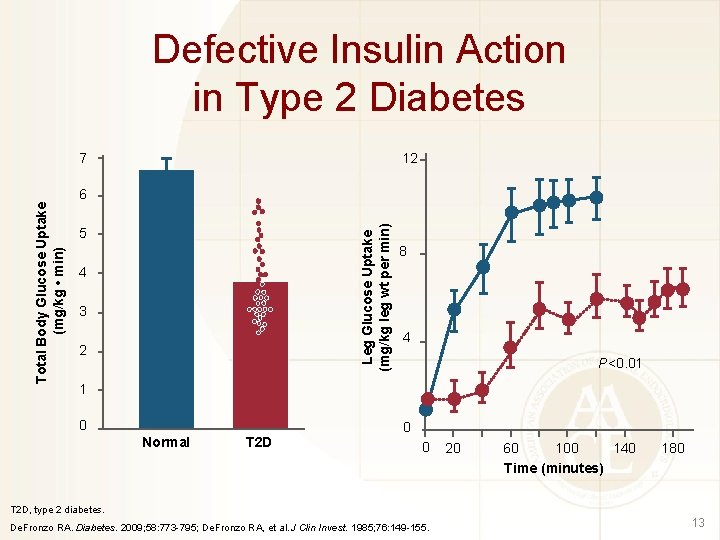
Defective Insulin Action in Type 2 Diabetes 7 12 Leg Glucose Uptake (mg/kg leg wt per min) Total Body Glucose Uptake (mg/kg • min) 6 5 4 3 2 8 4 P<0. 01 1 0 Normal T 2 D 0 0 20 60 100 140 Time (minutes) 180 T 2 D, type 2 diabetes. De. Fronzo RA. Diabetes. 2009; 58: 773 -795; De. Fronzo RA, et al. J Clin Invest. 1985; 76: 149 -155. 13
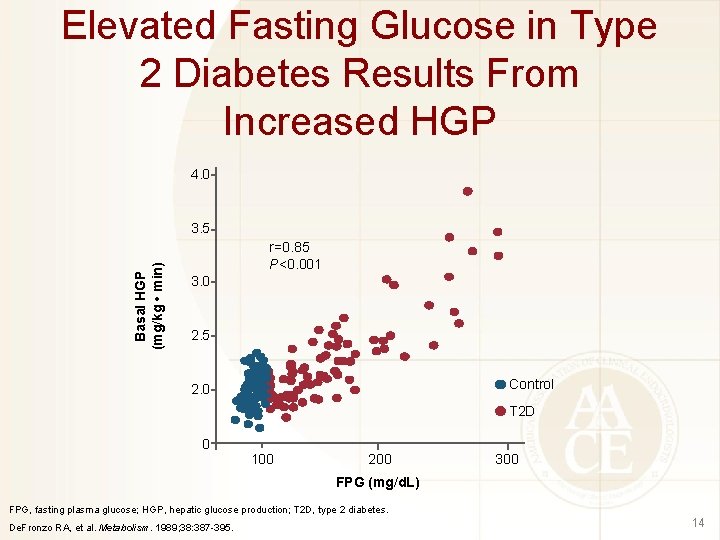
Elevated Fasting Glucose in Type 2 Diabetes Results From Increased HGP 4. 0 Basal HGP (mg/kg • min) 3. 5 r=0. 85 P<0. 001 3. 0 2. 5 Control 2. 0 T 2 D 0 100 200 300 FPG (mg/d. L) FPG, fasting plasma glucose; HGP, hepatic glucose production; T 2 D, type 2 diabetes. De. Fronzo RA, et al. Metabolism. 1989; 38: 387 -395. 14
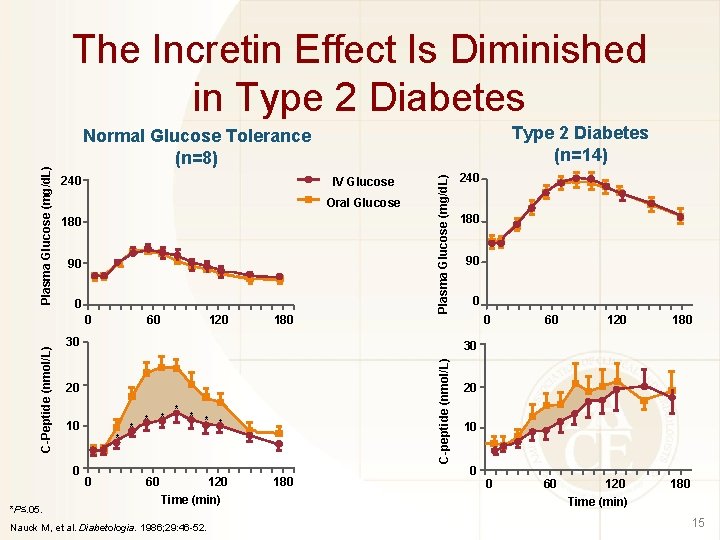
IV Glucose Oral Glucose 180 90 0 C-Peptide (nmol/L) 120 60 180 Plasma Glucose (mg/d. L) 240 0 30 240 180 90 0 0 60 120 180 30 20 10 0 *P≤. 05. Type 2 Diabetes (n=14) Normal Glucose Tolerance (n=8) C-peptide (nmol/L) Plasma Glucose (mg/d. L) The Incretin Effect Is Diminished in Type 2 Diabetes * 0 * * * * 60 120 Time (min) Nauck M, et al. Diabetologia. 1986; 29: 46 -52. 180 20 10 0 Time (min) 15

