Cleft Lip and Cleft palate Prepared by Mrs
Cleft Lip and Cleft palate Prepared by: Mrs. Renita Priya Dsouza Asst. Professor YNC
INTRODUCTION • Cleft is a fissure or opening – a gap. • It is the non-fusion of the body’s natural structures that form before birth. • Cleft lip (cheiloschisis) and cleft palate (palatoschisis) are birth defects, that affect the upper lip and roof of the mouth, in which there is an opening in the lip and/or palate that is caused by incomplete development during early fetal formation
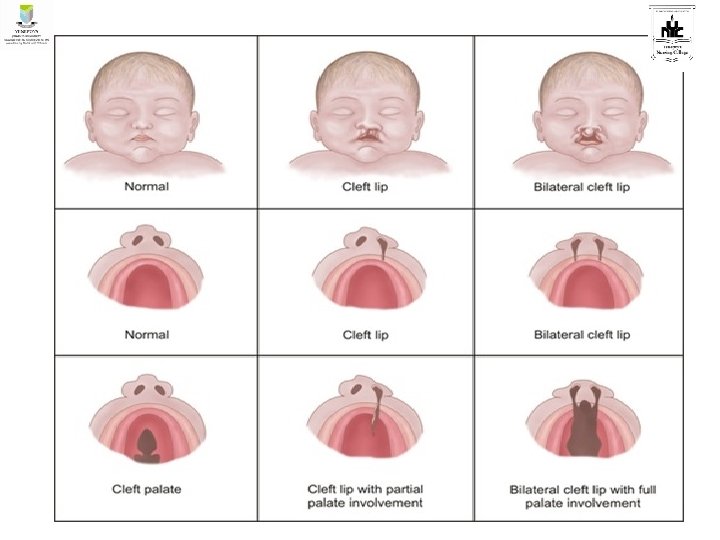
DEFINITION • Cleft Lip (Cheiloschisis): “ It is defined as a congenital anomaly in which there is presence of a fissure at upper lip which occurs due to failure of fusion of the maxillary and median nasal processes” • Cleft Palate (Palatoschisis): “It is defined as a congenital anomaly in which there is a fissure at roof of the mouth which occurs due to failure of fusion of the lateral palatine processes, the nasal septum and the median palatine processes. ”
CAUSES • Genetic factor • • Maternal factors: Viral infection, ingestion of drugs, exposure to radiation, anaemia, hypoproteinemia • • Environmental factors • • Teratogenic drugs • • Family history
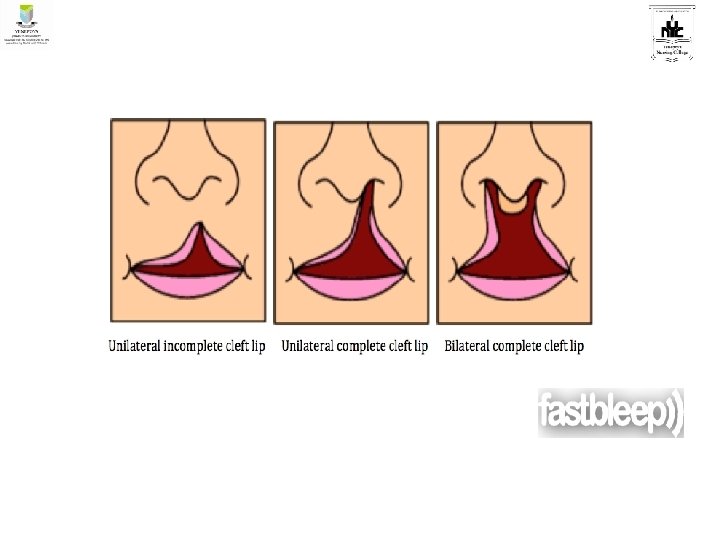
Cleft lip (cheiloschisis) • Is a congenital anomaly that occurs at a rate of 1 in 800 births. Ø If the cleft does not affect the palate structure of the mouth it is referred to as cleft lip. Ø Cleft lip is formed in the top of the lip as either a small gap or an indentation in the lip (partial or incomplete cleft) or it continues into the nose (complete cleft) Ø Cleft lip can be unilateral or bilateral. • It is due to the failure of fusion of the maxillary and medial nasal processes (formation of the primary palate).
