Clinical Case Study Nutrition Support for Multiple Traumas



- Slides: 27
Clinical Case Study: Nutrition Support for Multiple Traumas Brooklyn Harkness ARAMARK Dietetic Internship United Regional Healthcare System December 18, 2013
Disease State Multiple Traumas • Secondary to Motor Vehicle Accident • Complications: large lacerations to scalp, right elbow and right knee • Treatments: Surgical, Medicinal, & Nutritional
Metabolic Response to Trauma & Stress • Catabolism: destructive metabolism -Targets lean body mass -Negative nitrogen balance & muscle wasting • Characteristic Phases: -Ebb Phase (acute response) -Flow Phase (adaptive response)
Metabolic Response to Trauma & Stress • Ebb Phase - Immediately following injury: -Hypovolemia -Shock -Tissue Hypoxia -Decreased Metabolic Rate
Multiple Response to Trauma & Stress • Flow Phase: following fluid resuscitation & renewal of oxygen delivery -Acute Response -Adaptive Response
Multiple Response to Trauma & Stress • Flow Phase - Acute Response • Catabolism dominates: -Increase Glucagon -Increased excretion of nitrogen -Increased metabolic rate -Increased oxygen utilization

Multiple Trauma & Stress • Flow Phase - Adaptive Response • Anabolism Dominates: -Declined hormone response -Recovery -Possible repair of body protein -Healing
Evidence – Based Nutrition Recommendations • Adam et al, 2013 - Cohort study, Systematic review -N = 1, 179 -Intragastric versus Small Intestinal Feedings -Findings: Small Bowel Feedings will increase nutrient delivery & decrease pneumonia second to ventilation -Limited by data interpretation and subjective diagnosis of pneumonia (5) Deane adam M, Rupinder D, Day andrew G, Ridley emma J, Davies andrew R, Heyland daren K. Comparisons between intragastric and small intestinal delivery of enteral nutrition in the critically ill: a systematic review and meta-analysis. Crit Care. 2013; 17(3): R 125.
Evidence – Based Nutrition Recommendations • Alberda et al, 2009 -Cohort Study -N = 2, 884 - Additional Protein - Findings: More rapid healing & decreased mortality rate -Limitations: units across 5 different continents and 37 countries brought variability in standards of care. different -Limitations: BMI was the only indicator of nutritional reserve. (6) Alberda C, Gramlich L, Jones N, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. 2009; 35(10): 1728 -37.
Evidence – Based Nutrition Recommendations • Berger et al, 2008 - N = 200 -Early Feedings (24 -48 hours) after trauma or major surgery -Early antioxidant supplementation (within 24 hours) -Findings: significantly dulled the inflammatory response -Limitations: lack of power (7) Berger MM, Soguel L, Shenkin A, et al. Influence of early antioxidant supplements on clinical evolution and organ function in critically ill cardiac surgery, major trauma, and subarachnoid hemorrhage patients. Crit Care. 2008; 12(4): R 101.
