Classification Of Chronic Venous Disease rahul gupta History

- Slides: 17
Classification Of Chronic Venous Disease rahul gupta
History n n First anatomic classification in 1941 by Heyerdale & Stalker Widmer & Wandeler 1978 , Duffy 1988 & the ’Revised Vessel Classification’ suggested by Weiss and Weiss 1993 n n n more advanced classifications more complete and categorize the vessels according to their size and appearance in an increasing order However they did not take into account the tests of venous function and relied exclusively on the clinical appearance
n n Sytchev (1985) described a more comprehensive staging approach based on hemodynamic and phlebographic data in combination with clinical findings Reporting Standards in Venous Disease of the Ad Hoc Committee described classifications by anatomic region, by clinical severity, by physical examination and by functional assessment However none of these classifications achieved universal acceptance and widespread use No possibility for meaningful communication about chronic venous disease, and a basis for a more scientific analysis of management alternatives in CVD was missing
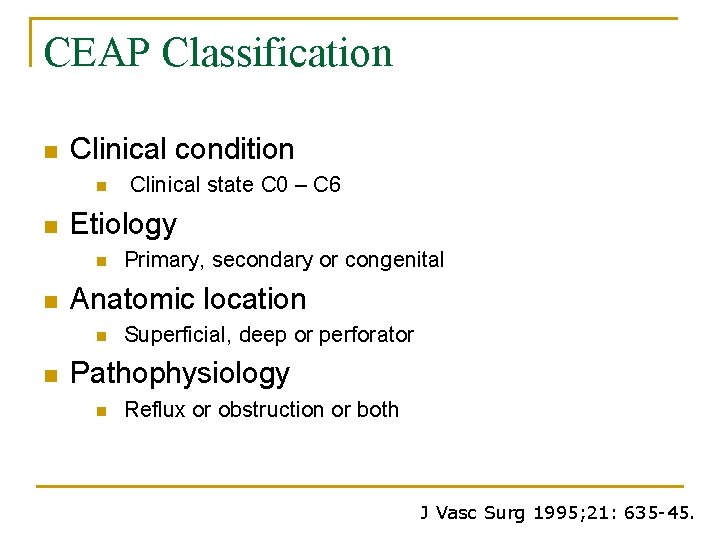
n n International Ad Hoc Committee of the American Venous Forum - consensus document for the classification and grading of chronic venous disease CEAP classification q q (Porter & Moneta 1995) It is intended to be a uniform and simple means for reporting and comparing patients
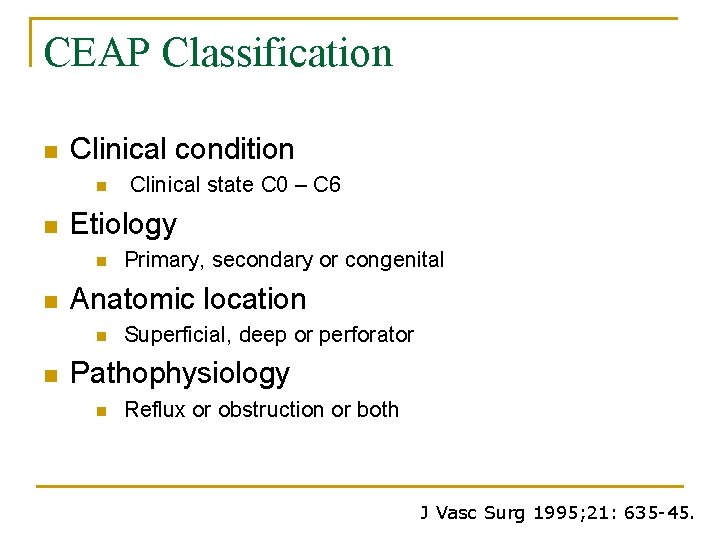
CEAP Classification n Clinical condition n n Etiology n n Primary, secondary or congenital Anatomic location n n Clinical state C 0 – C 6 Superficial, deep or perforator Pathophysiology n Reflux or obstruction or both J Vasc Surg 1995; 21: 635 -45.
