Clinical Information Systems Integrating Registries into Everyday Practice
- Slides: 21
Clinical Information Systems: Integrating Registries into Everyday Practice Mike Hindmarsh Improving Chronic Illness Care California Chronic Care Learning Communities Initiative Collaborative February 2, 2004 Oakland, CA
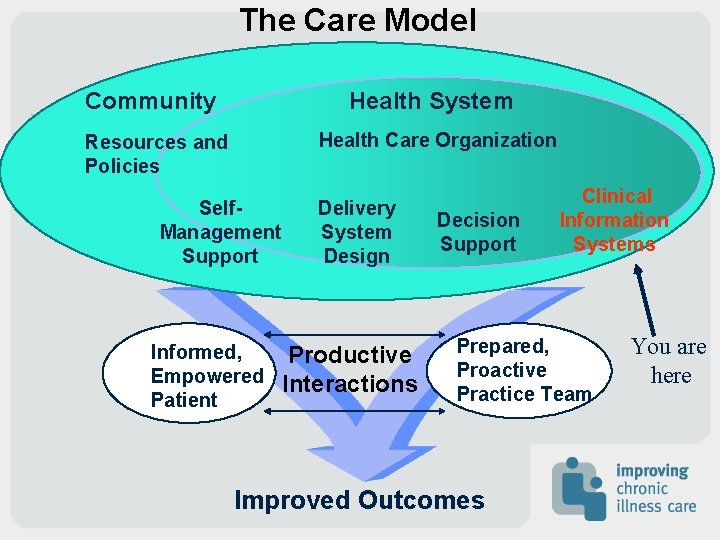
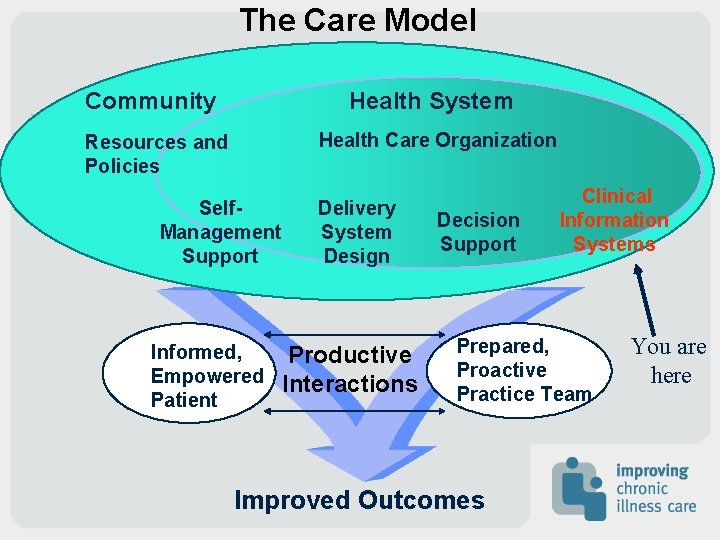
The Care Model Community Health System Health Care Organization Resources and Policies Self. Management Support Informed, Empowered Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Improved Outcomes You are here
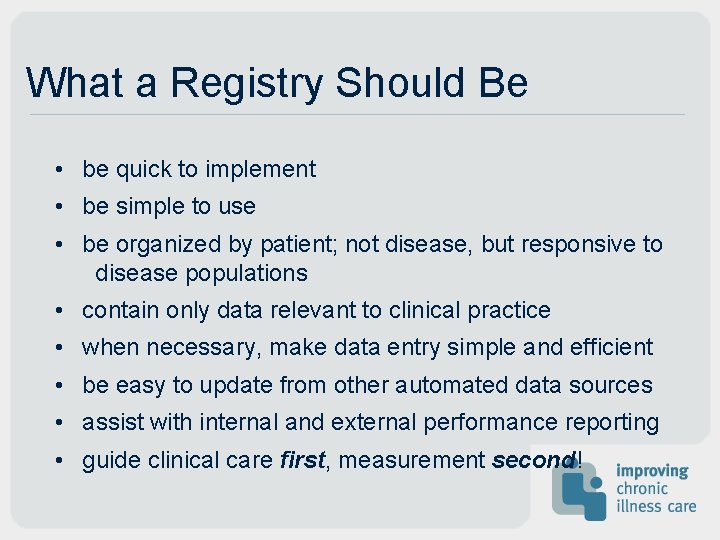
What a Registry Should Be • be quick to implement • be simple to use • be organized by patient; not disease, but responsive to disease populations • contain only data relevant to clinical practice • when necessary, make data entry simple and efficient • be easy to update from other automated data sources • assist with internal and external performance reporting • guide clinical care first, measurement second!
