Classification of snakes Colubridae Elapidae Viperidae Hydrophidae Most
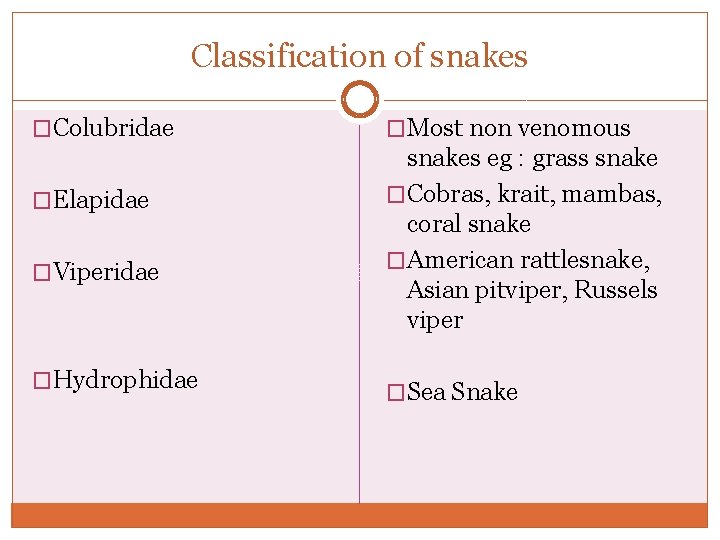
Classification of snakes �Colubridae �Elapidae �Viperidae �Hydrophidae �Most non venomous snakes eg : grass snake �Cobras, krait, mambas, coral snake �American rattlesnake, Asian pitviper, Russels viper �Sea Snake
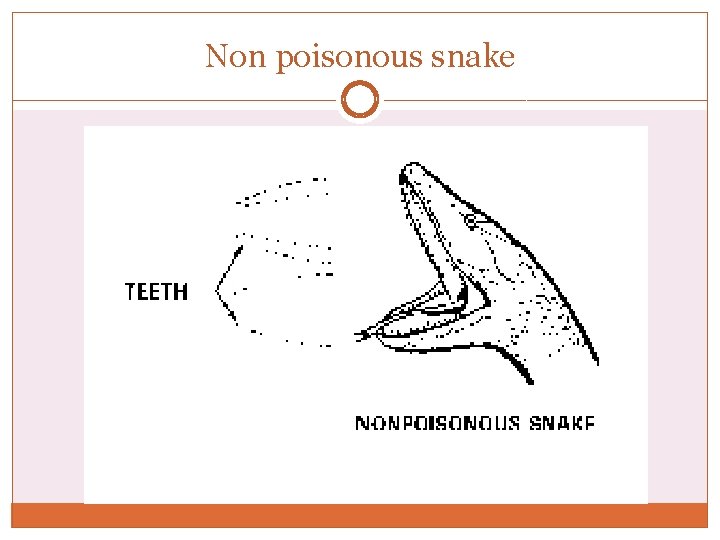
