Clinical Case Study ABBY PATTERSON DIETETIC INTERN AUGUSTA

Clinical Case Study ABBY PATTERSON DIETETIC INTERN AUGUSTA HEALTH
Facility -Community hospital w/255 beds -Located in Fishersville, VA -225+ active full-time physicians -875+ volunteers -2300 staff members -12, 000+ annual admissions -60, 000+ emergency room visits/year -500, 000+ visits to outpatient services Received Healthgrades award for 50 best hospitals in 2015
The Role of the RD �Part of the healthcare team �Provide care to patients w/various disease states and conditions �Monitor and assess nutrition status based on medical conditions and overall health status �Coordinates care with members of the medical team �Makes recommendations for nutrition support �Educates patients about discharge diet planning in order to prevent disease progression or manage disease, achieve/maintain healthy lifestyle �Outpatient services
C. M. 80 year old male w/bowel obstruction 5’ 9” 71. 1 kg BMI 23. 1 WNL (Obtained from EMR) Pmh: COPD, HTN, ? Et. OH abuse, PVD s/p recent aortic endograft placement, hx of DVT Social/family history: � Temporary resident at Kings Daughter Nursing Home in the one week between admission at Rockingham and AH. � Heavy smoker, about a pack/day since he was a teenager � Living independently before nursing home � Has 4 children
C. M. �History of low sodium diet PTA � 1 need per RN screen- poor app > 3 days �No previous admissions in EMR �No records of previous nutrition education or recent food intakes PTA. Pt w/poor po and appetite.
