Clinical indications for androgen assays in gynaecology Petra


- Slides: 35
Clinical indications for androgen assays in gynaecology Petra De Sutter Div. Reproductive Medicine UZ Gent
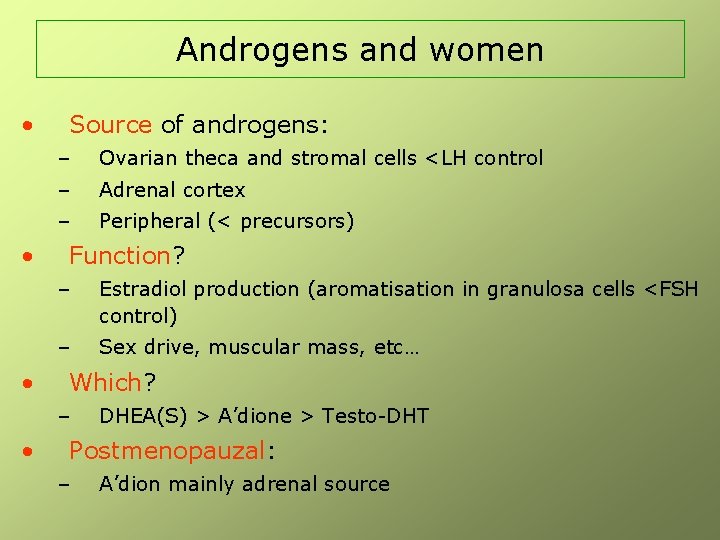
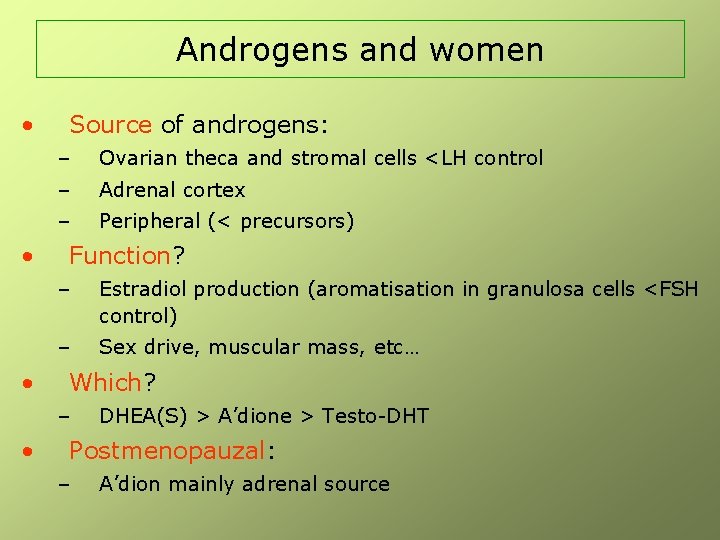
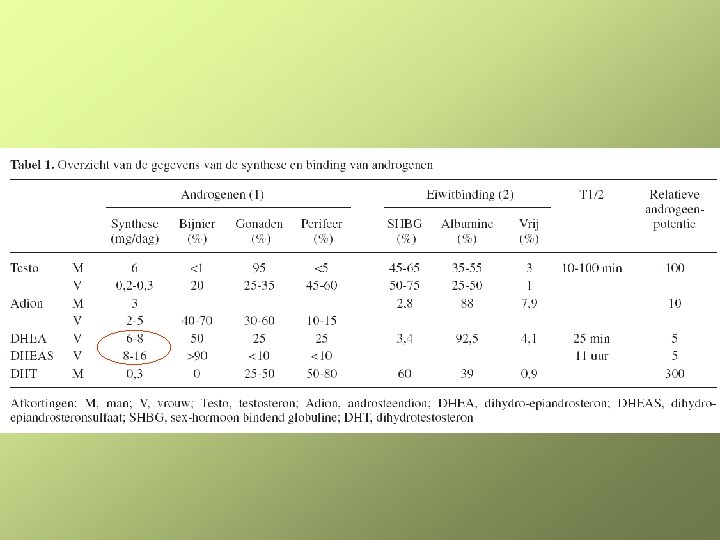
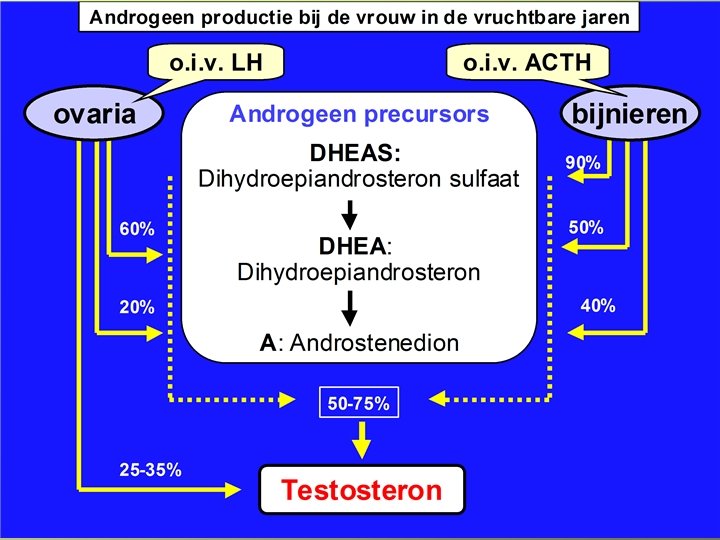
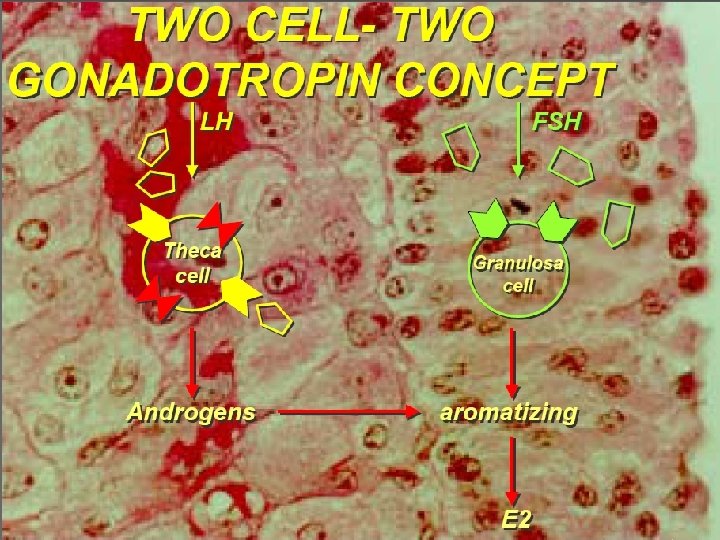
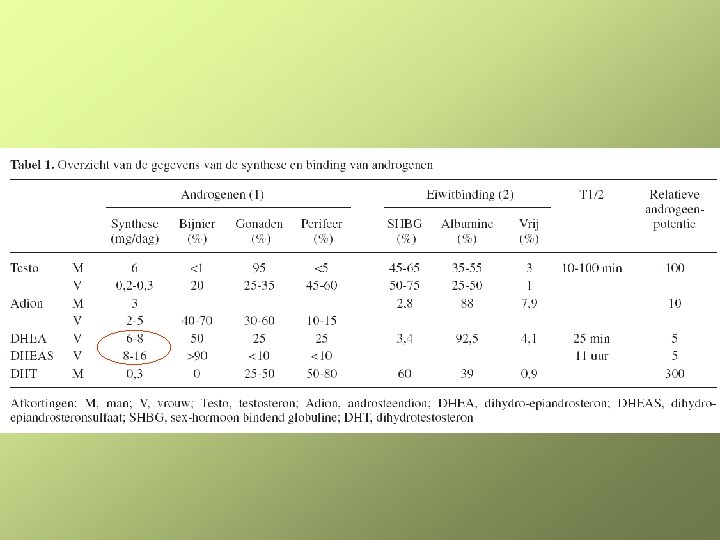
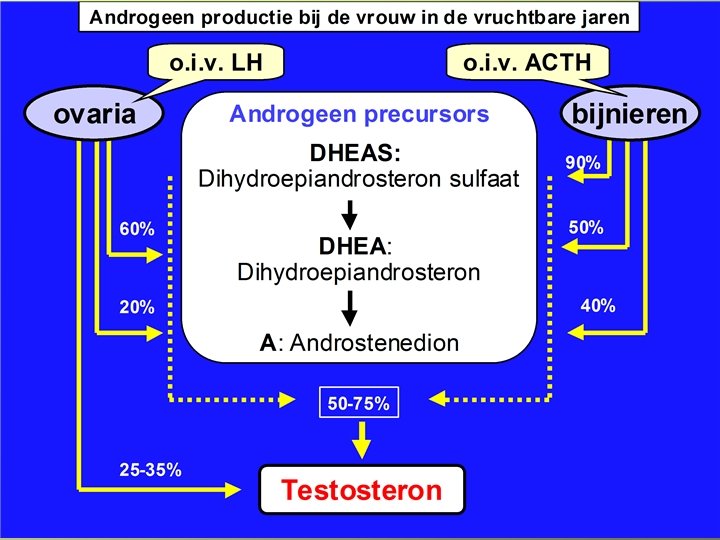
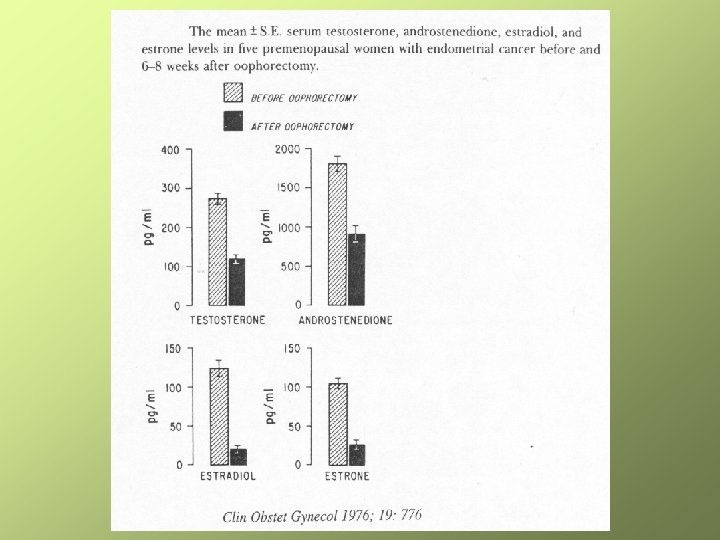
Androgens and women • • • Source of androgens: – Ovarian theca and stromal cells <LH control – Adrenal cortex – Peripheral (< precursors) Function? – Estradiol production (aromatisation in granulosa cells <FSH control) – Sex drive, muscular mass, etc… Which? – • DHEA(S) > A’dione > Testo-DHT Postmenopauzal: – A’dion mainly adrenal source
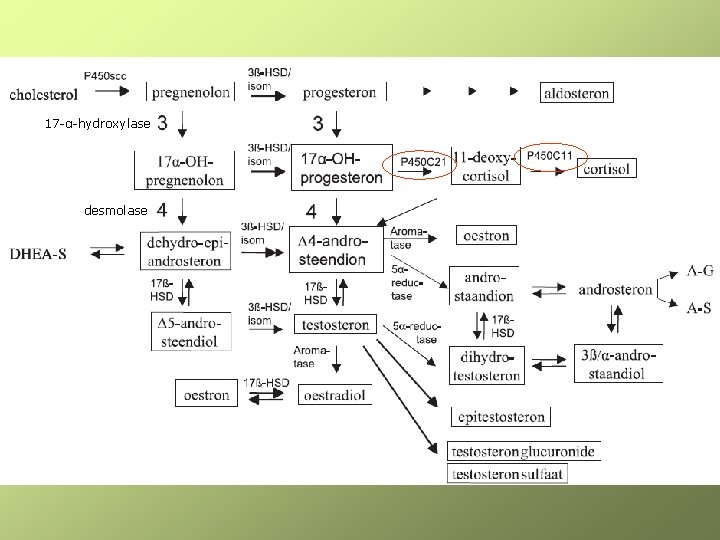
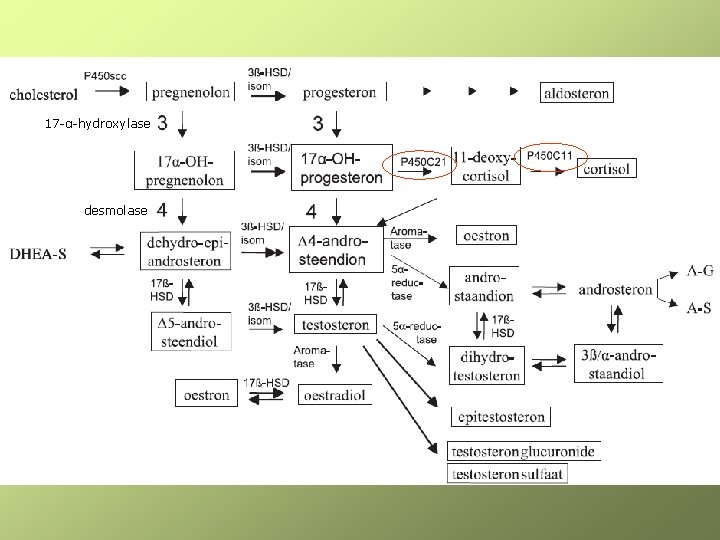
17 -α-hydroxylase desmolase
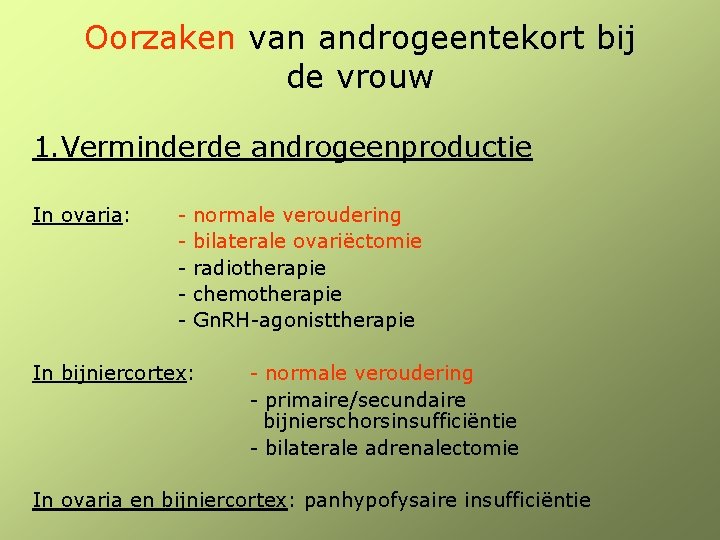
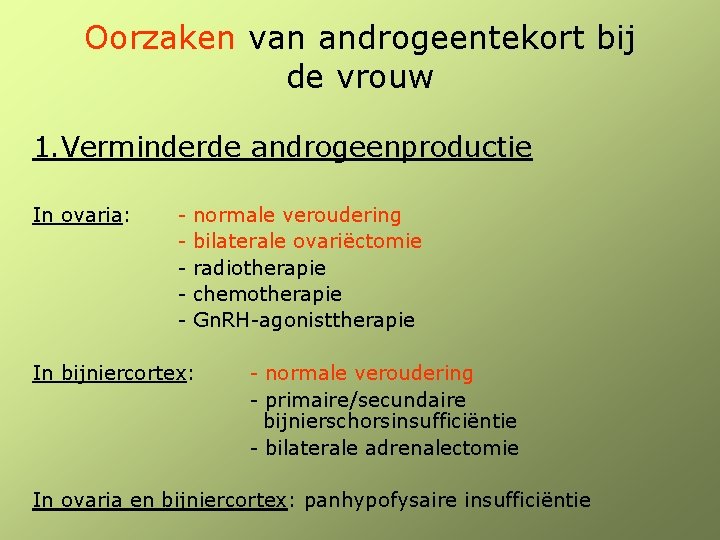
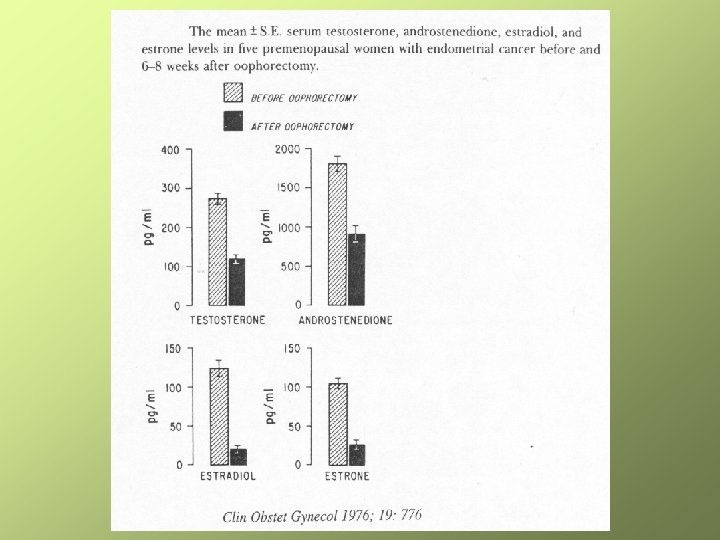
