Clinical Management of Airborne Hazards What Providers Need
Clinical Management of Airborne Hazards What Providers Need to Know Omowunmi Osinubi, MD Anays Sotolongo, MD
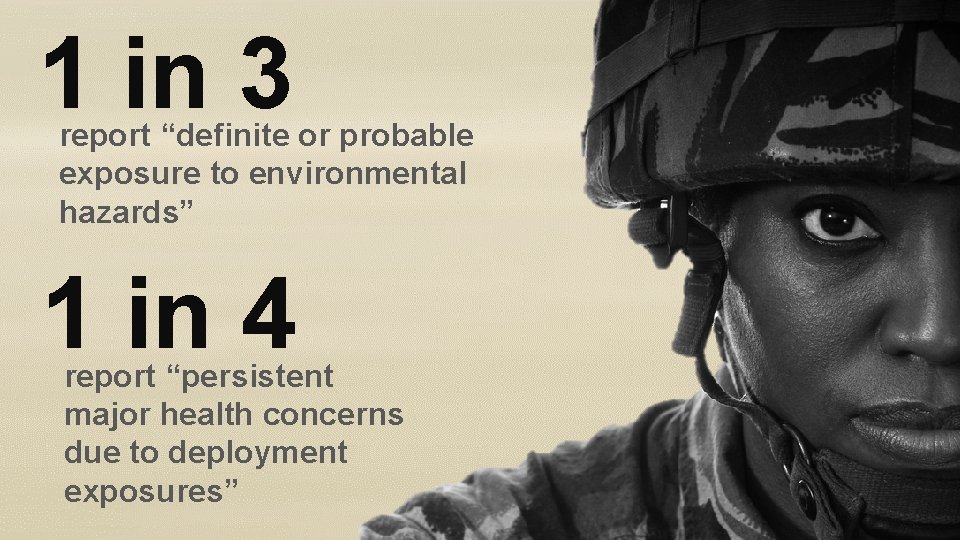
1 in 3 report “definite or probable exposure to environmental hazards” 1 in 4 report “persistent major health concerns due to deployment exposures”

Airborne Hazards & Post Deployment Health Burn Pit Smoke Sand Dust Oil Well Fires
IOM Report 2011 “…service in Iraq or Afghanistan –– might be associated with long-term health effects, in highly exposed. . or susceptible populations. . . ”

Airborne Hazards & Open Burn Pit Registry Public Law 112 -260 Monitor and ascertain health effects from exposures Monitor the health care of Veterans with concerns Provide high quality health services
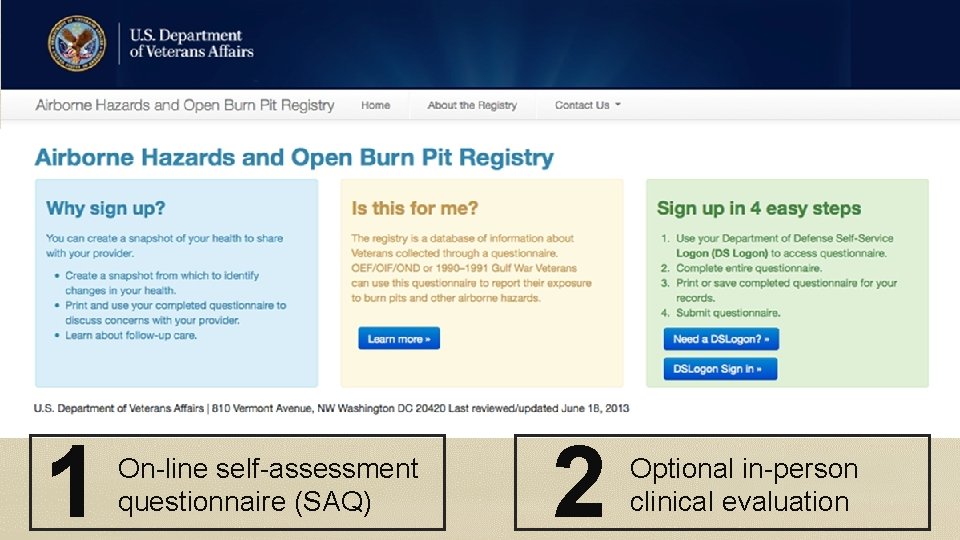
1 On-line self-assessment questionnaire (SAQ) 2 Optional in-person clinical evaluation
Addressing Veterans’ Health Concerns at the Initial In-person Registry Evaluation • Veteran may discuss: – Upper/lower respiratory symptoms – Physical activity limitations or decreased ability to exercise – Other health conditions or concerns related to: • Gastrointestinal, neurocognitive, neuroendocrine, rheumatologic, musculoskeletal, reproductive health and cancer OR – Have no current health problems, but concerned about possible future health effects of exposures