C. M. - PTA: King’s Daughter Nursing Home for three days, s/p aortic endograft placement at Rockingham Memorial Hospital - Patient presents to AH w/abdominal distention and vomiting, stating that he felt constipated. - Poor app PTA x 7 days since procedure at Rockingham. - Admitted for bowel obstruction. - Pt w/cecal obstruction, undergoes exploratory laparotomy w/R hemicolectomy.
Assessment of C. M. �Nutrition status: poor intakes and appetite for one week �Risks factors Recent procedure at RMH Bowel obstruction Age Past medical history Hx tobacco abuse and possible Et. OH Poor appetite/intakes Surgeon anticipating post-op ileus, orders TPN

Nutrition Diagnosis PES statements: Altered GI function related to bowel obstruction and Rhemicolectomy as evidenced by n/v/d, need for TPN Altered GI function related to post-op ileus as evidenced by the need for TPN and gradual diet advance. Inadequate protein-energy intake related to surgery, physical deconditioning, as evidenced by lack of appetite and po intakes thus far.
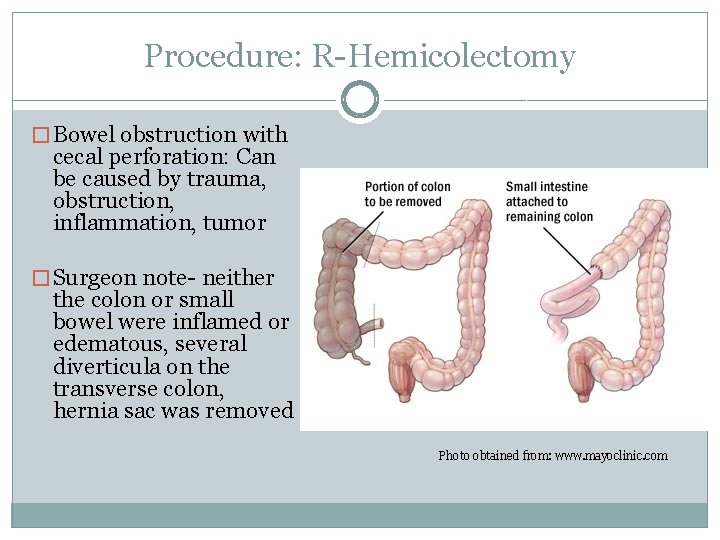
Procedure: R-Hemicolectomy � Bowel obstruction with cecal perforation: Can be caused by trauma, obstruction, inflammation, tumor � Surgeon note- neither the colon or small bowel were inflamed or edematous, several diverticula on the transverse colon, hernia sac was removed Photo obtained from: www. mayoclinic. com