Case Presentation • 23 Year old Caucasian Male • Dx: Multiple Trauma secondary to motor vehicle collision • Initial Emergency Room Care: Sedation, Intubation, & Cervical Collar • Glasglow Coma Scale: 3
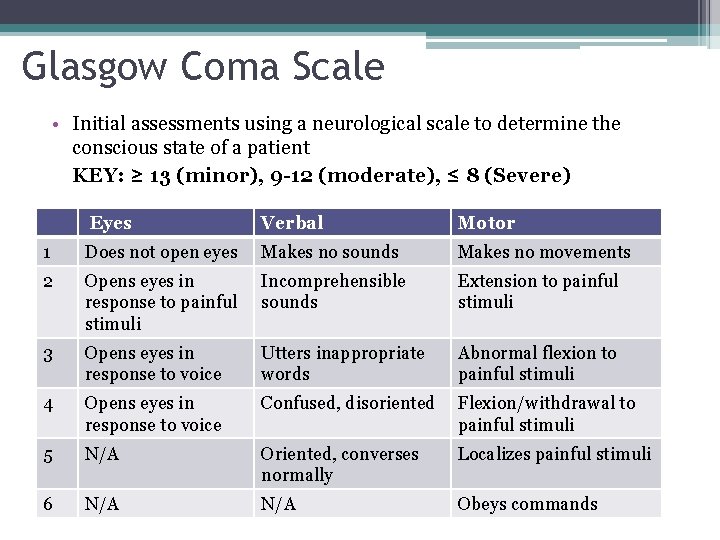
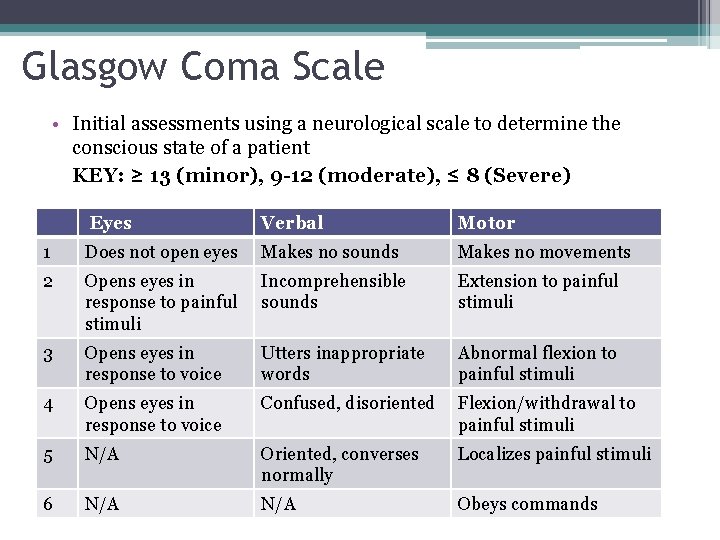
Glasgow Coma Scale • Initial assessments using a neurological scale to determine the conscious state of a patient KEY: ≥ 13 (minor), 9 -12 (moderate), ≤ 8 (Severe) Eyes Verbal Motor 1 Does not open eyes Makes no sounds Makes no movements 2 Opens eyes in response to painful stimuli Incomprehensible sounds Extension to painful stimuli 3 Opens eyes in response to voice Utters inappropriate words Abnormal flexion to painful stimuli 4 Opens eyes in response to voice