Oorzaken van androgeentekort bij de vrouw 1. Verminderde androgeenproductie In ovaria: - normale veroudering - bilaterale ovariëctomie - radiotherapie - chemotherapie - Gn. RH-agonisttherapie In bijniercortex: - normale veroudering - primaire/secundaire bijnierschorsinsufficiëntie - bilaterale adrenalectomie In ovaria en bijniercortex: panhypofysaire insufficiëntie
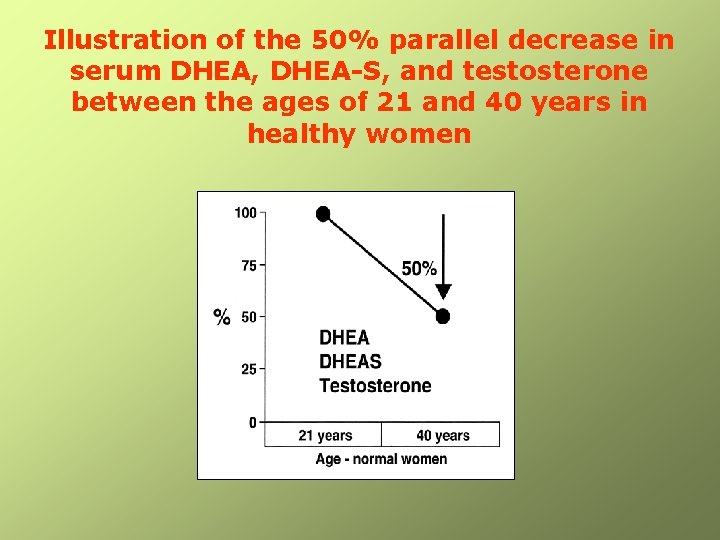
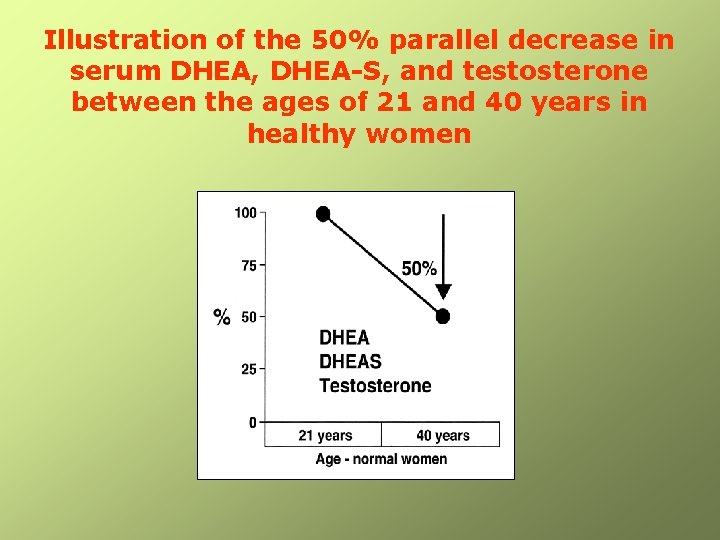
Illustration of the 50% parallel decrease in serum DHEA, DHEA-S, and testosterone between the ages of 21 and 40 years in healthy women
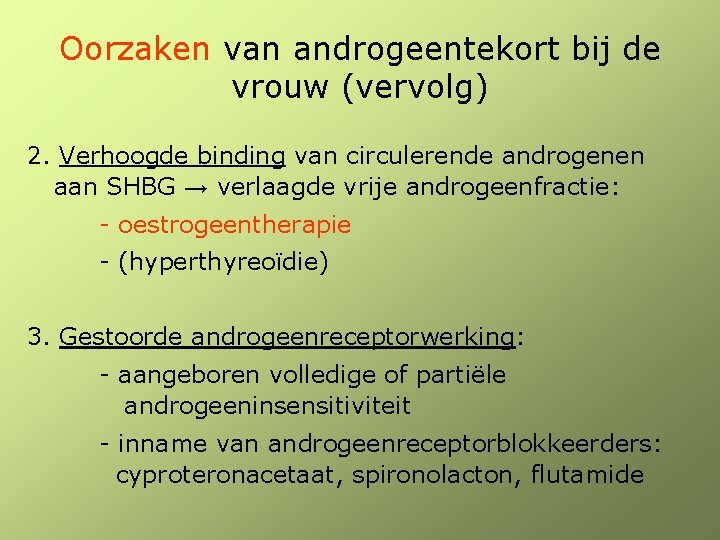
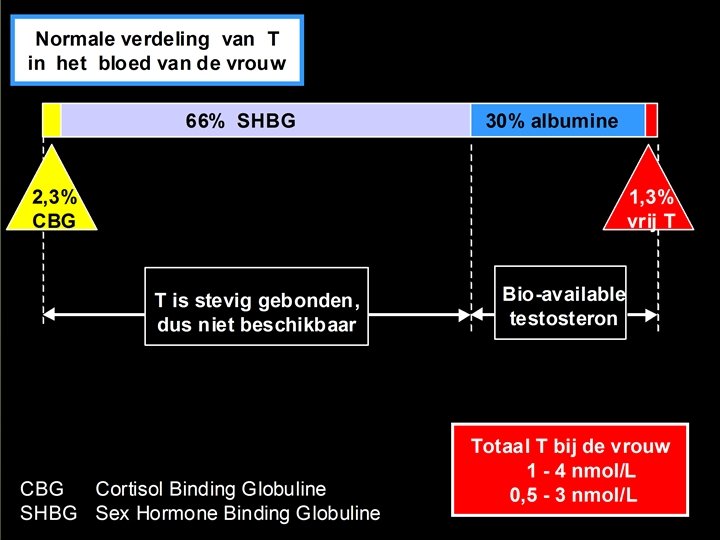
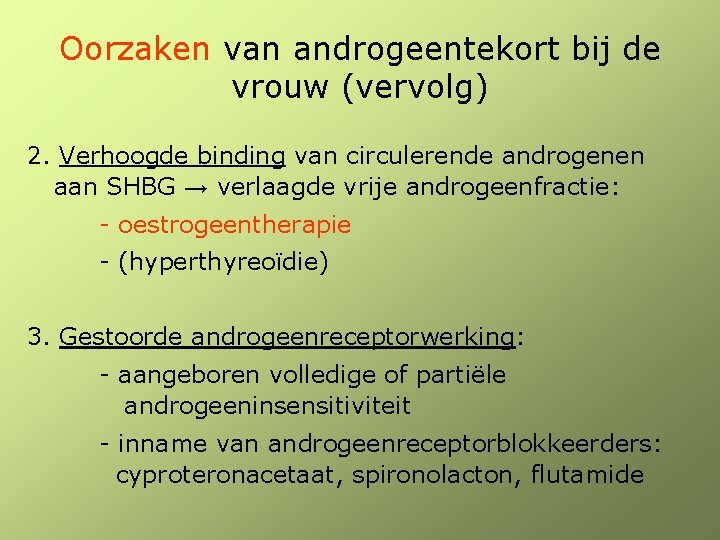
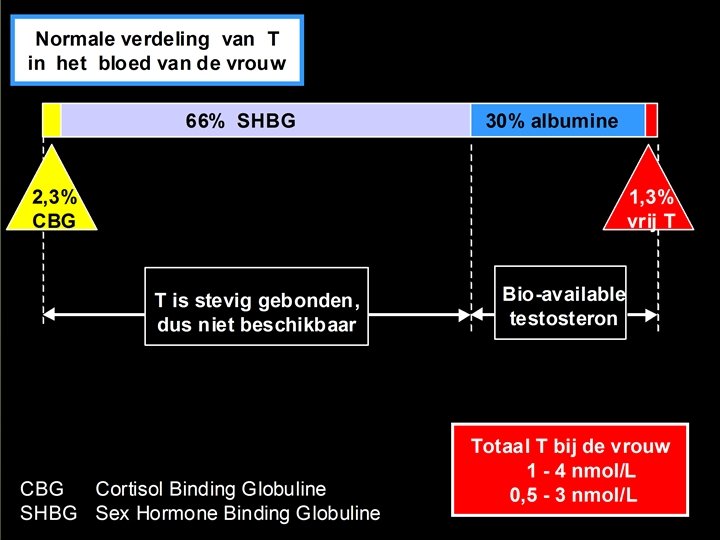
Oorzaken van androgeentekort bij de vrouw (vervolg) 2. Verhoogde binding van circulerende androgenen aan SHBG → verlaagde vrije androgeenfractie: - oestrogeentherapie - (hyperthyreoïdie) 3. Gestoorde androgeenreceptorwerking: - aangeboren volledige of partiële androgeeninsensitiviteit - inname van androgeenreceptorblokkeerders: cyproteronacetaat, spironolacton, flutamide
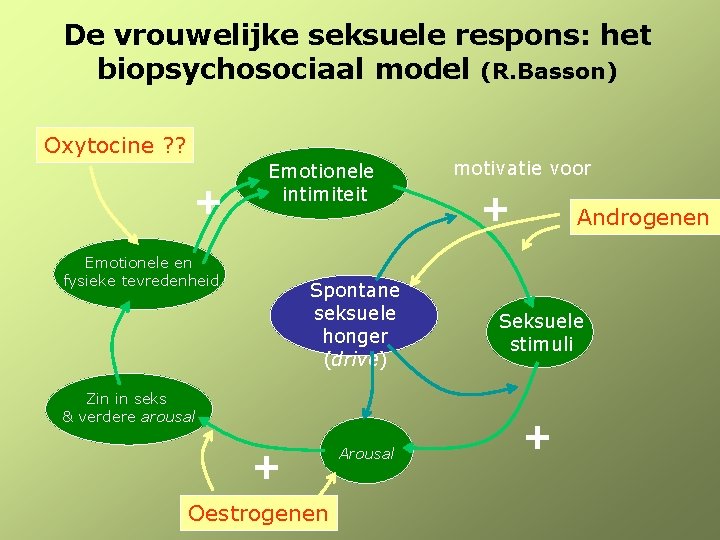
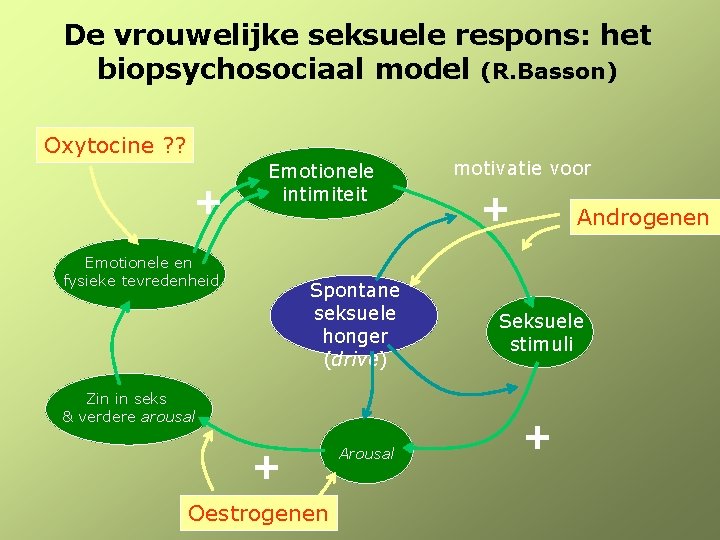