Bowel Obstruction � Blockage that prevents the passage of fluid/food � Causes: adhesions, hernia, tumors, inflammatory bowel disease � Pts with any type of bowel surgery should be considered high risk unless they are eating regularly prior to the surgery without any n/v/d � Higher risk patients: poor po prior to surgery, n/v/d, older age, comorbidities, reduced transport proteins indicating underlying inflammation or infection (albumin and prealbumin) � Potential risks w/surgery: malabsorption of fluids and nutrients, need for TPN � Must pay close attention to electrolytes postoperatively
Bowel Obstruction �Large intestine- important for fluid and electrolyte absorption (absorbs 1 -1. 5 L fluid/day), specifically Na, Chl, K �Research has shown that post-op patients showed no difference in tolerance on a CL diet vs regular diet. Advancing from CL to FL, not always necessary FL diets- high in fat, may not be tolerated well after bowel surgery �Normal progression: Wait for bowel function to return, initiate CL �If patient has an ileus, initiate TPN �Typical treatment: Bowel obstruction may resolve on it’s own or surgery may be indicated
Intervention �NPO �TPN until bowel function is restored- start with refeeding needs, advance to goal �Gradual diet advance
PPN/TPN PPN initiated immediately (1800 on 7/6) Dextrose, AA, lipids Mag sulf (16 m. L), MVI (10 m. L), Trace elements (10 m. L) , add Folic acid for about 1 day, Thiamin for about 3 days (Wernicke’s), Zantac (acid reflux) �Check triglycerides �Accuchecks every 6 hours for the first few days to make sure that blood sugars are <180 Patient’s BG was checked every 6 hours from 7/6 -7/9 and were within acceptable range of <180: 111, 146, 124, 148, 121, 124, 114