Confused, disoriented Flexion/withdrawal to painful stimuli 5 N/A Oriented, converses normally Localizes painful stimuli 6 N/A Obeys commands

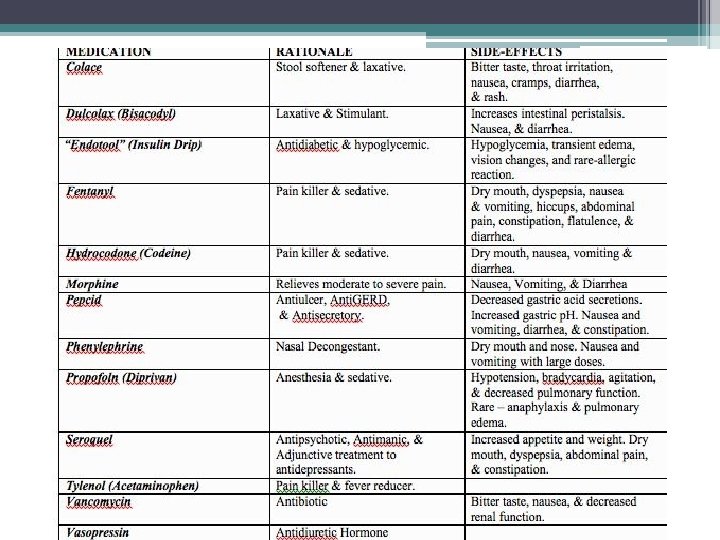
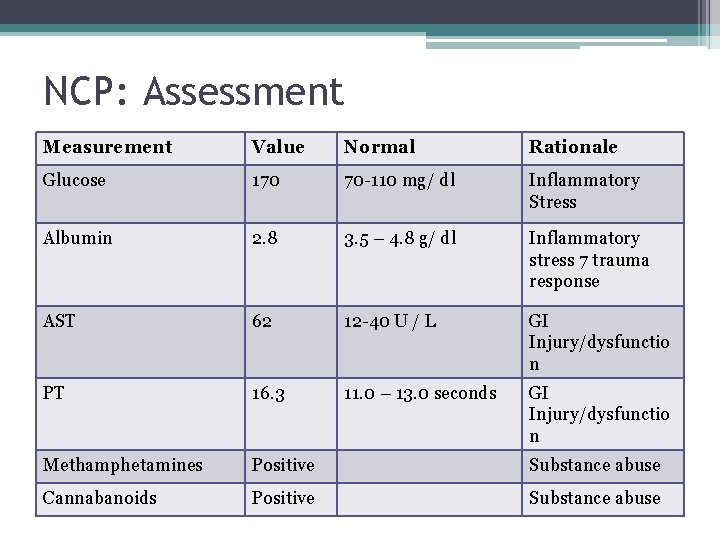
NCP: Assesment • Client History -No Prior Medical History -Substance abuse: positive for methamphetamines and cannabanoids
NCP: Assessment • Food/Nutrition-Related History - Unable to obtain information from pt due to sedation and intubation -Mother indicated no diet limitations
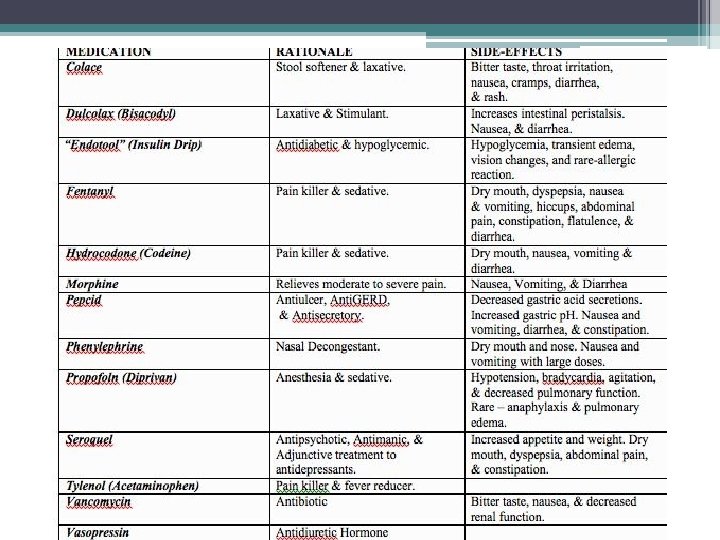
NCP: Assessment • Nutrition-Focused Physical Findings: -Intubation -Tracheostomy -Mild abdominal distension -Constipation -Hyperglycemia -Hypoalbuminemia
