Clinical Classification of Cardiomyopathy Dilated Left andor right
















- Slides: 46


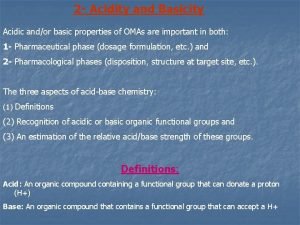
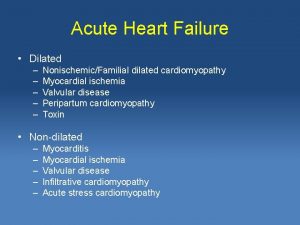
Clinical Classification of Cardiomyopathy • • • Dilated: Left and/or right ventricular enlargement, impaired systolic function, congestive heart failure, arrhythmias, emboli Restrictive: Endomyocardial scarring or myocardial infiltration resulting in restriction to left and/or right ventricular filling Hypertrophic: Disproportionate left ventricular hypertrophy, typically involving septum more than free wall, with or without an intraventricular systolic pressure gradient; usually of a nondilated left ventricular cavity
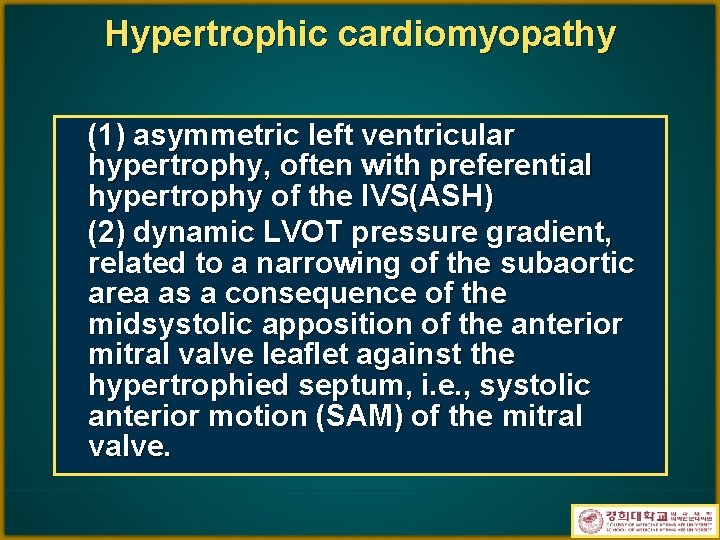
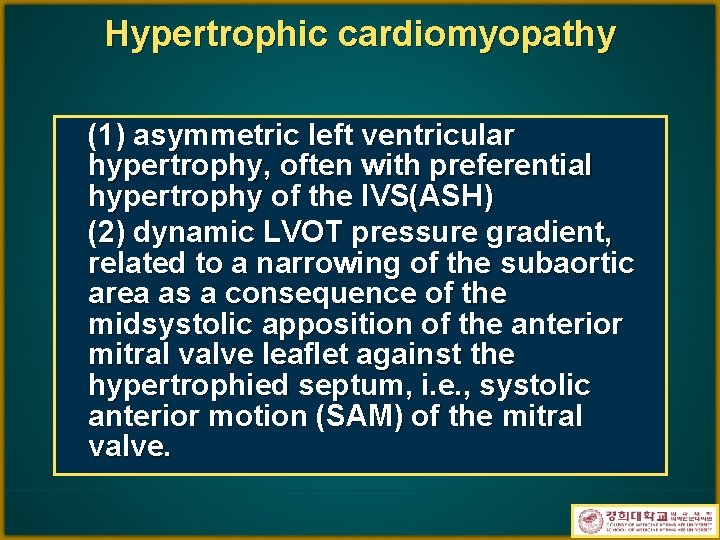
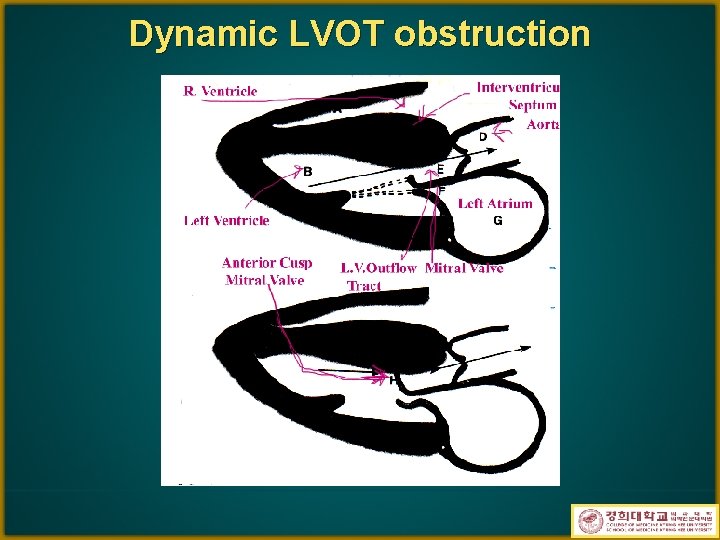
Hypertrophic cardiomyopathy (1) asymmetric left ventricular hypertrophy, often with preferential hypertrophy of the IVS(ASH) (2) dynamic LVOT pressure gradient, related to a narrowing of the subaortic area as a consequence of the midsystolic apposition of the anterior mitral valve leaflet against the hypertrophied septum, i. e. , systolic anterior motion (SAM) of the mitral valve.
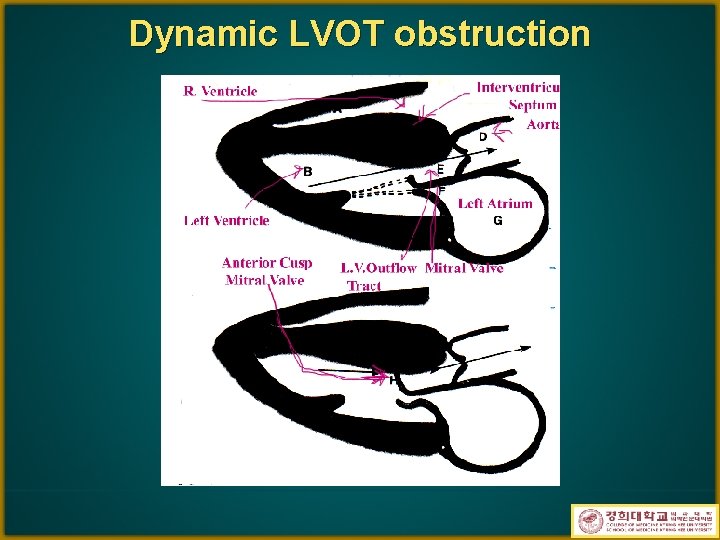
Dynamic LVOT obstruction
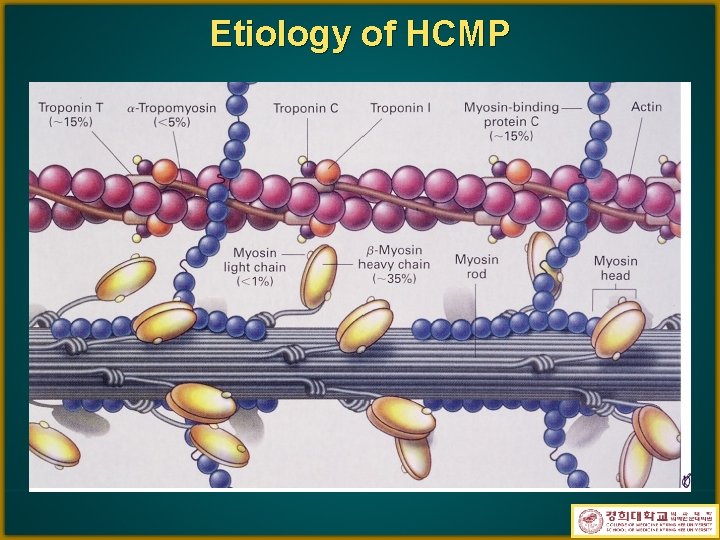
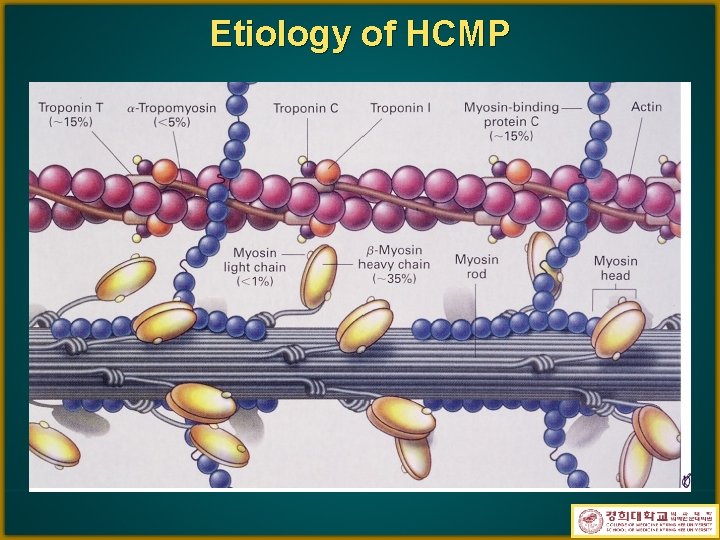
Etiology of HCMP
CLINICAL FEATURES • the first clinical manifestation of the disease may be • • sudden death ¡ frequently occurring in children and young adults ¡ often during or after physical exertion. m/c complaint is dyspnea ¡ d/t increased stiffness of the left ventricular walls angina pectoris, fatigue, and syncope Symptoms are not closely related to the presence or severity of an outflow pressure gradient Physical exam ¡ double or triple apical precordial impulse ¡ a rapidly rising carotid arterial pulse ¡ 4 th heart sound ¡ systolic murmur: harsh, diamond-shaped, best heard at the lower LSB, at the apex