PPN/TPN � PPN- short-term nutrition support � Because of the high volume of fluid needed, pts requiring fluid restrictions cannot receive PPN � Infusion rates >150 may be needed to meet patients needs � Peripheral lines should be changed every 48 -72 hours to reduce infection risk and thrombophlebitis � Easily placed and removed � PPN- larger volume than TPN, more diluted. � TPN- more concentrated, less volume with a central line � Decreased rate of infection compared to other central lines � PICC- Not as long term as other central catheters- ~1 year � May be placed by a trained RN
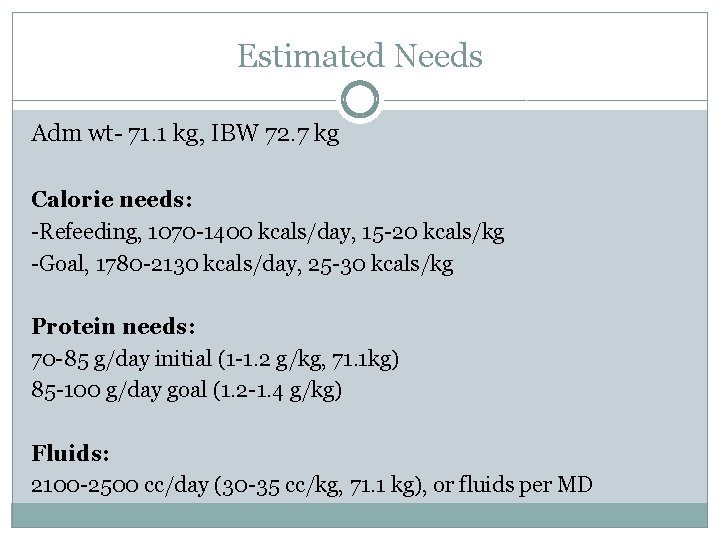
Estimated Needs Adm wt- 71. 1 kg, IBW 72. 7 kg Calorie needs: -Refeeding, 1070 -1400 kcals/day, 15 -20 kcals/kg -Goal, 1780 -2130 kcals/day, 25 -30 kcals/kg Protein needs: 70 -85 g/day initial (1 -1. 2 g/kg, 71. 1 kg) 85 -100 g/day goal (1. 2 -1. 4 g/kg) Fluids: 2100 -2500 cc/day (30 -35 cc/kg, 71. 1 kg), or fluids per MD
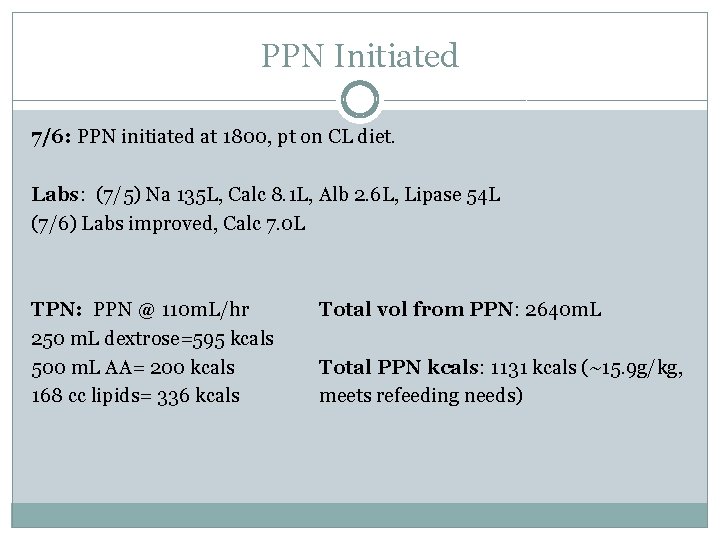
PPN Initiated 7/6: PPN initiated at 1800, pt on CL diet. Labs: (7/5) Na 135 L, Calc 8. 1 L, Alb 2. 6 L, Lipase 54 L (7/6) Labs improved, Calc 7. 0 L TPN: PPN @ 110 m. L/hr 250 m. L dextrose=595 kcals 500 m. L AA= 200 kcals 168 cc lipids= 336 kcals Total vol from PPN: 2640 m. L Total PPN kcals: 1131 kcals (~15. 9 g/kg, meets refeeding needs)
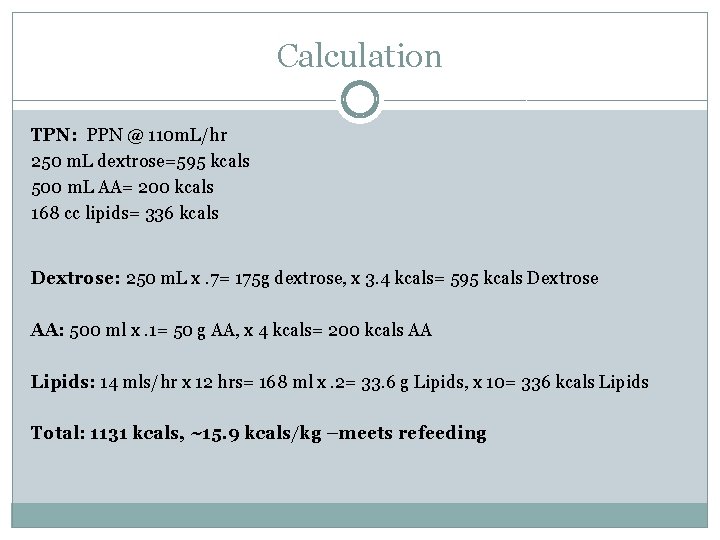
Calculation TPN: PPN @ 110 m. L/hr 250 m. L dextrose=595 kcals 500 m. L AA= 200 kcals 168 cc lipids= 336 kcals Dextrose: 250 m. L x. 7= 175 g dextrose, x 3. 4 kcals= 595 kcals Dextrose AA: 500 ml x. 1= 50 g AA, x 4 kcals= 200 kcals AA Lipids: 14 mls/hr x 12 hrs= 168 ml x. 2= 33. 6 g Lipids, x 10= 336 kcals Lipids Total: 1131 kcals, ~15. 9 kcals/kg –meets refeeding