NCP: Assessment • Anthropometric Measurements - Height: 6’ 0” -Admission wt: 198# (90 kg) -BMI: 26. 8, overweight -IBW: 180#
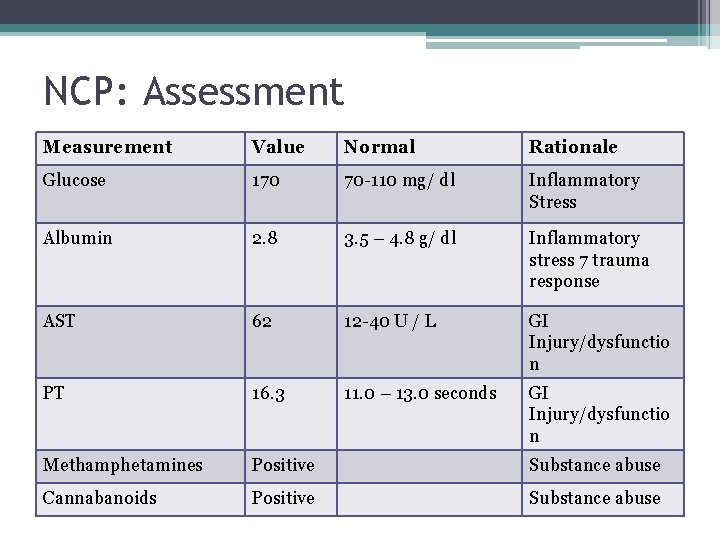
NCP: Assessment Measurement Value Normal Rationale Glucose 170 70 -110 mg/ dl Inflammatory Stress Albumin 2. 8 3. 5 – 4. 8 g/ dl Inflammatory stress 7 trauma response AST 62 12 -40 U / L GI Injury/dysfunctio n PT 16. 3 11. 0 – 13. 0 seconds GI Injury/dysfunctio n Methamphetamines Positive Substance abuse Cannabanoids Positive Substance abuse
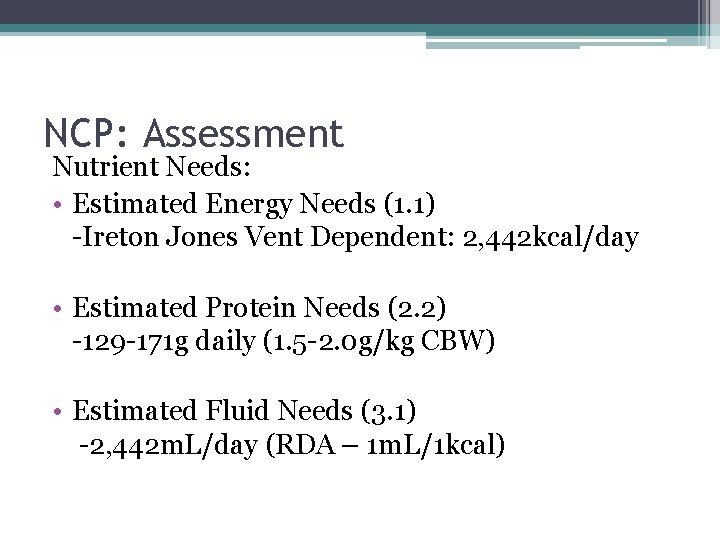
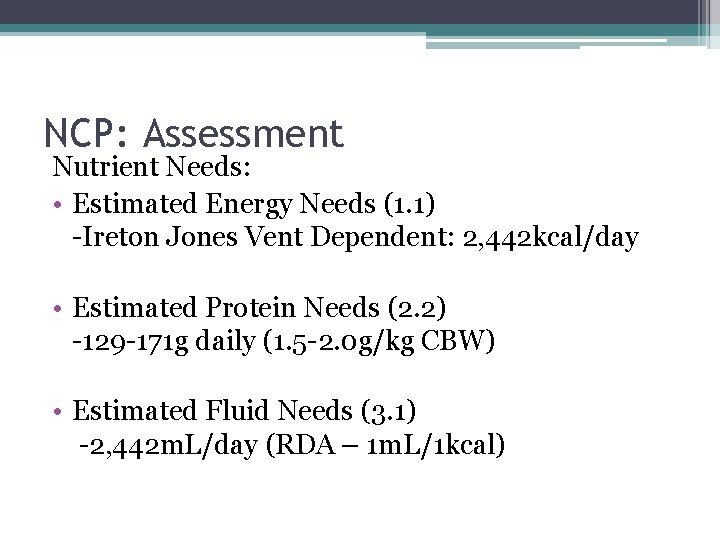
NCP: Assessment Nutrient Needs: • Estimated Energy Needs (1. 1) -Ireton Jones Vent Dependent: 2, 442 kcal/day • Estimated Protein Needs (2. 2) -129 -171 g daily (1. 5 -2. 0 g/kg CBW) • Estimated Fluid Needs (3. 1) -2, 442 m. L/day (RDA – 1 m. L/1 kcal)