LABORATORY EVALUATION • ECG LVH widespread, deep, broad Q waves that suggest an old myocardial infarction ¡ arrhythmias ¡ • both atrial (supraventricular tachycardia or atrial fibrillation) and ventricular (ventricular tachycardia), during ambulatory (Holter) monitoring • Chest X ray may be normal, mild to moderate increase in the cardiac silhouette is common
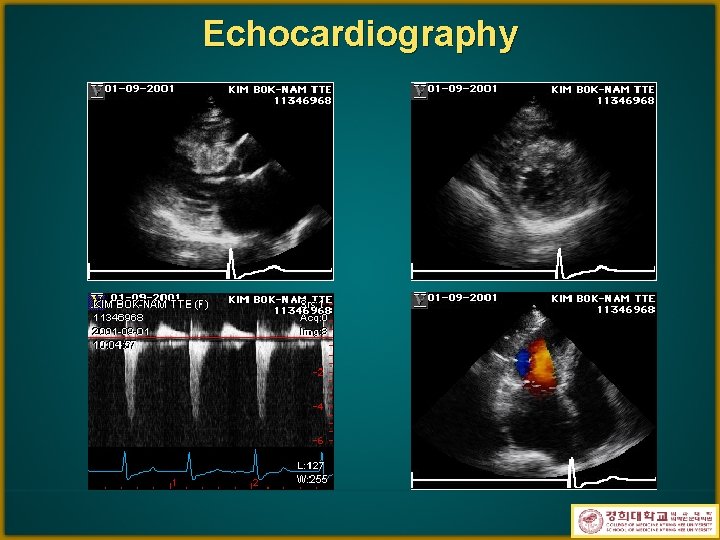
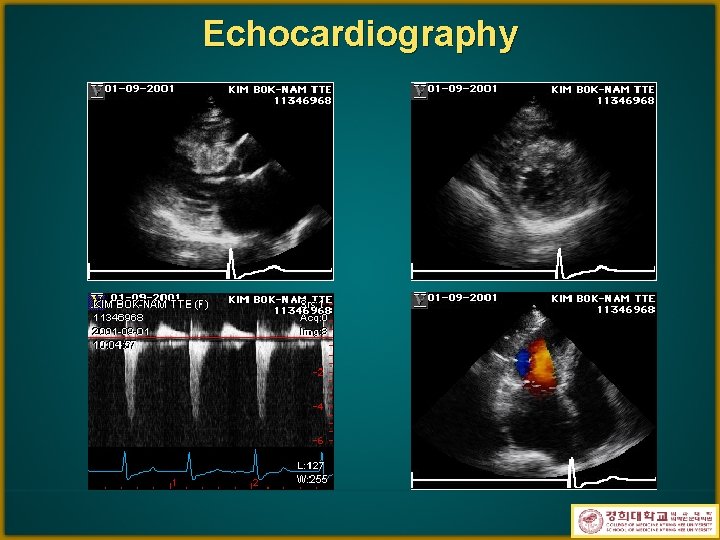
Echocardiography
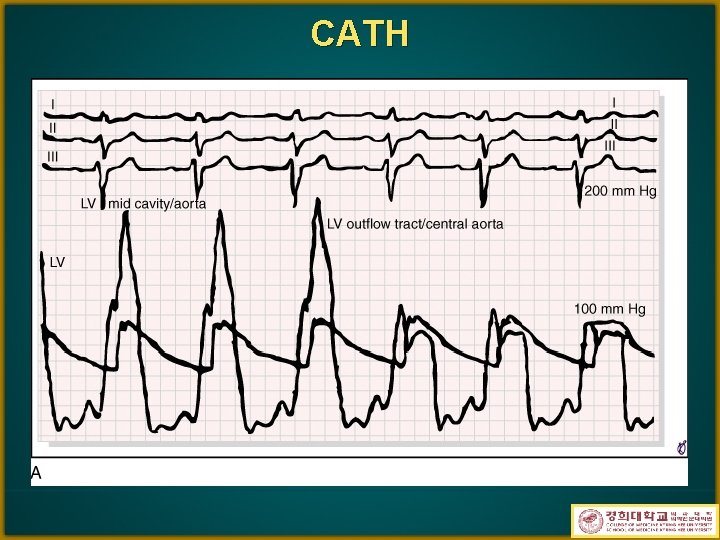
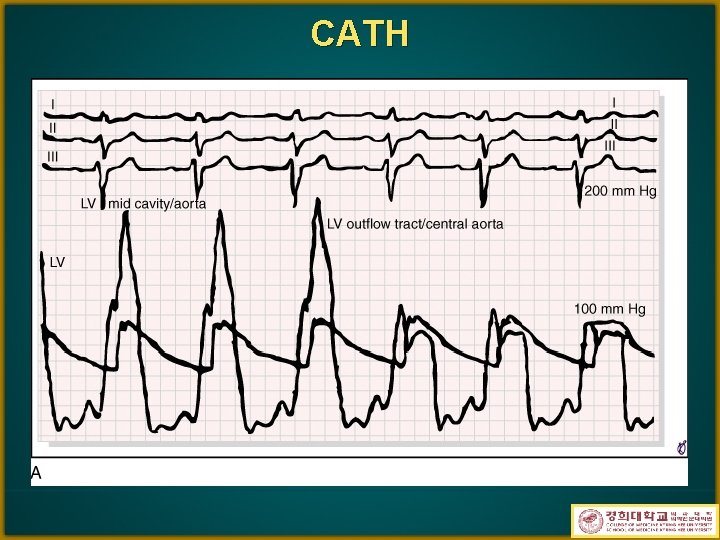
CATH



TREATMENT • • • 경쟁적인 힘든 운동 금지 탈수를 피한다 Beta blocker ¡ ¡ 흉통과 실신예방 운동시 pr. gradient증가를 억제 • Amiodarone supraventricular, life-threatening ventricular arrhythmia 감소 ¡ sudden death의 위험 감소 ¡ • Verapamil and diltiazem ¡ may reduce the stiffness of the ventricle, reduce the elevated diastolic pressures, increase exercise tolerance • Nifedipine 사용금지
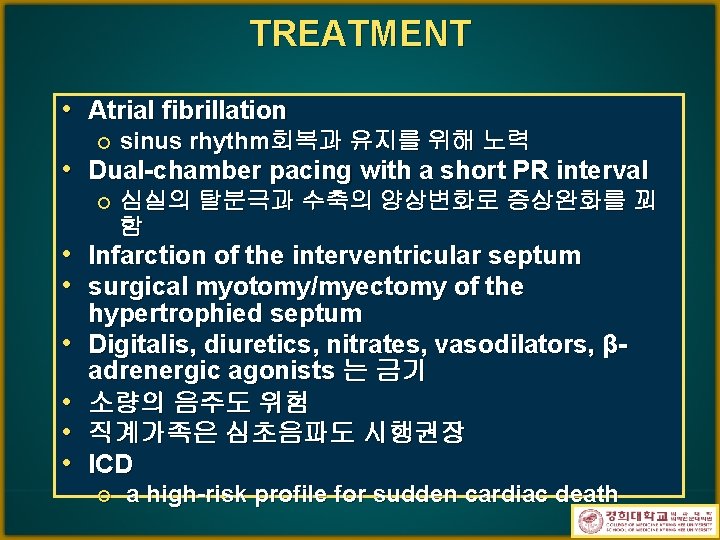
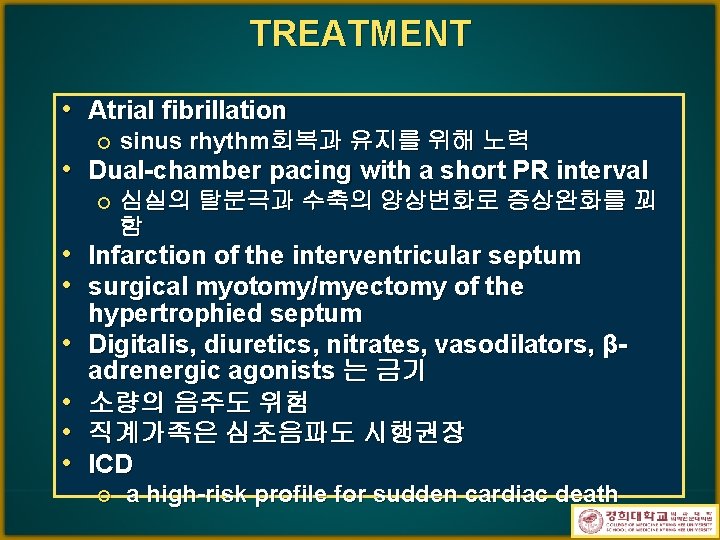
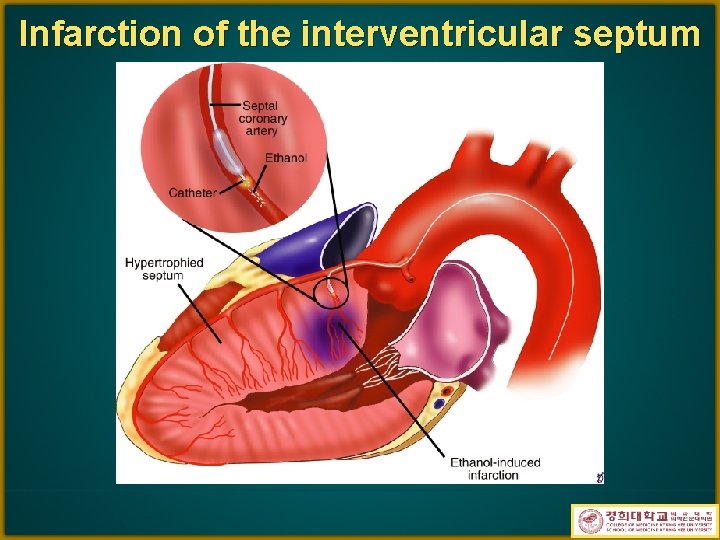
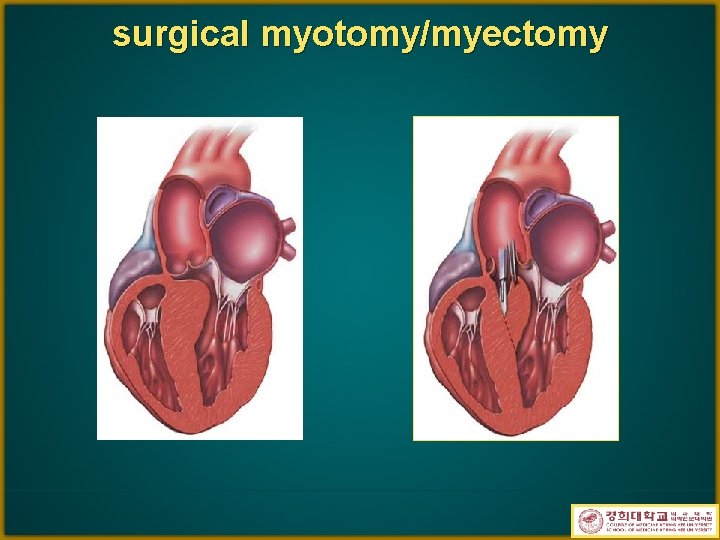
TREATMENT • Atrial fibrillation ¡ sinus rhythm회복과 유지를 위해 노력 • Dual-chamber pacing with a short PR interval ¡ • • • 심실의 탈분극과 수축의 양상변화로 증상완화를 꾀 함 Infarction of the interventricular septum surgical myotomy/myectomy of the hypertrophied septum Digitalis, diuretics, nitrates, vasodilators, βadrenergic agonists 는 금기 소량의 음주도 위험 직계가족은 심초음파도 시행권장 ICD ¡ a high-risk profile for sudden cardiac death
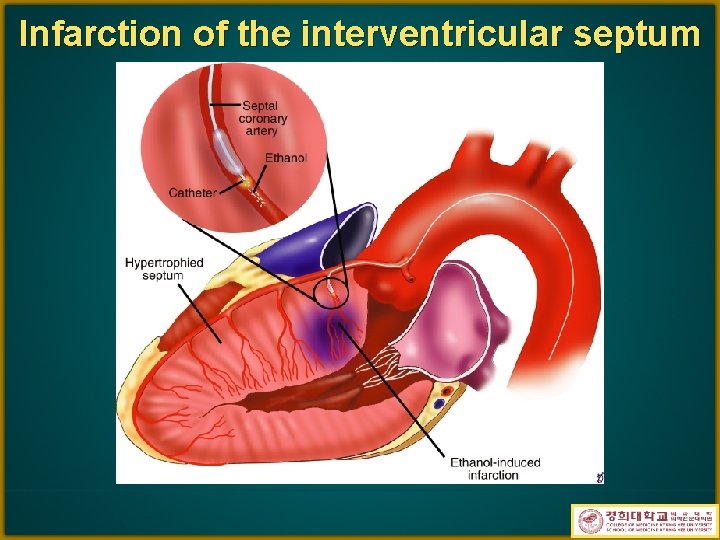
Infarction of the interventricular septum
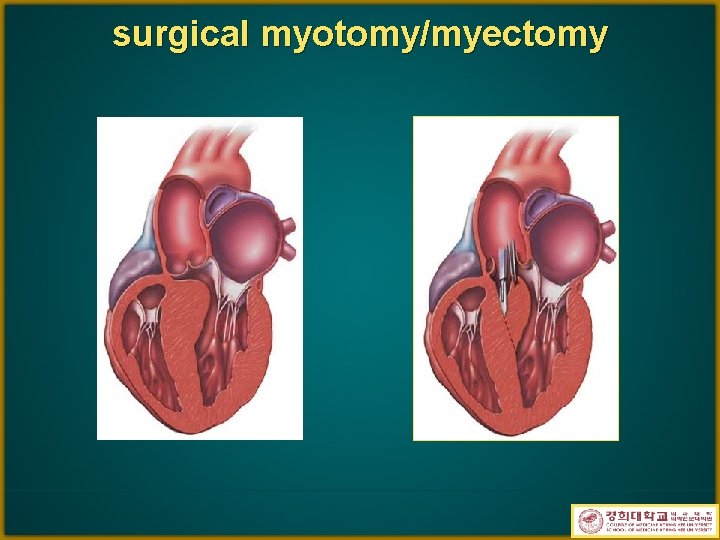