De vrouwelijke seksuele respons: het biopsychosociaal model (R. Basson) Oxytocine ? ? + Emotionele intimiteit Emotionele en fysieke tevredenheid Spontane seksuele honger (drive) Zin in seks & verdere arousal + Oestrogenen Arousal motivatie voor + Androgenen Seksuele stimuli +
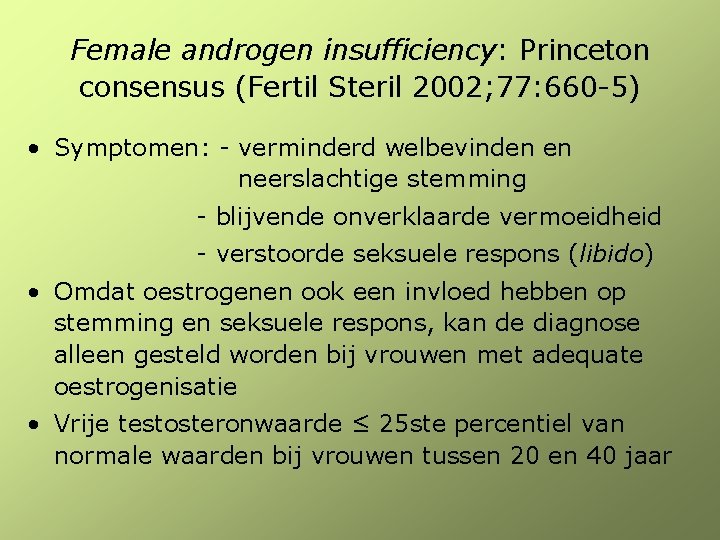
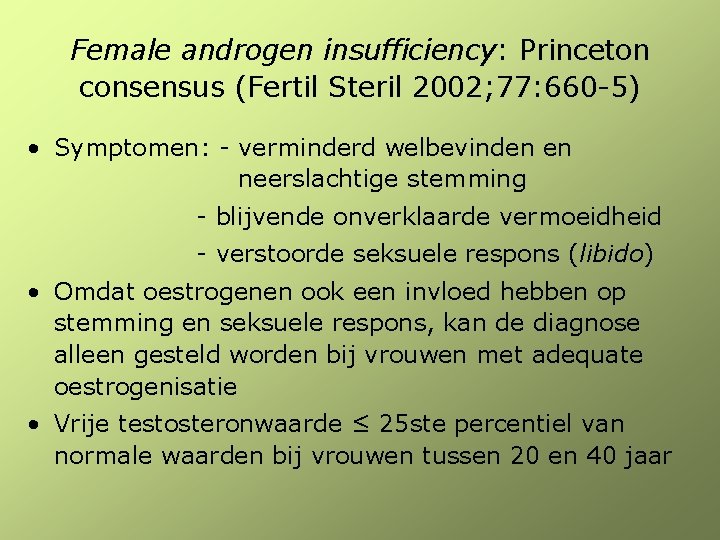
Female androgen insufficiency: Princeton consensus (Fertil Steril 2002; 77: 660 -5) • Symptomen: - verminderd welbevinden en neerslachtige stemming - blijvende onverklaarde vermoeidheid - verstoorde seksuele respons (libido) • Omdat oestrogenen ook een invloed hebben op stemming en seksuele respons, kan de diagnose alleen gesteld worden bij vrouwen met adequate oestrogenisatie • Vrije testosteronwaarde ≤ 25 ste percentiel van normale waarden bij vrouwen tussen 20 en 40 jaar
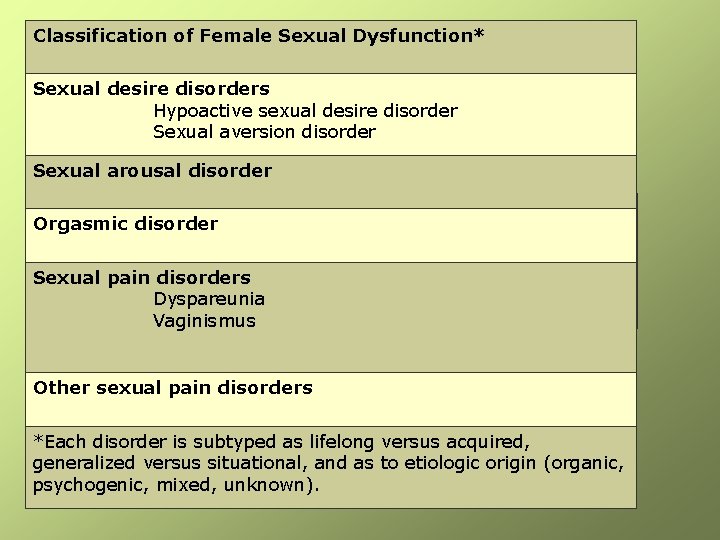
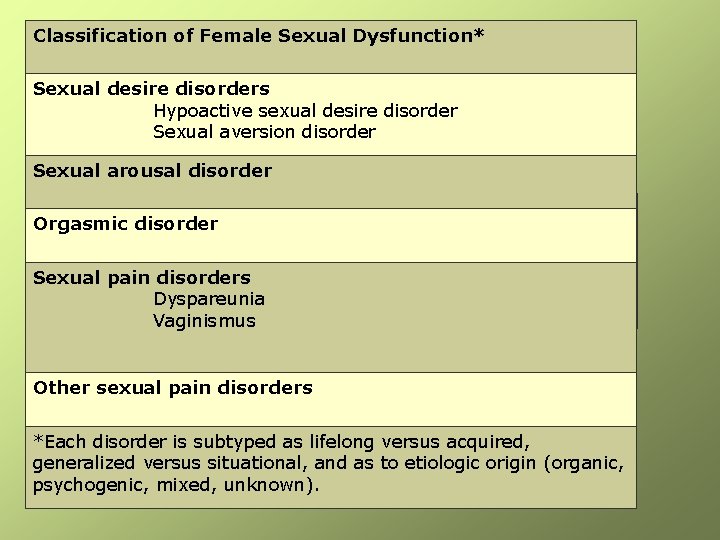
Classification of Female Sexual Dysfunction* Sexual desire disorders Hypoactive sexual desire disorder Sexual aversion disorder Sexual arousal disorder Orgasmic disorder Sexual pain disorders Dyspareunia Vaginismus Other sexual pain disorders *Each disorder is subtyped as lifelong versus acquired, generalized versus situational, and as to etiologic origin (organic, psychogenic, mixed, unknown).