Can I use my EMR for what I need to do? Yes, if… • It provides access to lab data, dx test results, and across settings in your system. • Guidelines and prompts are included for needed services • You can identify populations and subpopulations of patients
Can I…(cont. ) If… • Allows stratification of patients (complexity, disease severity for case management services) • Captures outcomes by provider • Captures all critical clinical information
Use the CIS to: 1. Create population-specific reports 2. Facilitate external reporting requirements 3. Create dashboard reports of the practice as a whole
CIS: Facts vs. Fears Fear: Why do we have to have a registry? Fact: Planned population-based care cannot be done without knowing your patient population and its key clinical data Fact: Primary care teams that implement registries are more likely to improve processes of care for all chronic conditions Fact: Teams with registries are less likely to lose patients to follow-up, and more likely to improve patient satisfaction as care improves
CIS: Facts vs. Fears Fear: I don’t need anyone telling me how to practice! I’m doing just fine with my patients! Fact: Surveys show that providers consistently under estimate the numbers of patients with chronic disease in their practice Fact: Surveys show that provider consistently over estimate their performance measures on process and clinical outcomes for chronically ill patients. Fact: The two are interdependent. Fact: Knowing you population of patients will help rectify this disparity.
CIS: Facts vs. Fears Fear: It’s just more work during our already hectic day! Fact: Using a patient summary form from a Registry will actually reduce charting time and make the visit run more smoothly Fact: The form gives a snapshot of past care, reminders of needed care and planning for future care all at the time of the visit Fact: Teams with registries feel better prepared for visits since they have the patient information when and where they need it.
CIS: Facts vs. Fears Fear: This will cost me a fortune and there’s no return on investment! Fact: Implementing a registry is simple, and there are economies of scale as you add more patients. Fact: Registries facilitate populations-based care which improves outcomes and patient satisfaction Fact: Planned care via the registry generates visits that are typically of higher intensity while reducing unexpected visits for acute exacerbations
Making Clinical Information Work for You in Clinical Practice
The Software • Assess available software for appropriate functionality • Install the software. • Identify training resources. • Highlight CIS importance to rest of team for buy-in
The Chronic Illness Data Manager • Identify best person on team to manage the disease management information. • Choose person with computer skills and interest. • Define roles and responsibilities for manager. • Secure training for manager as needed. • Train a back-up.
Populating a Registry • Use billing data and ICD 9 codes to identify specific populations or build prospectively. • Download names and contact information into registry. • Establish process for regular population updates.
Getting Clinical Data into the Registry • Define the relevant clinical data needs. • Use the visit for collecting non-automated data. • Develop and test data capture process. • Use chart audits judiciously. • Develop and test data entry process
Using Data at Point of Care • Establish process for producing patient summary data for use at time of visit. (acute or planned) • Make sure summary is replacing other data capture processes to avoid double entry. • Ensure summary is on chart or in the exam room. • Does the summary work for various patient types? • Ensure new data is captured on the summary. • Develop process for new summary data to be entered into registry.
Using Data for Care Reminders • Establish what you want “reminding” about. • Determine how you want to be reminded. (i. e, exception reports or individual patient prompts) • Identify team member responsible for monitoring reminders. • Create process for responding to reminders. (i. e. , who calls patient, when and for what purpose) • Create process for updating/modifying reminders.
Using Data to Monitor Performance • Determine what types of population reports are needed and reporting intervals. • Establish process for creating customized reports. • Who will generate reports? • Who receives reports? • Do the reports facilitate continued improvement?
Keys to Success from Others That Have Implemented Registries • Everyone understands the clinical utility and supports the time involved in registry upkeep. Care management using registry data is a team approach • Dedicated time each week for primary team to use data • Data forms are clear, roles are assigned, data review time allotted. • Data are clinically relevant, and used for patient care first, and measurement second. • Data can be shared with patient to improve understanding of treatment plan.
Barriers to CIS use • Lack of perceived value • Competing business and productivity demands • Lack of office flow expertise • Lack of information support • Lack of leadership support
For More Information: Please visit Improving Chronic Illness Care’s web site at www. improvingchroniccare. org