surgical myotomy/myectomy
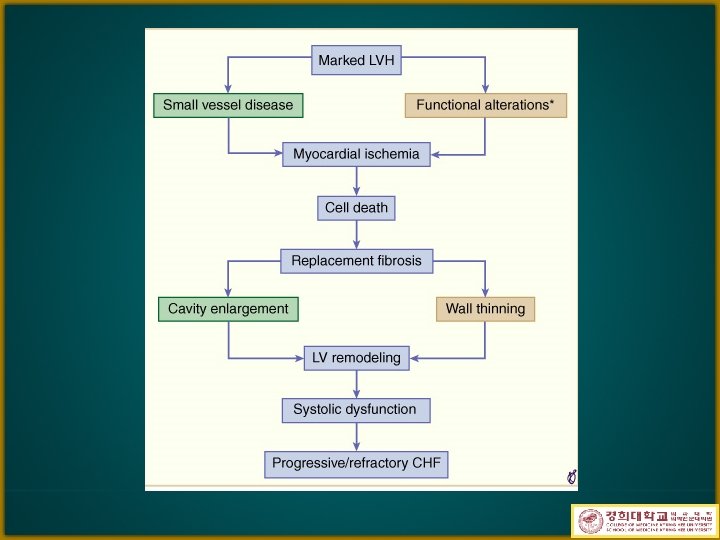

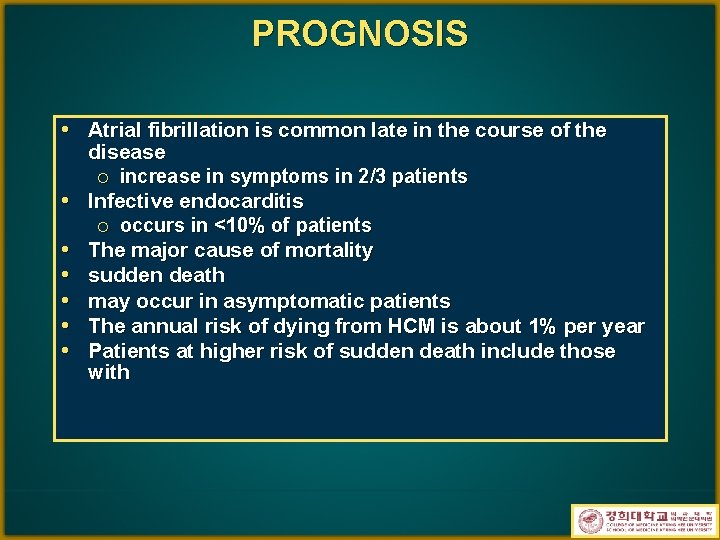
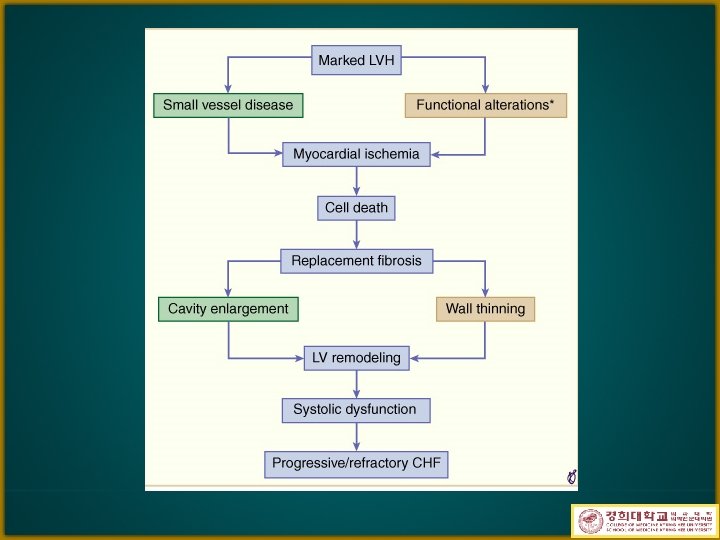
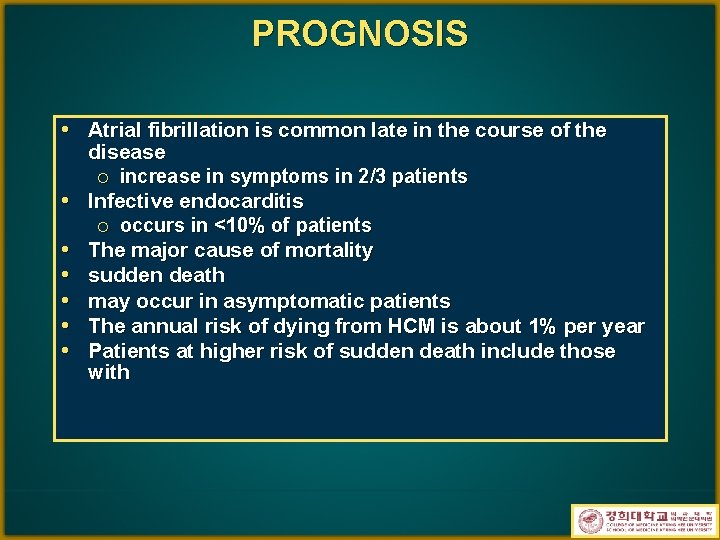
PROGNOSIS • Atrial fibrillation is common late in the course of the • • • disease ¡ increase in symptoms in 2/3 patients Infective endocarditis ¡ occurs in <10% of patients The major cause of mortality sudden death may occur in asymptomatic patients The annual risk of dying from HCM is about 1% per year Patients at higher risk of sudden death include those with
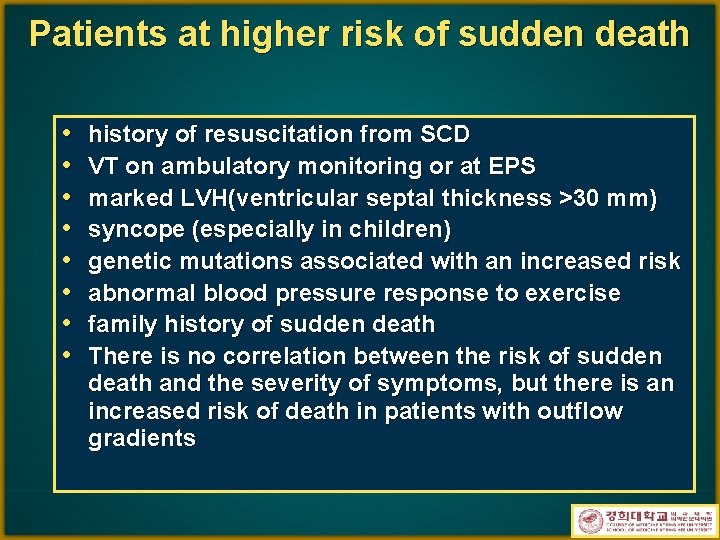
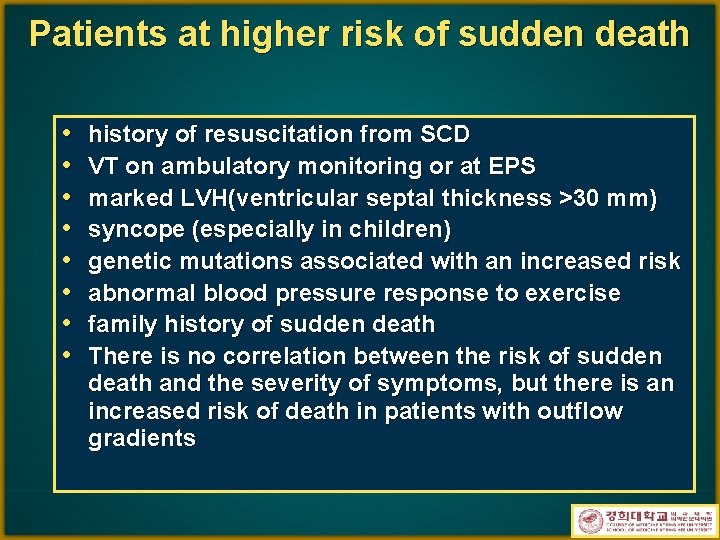
Patients at higher risk of sudden death • • history of resuscitation from SCD VT on ambulatory monitoring or at EPS marked LVH(ventricular septal thickness >30 mm) syncope (especially in children) genetic mutations associated with an increased risk abnormal blood pressure response to exercise family history of sudden death There is no correlation between the risk of sudden death and the severity of symptoms, but there is an increased risk of death in patients with outflow gradients
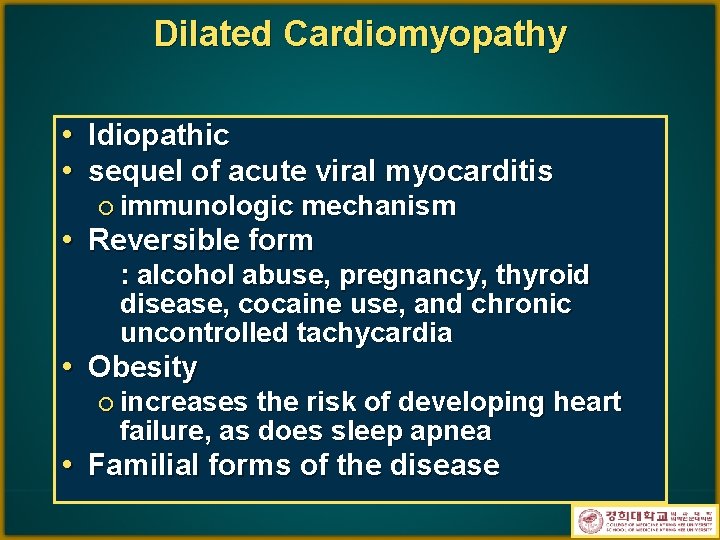
Dilated Cardiomyopathy • Idiopathic • sequel of acute viral myocarditis ¡ immunologic mechanism • Reversible form : alcohol abuse, pregnancy, thyroid disease, cocaine use, and chronic uncontrolled tachycardia • Obesity ¡ increases the risk of developing heart failure, as does sleep apnea • Familial forms of the disease
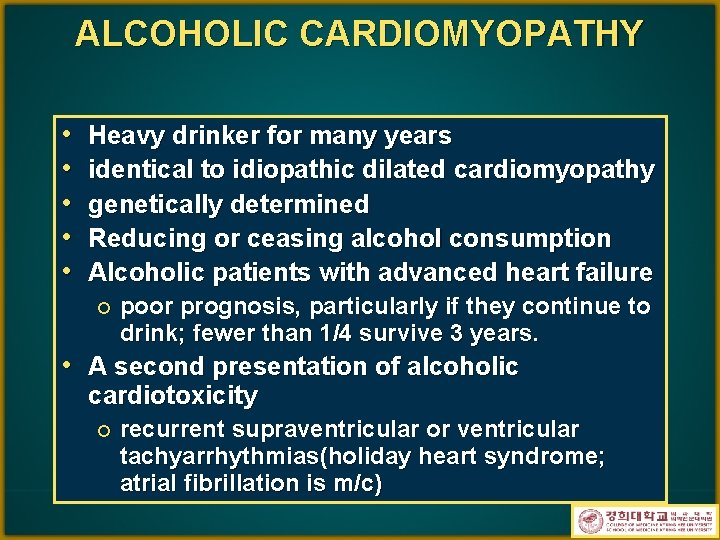
