Clinical Features and Evaluation COPD Dr Mazen Qusaibaty
Clinical Features and Evaluation COPD Dr Mazen Qusaibaty MD, DIS / Head Pulmonary and Internist Department Ibnalnafisse Hospital Ministry of Syrian health Email: qusaibaty@gmail. com
Smoking and inhalational exposure history
3 Smoking and inhalational exposure history • The most important risk factor for (COPD) ¶Cigarette Smoking
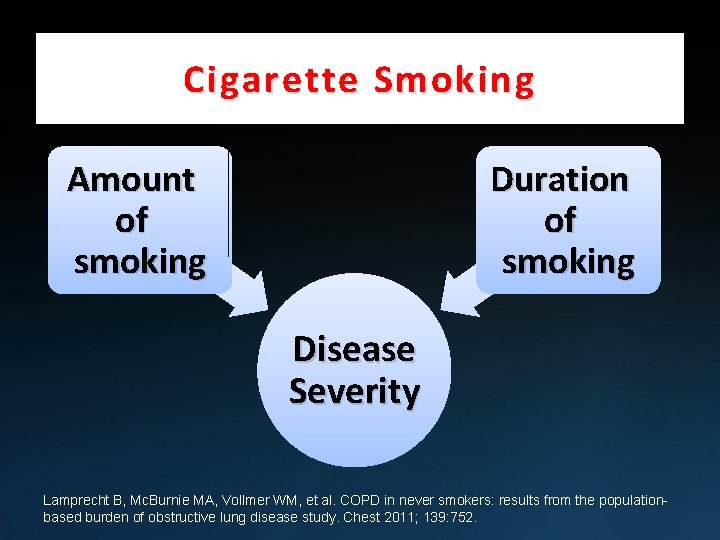
Cigarette Smoking Amount of smoking Duration of smoking Disease Severity Lamprecht B, Mc. Burnie MA, Vollmer WM, et al. COPD in never smokers: results from the populationbased burden of obstructive lung disease study. Chest 2011; 139: 752.
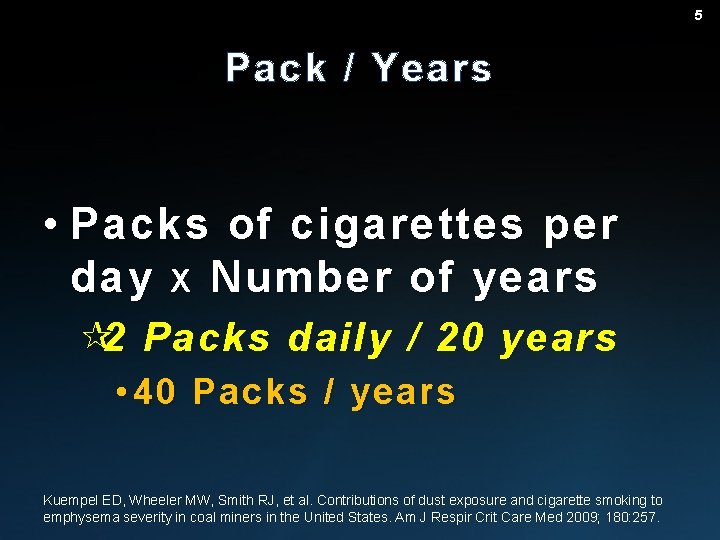
5 Pack / Years • Packs of cigarettes per day X Number of years ¶ 2 Packs daily / 20 years • 40 Packs / years Kuempel ED, Wheeler MW, Smith RJ, et al. Contributions of dust exposure and cigarette smoking to emphysema severity in coal miners in the United States. Am J Respir Crit Care Med 2009; 180: 257.
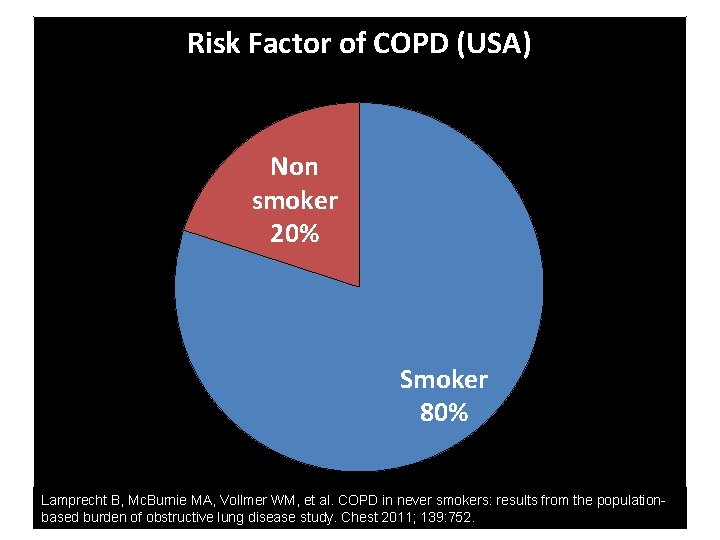
Risk Factor of COPD (USA) Non smoker 20% Smoker 80% Lamprecht B, Mc. Burnie MA, Vollmer WM, et al. COPD in never smokers: results from the populationbased burden of obstructive lung disease study. Chest 2011; 139: 752.
Nonsmoker COPD 7
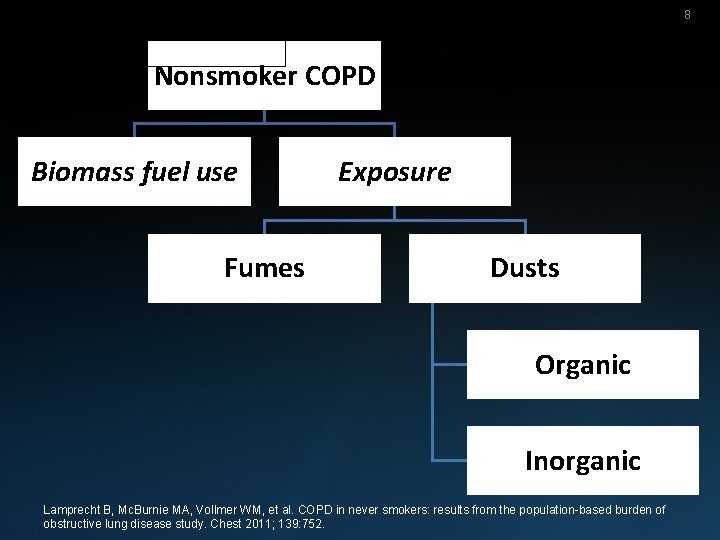
8 Nonsmoker COPD Biomass fuel use Fumes Exposure Dusts Organic Inorganic Lamprecht B, Mc. Burnie MA, Vollmer WM, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 2011; 139: 752.
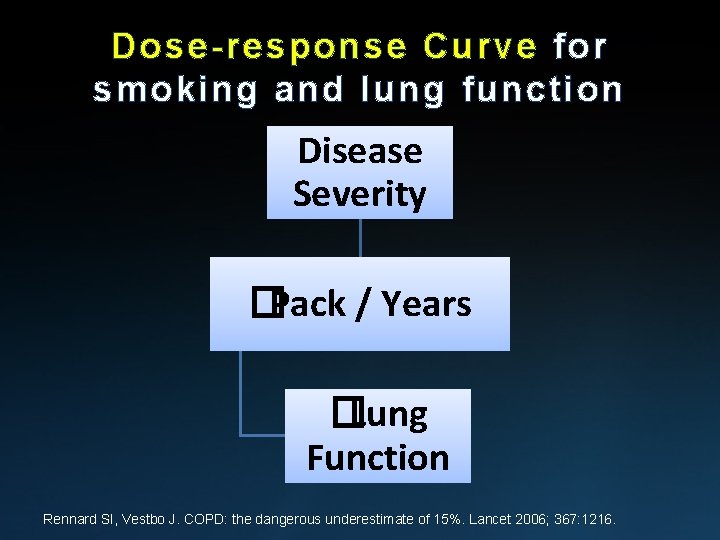
Dose-response Curve for smoking and lung function Disease Severity �Pack / Years �Lung Function Rennard SI, Vestbo J. COPD: the dangerous underestimate of 15%. Lancet 2006; 367: 1216.