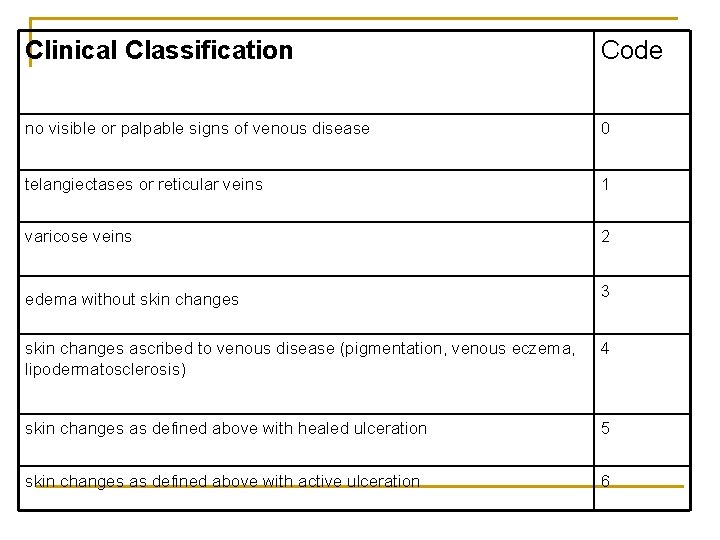
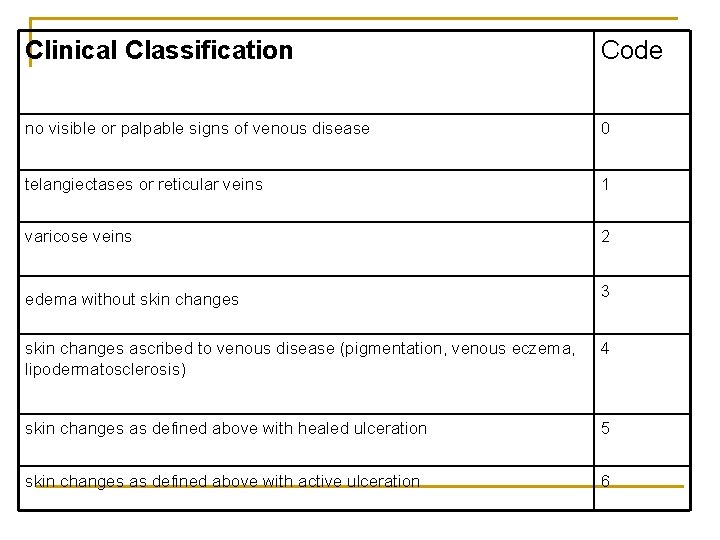
Clinical Classification Code no visible or palpable signs of venous disease 0 telangiectases or reticular veins 1 varicose veins 2 edema without skin changes 3 skin changes ascribed to venous disease (pigmentation, venous eczema, lipodermatosclerosis) 4 skin changes as defined above with healed ulceration 5 skin changes as defined above with active ulceration 6

“Spiders”: Telangiectasia & Venulectasia Reticular Veins Active ulceration VV
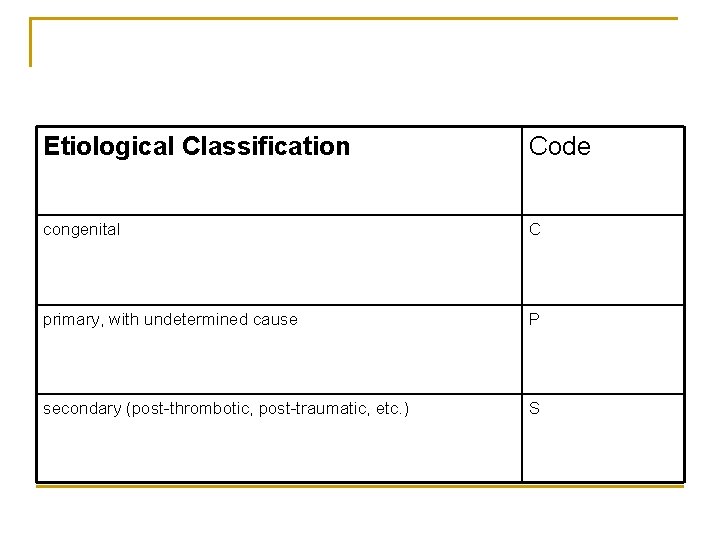
