Clinical Pharmacology of Antianginal Drugs ISCHEMIC HEART DISEASE












- Slides: 32
Clinical Pharmacology of Antianginal Drugs
ISCHEMIC HEART DISEASE There are 35 risk factors for development of IHD – The most important risk factors for coronary artery disease • Smoking • Hypertension • Hyperlipidaemia • Diabetes mellitus 95 % of patients with IHD are observed to have aterosclerotic changes in coronary arteries
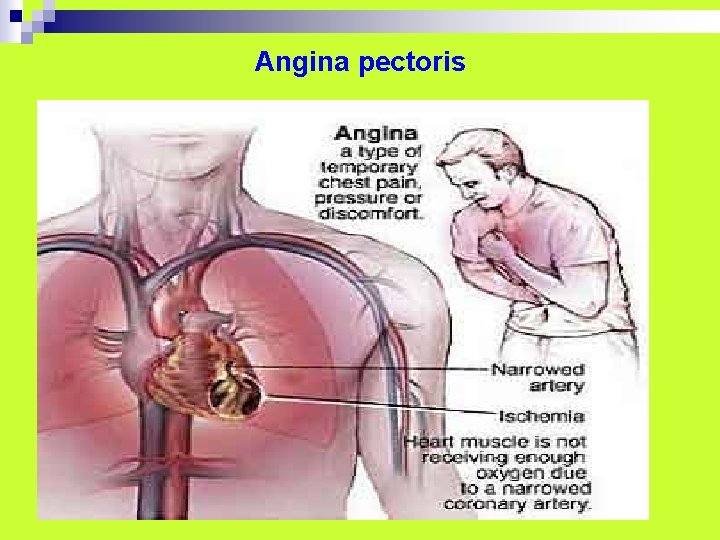
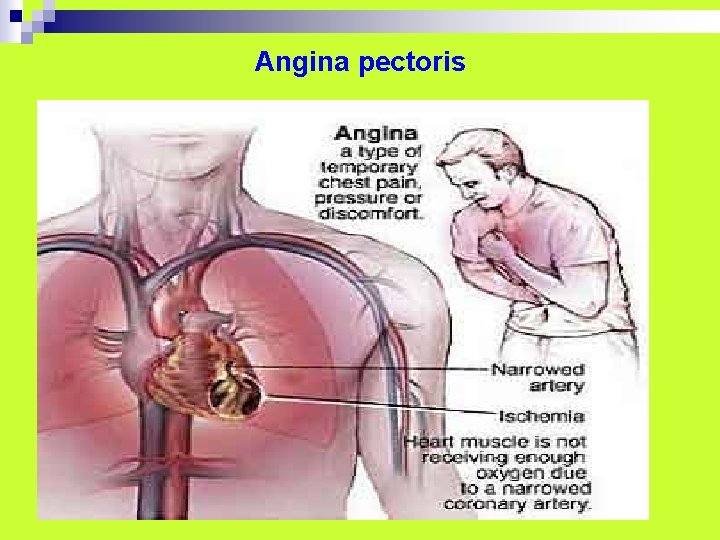
Angina pectoris
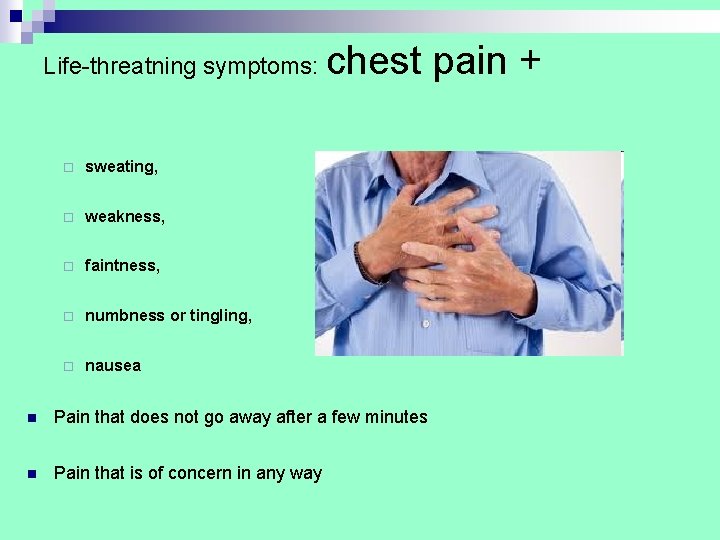
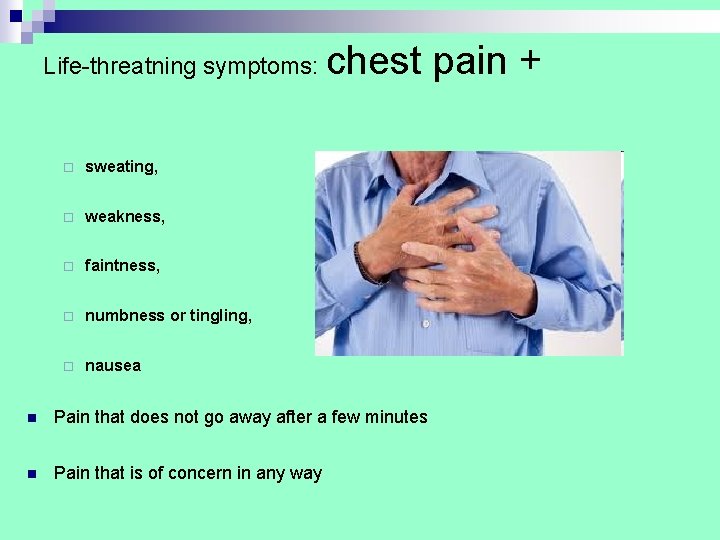