ALCOHOLIC CARDIOMYOPATHY • • • Heavy drinker for many years identical to idiopathic dilated cardiomyopathy genetically determined Reducing or ceasing alcohol consumption Alcoholic patients with advanced heart failure ¡ poor prognosis, particularly if they continue to drink; fewer than 1/4 survive 3 years. • A second presentation of alcoholic cardiotoxicity ¡ recurrent supraventricular or ventricular tachyarrhythmias(holiday heart syndrome; atrial fibrillation is m/c)
PERIPARTUM CARDIOMYOPATHY • during the last trimester of pregnancy or within 6 months after delivery ¡ most women develop symptoms in the month before or immediately after delivery. • usually multiparous, over the age of 30 • symptoms, signs, and treatment ¡ similar to those in patients with idiopathic DCMP • The prognosis mortality rate: 10 to 20%. ¡ related to whether the heart size returns to normal after the first episode of CHF ¡
NEUROMUSCULAR DISEASE • Duchenne's progressive muscular dystrophy, ¡ ¡ ¡ mutations in a gene that encodes a cardiac structural protein (dystrophin) lead to myocyte death ECG: tall R waves in right precordial leads with an R/S ratio >1. 0, often associated with deep Q waves in the limb and lateral precordial leads. A variety of supraventricular and ventricular: frequent arrhythmias • Myotonic dystrophy ¡ ¡ ECG: disorders of impulse formation and conduction syncope and sudden death are major hazards; in appropriate patients, insertion of a permanent pacemaker may be effective. • Friedreich's ataxia ¡ ¡ abnormal ECG: ST-segment and T-wave abnormalities or echo findings: LVH(may be asymmetric)
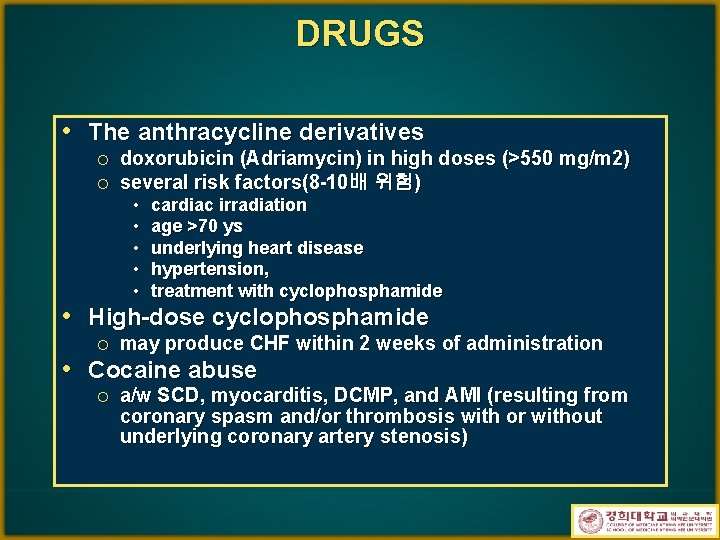
DRUGS • The anthracycline derivatives ¡ ¡ doxorubicin (Adriamycin) in high doses (>550 mg/m 2) several risk factors(8 -10배 위험) • • • cardiac irradiation age >70 ys underlying heart disease hypertension, treatment with cyclophosphamide • High-dose cyclophosphamide ¡ may produce CHF within 2 weeks of administration • Cocaine abuse ¡ a/w SCD, myocarditis, DCMP, and AMI (resulting from coronary spasm and/or thrombosis with or without underlying coronary artery stenosis)