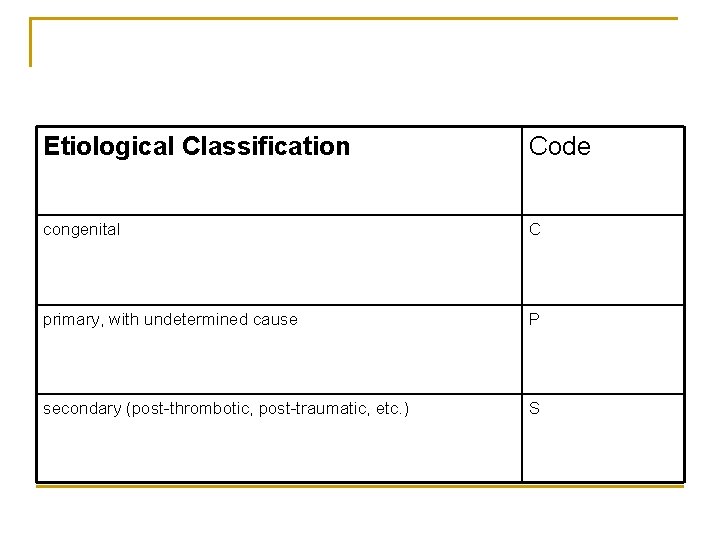
Etiological Classification Code congenital C primary, with undetermined cause P secondary (post-thrombotic, post-traumatic, etc. ) S
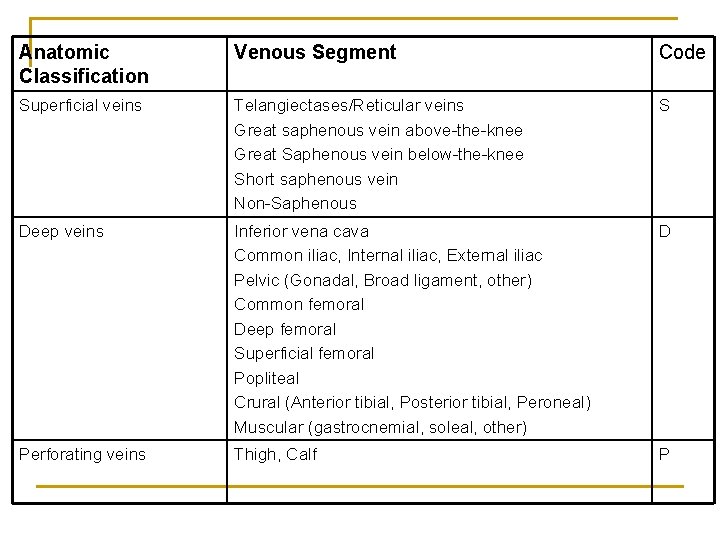
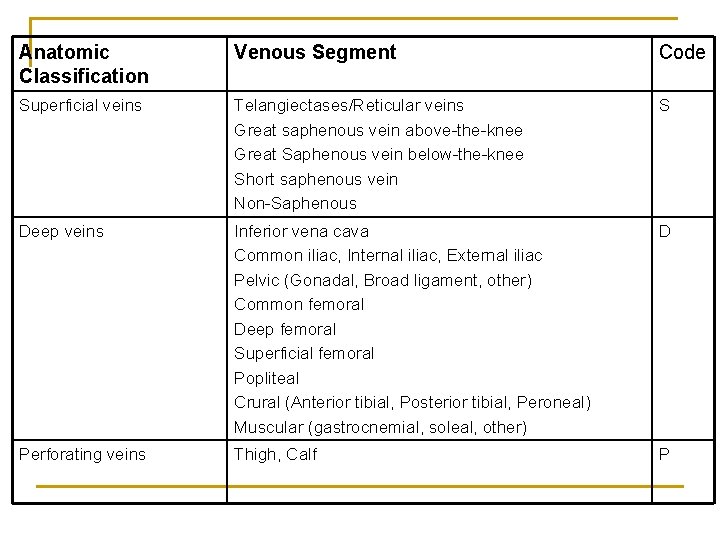
Anatomic Classification Venous Segment Code Superficial veins Telangiectases/Reticular veins Great saphenous vein above-the-knee Great Saphenous vein below-the-knee Short saphenous vein Non-Saphenous S Deep veins Inferior vena cava Common iliac, Internal iliac, External iliac Pelvic (Gonadal, Broad ligament, other) Common femoral Deep femoral Superficial femoral Popliteal Crural (Anterior tibial, Posterior tibial, Peroneal) Muscular (gastrocnemial, soleal, other) D Perforating veins Thigh, Calf P
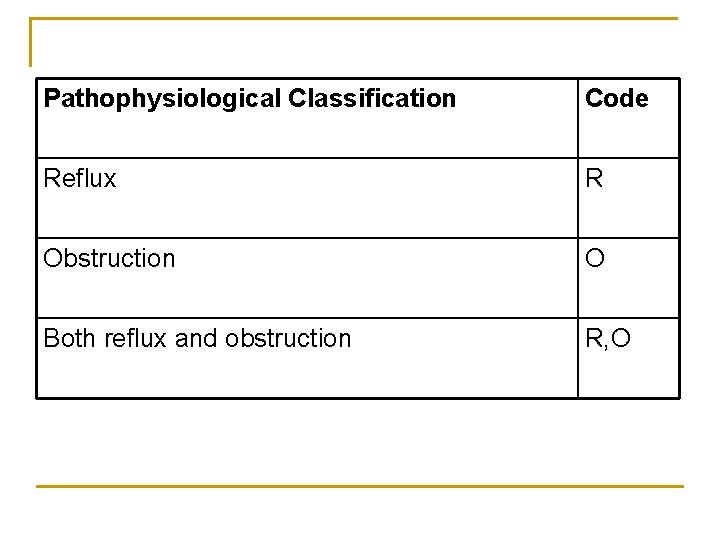
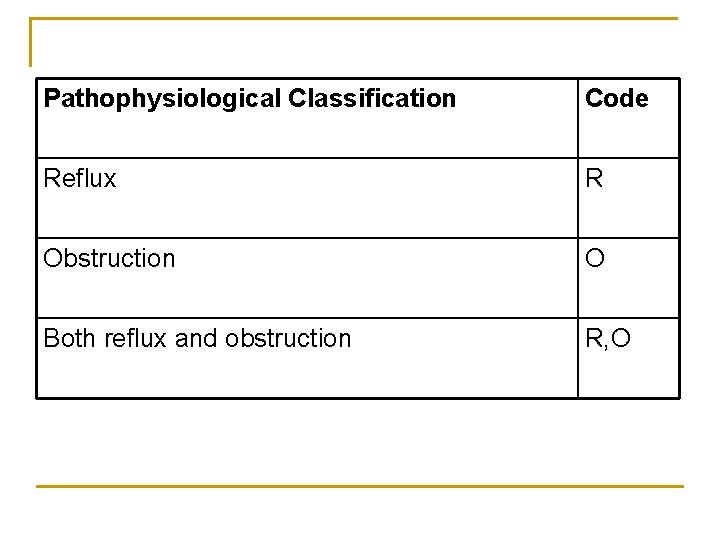
Pathophysiological Classification Code Reflux R Obstruction O Both reflux and obstruction R, O
CEAP designation n n C with clinical class as subscript E with etiological code as subscript A with anatomic code as subscript P with pathophysiological code as subscript