Non poisonous snake

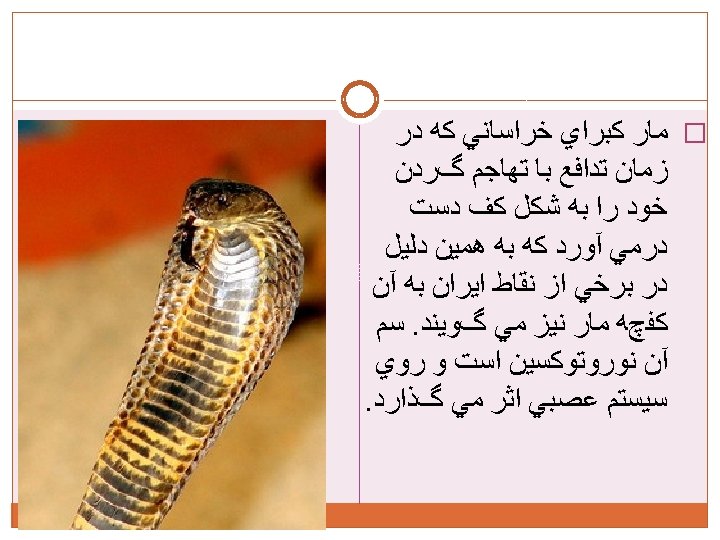
Indian cobra King cobra
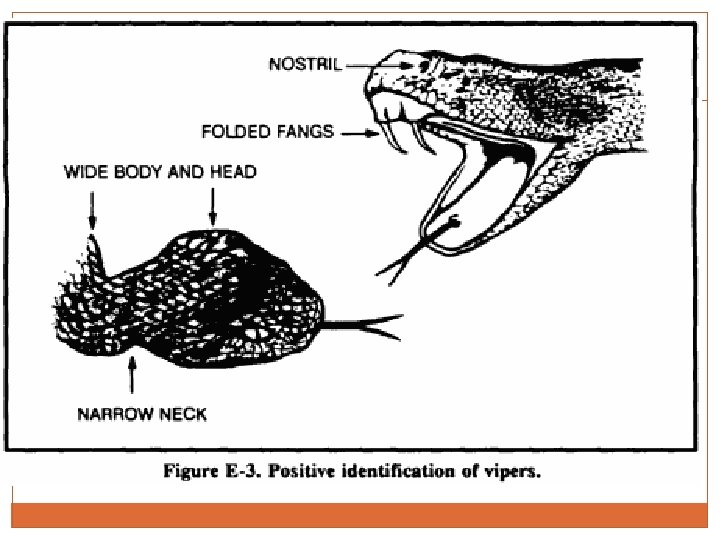
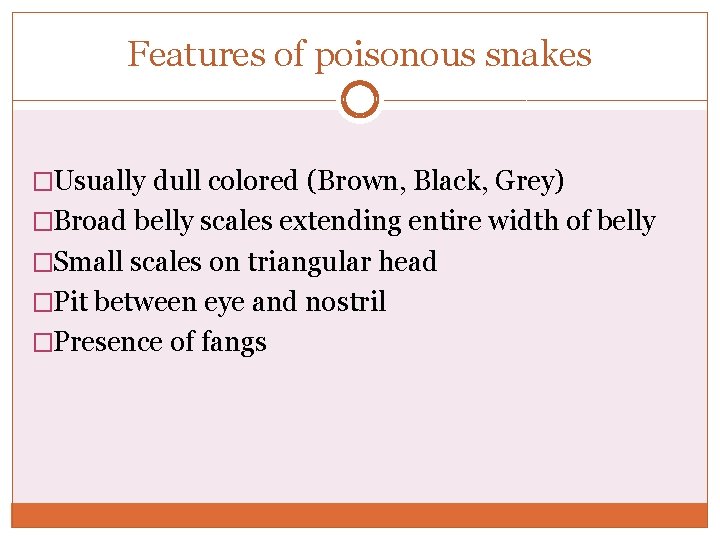
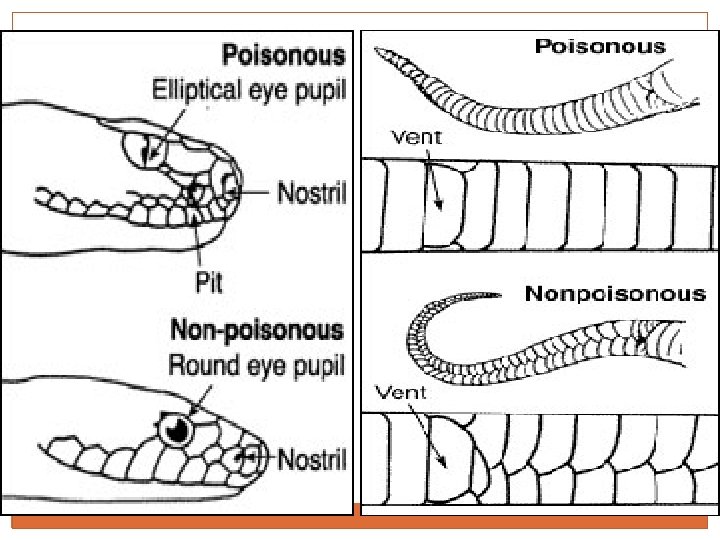
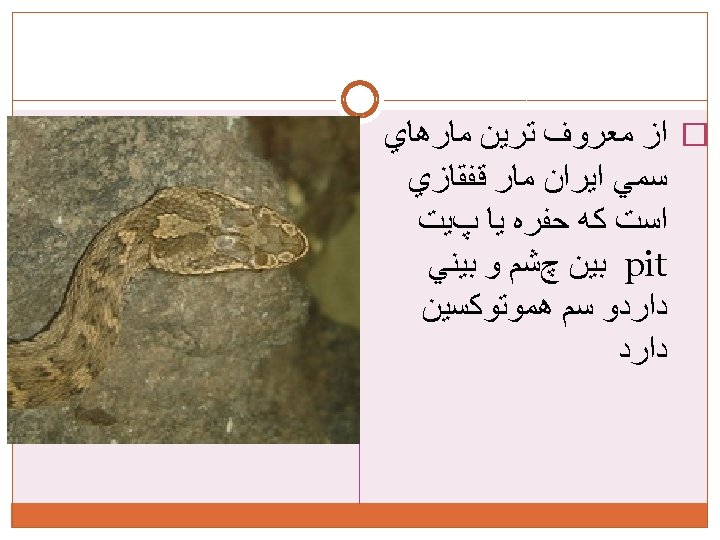
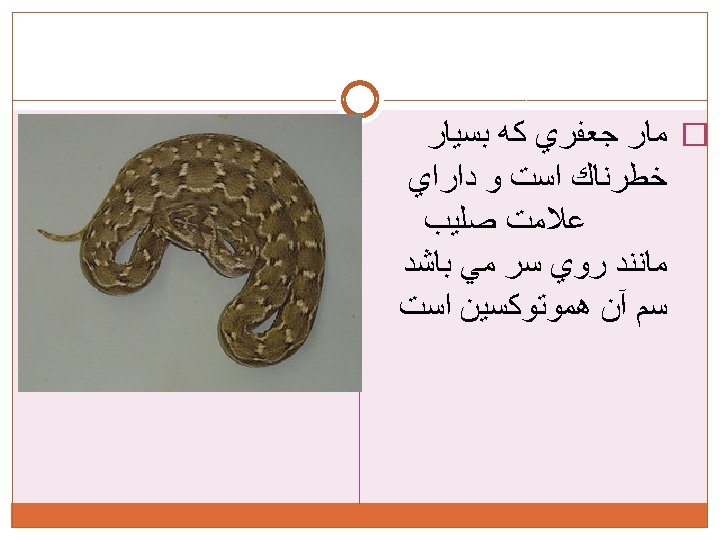
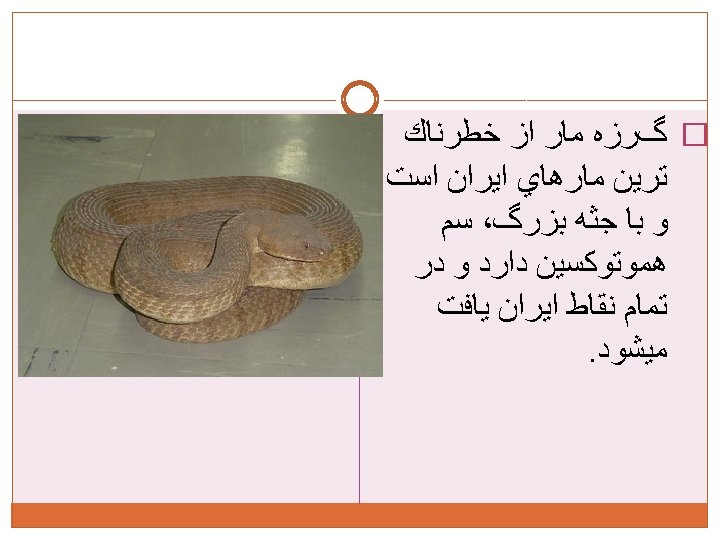
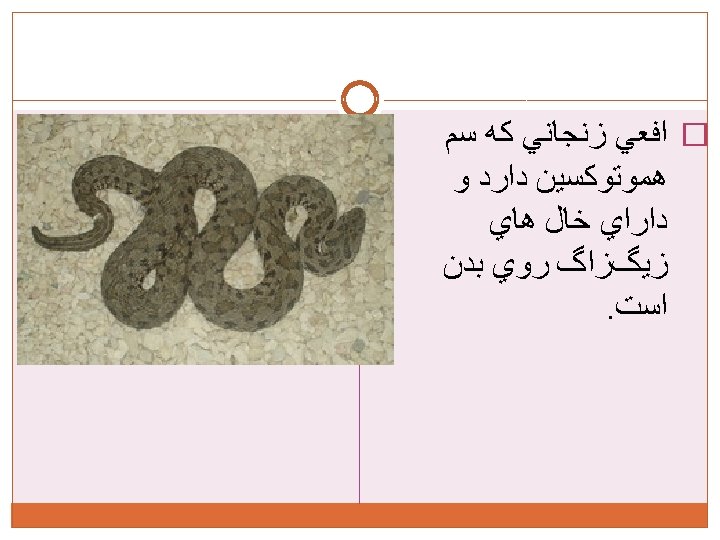
