Clinical Pearls for Finals TOPIC 1 NEUROLOGY CASES
- Slides: 29
Clinical Pearls for Finals TOPIC 1: NEUROLOGY CASES
Welcome What this IS • A revision tool for OSCEs/PACES • A safe space to practice presenting cases • Creating a link between the preclinical / clinical
Disclaimer What this IS NOT • An exhaustive overview of all neurology for finals • A debrief on exam practicalities (variation across medical schools)
Overview • Typical examinations of 1. Parkinson’s disease 2. MND 3. Upper motor neurone – cerebral palsy and stroke 4. Cerebellar syndrome 5. Myasthenia gravis
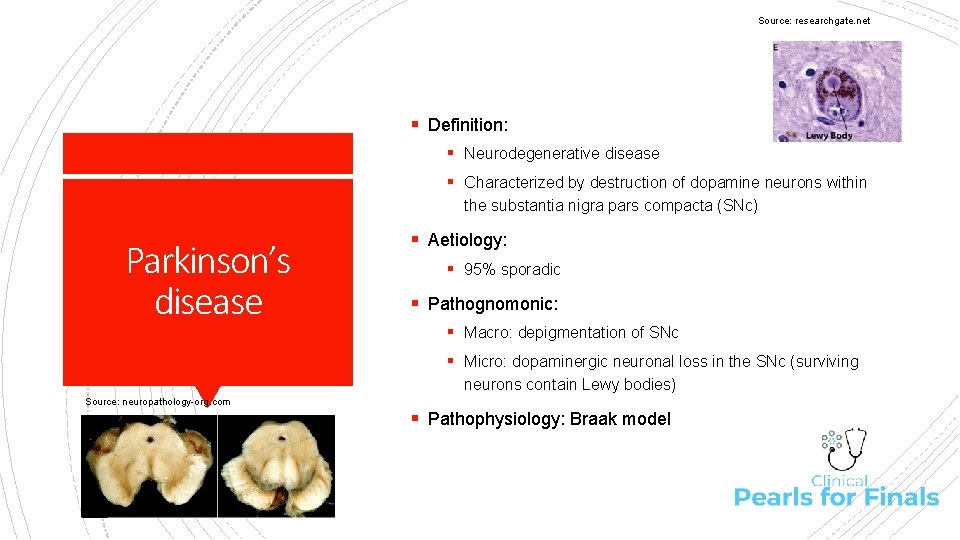
Source: researchgate. net § Definition: § Neurodegenerative disease § Characterized by destruction of dopamine neurons within the substantia nigra pars compacta (SNc) Parkinson’s disease § Aetiology: § 95% sporadic § Pathognomonic: § Macro: depigmentation of SNc § Micro: dopaminergic neuronal loss in the SNc (surviving neurons contain Lewy bodies) Source: neuropathology-org. com § Pathophysiology: Braak model
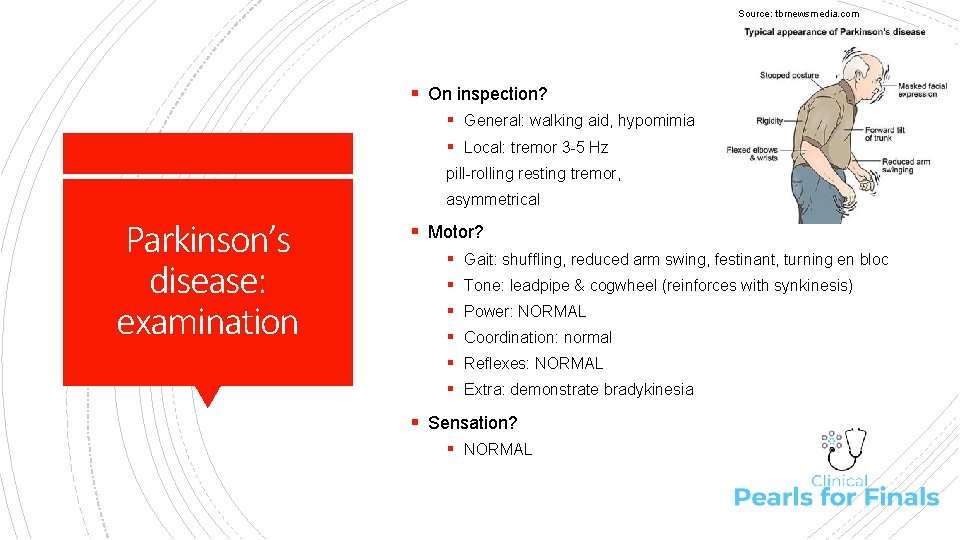
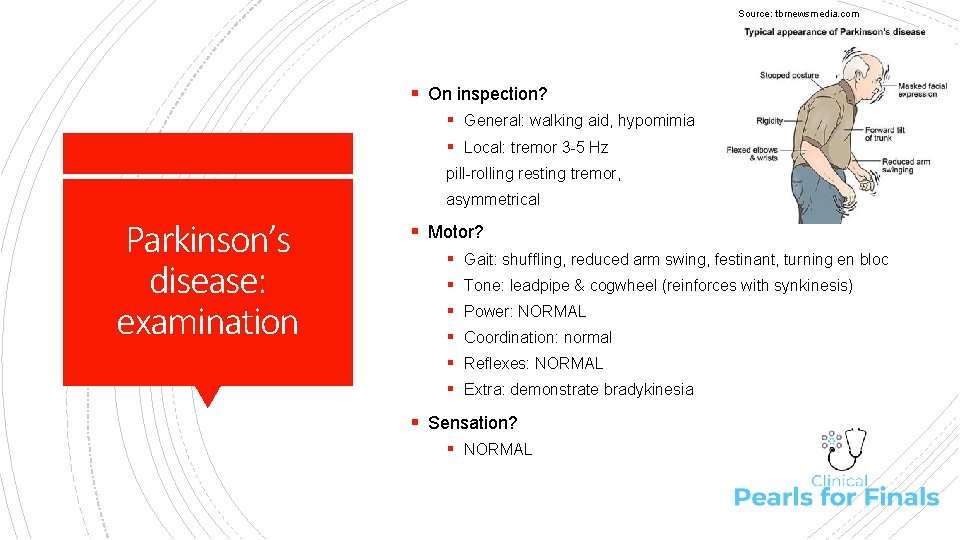
Source: tbrnewsmedia. com § On inspection? § General: walking aid, hypomimia § Local: tremor 3 -5 Hz pill-rolling resting tremor, asymmetrical Parkinson’s disease: examination § Motor? § § § Gait: shuffling, reduced arm swing, festinant, turning en bloc Tone: leadpipe & cogwheel (reinforces with synkinesis) Power: NORMAL Coordination: normal Reflexes: NORMAL Extra: demonstrate bradykinesia § Sensation? § NORMAL
