CKD MLLH 17 3 10 Chronic Kidney Disease

- Slides: 31

CKD ML/LH 17. 3. 10
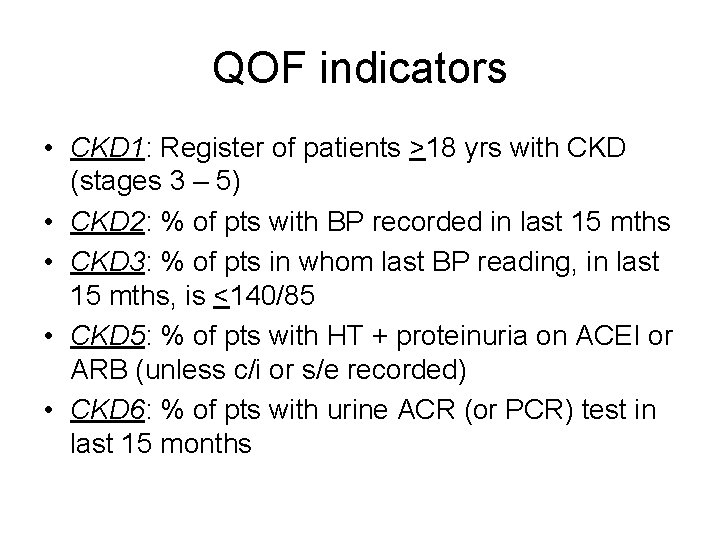
Chronic Kidney Disease • Are we correctly diagnosing CKD? • Have we the correct patients on our CKD register? • Are we managing them correctly?
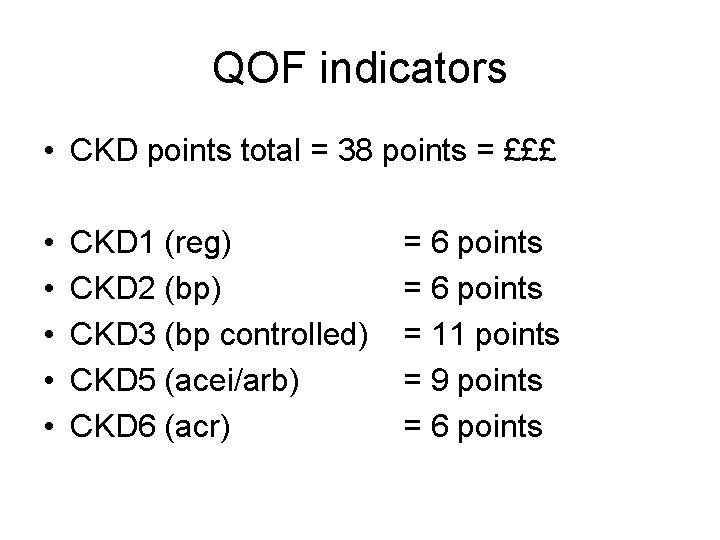
Plan for today Highlight a few issues around e. GFRs Review NICE and PACE guidance Discuss how we diagnose and manage CKD Identify and discuss any uncertain areas
Why introduce CKD QOF indicators? • End stage renal failure is costly to treat, and its prevalence is increasing • 30% of patients present late; they have worse outcomes and are more expensive to treat • It is hoped that managing CVD risk factors aggressively will slow or reduce the progression to ERF
Risks of a low e. GFR Renal • 1% of patients with CKD 3 will progress to ERF in their lifetime (99% won’t) Cardiovascular • If you have an e. GFR <60 you are at higher risk of all cause mortality and any cardiovascular event