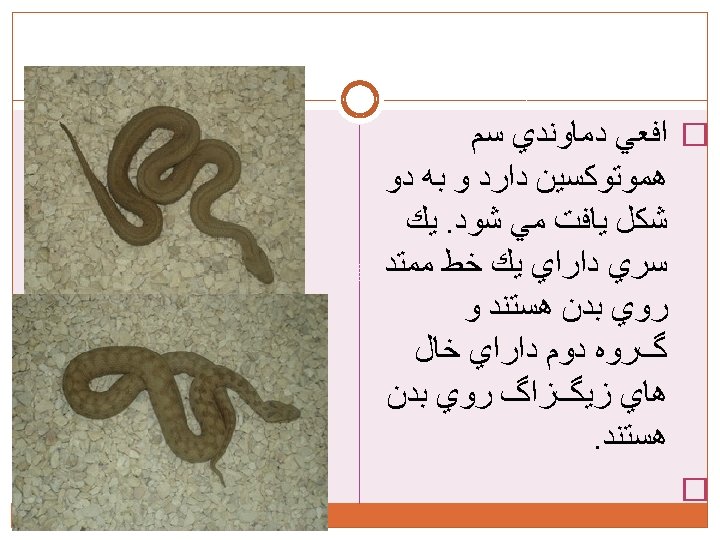
Features of poisonous snakes �Usually dull colored (Brown, Black, Grey) �Broad belly scales extending entire width of belly �Small scales on triangular head �Pit between eye and nostril �Presence of fangs
Snake venom It is complex mixture of enzymes, low. mol. wt polypeptides, glycoproteins, metal ions.