Androgen excess • Hyperandrogenism (virilisation) – Acne – Hirsutism – alopecia • Cycle disturbances – PCOS
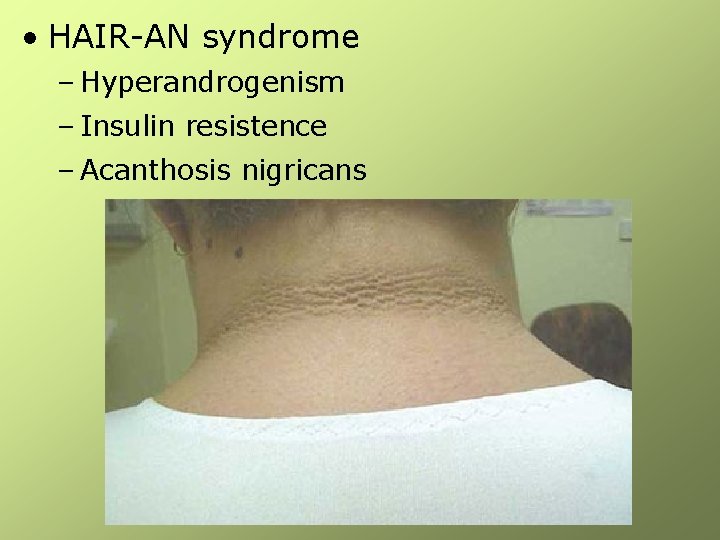
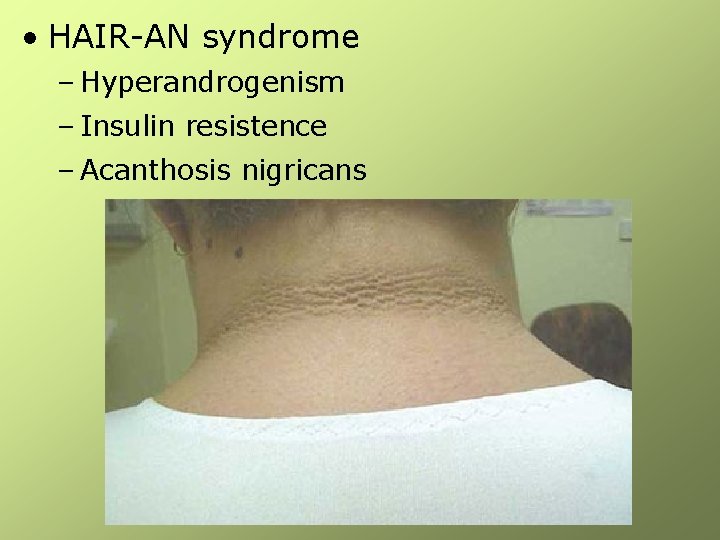
• HAIR-AN syndrome – Hyperandrogenism – Insulin resistence – Acanthosis nigricans
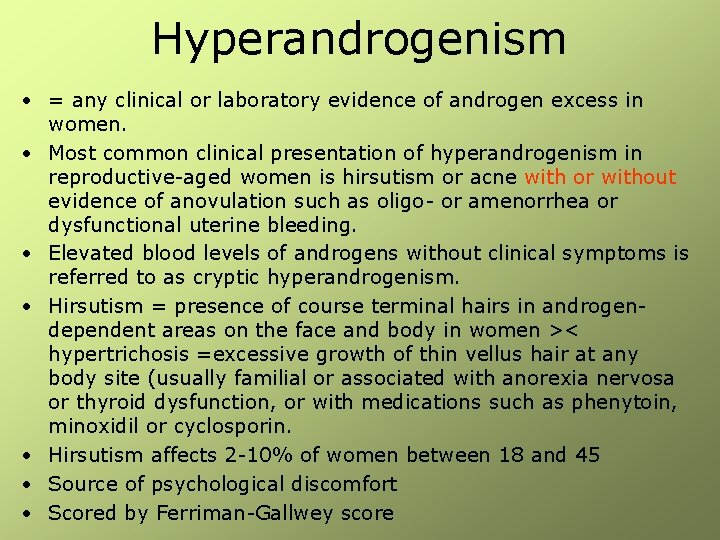
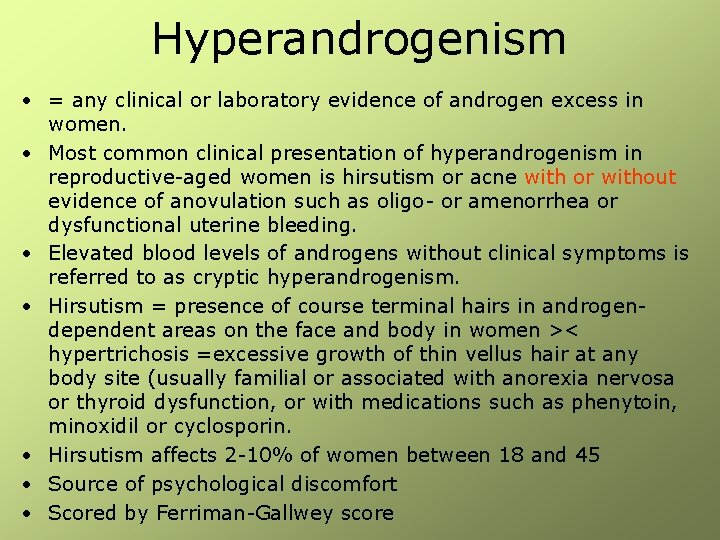
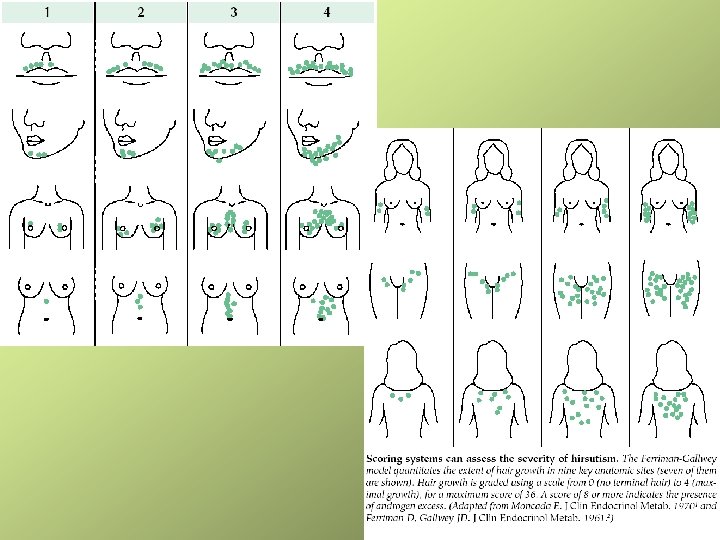
Hyperandrogenism • = any clinical or laboratory evidence of androgen excess in women. • Most common clinical presentation of hyperandrogenism in reproductive-aged women is hirsutism or acne with or without evidence of anovulation such as oligo- or amenorrhea or dysfunctional uterine bleeding. • Elevated blood levels of androgens without clinical symptoms is referred to as cryptic hyperandrogenism. • Hirsutism = presence of course terminal hairs in androgendependent areas on the face and body in women >< hypertrichosis =excessive growth of thin vellus hair at any body site (usually familial or associated with anorexia nervosa or thyroid dysfunction, or