Clinical Perspectives Glaucoma Glaucomatous cupping a Glaucomatous cupping
- Slides: 17
Clinical Perspectives Glaucoma
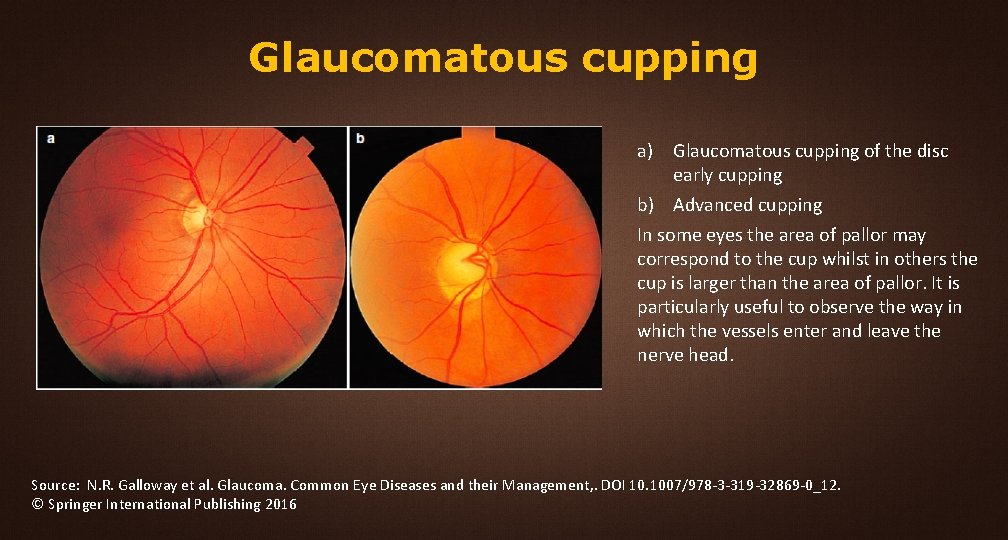
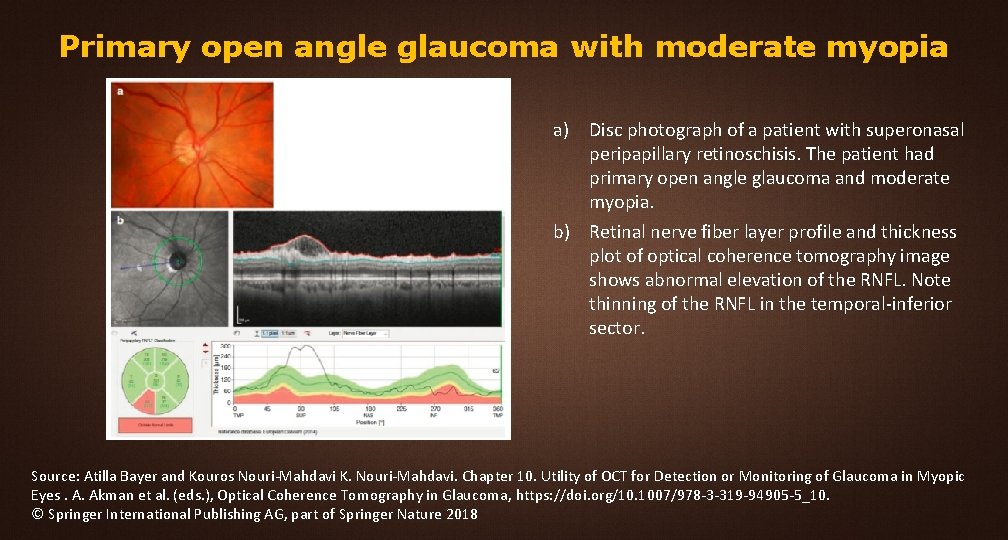
Glaucomatous cupping a) Glaucomatous cupping of the disc early cupping b) Advanced cupping In some eyes the area of pallor may correspond to the cup whilst in others the cup is larger than the area of pallor. It is particularly useful to observe the way in which the vessels enter and leave the nerve head. Source: N. R. Galloway et al. Glaucoma. Common Eye Diseases and their Management, . DOI 10. 1007/978 -3 -319 -32869 -0_12. © Springer International Publishing 2016
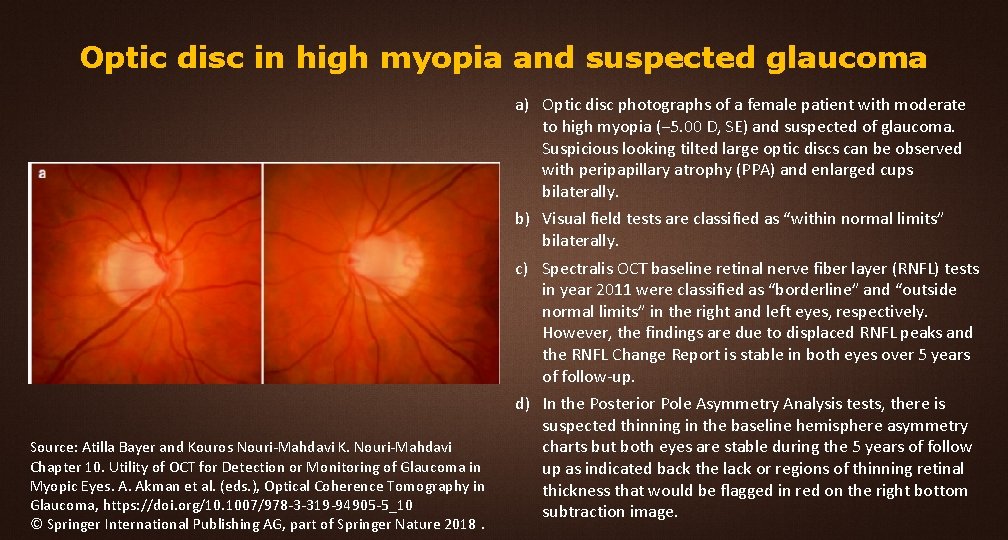
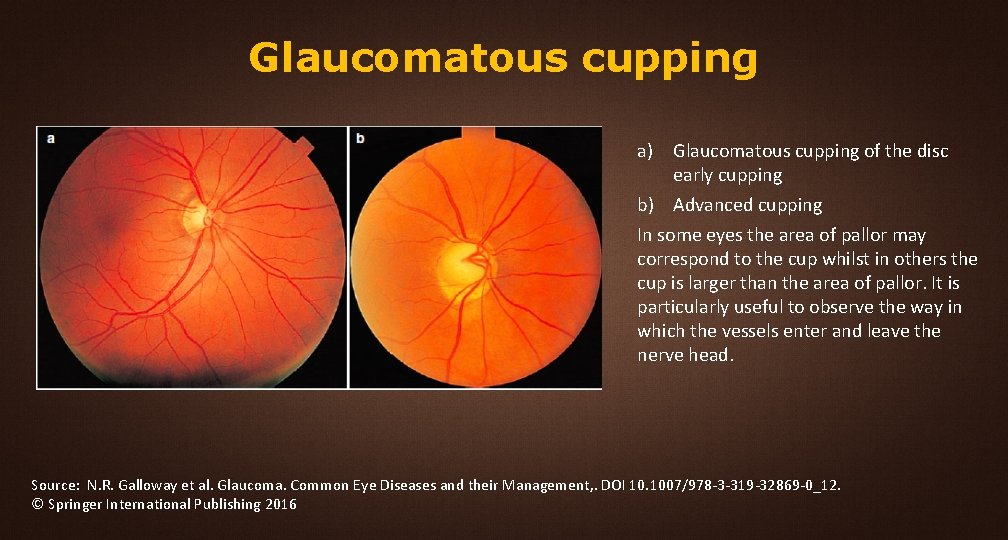
Optic disc in high myopia and suspected glaucoma Source: Atilla Bayer and Kouros Nouri-Mahdavi K. Nouri-Mahdavi Chapter 10. Utility of OCT for Detection or Monitoring of Glaucoma in Myopic Eyes. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_10 © Springer International Publishing AG, part of Springer Nature 2018. a) Optic disc photographs of a female patient with moderate to high myopia (− 5. 00 D, SE) and suspected of glaucoma. Suspicious looking tilted large optic discs can be observed with peripapillary atrophy (PPA) and enlarged cups bilaterally. b) Visual field tests are classified as “within normal limits” bilaterally. c) Spectralis OCT baseline retinal nerve fiber layer (RNFL) tests in year 2011 were classified as “borderline” and “outside normal limits” in the right and left eyes, respectively. However, the findings are due to displaced RNFL peaks and the RNFL Change Report is stable in both eyes over 5 years of follow-up. d) In the Posterior Pole Asymmetry Analysis tests, there is suspected thinning in the baseline hemisphere asymmetry charts but both eyes are stable during the 5 years of follow up as indicated back the lack or regions of thinning retinal thickness that would be flagged in red on the right bottom subtraction image.