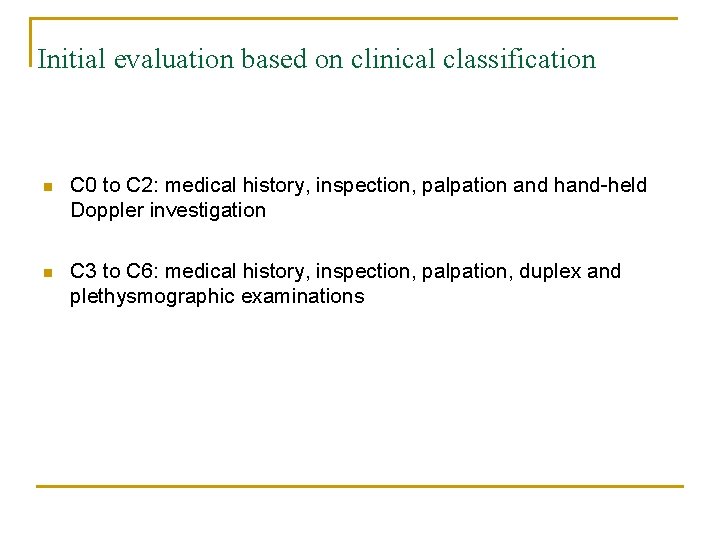
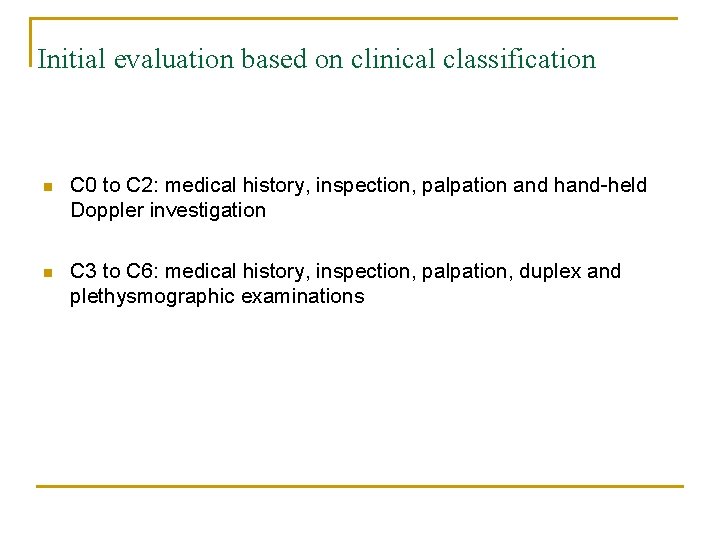
Initial evaluation based on clinical classification n C 0 to C 2: medical history, inspection, palpation and hand-held Doppler investigation n C 3 to C 6: medical history, inspection, palpation, duplex and plethysmographic examinations
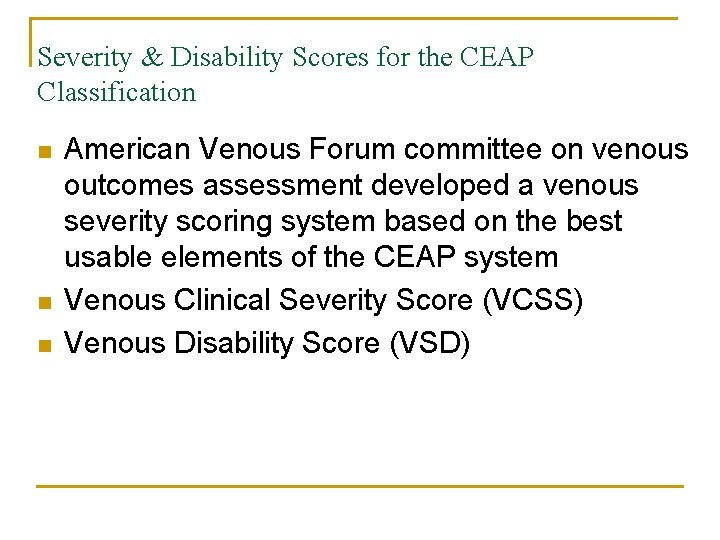
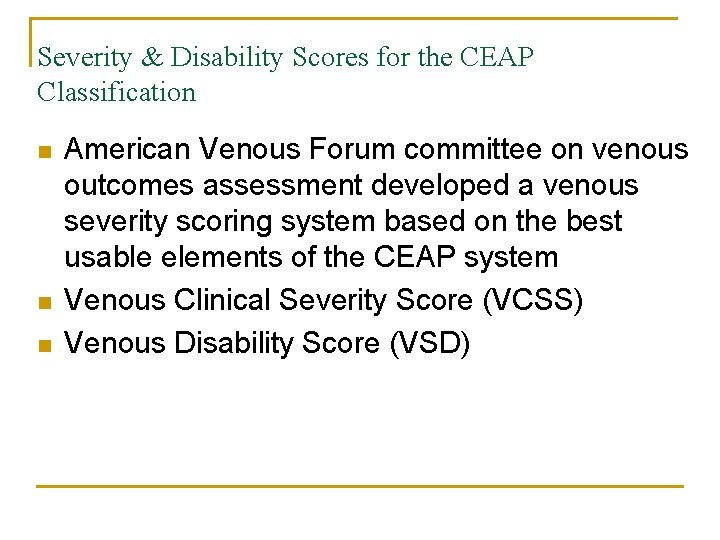
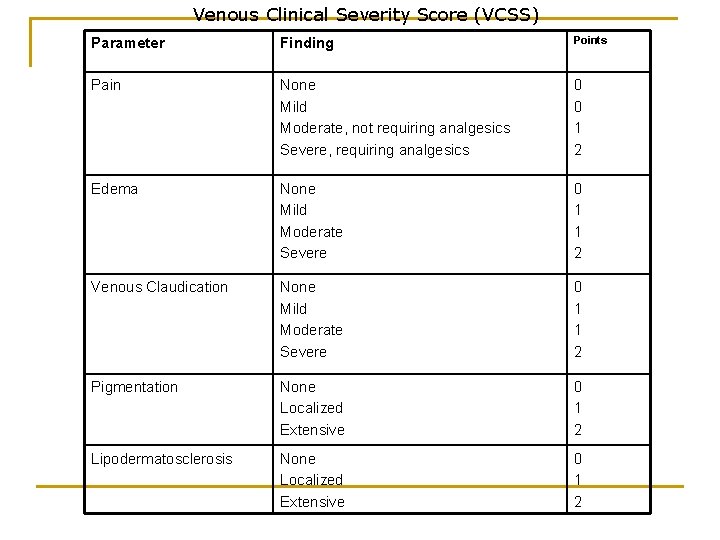
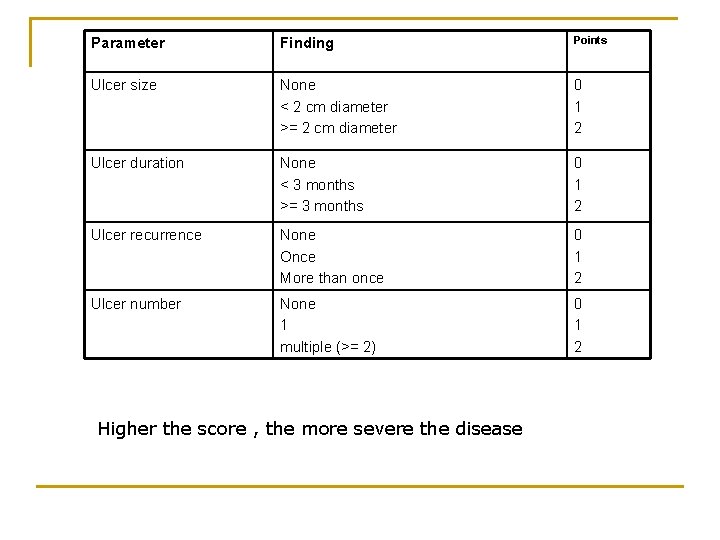
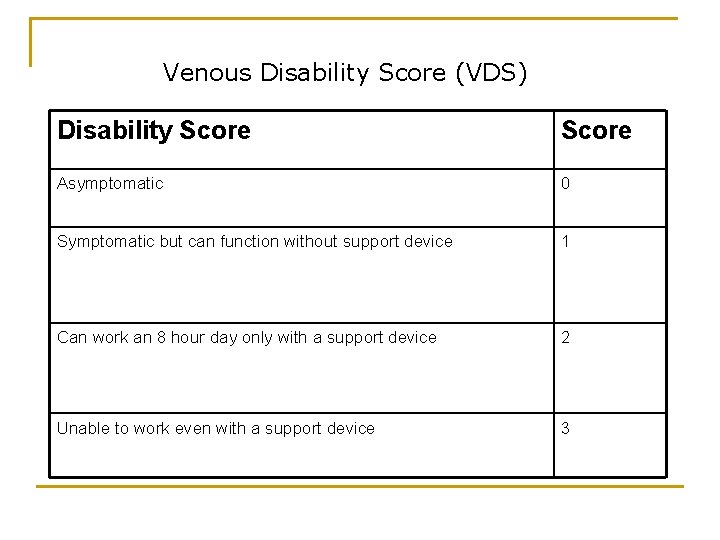