§ Introduction blurb § “General inspection hypomimia, reduced spontaneous movement” § Headline § “Cardinal motor features of Parkinsonism” § Unpick Parkinson’s disease: presenting your findings § § Tremor… describe it Rigidity: leadpipe @ elbow, cogwheel @ wrist Akinesia/bradykinesia Postural instability/gait § Important negatives: power + reflexes normal § Differentials: … § Functional impairment: mobilises with walking stick § To complete? § § Eye movements Lying & standing BP AMTS Drug chart
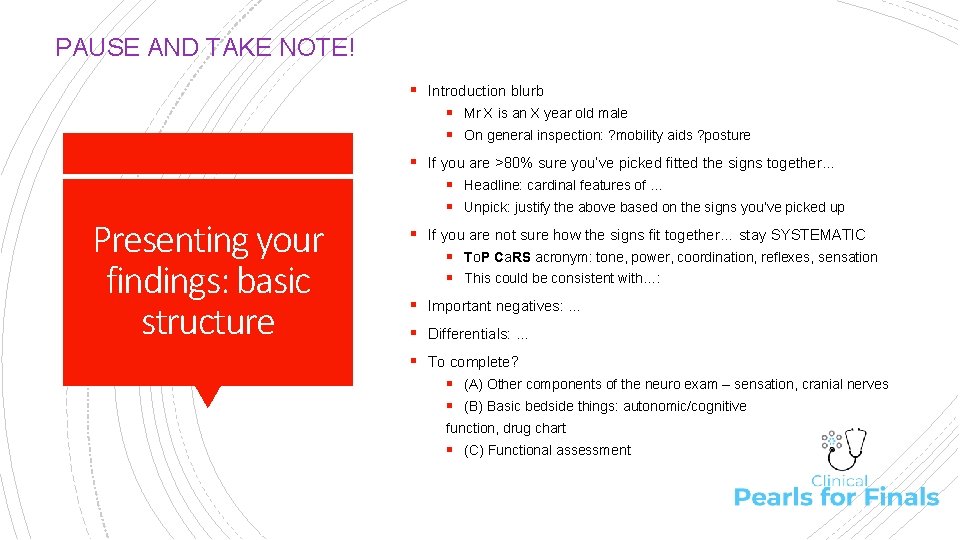
PAUSE AND TAKE NOTE! § Introduction blurb § Mr X is an X year old male § On general inspection: ? mobility aids ? posture § If you are >80% sure you’ve picked fitted the signs together… Presenting your findings: basic structure § Headline: cardinal features of … § Unpick: justify the above based on the signs you’ve picked up § If you are not sure how the signs fit together… stay SYSTEMATIC § To. P Ca. RS acronym: tone, power, coordination, reflexes, sensation § This could be consistent with…: § Important negatives: … § Differentials: … § To complete? § (A) Other components of the neuro exam – sensation, cranial nerves § (B) Basic bedside things: autonomic/cognitive function, drug chart § (C) Functional assessment
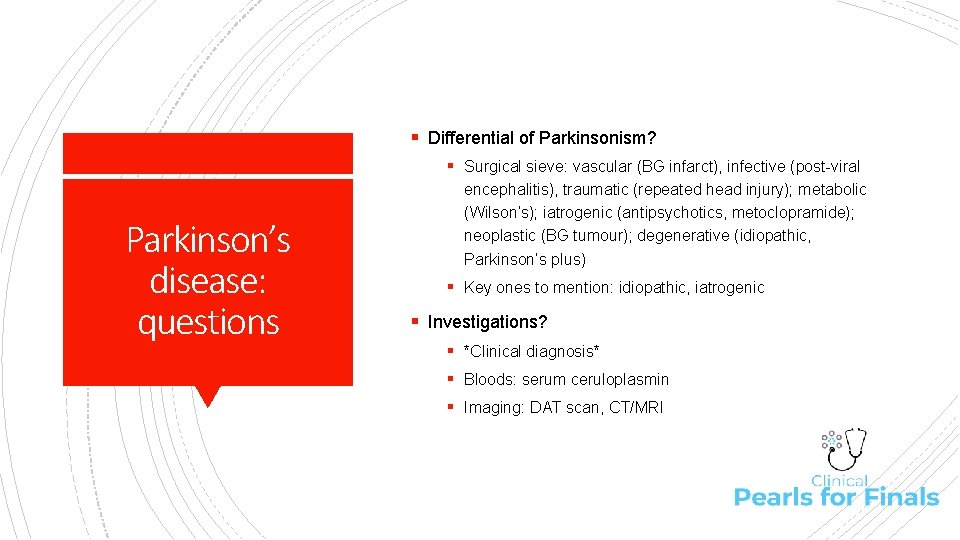
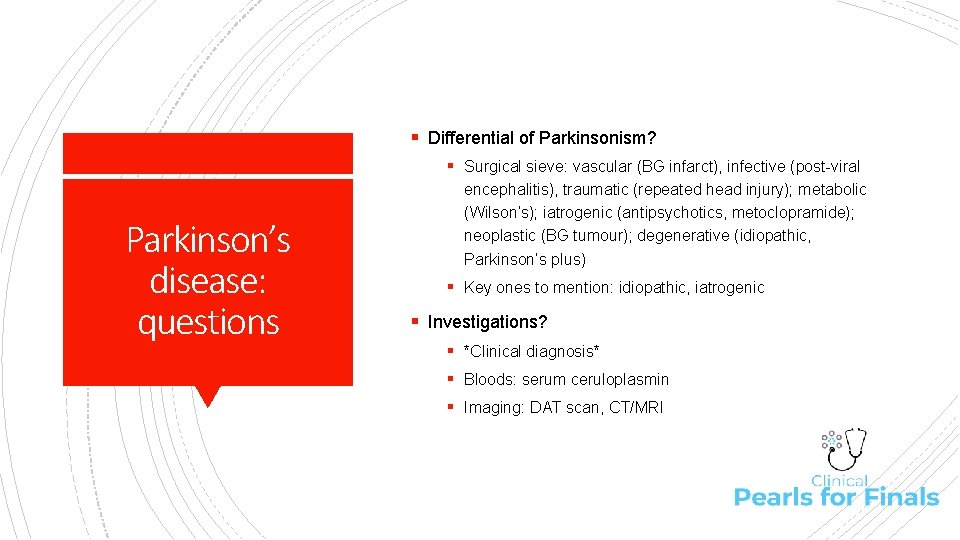
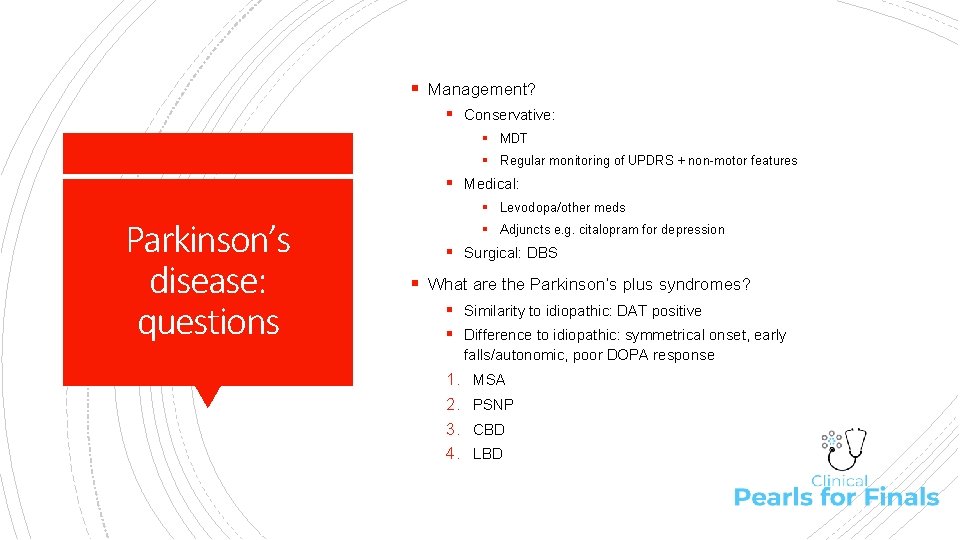