Mechanism of toxicity �Cytotoxic effects on tissues �Hemotoxic �Neurotoxic �Systemic effects. �Cardiotoxic �Nephrptoxic
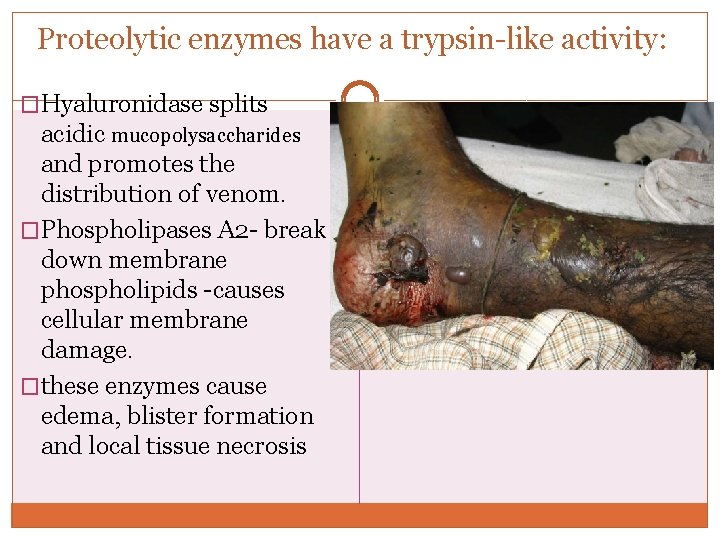
Proteolytic enzymes have a trypsin-like activity: �Hyaluronidase splits acidic mucopolysaccharides and promotes the distribution of venom. �Phospholipases A 2 - break down membrane phospholipids -causes cellular membrane damage. �these enzymes cause edema, blister formation and local tissue necrosis
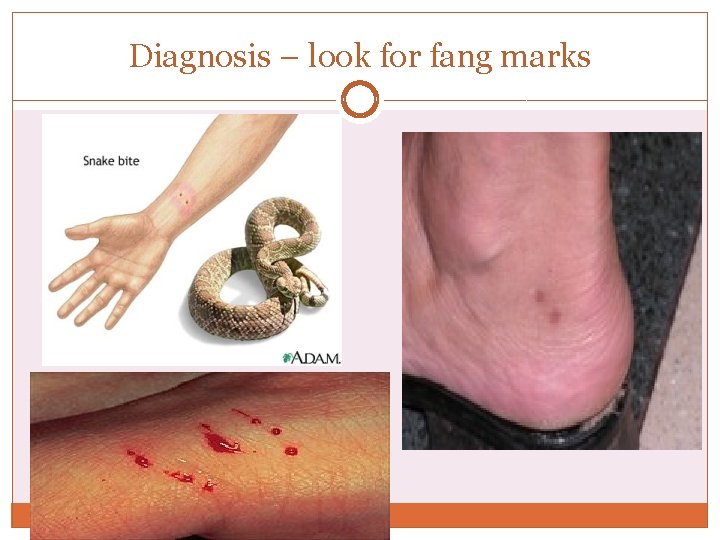
Diagnosis – look for fang marks

Investigations �Complete Blood Count: Anemia, Leukocytosis, Thrombocytopenia, HCT �Evidence of Hemolysis: Fragmented RBCs �Prolonged PT, PTT �Serum Electrolytes: Hyperkalemia �Raised Urea, Creatinine
investigations �U/A: Hematuria, Proteinuria, Hemoglobinuria, Myoglobinuria �ECG: Normal, Bradycardia with ST elevation or depression, T inversion, QT prolongation �ABG: Hypoxemia with Respiratory Acidosis, Metabolic / lactic Acidosis �Chest X- ray: Normal, Pulmonary Edema, Intrapulmonary Hemorrhages, Pleural Effusion
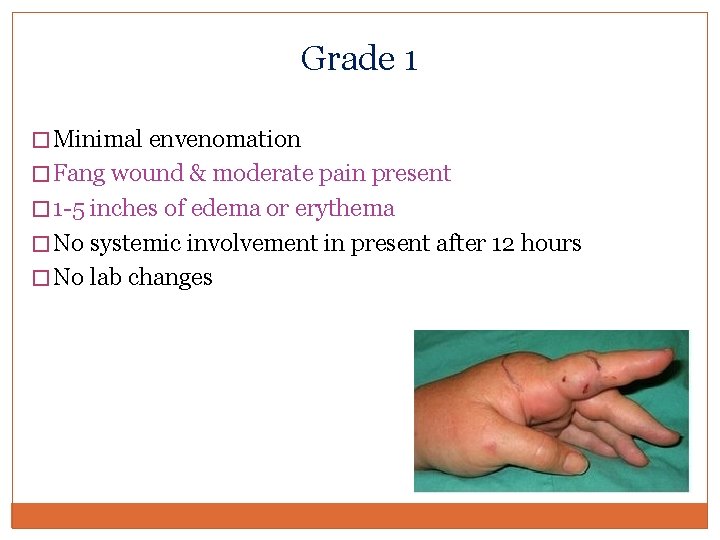
Grade 1 � Minimal envenomation � Fang wound & moderate pain present � 1 -5 inches of edema or erythema � No systemic involvement in present after 12 hours � No lab changes
