CLINICAL LABORATORY DIAGNOSTICS OF PATHOLOGICAL PROCESSESS IN LUNGS
CLINICAL LABORATORY DIAGNOSTICS OF PATHOLOGICAL PROCESSESS IN LUNGS Marushchak Maria
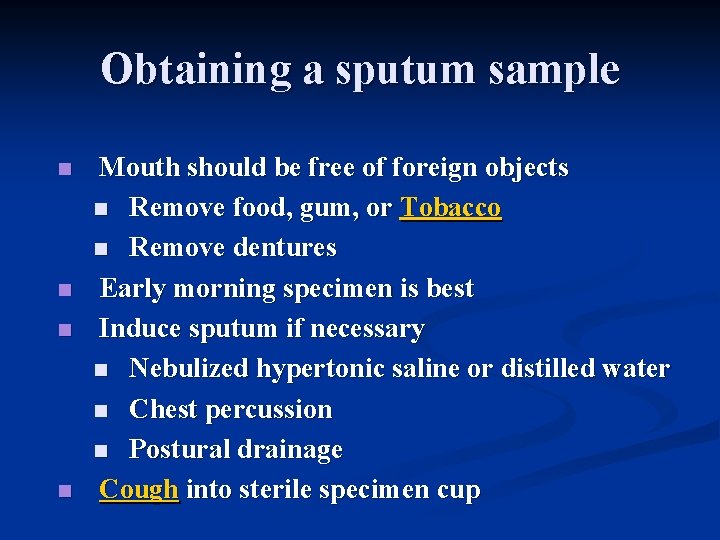
Obtaining a sputum sample n n Mouth should be free of foreign objects n Remove food, gum, or Tobacco n Remove dentures Early morning specimen is best Induce sputum if necessary n Nebulized hypertonic saline or distilled water n Chest percussion n Postural drainage Cough into sterile specimen cup
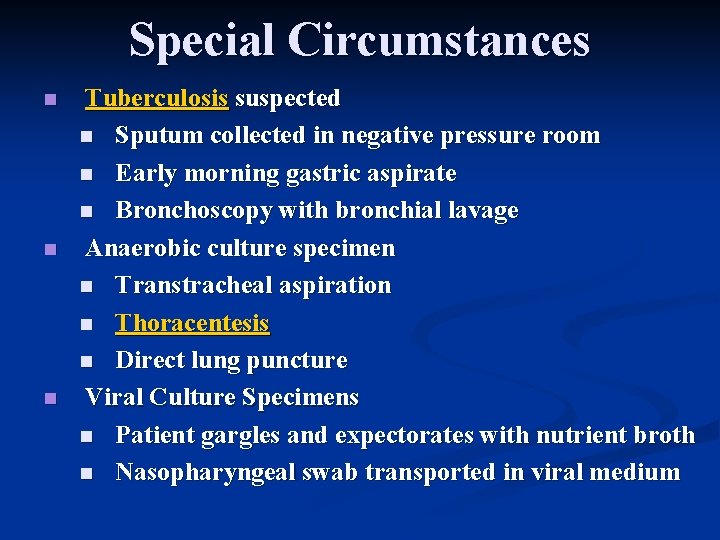
Special Circumstances n n n Tuberculosis suspected n Sputum collected in negative pressure room n Early morning gastric aspirate n Bronchoscopy with bronchial lavage Anaerobic culture specimen n Transtracheal aspiration n Thoracentesis n Direct lung puncture Viral Culture Specimens n Patient gargles and expectorates with nutrient broth n Nasopharyngeal swab transported in viral medium
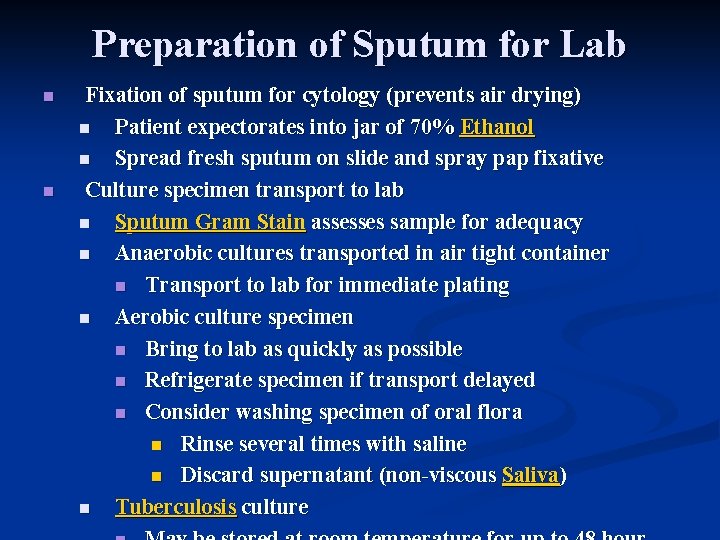