Life-threatning symptoms: ¨ sweating, ¨ weakness, ¨ faintness, ¨ numbness or tingling, ¨ nausea chest pain + n Pain that does not go away after a few minutes n Pain that is of concern in any way
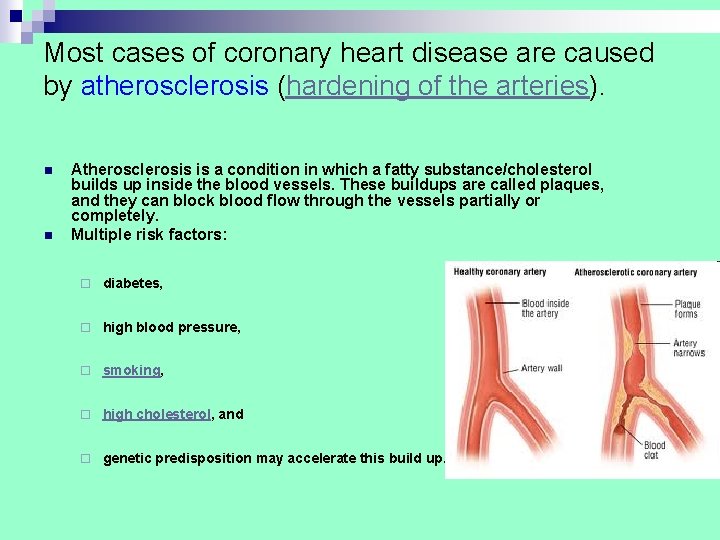
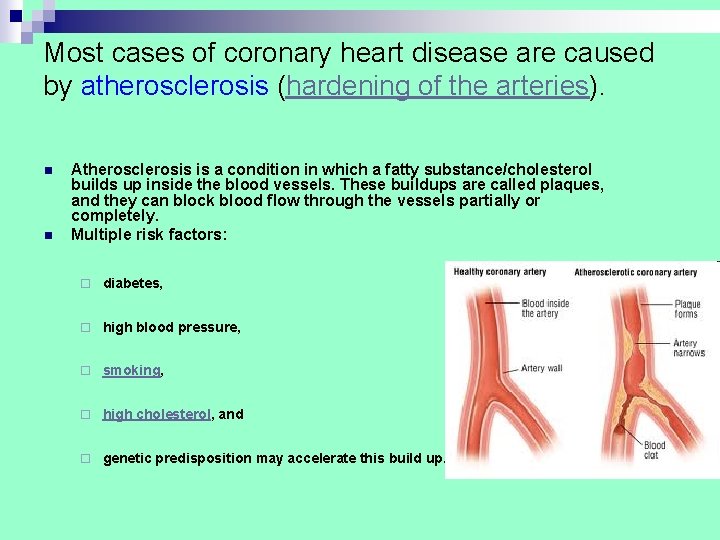
Most cases of coronary heart disease are caused by atherosclerosis (hardening of the arteries). n n Atherosclerosis is a condition in which a fatty substance/cholesterol builds up inside the blood vessels. These buildups are called plaques, and they can block blood flow through the vessels partially or completely. Multiple risk factors: ¨ diabetes, ¨ high blood pressure, ¨ smoking, ¨ high cholesterol, and ¨ genetic predisposition may accelerate this build up.