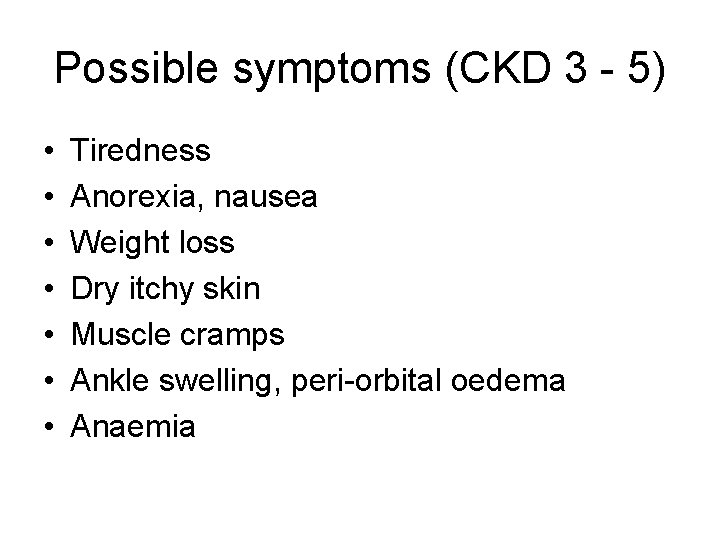
Possible symptoms (CKD 3 - 5) • • Tiredness Anorexia, nausea Weight loss Dry itchy skin Muscle cramps Ankle swelling, peri-orbital oedema Anaemia
NICE Sept 2008, Clinical Guideline 73
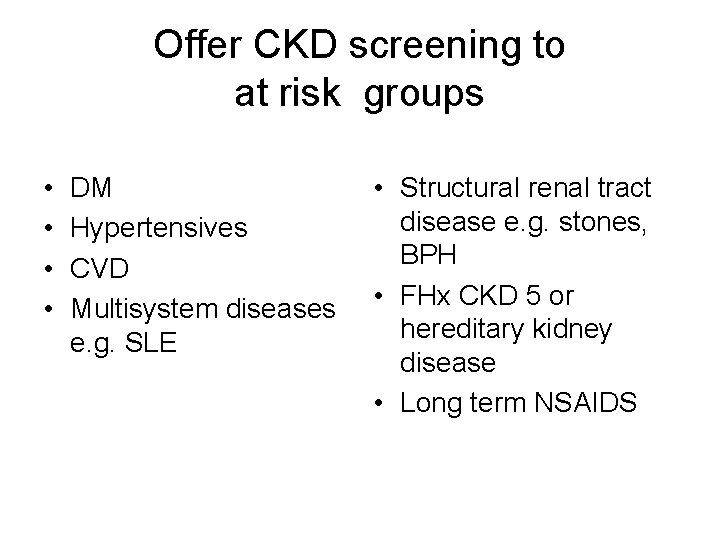
Offer CKD screening to at risk groups • • DM Hypertensives CVD Multisystem diseases e. g. SLE • Structural renal tract disease e. g. stones, BPH • FHx CKD 5 or hereditary kidney disease • Long term NSAIDS
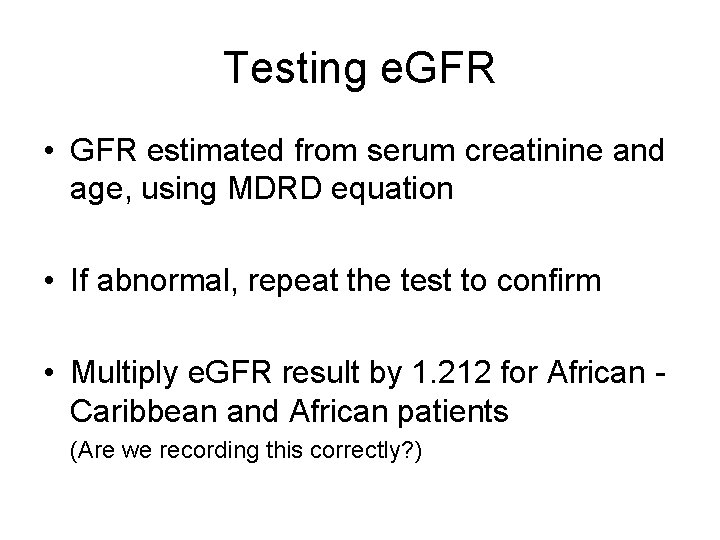
Testing e. GFR • GFR estimated from serum creatinine and age, using MDRD equation • If abnormal, repeat the test to confirm • Multiply e. GFR result by 1. 212 for African Caribbean and African patients (Are we recording this correctly? )
e. GFR and meat • NICE specifically advises no meat for 12 hours before e. GFR • Are we doing this? • How do we record it?