10 Dose-response Curve for smoking and lung function • Some Individuals • Severe disease with fewer pack years • Minimal to no symptoms despite many pack years Rennard SI, Vestbo J. COPD: the dangerous underestimate of 15%. Lancet 2006; 367: 1216.
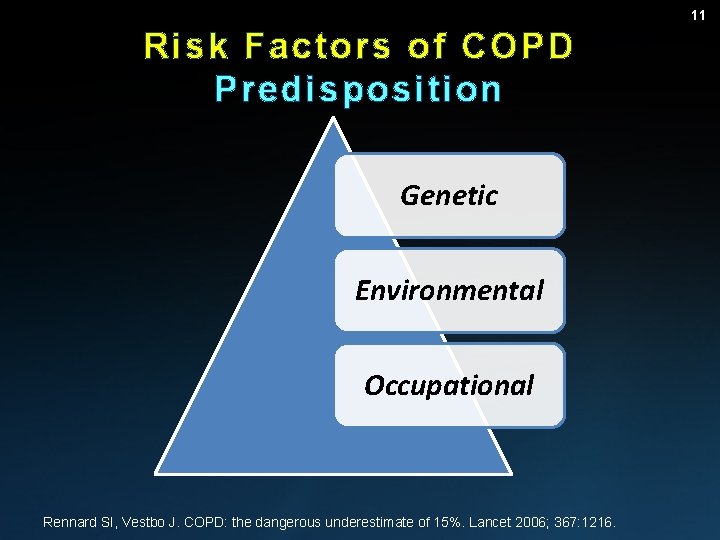
11 Risk Factors of COPD Predisposition Genetic Environmental Occupational Rennard SI, Vestbo J. COPD: the dangerous underestimate of 15%. Lancet 2006; 367: 1216.
12 Summary • Smoking < 10 to 15 pack years of cigarettes ¶Unlikely �COPD Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med 2011; 155: 179.
13 Summary • >40 pack years of smoking ¶Likely �COPD Simel D, Rennie D. The rational clinical examination: Evidence-based clinical diagnosis, Mc. Graw Hill. (Ed), New York 2008.
14 A history of Asthma should also be sought • Asthma may progress to fixed airflow limitation � COPD Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988 -1994. Arch Intern Med 2000; 160: 1683.
Symptoms and Pattern of Onset
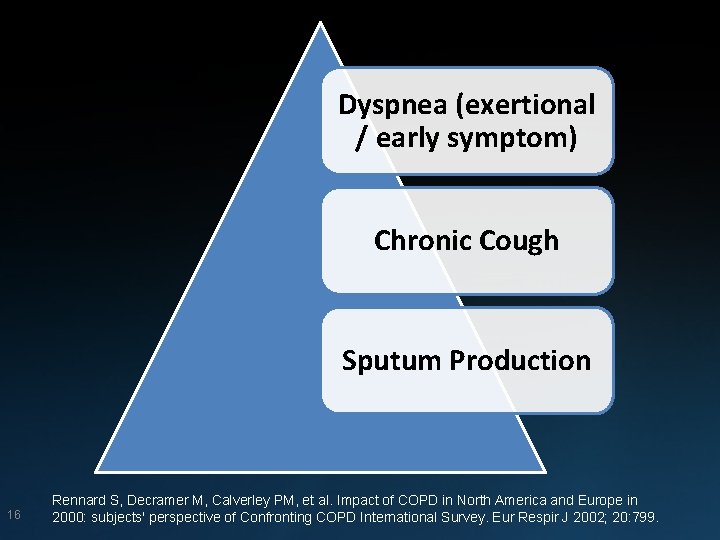
Dyspnea (exertional / early symptom) Chronic Cough Sputum Production 16 Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
17 Less common symptoms… • • Wheezing Chest tightness Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
There are three typical ways in which patients with COPD present
Group 01: Patients who have an extremely sedentary lifestyle Inaccurate assessment of the Exertional Dyspnea Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
Group 01: Patients who have an extremely sedentary lifestyle Few complaints require careful questioning Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
Group 01: Inaccurate assessment of the Exertional Dyspnea Giving another explanation: • Heart • Obesity
Group 2 • Patients who present with respiratory symptoms generally complain of: ¶Dyspnea ¶Chronic cough Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2 2000: 2 subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
23 The dyspnea • The dyspnea may initially be noticed only during exertion Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
24 The chronic cough • Insidious onset of sputum production • Occurs in the morning initially • Progress to occur throughout the day Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
25 The chronic cough • The daily volume rarely exceeds 60 m. L. • The sputum is usually mucoid , but becomes purulent During exacerbations Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799.
26 Group 03 • Patients who present with episodes of: ¶Increased cough ¶Purulent Sputum ¶Wheezing ¶Fatigue ¶Dyspnea that occur intermittently, with or without fever Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J 2011; 37: 264
Group 03 – Episodic Symptoms • Diseases that mimics COPD ¶Asthma ¶Heart Failure ¶Bronchiectasis ¶Bronchiolitis Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J 2011; 37: 264 27
28 In General • Approximately 62 percent of patients with moderate to severe COPD report variability in symptoms (eg, dyspnea, cough, sputum, wheezing, or chest tightness) over the course of the day or week-to-week Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European crosssectional study. Eur Respir J 2011; 37: 264
29 In General Morning is typically the worst time of day
30 Patients with COPD … • Weight gain ¶D ue to activity limitations
31 Patients with COPD … • The majority of COPD patients are overweight or obese
32 Patients with COPD … • Weight loss ¶Possibly due to dyspnea while eating
33 Patients with COPD … • Limitation of activity
34 Patients with COPD … • Cough syncope • Feelings of depression or anxiety
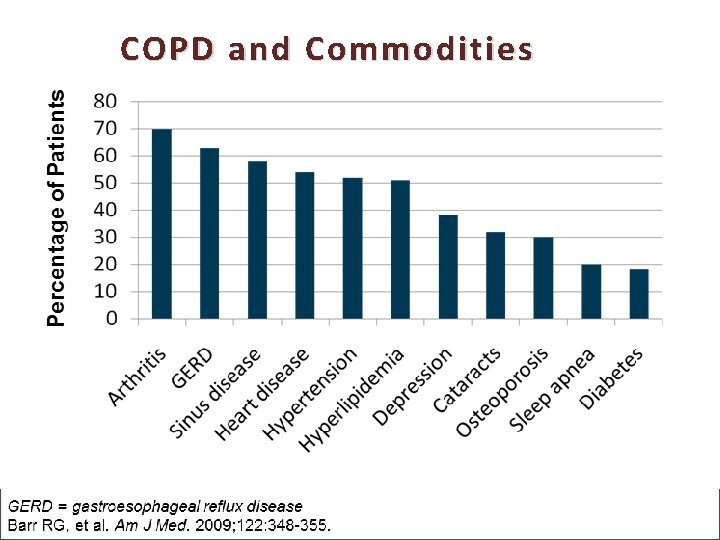
COPD and Commodities
36 Physical Examination
37 Physical Examination • Early in the disease ¶The physical examination may be normal or ¶May show only prolonged expiration or wheezes on forced exhalation Badgett RG, Tanaka DJ, Hunt DK, et al. Can moderate chronic obstructive pulmonary disease be diagnosed by historical and physical findings alone? Am J Med 1993; 94: 188.
38 As the severity of the airway obstruction increases • Hyperinflation �Resonance to percussion �Breath sounds • Wheezes • Crackles at the lung bases • Heart sounds are very distant Badgett RG, Tanaka DJ, Hunt DK, et al. Can moderate chronic obstructive pulmonary disease be diagnosed by historical and physical findings alone? Am J Med 1993; 94: 188.