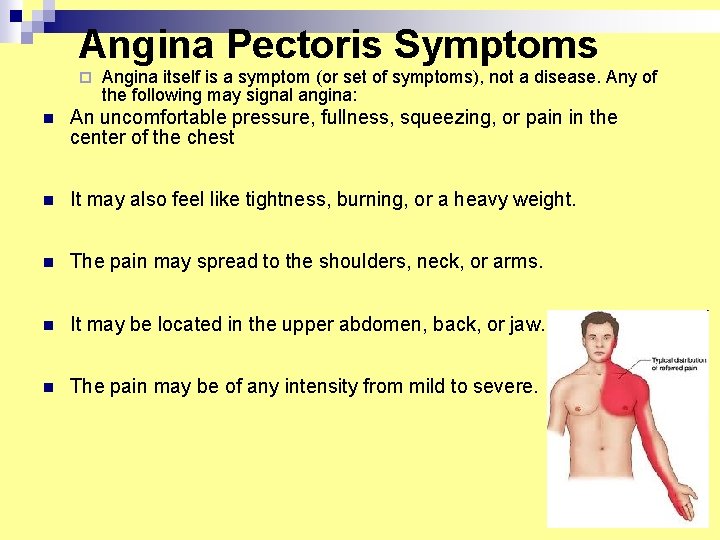
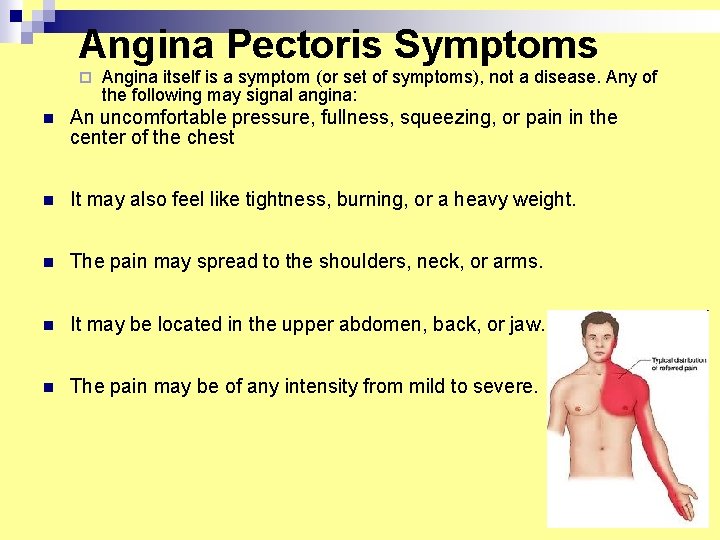
Angina Pectoris Symptoms ¨ Angina itself is a symptom (or set of symptoms), not a disease. Any of the following may signal angina: n An uncomfortable pressure, fullness, squeezing, or pain in the center of the chest n It may also feel like tightness, burning, or a heavy weight. n The pain may spread to the shoulders, neck, or arms. n It may be located in the upper abdomen, back, or jaw. n The pain may be of any intensity from mild to severe.

ANTIANGINAL (CORONARY ACTIVE) DRUGS І. Nitrates and sidnonims ІІ. Beta-adrenoblockers ІІІ. Calcium channel blockers ІУ. Activators of potassium channels

NITRATES