Actions of GLP-1 and GIP GLP-1 GIP • Released from L cells in ileum and colon • Stimulates insulin release from -cell in a glucose-dependent manner • Potent inhibition of gastric emptying • Potent inhibition of glucagon secretion • Reduction of food intake and body weight • Significant effects on -cell growth and survival • Released from K cells in duodenum • Stimulates insulin release from -cell in a glucose dependent manner • Minimal effects on gastric emptying • No significant inhibition of glucagon secretion • No significant effects on satiety or body weight • Potential effects on -cell growth and survival Drucker DJ. Diabetes Care 2003; 26: 2929 -2940. 16
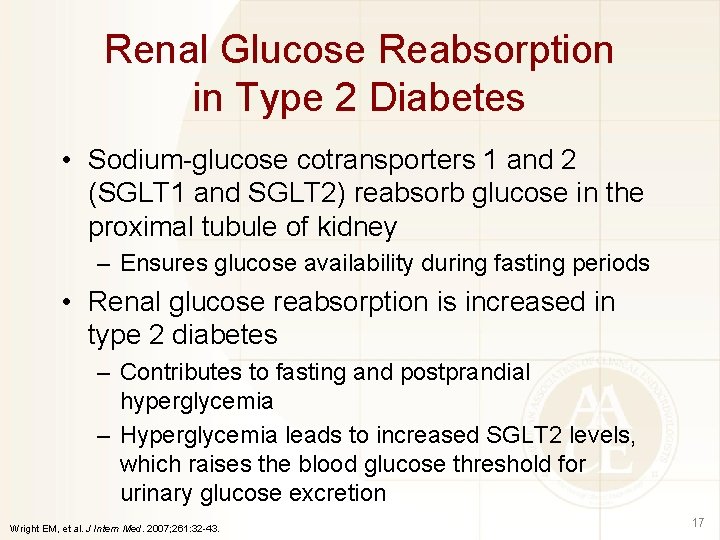
Renal Glucose Reabsorption in Type 2 Diabetes • Sodium-glucose cotransporters 1 and 2 (SGLT 1 and SGLT 2) reabsorb glucose in the proximal tubule of kidney – Ensures glucose availability during fasting periods • Renal glucose reabsorption is increased in type 2 diabetes – Contributes to fasting and postprandial hyperglycemia – Hyperglycemia leads to increased SGLT 2 levels, which raises the blood glucose threshold for urinary glucose excretion Wright EM, et al. J Intern Med. 2007; 261: 32 -43. 17
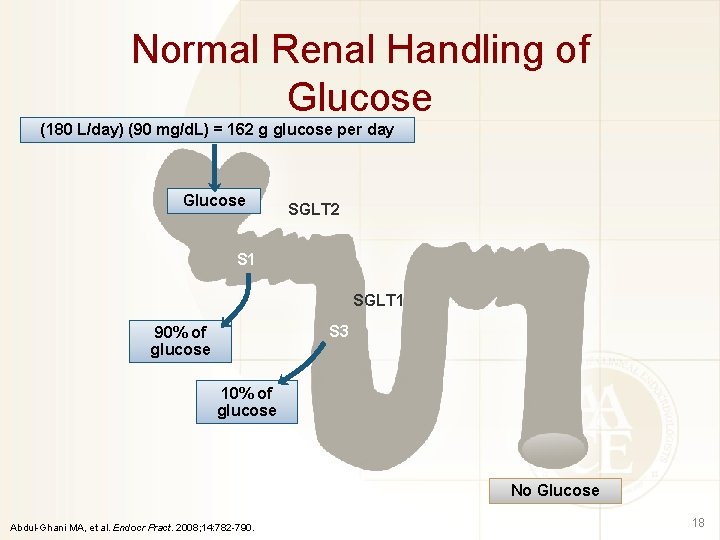