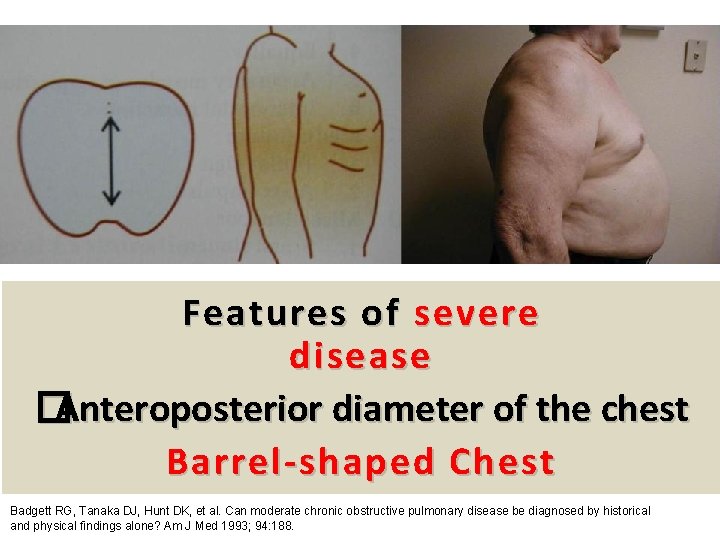
39 Features of severe disease �Anteroposterior diameter of the chest Barrel-shaped Chest Badgett RG, Tanaka DJ, Hunt DK, et al. Can moderate chronic obstructive pulmonary disease be diagnosed by historical and physical findings alone? Am J Med 1993; 94: 188.
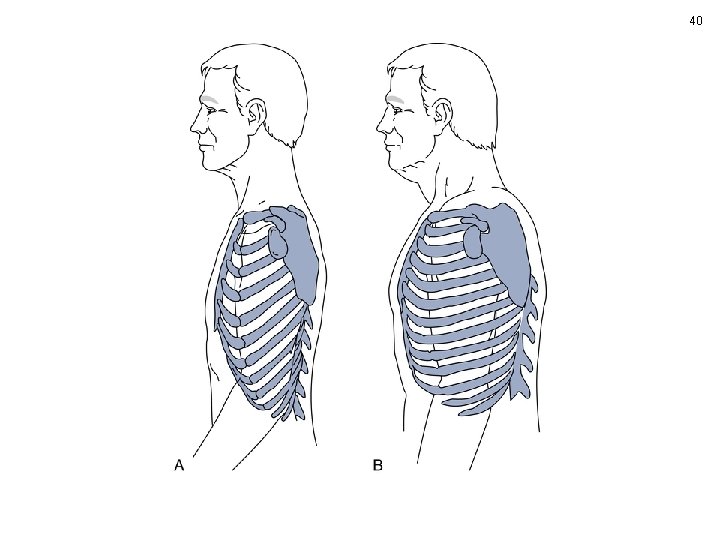
40
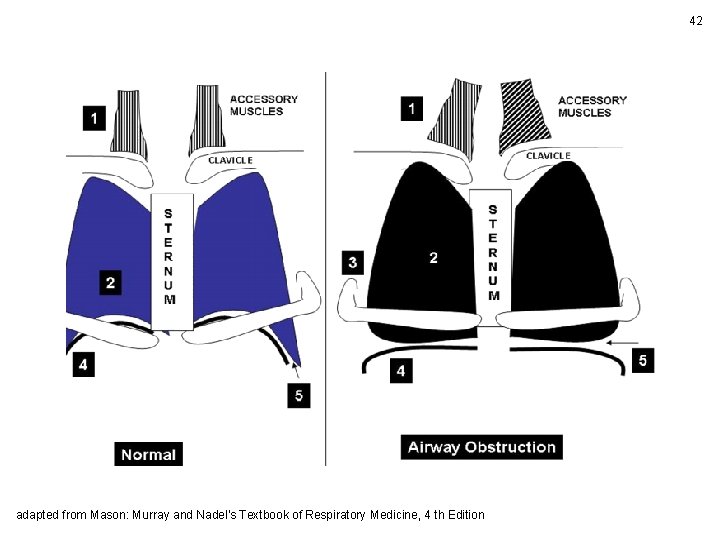
42 adapted from Mason: Murray and Nadel's Textbook of Respiratory Medicine, 4 th Edition

43 Lemyze M, Bart F. Hoover sign. CMAJ 2011; 183: E 133.
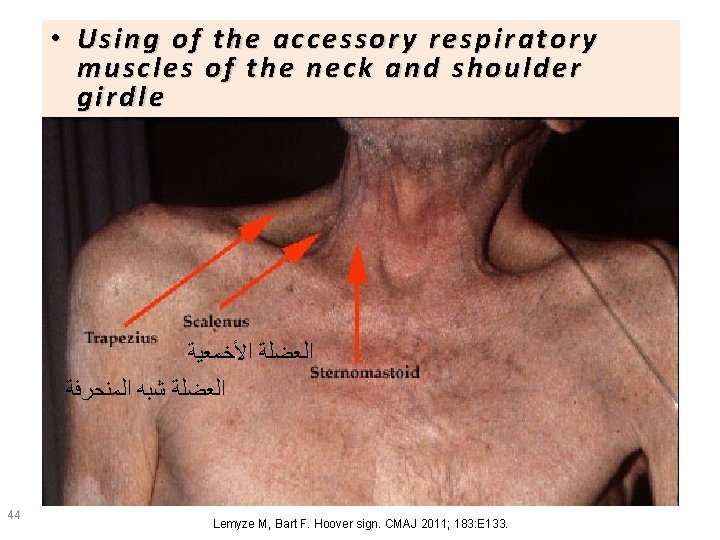
• Using of the accessory respir atory respira tory muscle muscl ess of the neck and shoulder shoul der girdle gi rdl e ﺍﻟﻌﻀﻠﺔ ﺍﻷﺨﻤﻌﻴﺔ ﺍﻟﻌﻀﻠﺔ ﺷﺒﻪ ﺍﻟﻤﻨﺤﺮﻓﺔ 44 Lemyze M, Bart F. Hoover sign. CMAJ 2011; 183: E 133.
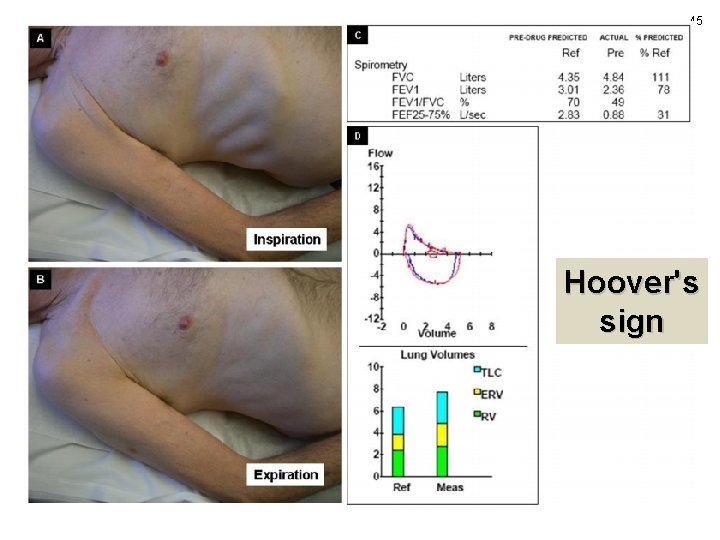
45 Hoover's sign

46 Garcia-Pachon E, Padilla-Navas I. Frequency of Hoover's sign in stable patients with chronic obstructive pulmonary disease. Int J Clin Pract 2006; 60: 514
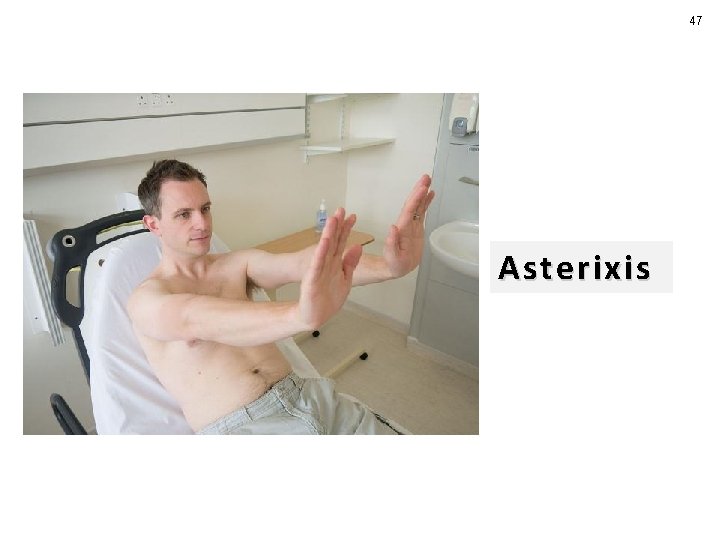
47 Asterixis
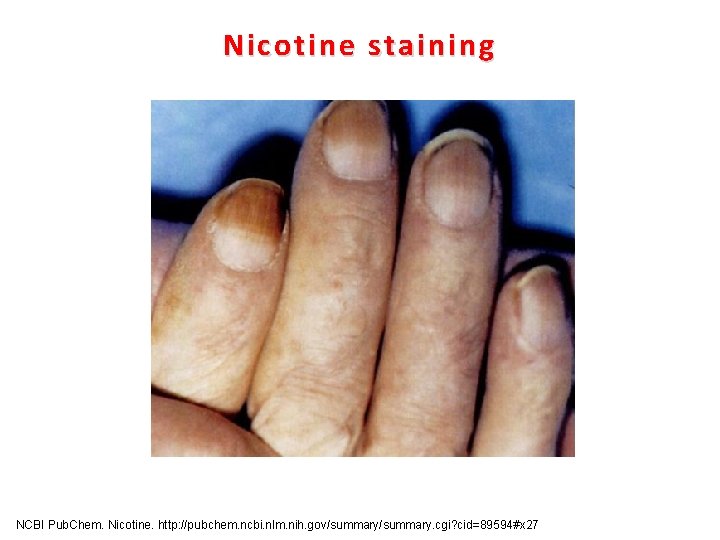
Nicotine staining NCBI Pub. Chem. Nicotine. http: //pubchem. ncbi. nlm. nih. gov/summary. cgi? cid=89594#x 27

Clubbing 49
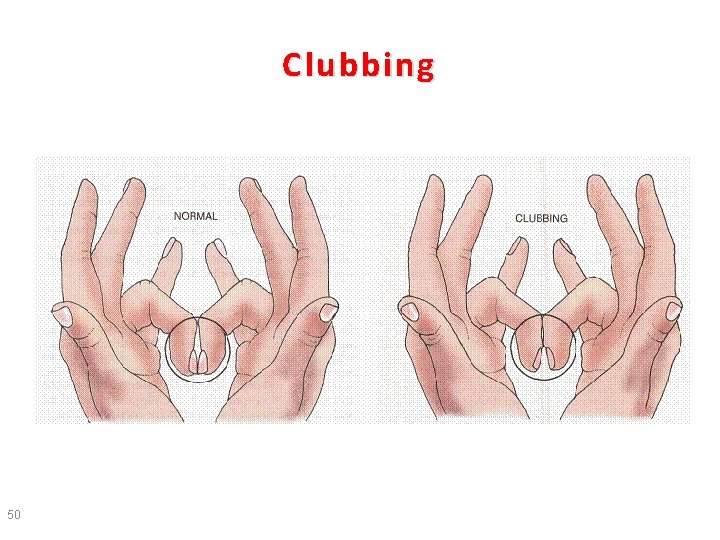
Clubbing 50
Evaluation
Laboratory 53
54 Laboratory • No laboratory test is diagnostic for COPD