NITRATES n n Glyceryl trinitrate isosorbid dinitrate isosorbid-5 -mononitrate INDICATIONS Treatment and prevention of angina. Treatment of acute left ventricular failure.
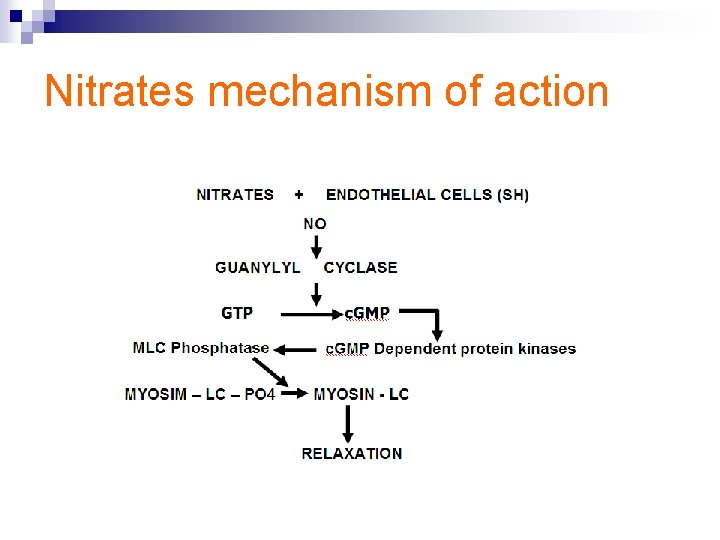
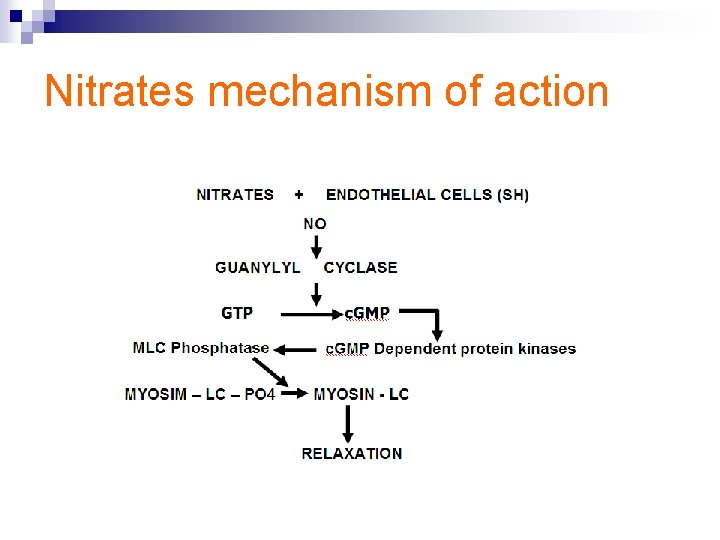
Nitrates mechanism of action
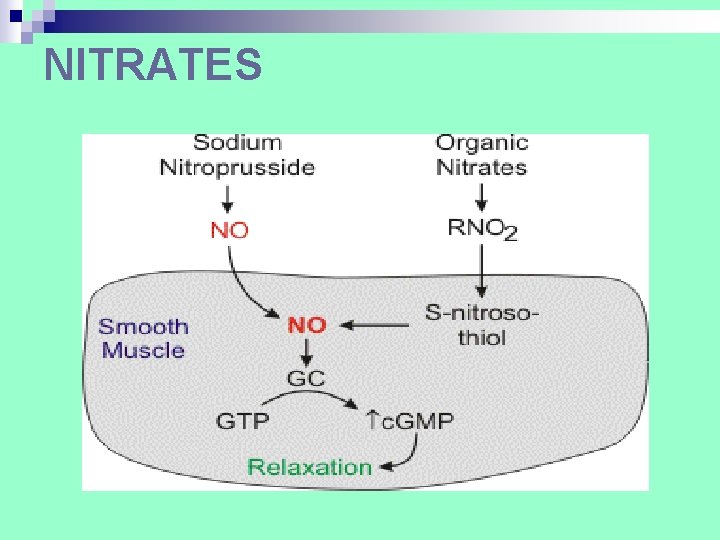
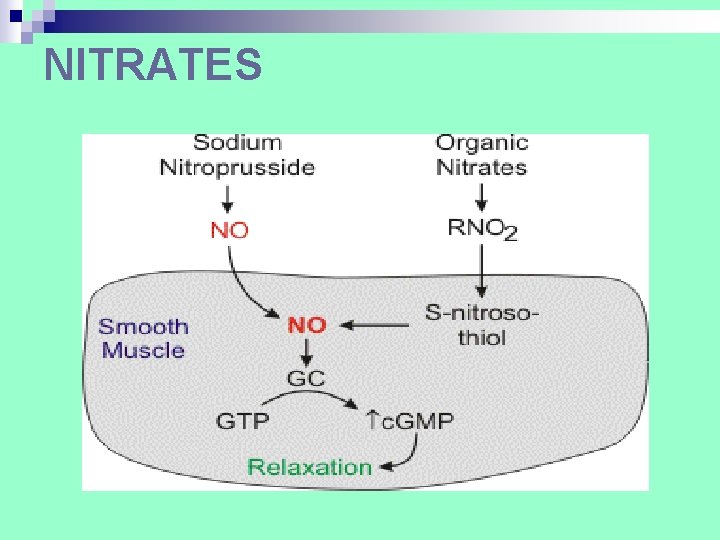
NITRATES
Nitroglycerine Unique transdermal system in a form of plaster

Contraindications for nitroglycerine use

Iso Mak Retard 20 mg Iso Mak Retard 40 mg Isomak Retard 60 mg (isosorbid dinitrate)
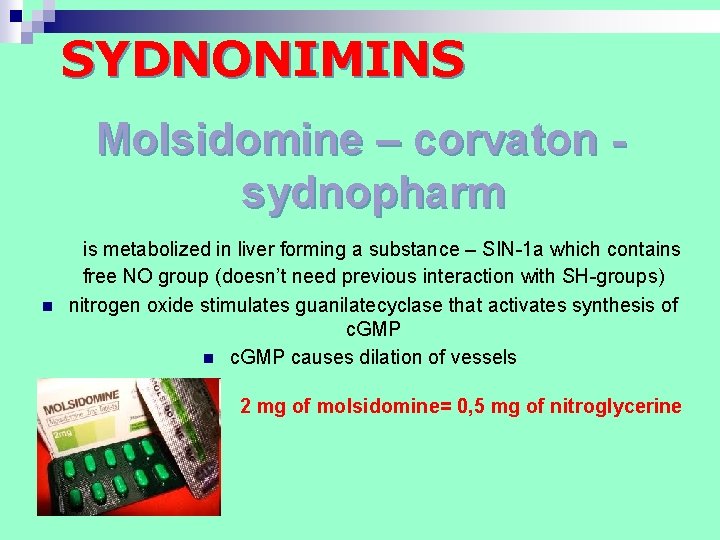
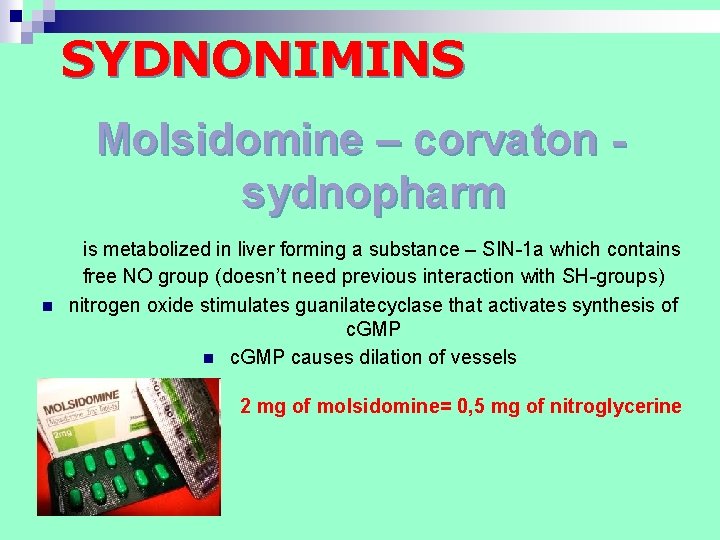