Preparation of Sputum for Lab n n Fixation of sputum for cytology (prevents air drying) n Patient expectorates into jar of 70% Ethanol n Spread fresh sputum on slide and spray pap fixative Culture specimen transport to lab n Sputum Gram Stain assesses sample for adequacy n Anaerobic cultures transported in air tight container n Transport to lab for immediate plating n Aerobic culture specimen n Bring to lab as quickly as possible n Refrigerate specimen if transport delayed n Consider washing specimen of oral flora n Rinse several times with saline n Discard supernatant (non-viscous Saliva) n Tuberculosis culture
Sputum Gross Exam
Estimate daily volume of Sputum n n Small amounts n Lung Abscess n Pneumonia n Tuberculosis Copious amounts (>200 cc/day) n Bronchiectasis n Bronchopleural Fistula
Sputum Color n n n Bloody Sputum (Hemoptysis) Rusty Sputum (Prune-juice) n Pneumococcal Pneumonia Purulent Sputum (yellow, green, dirtygray) n Color alone does not distinguish bacterial infection
Sputum Turbidity n n Frothy Sputum (air bubbles, Hemoglobin) n Pulmonary edema Foamy, clear material n Saliva n Nasal secretions
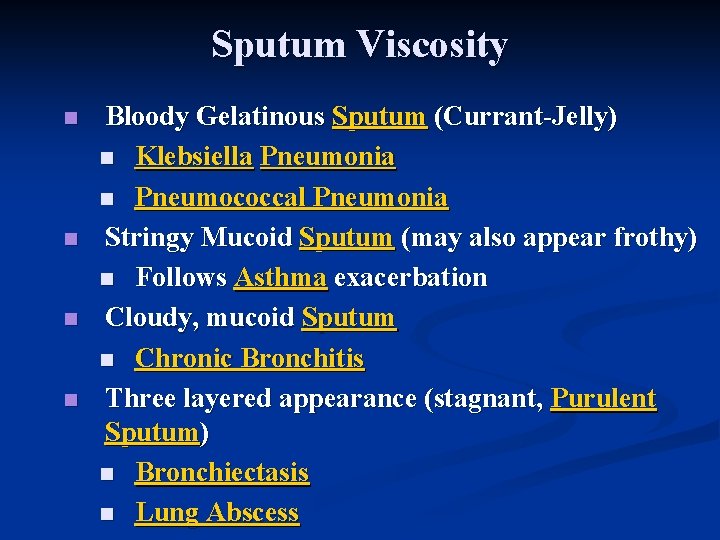
Sputum Viscosity n n Bloody Gelatinous Sputum (Currant-Jelly) n Klebsiella Pneumonia n Pneumococcal Pneumonia Stringy Mucoid Sputum (may also appear frothy) n Follows Asthma exacerbation Cloudy, mucoid Sputum n Chronic Bronchitis Three layered appearance (stagnant, Purulent Sputum) n Bronchiectasis n Lung Abscess

Sputum with Feculent Odor n n Anaerobic infection Bronchiectasis
Sputum Microscopy
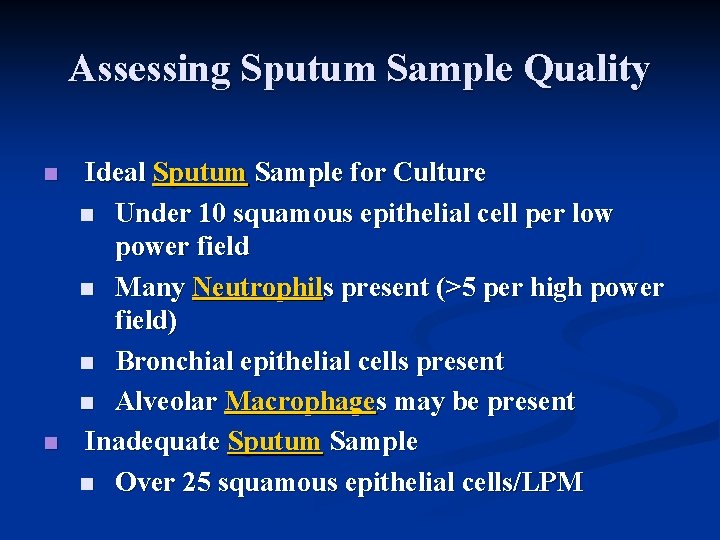
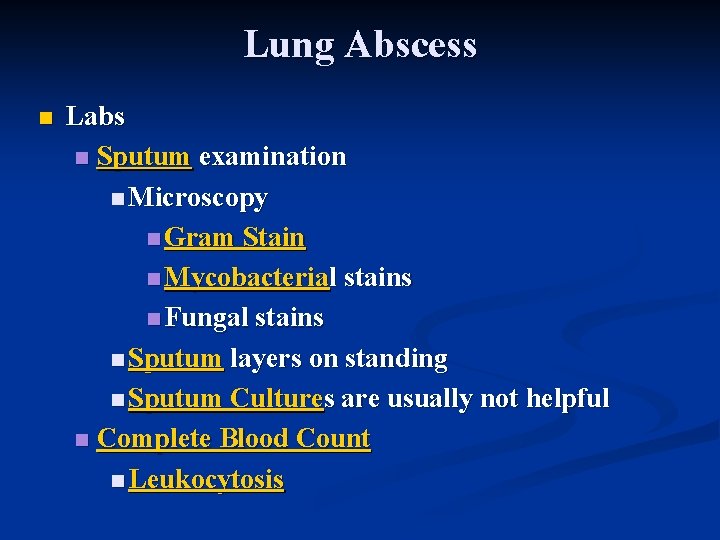
Assessing Sputum Sample Quality n n Ideal Sputum Sample for Culture n Under 10 squamous epithelial cell per low power field n Many Neutrophils present (>5 per high power field) n Bronchial epithelial cells present n Alveolar Macrophages may be present Inadequate Sputum Sample n Over 25 squamous epithelial cells/LPM
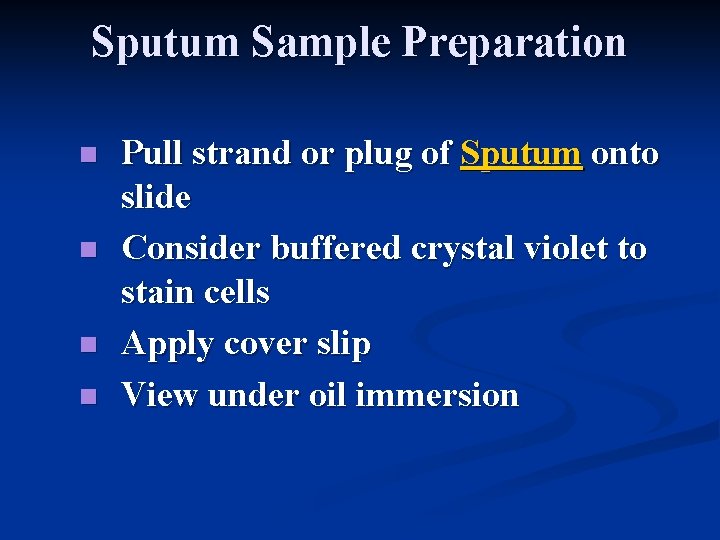
Sputum Sample Preparation n n Pull strand or plug of Sputum onto slide Consider buffered crystal violet to stain cells Apply cover slip View under oil immersion