§ Differential of Parkinsonism? § Surgical sieve: vascular (BG infarct), infective (post-viral Parkinson’s disease: questions encephalitis), traumatic (repeated head injury); metabolic (Wilson’s); iatrogenic (antipsychotics, metoclopramide); neoplastic (BG tumour); degenerative (idiopathic, Parkinson’s plus) § Key ones to mention: idiopathic, iatrogenic § Investigations? § *Clinical diagnosis* § Bloods: serum ceruloplasmin § Imaging: DAT scan, CT/MRI
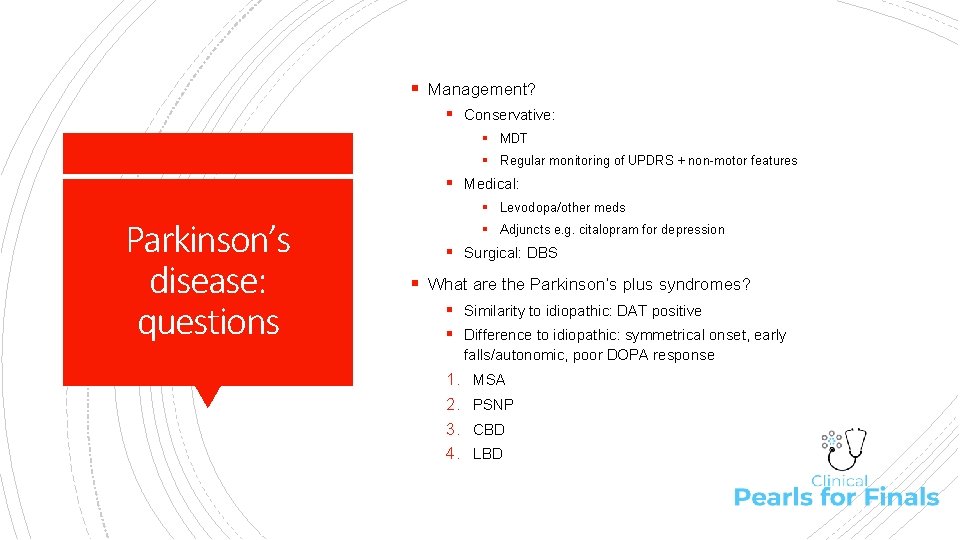
§ Management? § Conservative: § MDT § Regular monitoring of UPDRS + non-motor features § Medical: Parkinson’s disease: questions § Levodopa/other meds § Adjuncts e. g. citalopram for depression § Surgical: DBS § What are the Parkinson’s plus syndromes? § Similarity to idiopathic: DAT positive § Difference to idiopathic: symmetrical onset, early falls/autonomic, poor DOPA response 1. 2. 3. 4. MSA PSNP CBD LBD
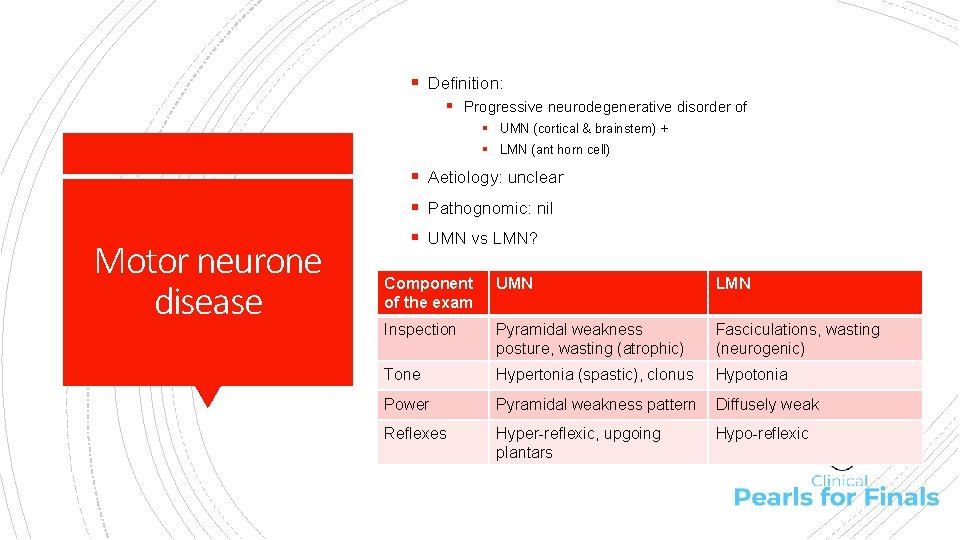
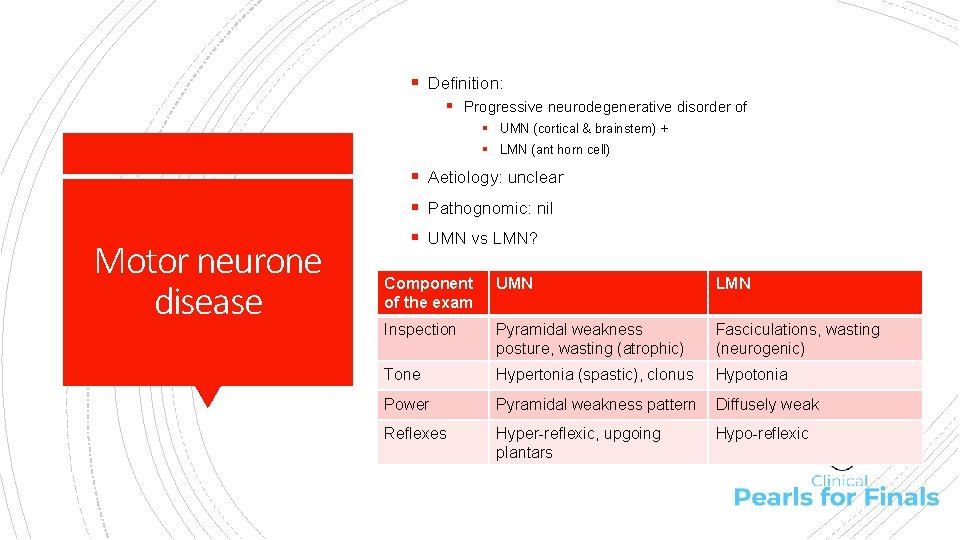
§ Definition: § Progressive neurodegenerative disorder of § UMN (cortical & brainstem) + § LMN (ant horn cell) § Aetiology: unclear § Pathognomic: nil Motor neurone disease § UMN vs LMN? Component of the exam UMN LMN Inspection Pyramidal weakness posture, wasting (atrophic) Fasciculations, wasting (neurogenic) Tone Hypertonia (spastic), clonus Hypotonia Power Pyramidal weakness pattern Diffusely weak Reflexes Hyper-reflexic, upgoing plantars Hypo-reflexic
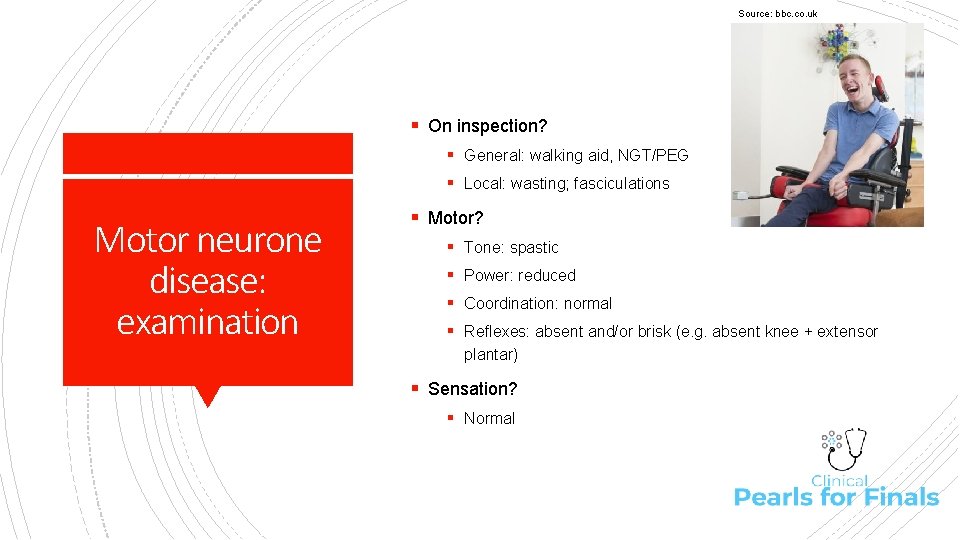