Severity & Disability Scores for the CEAP Classification n American Venous Forum committee on venous outcomes assessment developed a venous severity scoring system based on the best usable elements of the CEAP system Venous Clinical Severity Score (VCSS) Venous Disability Score (VSD)
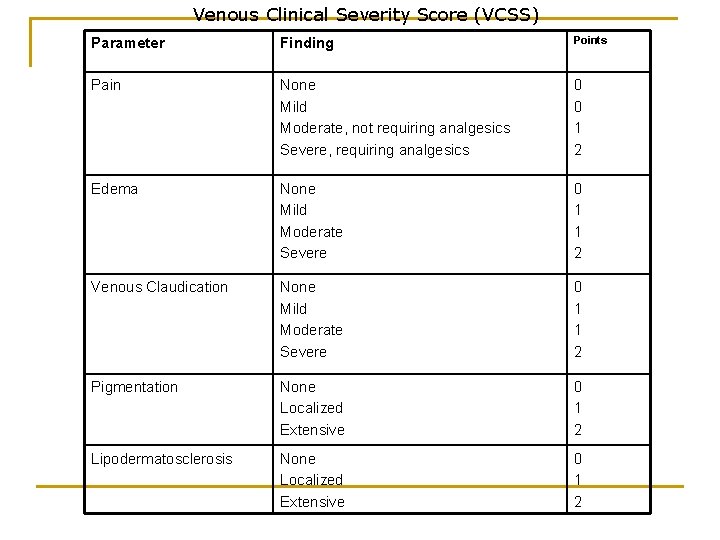
Venous Clinical Severity Score (VCSS) Parameter Finding Points Pain None Mild Moderate, not requiring analgesics Severe, requiring analgesics 0 0 1 2 Edema None Mild Moderate Severe 0 1 1 2 Venous Claudication None Mild Moderate Severe 0 1 1 2 Pigmentation None Localized Extensive 0 1 2 Lipodermatosclerosis None Localized Extensive 0 1 2