Airborne Hazards Referral Case Study #1 48 Year Old OIF Veteran Non-Smoker
Clinical History • • • “Breathing problems” & “Hoarseness” Started in 2005 in Iraq Worsening over time Limiting work activities Diagnostic work-up to date (normal) • Spirometry, Chest x-ray, cardiac stress test/echo • Chest CT – “small hiatal hernia” • Trial of inhalers – “Not helpful” • Psychiatry - “Severe PTSD”
“I was at Balad, …. I was next to the burn pit…. . I breathed in the smoke, now I can’t breathe! “VA Burn-pit Registry”
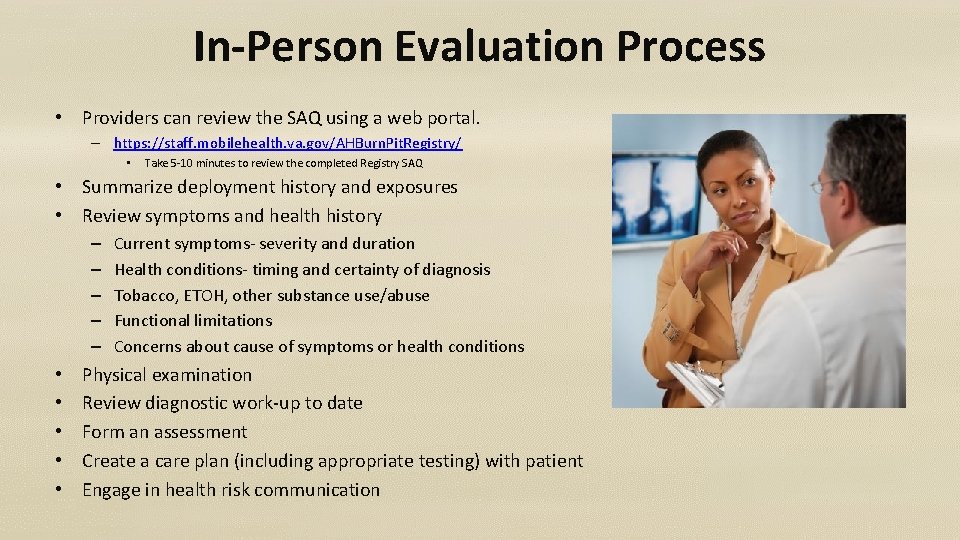
In-Person Evaluation Process • Providers can review the SAQ using a web portal. – https: //staff. mobilehealth. va. gov/AHBurn. Pit. Registry/ • Take 5 -10 minutes to review the completed Registry SAQ • Summarize deployment history and exposures • Review symptoms and health history – – – • • • Current symptoms- severity and duration Health conditions- timing and certainty of diagnosis Tobacco, ETOH, other substance use/abuse Functional limitations Concerns about cause of symptoms or health conditions Physical examination Review diagnostic work-up to date Form an assessment Create a care plan (including appropriate testing) with patient Engage in health risk communication
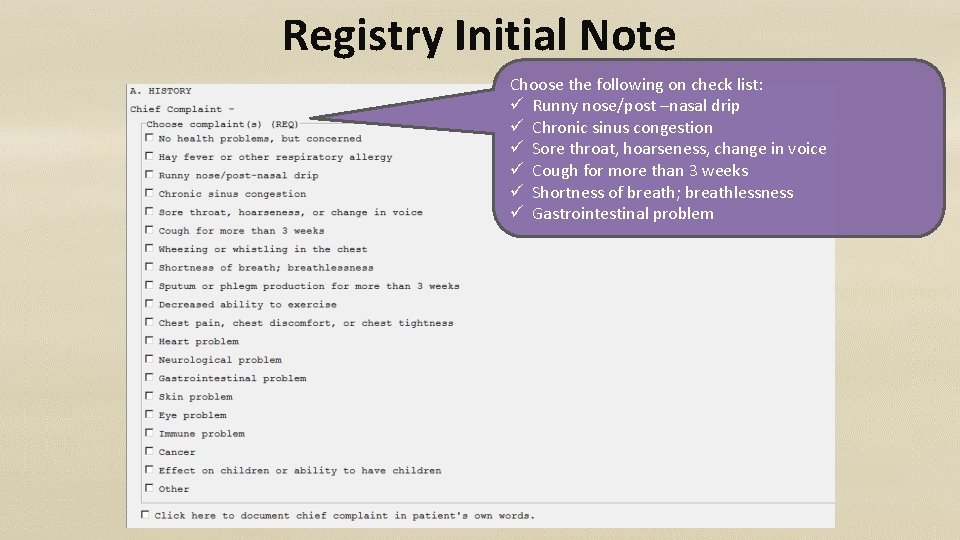