Source: bbc. co. uk § On inspection? § General: walking aid, NGT/PEG § Local: wasting; fasciculations Motor neurone disease: examination § Motor? § Tone: spastic § Power: reduced § Coordination: normal § Reflexes: absent and/or brisk (e. g. absent knee + extensor plantar) § Sensation? § Normal
§ Headline § “There is evidence of both UMN and LMN pathology” § Unpick… for example § “Features consistent with UMN pathology include: spastic gait; Motor neurone disease: presenting your findings spastic weakness in the lower limbs with hypertonia and reduced power particularly in the flexor compartment; brisk reflexes at the knees; and extensor plantar responses bilaterally” § “Features consistent with LMN pathology include: wasting of the distal muscles, particularly at thenar eminence; fasciculations in the forearm muscles; flaccid muscle weakness in the upper limbs with hypotonia and reduced power; hyporeflexia in the upper limbs” § Important negatives: sensation normal § This could be consistent with: MND, differentials include… § Functional impairment: mobilises in wheelchair § To complete? Bulbar function, eye movements, functional
§ Differential? § M: MND § A: Ataxia (Friedrich’s) § S: SADC Motor neurone disease: questions § T: tabes dorsalis § Investigations? § *Clinical diagnosis* § Bloods: normal § Imaging of brain + cord: exclude structural cause § Special: LP (to exclude inflammatory causes), NCS (to exclude a motor neuropathy)/EMG (widespread denervation)