Grade 2 l Moderate envenomation l Severe pain l Edema spreading towards trunk l Petechia and ecchymosis limited area l Nausea, vomiting, giddiness
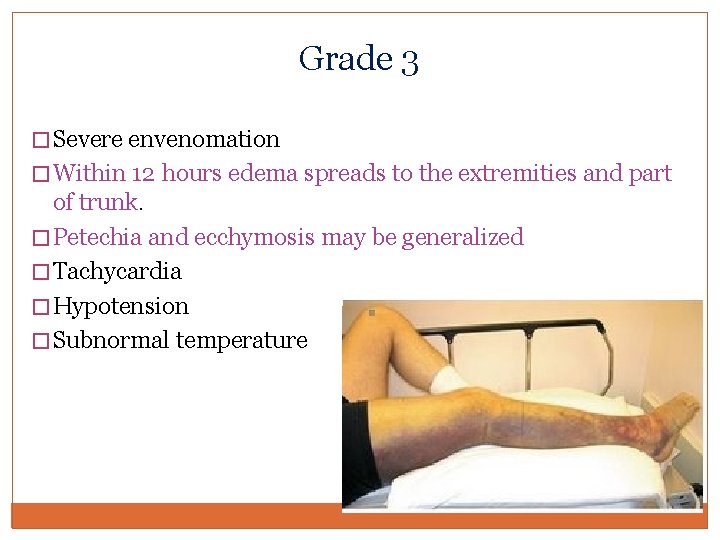
Grade 3 � Severe envenomation � Within 12 hours edema spreads to the extremities and part of trunk. � Petechia and ecchymosis may be generalized � Tachycardia � Hypotension � Subnormal temperature
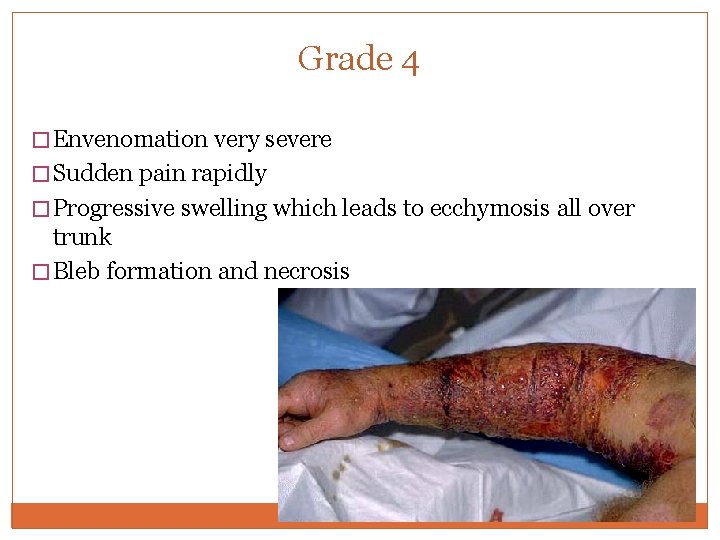
Grade 4 � Envenomation very severe � Sudden pain rapidly � Progressive swelling which leads to ecchymosis all over trunk � Bleb formation and necrosis
Grade 4 contd… � Systemic manifestations within 15 min after the bite � Weak pulse, N&V, vertigo � Convulsions, coma
Treatment protocol �Attend to AIRWAY , BREATHING, CIRCULATION �Tetanus toxoid �Routine antibiotic is not necessary �Identify the snake responsible �All patients should be kept under observation for a min period of 24 hrs. �Determine the exact time of bite �Ask the victim as to what he was doing at the time of bite
�Pain – give Acetaminophen �Not Aspirin & NSAIDS �Care must be taken when removing tight tourniquets tied by victim. Sudden removal can lead to massive surge of venom leading to neurological paralysis, hypotension and vasodilatation.