e. GFRs and age • e. GFR is not validated in the >75 s (How many patients >75 have we coded with CKD 3? ) • From the age of 40 the e. GFR declines by 1 ml/min/yr • NICE says that in those >70 yrs with a stable e. GFR >45, there is v little risk of developing CKD related complications.
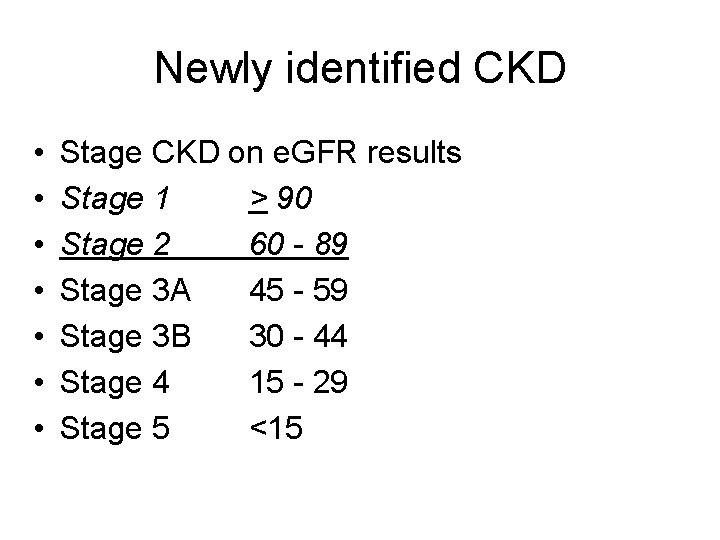
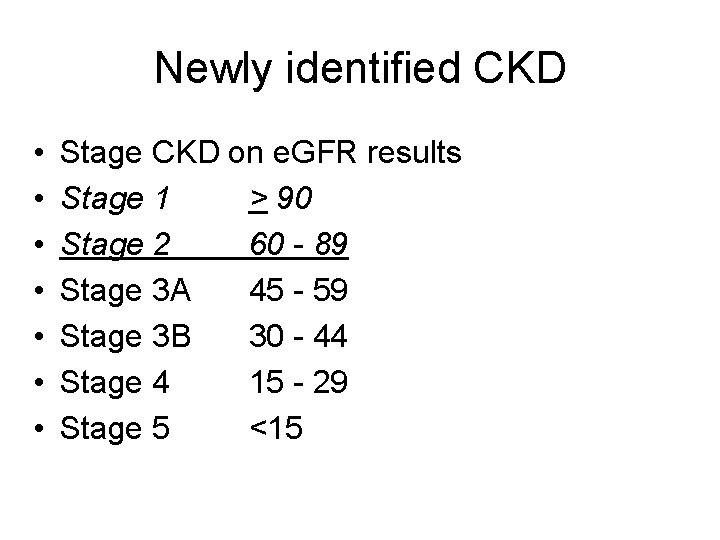
Newly identified CKD • • Stage CKD on e. GFR results Stage 1 > 90 Stage 2 60 - 89 Stage 3 A 45 - 59 Stage 3 B 30 - 44 Stage 4 15 - 29 Stage 5 <15
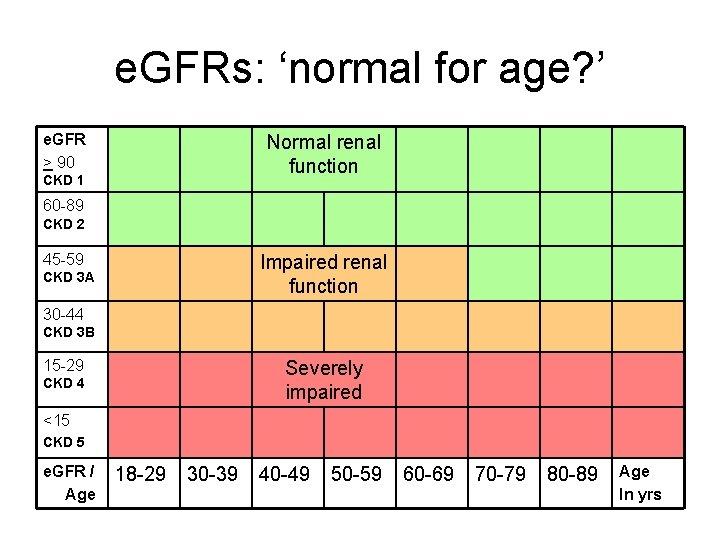
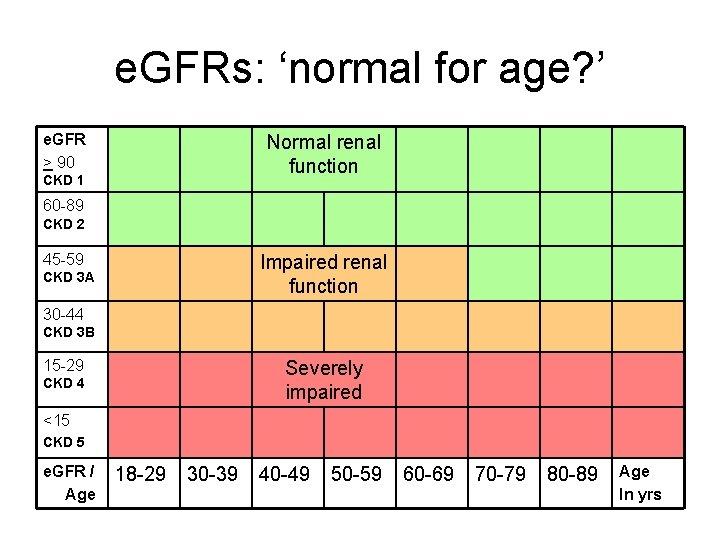
e. GFRs: ‘normal for age? ’ e. GFR > 90 Normal renal function CKD 1 60 -89 CKD 2 45 -59 Impaired renal function CKD 3 A 30 -44 CKD 3 B 15 -29 Severely impaired CKD 4 <15 CKD 5 e. GFR / Age 18 -29 30 -39 40 -49 50 -59 60 -69 70 -79 80 -89 Age In yrs
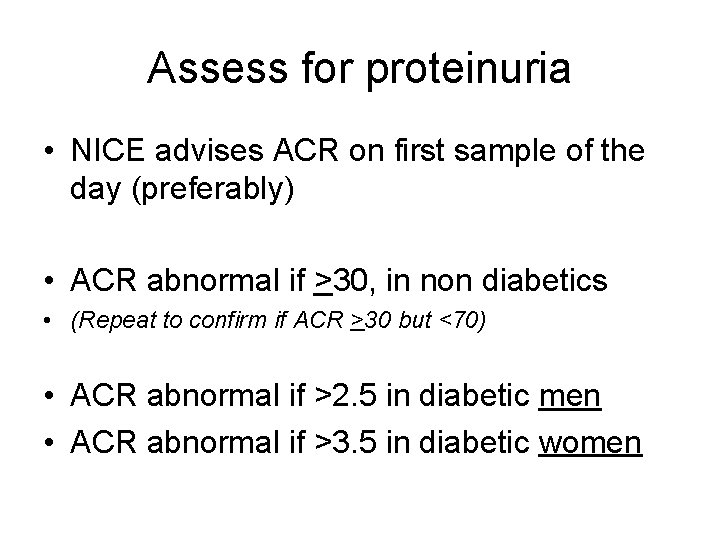