§ Management? § Conservative: MDT § Medical: § Disease-modifying: riluzole Motor neurone disease: questions § Supportive: physio, baclofen, NIV, thick foods/NGT/PEG § Complications? § Neurobehavioural § Dysphagia § Immobility § Muscular § Prognosis? § Mean survival 3 years § Poor indicators: elderly, female, bulbar
Source: forest-farm. org § On inspection? § General: walking aid § Local: limb position, atrophy, contracture Upper motor neurone: examination § Gait? § Unilateral: circumducting § Bilateral: scissoring § Motor? § Tone: spasticity, clonus § Power: pyramidal weakness § Reflexes: hyper-reflexic, extensor plantars
§ Headline § “Cardinal features of unilateral UMN lesion on RHS” § Unpick Upper motor neurone: presenting your findings § Spastic hypertonia, clonus § Pyramidal weakness patters – LL extensors stronger than extensors § Hyper-reflexia, extensor plantars § Findings could be consistent with: offer differentials § Functional impairment? § To complete? Sensation (? sensory level), DRE (? antal tone), cranial nerves & speech (? aphasia)
§ Differential? § Bilateral lower limbs (spastic paraparesis): hemisphere (CP, MS) cord (prolapse, vertebral #, malignancy, infection, trauma) § Unilateral lower limbs (spastic hemiparesis): hemisphere Upper motor neurone: questions (stroke, MS, SOL, CP) vs hemicord (MS, cord compression) § What is cerebral palsy? § A group of conditions characterized by a disorder of movement and