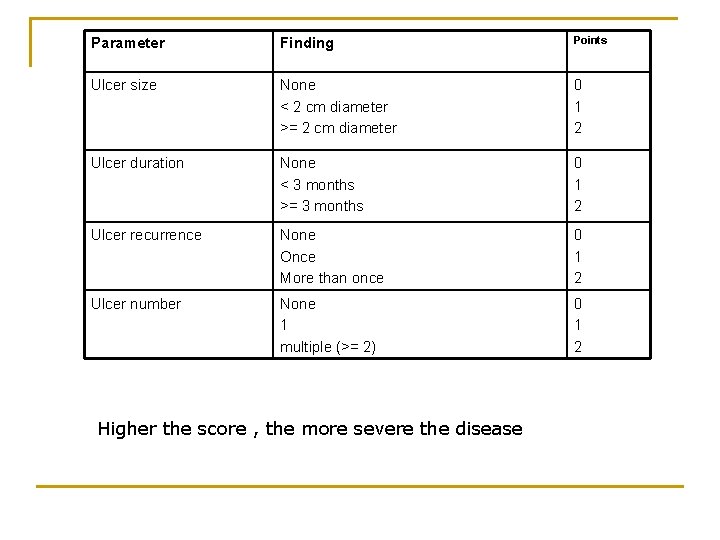
Parameter Finding Points Ulcer size None < 2 cm diameter >= 2 cm diameter 0 1 2 Ulcer duration None < 3 months >= 3 months 0 1 2 Ulcer recurrence None Once More than once 0 1 2 Ulcer number None 1 multiple (>= 2) 0 1 2 Higher the score , the more severe the disease
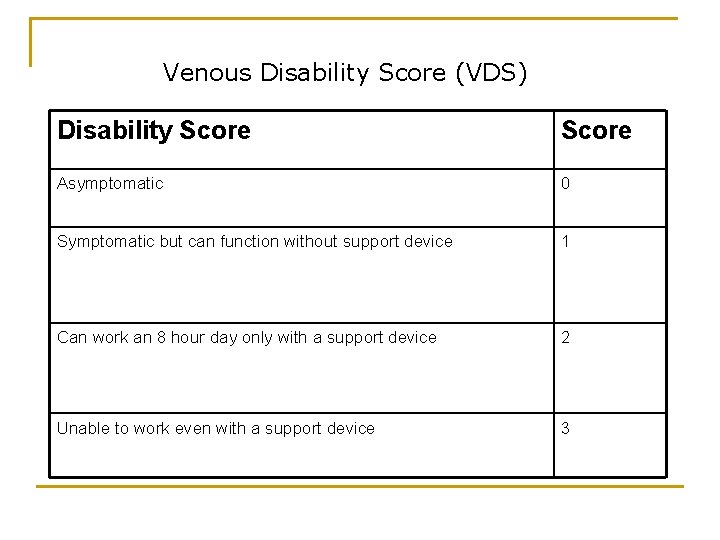
Venous Disability Score (VDS) Disability Score Asymptomatic 0 Symptomatic but can function without support device 1 Can work an 