SYDNONIMINS Molsidomine – corvaton sydnopharm n is metabolized in liver forming a substance – SIN-1 a which contains free NО group (doesn’t need previous interaction with SH-groups) nitrogen oxide stimulates guanilatecyclase that activates synthesis of c. GMP n c. GMP causes dilation of vessels 2 mg of molsidomine= 0, 5 mg of nitroglycerine
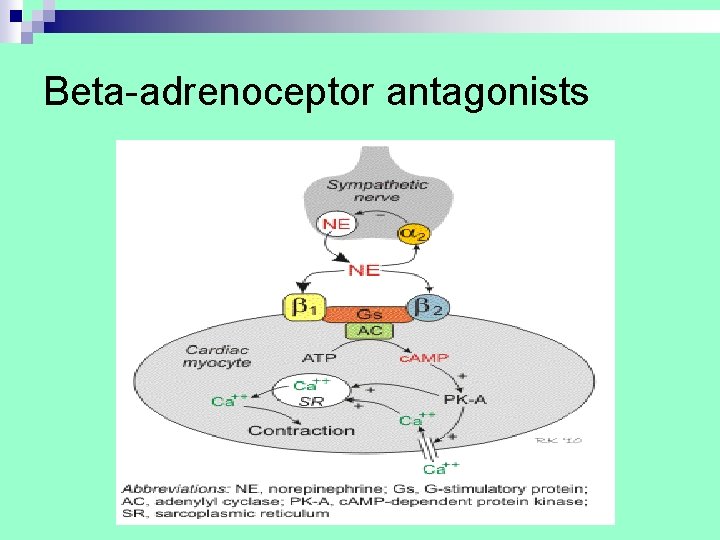
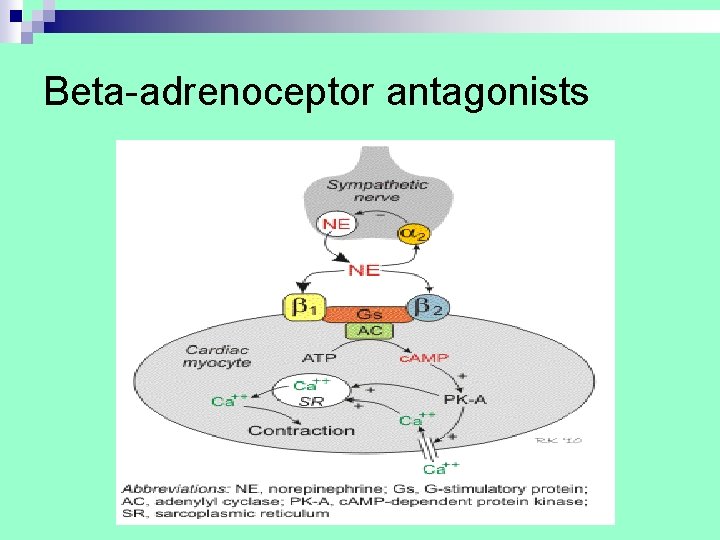
Beta-adrenoceptor antagonists

Nebivolol beta-blocker that also causes vasodilation by stimulating the release of nitric oxide
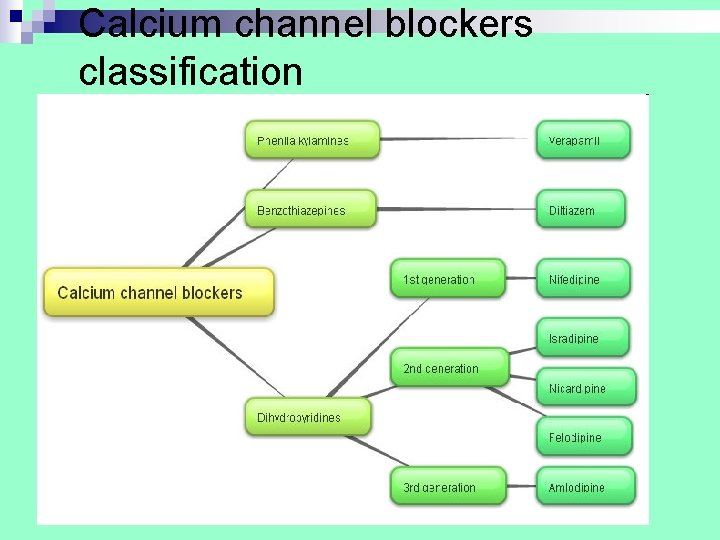
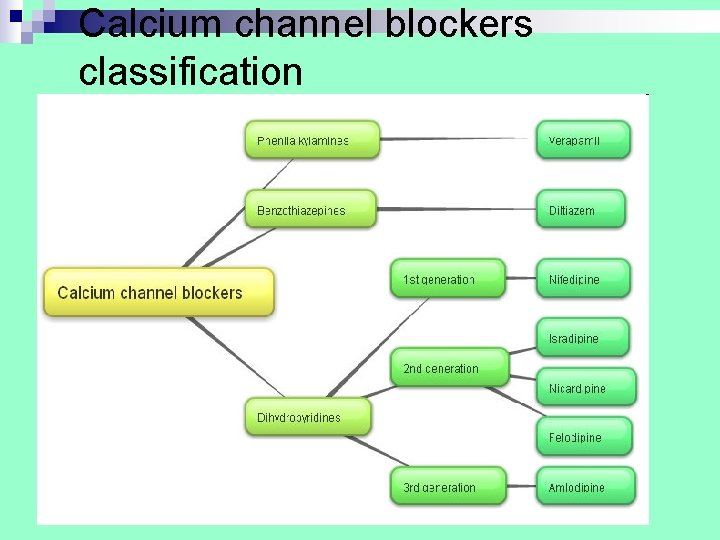
Calcium channel blockers classification