posture, resulting from a non-progressive lesion of the motor pathways in the developing brain § What are the causes of cerebral palsy? § Antenatal: cerebral malformation, congenital infection § Intrapartum: asphyxia, trauma § Postnatal: head injury, infection, metabolic insults
§ Classification of cerebral palsy? § Spastic (70%) § Ataxic (10%) Upper motor neurone: questions § Dyskinetic (10%) § Mixed (10%) § Management of cerebral palsy? § Supportive: § MDT § Medical: baclofen, botox, AEDs § ? Surgical: dorsal rhizotomy
Source: mssociety. org. uk § On inspection? § General: walking aid § Motor: upper limbs Cerebellar syndrome: examination § Tone: hypotonia § Coordination: dysdiadochokinesis, intention tremor, dysmetria § Extra: cerebellar rebound § Motor: lower limbs § Tone: hypotonia § Coordination: impaired heel-shin § Reflexes: knee jerk pendular § Gait: ataxic, unable to heel-toe, Romberg -ve
§ Introduction blurb § “General inspection evidence of walking aid” § Headline § “Cardinal features of cerebellar syndrome” Cerebellar syndrome : presenting your findings § Unpick § DANISH § Cerebellar vermis: truncal >> limb § Cerebellar hemisphere: limb § Important negatives: Romberg’s negative (excludes a proprioceptive deficit) § Differentials: § To complete? § Cranial nerves, speech § Fundoscopy § Drug chart