Registry Initial Note Choose the following on check list: ü Runny nose/post –nasal drip ü Chronic sinus congestion ü Sore throat, hoarseness, change in voice ü Cough for more than 3 weeks ü Shortness of breath; breathlessness ü Gastrointestinal problem

Exposure History • Military Exposures – Military occupation specialty – Deployment-related exposures • Non Military Exposures – Civilian occupational exposures – Civilian non-occupational exposures

Military Exposure History Army Corps of Engineers (10 years) Ø Motor pool construction trucks o Diesel exhaust fumes o Construction dusts

Military Exposure History Deployment-related exposures (1/04 -6/05) Ø Kuwait: “monster sand dust storms” Ø Iraq: “Balad burn pit- burned 24/7” Ø Sick often – “Iraqi crud”

Works in waste management Civilian Exposures Ø Grain dusts Ø Temperature extremes (-40 to 100+ degree F) Ø Heavy physical job demand (> 50 Ibs frequently) Non-vocational exposures/social history Ø Non-significant
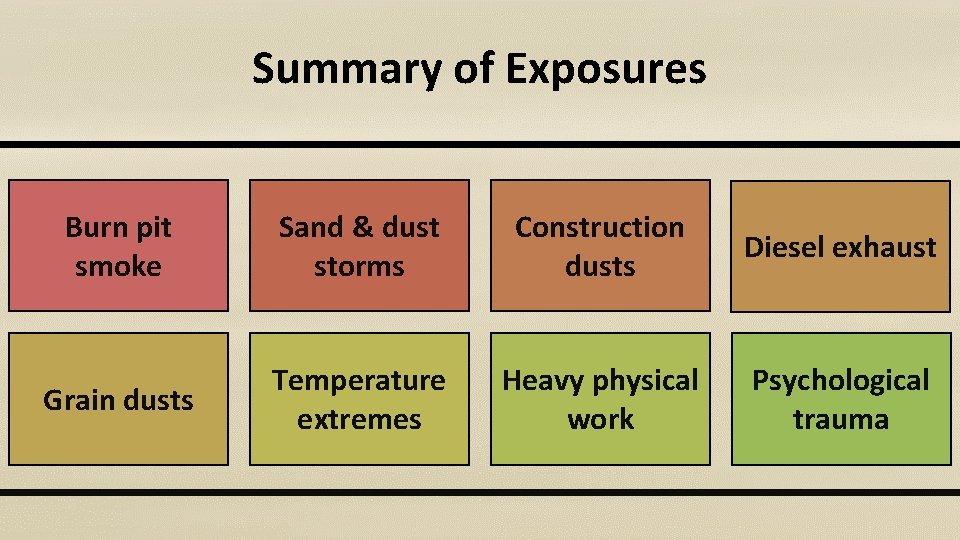
Summary of Exposures Burn pit smoke Sand & dust storms Construction dusts Diesel exhaust Grain dusts Temperature extremes Heavy physical work Psychological trauma
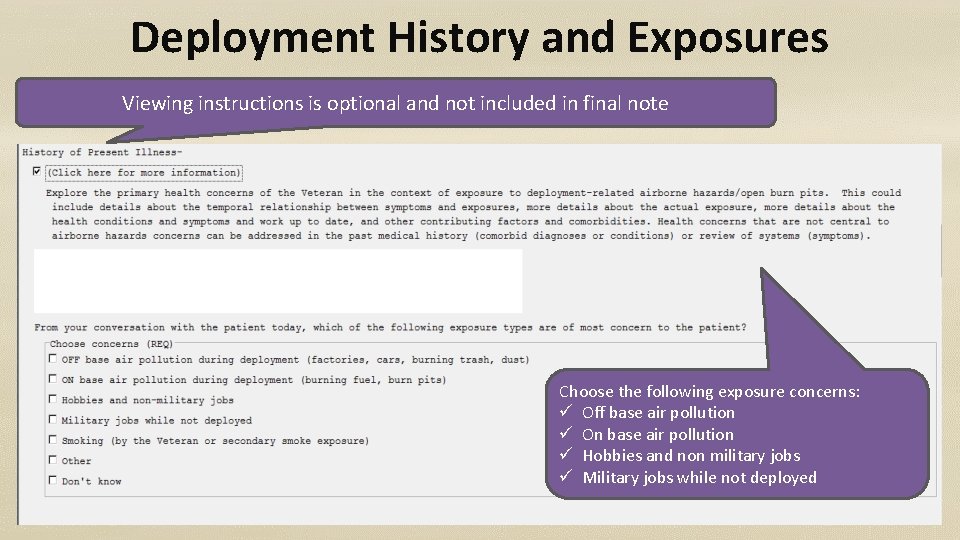
Deployment History and Exposures Viewing instructions is optional and not included in final note Choose the following exposure concerns: ü Off base air pollution ü On base air pollution ü Hobbies and non military jobs ü Military jobs while not deployed