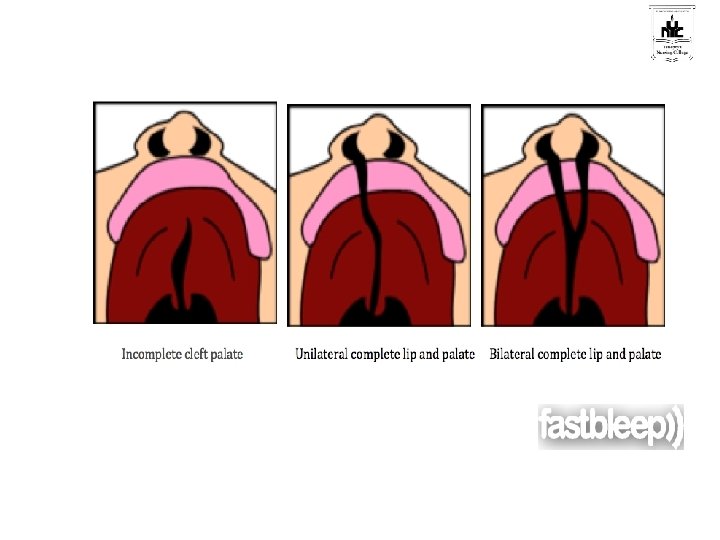
Cleft palate (palatoschisis) • is a congenital anomaly that occurs in approximately 1 of every 2000 births, and it is more common in boys than girls. • It is a condition in which the two plates of the skull that form the hard palate (roof of the mouth) are not completely joined. • It ranges in severity from soft palate involvement alone to a defect including the hard palate and portions of the maxilla. • Cleft palate may or may not be associated with cleft lip.
Pathophysiology • During embryonic development the lateral and medial tissues forming the upper lip palates fuse between weeks 7 and 8 of gestation; the palatal tissues forming the hard and soft palates fuse between weeks 7 and 12 gestation. • Cleft lip and cleft palate result when these tissues fail to fuse.
SIGN AND SYMPTOMS • Feeding problems • Failure to gain weight • Flow of milk through nasal passages during feeding • Poor growth • Repeated ear infections • Speech difficulties • Dental Abnormalities • Speech Difficulties • Middle Ear Fluid Buildup • Hearing Loss
Assessment findings 1. Clinical manifestations • a. Cleft lip and cleft palate are readily apparent at birth. Careful physical assessment should be performed to rule out other midline birth defects. • b. Cleft lip and cleft palate appear as incomplete or complete defects, and may be unilateral or bilateral. • 2. Laboratory and diagnostic study findings. Obstetric ultrasound will reveal cleft lip while the infant is in utero.
MEDICAL MANAGEMENT • Assessment of the child • Reassurance to parents • Feeding the child • Airway clearance • Infection prevention SURGICAL MANAGEMENT • Chieloplasty • Platatoplasty
Management: • Interdisciplinary approach • Management is focused on closure of clefts prevention of complications and facilitating growth and development. • Cleft lip is generally repaired before cleft palate • Cleft palate repair is usually done between 9 -18 months because speech patterns have not been set. • If repair is delayed to age 4 -5 years a special denture palate is used to occlude the cleft and to develop speech pattern.
NURSINGMANAGEMENT Nursing Assessment • Carefully perform the head to toe assessment of the child immediately after the birth • Assess the location and extent of the defect by using gloved finger. • Assess the feeding pattern of the child. • Assess the need for the surgical correction. • Assess the parents understanding of the defect and the need for the surgery.