CLINICAL MANIFESTATIONS • Symptoms develop gradually in most • • patients Vague chest pain may be present, typical angina pectoris is unusual and suggests the presence of concomitant ischemic heart disease. Syncope due to arrhythmias and systemic embolism (often emanating from a ventricular thrombus) may occur.

Echocardiography

TREATMENT(I) • the majority, particularly those >55 years, die within 3 years of the onset of symptoms • Death CHF ¡ VT or bradyarrhythmia; sudden death is a constant threat. ¡ • Systemic embolization ¡ considered for chronic anticoagulation. • Standard therapy of heart failure ¡ salt restriction, ACE inhibitors(ARB), diuretics, and digitalis

TREATMENT(II) • β-adrenergic blocker • Spironolactone • biopsy evidence of myocardial inflammation ¡ • • • immunosuppressive therapy, but long-term evidence of efficacy is lacking. Alcohol abstinence Avoid CCB, NSAIDs Antiarrhythmic agents ¡ ¡ risk of proarrhythmia needed to treat symptomatic or serious arrhythmias ¡ 1/3 of pts with intraventricular conduction delay, biventricular pacing improves symptoms, reduces hospitalizations, and perhaps reduces mortality. • Cardiac resynchronization therapy(CRT) • Implantable cardioverter-defibrillator(ICD) ¡ useful in symptomatic ventricular arrhythmias, • Cardiac transplantation
CRT

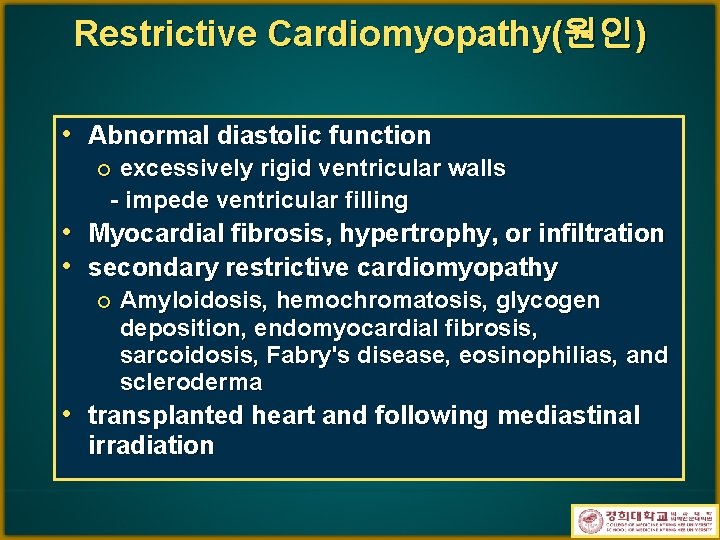
Restrictive Cardiomyopathy(원인) • Abnormal diastolic function excessively rigid ventricular walls - impede ventricular filling ¡ • Myocardial fibrosis, hypertrophy, or infiltration • secondary restrictive cardiomyopathy ¡ Amyloidosis, hemochromatosis, glycogen deposition, endomyocardial fibrosis, sarcoidosis, Fabry's disease, eosinophilias, and scleroderma • transplanted heart and following mediastinal irradiation