with medications such as phenytoin, minoxidil or cyclosporin. • Hirsutism affects 2 -10% of women between 18 and 45 • Source of psychological discomfort • Scored by Ferriman-Gallwey score
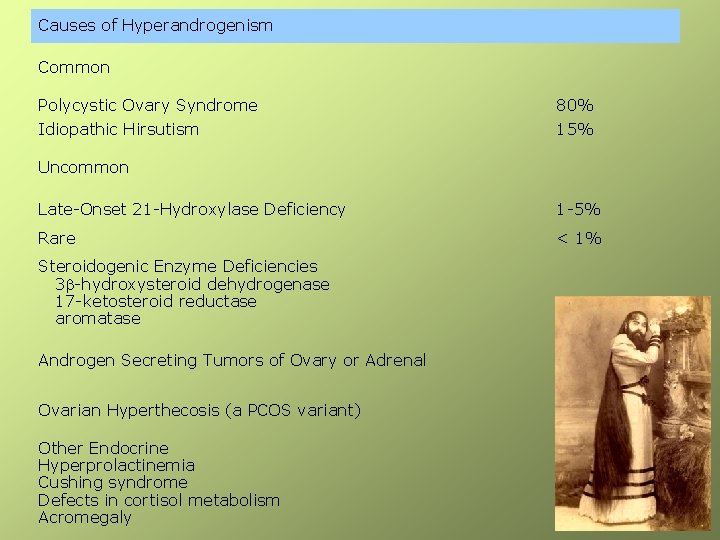
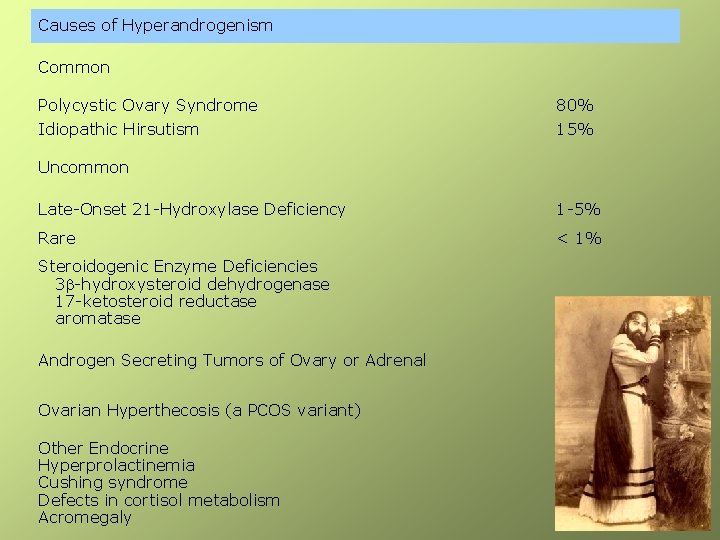
Causes of Hyperandrogenism Common Polycystic Ovary Syndrome 80% Idiopathic Hirsutism 15% Uncommon Late-Onset 21 -Hydroxylase Deficiency 1 -5% Rare < 1% Steroidogenic Enzyme Deficiencies 3 b-hydroxysteroid dehydrogenase 17 -ketosteroid reductase aromatase Androgen Secreting Tumors of Ovary or Adrenal Ovarian Hyperthecosis (a PCOS variant) Other Endocrine Hyperprolactinemia Cushing syndrome Defects in cortisol metabolism Acromegaly
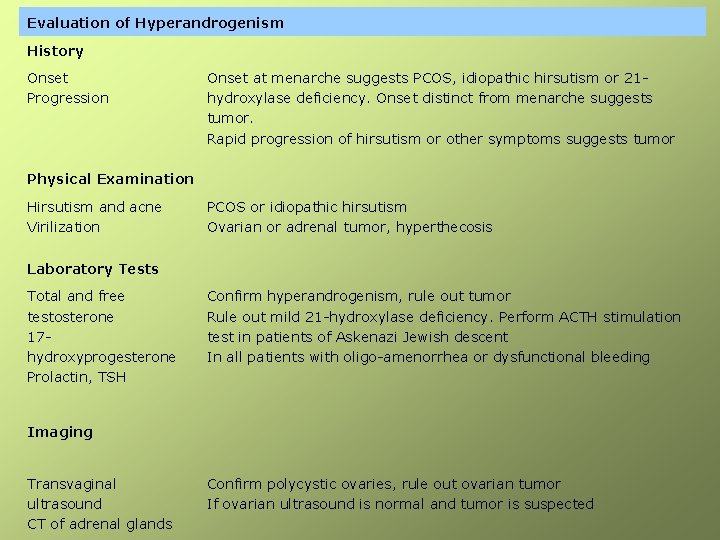
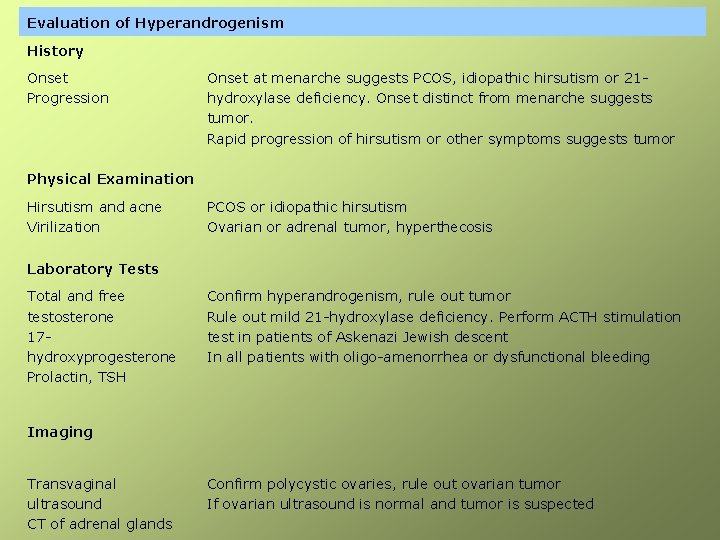
Evaluation of Hyperandrogenism History Onset Progression Onset at menarche suggests PCOS, idiopathic hirsutism or 21 hydroxylase deficiency. Onset distinct from menarche suggests tumor. Rapid progression of hirsutism or other symptoms suggests tumor Physical Examination Hirsutism and acne Virilization PCOS or idiopathic hirsutism Ovarian or adrenal tumor, hyperthecosis