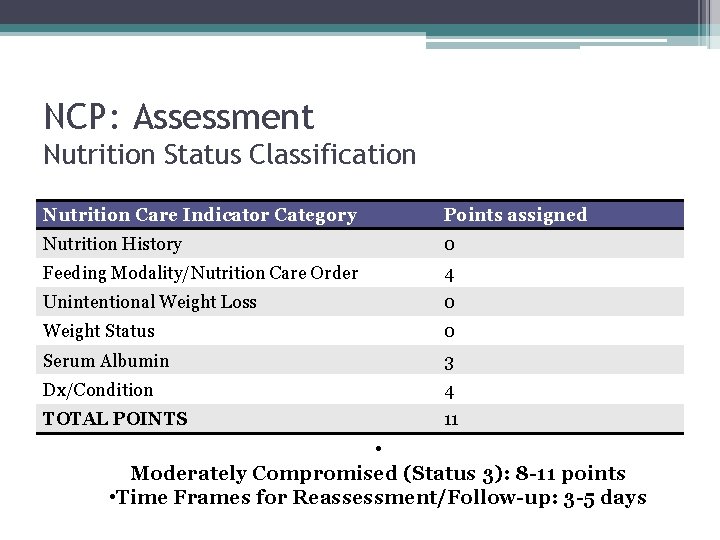
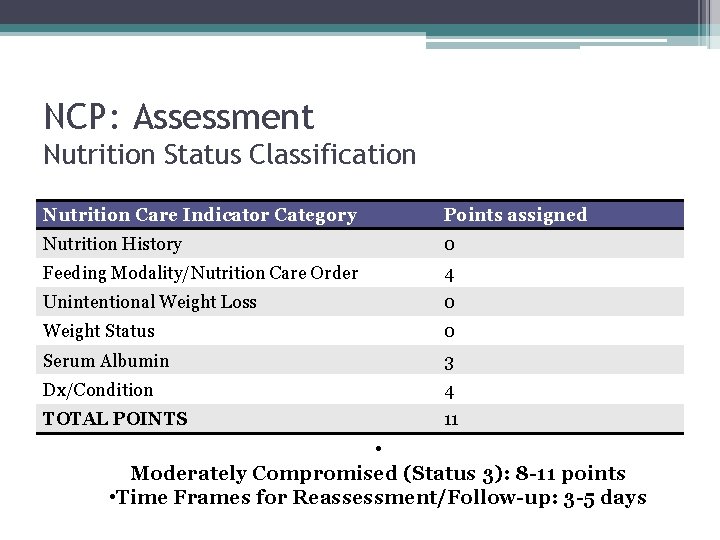
NCP: Assessment Nutrition Status Classification Nutrition Care Indicator Category Points assigned Nutrition History 0 Feeding Modality/Nutrition Care Order 4 Unintentional Weight Loss 0 Weight Status 0 Serum Albumin 3 Dx/Condition 4 TOTAL POINTS 11 • Moderately Compromised (Status 3): 8 -11 points • Time Frames for Reassessment/Follow-up: 3 -5 days
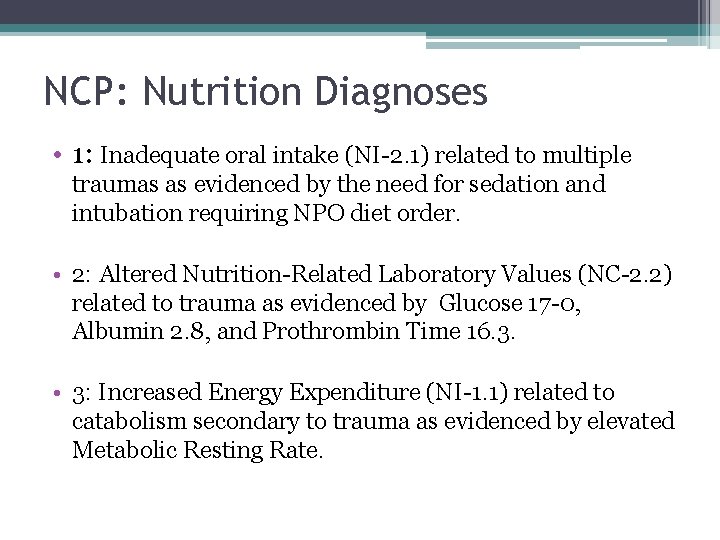
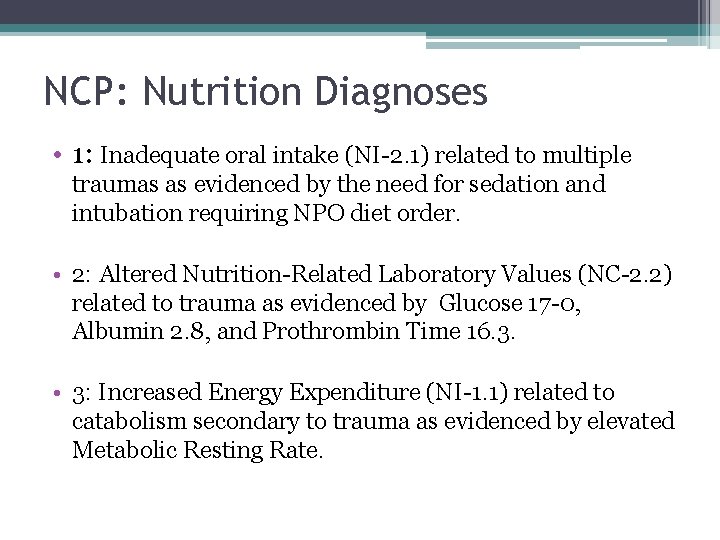
NCP: Nutrition Diagnoses • 1: Inadequate oral intake (NI-2. 1) related to multiple traumas as evidenced by the need for sedation and intubation requiring NPO diet order. • 2: Altered Nutrition-Related Laboratory Values (NC-2. 