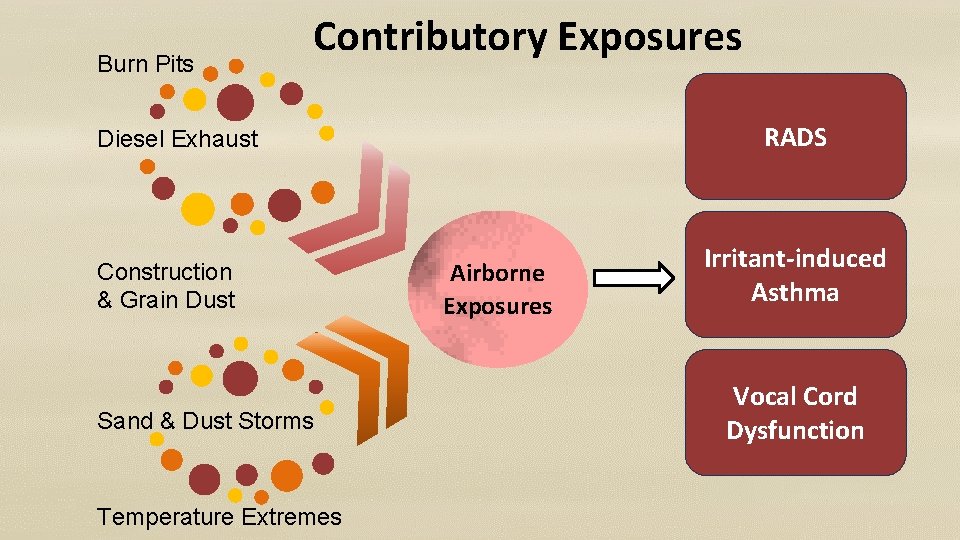
Burn Pits Contributory Exposures RADS Diesel Exhaust Construction & Grain Dust Sand & Dust Storms Temperature Extremes Airborne Exposures Irritant-induced Asthma Vocal Cord Dysfunction

Diagnostic Work-Up Work up: Diseases: • Cardiac Stress Test • Echocardiography o Cardiovascular dz • Spirometry • Imaging Studies o Obstructive Lung dz o Interstitial Lung dz • Inhaler Ineffectiveness o ? Vocal Cord Dysfunction
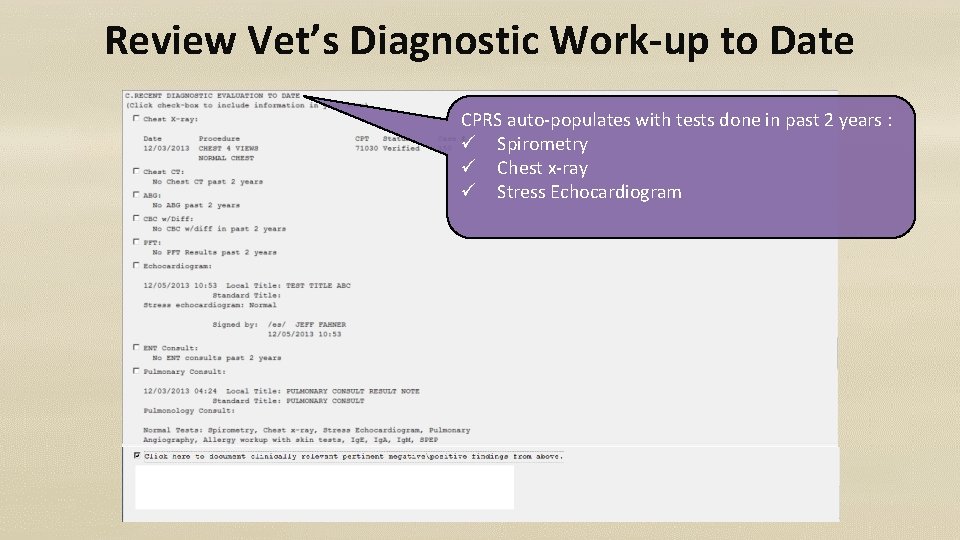
Review Vet’s Diagnostic Work-up to Date CPRS auto-populates with tests done in past 2 years : ü Spirometry ü Chest x-ray ü Stress Echocardiogram
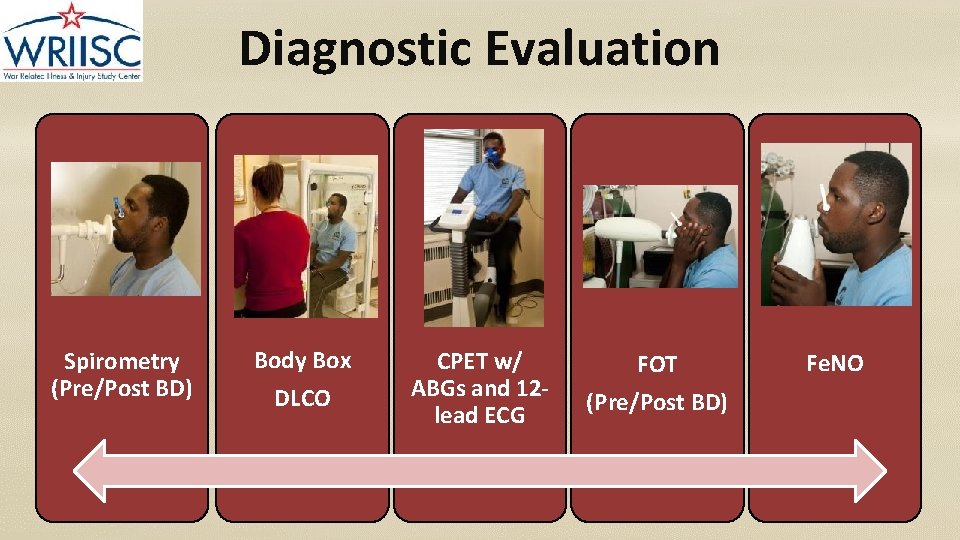
Diagnostic Evaluation Spirometry (Pre/Post BD) Body Box DLCO CPET w/ ABGs and 12 lead ECG FOT (Pre/Post BD) Fe. NO
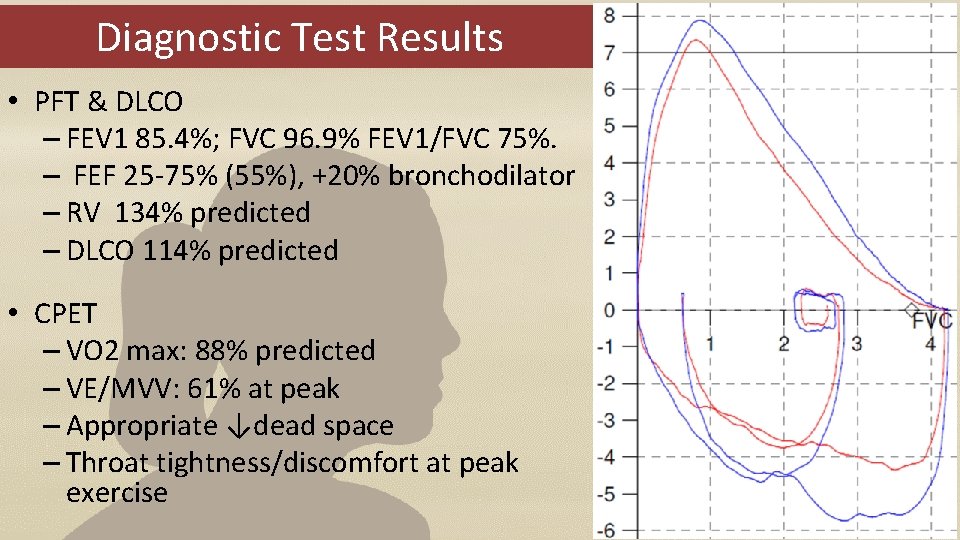
Diagnostic Test Results • PFT & DLCO – FEV 1 85. 4%; FVC 96. 9% FEV 1/FVC 75%. – FEF 25 -75% (55%), +20% bronchodilator – RV 134% predicted – DLCO 114% predicted • CPET – VO 2 max: 88% predicted – VE/MVV: 61% at peak – Appropriate ↓dead space – Throat tightness/discomfort at peak exercise
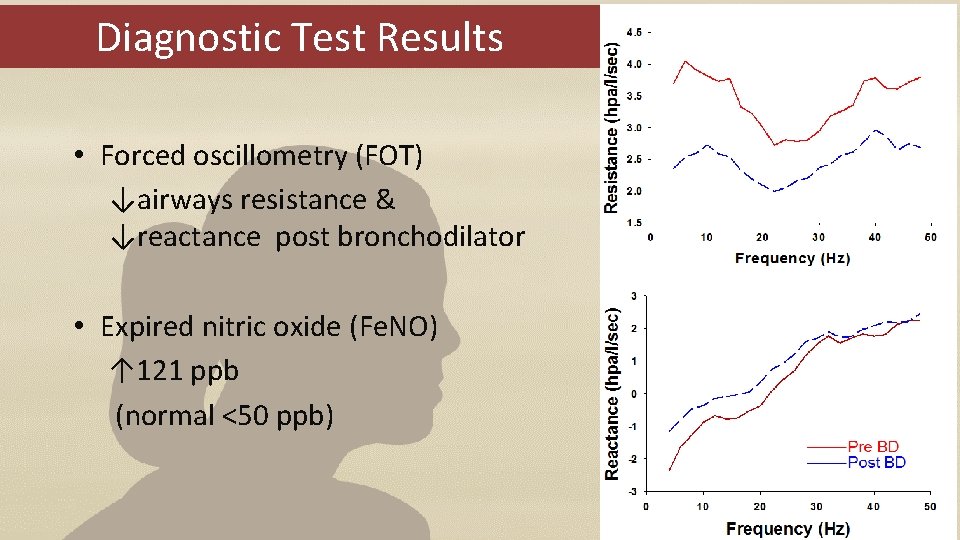
Diagnostic Test Results • Forced oscillometry (FOT) ↓airways resistance & ↓reactance post bronchodilator • Expired nitric oxide (Fe. NO) ↑ 121 ppb (normal <50 ppb)