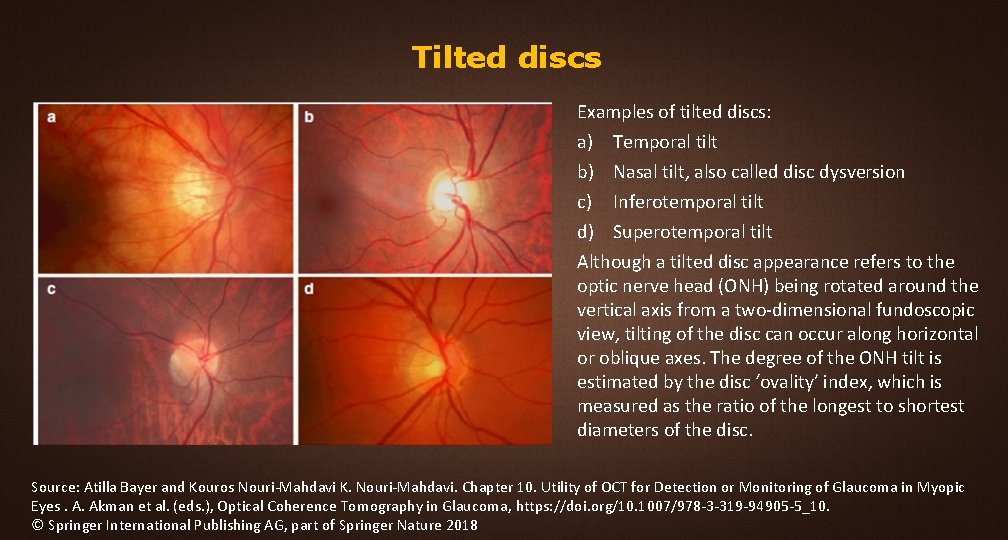
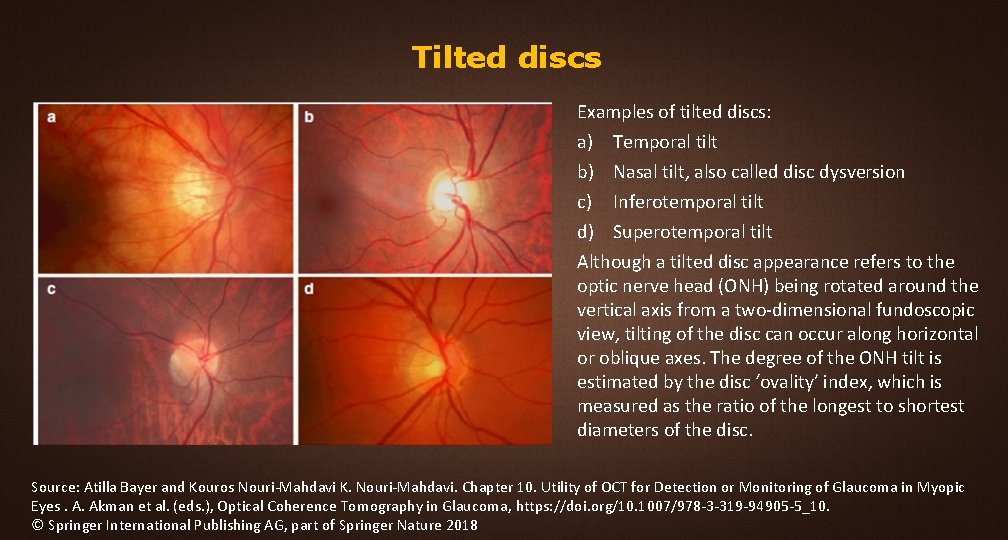
Tilted discs Examples of tilted discs: a) Temporal tilt b) Nasal tilt, also called disc dysversion c) Inferotemporal tilt d) Superotemporal tilt Although a tilted disc appearance refers to the optic nerve head (ONH) being rotated around the vertical axis from a two-dimensional fundoscopic view, tilting of the disc can occur along horizontal or oblique axes. The degree of the ONH tilt is estimated by the disc ‘ovality’ index, which is measured as the ratio of the longest to shortest diameters of the disc. Source: Atilla Bayer and Kouros Nouri-Mahdavi K. Nouri-Mahdavi. Chapter 10. Utility of OCT for Detection or Monitoring of Glaucoma in Myopic Eyes. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_10. © Springer International Publishing AG, part of Springer Nature 2018
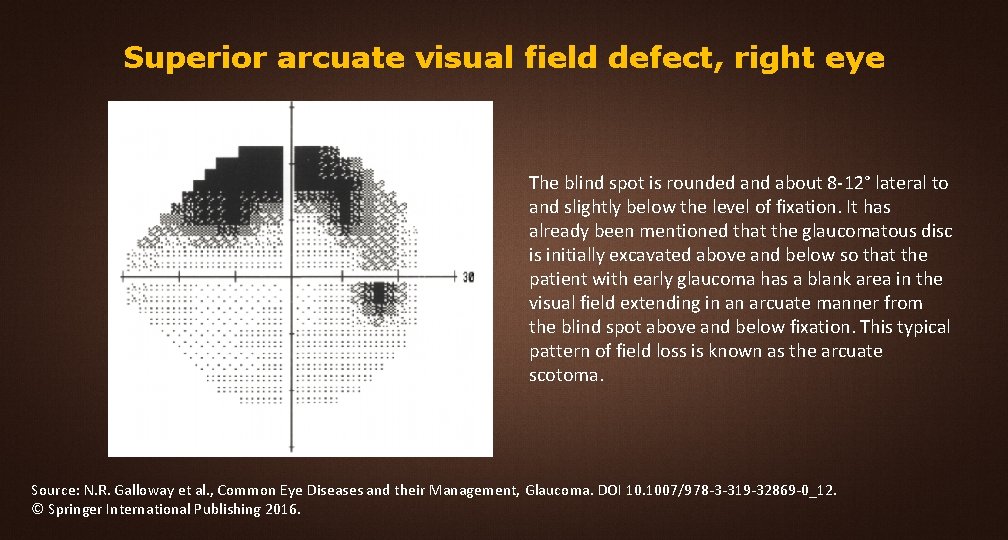
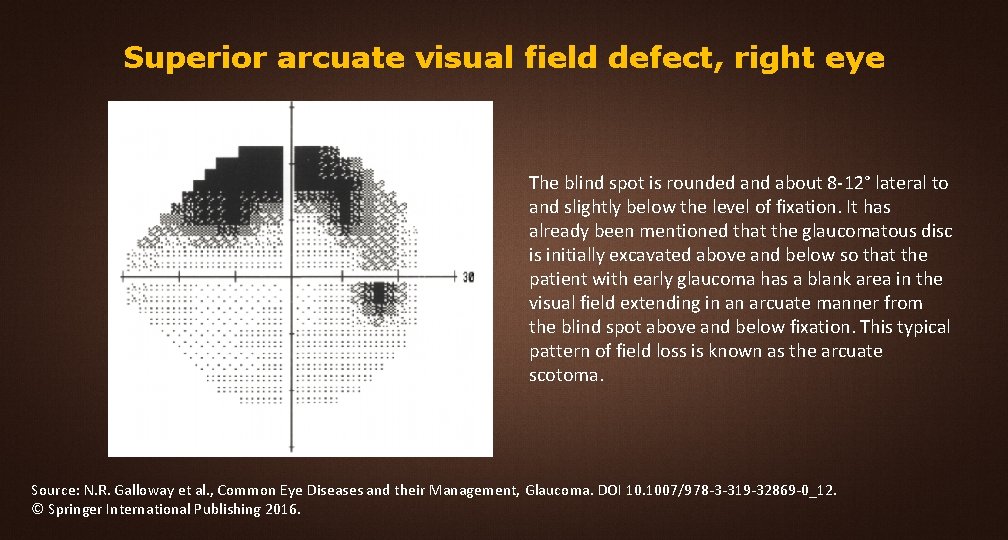
Superior arcuate visual field defect, right eye The blind spot is rounded and about 8 -12° lateral to and slightly below the level of fixation. It has already been mentioned that the glaucomatous disc is initially excavated above and below so that the patient with early glaucoma has a blank area in the visual field extending in an arcuate manner from the blind spot above and below fixation. This typical pattern of field loss is known as the arcuate scotoma. Source: N. R. Galloway et al. , Common Eye Diseases and their Management, Glaucoma. DOI 10. 1007/978 -3 -319 -32869 -0_12. © Springer International Publishing 2016.