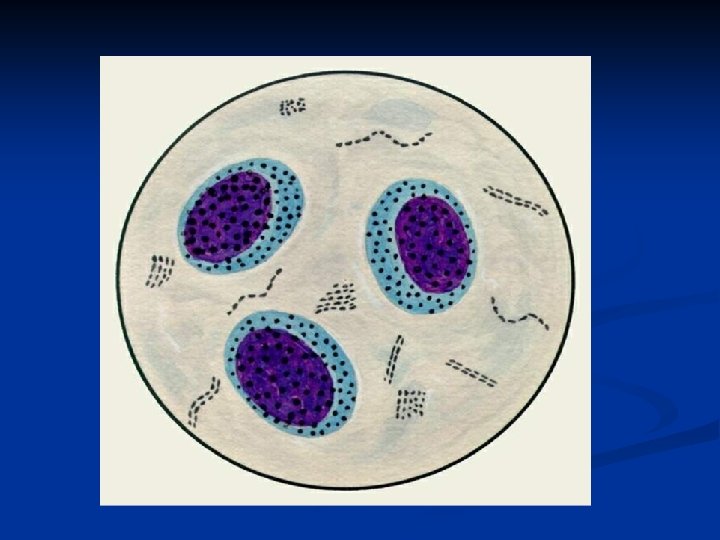
Cytology Stains n n No Stain n Blastomycosis n Cryptococcosis Gram Stain n Gram Positive Bacteria n Candida n Tuberculosis (weakly Gram Positive) n Nocardia (weakly Gram Positive) Direct Fluorescent Antibody Staining n Legionella Wright stain or Giemsa Stain n Intracellular organisms
Special Staining Circumstances
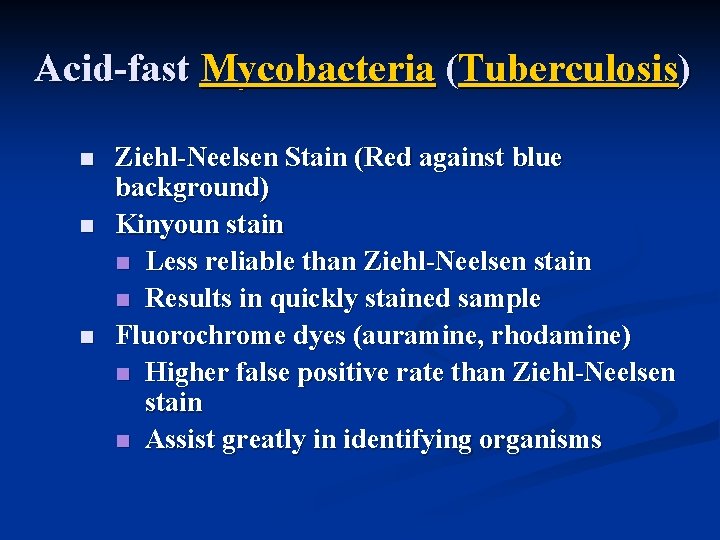
Acid-fast Mycobacteria (Tuberculosis) n n n Ziehl-Neelsen Stain (Red against blue background) Kinyoun stain n Less reliable than Ziehl-Neelsen stain n Results in quickly stained sample Fluorochrome dyes (auramine, rhodamine) n Higher false positive rate than Ziehl-Neelsen stain n Assist greatly in identifying organisms
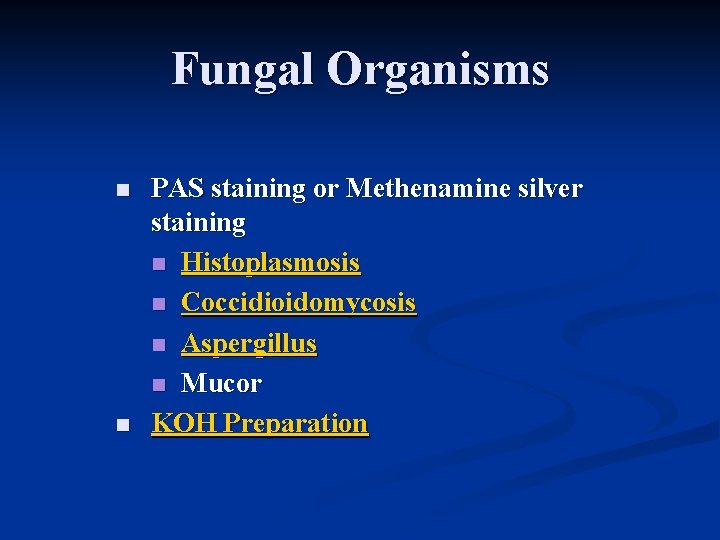
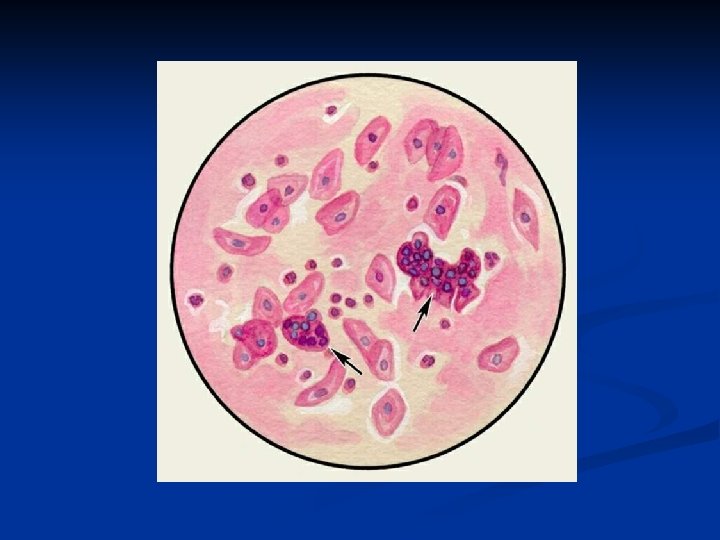
Fungal Organisms n n PAS staining or Methenamine silver staining n Histoplasmosis n Coccidioidomycosis n Aspergillus n Mucor KOH Preparation
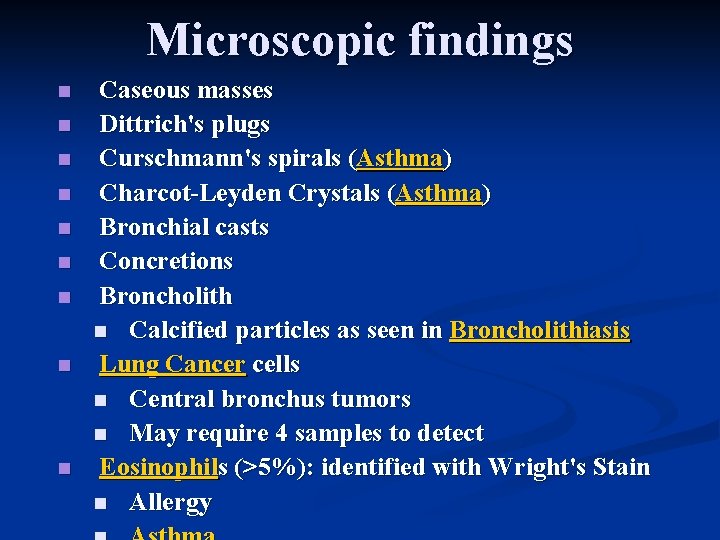