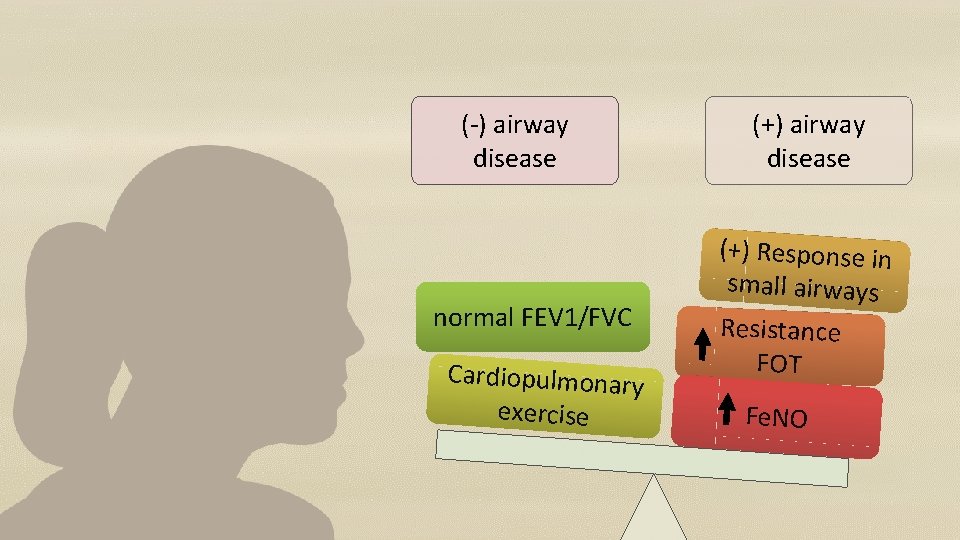
(-) airway disease normal FEV 1/FVC Cardiopulmonary exercise (+) airway disease (+) Response in small airways Resistance FOT Fe. NO
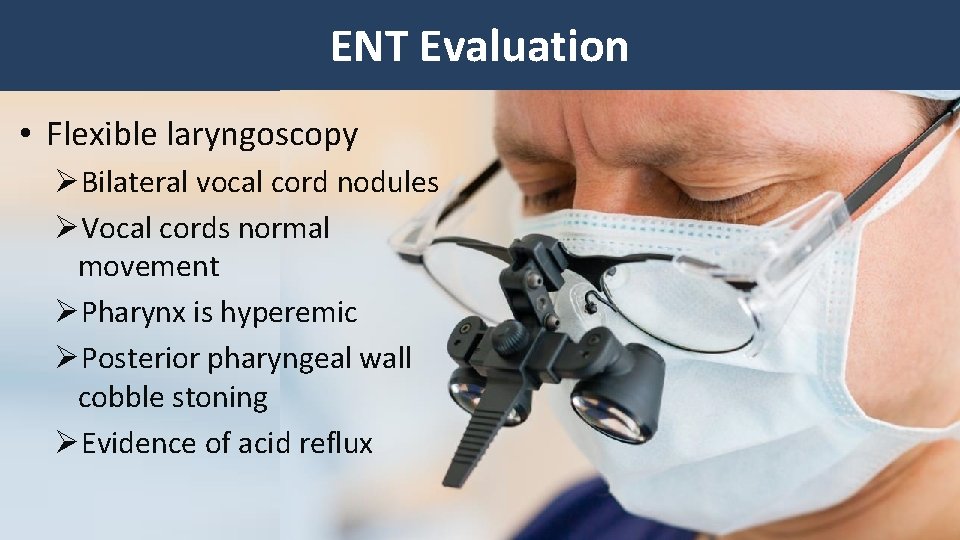
ENT Evaluation • Flexible laryngoscopy ØBilateral vocal cord nodules ØVocal cords normal movement ØPharynx is hyperemic ØPosterior pharyngeal wall cobble stoning ØEvidence of acid reflux
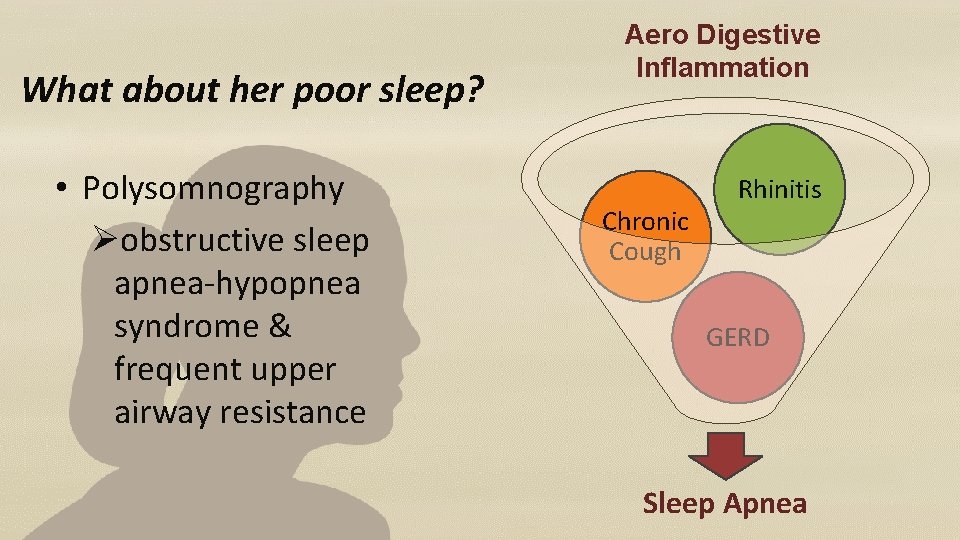
What about her poor sleep? • Polysomnography Øobstructive sleep apnea-hypopnea syndrome & frequent upper airway resistance Aero Digestive Inflammation Chronic Cough Rhinitis GERD Sleep Apnea
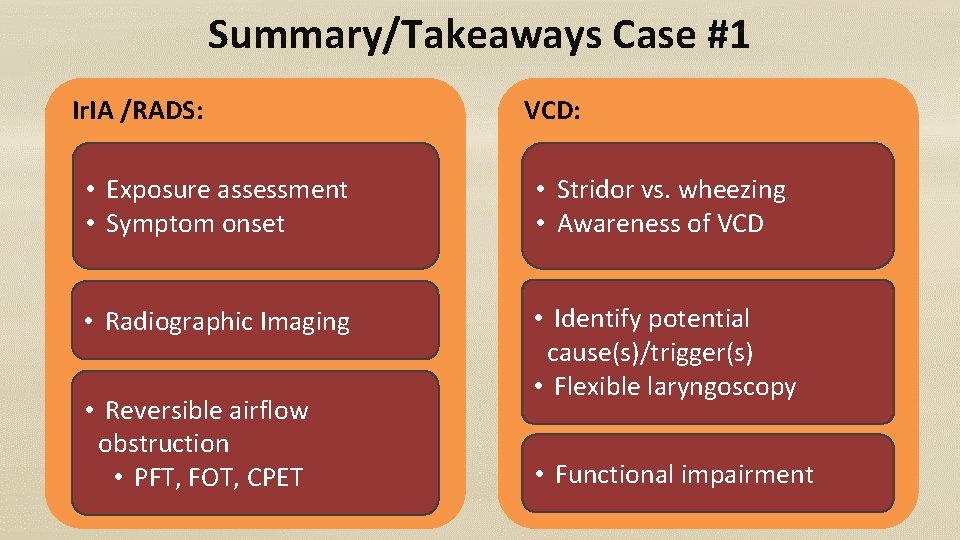
Summary/Takeaways Case #1 Ir. IA /RADS: VCD: • Exposure assessment • Symptom onset • Stridor vs. wheezing • Awareness of VCD • Radiographic Imaging • Identify potential cause(s)/trigger(s) • Flexible laryngoscopy • Reversible airflow obstruction • PFT, FOT, CPET • Functional impairment
Airborne Hazards Referral Case Study #2 31 year old OIF Marine Corps Veteran
Chief Concerns • Severe shortness of breath since Iraq • Decreased exercise capacity • Multiple episodes of acute respiratory distress

Military Exposure History ØCombat truck convoys ØSand dust storms

Military Exposure History Contd.