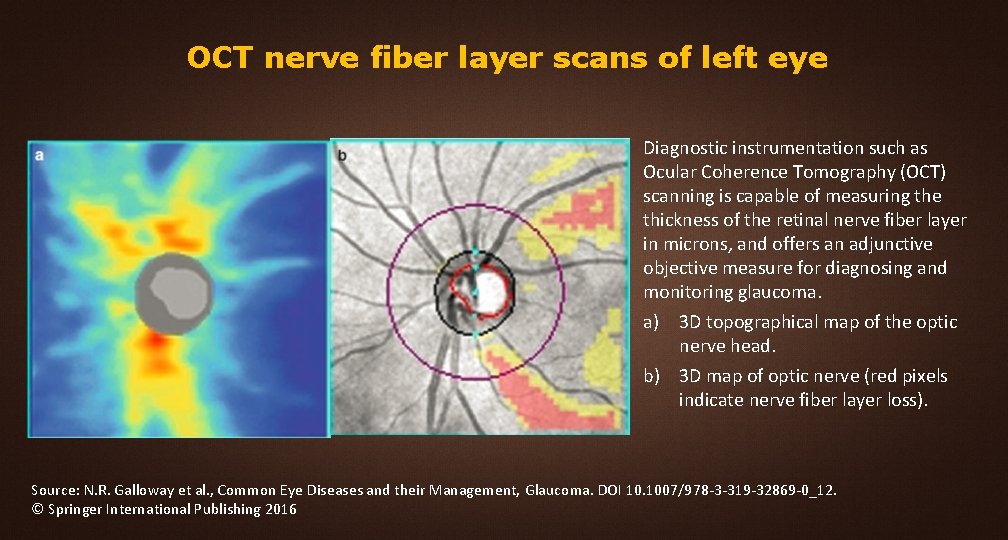
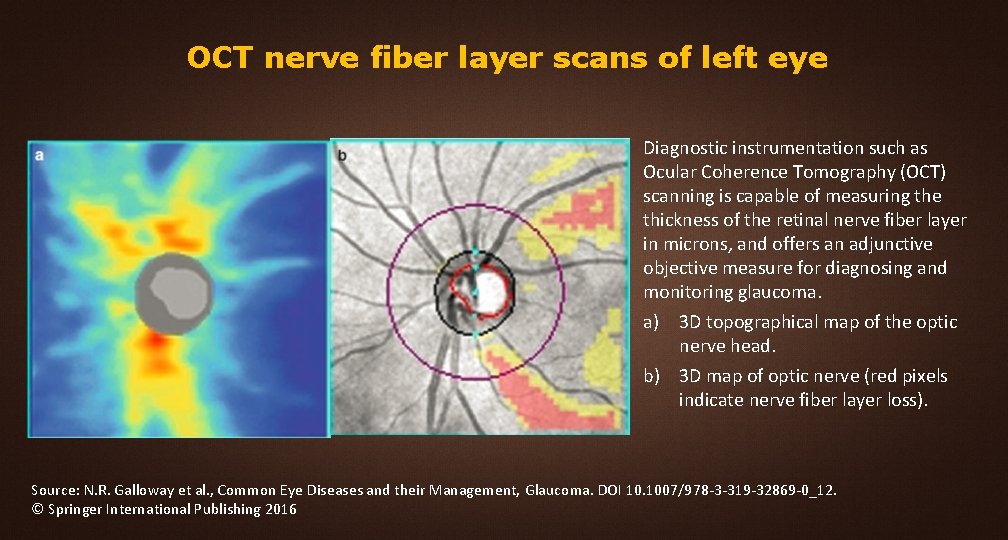
OCT nerve fiber layer scans of left eye Diagnostic instrumentation such as Ocular Coherence Tomography (OCT) scanning is capable of measuring the thickness of the retinal nerve fiber layer in microns, and offers an adjunctive objective measure for diagnosing and monitoring glaucoma. a) 3 D topographical map of the optic nerve head. b) 3 D map of optic nerve (red pixels indicate nerve fiber layer loss). Source: N. R. Galloway et al. , Common Eye Diseases and their Management, Glaucoma. DOI 10. 1007/978 -3 -319 -32869 -0_12. © Springer International Publishing 2016
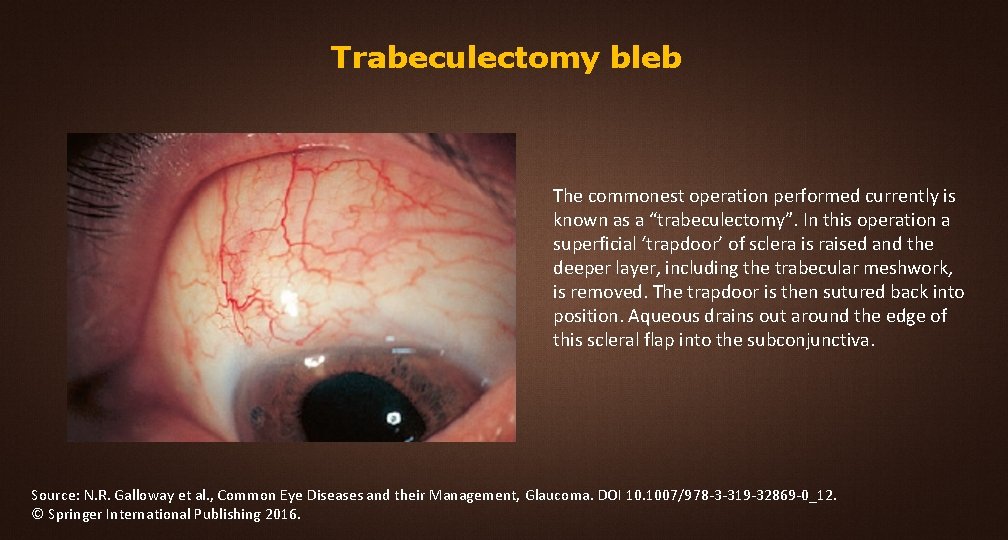
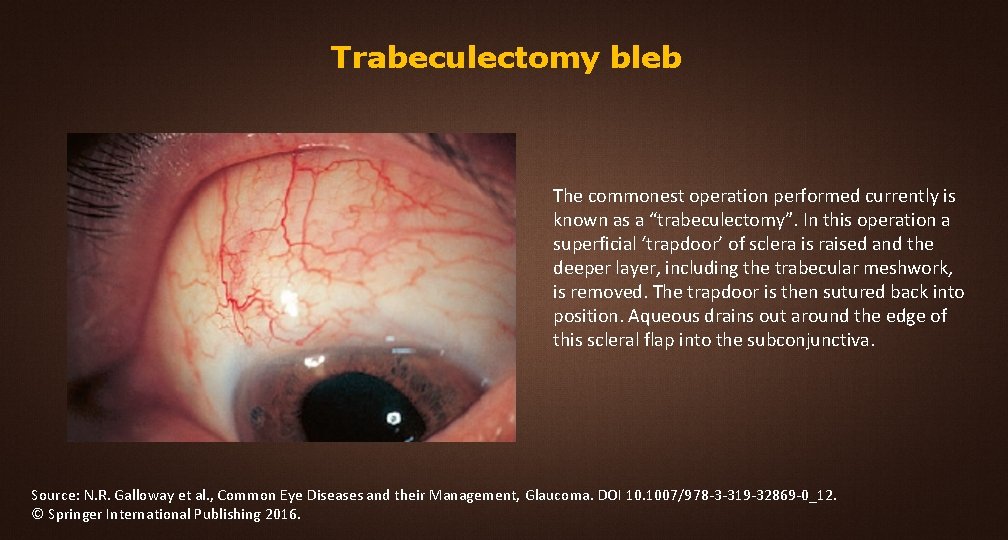
Trabeculectomy bleb The commonest operation performed currently is known as a “trabeculectomy”. In this operation a superficial ‘trapdoor’ of sclera is raised and the deeper layer, including the trabecular meshwork, is removed. The trapdoor is then sutured back into position. Aqueous drains out around the edge of this scleral flap into the subconjunctiva. Source: N. R. Galloway et al. , Common Eye Diseases and their Management, Glaucoma. DOI 10. 1007/978 -3 -319 -32869 -0_12. © Springer International Publishing 2016.