NURSING DIAGNOSIS • Altered nutrition less than body requirements • Risk for infection. • Risk for aspiration • Ineffective breathing pattern. • Altered family process • Impaired tissue integrity

PREOPERATIVE NURSING MANAGEMENT • Feeding the child: sterile breast feed, appropriate nipple, burp. • Provide right position • Airway clearance • Reassurance to parents. • Hygienic care • Timings – Follow “rule of ten” for surgery-"Rule of 10 s" – 10 weeks old, weight of 10 pounds and 10 grams of hemoglobin.
• Immunization – complete all immunization accordingly before surgery. • Thumb sucking – discourage thumb sucking and prevent it. • Encourage the child to lie on its back for practice regarding post-operative positioning. • Monitor the nutritional status of the child.
• Assess for problems with feeding, breathing parental bonding, and speech. • Ensure adequate nutrition and prevent aspiration. a. Provide special nipples or feeding devices (e. g. , soft pliable bottle with soft nipple with enlarged opening) for a child unable to suck adequately on standard nipples. b. Hold the child in a semi-upright position; direct the formula away from the cleft and toward the side and back of the mouth to prevent aspiration. c. Feed the infant slowly and burp frequently to prevent excessive swallowing of air and regurgitation. d. Stimulate sucking by gently rubbing the nipple against the lower lip.
Provide postoperative care. • Assess airway patency and vital signs; observe for edema and respiratory distress. • Use a mist tent, if prescribed, to minimize edema, liquefy secretions, and minimize distress. • Position the child with cleft lip on her back, in an infant seat, or propped on a side to avoid injury to the operative site; position the child with a cleft palate on the abdomen to facilities drainage. • Clean the suture line and apply an antibacterial ointment as prescribed to prevent infection and scarring. Monitor the site for signs of infection.
• Use elbow restraints to maintain suture line integrity. Remove them every 2 hours for skin care and range-of-motion exercises. • Feed the infant with a rubber-tipped medicine dropper, bulb syringe, or soft bottle-nipples, as prescribed, to help preserve suture integrity. • For older children, diet progresses from clear fluids; they should not use straws or sharp objects. • Attempt to keep the child from putting tongue up to palate sutures. • Manage pain by administering analgesic as prescribed.
POST OPERATIVE NURSING MANAGEMENT • Assess vital signs of child regularly • Reposition the infant every 2 hourly • Clean the suture line with the saline solution and a cotton tipped applicator • Anticipate the child’s need to decrease his crying • Give general post-operative care to the child • Provide side-lying position to drain secretions and prevent aspiration • Protection of surgical sutured • Provide supine position • Maintain protective device on sutures • Provide elbow restrain • Assess the child for irritability, loss of appetite and restlessness every 2 hrs of the surgery • Maintain aseptic dressing with precautions • Avoid injury to mouth of the child • Feeding with medicine dropper • Parental counselling is an important thing and advise about care, feeding and follow up etc

Provide child and family teaching. • Demonstrate surgical wound care. • Show proper feeding techniques and positions. • Explain that temperature of feeding formulas should be monitored closely because new palate has no nerve endings; therefore; the child can suffer a burn to the palate easily and without knowing it. • Explain handling of prosthesis if indicated. • Stress the importance of long-term follow up, including speech therapy, and preventing or correcting dental abnormalities. • Discuss the need for, at least, annual hearing evaluations because of the increased susceptibility to recurrent otitis. The child may require myringotomy and surgical placement of drainage tubes. • Teach infection control measures.
Reference • Hockenberry, Wilson, Judie. Wong’s essentials of pediatric Nursing. South India Edition. Elsevier publication. • Dorothy R Marlow, Barbara A Redding, Raman Kalia. Marlow’s textbook of pediatric Nursing. Harcourt Brace & Company Asia Pte Ltd. • Parul Datta. Pediatric Nursing. 4 th edition. Jaypee Publishers. New Delhi.

THANK YOU
- Slides: 25