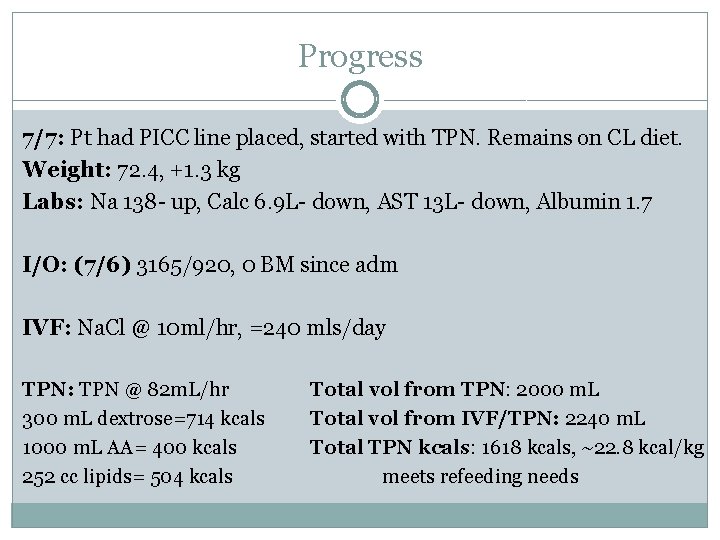
Progress 7/7: Pt had PICC line placed, started with TPN. Remains on CL diet. Weight: 72. 4, +1. 3 kg Labs: Na 138 - up, Calc 6. 9 L- down, AST 13 L- down, Albumin 1. 7 I/O: (7/6) 3165/920, 0 BM since adm IVF: Na. Cl @ 10 ml/hr, =240 mls/day TPN: TPN @ 82 m. L/hr 300 m. L dextrose=714 kcals 1000 m. L AA= 400 kcals 252 cc lipids= 504 kcals Total vol from TPN: 2000 m. L Total vol from IVF/TPN: 2240 m. L Total TPN kcals: 1618 kcals, ~22. 8 kcal/kg meets refeeding needs
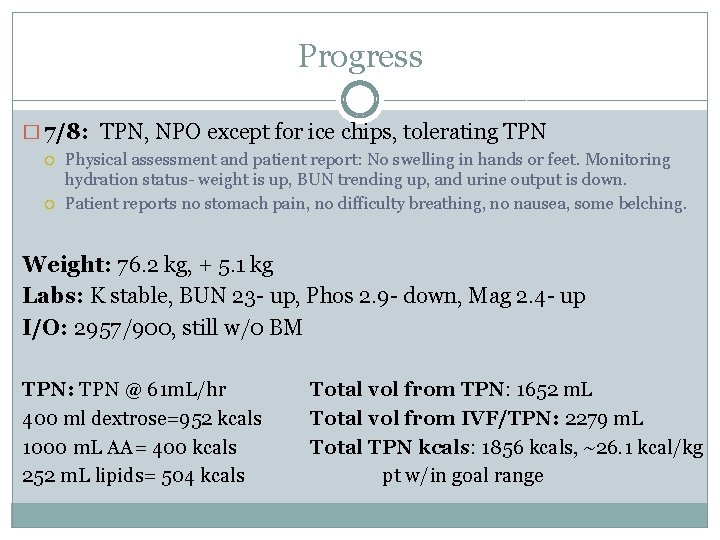
Progress � 7/8: TPN, NPO except for ice chips, tolerating TPN Physical assessment and patient report: No swelling in hands or feet. Monitoring hydration status- weight is up, BUN trending up, and urine output is down. Patient reports no stomach pain, no difficulty breathing, no nausea, some belching. Weight: 76. 2 kg, + 5. 1 kg Labs: K stable, BUN 23 - up, Phos 2. 9 - down, Mag 2. 4 - up I/O: 2957/900, still w/0 BM TPN: TPN @ 61 m. L/hr 400 ml dextrose=952 kcals 1000 m. L AA= 400 kcals 252 m. L lipids= 504 kcals Total vol from TPN: 1652 m. L Total vol from IVF/TPN: 2279 m. L Total TPN kcals: 1856 kcals, ~26. 1 kcal/kg pt w/in goal range
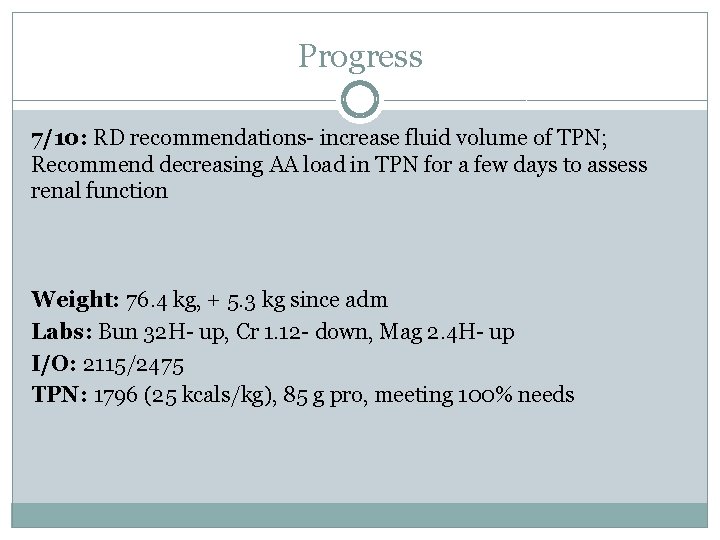
Progress 7/10: RD recommendations- increase fluid volume of TPN; Recommend decreasing AA load in TPN for a few days to assess renal function Weight: 76. 4 kg, + 5. 3 kg since adm Labs: Bun 32 H- up, Cr 1. 12 - down, Mag 2. 4 H- up I/O: 2115/2475 TPN: 1796 (25 kcals/kg), 85 g pro, meeting 100% needs