Laboratory Tests Total and free testosterone 17 hydroxyprogesterone Prolactin, TSH Confirm hyperandrogenism, rule out tumor Rule out mild 21 -hydroxylase deficiency. Perform ACTH stimulation test in patients of Askenazi Jewish descent In all patients with oligo-amenorrhea or dysfunctional bleeding Imaging Transvaginal ultrasound CT of adrenal glands Confirm polycystic ovaries, rule out ovarian tumor If ovarian ultrasound is normal and tumor is suspected
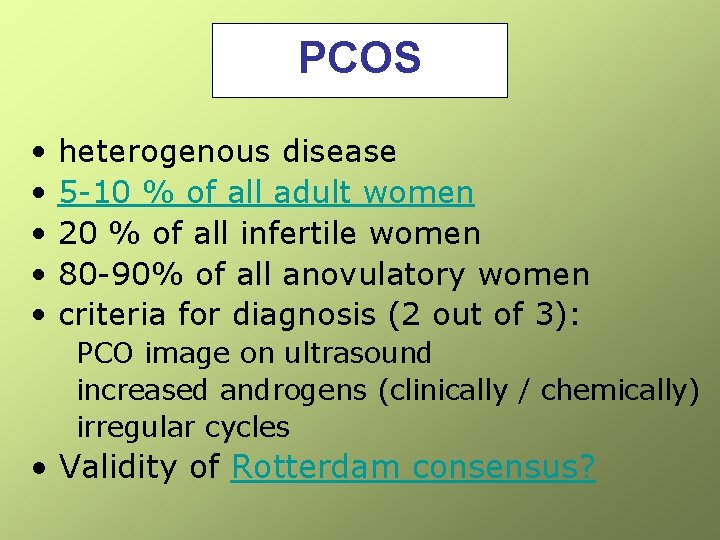
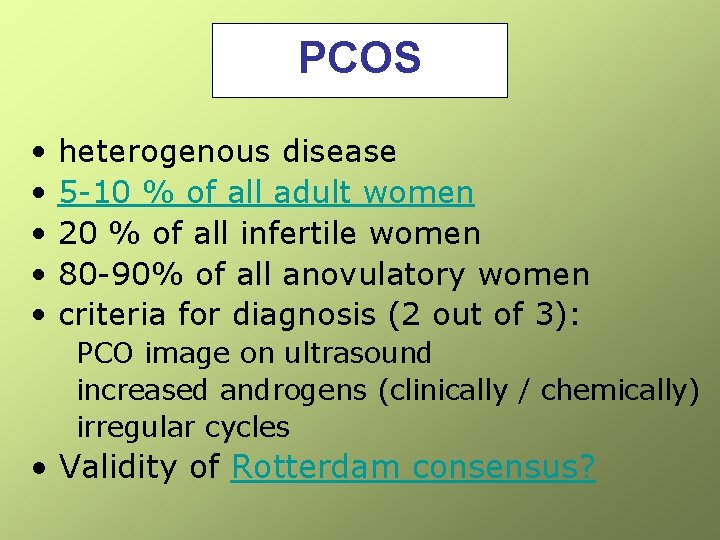
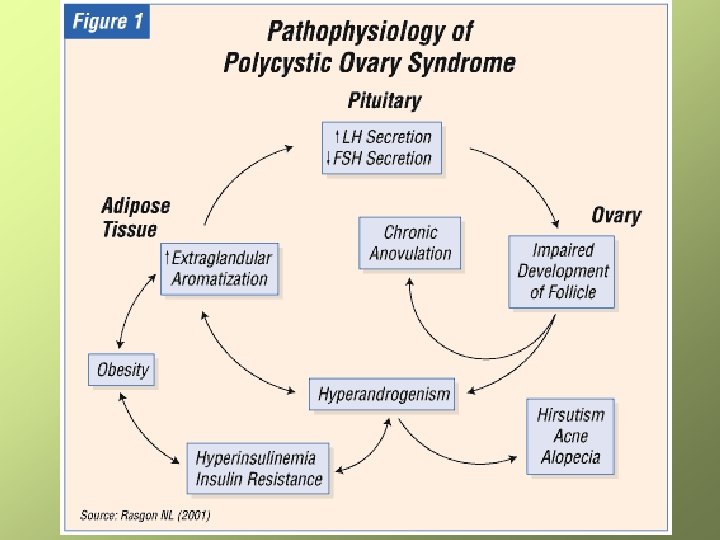
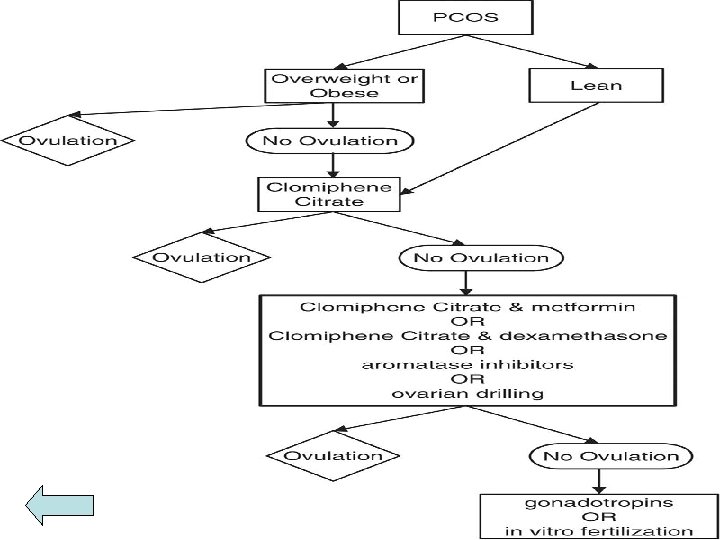
PCOS • heterogenous disease • 5 -10 % of all adult women • 20 % of all infertile women • 80 -90% of all anovulatory women • criteria for diagnosis (2 out of 3): PCO image on ultrasound increased androgens (clinically / chemically) irregular cycles • Validity of Rotterdam consensus?
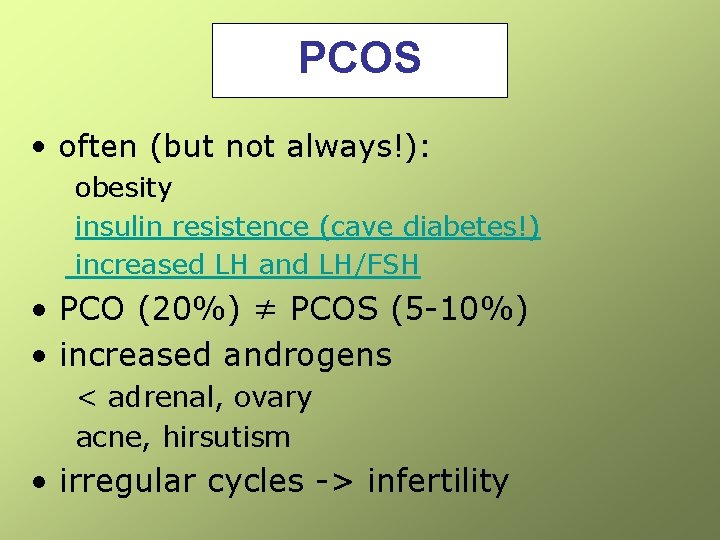
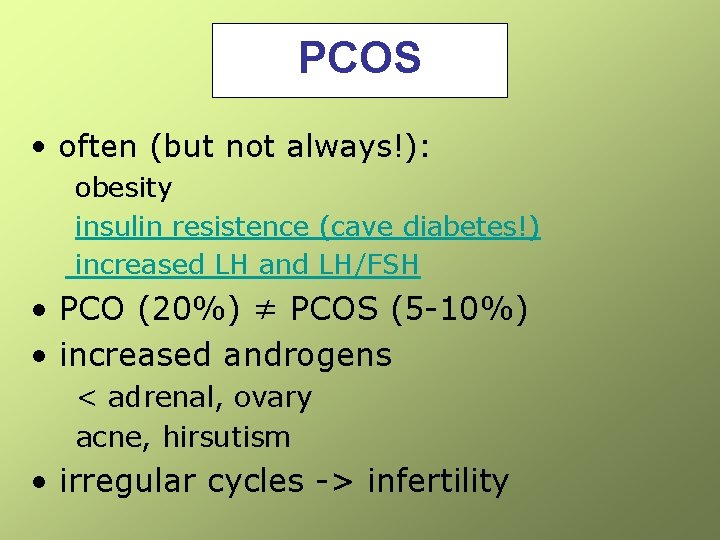
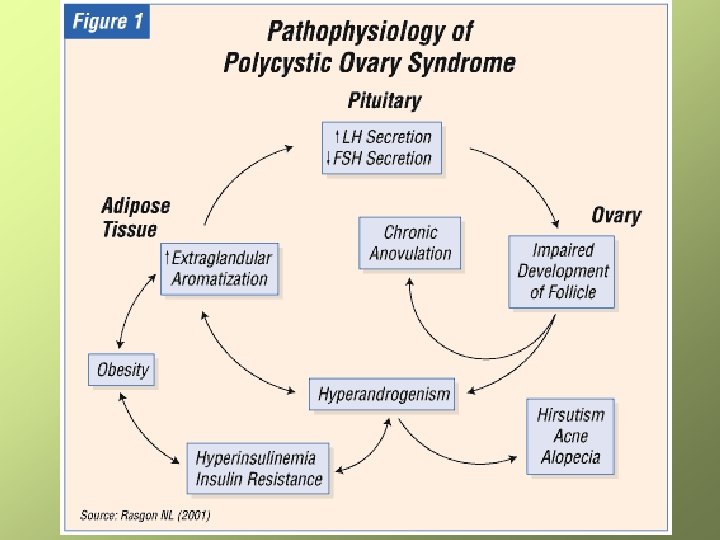
PCOS • often (but not always!): obesity insulin resistence (cave diabetes!) increased LH and LH/FSH • PCO (20%) ≠ PCOS (5 -10%) • increased androgens < adrenal, ovary acne, hirsutism • irregular cycles -> infertility