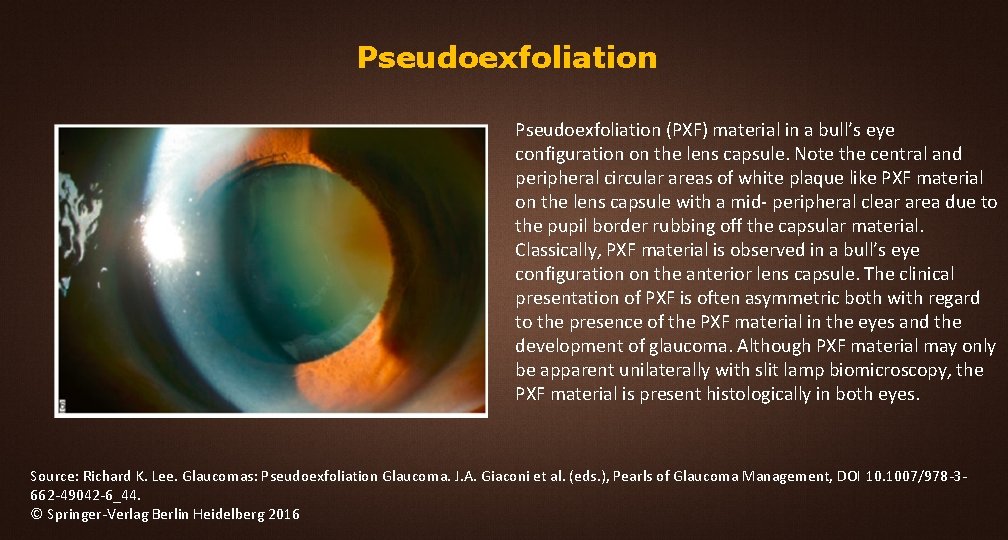
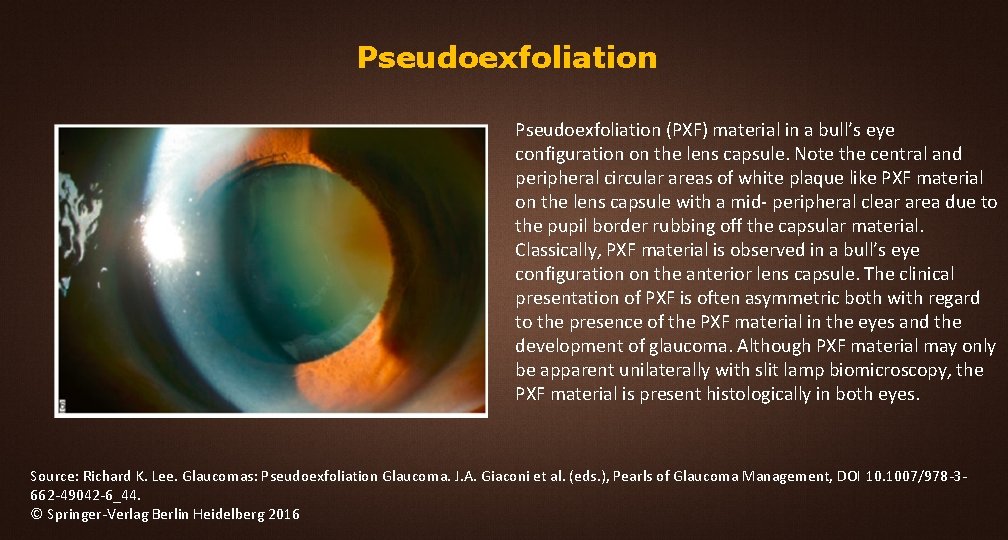
Pseudoexfoliation (PXF) material in a bull’s eye configuration on the lens capsule. Note the central and peripheral circular areas of white plaque like PXF material on the lens capsule with a mid- peripheral clear area due to the pupil border rubbing off the capsular material. Classically, PXF material is observed in a bull’s eye configuration on the anterior lens capsule. The clinical presentation of PXF is often asymmetric both with regard to the presence of the PXF material in the eyes and the development of glaucoma. Although PXF material may only be apparent unilaterally with slit lamp biomicroscopy, the PXF material is present histologically in both eyes. Source: Richard K. Lee. Glaucomas: Pseudoexfoliation Glaucoma. J. A. Giaconi et al. (eds. ), Pearls of Glaucoma Management, DOI 10. 1007/978 -3662 -49042 -6_44. © Springer-Verlag Berlin Heidelberg 2016
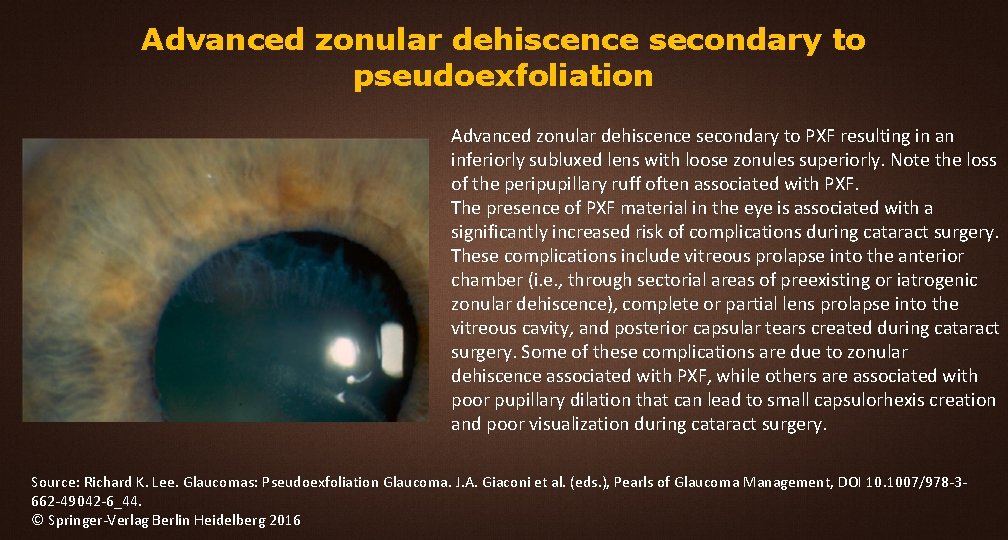
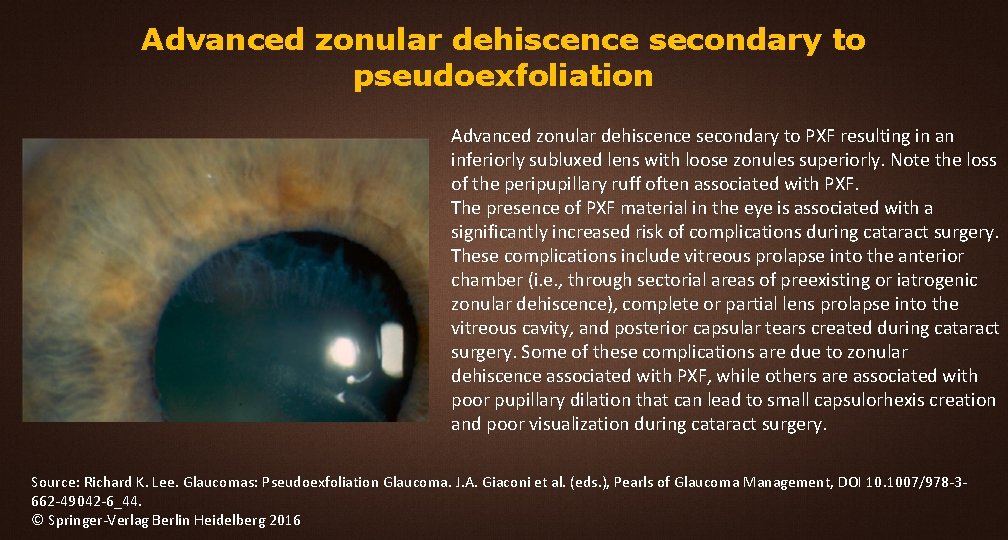
Advanced zonular dehiscence secondary to pseudoexfoliation Advanced zonular dehiscence secondary to PXF resulting in an inferiorly subluxed lens with loose zonules superiorly. Note the loss of the peripupillary ruff often associated with PXF. The presence of PXF material in the eye is associated with a significantly increased risk of complications during cataract surgery. These complications include vitreous prolapse into the anterior chamber (i. e. , through sectorial areas of preexisting or iatrogenic zonular dehiscence), complete or partial lens prolapse into the vitreous cavity, and posterior capsular tears created during cataract surgery. Some of these complications are due to zonular dehiscence associated with PXF, while others are associated with poor pupillary dilation that can lead to small capsulorhexis creation and poor visualization during cataract surgery. Source: Richard K. Lee. Glaucomas: Pseudoexfoliation Glaucoma. J. A. Giaconi et al. (eds. ), Pearls of Glaucoma Management, DOI 10. 1007/978 -3662 -49042 -6_44. © Springer-Verlag Berlin Heidelberg 2016