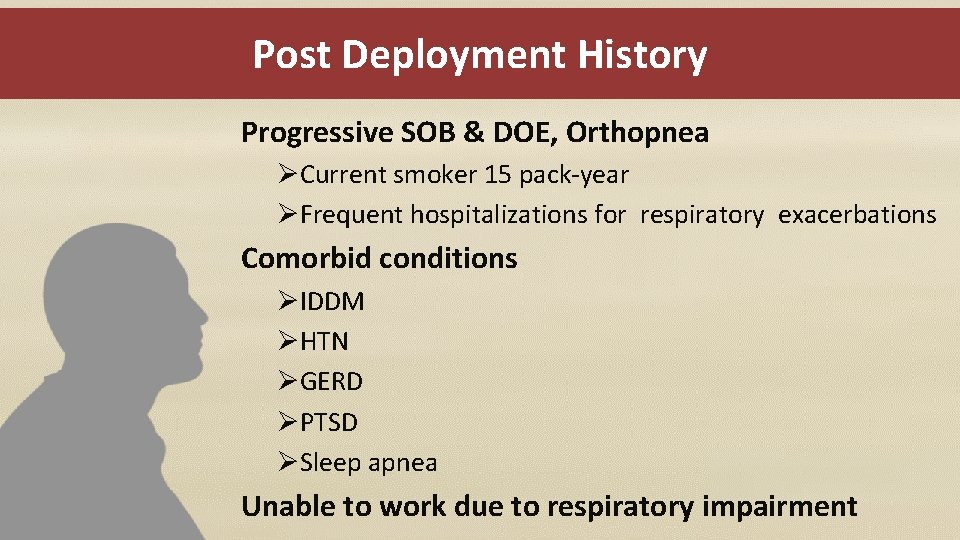
Post Deployment History Progressive SOB & DOE, Orthopnea ØCurrent smoker 15 pack-year ØFrequent hospitalizations for respiratory exacerbations Comorbid conditions ØIDDM ØHTN ØGERD ØPTSD ØSleep apnea Unable to work due to respiratory impairment
Airborne Hazard Concerns - Clinical Assessment • Physical exam & oxygen sat • Chest X-ray (PA and lateral) • Pulmonary function tests • Allergy consult • Cardiac evaluation - EKG, Echo, • Pulmonary consult
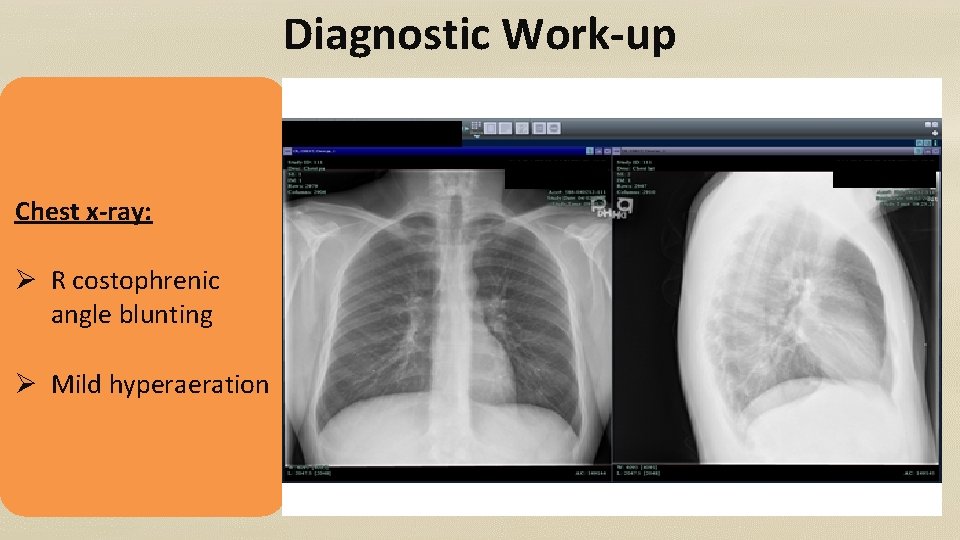
Diagnostic Work-up Chest x-ray: Ø R costophrenic angle blunting Ø Mild hyperaeration
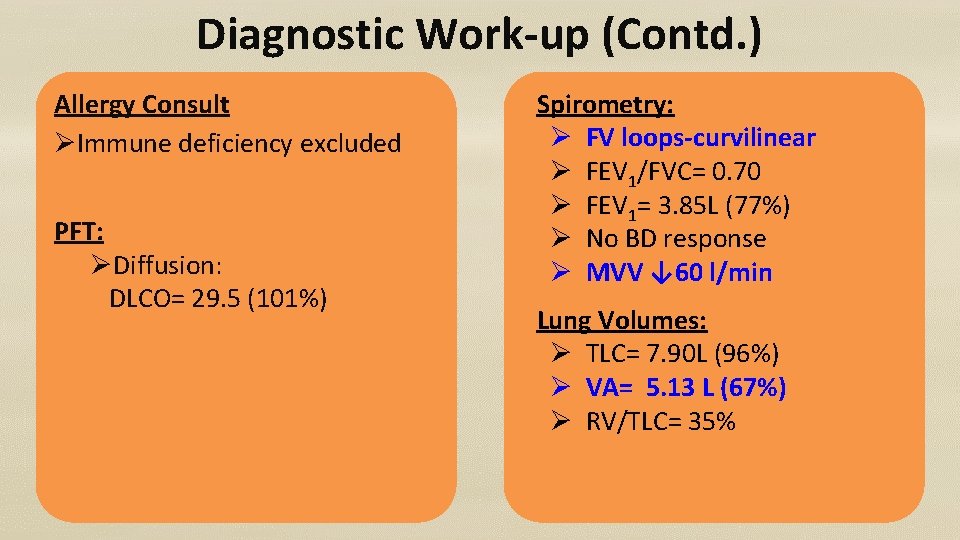
Diagnostic Work-up (Contd. ) Allergy Consult ØImmune deficiency excluded PFT: ØDiffusion: DLCO= 29. 5 (101%) Spirometry: Ø FV loops-curvilinear Ø FEV 1/FVC= 0. 70 Ø FEV 1= 3. 85 L (77%) Ø No BD response Ø MVV ↓ 60 l/min Lung Volumes: Ø TLC= 7. 90 L (96%) Ø VA= 5. 13 L (67%) Ø RV/TLC= 35%
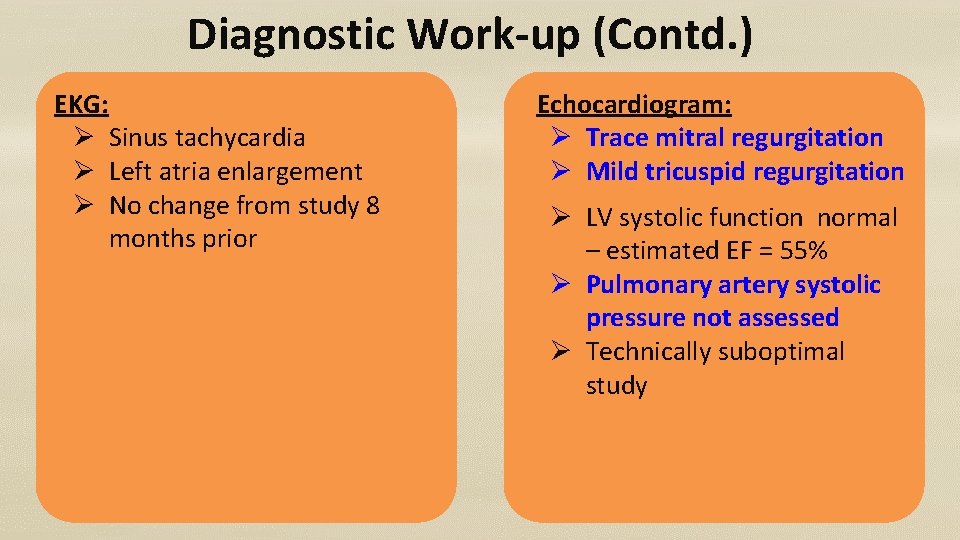
Diagnostic Work-up (Contd. ) EKG: Ø Sinus tachycardia Ø Left atria enlargement Ø No change from study 8 months prior Echocardiogram: Ø Trace mitral regurgitation Ø Mild tricuspid regurgitation Ø LV systolic function normal – estimated EF = 55% Ø Pulmonary artery systolic pressure not assessed Ø Technically suboptimal study
“It was when I was under the care of a pulmonologist. . . that my condition … received a more thorough workup” What types of additional work-up would be appropriate for this Veteran?