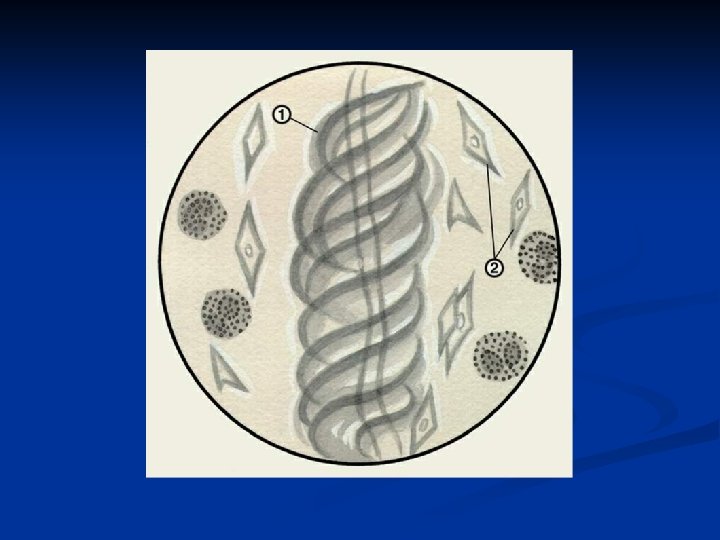
Microscopic findings n n n n n Caseous masses Dittrich's plugs Curschmann's spirals (Asthma) Charcot-Leyden Crystals (Asthma) Bronchial casts Concretions Broncholith n Calcified particles as seen in Broncholithiasis Lung Cancer cells n Central bronchus tumors n May require 4 samples to detect Eosinophils (>5%): identified with Wright's Stain n Allergy

Pneumonia n General n Lab Indications n Moderate or severe community acquired pneumonia n Patient with comorbid conditions n Efficacy of Labs n No value in non-severe community acquired pneumonia
Sputum Examination n n Tests n Sputum Gram Stain n Sputum Culture Efficacy of Sputum exam n Sputum has low diagnostic yield in CAP n Not recommended in community acquired pneumonia
Blood Culture n n Indications n Not indicated unless severe disease n Recommended by ATS in hospitalized CAP Efficacy n Low sensitivity: Positive in only 510% of cases n Does not predict severity or outcome