Assess for proteinuria • NICE advises ACR on first sample of the day (preferably) • ACR abnormal if >30, in non diabetics • (Repeat to confirm if ACR >30 but <70) • ACR abnormal if >2. 5 in diabetic men • ACR abnormal if >3. 5 in diabetic women
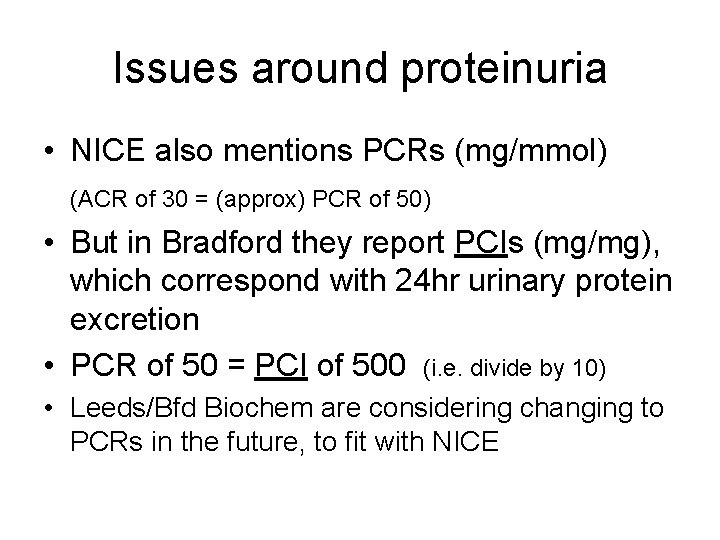
Issues around proteinuria • NICE also mentions PCRs (mg/mmol) (ACR of 30 = (approx) PCR of 50) • But in Bradford they report PCIs (mg/mg), which correspond with 24 hr urinary protein excretion • PCR of 50 = PCI of 500 (i. e. divide by 10) • Leeds/Bfd Biochem are considering changing to PCRs in the future, to fit with NICE
False positives • Urinary Tract Infection Do MSU if dipstix +ve for protein • Menstrual contamination • Benign orthostatic proteinuria
Assess for progressive CKD • Check at least 3 e. GFRs over at least 90 days • Defined as a decline in e. GFR of >5 within 1 year, or >10 within 5 years • Risk factors include NSAIDS, smoking, hypertension, urinary outflow obstruction, proteinuria and diabetes