55 Laboratory • Assessment for anemia is an important step in the evaluation of dyspnea
• Suspected Heart Failure ¶Measurement of • Plasma Brain Natriuretic Peptide ( BNP ) • or • N-terminal pro-BNP (NTpro. BNP) concentrations is useful 56
• Among stable COPD patients with normal kidney function ¶An elevated serum bicarbonate may indirectly identify chronic hypercapnia 57
58 Testing for alpha-1 antitrypsin (AAT) deficiency • The presence of emphysema in a young individual (eg, age ≤ 45 years ) • Emphysema in a nonsmoker or minimal smoker American Thoracic Society, European Respiratory Society. American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med 2003; 168: 818.
59 Testing for alpha-1 antitrypsin (AAT) deficiency • Emphysema characterized by predominantly basilar changes on the chest radiograph • A family history of emphysema American Thoracic Society, European Respiratory Society. American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med 2003; 168: 818.
60 Testing for alpha-1 antitrypsin (AAT) deficiency • A serum level of AAT ¶below 11 micromol/L (~57 mg/d. L by nephelometry ) in combination with a severe deficient genotype is diagnostic American Thoracic Society, European Respiratory Society. American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med 2003; 168: 818.
61 Pulmonary function tests
Airflow Limitation Spirometry
63 Spirometry • Spirometry should be performed in patients with suggestive symptoms Oh YM, Bhome AB, Boonsawat W, et al. Characteristics of stable chronic obstructive pulmonary disease patients in the pulmonology clinics of seven Asian cities. Int J Chron Obstruct Pulmon Dis 2013; 8: 31
64 Spirometry • Spirometry is performed pre and post bronchodilator administration (eg, inhalation of Salbutamol 400 mcg )
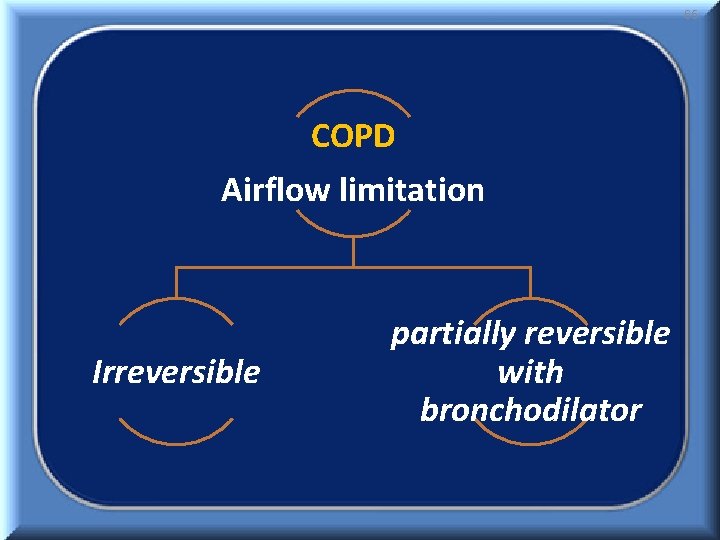
65 COPD Airflow limitation Irreversible partially reversible with bronchodilator
66 Classification of Severity of Airflow Limitation in COPD
67 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted
68 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade GOLD 4 GOLD 3 GOLD 2 GOLD 1
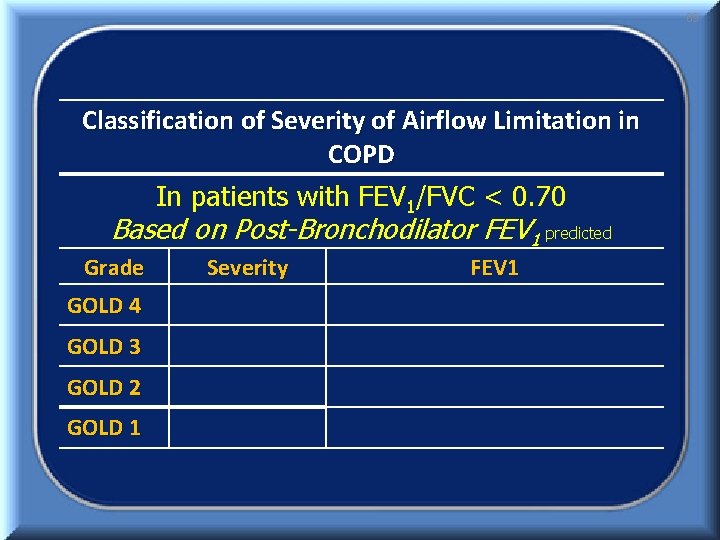
69 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade GOLD 4 GOLD 3 GOLD 2 GOLD 1 Severity FEV 1
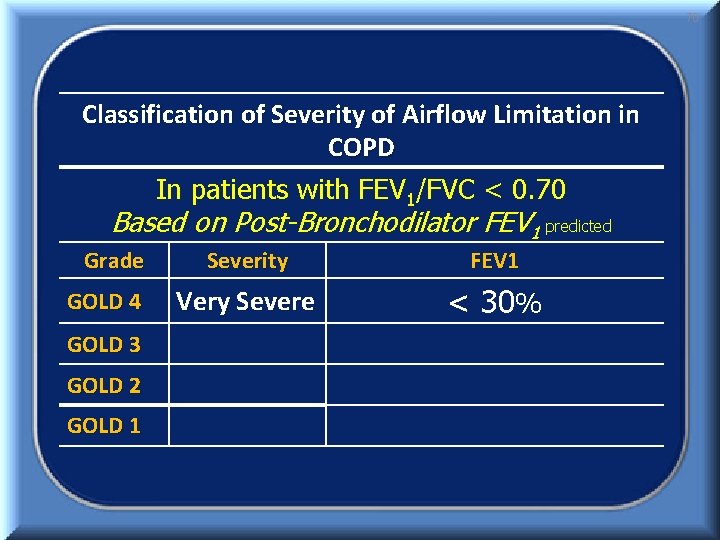
70 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade GOLD 4 GOLD 3 GOLD 2 GOLD 1 Severity FEV 1 Very Severe < 30%
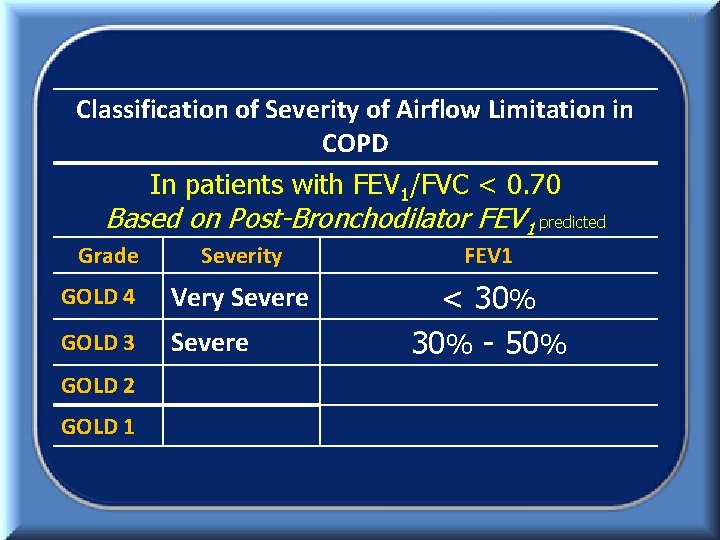
71 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade Severity FEV 1 GOLD 4 Very Severe GOLD 3 Severe < 30% - 50% GOLD 2 GOLD 1
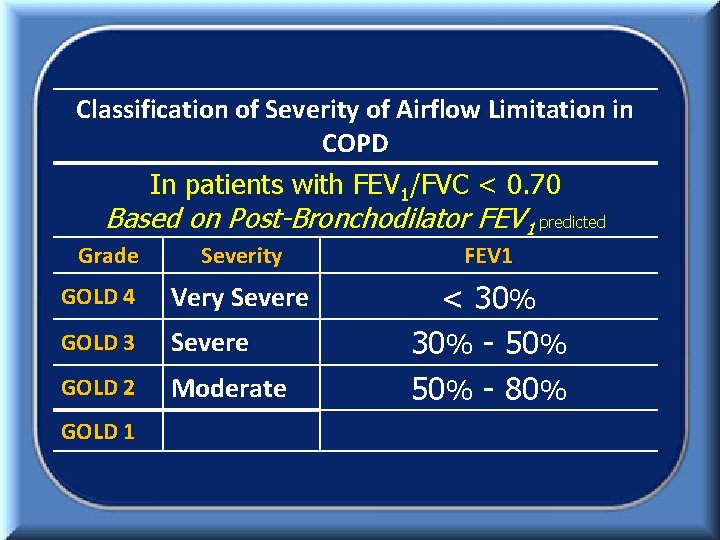
72 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade Severity FEV 1 GOLD 4 Very Severe GOLD 3 Severe GOLD 2 Moderate < 30% - 50% - 80% GOLD 1
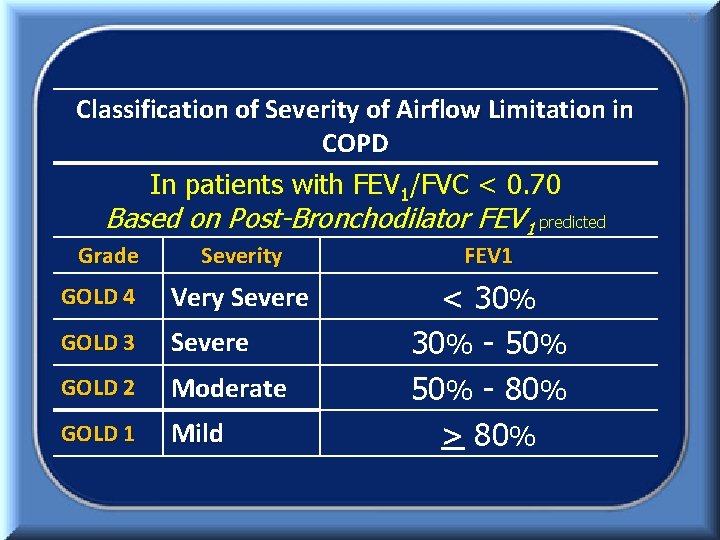