Symptom and sign • The inability of the ventricle to fill limits cardiac output and raises filling pressure • exercise intolerance and dyspnea • elevated venous pressure ¡ dependent edema, ascites, and an enlarged, tender, and often pulsatile liver. • Elevated JVP : does not fall normally, or it may rise with inspiration (Kussmaul's sign)
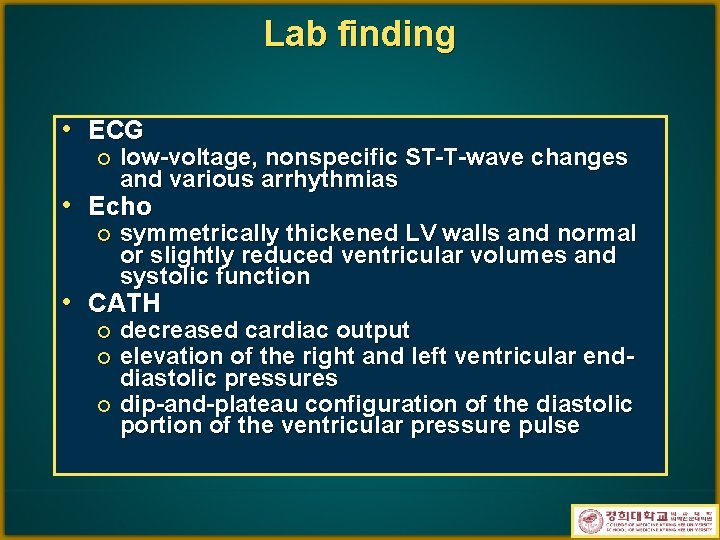
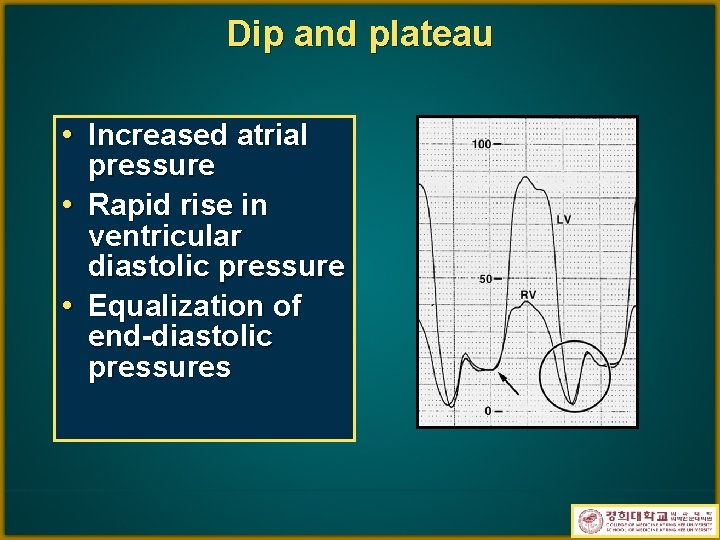
Lab finding • ECG ¡ low-voltage, nonspecific ST-T-wave changes and various arrhythmias • Echo ¡ symmetrically thickened LV walls and normal or slightly reduced ventricular volumes and systolic function • CATH decreased cardiac output elevation of the right and left ventricular enddiastolic pressures ¡ dip-and-plateau configuration of the diastolic portion of the ventricular pressure pulse ¡ ¡
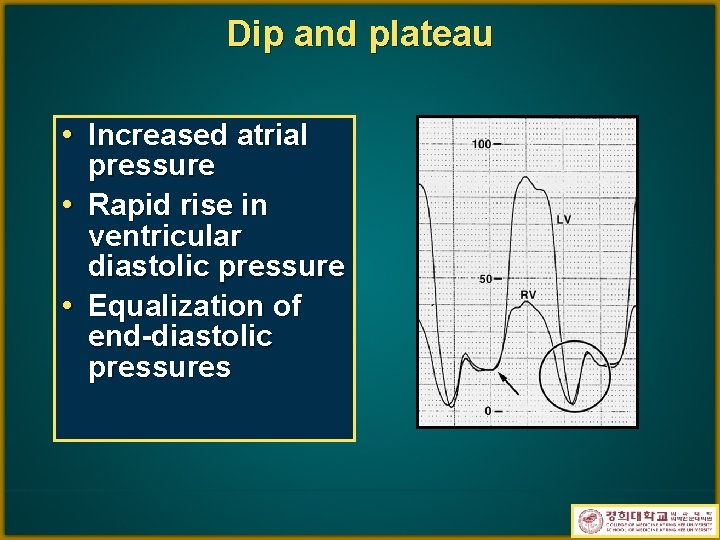
Dip and plateau • Increased atrial • • pressure Rapid rise in ventricular diastolic pressure Equalization of end-diastolic pressures

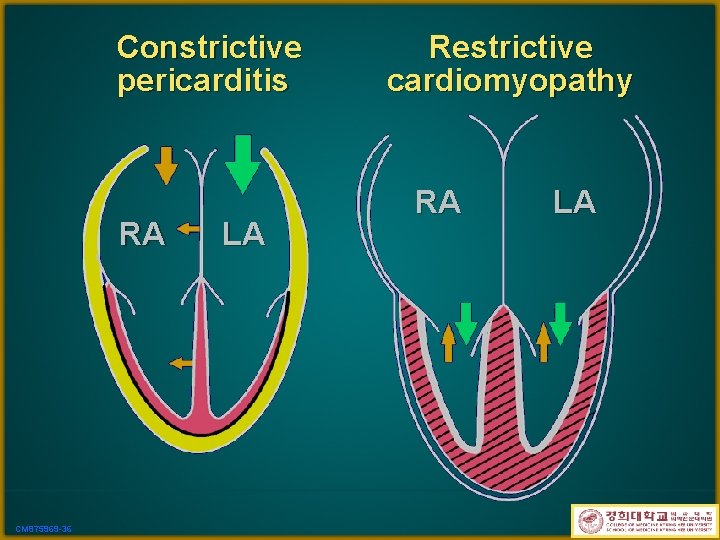
DDx. from constrictive pericarditis Constrictive Pericarditis Restrictive Cardiomyopathy CP 983059 -6
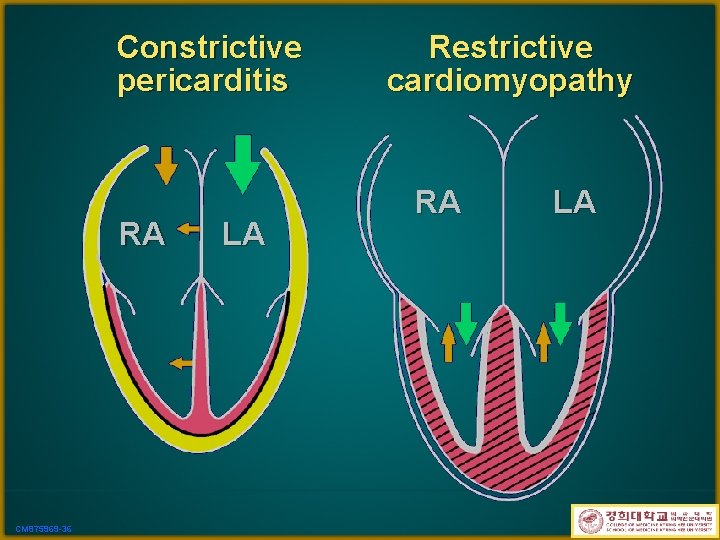
Constrictive pericarditis RA CM 875969 -36 LA Restrictive cardiomyopathy RA LA
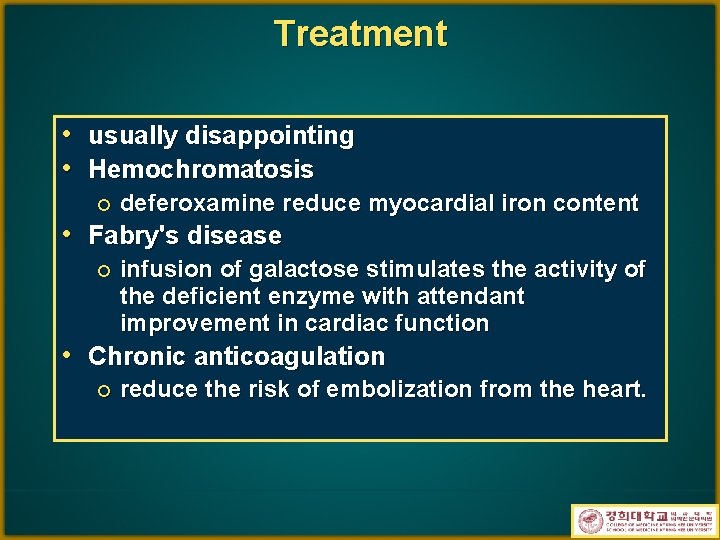
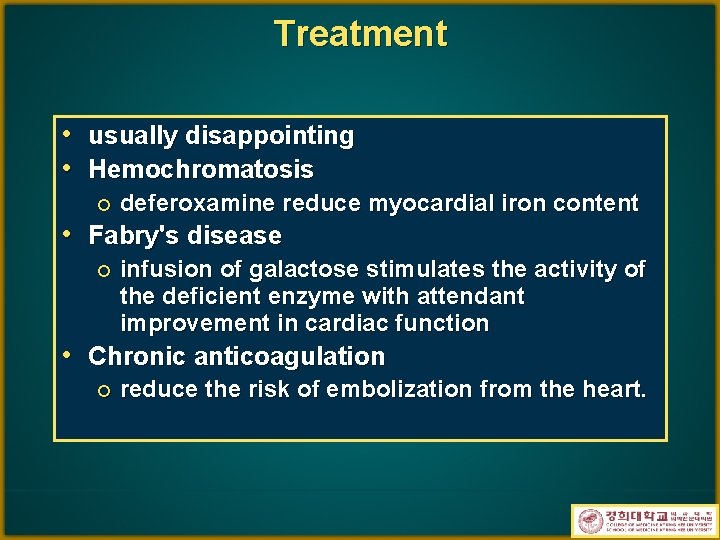
Treatment • usually disappointing • Hemochromatosis ¡ deferoxamine reduce myocardial iron content • Fabry's disease ¡ infusion of galactose stimulates the activity of the deficient enzyme with attendant improvement in cardiac function • Chronic anticoagulation ¡ reduce the risk of embolization from the heart.