8 hour day only with a support device 2 Unable to work even with a support device 3
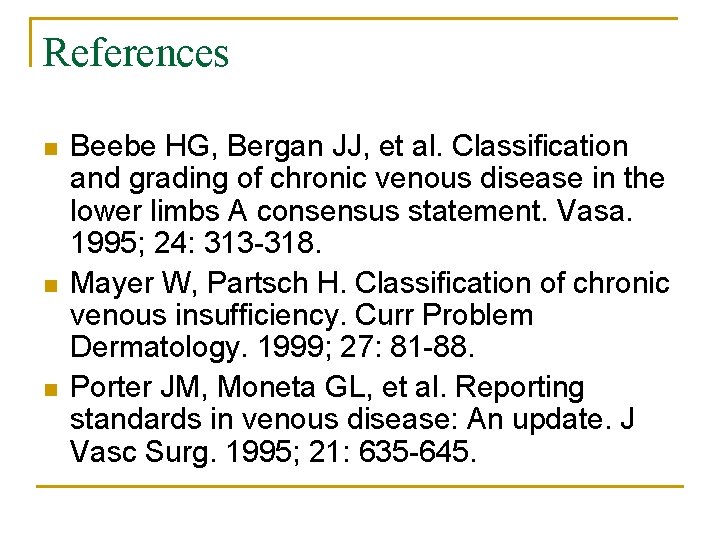
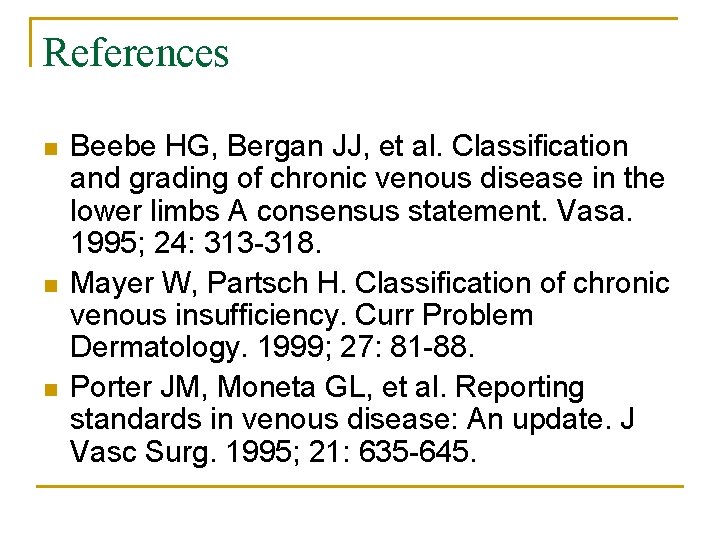
References n n n Beebe HG, Bergan JJ, et al. Classification and grading of chronic venous disease in the lower limbs A consensus statement. Vasa. 1995; 24: 313 -318. Mayer W, Partsch H. Classification of chronic venous insufficiency. Curr Problem Dermatology. 1999; 27: 81 -88. Porter JM, Moneta GL, et al. Reporting standards in venous disease: An update. J Vasc Surg. 1995; 21: 635 -645.