Calcium channel blockers 1. Phenyalkylamines(verapamil) 2. Benzthiazepines(dilthiazem) 3. Derivatives of Dihydropyridine (nifedipine, amlodipine, nimodipine)
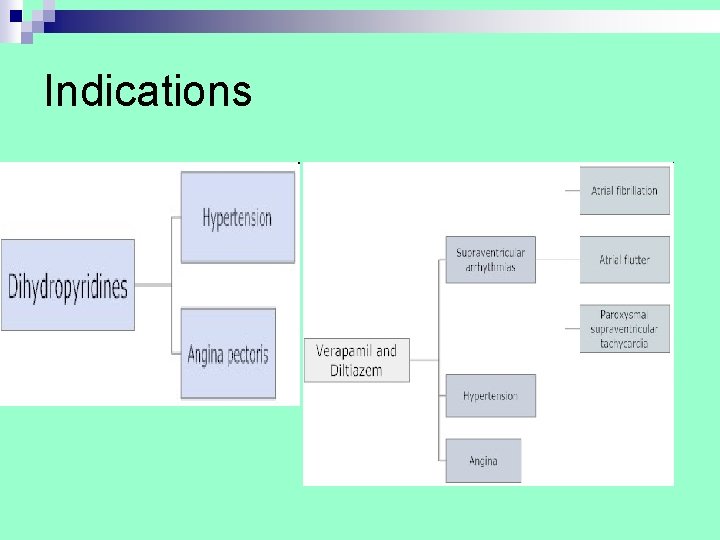
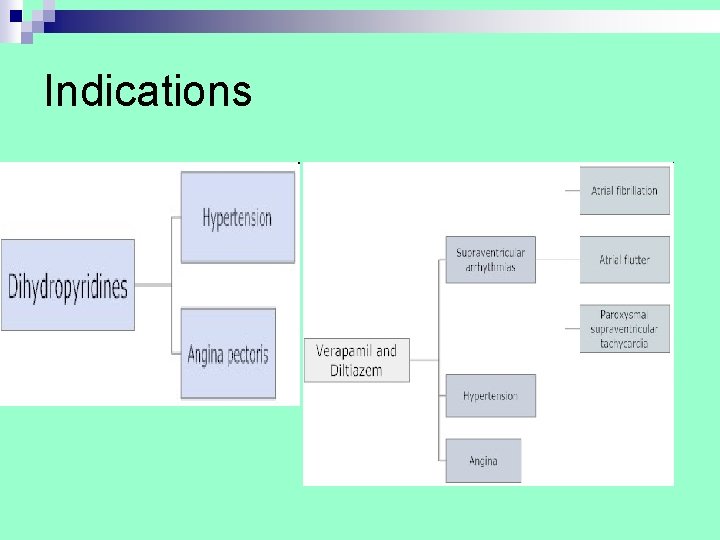
Indications

Common side effects of calcium channel blockers include: n n n n n headache, constipation, rash, nausea, flushing, edema (fluid accumulation in tissues), drowsiness, low blood pressure, and dizziness. Sexual dysfunction, overgrowth of gums, and liver dysfunction also have been associated with calcium channel blockers. Verapamil (Covera-HS, Verelan PM, Calan) and diltiazem (Cardizem LA, Tiazac) worsen heart failure because they reduce the ability of the heart to contract and pump blood.