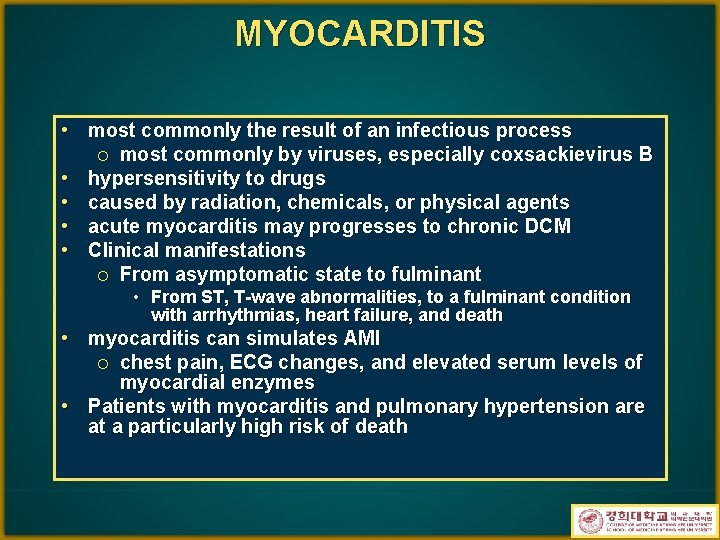
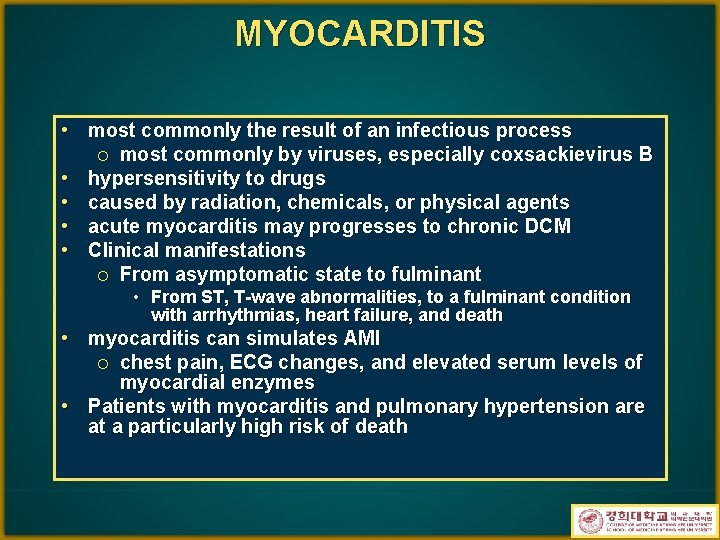
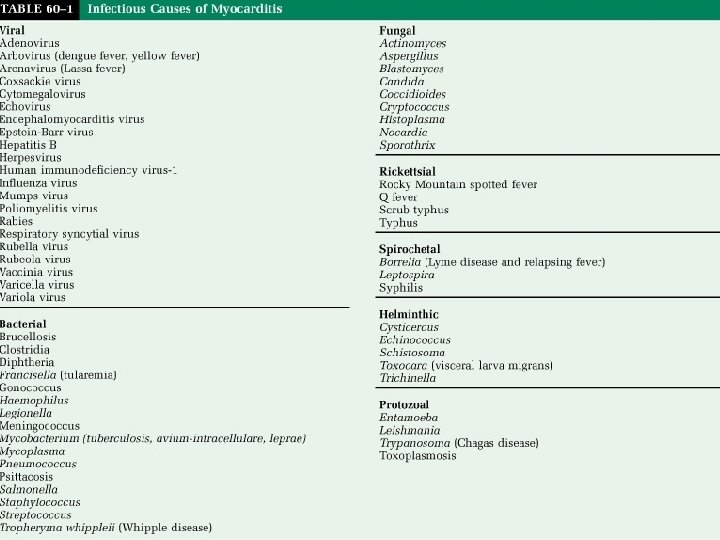
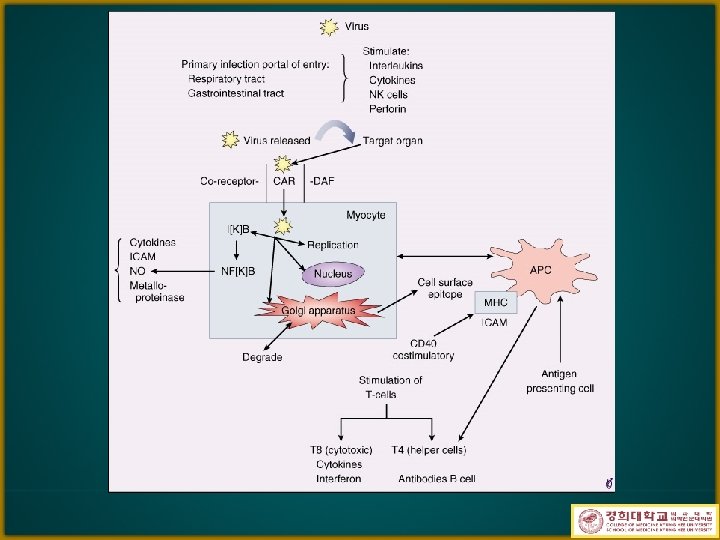
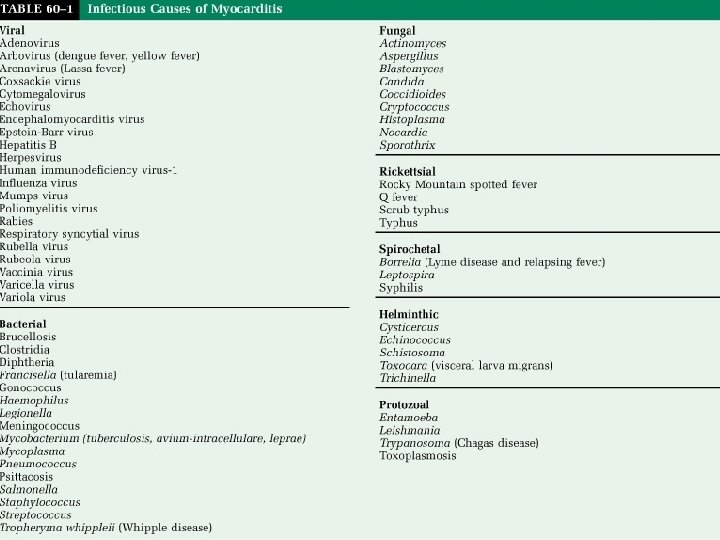
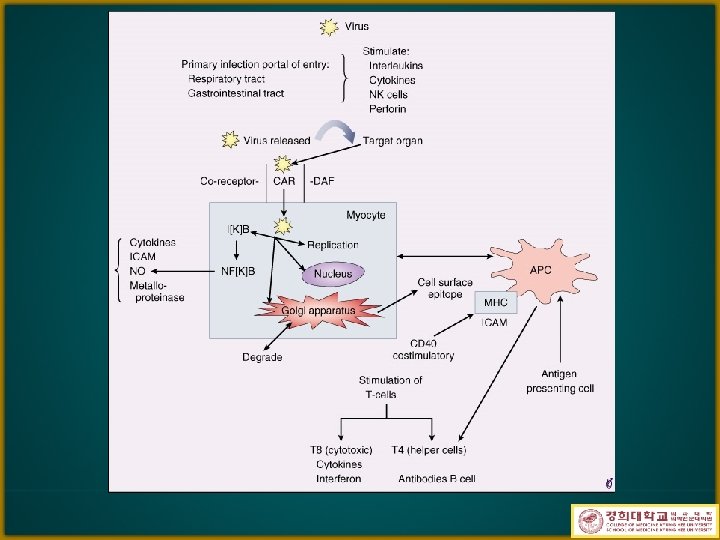
MYOCARDITIS • most commonly the result of an infectious process most commonly by viruses, especially coxsackievirus B hypersensitivity to drugs caused by radiation, chemicals, or physical agents acute myocarditis may progresses to chronic DCM Clinical manifestations ¡ From asymptomatic state to fulminant ¡ • • • From ST, T-wave abnormalities, to a fulminant condition with arrhythmias, heart failure, and death • myocarditis can simulates AMI chest pain, ECG changes, and elevated serum levels of myocardial enzymes • Patients with myocarditis and pulmonary hypertension are at a particularly high risk of death ¡

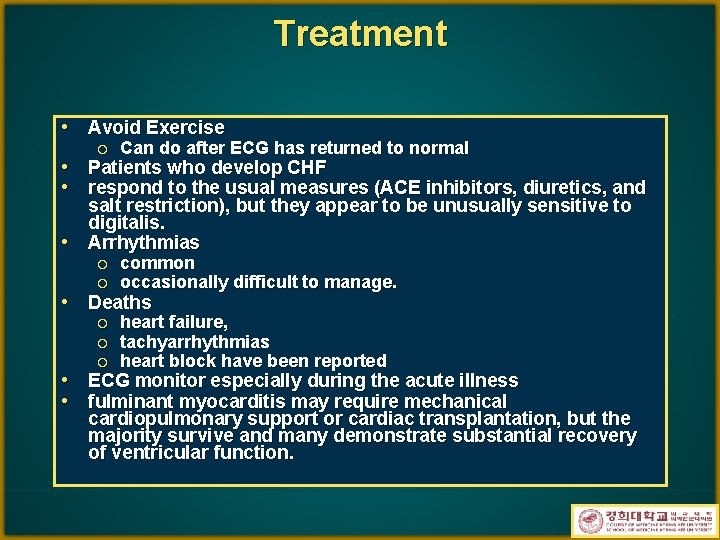
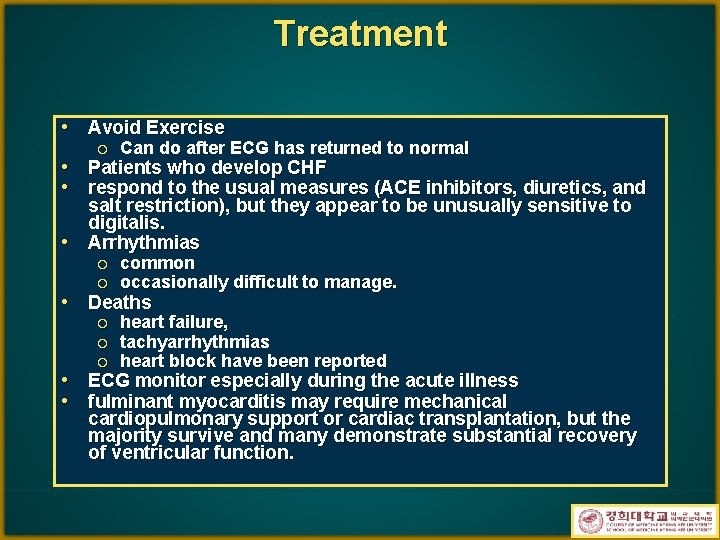
Treatment • Avoid Exercise ¡ Can do after ECG has returned to normal • Patients who develop CHF • respond to the usual measures (ACE inhibitors, diuretics, and salt restriction), but they appear to be unusually sensitive to digitalis. • Arrhythmias ¡ ¡ common occasionally difficult to manage. ¡ ¡ ¡ heart failure, tachyarrhythmias heart block have been reported • Deaths • • ECG monitor especially during the acute illness fulminant myocarditis may require mechanical cardiopulmonary support or cardiac transplantation, but the majority survive and many demonstrate substantial recovery of ventricular function.



 Paresis
Paresis Left left right right turn around go go go
Left left right right turn around go go go Left left right right go go go
Left left right right go go go Right product right place right time right price
Right product right place right time right price Family time
Family time Heart disease cat
Heart disease cat The right man on the right place at the right time
The right man on the right place at the right time Edu gtk bme
Edu gtk bme How are the inner and outer planets alike
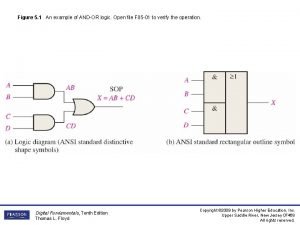
How are the inner and outer planets alike Andor logic