Indications �As per W. H. O Guidelines ONLY if a pt develops one / more of the following signs/symptoms ASV should be administered : Ø SYSTEMIC ENVENOMING • Evidence of coagulopathy • Evidence of neurotoxicity : ptosis, ophthalmoplegia • CVS abn : hypotension, shock, arrhythmias • ARF • Hemoglobinuria / myoglobinuria • Persistant severe vomiting / abd. pain
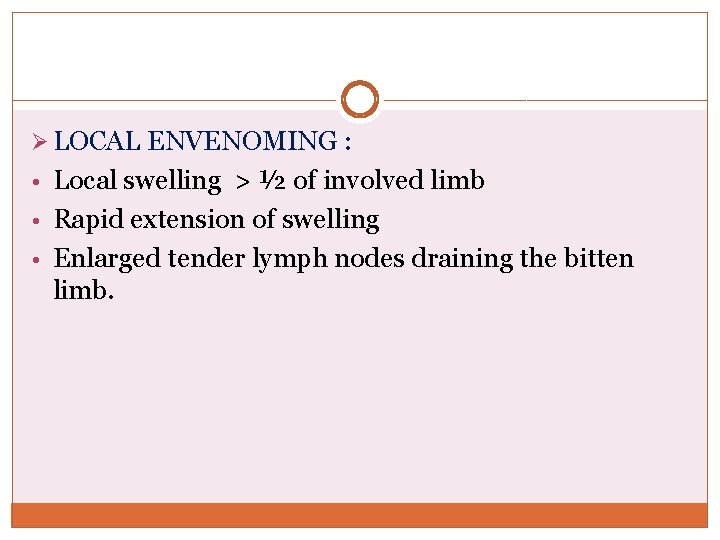
Ø LOCAL ENVENOMING : • Local swelling > ½ of involved limb • Rapid extension of swelling • Enlarged tender lymph nodes draining the bitten limb.
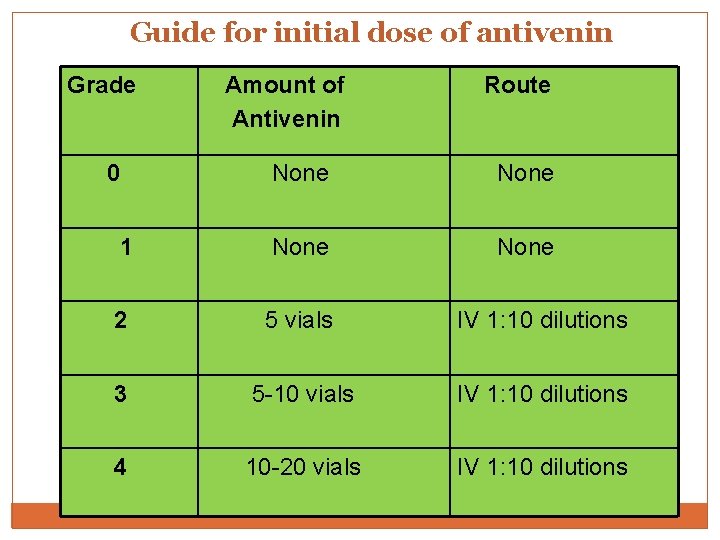
Guide for initial dose of antivenin Grade Amount of Antivenin Route 0 None 1 None 2 5 vials IV 1: 10 dilutions 3 5 -10 vials IV 1: 10 dilutions 4 10 -20 vials IV 1: 10 dilutions
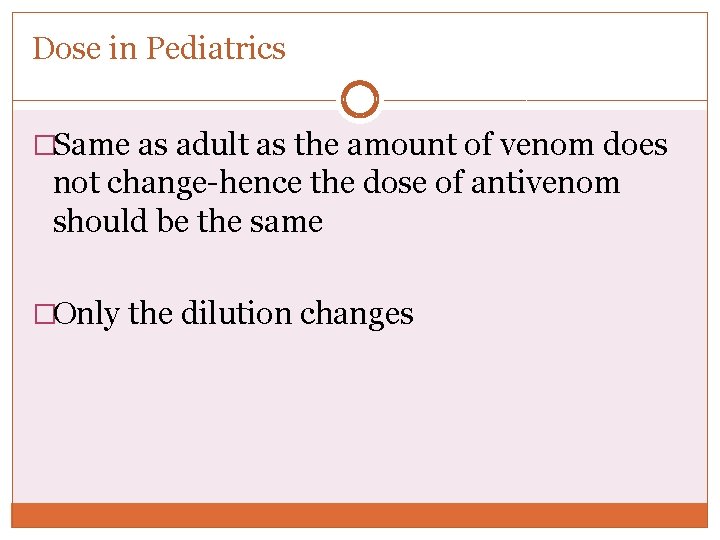
Dose in Pediatrics �Same as adult as the amount of venom does not change-hence the dose of antivenom should be the same �Only the dilution changes
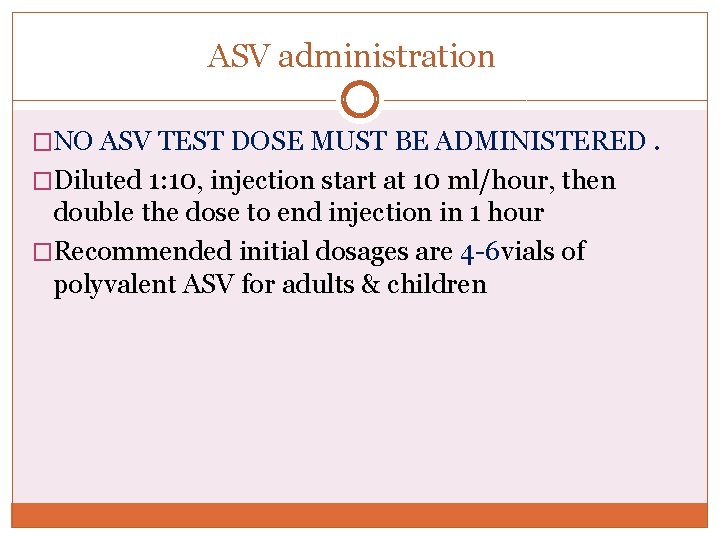
ASV administration �NO ASV TEST DOSE MUST BE ADMINISTERED. �Diluted 1: 10, injection start at 10 ml/hour, then double the dose to end injection in 1 hour �Recommended initial dosages are 4 -6 vials of polyvalent ASV for adults & children
When to stop using ASV �Bleeding subsides �Lab values returns to baseline �Signs of neurotoxicity reverses �Local effects halts progression
Bites by Elapids �Generally cause minimal local effects �Swelling, local pain & local necrosis ( cobra ) �Descending paralysis, initially of muscles innervated by cranial nerves commencing with PTOSIS, DIPLOPIA, OPHTHALMOPLEGIA �Numbness around lips & mouth, progressing to pooling of secretions, bulbar paralysis & resp. failure �Paradoxical resp – intercostal muscle paralysis
�Postsynaptic effects are reversible with antivenom and neostigmine. �Presynaptic nerve terminal, e. g. beta-bungarotoxin and here neostigmine will not be effective.
Compartment syndrome If signs of compartment syndrome are present and compartment pressure > 30 mm Hg: � Elevate limb � Administer Mannitol 1 -2 g/kg IV over 30 min � Simultaneously administer additional antivenom, 4 -6 vials IV over 60 min If elevated compartment pressure persists another 60 min, consider fasciotomy
Hydrophid bites �Stiffness, ache, tenderness in muscles �Later, rhabdomyolysis, myoglobinuria – resulting in acute renal failure.