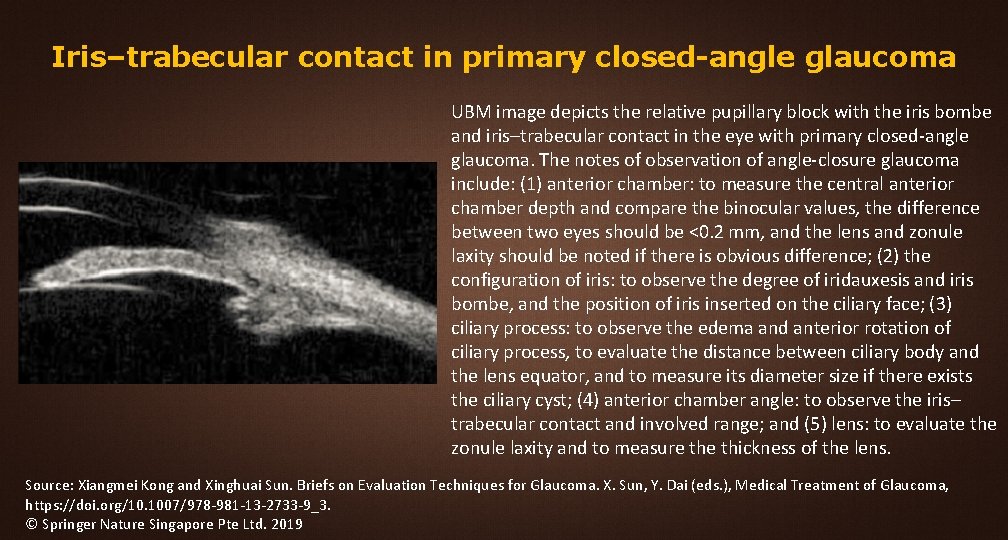
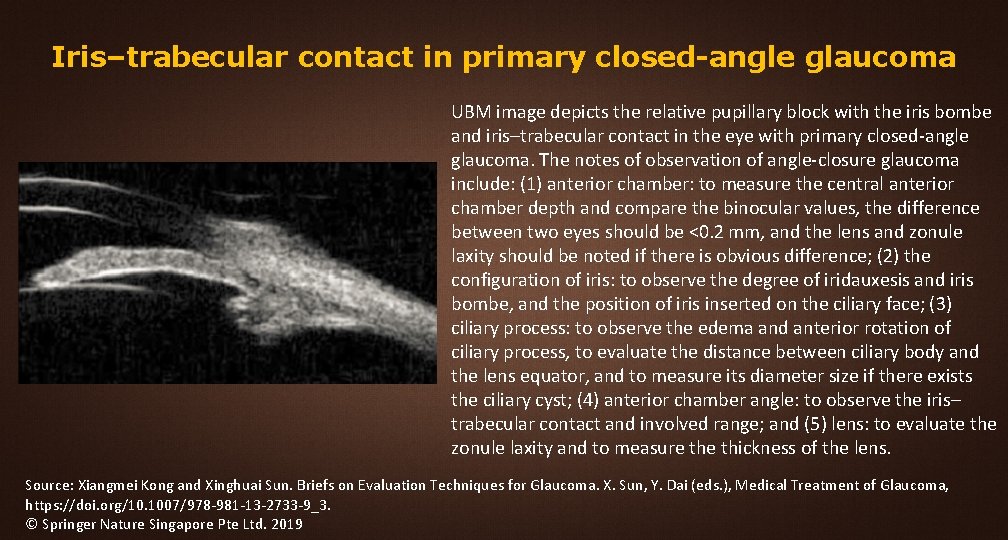
Iris–trabecular contact in primary closed-angle glaucoma UBM image depicts the relative pupillary block with the iris bombe and iris–trabecular contact in the eye with primary closed-angle glaucoma. The notes of observation of angle-closure glaucoma include: (1) anterior chamber: to measure the central anterior chamber depth and compare the binocular values, the difference between two eyes should be <0. 2 mm, and the lens and zonule laxity should be noted if there is obvious difference; (2) the configuration of iris: to observe the degree of iridauxesis and iris bombe, and the position of iris inserted on the ciliary face; (3) ciliary process: to observe the edema and anterior rotation of ciliary process, to evaluate the distance between ciliary body and the lens equator, and to measure its diameter size if there exists the ciliary cyst; (4) anterior chamber angle: to observe the iris– trabecular contact and involved range; and (5) lens: to evaluate the zonule laxity and to measure thickness of the lens. Source: Xiangmei Kong and Xinghuai Sun. Briefs on Evaluation Techniques for Glaucoma. X. Sun, Y. Dai (eds. ), Medical Treatment of Glaucoma, https: //doi. org/10. 1007/978 -981 -13 -2733 -9_3. © Springer Nature Singapore Pte Ltd. 2019
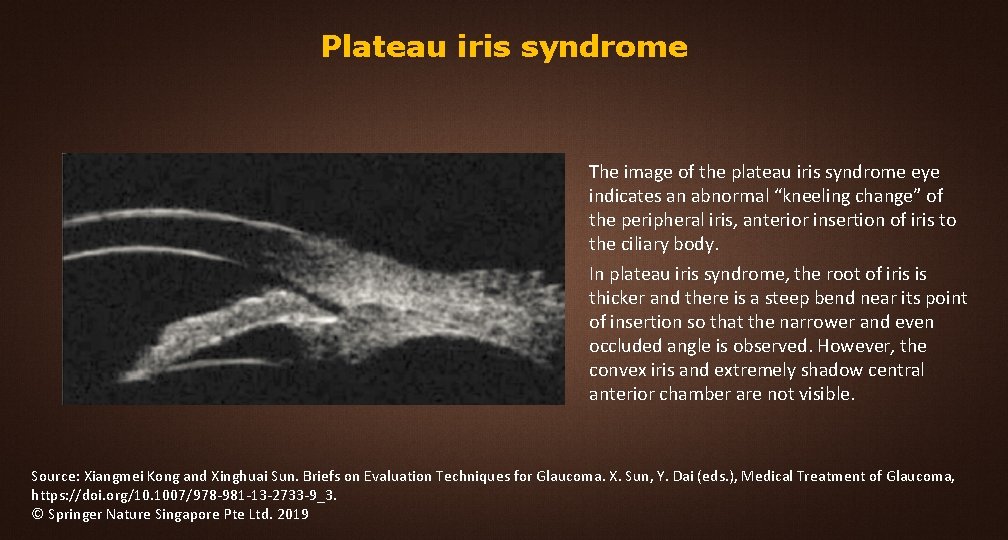
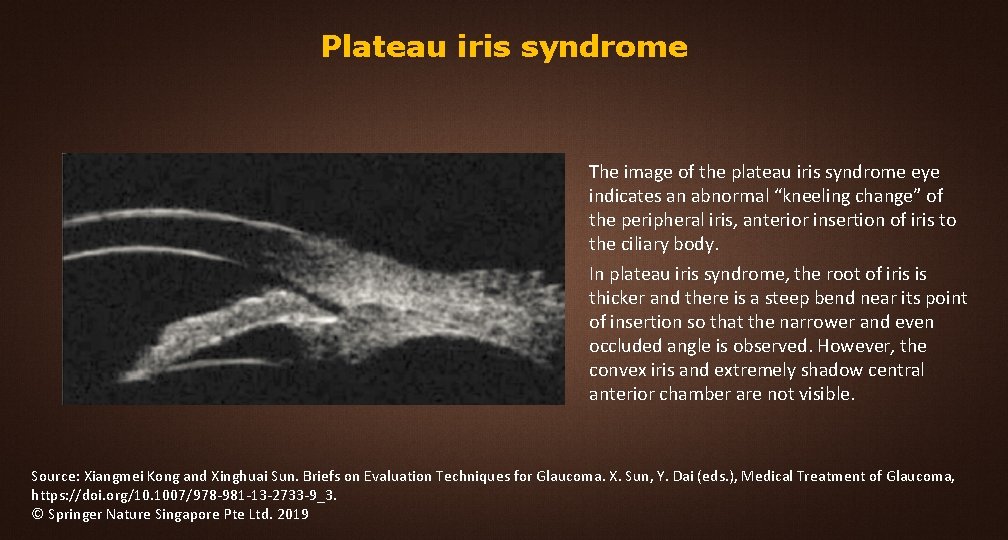
Plateau iris syndrome The image of the plateau iris syndrome eye indicates an abnormal “kneeling change” of the peripheral iris, anterior insertion of iris to the ciliary body. In plateau iris syndrome, the root of iris is thicker and there is a steep bend near its point of insertion so that the narrower and even occluded angle is observed. However, the convex iris and extremely shadow central anterior chamber are not visible. Source: Xiangmei Kong and Xinghuai Sun. Briefs on Evaluation Techniques for Glaucoma. X. Sun, Y. Dai (eds. ), Medical Treatment of Glaucoma, https: //doi. org/10. 1007/978 -981 -13 -2733 -9_3. © Springer Nature Singapore Pte Ltd. 2019
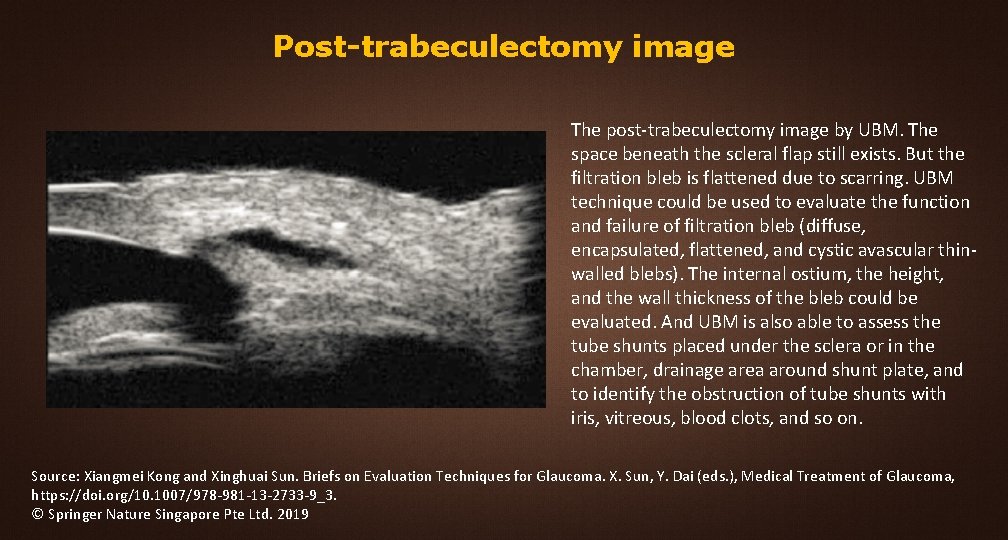