Other baseline tests For all • Dipstix for haematuria • CVD risk assessment • Consider DEXA scan CKD 4 and 5 • FBC and ferritin • Calcium, phosphate, PTH
Consider renal USS • • • If CKD 4 or 5 Progressive CKD Visible or persistent invisible haematuria Symptoms of urinary tract obstruction FHx polycystic kidney disease and >20 yrs of age
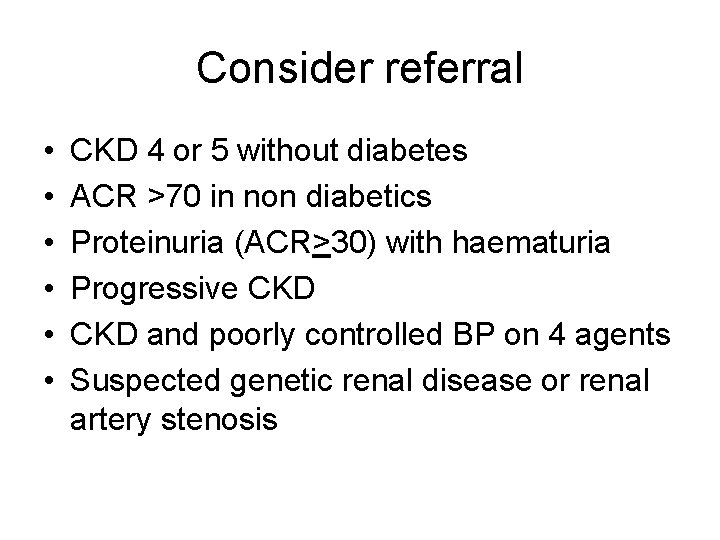
Consider referral • • • CKD 4 or 5 without diabetes ACR >70 in non diabetics Proteinuria (ACR>30) with haematuria Progressive CKD and poorly controlled BP on 4 agents Suspected genetic renal disease or renal artery stenosis
Routine management Lifestyle modification • Smoking increases risk of progressive CKD • Lose weight if obese • Regular exercise • Reduce salt if hypertensive
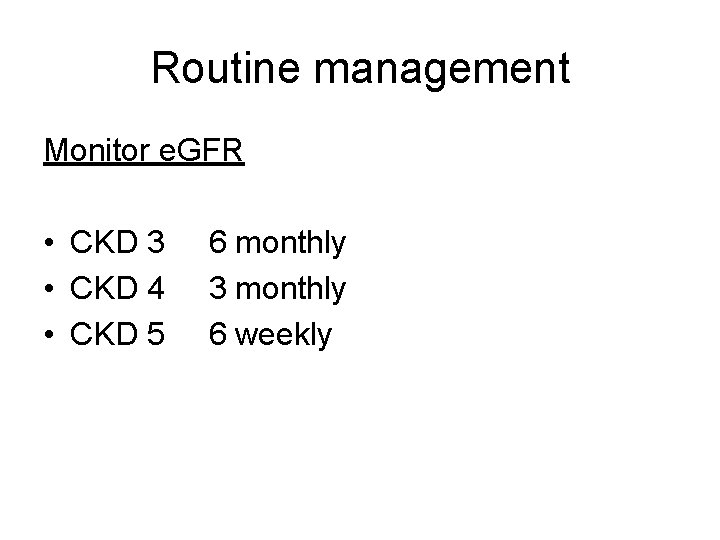
Routine management Monitor e. GFR • CKD 3 • CKD 4 • CKD 5 6 monthly 3 monthly 6 weekly
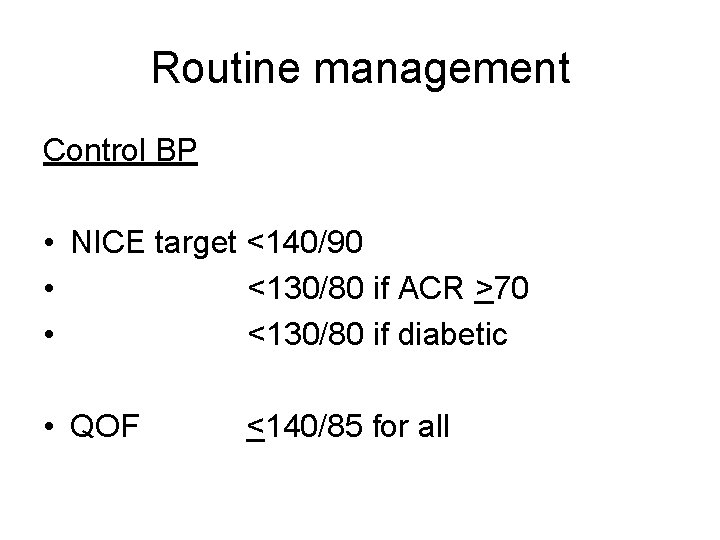
Routine management Control BP • NICE target <140/90 • <130/80 if ACR >70 • <130/80 if diabetic • QOF <140/85 for all
