CLINICAL AUDIT Practical Considerations for Allied Health Professionals
- Slides: 22
CLINICAL AUDIT Practical Considerations for Allied Health Professionals www. unisa. edu. au/cahe
Clinical Audit • Clinical effectiveness • Process for comparing • Improving standards of care
Clinical Audit Clinical audit is a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change. Aspects of the structure, process and outcomes of care selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at an individual, team, or service level and further monitoring is used to confirm improvement in healthcare delivery. Principles of Best Practice in Clinical Audit
Goals of Clinical Audit • Improve patient care • Improve health outcomes • Translate research into practice
Why do a clinical quality audit? Benefits all stakeholders in health care • Monitor clinical performance • Continuous improvement in the standards of patient care • Used as a change management tool • Allows for the best use of resources • Overall improved satisfaction from consumers 5
The Audit Cycle Answers 3 key questions 1. What are you trying to accomplish? 2. What changes can be made to produce an improvement? 3. How will you know that such changes have produced an improvement? 6
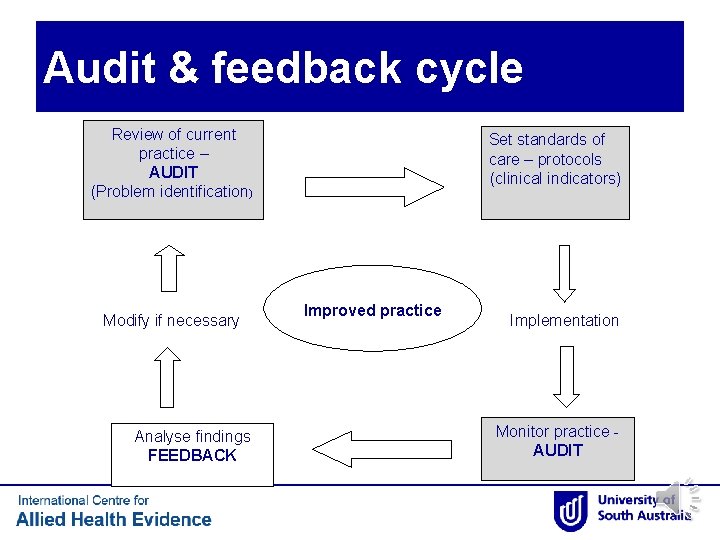
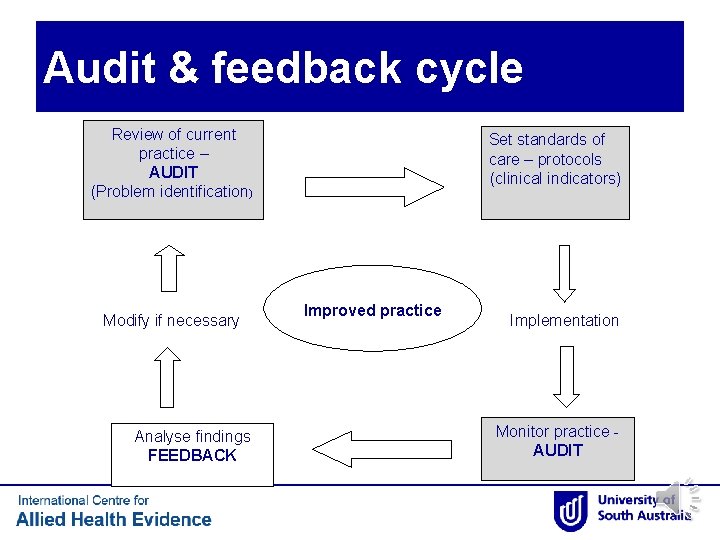
Audit & feedback cycle Review of current practice – AUDIT (Problem identification) Modify if necessary Analyse findings FEEDBACK Set standards of care – protocols (clinical indicators) Improved practice Implementation Monitor practice AUDIT
Problem Identification • Focus on areas that there is perceived inadequacy • Look at research evidence • Clinical governance • Complaints • New standards/guidelines are made available
Setting Standards • Evidence-based research • Consensus-based standards • Gold standard
Measurement • Structure Criteria – What is needed to implement the standard • Process Criteria – What needs to be done to implement the standard • Outcome Criteria – What is the expected to be achieved by implementing the standard
Patient Perspective and Input • Satisfaction measures • Experience measures • Outcome measures
Clinical indicators Also called process indicators, performance indicators • They define your standards of care by setting a specific and objective measure. • They describe an element of clinical care – Example: PEG insertion prior to head/neck cancer surgery • Can be a measure of compliance only, or include timeliness or other elements
Auditable clinical indicators • Make your clinical indicators auditable • Retrospective audits - the information must routinely be in medical records • Prospective audits - information collected on purpose built data sheets as you go (harder to set up) • Write the clinical indicator carefully – make sure you can measure it.
Auditable clinical indicators • Define eligibility - the patients who will /will not be expected to get the care. • Are there exceptions? For instance if patient admitted over a weekend do you expect the same timeliness of care? • Define the compliance standards for eligible patients (% compliance)
Audit data What audit data will you collect? • Keep it simple = manageable. • What do you really need to know? • What demographics are important? (often none) • Enable double checking if required
How to sample • Sample size? • Often don’t need many for an in-house quality audit. Consider the proportion of your patients (10 patients may be 20% of your annual patient population if n=50) • Sample bias – don’t cherry pick. Consecutive admission is good and simple.
Data management • Collect data onto specifically developed tables/ spread sheets • Set it out in an order that makes auditing easier & time efficient
Achieving Change • Developing an action plan – Training – System-wide change – Behavioural change
Reflection post-audit • Clinical audit must be cyclical • Sustainability of change • Share your success story!
How can i. CAHE help? • ASPIRE – The ASPIRE for quality is an evidence-based tool developed by the International Centre for Allied Health Evidence to evaluate clinical service performance in South Australian Local Health Networks. – Lizarondo L, Grimmer K, Kumar S. Assisting allied health in performance evaluation: a systematic review. BMC health services research. 2014; 14(1): 572. – http: //www. unisa. edu. au/Research/Sansom-Institute-for-Health. Research/Allied-Health-Evidence/Quality-Care/ASPIREfor-quality/
Acknowledgments We would like to recognise the contributions of • Dr Julie Luker • Ms Deb Kay 21
References 1. 2. 3. 4. Buckingham, R. , J. Potter, and A. Wagg, Clinical Audit of Healthcare, in Pathy's Principles and Practice of Geriatric Medicine. 2012, John Wiley & Sons, Ltd. p. 1673 -1685. Johnston, G. , et al. , Reviewing audit: barriers and facilitating factors for effective clinical audit. Qual Health Care, 2000. 9(1): p. 23 -36. Patel, S. , Identifying best practice principles of audit in health care. Nurs Stand, 2010. 24(32): p. 40 -8; quiz 49. Seddon, M. and J. Buchanan, Quality improvement in New Zealand healthcare. Part 3: achieving effective care through clinical audit. N Z Med J, 2006. 119(1239): p. U 2108.