73 Classification of Severity of Airflow Limitation in COPD In patients with FEV 1/FVC < 0. 70 Based on Post-Bronchodilator FEV 1 predicted Grade Severity FEV 1 GOLD 4 Very Severe GOLD 3 Severe GOLD 2 Moderate GOLD 1 Mild < 30% - 50% - 80% > 80%
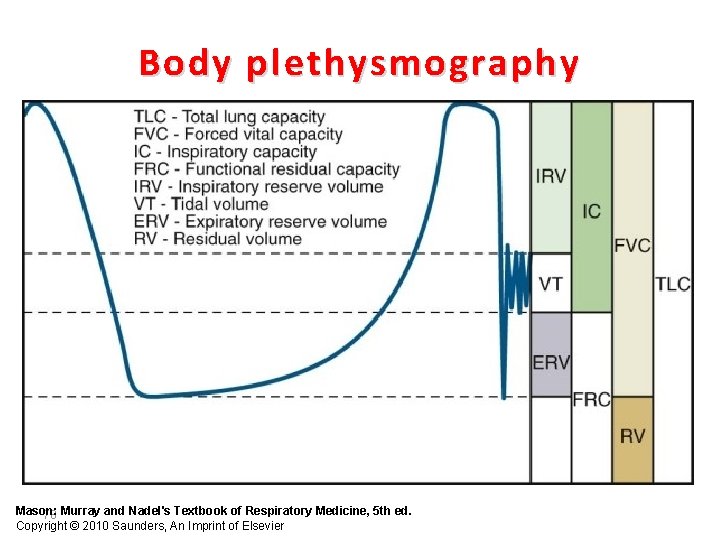
Body plethysmography Mason: 78 Murray and Nadel's Textbook of Respiratory Medicine, 5 th ed. Copyright © 2010 Saunders, An Imprint of Elsevier
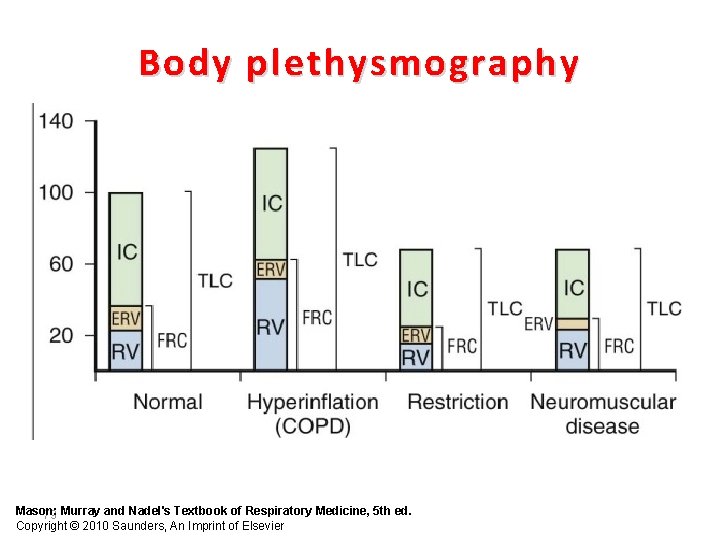
Body plethysmography Mason: 79 Murray and Nadel's Textbook of Respiratory Medicine, 5 th ed. Copyright © 2010 Saunders, An Imprint of Elsevier
At rest Healthy Adulte Images by courtesy of Dr. de Zeeuw, Wuppertal Fixed airway obstruction
During Exercise Healthy Adulte Images by courtesy of Dr. de Zeeuw, Wuppertal Fixed airway obstruction COPD
Diffusing capacity for carbon monoxide • Measurement of DLCO can help establish the presence of emphysema ¶But is not necessary for the routine diagnosis of COPD
84 • Pulse oximetry is a noninvasive • Easily performed test that assesses blood oxygen saturation
The indications for measuring ABGs • Low FEV 1 (eg, <50 percent predicted) • Low oxygen saturation by pulse oximetry (eg, <92 percent) • Depressed level of consciousness
The indications for measuring ABGs • Acute exacerbation of COPD • Assessment for hypercapnia in at risk patients 30 to 60 minutes after initiation of supplemental oxygen