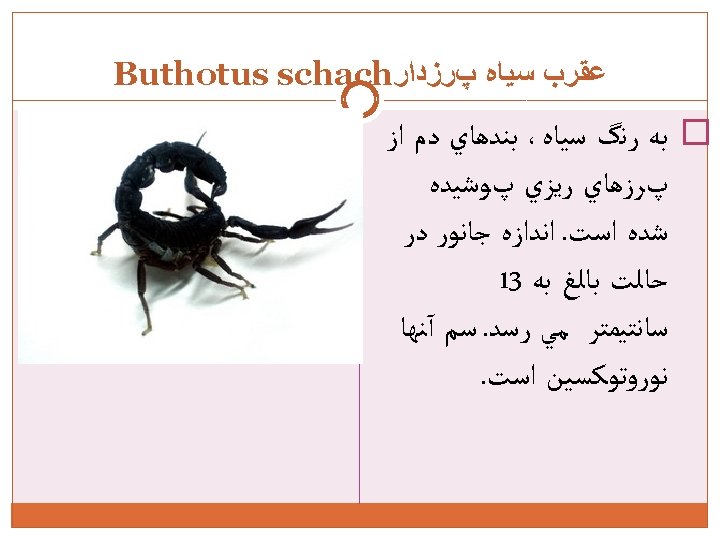

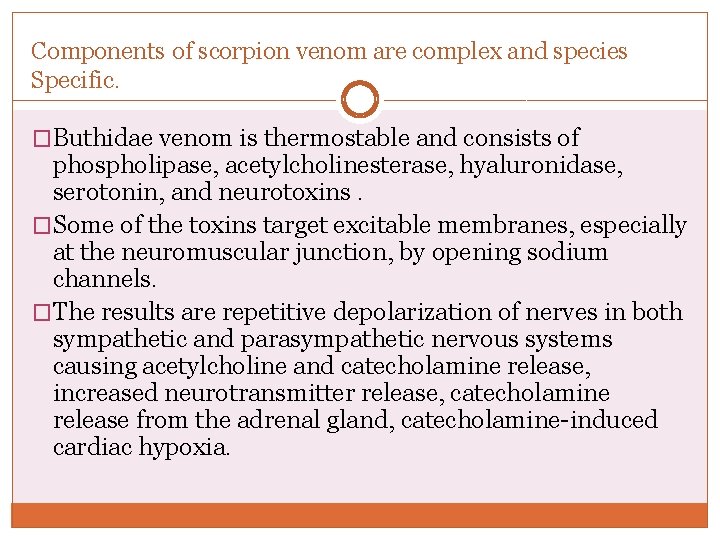
Components of scorpion venom are complex and species Specific. �Buthidae venom is thermostable and consists of phospholipase, acetylcholinesterase, hyaluronidase, serotonin, and neurotoxins. �Some of the toxins target excitable membranes, especially at the neuromuscular junction, by opening sodium channels. �The results are repetitive depolarization of nerves in both sympathetic and parasympathetic nervous systems causing acetylcholine and catecholamine release, increased neurotransmitter release, catecholamine release from the adrenal gland, catecholamine-induced cardiac hypoxia.
� Excessive motor activity � Nausea, vomiting, tachycardia, and severe agitation can also be present. � Cardiac dysfunction, pulmonary edema, pancreatitis, bleeding disorders, skin necrosis, and occasionally death can occur
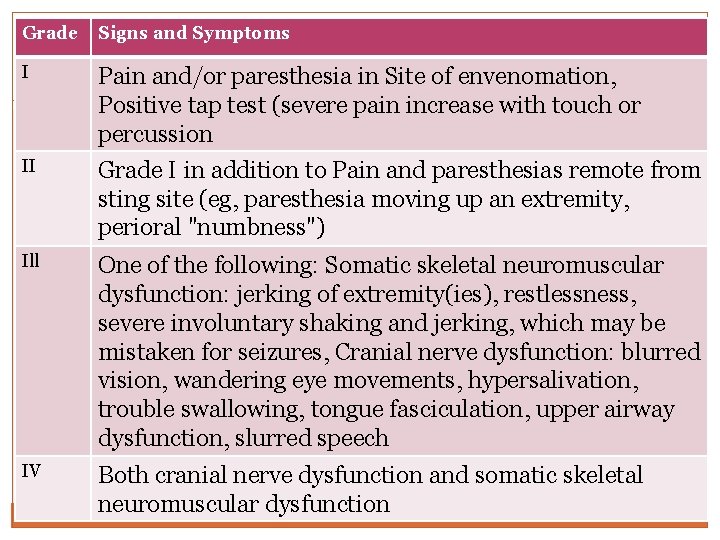
Grade Signs and Symptoms I Pain and/or paresthesia in Site of envenomation, Positive tap test (severe pain increase with touch or percussion II Grade I in addition to Pain and paresthesias remote from sting site (eg, paresthesia moving up an extremity, perioral "numbness") Ill One of the following: Somatic skeletal neuromuscular dysfunction: jerking of extremity(ies), restlessness, severe involuntary shaking and jerking, which may be mistaken for seizures, Cranial nerve dysfunction: blurred vision, wandering eye movements, hypersalivation, trouble swallowing, tongue fasciculation, upper airway dysfunction, slurred speech IV Both cranial nerve dysfunction and somatic skeletal neuromuscular dysfunction
Treatment � Pain Management � Ice pack � Immobilization of limb � Local anesthetics are better than opiates � Tetanus prophylaxis, wound care and antibiotics � Benzodiazepines for motor activity.
Contd. . � Stabilize Airway Breathing and Circulation � Hyperdynamic circulation Always combination of alpha blocker with beta blocker to prevent unopposed alpha action causing tachycardia � Nitrates for Hypertension/MI
Contd. . � Hypodynamic Circulation: CVP guided fluids Decrease preload with furosemide (not hypovolumic) Reduction of afterload improves outcome-Prazosin, nitroprusside, hydralizine, ACE inhibitor � Dobutamine is the best inotrope. � Noradrenaline can be used


THANK YOU
- Slides: 55