Routine management Reduce proteinuria • ACEIs first line • ARBs if not tolerated
Routine management ACEI or ARB: • Diabetes + ACR (>2. 5 men, or 3. 5 women) (irrespective of hypertension or CKD stage) • Non-Diabetic with CKD + HT + ACR >30 • Non-Diabetic with CKD + ACR >70 (irrespective of presence of HT or CVD)
Routine management Routine anti-hypertensive treatment • Non-diabetic + CDK + HT + ACR <30 (See NICE Hypertension guideline 34)
Routine management CVD risk assessment • treat with a statin if CVD risk >20% (Systm. One CVD risk calculator does NOT include adjustment for chronic renal disease, but QRISK 2 does) Immunizations • Influenza - annually • Pneumococcal - 5 yearly, due to declining antibody levels
Routine management Drugs • Check BNF Appendix 3: Renal Impairment Test for anaemia • If Hb <11 first consider other causes of anaemia • Determine iron status – if serum ferritin <100 start oral iron • Consider referral for erythropoeisis stimulaing agents (ESA’s)
Routine management Manage bone conditions • Ca, PTH and phosphate if CKD 4 or 5 • Offer biphosphonates to all “if indicated” • If indicated offer vitamin D supplements: - cholecalciferol or ergocalciferol in CKD 3 - alfacalcidol or calcitriol in CKD 4 and 5 • If on vit D supplements they need to be monitored
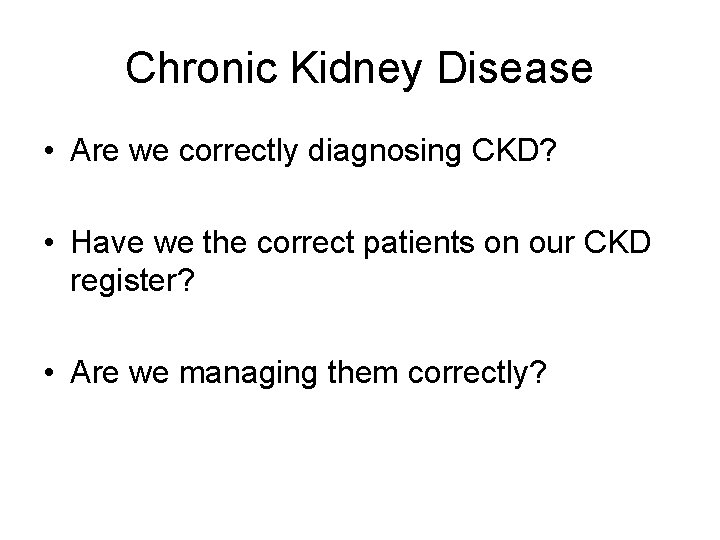
QOF indicators • CKD 1: Register of patients >18 yrs with CKD (stages 3 – 5) • CKD 2: % of pts with BP recorded in last 15 mths • CKD 3: % of pts in whom last BP reading, in last 15 mths, is <140/85 • CKD 5: % of pts with HT + proteinuria on ACEI or ARB (unless c/i or s/e recorded) • CKD 6: % of pts with urine ACR (or PCR) test in last 15 months
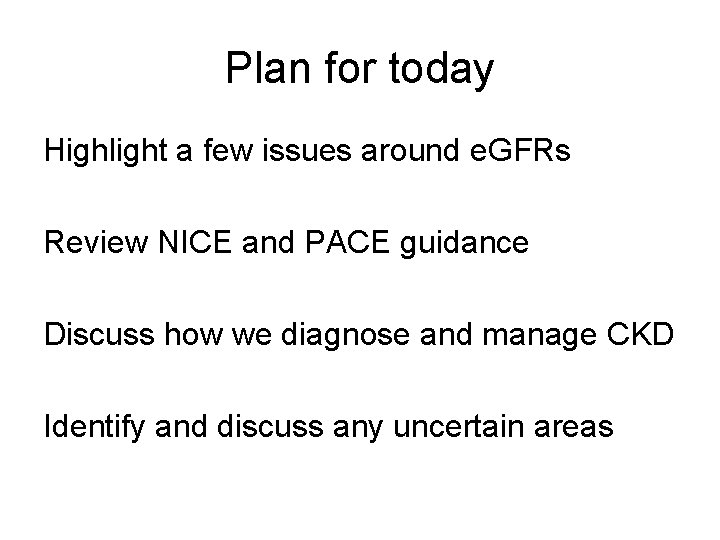
QOF indicators • CKD points total = 38 points = £££ • • • CKD 1 (reg) CKD 2 (bp) CKD 3 (bp controlled) CKD 5 (acei/arb) CKD 6 (acr) = 6 points = 11 points = 9 points = 6 points