2) related to trauma as evidenced by Glucose 17 -0, Albumin 2. 8, and Prothrombin Time 16. 3. • 3: Increased Energy Expenditure (NI-1. 1) related to catabolism secondary to trauma as evidenced by elevated Metabolic Resting Rate.
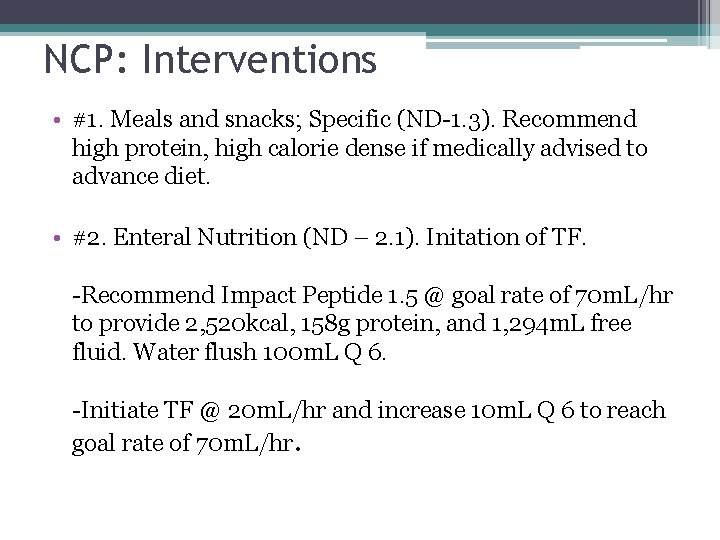
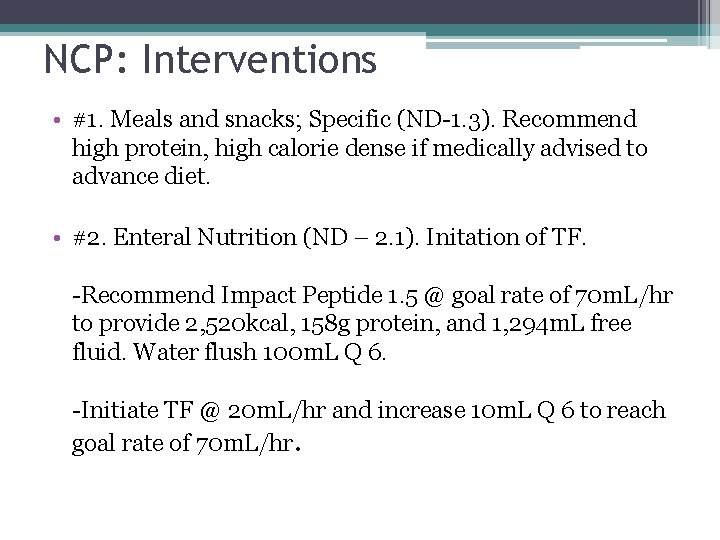
NCP: Interventions • #1. Meals and snacks; Specific (ND-1. 3). Recommend high protein, high calorie dense if medically advised to advance diet. • #2. Enteral Nutrition (ND – 2. 1). Initation of TF. -Recommend Impact Peptide 1. 5 @ goal rate of 70 m. L/hr to provide 2, 520 kcal, 158 g protein, and 1, 294 m. L free fluid. Water flush 100 m. L Q 6. -Initiate TF @ 20 m. L/hr and increase 10 m. L Q 6 to reach goal rate of 70 m. L/hr.