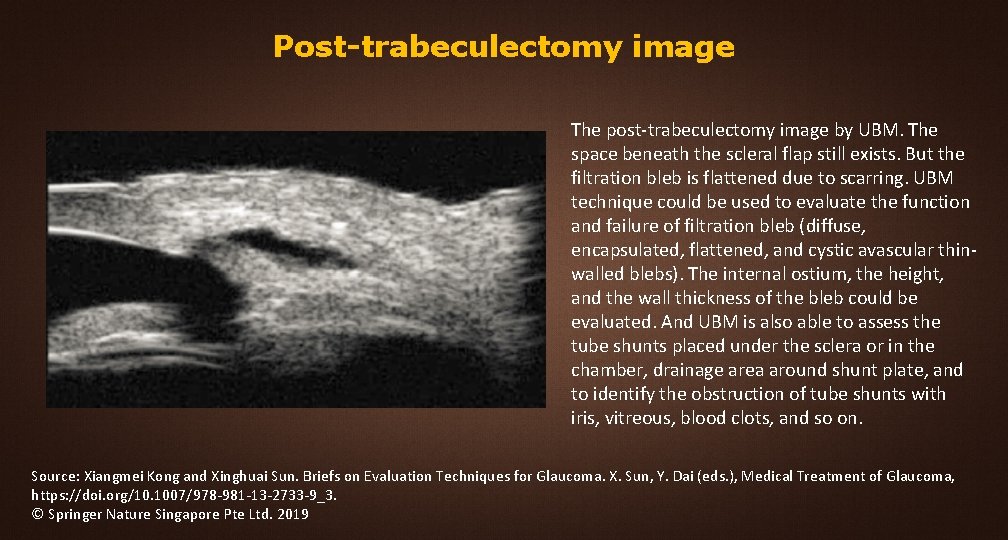
Post-trabeculectomy image The post-trabeculectomy image by UBM. The space beneath the scleral flap still exists. But the filtration bleb is flattened due to scarring. UBM technique could be used to evaluate the function and failure of filtration bleb (diffuse, encapsulated, flattened, and cystic avascular thinwalled blebs). The internal ostium, the height, and the wall thickness of the bleb could be evaluated. And UBM is also able to assess the tube shunts placed under the sclera or in the chamber, drainage area around shunt plate, and to identify the obstruction of tube shunts with iris, vitreous, blood clots, and so on. Source: Xiangmei Kong and Xinghuai Sun. Briefs on Evaluation Techniques for Glaucoma. X. Sun, Y. Dai (eds. ), Medical Treatment of Glaucoma, https: //doi. org/10. 1007/978 -981 -13 -2733 -9_3. © Springer Nature Singapore Pte Ltd. 2019
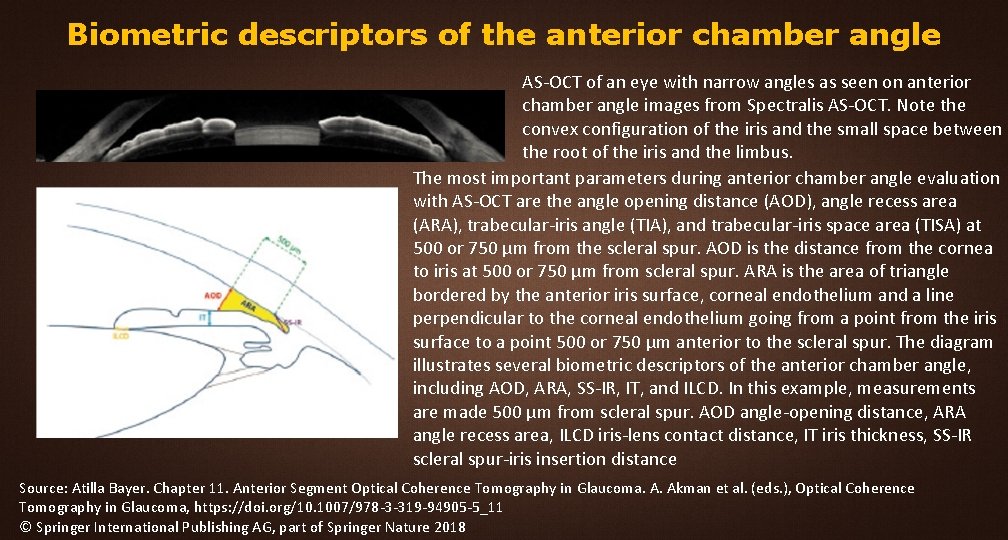
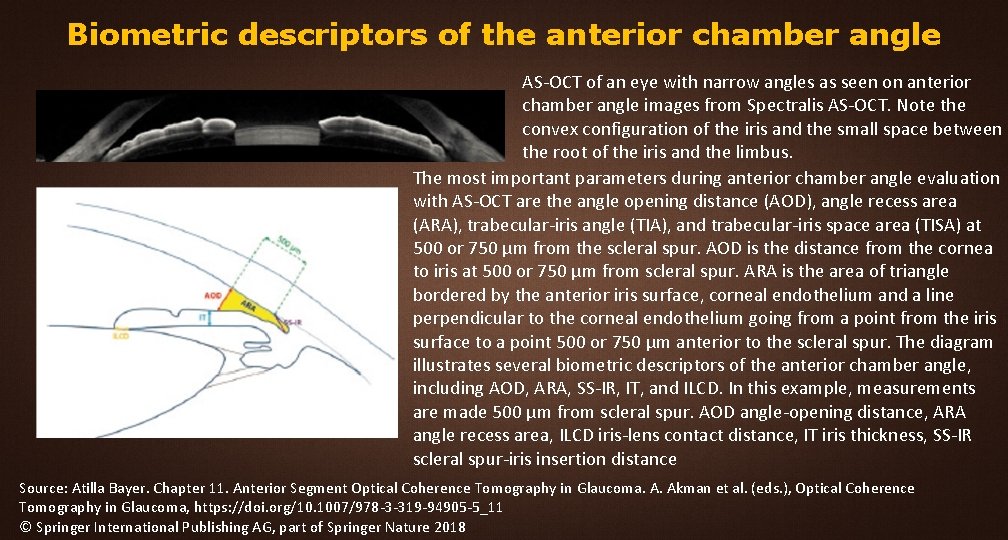
Biometric descriptors of the anterior chamber angle AS-OCT of an eye with narrow angles as seen on anterior chamber angle images from Spectralis AS-OCT. Note the convex configuration of the iris and the small space between the root of the iris and the limbus. The most important parameters during anterior chamber angle evaluation with AS-OCT are the angle opening distance (AOD), angle recess area (ARA), trabecular-iris angle (TIA), and trabecular-iris space area (TISA) at 500 or 750 μm from the scleral spur. AOD is the distance from the cornea to iris at 500 or 750 μm from scleral spur. ARA is the area of triangle bordered by the anterior iris surface, corneal endothelium and a line perpendicular to the corneal endothelium going from a point from the iris surface to a point 500 or 750 μm anterior to the scleral spur. The diagram illustrates several biometric descriptors of the anterior chamber angle, including AOD, ARA, SS-IR, IT, and ILCD. In this example, measurements are made 500 μm from scleral spur. AOD angle-opening distance, ARA angle recess area, ILCD iris-lens contact distance, IT iris thickness, SS-IR scleral spur-iris insertion distance Source: Atilla Bayer. Chapter 11. Anterior Segment Optical Coherence Tomography in Glaucoma. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_11 © Springer International Publishing AG, part of Springer Nature 2018