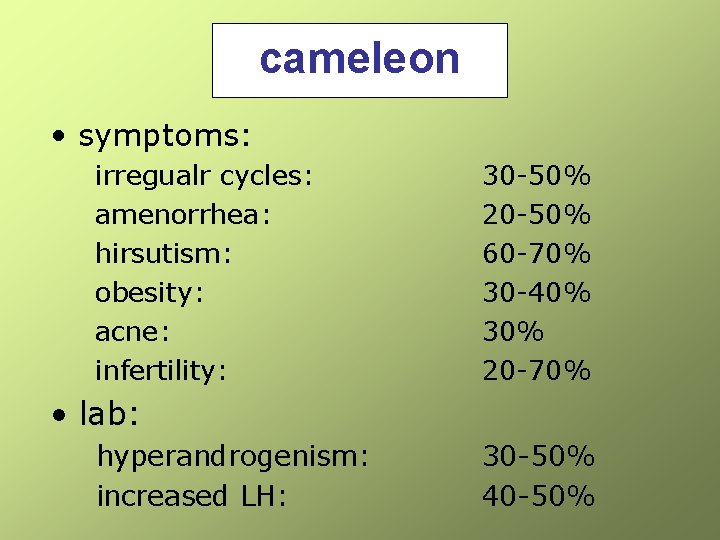
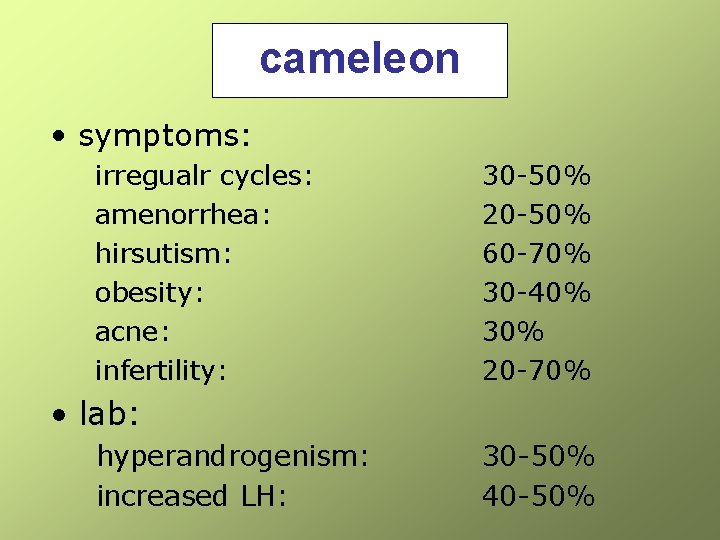
cameleon • symptoms: irregualr cycles: amenorrhea: hirsutism: obesity: acne: infertility: 30 -50% 20 -50% 60 -70% 30 -40% 30% 20 -70% • lab: hyperandrogenism: increased LH: 30 -50% 40 -50%
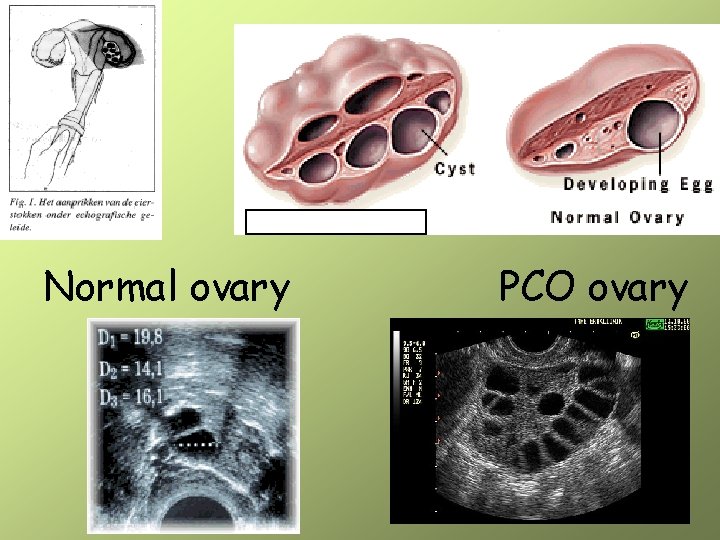
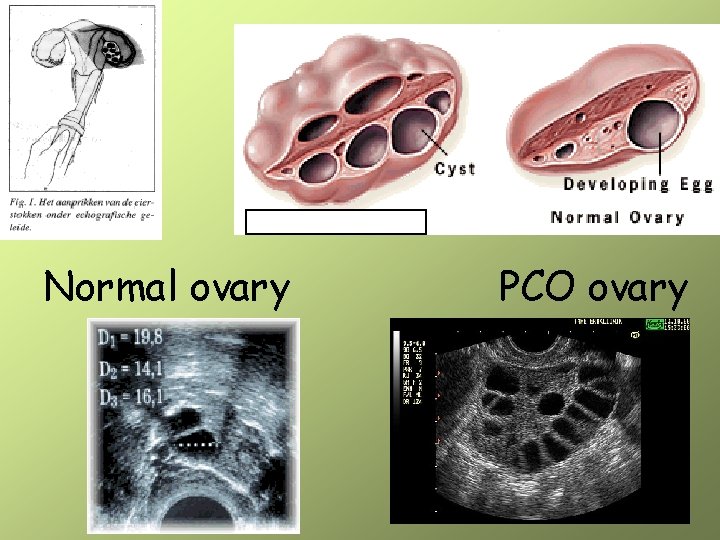
Normal ovary PCO ovary
Prevalence • genetic factors: families, twins insulin? Hormone receptors? exogeneous factors • racial factors Genetic? Food? Surroundings? Asian > mediterranean > Caucasian women
Short term problems • obesity, acne and hirsutism -> cosmetic problem, psychologic problems, low self image, depression • irregular cycles -> infertility • during pregnancy increased risk for miscarriage increased risk for pregnancy diabetes and hypertension
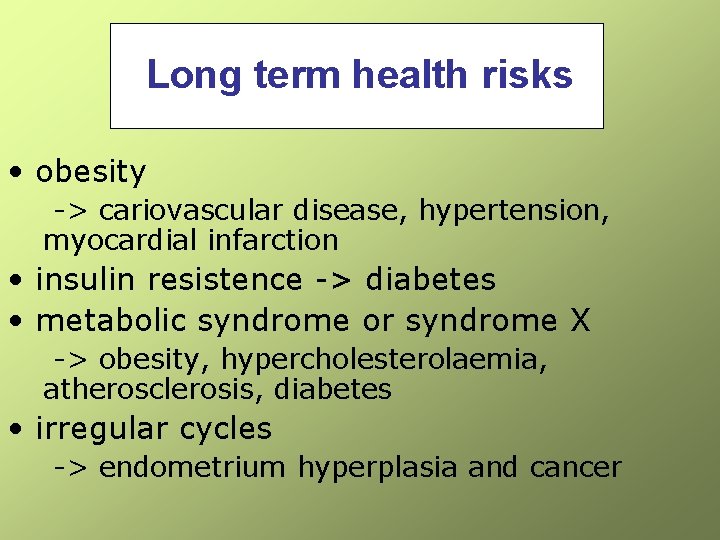
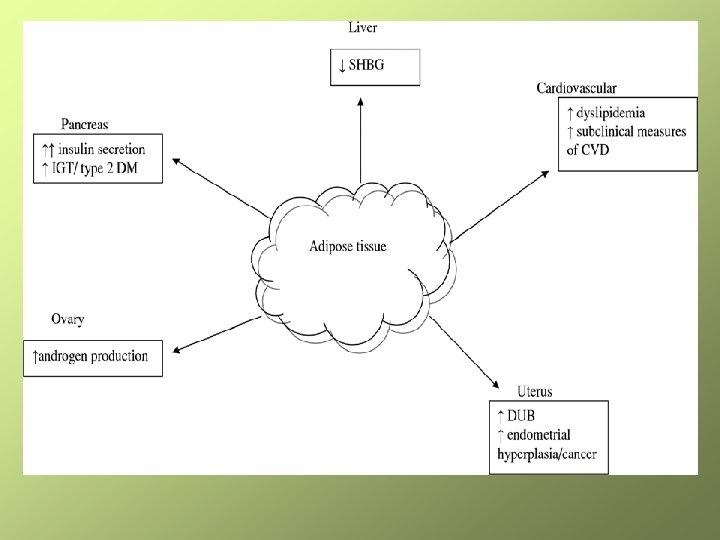
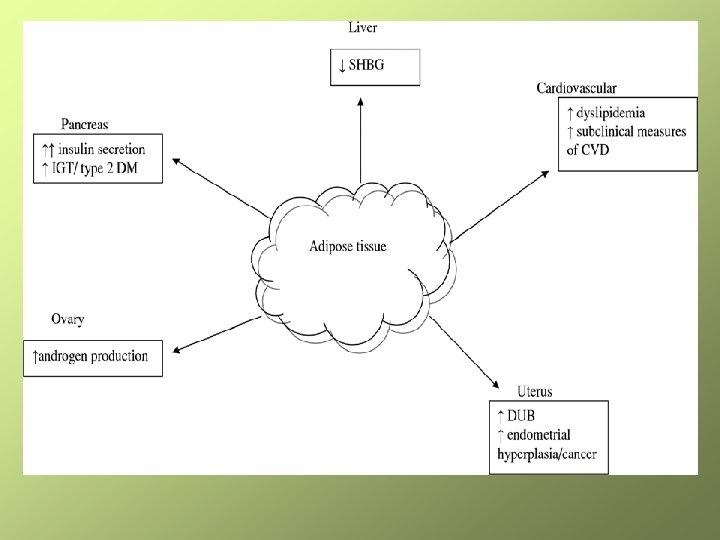
Long term health risks • obesity -> cariovascular disease, hypertension, myocardial infarction • insulin resistence -> diabetes • metabolic syndrome or syndrome X -> obesity, hypercholesterolaemia, atherosclerosis, diabetes • irregular cycles -> endometrium hyperplasia and cancer