Normal Renal Handling of Glucose (180 L/day) (90 mg/d. L) = 162 g glucose per day Glucose SGLT 2 S 1 SGLT 1 S 3 90% of glucose 10% of glucose No Glucose Abdul-Ghani MA, et al. Endocr Pract. 2008; 14: 782 -790. 18
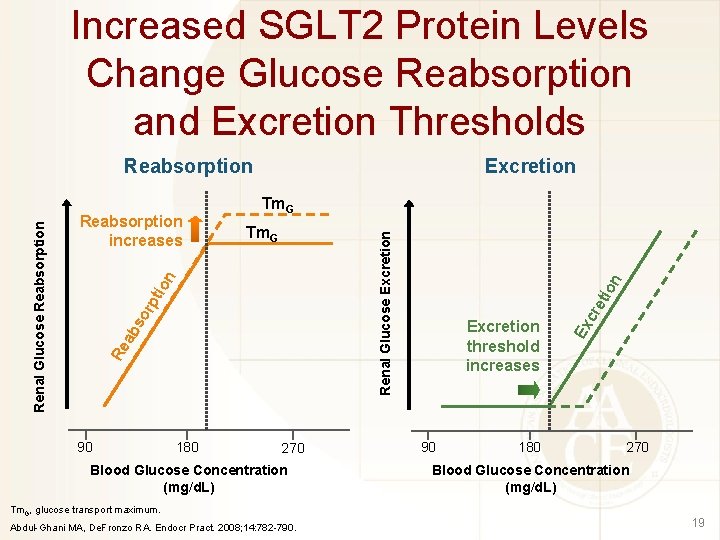
Increased SGLT 2 Protein Levels Change Glucose Reabsorption and Excretion Thresholds Tm. G 180 270 Blood Glucose Concentration (mg/d. L) Tm. G, glucose transport maximum. Abdul-Ghani MA, De. Fronzo RA. Endocr Pract. 2008; 14: 782 -790. eti 90 180 cr Excretion threshold increases Ex pt or ab s 90 on Renal Glucose Excretion Tm. G ion Reabsorption increases Excretion Re Renal Glucose Reabsorption 270 Blood Glucose Concentration (mg/d. L) 19
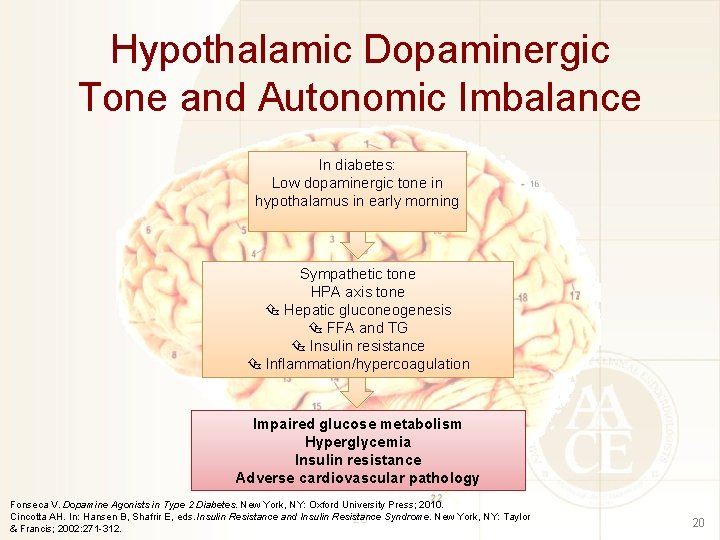
Hypothalamic Dopaminergic Tone and Autonomic Imbalance In diabetes: Low dopaminergic tone in hypothalamus in early morning Sympathetic tone HPA axis tone Hepatic gluconeogenesis FFA and TG Insulin resistance Inflammation/hypercoagulation Impaired glucose metabolism Hyperglycemia Insulin resistance Adverse cardiovascular pathology Fonseca V. Dopamine Agonists in Type 2 Diabetes. New York, NY: Oxford University Press; 2010. Cincotta AH. In: Hansen B, Shafrir E, eds. Insulin Resistance and Insulin Resistance 20 Syndrome. New York, NY: Taylor & Francis; 2002: 271 -312. 20
- Slides: 20