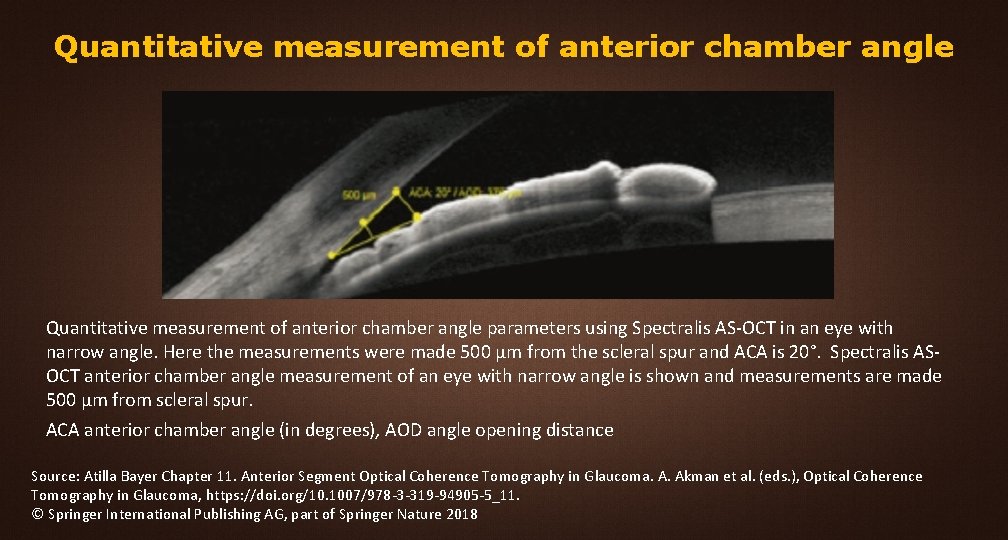
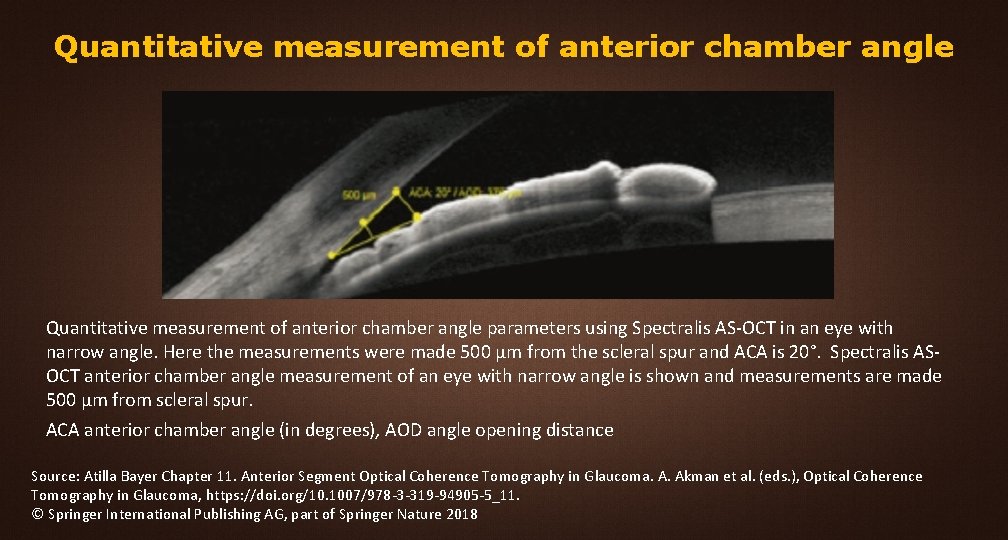
Quantitative measurement of anterior chamber angle parameters using Spectralis AS-OCT in an eye with narrow angle. Here the measurements were made 500 μm from the scleral spur and ACA is 20°. Spectralis ASOCT anterior chamber angle measurement of an eye with narrow angle is shown and measurements are made 500 μm from scleral spur. ACA anterior chamber angle (in degrees), AOD angle opening distance Source: Atilla Bayer Chapter 11. Anterior Segment Optical Coherence Tomography in Glaucoma. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_11. © Springer International Publishing AG, part of Springer Nature 2018
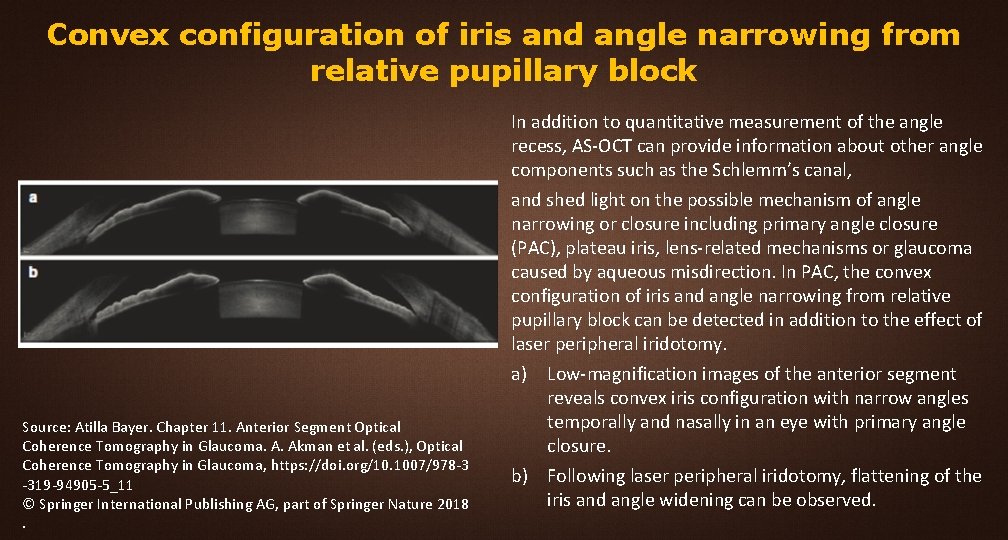
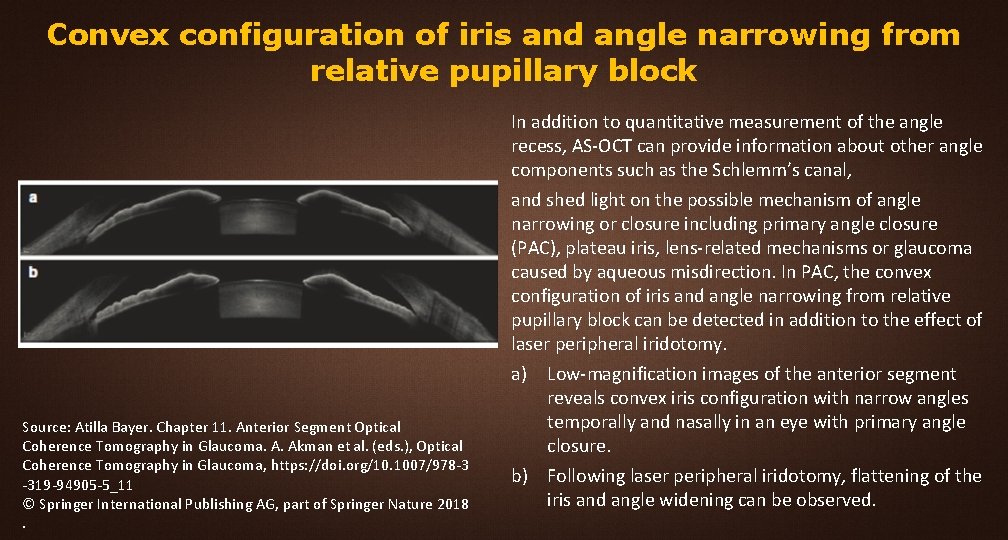
Convex configuration of iris and angle narrowing from relative pupillary block Source: Atilla Bayer. Chapter 11. Anterior Segment Optical Coherence Tomography in Glaucoma. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_11 © Springer International Publishing AG, part of Springer Nature 2018. In addition to quantitative measurement of the angle recess, AS-OCT can provide information about other angle components such as the Schlemm’s canal, and shed light on the possible mechanism of angle narrowing or closure including primary angle closure (PAC), plateau iris, lens-related mechanisms or glaucoma caused by aqueous misdirection. In PAC, the convex configuration of iris and angle narrowing from relative pupillary block can be detected in addition to the effect of laser peripheral iridotomy. a) Low-magnification images of the anterior segment reveals convex iris configuration with narrow angles temporally and nasally in an eye with primary angle closure. b) Following laser peripheral iridotomy, flattening of the iris and angle widening can be observed.