§ Differential? § Sieve: vascular (BS stroke); inflammatory (MS); traumatic; Cerebellar syndrome: questions toxins (alcohol); iatrogenic (phenytoin); neoplastic (schwannoma/CPA lesion); congenital (Friedrich’s, VHL); degenerative (MSA) § Key to mention: MS, alcohol, SOL, phenytoin § Classification of MS? § Relapsing-remitting § Secondary progressive § Primary progressive § Fulminant
§ Investigations in MS work-up? § § Cerebellar syndrome : questions Diagnosis according to Mc. Donald’s criteria Bloods: anti-MBP, NMO-Ig. G (Devic’s) Imaging: MRI Special tests: LP (CSF oligoclonal bands), SEP § Management of MS? § Supportive: MDT § Medical: acute vs. long-term § Disease-modifying e. g. IFN-beta, glatiramer, natalizumab § Symptomatic: for pain e. g. gabapentin, for spasticity e. g. baclofen, for bladder dysfunction e. g. oxybutynin § Surgical e. g. dorsal column stimulation § Prognostic factors in MS? § GOOD: female, <25, sensory features at onset, few MRI lesions
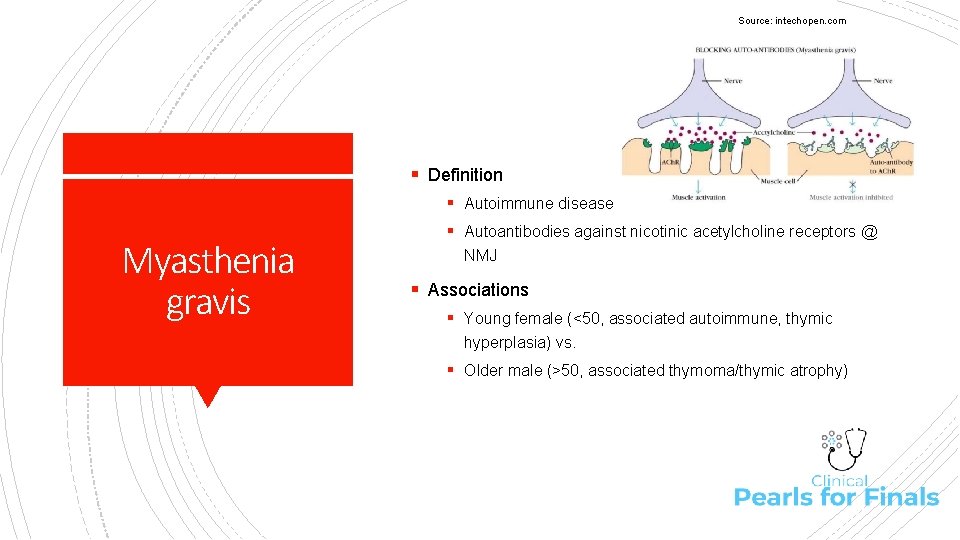
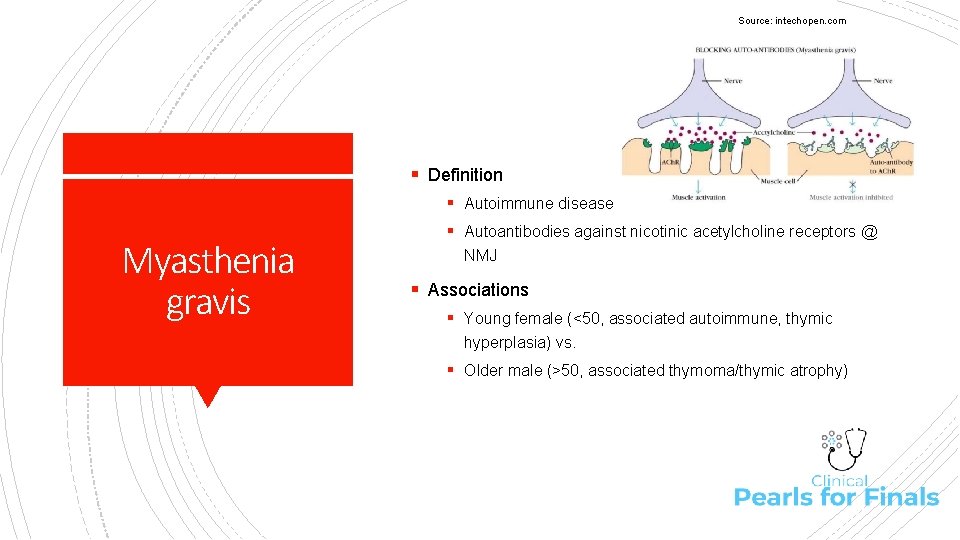
Source: intechopen. com § Definition § Autoimmune disease Myasthenia gravis § Autoantibodies against nicotinic acetylcholine receptors @ NMJ § Associations § Young female (<50, associated autoimmune, thymic hyperplasia) vs. § Older male (>50, associated thymoma/thymic atrophy)
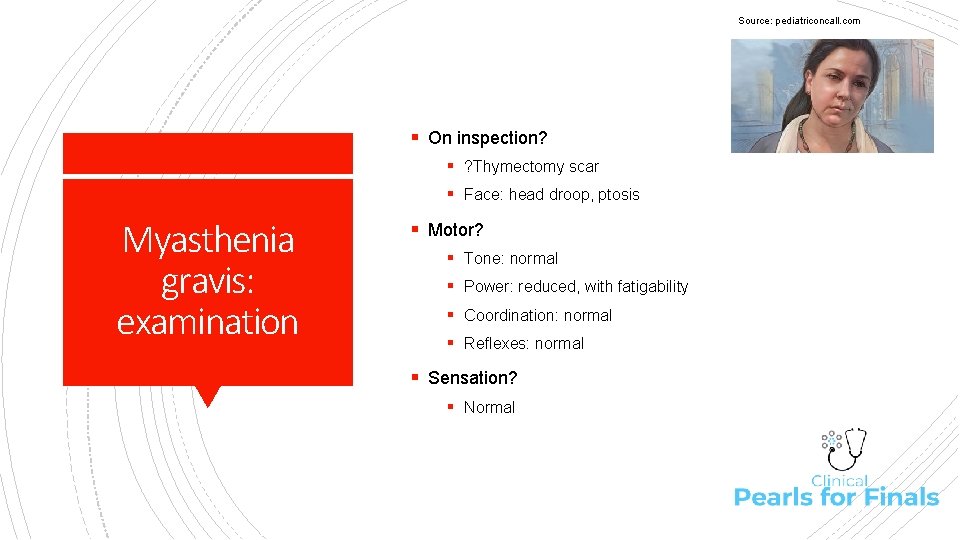
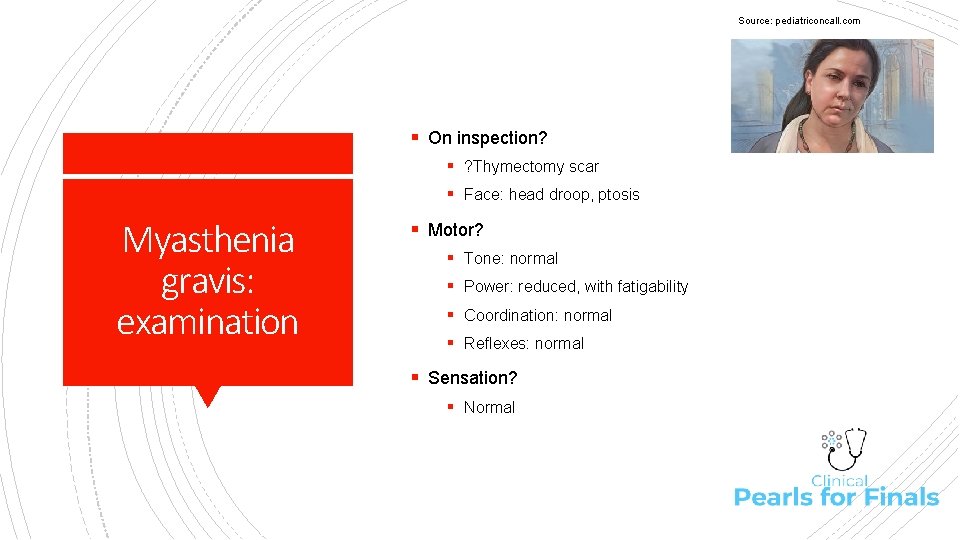
Source: pediatriconcall. com § On inspection? § ? Thymectomy scar § Face: head droop, ptosis Myasthenia gravis: examination § Motor? § Tone: normal § Power: reduced, with fatigability § Coordination: normal § Reflexes: normal § Sensation? § Normal