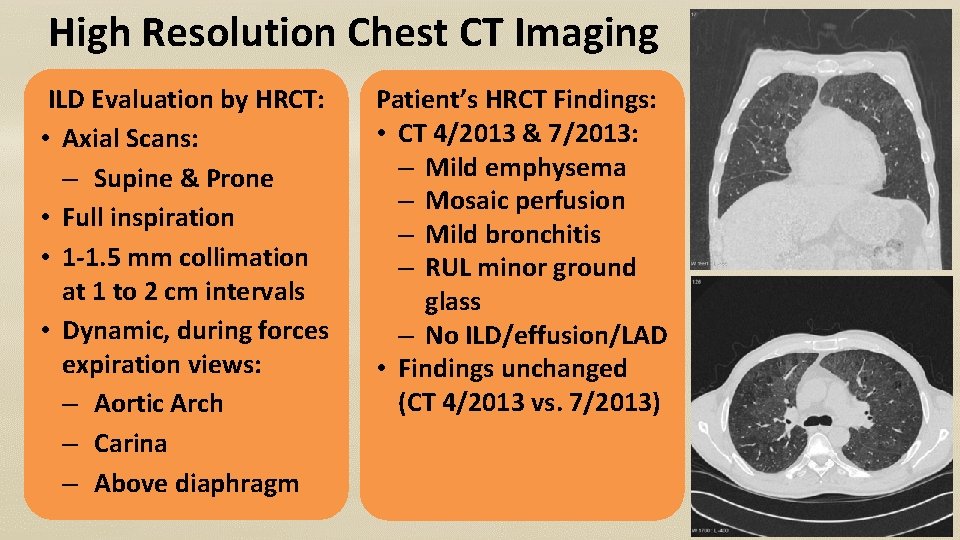
High Resolution Chest CT Imaging ILD Evaluation by HRCT: • Axial Scans: – Supine & Prone • Full inspiration • 1 -1. 5 mm collimation at 1 to 2 cm intervals • Dynamic, during forces expiration views: – Aortic Arch – Carina – Above diaphragm Patient’s HRCT Findings: • CT 4/2013 & 7/2013: – Mild emphysema – Mosaic perfusion – Mild bronchitis – RUL minor ground glass – No ILD/effusion/LAD • Findings unchanged (CT 4/2013 vs. 7/2013)
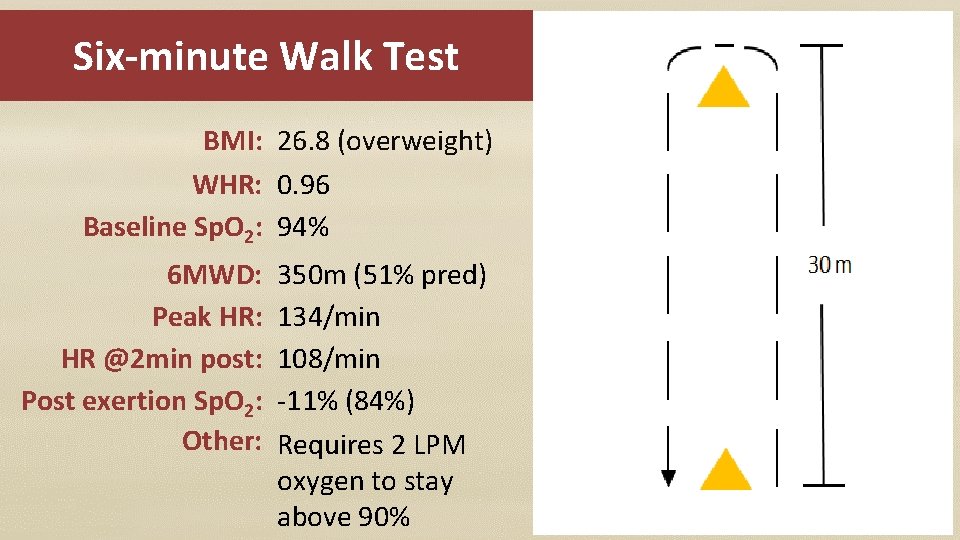
Six-minute Walk Test BMI: 26. 8 (overweight) WHR: 0. 96 Baseline Sp. O 2: 94% 6 MWD: Peak HR: HR @2 min post: Post exertion Sp. O 2: Other: 350 m (51% pred) 134/min 108/min -11% (84%) Requires 2 LPM oxygen to stay above 90%
What about lung biopsy? • When is lung biopsy indicated? • What type of biopsy is indicated? – Bronchoscopy with biopsy – Surgical lung biopsy (VATs) • What are the limitations of each type? • What are the possible complications?