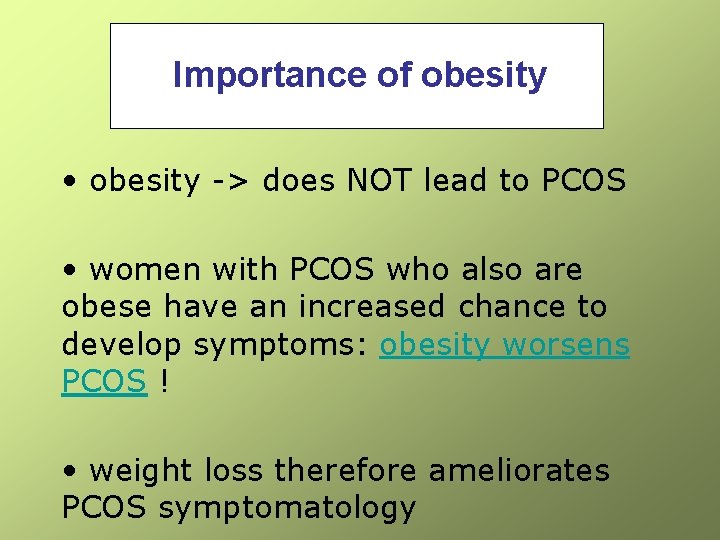
Importance of obesity • obesity -> does NOT lead to PCOS • women with PCOS who also are obese have an increased chance to develop symptoms: obesity worsens PCOS ! • weight loss therefore ameliorates PCOS symptomatology
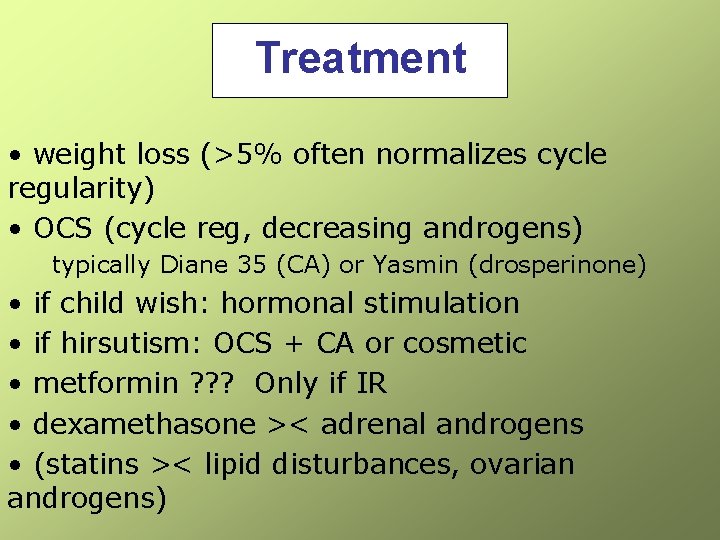
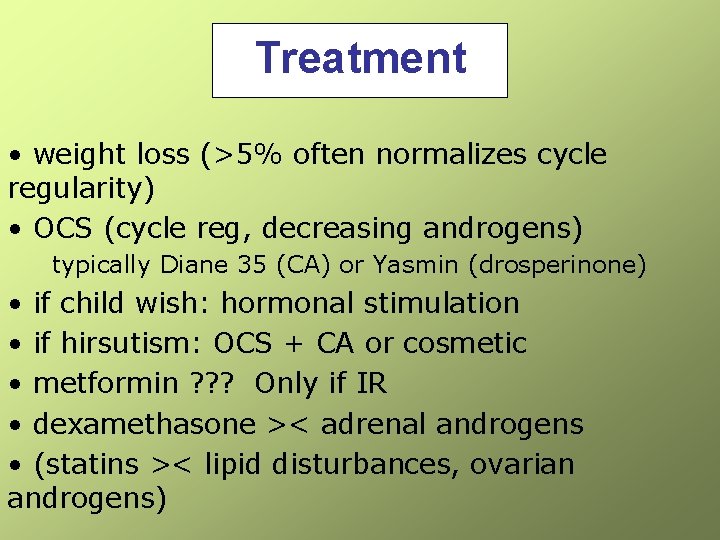
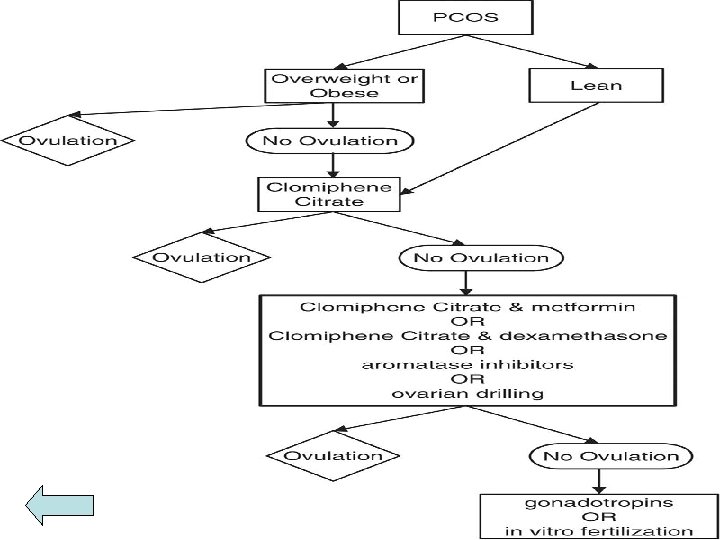
Treatment • weight loss (>5% often normalizes cycle regularity) • OCS (cycle reg, decreasing androgens) typically Diane 35 (CA) or Yasmin (drosperinone) • if child wish: hormonal stimulation • if hirsutism: OCS + CA or cosmetic • metformin ? ? ? Only if IR • dexamethasone >< adrenal androgens • (statins >< lipid disturbances, ovarian androgens)
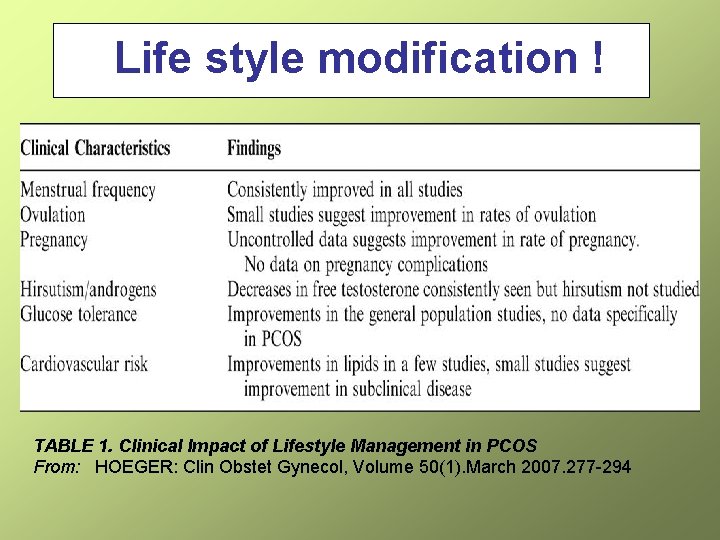
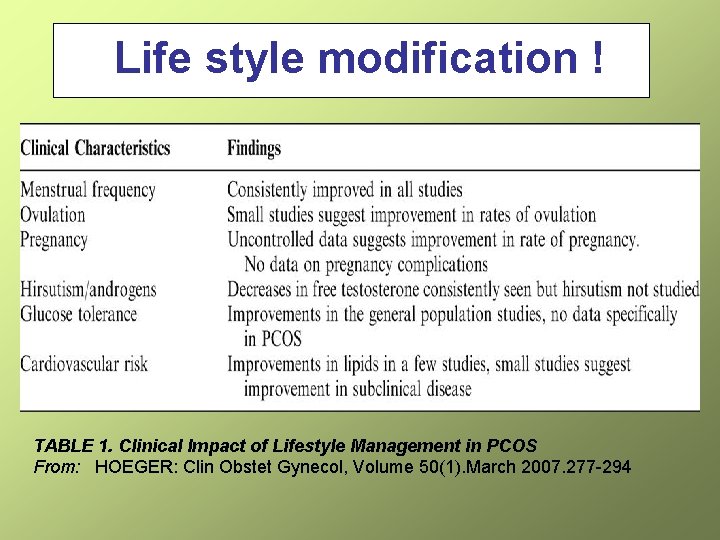
Life style modification ! TABLE 1. Clinical Impact of Lifestyle Management in PCOS From: HOEGER: Clin Obstet Gynecol, Volume 50(1). March 2007. 277 -294
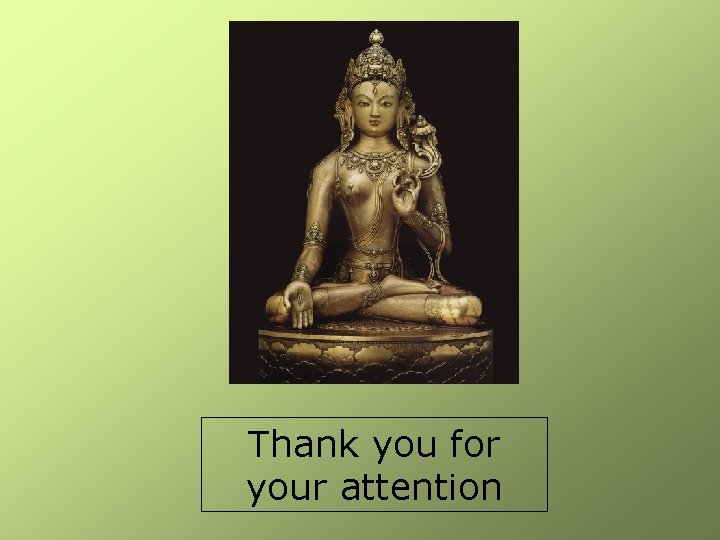
Thank you for your attention