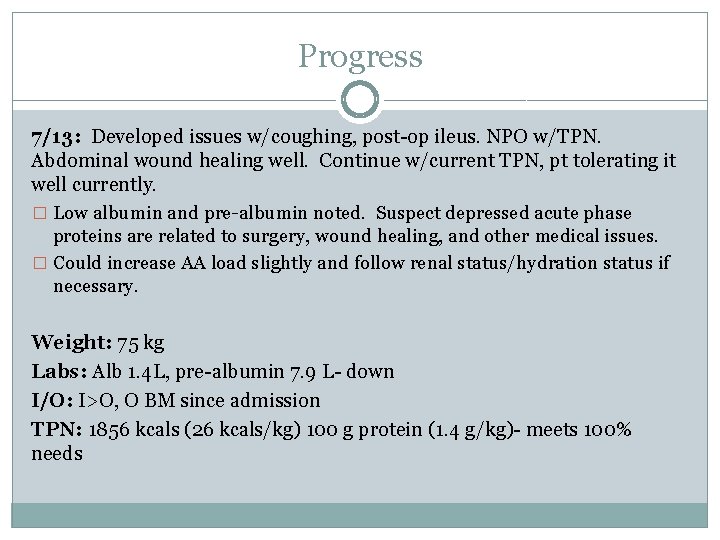
Progress 7/13: Developed issues w/coughing, post-op ileus. NPO w/TPN. Abdominal wound healing well. Continue w/current TPN, pt tolerating it well currently. � Low albumin and pre-albumin noted. Suspect depressed acute phase proteins are related to surgery, wound healing, and other medical issues. � Could increase AA load slightly and follow renal status/hydration status if necessary. Weight: 75 kg Labs: Alb 1. 4 L, pre-albumin 7. 9 L- down I/O: I>O, O BM since admission TPN: 1856 kcals (26 kcals/kg) 100 g protein (1. 4 g/kg)- meets 100% needs
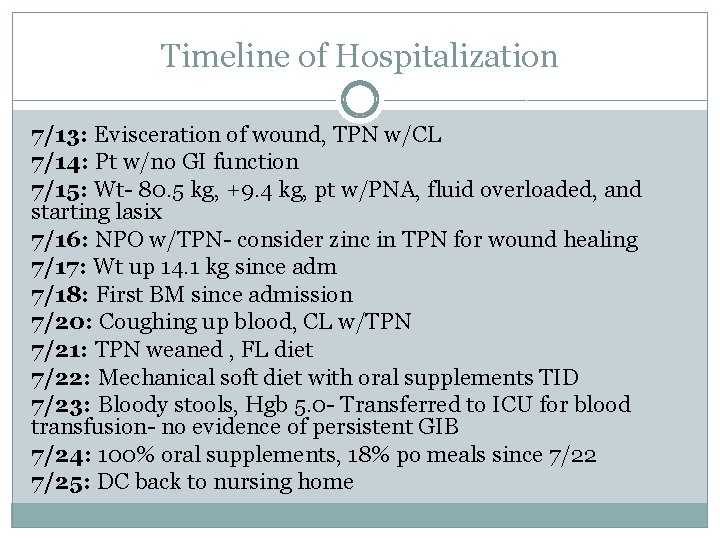
Timeline of Hospitalization 7/13: Evisceration of wound, TPN w/CL 7/14: Pt w/no GI function 7/15: Wt- 80. 5 kg, +9. 4 kg, pt w/PNA, fluid overloaded, and starting lasix 7/16: NPO w/TPN- consider zinc in TPN for wound healing 7/17: Wt up 14. 1 kg since adm 7/18: First BM since admission 7/20: Coughing up blood, CL w/TPN 7/21: TPN weaned , FL diet 7/22: Mechanical soft diet with oral supplements TID 7/23: Bloody stools, Hgb 5. 0 - Transferred to ICU for blood transfusion- no evidence of persistent GIB 7/24: 100% oral supplements, 18% po meals since 7/22 7/25: DC back to nursing home
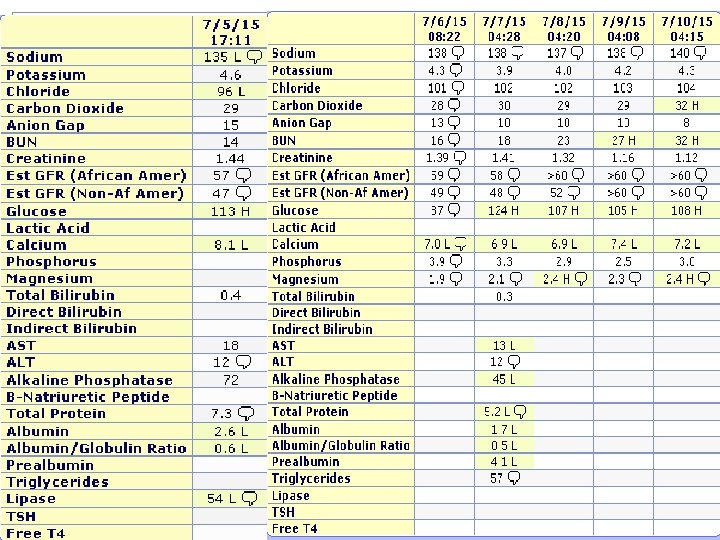
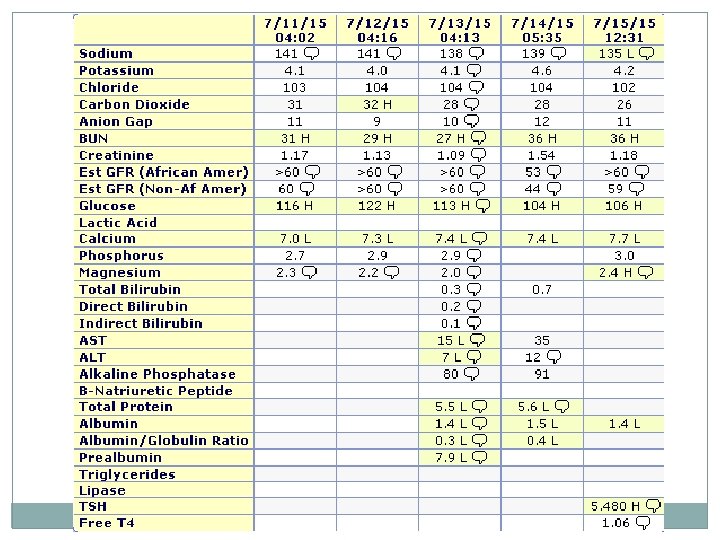
Labs
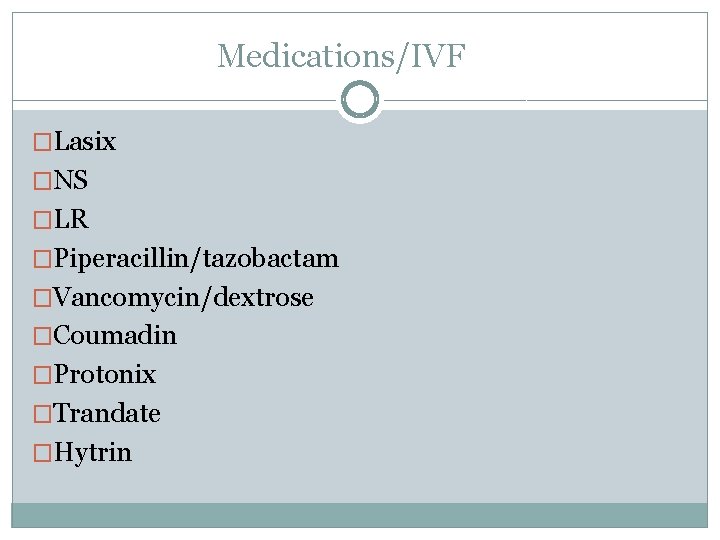
Medications/IVF �Lasix �NS �LR �Piperacillin/tazobactam �Vancomycin/dextrose �Coumadin �Protonix �Trandate �Hytrin