Specific Testing with reasonable efficacy n n Chlamydia pneumonia n Rapid PCR (>30% Test Sensitivity) Influenza n Rapid Influenza Test (Influenza DFA) Legionella pneumophila n Rapid PCR of Sputum (80% Test Sensitivity) n Urinary antigen (>50% Test Sensitivity) Mycoplasma pneumoniae n Rapid PCR of Sputum (>30% Test Sensitivity)
Chronic Bronchitis n Labs n Arterial Blood Gas (ABG) n Markedly reduced arterial p. O 2 n Elevated arterial p. CO 2 (40 -50 mm. Hg) n Pulmonary Function Tests n Residual Volume increased n FEV 1 decreased n FEV 1/FVC decreased n FEF 25 -75 (mid-flows) decreased n Diffusion capacity (DLCO) near normal

Bronchiectasis n Labs: Sputum n Sputum forms layers on standing n Top: Mucus n Middle: Clear fluid n Bottom: Pus n Sputum Culture not diagnostic (mixture of organisms) n Fungal Culture
Lung Abscess n Labs n Sputum examination n Microscopy n Gram Stain n Mycobacterial stains n Fungal stains n Sputum layers on standing n Sputum Cultures are usually not helpful n Complete Blood Count n Leukocytosis


Саrре diem
- Slides: 31