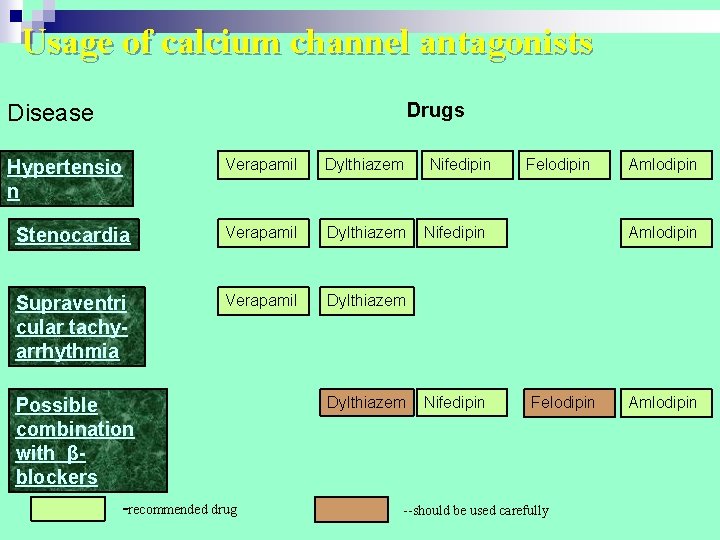
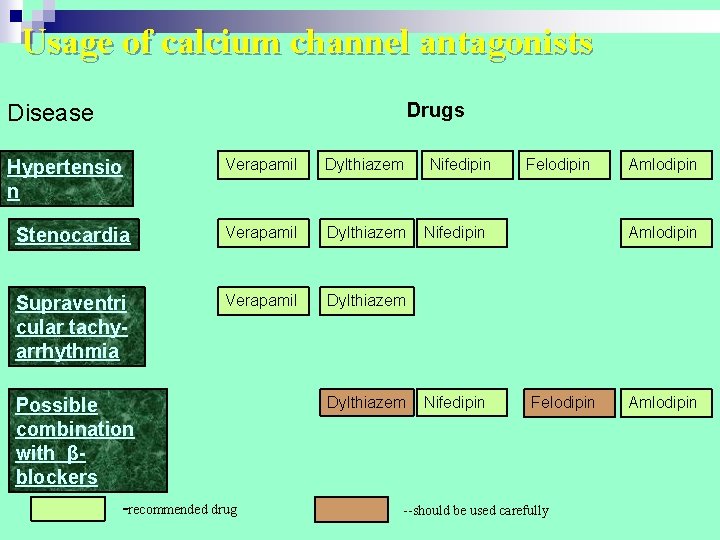
Usage of calcium channel antagonists Drugs Disease Verapamil Dylthiazem Stenocardia Verapamil Dylthiazem Supraventri cular tachyarrhythmia Verapamil Dylthiazem Hypertensio n Possible combination with βblockers -recommended drug Dylthiazem Nifedipin Felodipin Nifedipin Amlodipin Felodipin --should be used carefully Amlodipin

Nifedipin (Са 2+ ions antagonist of dyhydropyrydine series)

Nicorandil Potassium channel activator

Adjunctive Antianginal Drugs Acetylsalicylic acid
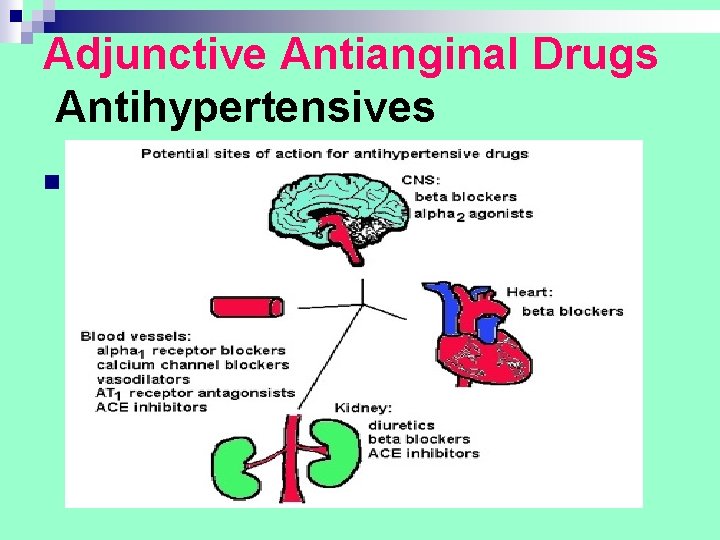
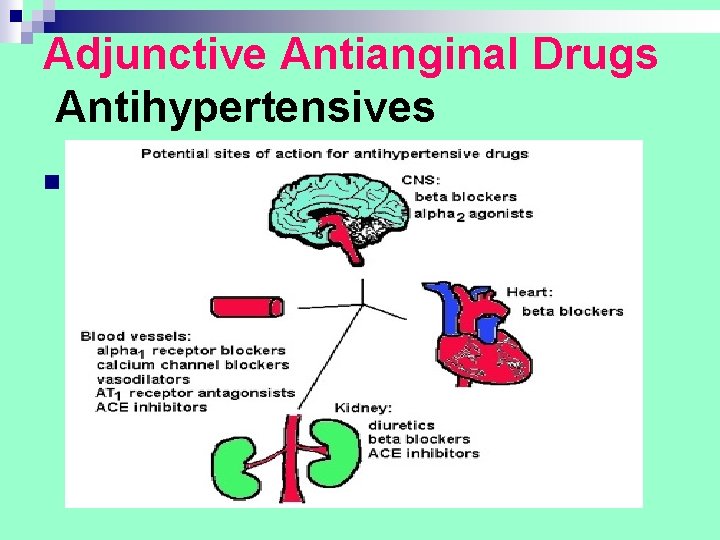
Adjunctive Antianginal Drugs Antihypertensives n .

Amiodarone Antiarrhythmic drug acting on atrial and ventricular tissues