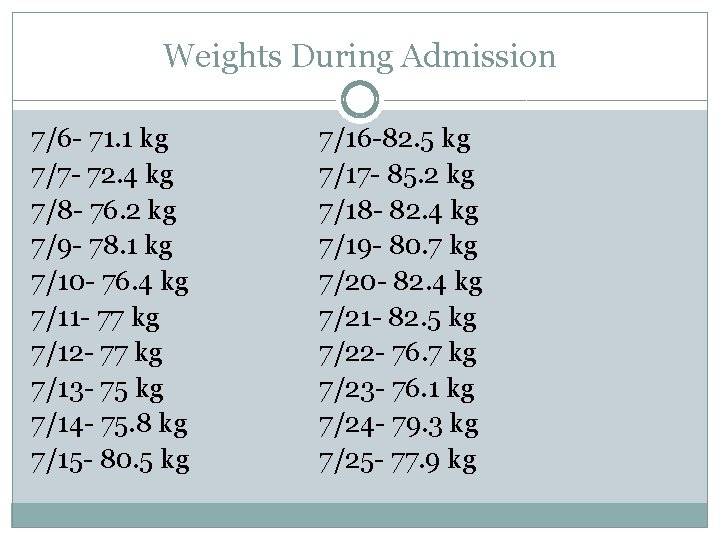
Weights During Admission 7/6 - 71. 1 kg 7/7 - 72. 4 kg 7/8 - 76. 2 kg 7/9 - 78. 1 kg 7/10 - 76. 4 kg 7/11 - 77 kg 7/12 - 77 kg 7/13 - 75 kg 7/14 - 75. 8 kg 7/15 - 80. 5 kg 7/16 -82. 5 kg 7/17 - 85. 2 kg 7/18 - 82. 4 kg 7/19 - 80. 7 kg 7/20 - 82. 4 kg 7/21 - 82. 5 kg 7/22 - 76. 7 kg 7/23 - 76. 1 kg 7/24 - 79. 3 kg 7/25 - 77. 9 kg
Monitor/Evaluate � Labs � Weights � TPN orders � Physical assessment � I/O � Bowel function � Wound healing � IVF/Med changes � Plan of care Goals: Prevent significant weight loss, PO to meet needs, tolerate TPN, maintain hydration, promote wound healing, improvement in GI function, 75% oral supplement- goals were met!
Discharge Planning �King’s Daughter Nursing Home �Mechanical soft diet �Oral supplements 5 x/day �Pertinent meds: Lasix, iron supplement �Discharged on July 25 after 20 days at AH
References Jeffery KM, Harkins B, Cresci GA, Martindale RG. The clear liquid diet is no longer a necessity in the routine postoperative management of surgical patients. Am Surg. 1996; 62(3): 167 -170. Madsen, H, Frankel, E. The Hitchhiker’s Guide to Parenteral Nutrition Management. Nutrition Issues in Gastroenterology, series #40. July 2006. Parrish, CR. A Patient’s Guide to Managing a Short Bowel. 2011. Parrish CR. The Clinician's Guide to Short Bowel Syndrome. Pract Gastroenterol. 2005: 67. Shopbell JM, Hopkins B, Shronts EP. Nutrition Screening and Assessment. The Science and Practice of Nutrition Support. 2001: 124 -130.
- Slides: 29