• In patients with mild to moderate COPD ¶Arterial blood gases usually reveal mild or moderate hypoxemia without hypercapnia 87
• As the disease progresses, the hypoxemia becomes more severe and hypercapnia may develop 88
• Hypercapnia becomes progressively more likely ¶when the FEV 1 approaches or falls > one liter 89
• Blood gas abnormalities worsen during ¶Acute exacerbations ¶Exercise ¶Sleep 90
• Blood gas abnormalities worsen during ¶Acute exacerbations ¶Exercise ¶Sleep 91
Imaging
93 Chest radiography • Plain chest radiographs have a poor sensitivity for detecting COPD ¶Sensitivity of 50 percent
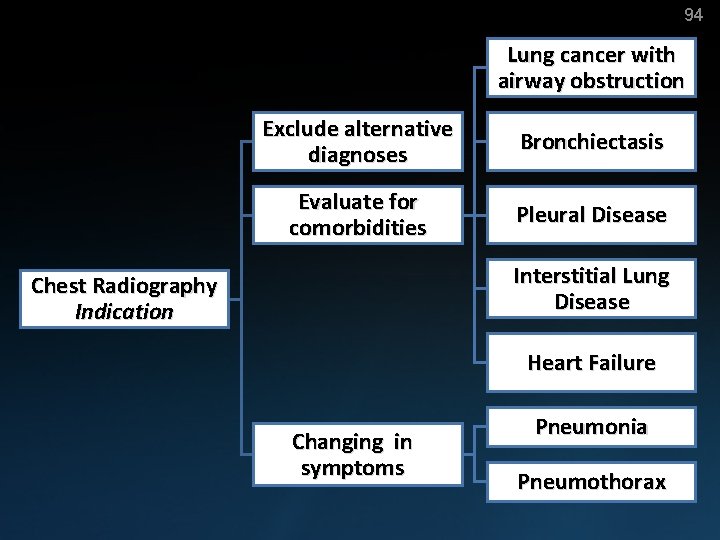
94 Lung cancer with airway obstruction Exclude alternative diagnoses Bronchiectasis Evaluate for comorbidities Pleural Disease Interstitial Lung Disease Chest Radiography Indication Heart Failure Changing in symptoms Pneumonia Pneumothorax
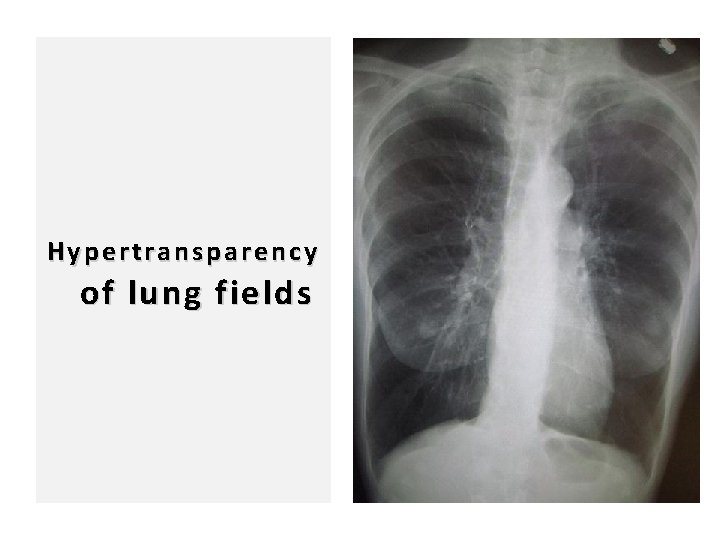
96 Hypertransparency of lung fields
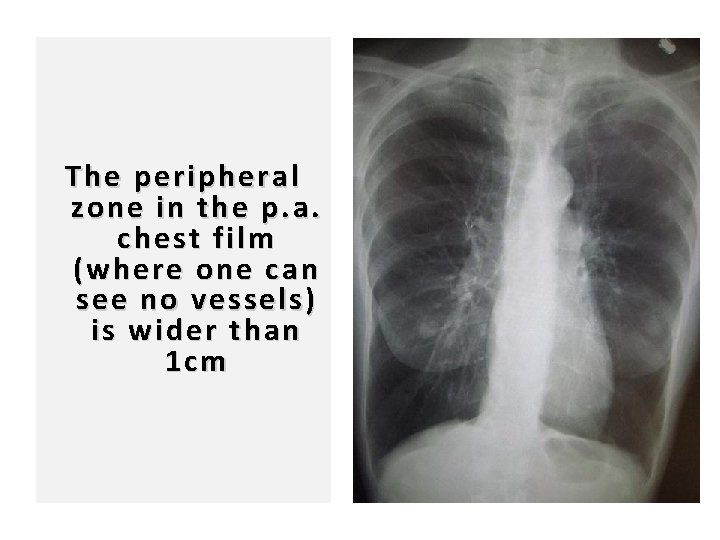
97 The peripheral zone in the p. a. chest film (where one can see no vessels) is wider than 1 cm
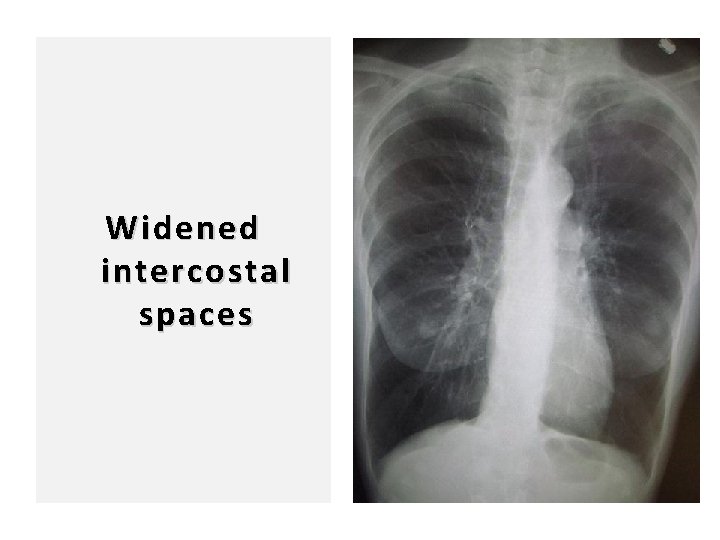
98 Widened intercostal spaces
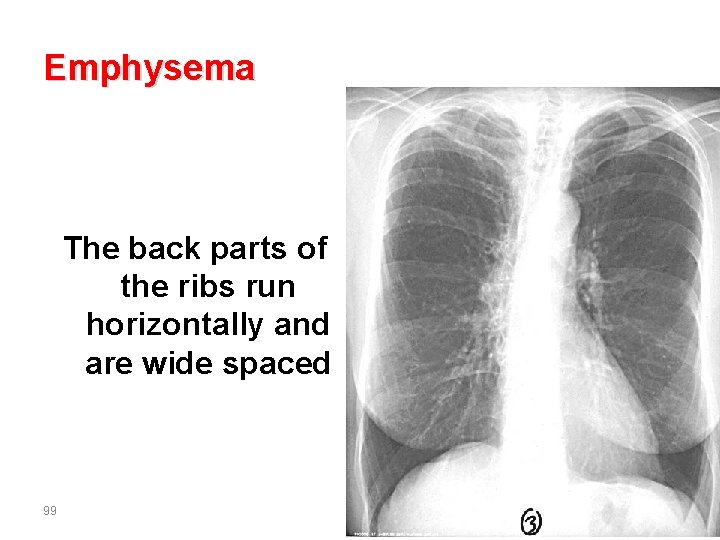
Emphysema The back parts of the ribs run horizontally and are wide spaced 99
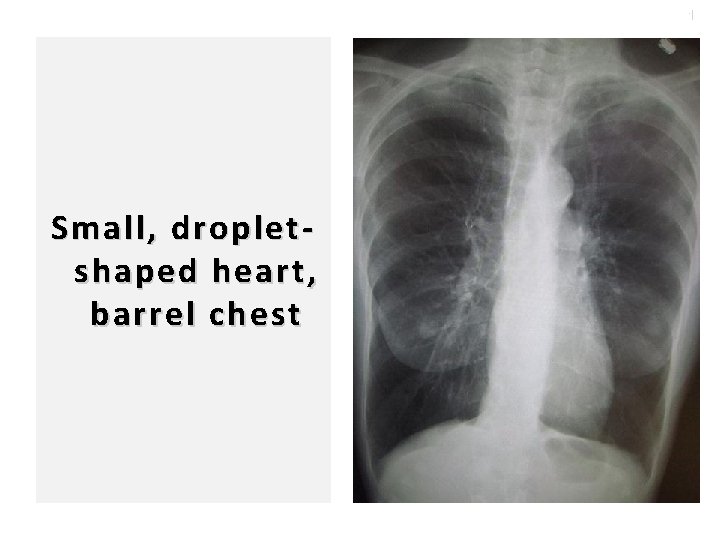
100 Small, dropletshaped heart, barrel chest