Hospitalized in 2013 ØPresented with acute respiratory distress ØBronchoscopy: • Early granulomatous reaction • Consistent with silicosis • Larger tissues sample was recommended
Constrictive Bronchiolitis in OEF/OIF NEJM: CB in soldiers exertional dyspnea Ø 38 of 49 (78%) diagnosed with CB • PFTs, CPET within normal limits • Moderate reduction in DLCO ATS Research abstract: National Jewish Hospital US Army Public Health Command (USAPHC): ØEpidemiologic evidence to date is inadequate to support or refute an association between deployment and chronic respiratory conditions
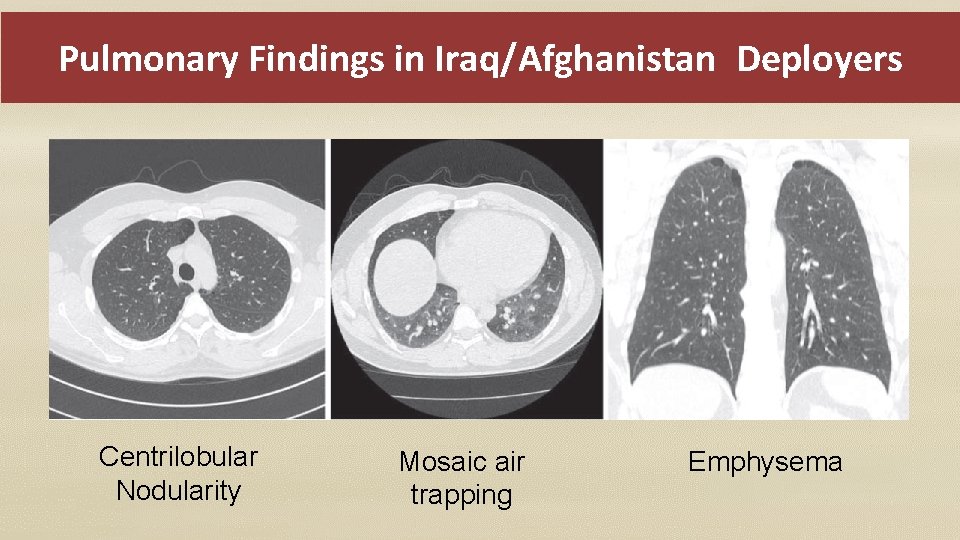
Pulmonary Findings in Iraq/Afghanistan Deployers Centrilobular Nodularity Mosaic air trapping Emphysema

Right Upper & Lower Lobe Open Biopsies Preliminary Pathology report: ØMild anthracosilicotic deposits ØHemosiderin-laden intra-alveolar macrophages ØDx: Smoking-related interstitial lung disease Addendum to pathology report (SEM/EDXA) ØParticles contain Si, Al, & O; K & Na (environmental silicates) ØRare particles Ti, Fe & Cr (possibly steel)
What is the Diagnosis? RB-ILD CB DIP
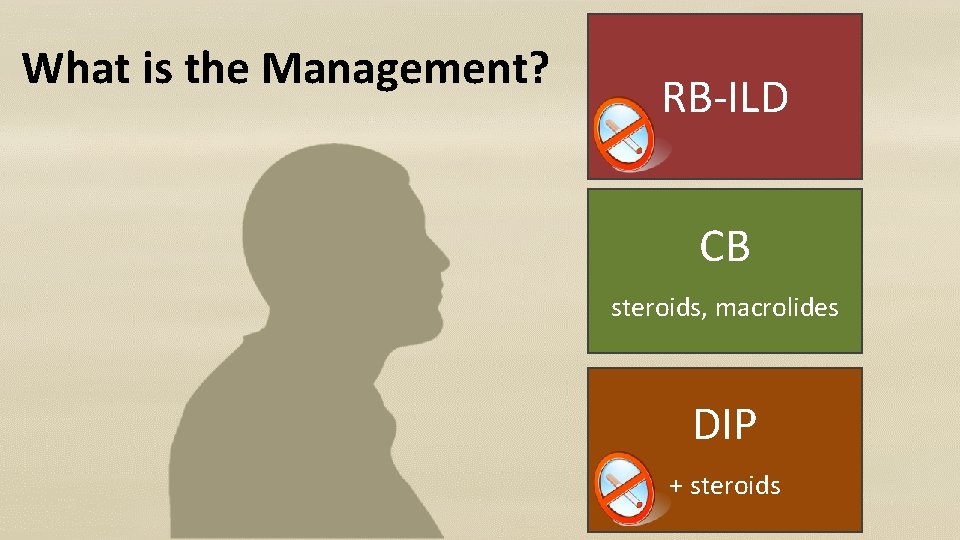
What is the Management? RB-ILD CB steroids, macrolides DIP + steroids
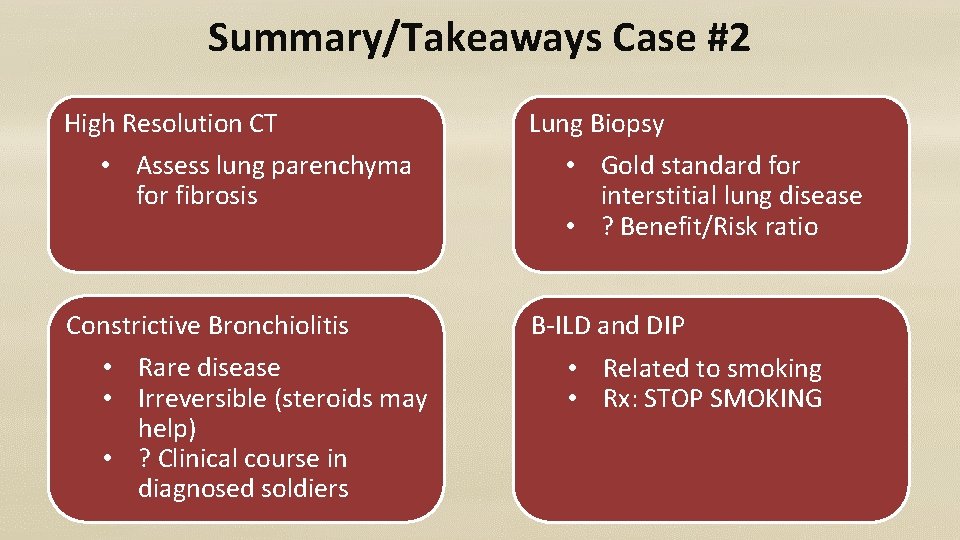
Summary/Takeaways Case #2 High Resolution CT • Assess lung parenchyma for fibrosis Constrictive Bronchiolitis • Rare disease • Irreversible (steroids may help) • ? Clinical course in diagnosed soldiers Lung Biopsy • Gold standard for interstitial lung disease • ? Benefit/Risk ratio B-ILD and DIP • Related to smoking • Rx: STOP SMOKING
Airborne Hazard Concerns Iraq & Afghanistan War Veterans • Many combat Veterans have airborne hazard exposure concerns. – Have high index of suspicion for upper & lower respiratory problems & a low bar for further evaluation. – Identify physical /behavioral health co-morbidities early and treat. • Case management services to support change in lifestyle interventions.

THANK YOU !
Questions? New Jersey War-related Illness and Injury Study Center http: //www. warrelatedillness. va. gov/ omowunmi. osinubi@va. gov 1 -800 -248 -8005 anays. sotolongo@va. gov
- Slides: 51