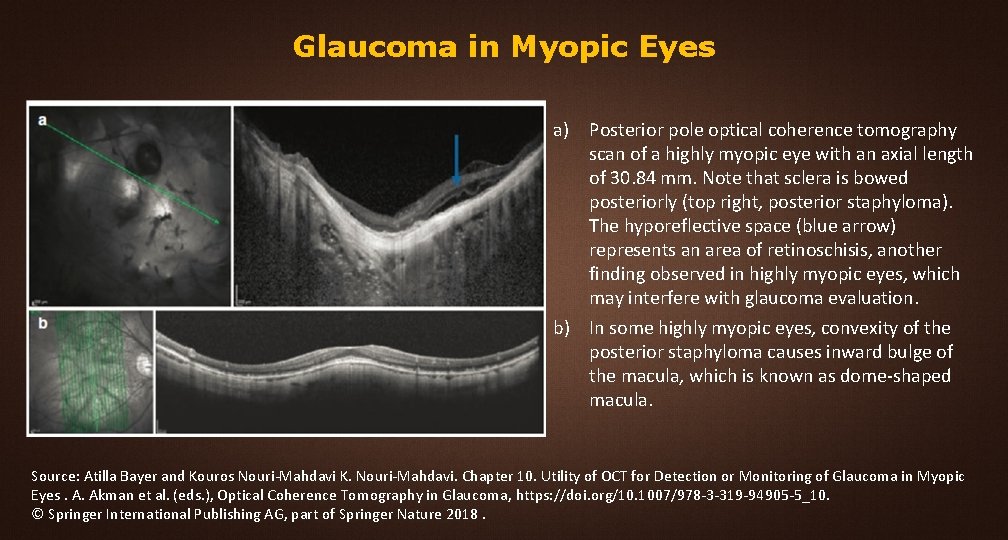
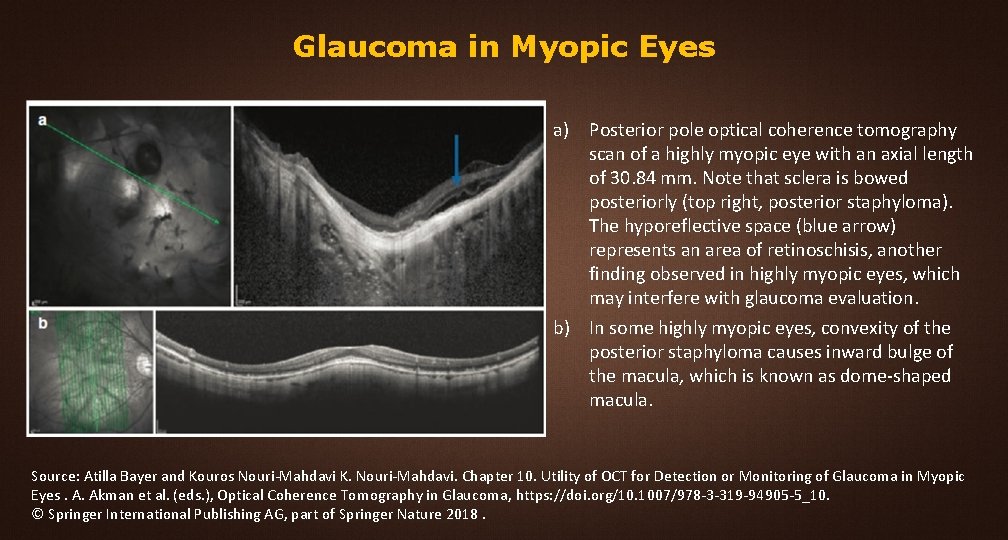
Glaucoma in Myopic Eyes a) Posterior pole optical coherence tomography scan of a highly myopic eye with an axial length of 30. 84 mm. Note that sclera is bowed posteriorly (top right, posterior staphyloma). The hyporeflective space (blue arrow) represents an area of retinoschisis, another finding observed in highly myopic eyes, which may interfere with glaucoma evaluation. b) In some highly myopic eyes, convexity of the posterior staphyloma causes inward bulge of the macula, which is known as dome-shaped macula. Source: Atilla Bayer and Kouros Nouri-Mahdavi K. Nouri-Mahdavi. Chapter 10. Utility of OCT for Detection or Monitoring of Glaucoma in Myopic Eyes. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_10. © Springer International Publishing AG, part of Springer Nature 2018.
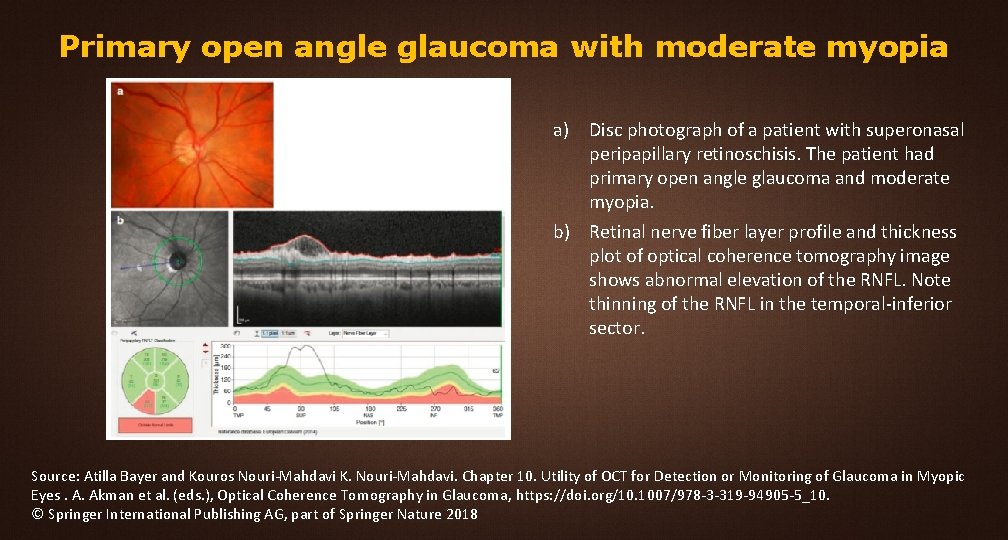
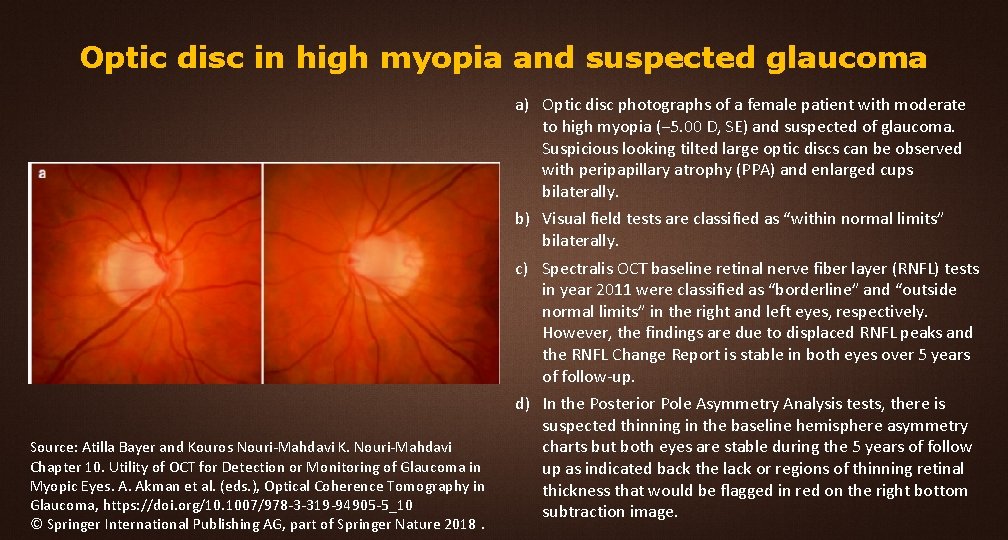
Primary open angle glaucoma with moderate myopia a) Disc photograph of a patient with superonasal peripapillary retinoschisis. The patient had primary open angle glaucoma and moderate myopia. b) Retinal nerve fiber layer profile and thickness plot of optical coherence tomography image shows abnormal elevation of the RNFL. Note thinning of the RNFL in the temporal-inferior sector. Source: Atilla Bayer and Kouros Nouri-Mahdavi K. Nouri-Mahdavi. Chapter 10. Utility of OCT for Detection or Monitoring of Glaucoma in Myopic Eyes. A. Akman et al. (eds. ), Optical Coherence Tomography in Glaucoma, https: //doi. org/10. 1007/978 -3 -319 -94905 -5_10. © Springer International Publishing AG, part of Springer Nature 2018