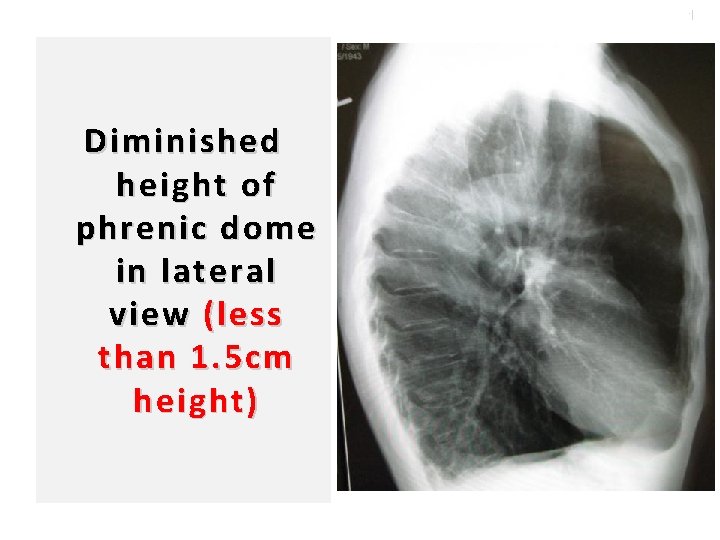
101 Diminished height of phrenic dome in lateral view (less than 1. 5 cm height)
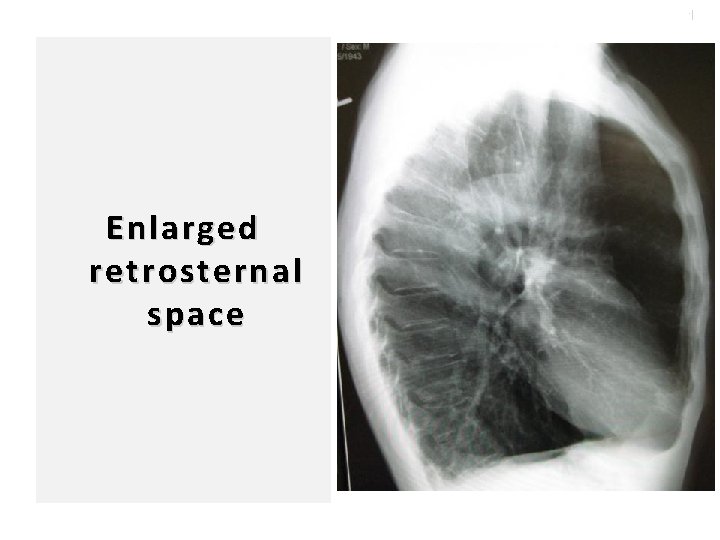
102 Enlarged retrosternal space
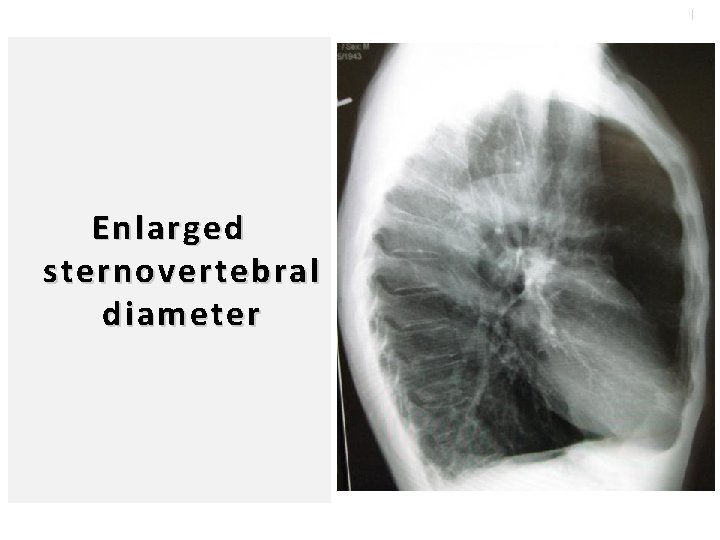
103 Enlarged sternovertebral diameter
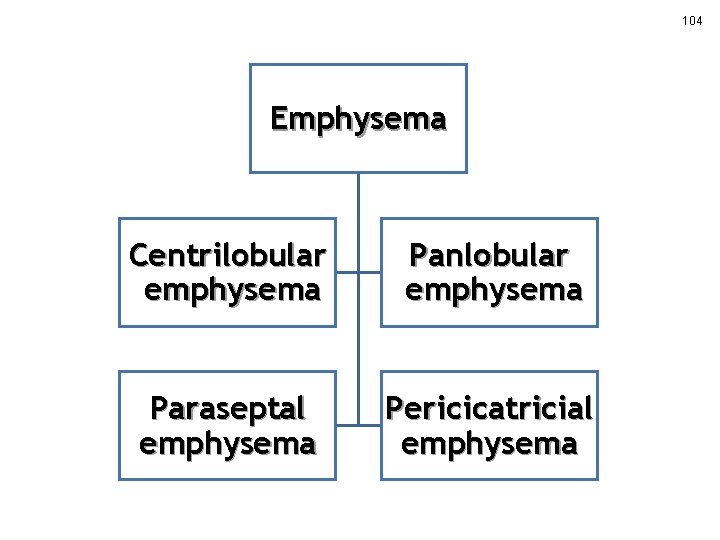
104 Emphysema Centrilobular emphysema Panlobular emphysema Paraseptal emphysema Pericicatricial emphysema
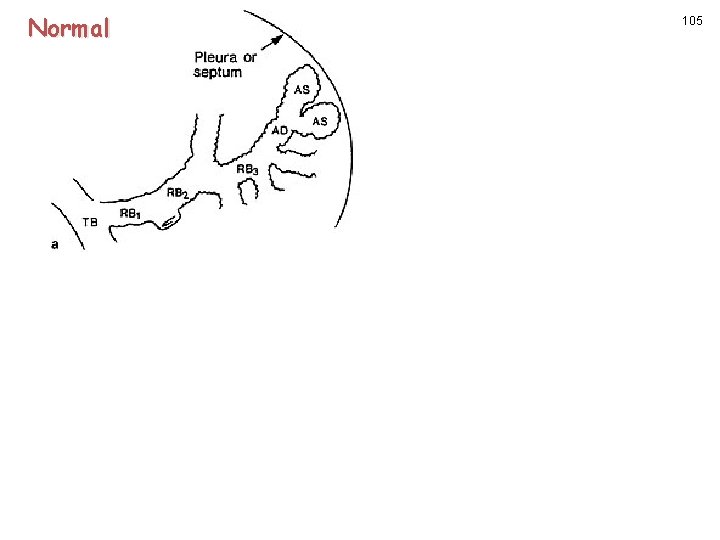
Normal 105
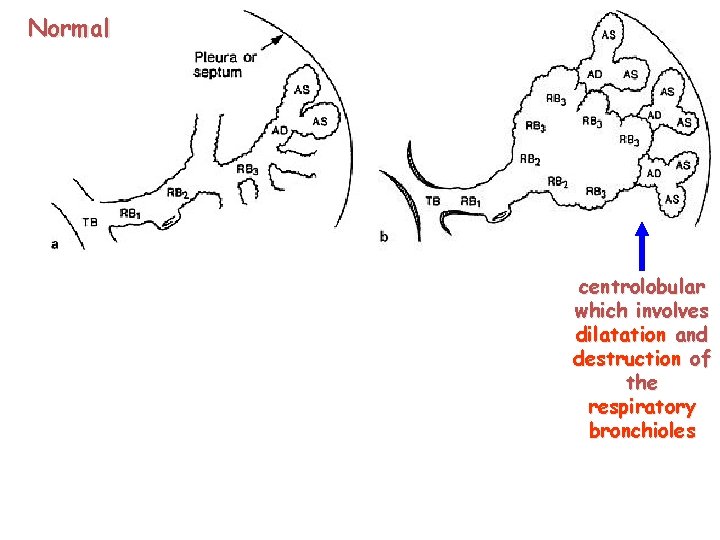
Normal 106 centrolobular which involves dilatation and destruction of the respiratory bronchioles
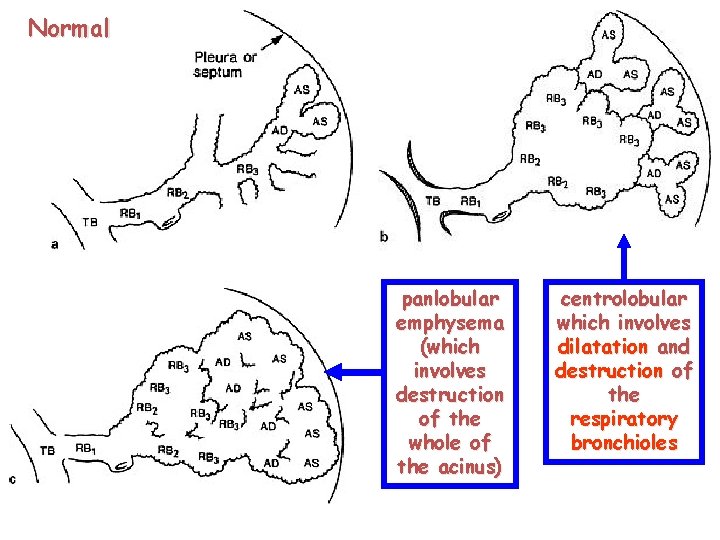
Normal 107 panlobular emphysema (which involves destruction of the whole of the acinus) centrolobular which involves dilatation and destruction of the respiratory bronchioles
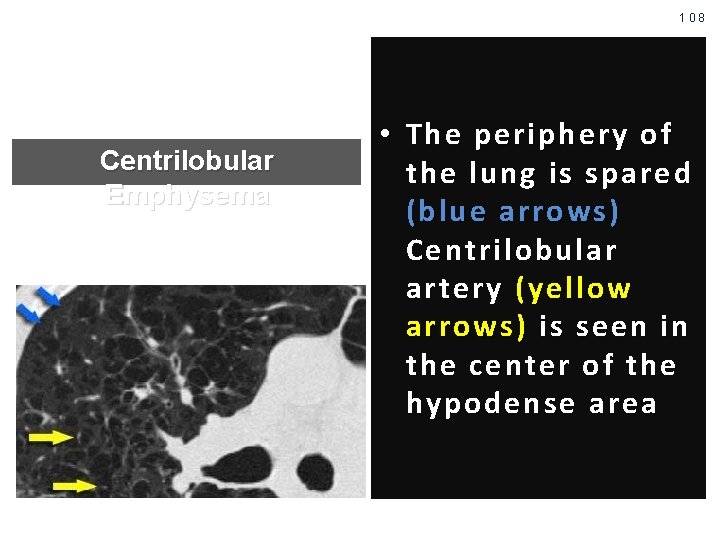
108 Centrilobular Emphysema • The periphery of the lung is spared (blue arrows ) Centrilobular artery (yellow arrows) is seen in the center of the hypodense area
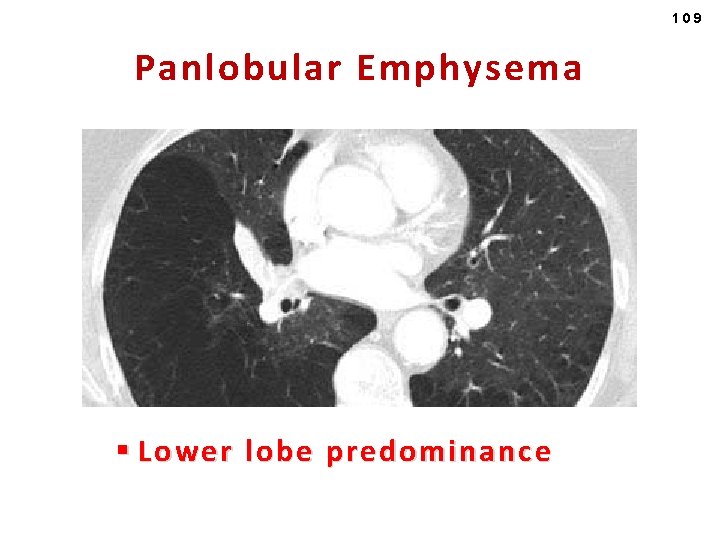
109 Panlobular Emphysema § Lower lobe predominance
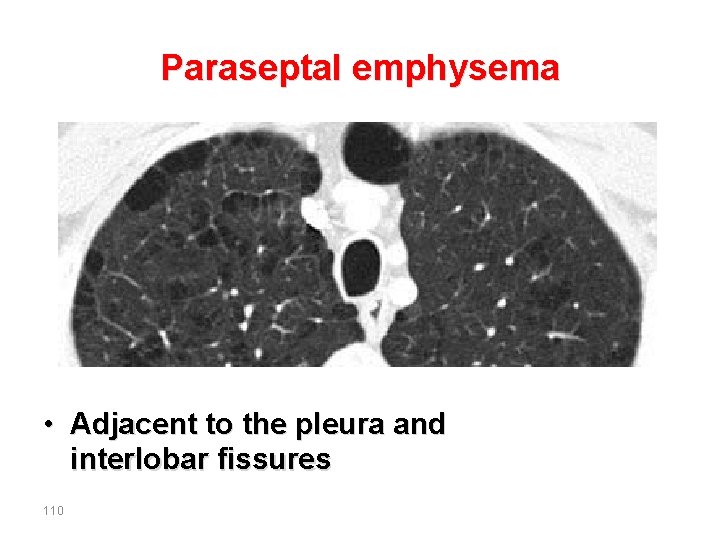
Paraseptal emphysema • Adjacent to the pleura and interlobar fissures 110
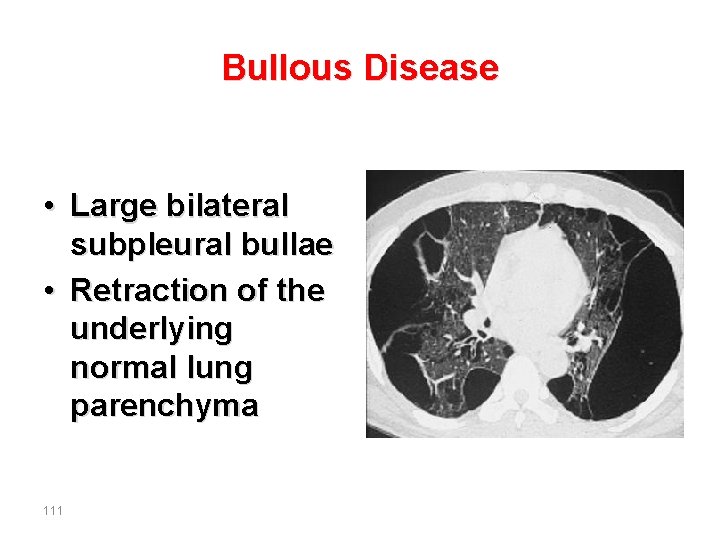
Bullous Disease • Large bilateral subpleural bullae • Retraction of the underlying normal lung parenchyma 111

- Slides: 104