• Short-Term Goals/Expected Outcomes: 1. Tolerance of TF @ goal rate of 70 m. L/hr within 36 -48 hours of initiation. 2. EN to provide >85% assessed nutritional needs. • Long-Term Goals/Expected Outcomes: 1. Initiation of oral intake within the patient’s length of stay. 2. Patient to consume 100% of nutrient needs via oral intake with no complications.

NCP: Monitoring and Evaluation • #1. Food/Nutrition-Related History (FH). Energy Intake (1. 2. 1) Total Energy Intake (FH 1. 1) • #2. Biochemical Data, Medical Tests, and Procedures (BD). Glucose (1. 5) Albumin (BD 1. 1) and Prothrombin Time (BD-1. 4. 9) • #3. Anthropometric Measurements (AD). Weight (AD 1. 1. 2)
Conclusion • Patient transferred to Rehabilitation Institute on EN support • Discharged tolerating at goal rate of 70 m. L/hr: -2, 520 kcal, 158 g protein, 1, 294 m. L free fluids -water flushes 100 m. L Q 6 hours
References • 1) (http: //www-nrd. nhtsa. dot. gov/Pubs/811856. pdf). National Highway Traffic Safety Administration (non-article) (2) Manhan LK, Escott-Stump S, Raymond JL. Krause's Food and Nutrition Care Process. 13 th ed. St. Louis, MO: EL Sevier Saunders: 2012. (3) Escott-Stump S. Nutrition and Diagnosis – Related Care. 7 th ed. Baltimure, ND: Lippimcott Williams & Wilkins: 2012. (4) Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009; 361(14): 1339 -48. (5) Deane adam M, Rupinder D, Day andrew G, Ridley emma J, Davies andrew R, Heyland daren K. Comparisons between intragastric and small intestinal delivery of enteral nutrition in the critically ill: a systematic review and meta-analysis. Crit Care. 2013; 17(3): R 125. (6) Alberda C, Gramlich L, Jones N, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. 2009; 35(10): 1728 -37. (7) Berger MM, Soguel L, Shenkin A, et al. Influence of early antioxidant supplements on clinical evolution and organ function in critically ill cardiac surgery, major trauma, and subarachnoid hemorrhage patients. Crit Care. 2008; 12(4): R 101. (8) Mcclave SA, Martindale RG, Vanek VW, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A. S. P. E. N. ). JPEN J Parenter Enteral Nutr. 2009; 33(3): 277 -316. (9) Academy of Nutrition and Dietetics. Pocket Guide for International Dietetics & Nutrition Terminology (IDNT) Reference Manual: Standardized Language for the Nutrition Care Process. Chicago, IL; 2013. (10) Available at: http: //www. mc. vanderbilt. edu/surgery/trauma/Protocols/nutrition-protocol. Accessed December 10, 2013. (11) Pronsky Z, Crowe J. Food Medication Interactions. 16 th ed. Birchrunville, PA: Food-Medication Interactions: 2008.
Questions?