Amiodarone n Treatment by mouth 200 mg 3 times daily for 1 week reduced to 200 mg twice daily for a further week. ¨ Maintenance dose, usually 200 mg daily or the minimum required to control the arrhythmia. ¨ n Treatment by intravenous infusion ¨ n Via a central line, 5 mg/kg over 20 -120 minutes with ECG monitoring; maximum 1. 2 g in 24 hours. Emergency treatment during cardiopulmonary resuscitation ¨ VF or pulseless VT, 300 mg by intravenous injection over at least 3 minutes (pre-filled syringe).
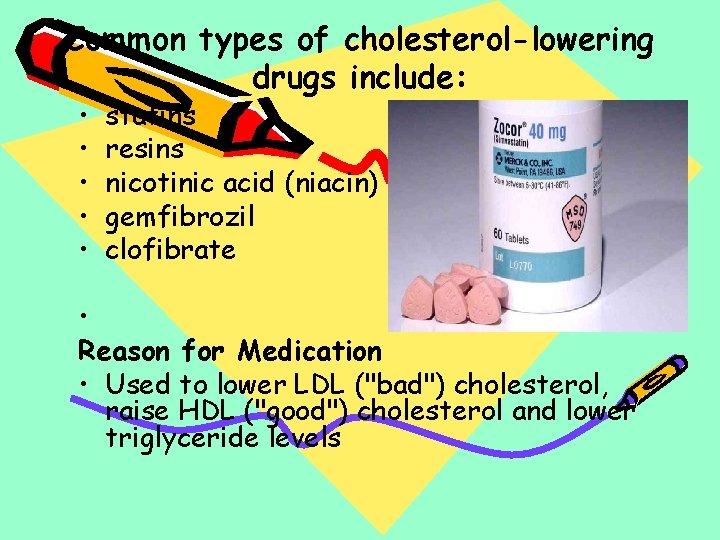
Common types of cholesterol-lowering drugs include: • • • statins resins nicotinic acid (niacin) gemfibrozil clofibrate • Reason for Medication • Used to lower LDL ("bad") cholesterol, raise HDL ("good") cholesterol and lower triglyceride levels

Cholesterol-lowering drugs
Choose good nutrition Reduce blood cholesterol Lower high blood pressure Be physically active every day Aim for a healthy weight Manage diabetes Reduce stress Limit alcohol Stop smoking