§ Headline § “Features of dysfunction at NMJ” § Key features § Weakness with fatigability in upper limbs § Ptosis with fatigability Myasthenia gravis: presenting your findings § Nasal speech with fatigability § Important negatives § Normal tone, coordination, reflexes, sensation § Differentials: § To complete? § Cranial nerves: complex ophthalmoplegia, ptosis with fatiguability § Speech: nasal speech with fatigability, dysphagia
§ Investigations? § Suggestive: Myasthenia gravis: questions § Bloods (ACh. R antibody, antistriated muscle antibody) § Respiratory function (lung function tests) § Diagnostic: § Tensilon test (IV endrophonium = rapid transient improvement) § EMG (repetitive stimulation = decrement in muscle AP) § Associations: § TFT (association with Graves’) § CT mediastinum (? thymoma)
§ Management? § Supportive: MDT § Medical: acute (IVIG/plasmapheresis) vs chronic (cholinesterase inhibitors e. g. neostigmine) Myasthenia gravis: questions § Surgical: thymectomy § What is LEMS and how would you differentiate it from myasthenia gravis? § LEMS: antibodies to pre-synaptic VGCC § Causes: paraneoplastic (SCLC), autoimmune § LMES: Leg weakness early, Extra features (autonomic, areflexia), Movement improves symptoms, Small response to endrophonium
Thanks for listening! Any questions? Please give feedback: https: //forms. gle/4 Hs. Ja. Xe. G 13 Uzt. Boy 5 Feel free to email me: m. jensen@cantab. net