Andor logic Andor györgy üzleti gazdaságtan
Andor györgy üzleti gazdaságtan Levophenol
Levophenol Andor györgy üzleti gazdaságtan
Andor györgy üzleti gazdaságtan Andor györgy üzleti gazdaságtan
Andor györgy üzleti gazdaságtan Whatever text
Whatever text Python jumpstart
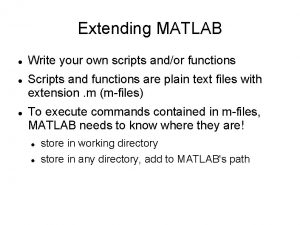
Python jumpstart Andor matlab
Andor matlab Time dilation equation
Time dilation equation Brain stem reflexes ppt
Brain stem reflexes ppt Dilated pupils death
Dilated pupils death Achalasia cardia
Achalasia cardia Cervix dilation chart
Cervix dilation chart What is dilated in math
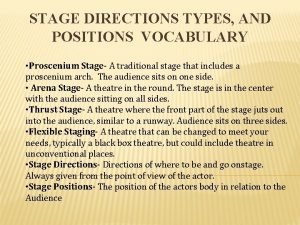
What is dilated in math Upstage vs downstage
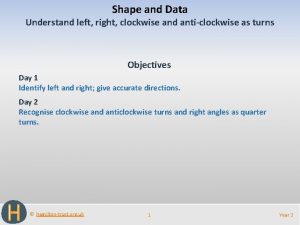
Upstage vs downstage Go straight and then turn left
Go straight and then turn left Left on left sacral torsion
Left on left sacral torsion For top-down parsing left recursion removal is
For top-down parsing left recursion removal is Put your left foot in
Put your left foot in Don't turn left here
Don't turn left here Dr tulika jain
Dr tulika jain Left child right sibling
Left child right sibling Answer. go straight turn left turn right
Answer. go straight turn left turn right Spatres meaning
Spatres meaning Left right story game for summer
Left right story game for summer What are peristaltic movements
What are peristaltic movements Upstage downstage definition
Upstage downstage definition 3/4 thrust stage
3/4 thrust stage What is stage blocking
What is stage blocking Which day is anti clockwise left or right
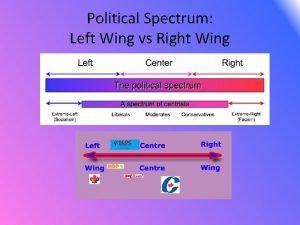
Which day is anti clockwise left or right Left wing and right wing spectrum
Left wing and right wing spectrum Atomic radii trend
Atomic radii trend Method study flow process chart
Method study flow process chart Masonic fire toast
Masonic fire toast Pleura parietal visceral
Pleura parietal visceral Look down look up
Look down look up Uniform bell-shaped skewed-right skewed-left
Uniform bell-shaped skewed-right skewed-left Superior rectal artery is a branch of
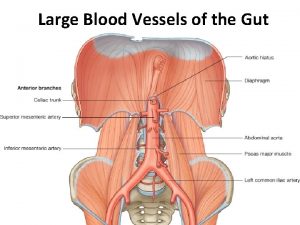
Superior rectal artery is a branch of